Beruflich Dokumente
Kultur Dokumente
Mds Sle
Hochgeladen von
Anonymous plYGwXOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Mds Sle
Hochgeladen von
Anonymous plYGwXCopyright:
Verfügbare Formate
Hematology Reports 2016; volume 8:6480
Autoimmune syndromes pre- and progression.8 Autoimmune (AI) symptoms
have been reported in up to 10-30% of MDS Correspondence: Heather A. Leitch, St. Paul’s
senting as a paraneoplastic patients.9-11 Patients with AI disorders or Hospital and the University of British Columbia,
manifestation of myelodysplas- receiving immunosuppressive agents are more 440-1144 Burrard Street, Vancouver V6Z 2A5, BC,
likely to be diagnosed with MDS.12 Canada.
tic syndromes: clinical features, Tel.: +1.604.684.5794 - Fax: +1.604.684.5705.
Paraneoplastic inflammatory syndromes
course, treatment and outcome concomitant with MDS diagnosis have also E-mail: hleitch@providencehematology.com
been reported.9,13-15 To better understand the Key words: Autoimmune; myelodysplastic syn-
Bradley T. Williamson,1 Lynda Foltz,2 incidence and outcomes of patients with MDS dromes; HDS.
Heather A. Leitch2 and AI disorders, we conducted a retrospective
Departments of 1Medicine and chart review of patients with MDS, looking for Contributions: BTW reviewed the charts and
2Hematology, St. Paul’s Hospital and the symptoms of AI disorders. wrote the paper; LMF, critically revised the paper;
HAL, supervised the chart review, revised the
University of British Columbia,
paper and performed statistical analyses.
Vancouver, BC, Canada
Conflict of interest: BTW was supported by a
Materials and Methods Summer Studentship from Celgene. LMF has
consulted for Novartis and Janssen; has received
Abstract Myelodysplastic syndromes patients were research funding from Novartis, Incyte, Gilead
identified from a single-center MDS database. and Promedior; and has received honoraria from
Charts were reviewed for the presence of Novartis. HAL has received research funding and
Autoimmune manifestations (AIM) are honoraria from Novartis, Celgene and Alexion;
reported in up to 10-30% of myelodysplastic syn- autoimmune manifestations (AIM) within a 3-
has received an educational grant from Celgene;
dromes (MDS) patients; this association is not year period prior to or following the diagnosis
and is a member of the Exjade Speaker’s Bureau.
well defined. We present herein a retrospective of MDS, treatment and outcome. Patients with
chart review of single center MDS patients for a longstanding history of connective tissue dis- Poster presentation: Norman Bethune
AIM, a case discussion and a literature review. orders were excluded. The term culture nega- Symposium, Vancouver, BC, November 13, 2014.
Of 252 MDS patients examined, 11 (4.4%) had tive sepsis was used to describe fevers or Canadian Conference on MDS, Banff, AB,
drenching sweats with a negative workup for September 12-13, 2014.
AIM around MDS diagnosis. International
infectious and other causes such as drug
Prognostic Scoring System scores were: low or Received for publication: 20 February 2016.
fevers. Although these symptoms may be a
intermediate (int)-1 (n=7); int-2 or high (n=4). Revision received: 30 April 2016.
manifestation of systemic vasculitis, the latter
AIM were: culture negative sepsis (n=7); Accepted for publication: 2 May 2016.
term was reserved for patients with biopsy-
inflammatory arthritis (n=3); vasculitis (n=4);
proven vasculitis. Cases that are illustrative of This work is licensed under a Creative Commons
sweats; pericarditis; polymyalgia rheumatica
AIM were selected for presentation. Attribution-NonCommercial 4.0 International
(n=2 each); mouth ulcers; pulmonary infil- License (CC BY-NC 4.0).
Survival analyses were conducted by the log-
trates; suspicion for Behcet’s; polychondritis
rank method using SPSS for Windows, version ©Copyright B.T. Williamson et al., 2016
and undifferentiated (n=1 each). AIM treat-
20. This review was conducted in accordance Licensee PAGEPress, Italy
ment and outcome were: prednisone +/- steroid
with the requirements of the institutional Hematology Reports 2016; 8:6480
sparing agents, n=8, ongoing symptoms in 5;
Research Ethics Board. doi:10.4081/hr.2016.6480
azacitidine (n=3), 2 resolved; and observation,
n=1, ongoing symptoms. At a median follow up
of 13 months, seven patients are alive. In sum- period of more than 7 years. Two patients had
mary, 4.4% of MDS patients presented with con- ferritin levels done; the maximum level was
Results 1200 ng/mL. None of the patients had
comitant AIM. MDS should remain on the differ-
ential diagnosis of patients with inflammatory splenomegaly on physical examination, and
Of 252 MDS patients, eleven (4.4%) had AIM one underwent CT scanning of the abdomen
symptoms.
presenting at or shortly before MDS diagnosis. because of abdominal pain; the spleen was
Baseline and MDS characteristics, treatment normal on imaging.
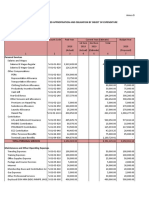
and outcome are shown in Table 1. Eight At a median follow up of 13 (4-87) months,
patients were documented to have had a
Introduction seven patients are alive, six with stable MDS
workup by the rheumatology service, and
and one is undergoing allogeneic myeloabla-
seven were followed regularly by rheumatol-
The myelodysplastic syndromes (MDS) are tive hematopoietic stem cell transplantation
ogy; all rheumatology-assigned diagnoses of
clonal hematopoietic disorders of ineffective (HSCT). Four patients died; causes were: MDS
autoimmune diseases are listed in Table 1.
hematopoiesis and risk of acute myeloid Of seven patients with culture negative sep- progression, n=2; infection, n=1; and
leukemia (AML) progression.1 Prognosis is sis, all underwent an extensive workup for unknown, n=1.
determined by the International Prognostic infectious causes, five by the Infectious Of four patients with int-2 or high IPSS risk
Scoring System (IPSS) and other scores.2 Diseases service. Three received intravenous MDS, three were treated with azacitidine. One
Mutations in the pluripotent hematopoietic antibiotics with no improvement. Other causes patient receiving azacitidine did not respond,
stem cell occur in MDS, with disruption of RNA of fevers, such as medications, were consid- there was one early infectious death, and the
splicing, ribosomal proteins, telomeres, ered but none identified. All seven had at least third is undergoing HSCT.
microRNA expression, and DNA methylation.3-6 one bone marrow aspirate and biopsy per- Overall survival (OS) analyses were per-
Reports suggest an association between MDS formed during a symptomatic episode, with no formed comparing MDS patients with AIM to
and immune dysregulation.7 Cytokine dysregu- hemophagocytosis seen. Four of these patients those without AIM. The OS of seven lower IPSS
lation and impaired cellular immunity have had 3 bone marrows performed, and one had risk patients with AIM were compared to 204
been noted in MDS initiation, development, more than ten done in two countries over a lower risk MDS diagnosed over the same time
[Hematology Reports 2016; 8:6480] [page 23]
Case Report
period. The median follow up of all lower risk Table 1. Autoimmune manifestations of myelodysplastic syndromes in 11 patients: clini-
patients was 27.3 (0.5-161) months. There was cal features, treatment and outcome.
no significant difference in OS between
Characteristic N (%) /Median (range)
groups; all seven (100%) patients with AIM are
alive compared to 166 (78.7%) patients with- Age (years) 68 (34-84)
out AIM, and the median OS was not reached Gender (male) 7 (64)
at 43 months compared to 78.8 months, respec- FAB* or WHO MDS diagnosis
tively (P=NS). RCUD 2
Of higher IPSS risk patients, we restricted RCMD-RS 2
the analysis to patients diagnosed since azaci- RA 1
tidine was available in Canada and compared RARS 1
three patients with AIM receiving azacitidine RCMD 1
RAEB-t° 1
to 29 patients without AIM, but also receiving MDS-NOS 1
azacitidine. The median follow up of this group CMML-2 1
was 7.3 (0.5-46) months. There was no signif- IPSS risk
icant difference in OS between groups Low 3
(P=NS). Intermediate-1 4
Of eight patients receiving immunosuppres- Intermediate-2 3
sion for AIM, one died of AML progression at 4 High 1
months, one died of progressive (higher IPSS IPSS cytogenetics group
risk) MDS in the context of stopping azaciti- Good 6
dine at 6 months, and one died suddenly of Intermediate 2
Poor 3
unknown causes 32 months from MDS diagno-
Significant conditions
sis. The remaining five patients had stable
No 8
MDS at a median of 14 (5-23) months from Yes# 3
MDS diagnosis. Four of these patients were
MDS treatment
followed by Rheumatology and the fifth was Observation 5
given immunosuppressive medications by Supportive care§ 3
emergency room physicians for pericarditis. Azacitidine 3
Both patients with systemic vasculitis had this MDS outcome
diagnosis made on biopsy, one on open lung Stable 6
biopsy, and one on skin biopsy. Only one Good response 1
patient, without biopsy proven vasculitis but Died^ 4
with culture negative sepsis, had anti-neu- Autoimmune manifestation (AIM)
trophil cytoplasmic antibody (ANCA) levels Culture negative sepsis 7
Inflammatory arthritis 3
done, which were negative. Systemic vasculitis 2
Cutaneous vasculitis 1
Patient #1 Polymyalgia rheumatica 2
A 31 year-old woman presented with fatigue Connective tissue disorder NOS 2
and cytopenias. White blood cell (WBC) count Polychondritis 1
Pericarditis 2
was 3.9×109/L, neutrophils 1.8×109/L, hemo-
globin (Hb) 125 g/L and platelet count (PLTS) AIM months in relation to MDS diagnosis 1 (-38-34)
100×109/L. Peripheral blood morphology Serological abnormalities
showed macrocytosis. Antinuclear antibody Positive ANA 6
Elevated CRP 5
(ANA) was positive at a 1:320 dilution. She did Elevated ESR 2
not fulfill criteria for systemic lupus erythe- Monoclonal paraprotein 1
matosus (SLE) and was observed. Neutropenia Positive RF 1
and thrombocytopenia persisted and mild ane- AIM treatment
mia developed (Hb 119 g/L). A bone marrow Observation 3
aspirate and biopsy (BMBx) showed erythroid Prednisone 8$
Methotrexate 4
dysplasia, 1% blasts and trisomy 8. A diagnosis Hydroxychloroquine 4
of refractory cytopenia with unilineage dyspla- Azathioprine 2
sia (RCUD) was made and the IPSS was int-1. Gold 1
The patient declined HSCT and yearly BMBx’s Chlorambucil 2
remained stable. Within one year of MDS diag- Dapsone 1
nosis, she developed a rash to sun exposure. AIM outcome
She experienced culture negative fevers and Resolution of all symptoms 3
mouth ulcers suspicious for Behcet’s disease. Partial resolution of symptoms 4
Persistent symptoms 4
Symptoms are ongoing 9.75 years from MDS ANA, anti-nuclear antibody; CMML; chronic myelomonocytic leukemia; CRP, C-reactive protein; EB-t; excess blasts in transformation; ESR, ery-
diagnosis despite the use of non-steroidal anti- throcyte sedimentation rate; FAB, French-American-British; IPSS, International Prognostic Scoring System; MD, multilineage dysplasia; MDS,
myelodysplastic syndrome; NOS, not otherwise specified; RA, refractory anemia; RS, ring sideroblasts; RF, rheumatoid factor; t-, treatment
inflammatory medications. AIM nearly com- related; UD, Unilineage dysplasia. *According to era of MDS diagnosis; °t-MDS; #myasthenia gravis and systemic lupus erythematosus; psoriatic
pletely abated during three pregnancies. arthritis, polychondritis and vasculitis; well-controlled HIV infection; n=1 each. The course of the HIV-positive patient has been published in
detail (Williamson BT & Leitch HA, 2016). §Erythropoietin, n=2; red blood cell transfusions + iron chelation therapy, n=1. ^MDS progression,
n=2; complications of treatment, n=1; unknown cause, n=1. $7 in combination with other agents.
[page 24] [Hematology Reports 2016; 8:6480]
Case Report
Patient #2 ty and remained non-diagnostic. Cytogenetic months compared to 9 months in patients with
analysis was normal male karyotype. Eight AIM.9 Acute vasculitis had a particularly poor
A 77 year-old man presented with fatigue. months from the second BMBx, the diagnosis prognosis, with a median survival of only 6
Hb was 127 g/L, neutrophils 1.8×109/L, and was amended to MDS following a review of the months. However, this study did not take into
PLTS 133×109/L. ANA titer was 1:80. A BMBx previous BMBx at our center. The IPSS was low account the IPSS score. In another study that
showed trilineage dysplasia, <5% blasts and a risk. Five months later, a third BMBx indicated considered IPSS score and treatment, patients
normal male karyotype. A diagnosis of refracto- no MDS progression, and cytogenetics with AIM (n=13) did not have an inferior prog-
ry cytopenia with multilineage dysplasia and remained normal. nosis to those without (n=57).10 We separated
ring sideroblasts (RCMD-RS) was made and This patient has ongoing arthritic symp- our patients into lower IPSS risk, and higher
the IPSS was int-1. toms. Following 15 months of treatment with risk receiving azacitidine, and compared the
Six months after MDS diagnosis he devel- immunosuppressive medications, culture neg- outcomes of those with and without AIM. In
oped progressive stiffness of the thighs, shoul- ative fevers have not recurred. both instances we did not find a significant dif-
ders and neck. Workup revealed a positive
ference in OS between groups, though small
rheumatoid factor (RF), C-reactive protein Patient #5
numbers limits interpretation of these analy-
(CRP) of 44.2 mg/L (>7 mg/L indicates inflam-
A 39-year-old man presented with drenching ses. Supportive treatment of AIM in MDS
mation) and erythrocyte sedimentation rate
sweats and chest pain, the latter diagnosed as requires careful consideration, as immunosup-
(ESR) of 34 mm/hr (upper limit of normal 10
pericarditis and treated with aspirin and pressive medications (ISM) may increase
mm/hr). He was diagnosed with rheumatoid
colchicine. One week later, he developed infectious risk and exacerbate cytopenias. In
arthritis (RA) with a polymyalgia rheumatica
abdominal pain suspicious for Behcet’s dis- one study, however, 26 of 27 of MDS patients
(PMR)-type onset. He received 40 mg pred-
ease. A CBCD revealed a Hb of 110 g/L and a with AIM responded favorably to ISM but only 6
nisone daily with near complete resolution of
leukoerythroblastic picture. WBC count was experienced sustained AIM remission.27 There
symptoms, and was transitioned to hydroxy-
5.9×109/L, neutrophils 1.1×109/L, PLTS are reports of MDS progression with immuno-
chloroquine and methotrexate.
decreased (count unavailable due to clump- suppression,28 but on the other hand, immuno-
Patient #3 ing). A BMBx showed multilineage dysplasia, suppressive therapy such as anti-thymocyte
ring sideroblasts, 4% blasts and a complex globulin (ATG) and cyclosporine may result in
A 70 year-old man presented with a Hb of 82 karyotype. A diagnosis of RCMD-RS was made
g/L. A BMBx showed erythroid dysplasia with responses in some MDS patients.7 Given the
and the IPSS was int-2. He was initiated on uncertain safety of ISM for the treatment of
ring sideroblasts, no increase in blasts, and azacitidine. Four months later, he developed
deletion of chromosome 7. A diagnosis of AIM in MDS, these medications should be used
culture-negative sepsis, three episodes in with caution and patients monitored closely.
refractory anemia with ring sideroblasts total. He also had a widespread, recurrent
(RARS) was made and IPSS was int-1. He Treatment of MDS may improve AIM. In one
petechial rash without significant thrombocy-
received blood transfusion support. series of 22 patients with AIM receiving azaci-
topenia. A second BMBx one month after cycle
For 12 months prior to MDS diagnosis, he tidine for MDS, 19 (86%) had an AIM response
two of azacitidine showed no MDS progres-
experienced intermittent swelling around the within 3-6 azacitidine cycles, allowing discon-
sion. He received four cycles of azacitidine in
eyes and ears, fatigue and arthralgias. Five tinuation of ISM.29 Azacitidine is thought to
total with hematologic improvement in all lin-
months after MDS diagnosis, he developed a act in this regard by increasing the number of
eages. He continues to suffer from fatigue and
skin rash; biopsy showed leukocytoclastic vas- FOXP3+ regulatory T-cells and inhibiting
episodes of pericarditis; however, the other
culitis. He received 50 mg prednisone daily, CD4+ T-cells.13,30
symptoms abated. He is undergoing HSCT.
with marked improvement, allowing a taper to In six patients with AIM in MDS relapsed or
10 mg daily, which controlled symptoms. He refractory to steroid treatment, 5 had a
died suddenly thirty-two months from MDS response to lenalidomide, with 3 complete
diagnosis. Discussion and Conclusions remissions.31 There are reports, however,
implicating lenalidomide in increased AIM.32
Patient #4 Lenalidomide modulates the function of NK
Reports suggest an association between AI
A 66 year-old man presented with pancy- manifestations and MDS, including: acute sys- cells, monocytes, dendritic cells, and T-cells,
topenia. WBC count was 2.5×109/L, neutrophils temic vasculitis; chronic AI syndromes; con- and increases cytokines involved in attenuat-
0.3×109/L, Hb 129 g/L, and PLTS 143×109/L. nective tissue disorders; immune-mediated ing inflammatory responses.25,26
The ANA was 1:160. A BMBx was non-diagnos- cytopenias; and serological abnormalities.9,13- The findings in our patients are consistent
tic. Five months later, he developed widespread 21 Inflammatory syndromes may precede or fol- with other reports, with AIM occurring con-
myalgias and swelling of the hands. He was low the diagnosis of MDS.9,19,22 comitant with MDS diagnosis in 4.4%, in
diagnosed with PMR and inflammatory arthri- Cytokines implicated in MDS include tumor patients with a median age of 68 years, 9 of 11
tis not otherwise specified (NOS). Six months necrosis factor alpha (TNF-a) and transform- having adverse karyotype, and present in all
later, he developed hyperkeratotic patches on ing growth factor beta (TGF-b), which result in IPSS risk groups.9-11,16,33 Though this percent-
the scalp and hands. Skin biopsies showed a upregulation of proinflammatory and myelo- age is lower than in previous reports, we
connective tissue disorder NOS. The diagnosis suppressive cytokines, respectively.23,24 restricted the analysis to patients presenting
was amended to mixed connective tissue dis- Interferon regulatory factor-1 (IRF-1) is with AIM around the time of MDS diagnosis
order, and he received azathioprine, hydroxy- involved in activities including inflammatory and excluded patients with longstanding
chloroquine and prednisone. Five months responses, and IRF mRNA was increased in autoimmune disorders.
later, the ESR was 64 mm/hr. MDS patients with AIM.10 Immune cells that In conclusion, MDS should remain on the
Three months later, he experienced three may be involved in AIM include natural killer differential diagnosis of patients undergoing
episodes of culture negative sepsis. After an (NK) cells and regulatory T-cells.25,26 work up for AIM. Similarly, MDS patients with
additional two months, dysplastic features in The prognostic impact of AIM in MDS is a AIM should be identified as symptoms may
neutrophil precursors were seen. A repeat matter of debate. In one study, the median sur- respond to therapy with immunosuppressive
BMBx showed <1% blasts, increased cellulari- vival of MDS patients with no AIM was 25 medications or specific MDS treatments.
[Hematology Reports 2016; 8:6480] [page 25]
Case Report
12. Anderson LA, Pfeiffer RM, Landgren O, et clues to the pathophysiology of MDS? Br J
References al. Risks of myeloid malignancies in Haematol 2008;140:444-53.
patients with autoimmune conditions. Br J 24. Zhou L, Nguyen AN, Sohal D, et al.
1. Ades L, Itzykson R, Fenaux P. Cancer 2009;100:822-8. Inhibition of the TGF-beta receptor I
Myelodysplastic syndromes. Lancet 13. Frietsch JJ, Dornaus S, Neumann T, et al. kinase promotes hematopoiesis in MDS.
2014;383:2239-52. Paraneoplastic inflammation in myelodys- Blood 2008;112:3434-43.
2. Greenberg P, Cox C, LeBeau MM, et al. plastic syndrome or bone marrow failure: 25. McDaniel JM, Pinilla-Ibarz J, Epling-
International scoring system for evaluat- case series with focus on 5-azacytidine Burnette PK. Molecular action of lenalido-
ing prognosis in myelodysplastic syn- and literature review. Eur J Haematol mide in lymphocytes and hematologic
dromes. Blood 1997;89:2079-88. 2014;93:247-59. malignancies. Adv Hematol 2012;2012:
3. Will B, Zhou L, Vogler TO, et al. Stem and 14. Bouali F, Berrah A, Si Ahmed-Bouali D, et 513702.
progenitor cells in myelodysplastic syn- al. [Immunological abnormalities in
26. Castelli R, Cassin R, Cannavo A, Cugno M.
dromes show aberrant stage-specific myelodysplastic syndromes. Prospective
Immunomodulatory drugs: new options for
expansion and harbor genetic and epige- study (series of 40 patients)]. Rev Med
the treatment of myelodysplastic syn-
netic alterations. Blood 2012;120:2076-86. Interne 2005;26:777-83. [Article in
dromes. Clin Lymphoma Myeloma Leuk
4. Gadji M, Adebayo Awe J, et al. Profiling French].
2013;13:1-7.
three-dimensional nuclear telomeric 15. Mekinian A, Braun T, Decaux O, et al.
Inflammatory arthritis in patients with 27. Enright H, Miller W. Autoimmune phenom-
architecture of myelodysplastic syndromes
and acute myeloid leukemia defines myelodysplastic syndromes: a multicenter ena in patients with myelodysplastic syn-
patient subgroups. Clin Cancer Res retrospective study and literature review dromes. Leuk Lymphoma 1997;24:483-9.
2012;18:3293-304. of 68 cases. Medicine (Baltimore) 28. Kwong YL, Au WY, Liang RH. Acute
5. Rhyasen GW, Starczynowski DT. 2014;93:1-10. myeloid leukemia after azathioprine treat-
Deregulation of microRNAs in myelodys- 16. Castro M, Conn DL, Su WP, Garton JP. ment for autoimmune diseases: associa-
plastic syndrome. Leukemia 2012;26:13- Rheumatic manifestations in myelodys- tion with -7/7q. Cancer Genet Cytogenet
22. plastic syndromes. J Rheumatol 1991;18: 199815;104:94-7.
6. del Rey M, O’Hagan K, Dellett M, et al. 721-7. 29. Fraison JB, Mekinian A, Grignano E, et al.
Genome-wide profiling of methylation 17. Hamblin TJ. Immunological abnormalities Efficacy of azacitidine (AZA) in autoim-
identifies novel targets with aberrant in myelodysplastic syndromes. Semin mune and inflammatory disorders (AID)
hypermethylation and reduced expression Hematol 1996;33:150-62. associated with myelodysplastic syn-
in low-risk myelodysplastic syndromes. 18. Ramakrishna R, Chaudhuri K, Sturgess A, dromes (MDS) and chronic myelomono-
Leukemia 2013;27:610-8. Manoharan A. Haematological manifesta- cytic leukemia (CMML). Blood 2015;126:
7. Sloand EM, Wu CO, Greenberg P, et al. tions of primary Sjogren’s syndrome: a 1695.
Factors affecting response and survival in clinicopathological study. Q J Med 30. Aggarwal S, van de Loosdrecht AA, Alhan
patients with myelodysplasia treated with 1992;83:547-54. C, et al. Role of immune responses in the
immunosuppressive therapy. J Clin Oncol 19. Hebbar M, Brouillard M, Wattel E, et al. pathogenesis of low-risk MDS and high-
2008;26:2505-11. Association of myelodysplastic syndrome risk MDS: implications for immunothera-
8. Zeng W, Miyazato A, Chen G, et al. and relapsing polychondritis: further evi- py. Br J Haematol 2011;153:568-81.
Interferon-gamma-induced gene expres- dence. Leukemia 1995;9:731-3. 31. Takeoka Y, Miura A, Nakamura K, et al. A
sion in CD34 cells: identification of patho- 20. Sokol RJ, Hewitt S, Booker DJ. Erythrocyte
detailed analysis of myelodysplastic syn-
logic cytokine-specific signature profiles. autoantibodies, autoimmune haemolysis,
drome complicated by autoimmune or
Blood 2006;107:167-75. and myelodysplastic syndromes. J Clin
inflammatory disorders: a possible efficacy
9. Enright H, Jacob HS, Vercellotti G, et al. Pathol 1989;42:1088-91.
of low-dose lenalidomide. Blood 2014;124:
Paraneoplastic autoimmune phenomena 21. Okamoto T, Okada M, Mori A, et al.
3256.
in patients with myelodysplastic syn- Correlation between immunological
dromes: response to immunosuppressive abnormalities and prognosis in myelodys- 32. Montefusco V, Galli M, Spina F, et al.
therapy. Br J Haematol 1995;91:403-8. plastic syndrome patients. Int J Hematol Autoimmune diseases during treatment
10. Giannouli S, Voulgarelis M, Zintzaras E, et 1997;66:345-51. with immunomodulatory drugs in multiple
al. Autoimmune phenomena in myelodys- 22. Ahn JK, Cha HS, Koh EM, et al. Behcet’s myeloma: selective occurrence after
plastic syndromes: a 4-yr prospective disease associated with bone marrow fail- lenalidomide. Leuk Lymphoma 2014:1-6.
study. Rheumatology (Oxford) ure in Korean patients: clinical character- 33. Mekinian A, Grignano E, Braun T, et al.
2004;43:626-32. istics and the association of intestinal Systemic inflammatory and autoimmune
11. de Hollanda A, Beucher A, Henrion D, et al. ulceration and trisomy 8. Rheumatology manifestations associated with myelodys-
Systemic and immune manifestations in (Oxford) 2008;47:1228-30. plastic syndromes and chronic
myelodysplasia: a multicenter retrospec- 23. Stirewalt DL, Mhyre AJ, Marcondes M, et myelomonocytic leukaemia: a French mul-
tive study. Arthritis Care Res (Hoboken) al. Tumour necrosis factor-induced gene ticentre retrospective study. Rheumatology
2011;63:1188-94. expression in human marrow stroma: (Oxford) 2016;55:291-300.
[page 26] [Hematology Reports 2016; 8:6480]
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- HemaDokument6 SeitenHemaAnonymous plYGwXNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- EndokrinDokument5 SeitenEndokrinAnonymous plYGwXNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- CardioDokument2 SeitenCardioAnonymous plYGwXNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- GastroDokument6 SeitenGastroAnonymous plYGwXNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- EndokrinDokument7 SeitenEndokrinAnonymous plYGwXNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- GastroDokument9 SeitenGastroAnonymous plYGwXNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- CardioDokument7 SeitenCardioAnonymous plYGwXNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- EndokrinDokument7 SeitenEndokrinAnonymous plYGwXNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- EndokrinDokument25 SeitenEndokrinAnonymous plYGwXNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- International Journal of CardiologyDokument5 SeitenInternational Journal of CardiologyAnonymous plYGwXNoch keine Bewertungen
- Association Between Lipid Fractions and Age of First Myocardial InfarctionDokument7 SeitenAssociation Between Lipid Fractions and Age of First Myocardial InfarctionAnonymous plYGwXNoch keine Bewertungen
- CardioDokument6 SeitenCardioAnonymous plYGwXNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Pancreas, Biliary Tract, and Liver: Clinical Features of COVID-19-Related Liver Functional AbnormalityDokument6 SeitenPancreas, Biliary Tract, and Liver: Clinical Features of COVID-19-Related Liver Functional AbnormalityAnonymous plYGwXNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- GastroDokument8 SeitenGastroAnonymous plYGwXNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Ca Recti PDFDokument9 SeitenCa Recti PDFAnonymous plYGwXNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Ca Recti PDFDokument9 SeitenCa Recti PDFAnonymous plYGwXNoch keine Bewertungen
- Elektrolit Urine 1 PDFDokument7 SeitenElektrolit Urine 1 PDFAnonymous plYGwXNoch keine Bewertungen
- Partial Prediction of Postpartum Graves' Thyrotoxicosis by Sensitive Bioassay For Thyroid-Stimulating Antibody Measured in Early PregnancyDokument4 SeitenPartial Prediction of Postpartum Graves' Thyrotoxicosis by Sensitive Bioassay For Thyroid-Stimulating Antibody Measured in Early Pregnancykartini ciatawiNoch keine Bewertungen
- Kimia Ar 1Dokument7 SeitenKimia Ar 1Anonymous plYGwXNoch keine Bewertungen
- Jurnal Mikro 2Dokument9 SeitenJurnal Mikro 2Anonymous plYGwXNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Severe Aplastic Anemia: A Prospective Study of The Effect of Early Marrow Transplantation On Acute MortalityDokument9 SeitenSevere Aplastic Anemia: A Prospective Study of The Effect of Early Marrow Transplantation On Acute MortalityAnonymous plYGwXNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The RIFLE and AKIN Classifications For Acute Kidney Injury: A Critical and Comprehensive ReviewDokument7 SeitenThe RIFLE and AKIN Classifications For Acute Kidney Injury: A Critical and Comprehensive ReviewAnonymous plYGwXNoch keine Bewertungen
- Severe Aplastic Anemia: A Prospective Study of The Effect of Early Marrow Transplantation On Acute MortalityDokument9 SeitenSevere Aplastic Anemia: A Prospective Study of The Effect of Early Marrow Transplantation On Acute MortalityAnonymous plYGwXNoch keine Bewertungen
- Vitamin K Deficiency in Critical Ill Patients - A Prospective Observational StudyDokument5 SeitenVitamin K Deficiency in Critical Ill Patients - A Prospective Observational Studykartini ciatawiNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Racial Disparities in Survival of Children and Young Adults With Leukemia and LymphomaDokument8 SeitenRacial Disparities in Survival of Children and Young Adults With Leukemia and LymphomaAnonymous plYGwXNoch keine Bewertungen
- GGT-HD 1Dokument8 SeitenGGT-HD 1Anonymous plYGwXNoch keine Bewertungen
- Mds SleDokument4 SeitenMds SleAnonymous plYGwXNoch keine Bewertungen
- Jurnal ICUSDokument5 SeitenJurnal ICUSAnonymous plYGwXNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Vitamin K Deficiency in Critical Ill Patients - A Prospective Observational StudyDokument5 SeitenVitamin K Deficiency in Critical Ill Patients - A Prospective Observational Studykartini ciatawiNoch keine Bewertungen
- Gastrointestinal Endoscopy Volume 71 Issue 7 2010 (Doi 10.1016/j.gie.2009.12.029) Lisette G. Capelle Annemarie C. de Vries Jelle Haringsma Fran - The Staging of Gastritis With The OLGA System by PDFDokument9 SeitenGastrointestinal Endoscopy Volume 71 Issue 7 2010 (Doi 10.1016/j.gie.2009.12.029) Lisette G. Capelle Annemarie C. de Vries Jelle Haringsma Fran - The Staging of Gastritis With The OLGA System by PDFAleida VivalloNoch keine Bewertungen
- Prostrolane Intra Articular en INGLESDokument6 SeitenProstrolane Intra Articular en INGLESjuanNoch keine Bewertungen
- Clinical Summary Guide 05Dokument2 SeitenClinical Summary Guide 05Diarti_PMIKNoch keine Bewertungen
- AM19-Proceedings-Full ASCO PDFDokument652 SeitenAM19-Proceedings-Full ASCO PDFrusgal8992100% (1)
- Soft tissue sarcoma overviewDokument123 SeitenSoft tissue sarcoma overviewOana BarbuNoch keine Bewertungen
- ScrofulodermDokument4 SeitenScrofulodermIzmi AzizahNoch keine Bewertungen
- Interventional BronchosDokument323 SeitenInterventional BronchosFranspol100% (1)
- Simple GoitreDokument13 SeitenSimple GoitreEmad WalyNoch keine Bewertungen
- Thrombo PhiliaDokument226 SeitenThrombo PhiliawalkerbestNoch keine Bewertungen
- Kjjhhgfdsasdf HJKLKJHGFDSSDFG HJKLDokument4 SeitenKjjhhgfdsasdf HJKLKJHGFDSSDFG HJKLbubble_inNoch keine Bewertungen
- 2016 Guía Europea de Prevención de La Enfermedad Cardiovascular en La PrácticaDokument68 Seiten2016 Guía Europea de Prevención de La Enfermedad Cardiovascular en La PrácticaPaty Alatorre IcazaNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Digestive System: Maria Victoria M. Villarica MD OLFU College of Medicine Department of PediatricsDokument81 SeitenThe Digestive System: Maria Victoria M. Villarica MD OLFU College of Medicine Department of PediatricsSven OrdanzaNoch keine Bewertungen
- Course Work EssayDokument12 SeitenCourse Work EssayKanza NajamNoch keine Bewertungen
- Lista de Lucrari 3Dokument30 SeitenLista de Lucrari 3Anonymous 0epuGwQTJNoch keine Bewertungen
- Middle-Range Theory of Chronic Sorrow: A Framework for Understanding Recurring GriefDokument6 SeitenMiddle-Range Theory of Chronic Sorrow: A Framework for Understanding Recurring GriefRizkia100% (2)
- Adrenal Cortex Disease and PhaeochromocytomasDokument47 SeitenAdrenal Cortex Disease and PhaeochromocytomasJamaluddin Ahmad A.MNoch keine Bewertungen
- Intravenous PyelogramDokument23 SeitenIntravenous Pyelogramrachael100% (1)
- Msds Control KimiaDokument16 SeitenMsds Control KimiaEny Sucitrayati SucitrayatiNoch keine Bewertungen
- The Digestive System AvrDokument29 SeitenThe Digestive System AvrMatthew Benoza ARCEGANoch keine Bewertungen
- Imaging Classification of Vascular MalformationsDokument16 SeitenImaging Classification of Vascular MalformationsHector Hernandez-SoriaNoch keine Bewertungen
- Healthmedicinet I 2017 3Dokument667 SeitenHealthmedicinet I 2017 3tuni santeNoch keine Bewertungen
- Uveal Coloboma: The Related SyndromesDokument3 SeitenUveal Coloboma: The Related Syndromeslavinia diaNoch keine Bewertungen
- مجلة توفيقTJMSDokument89 Seitenمجلة توفيقTJMSTaghreed Hashim al-NoorNoch keine Bewertungen
- Ultrasound in Obstetrics and Gynaecology: ReviewDokument9 SeitenUltrasound in Obstetrics and Gynaecology: ReviewGustina Maryanti MooyNoch keine Bewertungen
- Herpetiform Pemphigus: Courtesy, Ronald P Rapini, MDDokument1 SeiteHerpetiform Pemphigus: Courtesy, Ronald P Rapini, MDCristian QuitoNoch keine Bewertungen
- Kingfisher Business CupcakesDokument14 SeitenKingfisher Business Cupcakesjeffrey A. FerrerNoch keine Bewertungen
- Who Edl 2018 PDFDokument30 SeitenWho Edl 2018 PDFanggoenzNoch keine Bewertungen
- Breast MRIDokument170 SeitenBreast MRICosas CuponaticNoch keine Bewertungen
- Puberdade PrecoceDokument12 SeitenPuberdade PrecoceCaio AlvesNoch keine Bewertungen
- Programmed Appropriation and Obligation by Object of ExpenditureDokument7 SeitenProgrammed Appropriation and Obligation by Object of ExpenditureKristin Villaseñor-MercadoNoch keine Bewertungen
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisVon EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (13)