Beruflich Dokumente
Kultur Dokumente
Gyne - Case 12 Upper Genital UTI
Hochgeladen von
cbac19900 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
6 Ansichten2 SeitenGyne - Case 12 Upper Genital UTI
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenGyne - Case 12 Upper Genital UTI
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
6 Ansichten2 SeitenGyne - Case 12 Upper Genital UTI
Hochgeladen von
cbac1990Gyne - Case 12 Upper Genital UTI
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 2
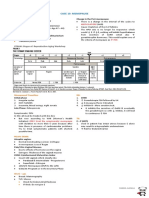
CASE 12: UPPER GENITAL INFECTION
UPPER GENITAL INFECTION Other PE Finding:
MOT: Ascending of Lower Genital Infection If there is leakage of the pus, it would gravitate on the
Organs involved: Uterus, Fallopian tube, Ovaries most dependent portion: FORNICES which would be
manifested as FULLNESS or BULGING
Uterus: Do IE: presence of fluid accumulating in the cul de sac
Endometrial lining - Mucosal spread not vascular or which pushes the fornix downwards (Remember thin
Lymphatic mucosa & if you have any accumulation of fluid/ blood/
Endometrium - Endometritis pus then it will be full or bulging)
Chronic PID: Long standing infection or inflammation
Fallopian tube: Salpingitis causing fibrosis/adhesions felt as thickened uterosacrals
Spills out from the fimbriated end: "oopohirits or Dyspareunia (Chronic PID)
salphingooophporitis"
IF everything else is involved: PID (Irritation of Peritoneal Triad:
surface) Abdominal pain, Cervical motion tenderness, & Adnexal
tenderness
Symptoms:
Abdominal pain, DDX:
Fever, general malaise Acute appendicitis: Progression of the pain from
GI irritation (peritoneal irritation): nausea & vomiting periumbilical to RLQ pain + nausea
sometimes diarrhea Ectopic pregnancy: LMP (Missed period, Delay, + PT)
Bleeding due to endometritis Ureterolithiasis: Colicky pain (Squeezing) Spasmodic,
Genitourinary symptoms: dysuria frequency, dribbling Intermittent
(UTI symptoms, Note the proximity to the bladder) Ovarian cyst (rupture or leak): ask for risk factors
o Remember: UTI cannot cause PID
Abnormal discharge Laboratory Test:
IF Chronic Stage: Pelvic or Lower abdominal mass as TOA CBC: Leukocytosis (PMN: Inflammation)
(Ultimate End Stage of PID) Gram stain/ culture:
What if there is no discharge, where is the ideal site?
Risk Factors: ENDOCERVICAL CANAL & not from the pooling of the
Sexual HX: discharge (remember it has crypts wherein bacteria hide:
Use of barrier devices (IUD, Cervical diaphragms/cuff, commensalism)
condoms, family planning devices Urinalysis
If had ligation (metal clips inserted on the fallopian tube) TVS: TOA (complex mass filled with fluid, pus presenting
Diagnosed to have STID, as hypoechoic & hyperechoic within the tube), fluid,
# of sexual partners bulbous tube, hydrosalpinx or blunted end of the tube
wherein fimbriae cannot be appreciated anymore.
PMH: LAPAROSCOPY: GOLD STANDARD, Can determine the
Minor surgical procedures that enter the uterine cavity severity of the disease, visualize the pelvis
(endometrial biopsy, curettage, hysteroscopy, HSG) with DX: gross inspection (erythema, adhesions (acute -
introduction of medias such as water, saline or dye flimsy, chronic - dense), aspirate the pus for gram stain
producing microorganisms to infect the endometrium TX: drain the abscess, washing or peritoneal
causing endosalpinx from DX of AUB or infertility cases
Recent abdominal surgery or pelvic surgery in the form Etiology: Polymicrobial
of oophorecystectomy for infected ovarian cyst causing Peculiar in developing countries: TB (take a look at the
post op morbidity in the form of pelvic infection physique: thin tuberculous looking)
(secondary not primary) Work up: CXR, endometrial sampling to see the (+)
Primary: a direct mucosal infection, ascending infection tubercle bacilli
from the lower genital tract
TX:
What other structures aside from the ovary might involve the Antibiotic Regimen for PID
tubes forming or notorious for forming secondary infections? Quadruple Anti-Kochs Regimen
Appendix: Perforated appendicitis or Peri-appendicial
abscess Treatment: Medical or Surgical
Cancer or Malignancy with Necrosis (serosal spread Medical: Ambulatory or Outpatient/ Inpatient
before mucosal spread)
Indications for admitting a patient:
PE: (Confirmatory) 1. Unsure diagnosis
Abdominal tenderness (inguinal area or lower quadrant 2. Unable to tolerate or unresponsive treatment (have to
area) give it parenteral form)
Cervical motion tenderness (elicited by IE from moving to 3. Presence of TOA
the sides), 4. Acute abdomen, direct & rebound tenderness, rigidity or
If (+) due to peritoneal irritation: Ectopic pregnancy, TOA board like
Uterine Tenderness 5. Pregnant
Adnexal Tenderness 6. Systemic or full blown?
Speculum Exam: Abnormal cervical discharge, erythematous
How long is the antibiotic treatment? 2 WEEKS
If Salpingitis: Inflammation can lead to abscess How much time for the medical TX to take effect before
giving surgical intervention or shift to another medication &
Mass can be elicited represented as TOA or
when do you expect resolution of the symptoms? 48 – 72
Hematosalpinx, Hydrosalpinx or Pyosalpinx (bulbous,
hours
edematous mass due to fluid inside)
For both gram (+) & (-) organisms: 2nd Gen Cephalosporin
For chlamydial infection: Tetracycline, Doxycycline it will take a while for the abscess to dissolve but if there
is resolution of the SX continue the antibiotics & do UTZ
CDC Regimen A: at the end of 2 weeks (no point in stopping 3 days)
How long would be the IV route? 48 - 72 hours where in Less IE the better
observe for resolution of symptoms: ↓ abdominal pain,
lysis of fever, ↓ WBC (PMN) If with TOA:
If responsive in IV: Shift to oral preparation & continue For the anaerobes: Clindamycin + Gentamycin +
for 1 - 2 weeks. Metronidazole
For the chlamydia: + Tetracycline
What is important in PID & should be remembered?
Not only the choice of antibiotics, but ALWAYS TREAT If there is no resolution for the TOA by progression of pain &
THE PARTNER (to prevent recurrence or development ↑ WBC:
into chronic PID) Do surgical intervention by draining the abscess via
aspiration in laparoscopy, or laparotomy, or UTZ.
If the patient had TOA 48 - 72 hours can you expect
resolution?
Case 12
th
24 y/o nulligravid consults because of abdominal pain accompanied by fever of 3 days duration. Today is the 6
O
day of her menstrual cycle. PPE: BP – 110/70 PR 100/min full RR – 20/ min Temp – 39.2 C. Heart & lungs
unremarkable; Abdomen: flat, soft, (+) direct tenderness on the hypogastric area & both lower quadrants.
Speculum exam: Cervix – pink with purulent discharge at the cervical os. IE: Cervix – firm, long, closed, (+) cervical
motion tenderness. Uterus – normal sized anteverted tender. Adnexa – could not be assessed due to guarding
DX: Acute PID
If chronic PID, there is minimal systemic symptoms & IE:
thickening of the parametria representing adhesions
secondary to infections
D6 of menstrual period & abdominal pain happen 3 days ago:
It is typical after menstruation to have presence of pain.
The cervix is open which gives easy access to bacteria
going upwards to the endometrium, tubes & the blood
coming out consisting of proteins is a good medium for
the cultivation of bacteria.
Work-up:
CBC: Leukocytosis (systemic illness can cause anemia)
UTZ: check for TOA
UA: check for UTI
Management:
Admission due to tenderness, fever, tachycardia &,
presence of peritoneal irritation (e.x. Fitz-High-Curtis
syndrome: Liver)
Give IV fluids, monitor VS (patient can go to septic shock)
& antibiotics
Do gram stain & culture of the purulent discharge
IF UTZ result is presence of normal size bulbous tubes
bilateral &swollen edematous tubes but ovaries are
normal: Give REGIMEN A
If UTZ result is presence of TOA: Give REGIMEN B
If there is no improvement: Drain the abscess, do
Fowler’s position to drain in the pelvic area & not spread
to other areas
If 52 year old G3P3 with the same PE in the case either
with TOA or swollen tube & after 3 days no resolution:
Do clean up by TAHBSO (but do not do in septic
environment)
If young: USO (Affected side only)
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Gyne - Lec 03 CytologyDokument3 SeitenGyne - Lec 03 Cytologycbac1990Noch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Gynecology - Case 14 - Benign Lesions For Ovaries (Gonzalez)Dokument2 SeitenGynecology - Case 14 - Benign Lesions For Ovaries (Gonzalez)cbac1990Noch keine Bewertungen
- Gyne - Case 18 - Neoplastic Lesions of The Ovaries (Gonzalez) PDFDokument3 SeitenGyne - Case 18 - Neoplastic Lesions of The Ovaries (Gonzalez) PDFcbac1990Noch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Gynecology - Case 13 - Benign Lesions of The Uterus (Gonzalez)Dokument2 SeitenGynecology - Case 13 - Benign Lesions of The Uterus (Gonzalez)cbac1990Noch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Gyne Notes Abnormal Uterine Bleeding - Dra TrinidadDokument3 SeitenGyne Notes Abnormal Uterine Bleeding - Dra Trinidadcbac1990Noch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Gynecology - Case 13 - Benign Lesions of The Uterus (Gonzalez)Dokument2 SeitenGynecology - Case 13 - Benign Lesions of The Uterus (Gonzalez)cbac1990Noch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Gyne - Case 15 Benign Lesions of The Vulva & VaginaDokument2 SeitenGyne - Case 15 Benign Lesions of The Vulva & Vaginacbac1990Noch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Gyne - Case 17 - Intraepithelial & Neoplastic Lesions of The Uterus (Gonzalez)Dokument1 SeiteGyne - Case 17 - Intraepithelial & Neoplastic Lesions of The Uterus (Gonzalez)cbac1990Noch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Gyne - Case 18 - Neoplastic Lesions of The Ovaries (Gonzalez) PDFDokument3 SeitenGyne - Case 18 - Neoplastic Lesions of The Ovaries (Gonzalez) PDFcbac1990Noch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Gyne - Case 16 - Intraepithelial & Neoplastic Lesions of Cervix (Gonzalez)Dokument2 SeitenGyne - Case 16 - Intraepithelial & Neoplastic Lesions of Cervix (Gonzalez)cbac1990Noch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Gyne - Case 16 Neoplastic Lesions of The CevixDokument1 SeiteGyne - Case 16 Neoplastic Lesions of The Cevixcbac1990Noch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Case 3 Congenital Anomalies, Primary AmenorrheaDokument3 SeitenCase 3 Congenital Anomalies, Primary Amenorrheacbac1990Noch keine Bewertungen
- Gyne - Case 17 - Intraepithelial & Neoplastic Lesions of The Uterus (Gonzalez)Dokument1 SeiteGyne - Case 17 - Intraepithelial & Neoplastic Lesions of The Uterus (Gonzalez)cbac1990Noch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Gyne - Case 14 Benign Lesions of The OvariesDokument2 SeitenGyne - Case 14 Benign Lesions of The Ovariescbac1990Noch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Gyne - Case 05 Abnormal Uterine BleedingDokument3 SeitenGyne - Case 05 Abnormal Uterine Bleedingcbac1990Noch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Gyne - Case 11 Lower Genital UTI PDFDokument2 SeitenGyne - Case 11 Lower Genital UTI PDFcbac1990Noch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Gyne - Case 13 Benign Lesions of The UterusDokument2 SeitenGyne - Case 13 Benign Lesions of The Uteruscbac1990Noch keine Bewertungen
- Gyne - Case 07 Secondary Amenorrhea (Hyperprolactinemia)Dokument1 SeiteGyne - Case 07 Secondary Amenorrhea (Hyperprolactinemia)cbac1990Noch keine Bewertungen
- Gyne - Case 07 Secondary Amenorrhea (Hyperprolactinemia)Dokument1 SeiteGyne - Case 07 Secondary Amenorrhea (Hyperprolactinemia)cbac1990Noch keine Bewertungen
- Gyne - Case 08 Dysmenorrhea & Endometriosis PDFDokument3 SeitenGyne - Case 08 Dysmenorrhea & Endometriosis PDFcbac1990Noch keine Bewertungen
- Case 9 Infertility PDFDokument4 SeitenCase 9 Infertility PDFcbac1990Noch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Case 4 Anatomic Defect On Pelvic Floor & UrogynecologyDokument1 SeiteCase 4 Anatomic Defect On Pelvic Floor & Urogynecologycbac1990Noch keine Bewertungen
- Gyne - Case 06 Secondary Amenorrhea (Hyperandrogenism)Dokument2 SeitenGyne - Case 06 Secondary Amenorrhea (Hyperandrogenism)cbac1990Noch keine Bewertungen
- Gyne - Case 10 MenopauseDokument2 SeitenGyne - Case 10 Menopausecbac1990Noch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Case 3 Congenital Anomalies, Primary AmenorrheaDokument3 SeitenCase 3 Congenital Anomalies, Primary Amenorrheacbac1990Noch keine Bewertungen
- Case 2 Pre-Op & Post-Op CareDokument1 SeiteCase 2 Pre-Op & Post-Op Carecbac1990Noch keine Bewertungen
- Case 1 History & PEDokument3 SeitenCase 1 History & PEcbac1990Noch keine Bewertungen
- AMC-Residency CV Worksheet-III PDFDokument1 SeiteAMC-Residency CV Worksheet-III PDFcbac1990Noch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- PTAL Residency CaliforniaDokument24 SeitenPTAL Residency Californiacbac1990Noch keine Bewertungen
- 11.3 MGR UniversityDokument15 Seiten11.3 MGR UniversityValarmathiNoch keine Bewertungen
- Child Health Problems GlobalDokument86 SeitenChild Health Problems GlobalBagus P Agen SuplierNoch keine Bewertungen
- Medical Nutrition Therapy Paper - 2Dokument18 SeitenMedical Nutrition Therapy Paper - 2madiha altafNoch keine Bewertungen
- Antimicrobial RsistanceDokument548 SeitenAntimicrobial RsistanceLemayanNoch keine Bewertungen
- BREASTFEEDINGDokument2 SeitenBREASTFEEDINGFianisa RizkaNoch keine Bewertungen
- Reflex Anal Dilatation An Observational Study On Non-Abused ChildrenDokument5 SeitenReflex Anal Dilatation An Observational Study On Non-Abused Childrenaniendyawijaya0% (1)
- Immunopotentiation: Immunopotentiation Can Be Defined As The ProcessDokument67 SeitenImmunopotentiation: Immunopotentiation Can Be Defined As The ProcesssamyNoch keine Bewertungen
- 10 3889@oamjms 2019 300Dokument6 Seiten10 3889@oamjms 2019 300Rudi WsNoch keine Bewertungen
- Ac 76583 Pfdqwertaf 79898 TseDokument548 SeitenAc 76583 Pfdqwertaf 79898 TseMerve EmelNoch keine Bewertungen
- On Burns ManagementDokument13 SeitenOn Burns ManagementNujella BalajiNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Ratio For Cmca UesDokument3 SeitenRatio For Cmca UesJeralyn Delarosa GabagatNoch keine Bewertungen
- Equine Colic Putting The Puzzle Together 2017Dokument3 SeitenEquine Colic Putting The Puzzle Together 2017Danahe CastroNoch keine Bewertungen
- Vehling Annika ResumeDokument1 SeiteVehling Annika Resumeapi-733364471Noch keine Bewertungen
- Focus On Nursing Pharmacology Karch 5th Edition Test BankDokument16 SeitenFocus On Nursing Pharmacology Karch 5th Edition Test BankPeggie Edwards100% (31)
- Unit Plan ObgDokument21 SeitenUnit Plan Obgshivani das67% (3)
- Breast Self ExaminationDokument40 SeitenBreast Self ExaminationPrince Rener Velasco PeraNoch keine Bewertungen
- Quadrivalent Inactivated Influenza Vaccine (Vaxigriptetra™) : Expert Review of VaccinesDokument41 SeitenQuadrivalent Inactivated Influenza Vaccine (Vaxigriptetra™) : Expert Review of VaccinesMarco LealiNoch keine Bewertungen
- Murottal and Clasical Music Therapy Reducing Pra Cardiac Chateterization AnxietyDokument9 SeitenMurottal and Clasical Music Therapy Reducing Pra Cardiac Chateterization AnxietyElsaNoch keine Bewertungen
- Yökdil Sağlik Bilimleri ŞUBAT 2021Dokument27 SeitenYökdil Sağlik Bilimleri ŞUBAT 2021Gizem Elat0% (1)
- Effect of Self-Acupressure On Middle Ear Barotrauma Associated With HyperbaricDokument5 SeitenEffect of Self-Acupressure On Middle Ear Barotrauma Associated With Hyperbariclia indria watiNoch keine Bewertungen
- Benign Prostatic Hyperplasia PDFDokument496 SeitenBenign Prostatic Hyperplasia PDFnurul_nufafinaNoch keine Bewertungen
- VM in BpocDokument19 SeitenVM in BpocAndreea Livia DumitrescuNoch keine Bewertungen
- Biopharmaceutical: What Is A ?Dokument6 SeitenBiopharmaceutical: What Is A ?NarendrakumarNoch keine Bewertungen
- Alfeche Kathleen Rose BSN 1 E TFN Case Application Interactive TheoriesDokument4 SeitenAlfeche Kathleen Rose BSN 1 E TFN Case Application Interactive TheoriesAiza CeciliaNoch keine Bewertungen
- Dice Hospital Rules v2.12 Draft Black Background BDokument9 SeitenDice Hospital Rules v2.12 Draft Black Background BViktorNoch keine Bewertungen
- Sea rc69 r4Dokument3 SeitenSea rc69 r4im.ramNoch keine Bewertungen
- Clinical Examination Techniques in OtologyDokument44 SeitenClinical Examination Techniques in OtologyDr. T. Balasubramanian100% (2)
- AA Discharge-SummaryDokument7 SeitenAA Discharge-SummaryMMW MNoch keine Bewertungen
- IARC CX Ca Screening PDFDokument313 SeitenIARC CX Ca Screening PDFderr barrNoch keine Bewertungen
- 4564 2934 p436 Pages Deleted EditedDokument4 Seiten4564 2934 p436 Pages Deleted EditedHaniNoch keine Bewertungen
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (24)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4 von 5 Sternen4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (80)