Beruflich Dokumente
Kultur Dokumente
Routine Antibiotics For BreastConserving
Hochgeladen von
Quennie Abellon QuimanOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Routine Antibiotics For BreastConserving
Hochgeladen von
Quennie Abellon QuimanCopyright:
Verfügbare Formate
46
Study: Routine Antibiotics for Breast-
Oncology Times • June 25, 2015 • oncology-times.com
Conserving Surgery Can Be Safely Omitted
By Ed Susman
O
RLANDO, Fla.—Providing cer surgery unless they are undergoing
prophylactic antibiot- reconstruction,” she said.
ics to prevent infections “If surgeons have been using antibi-
in women undergoing otics when a wire localization has been
breast cancer needle-directed lumpec- done, this study certainly would sup-
tomy procedures may be wasted ef- port their discontinuing that practice.
forts, researchers suggested here at the We do tend to over-utilize antibiotics,
American Society of Breast Surgeons which expose patients to allergic reac-
(ASBrS) Annual Meeting. tions, resistance to antibiotics in the fu-
“Our analysis showed no difference ture, and increased costs.”
in infection rate, leading to the con-
clusion that it is safe to omit the use
Contrary to ASBrS
Ed Susman
of antibiotics prior to needle-localized
lumpectomy and avoid the cost of the Position Statement
medication, patient adverse reactions, The findings appear contrary to the
and the increased risk of resistant or- American Society of Breast Surgeons Lindsay Petersen, MD: “Our
ganisms,” said Lindsay Petersen, MD, position statement on antibiotics and analysis showed no difference
Senior Resident in General Surgery at surgical site infections (http://bit. in infection rate, leading to the
Rush University in Chicago and sched- ly/1AsS2ES), which were released in conclusion that it is safe to omit
uled to start in July as a Fellow in Breast 2012. “Those guidelines recommend the use of antibiotics prior to
Surgery at the University of Michigan. a preoperative prophylactic dose of needle-localized lumpectomy and
Of the 140 patients in the study who an antibiotic prior to needle-localized avoid the cost of the medication,
were not given prophylactic antibiotics, lumpectomy for cancer or prior to patient adverse reactions, and
only three developed infections—a rate any excisional biopsy if risk factors are increase in resistant organisms.”
“We are being
much too cautious patients who received antibiotics were
treated with cefazolin (79%); another
in ordering 19 percent received clindamycin, one
antibiotics in patient received ertapenem, and an-
other received levofloxacin.
patients undergoing Petersen said that after examining
the patient characteristics of the four
these procedures. of two percent, compared with one per- present, but it is unclear if this practice individuals who developed an infection
We are not violating cent (one infection) in the 80 patients reduces the rate of infection,” Petersen and the 216 patients who did not, she
given antibiotics, she noted in an inter- said. was unable to find any significant cor-
anything other than view at her poster presentation. For the study, she and her colleagues relations. Although three of the four pa-
“We are being much too cautious in conducted a retrospective chart review tients with infections (75%) were older
the skin and soft ordering antibiotics in patients under- of patients who underwent needle- than 65, 71 percent of the women who
so there should not going these procedures,” she said. “We localized lumpectomy from 2010 to did not have infections were also over
are not violating anything other than 2012, collecting data on patient demo- 65; four patients with an infection had
be a great risk for the skin and soft tissue so there should graphics, comorbid conditions, medical received antibiotics (24%) and 37% of
not be a great risk for infection.” history, operative details, and pathology. the patients who did not have an infec-
infection.” Karen Kostroff, MD, Chief of Breast Surgical infections requiring opening of tion received antibiotics. Two of the
Surgery at North Shore-LIJ Cancer the wound or treatment with antibiotics four women undergoing lumpectomy
were documented if they occurred during who had infections had a malignancy
the first three months following surgery. diagnosis compared with 38 percent of
“The fears that During the study period, a total the women without infection.
of 220 patients underwent needle- “The fears that longer wait times for
longer wait times localized lumpectomy at one Chicago surgery and more exposure to the nee-
institution. Their mean age was 57, and dle lead to higher infection rates have
for surgery and average body mass index was 32 kg/m2. not been justified by data we reviewed,”
About 14 percent of the patients were Petersen summed up. She said there
more exposure to smokers. The mean duration of sur- have been no studies that addressed
the needle lead gery was 92 minutes. The mean dura- the question of whether long-term nee-
tion of time the needle was in place was dle exposure in the breast is linked to
to higher infection 233 minutes. Thirty eight percent of infection.
patients had malignant pathology. In the study, 215 of 216 patients who
rates have not been A greater percentage of patients un- did not have infection had the needle in
justified by data we dergoing re-excision procedures were place for at least 90 minutes, but none
given antibiotics—15 of 80 patients of the women with infections had the
reviewed.” (19 percent) compared with 13 of 140 needle in place for longer than that.
patients (9%) not given antibiotics. Length of surgery also did not appear to
All other differences between the make a difference: About 98 percent of
Institute in Lake Success, N.Y., con- groups—diabetes status, radiation, the patients who did not have infections
curred with the findings: “I have not neoadjuvant chemotherapy, and malig- were in surgery for more than 45 min-
routinely given antibiotics to patients nant pathology—were not significantly utes compared with none of the women
undergoing uncomplicated breast can- different, Petersen said. Most of the 80 who did have infections. OT
Das könnte Ihnen auch gefallen
- Making Cancer Immunotherapy A Surer BetDokument1 SeiteMaking Cancer Immunotherapy A Surer BetMicheleFontanaNoch keine Bewertungen
- The Benefits of Immunotherapy CombinationsDokument1 SeiteThe Benefits of Immunotherapy CombinationsMicheleFontanaNoch keine Bewertungen
- Jac-Antimicrobial ResistanceDokument7 SeitenJac-Antimicrobial ResistanceJuan Manuel Jiménez LeónNoch keine Bewertungen
- Jac-Antimicrobial ResistanceDokument7 SeitenJac-Antimicrobial ResistanceKarla HernandezNoch keine Bewertungen
- Aspirin Use and Potential Mechanism For Colorectal Cancer PreventionDokument6 SeitenAspirin Use and Potential Mechanism For Colorectal Cancer PreventionMidas PatraNoch keine Bewertungen
- Antibiotic Prophylaxis in Cesarean SectionDokument6 SeitenAntibiotic Prophylaxis in Cesarean Sectionnurul wahyuniNoch keine Bewertungen
- Estrategias Inmunosupresivas de Tumores RabinovichDokument33 SeitenEstrategias Inmunosupresivas de Tumores RabinovichLyanna StarkNoch keine Bewertungen
- AztrioDokument6 SeitenAztriooscarNoch keine Bewertungen
- Steinberg 2009Dokument7 SeitenSteinberg 2009majedNoch keine Bewertungen
- 4.the Management of Patients On Anticoagulants Prior.16Dokument8 Seiten4.the Management of Patients On Anticoagulants Prior.16Gabriela Catana TurcuNoch keine Bewertungen
- JNMD DMM Cancer 2017Dokument6 SeitenJNMD DMM Cancer 2017edtsendayushNoch keine Bewertungen
- Beneficios y Riesgos de Esterilizacion InglésDokument14 SeitenBeneficios y Riesgos de Esterilizacion InglésCecilia EstradaNoch keine Bewertungen
- The Struggle To Do No Harm in Clinical TrialsDokument1 SeiteThe Struggle To Do No Harm in Clinical TrialsMicheleFontanaNoch keine Bewertungen
- Intl Journal of Cancer - 2021 - Yang - Intrauterine Device Use and Risk of Ovarian Cancer Results From The New EnglandDokument9 SeitenIntl Journal of Cancer - 2021 - Yang - Intrauterine Device Use and Risk of Ovarian Cancer Results From The New EnglandAnggie DiniayuningrumNoch keine Bewertungen
- AmbasDokument5 SeitenAmbasNilaaharan RobinsonNoch keine Bewertungen
- Antibiotic Prophylaxis in The Surgical ManagementDokument7 SeitenAntibiotic Prophylaxis in The Surgical ManagementRAHUL SHINDENoch keine Bewertungen
- 1 s2.0 S000293781830019XDokument4 Seiten1 s2.0 S000293781830019XsaryindrianyNoch keine Bewertungen
- Prior Antibiotics and Risk of Antibiotic-Resistant Community-Acquired Urinary Tract Infection: A Case - Control StudyDokument8 SeitenPrior Antibiotics and Risk of Antibiotic-Resistant Community-Acquired Urinary Tract Infection: A Case - Control StudySyed AmanNoch keine Bewertungen
- Surgical-Site Infection in Gynecologic Surgery: Pathophysiology and PreventionDokument8 SeitenSurgical-Site Infection in Gynecologic Surgery: Pathophysiology and Preventionw yNoch keine Bewertungen
- Adjunctive Azithromycin Prophylaxis For Cesarean DeliveryDokument11 SeitenAdjunctive Azithromycin Prophylaxis For Cesarean DeliveryrizkiNoch keine Bewertungen
- 38-Article Text-229-2-10-20190710 PDFDokument8 Seiten38-Article Text-229-2-10-20190710 PDFnie raniNoch keine Bewertungen
- Antibiotic Prophylaxis in Plastic Surgery Correlation Between Practice and EvidenceDokument7 SeitenAntibiotic Prophylaxis in Plastic Surgery Correlation Between Practice and EvidenceVictor Andre PeraltaNoch keine Bewertungen
- Bacteriological Profile and Antibiotic Sensitivity Pattern of Clinical Isolates in A Tertiary Cancer Care Center in The Northeast IndiaDokument5 SeitenBacteriological Profile and Antibiotic Sensitivity Pattern of Clinical Isolates in A Tertiary Cancer Care Center in The Northeast IndiaAtul Kumar GoyalNoch keine Bewertungen
- Infeksi Post SCDokument11 SeitenInfeksi Post SCAprilliaNoch keine Bewertungen
- Aspirin A Day Keep Cancer AwayDokument3 SeitenAspirin A Day Keep Cancer Awayjoy mukherjiNoch keine Bewertungen
- Negative Pressure Wound Therapy (NPWT) in Breast SurgeryDokument7 SeitenNegative Pressure Wound Therapy (NPWT) in Breast SurgerydokterhelmaNoch keine Bewertungen
- Systematic Review: Scandinavian Journal of Surgery 103: 14 - 20, 2013Dokument7 SeitenSystematic Review: Scandinavian Journal of Surgery 103: 14 - 20, 2013Jenry Himawan SinagaNoch keine Bewertungen
- Vaccine Covid19Dokument5 SeitenVaccine Covid19Đỗ Ngọc Huyền TrangNoch keine Bewertungen
- Erythromycin Vs Azithromycin For Treatment of Preterm Prelabor Rupture of Membranes: A Systematic Review and Meta-AnalysisDokument9 SeitenErythromycin Vs Azithromycin For Treatment of Preterm Prelabor Rupture of Membranes: A Systematic Review and Meta-AnalysisErik SusantoNoch keine Bewertungen
- Antibiotic Stewardship in The Newborn Surgical PatientDokument9 SeitenAntibiotic Stewardship in The Newborn Surgical PatientMukhamad Arif MunandarNoch keine Bewertungen
- Risk Factors of Adverse Event Amb - AnesDokument8 SeitenRisk Factors of Adverse Event Amb - AnesAulia Muzizatun FitrianiNoch keine Bewertungen
- Chem Soc Rev: Review ArticleDokument50 SeitenChem Soc Rev: Review ArticleLi MenghuanNoch keine Bewertungen
- Measuring Ovarian Toxicity in Clinical Trials AnDokument9 SeitenMeasuring Ovarian Toxicity in Clinical Trials AnEdgar LNoch keine Bewertungen
- Muellenhoff 2011Dokument15 SeitenMuellenhoff 2011Mariana JuravleNoch keine Bewertungen
- 1933 0715 Article p350Dokument8 Seiten1933 0715 Article p350Alan padilla sesmaNoch keine Bewertungen
- Ju 0000000000003038Dokument10 SeitenJu 0000000000003038sridharchadaNoch keine Bewertungen
- Braga Et Al 2019 Clinical Implications of Febrile Neutropenia Guidelines in The Cancer Patient PopulationDokument3 SeitenBraga Et Al 2019 Clinical Implications of Febrile Neutropenia Guidelines in The Cancer Patient PopulationRafael SuzukiNoch keine Bewertungen
- Effect of Postoperative Continuation of Antibiotic Prophylaxis On The Incidence of Surgical Site InfectionDokument11 SeitenEffect of Postoperative Continuation of Antibiotic Prophylaxis On The Incidence of Surgical Site InfectionAde Ewa Permana100% (1)
- Otley1996 Warfarina, Aas, Ains-ComplicatiiDokument6 SeitenOtley1996 Warfarina, Aas, Ains-ComplicatiiGabriela Catana TurcuNoch keine Bewertungen
- E002435 FullDokument33 SeitenE002435 FullAlizaPinkyNoch keine Bewertungen
- putcha-et-al-2021-multicancer-screening-one-size-does-not-fit-allDokument3 Seitenputcha-et-al-2021-multicancer-screening-one-size-does-not-fit-allfoodiejulian1994Noch keine Bewertungen
- 874 FullDokument28 Seiten874 FullCarolina RibeiroNoch keine Bewertungen
- Mitos InfeccionesDokument8 SeitenMitos InfeccionesAmmon10famNoch keine Bewertungen
- Incidence and Risk Factors of Surgical Site Infection Among Patients Undergoing Cesarean SectionDokument7 SeitenIncidence and Risk Factors of Surgical Site Infection Among Patients Undergoing Cesarean Sectionreza amahoruNoch keine Bewertungen
- Chargari Et Al 2024 Vulvar Carcinoma Standard of Care and PerspectivesDokument13 SeitenChargari Et Al 2024 Vulvar Carcinoma Standard of Care and Perspectivessilva.michelleNoch keine Bewertungen
- AmoxiDokument11 SeitenAmoxiflorinela gheorghiuNoch keine Bewertungen
- 1 s2.0 S0039606018302721 MainDokument7 Seiten1 s2.0 S0039606018302721 MainMelo Pérez Pamela J.Noch keine Bewertungen
- Preoperative AssessmentDokument3 SeitenPreoperative AssessmentDR BUYINZA TITUSNoch keine Bewertungen
- PredictorsforAnastomoticLeak PDFDokument6 SeitenPredictorsforAnastomoticLeak PDFPatrick JohnNoch keine Bewertungen
- Virus Oncolytic Sebagai Agen Terapi Untuk Kanker ProstatDokument18 SeitenVirus Oncolytic Sebagai Agen Terapi Untuk Kanker ProstatReza SudrajatNoch keine Bewertungen
- 10 1089@jwh 2018 7391Dokument4 Seiten10 1089@jwh 2018 7391iqlimaikkeNoch keine Bewertungen
- Imaging During Pregnancy: What The Radiologist Needs To KnowDokument11 SeitenImaging During Pregnancy: What The Radiologist Needs To KnowGabriela Serra del CarpioNoch keine Bewertungen
- AB Untuk FrakturDokument15 SeitenAB Untuk FrakturRifda LatifaNoch keine Bewertungen
- Ovarian Cancer Prevention and Screening.22Dokument19 SeitenOvarian Cancer Prevention and Screening.22tri erdiansyahNoch keine Bewertungen
- Sham Controls in Medical Device Trials: PerspectiveDokument2 SeitenSham Controls in Medical Device Trials: PerspectiveAymen BekirNoch keine Bewertungen
- Ewald MJA Letter-Communicating Air Pollution RiskDokument5 SeitenEwald MJA Letter-Communicating Air Pollution RiskBen EwaldNoch keine Bewertungen
- Ajhp2312 Antibiotic ProphylaxisDokument2 SeitenAjhp2312 Antibiotic Prophylaxisarvi awaludinNoch keine Bewertungen
- NGS Replaces CultureDokument1 SeiteNGS Replaces CultureDhruvil ShahNoch keine Bewertungen
- Patterns of and Risk Factors For Recurrence in Women With Ovarian EndometriomasDokument10 SeitenPatterns of and Risk Factors For Recurrence in Women With Ovarian EndometriomasPutri Tamara DasantosNoch keine Bewertungen
- Atypical Breast Proliferative Lesions and Benign Breast DiseaseVon EverandAtypical Breast Proliferative Lesions and Benign Breast DiseaseFarin AmersiNoch keine Bewertungen
- How To Pray Effectively For MiraclesDokument3 SeitenHow To Pray Effectively For MiraclesQuennie Abellon QuimanNoch keine Bewertungen
- New Month Prayer PointsDokument4 SeitenNew Month Prayer PointsQuennie Abellon Quiman100% (1)
- Not All Blood Is AlikeDokument11 SeitenNot All Blood Is AlikeQuennie Abellon QuimanNoch keine Bewertungen
- Prayers To St. AnthonyDokument14 SeitenPrayers To St. AnthonyQuennie Abellon QuimanNoch keine Bewertungen
- PSALM 19 Meaning ExplainedDokument6 SeitenPSALM 19 Meaning ExplainedQuennie Abellon QuimanNoch keine Bewertungen
- Learn About PneumoniaDokument5 SeitenLearn About PneumoniaQuennie Abellon QuimanNoch keine Bewertungen
- 40 Prayer Points For A New BeginningDokument4 Seiten40 Prayer Points For A New BeginningQuennie Abellon Quiman100% (4)
- Prayer Points To Walk in LoveDokument3 SeitenPrayer Points To Walk in LoveQuennie Abellon QuimanNoch keine Bewertungen
- Prayers to Overcome Jealousy and EnvyDokument3 SeitenPrayers to Overcome Jealousy and EnvyQuennie Abellon Quiman100% (1)
- 6 Authoritative Prayer Points For Healing and DeliveranceDokument3 Seiten6 Authoritative Prayer Points For Healing and DeliveranceQuennie Abellon Quiman100% (1)
- Prayers for Studying and ExamsDokument3 SeitenPrayers for Studying and ExamsQuennie Abellon QuimanNoch keine Bewertungen
- A Prayer For The Gift of Wisdom PDFDokument1 SeiteA Prayer For The Gift of Wisdom PDFroseNoch keine Bewertungen
- Distancelearning 130729100245 Phpapp01 PDFDokument17 SeitenDistancelearning 130729100245 Phpapp01 PDFQuennie Abellon QuimanNoch keine Bewertungen
- A Prayer For The Gift of Wisdom PDFDokument1 SeiteA Prayer For The Gift of Wisdom PDFroseNoch keine Bewertungen
- Connecting Professional Practice and Technology At.6Dokument9 SeitenConnecting Professional Practice and Technology At.6Quennie Abellon QuimanNoch keine Bewertungen
- Developing and Implementing A Simulated Electronic.4Dokument9 SeitenDeveloping and Implementing A Simulated Electronic.4Quennie Abellon QuimanNoch keine Bewertungen
- Chapter 9Dokument30 SeitenChapter 9saba shaukatNoch keine Bewertungen
- Distanceeducationreportingsirmijares 140503093910 Phpapp01 PDFDokument13 SeitenDistanceeducationreportingsirmijares 140503093910 Phpapp01 PDFQuennie Abellon QuimanNoch keine Bewertungen
- Tabloski ch08 LectureDokument24 SeitenTabloski ch08 LectureQuennie Abellon QuimanNoch keine Bewertungen
- Legal Rights and Responsibilities in Gerontological NursingDokument42 SeitenLegal Rights and Responsibilities in Gerontological NursingQuennie Abellon QuimanNoch keine Bewertungen
- Tabloski ch10 LectureDokument22 SeitenTabloski ch10 LectureQuennie Abellon QuimanNoch keine Bewertungen
- Hospice CareDokument31 SeitenHospice CareQuennie Abellon QuimanNoch keine Bewertungen
- 1711 05225v3Dokument7 Seiten1711 05225v3Vikas SangwanNoch keine Bewertungen
- Tabloski ch24 LectureDokument28 SeitenTabloski ch24 LectureQuennie Abellon QuimanNoch keine Bewertungen
- Tabloski ch09 LectureDokument26 SeitenTabloski ch09 LectureQuennie Abellon QuimanNoch keine Bewertungen
- Who PneumoniaDokument4 SeitenWho PneumoniaQuennie Abellon QuimanNoch keine Bewertungen
- Tabloski ch11 LectureDokument23 SeitenTabloski ch11 LectureQuennie Abellon QuimanNoch keine Bewertungen
- Hospital Aquired Pneumonia - FullDokument26 SeitenHospital Aquired Pneumonia - FullSuvad Dedic100% (1)
- Learn About PneumoniaDokument4 SeitenLearn About PneumoniaQuennie Abellon QuimanNoch keine Bewertungen
- Mycobacterium Tuberculosis 2019Dokument3 SeitenMycobacterium Tuberculosis 2019Quennie Abellon QuimanNoch keine Bewertungen
- Controversias en El Manejo de Las Fracturas Abiertas (2014)Dokument7 SeitenControversias en El Manejo de Las Fracturas Abiertas (2014)J. Adrian NogueraNoch keine Bewertungen
- Med Surg Test AnswersDokument9 SeitenMed Surg Test AnswersAshley Rose100% (3)
- Prevalence of Gestational Diabetes and Contributing Factors Among Pregnant Jordanian Women Attending Jordan University HospitalDokument8 SeitenPrevalence of Gestational Diabetes and Contributing Factors Among Pregnant Jordanian Women Attending Jordan University HospitalManar ShamielhNoch keine Bewertungen
- PLE 2019 - Medicine Questions and Answer KeyDokument24 SeitenPLE 2019 - Medicine Questions and Answer KeydicksonNoch keine Bewertungen
- Individualized Neoantigen-Specific ImmunotherapyDokument16 SeitenIndividualized Neoantigen-Specific ImmunotherapyEhed AymazNoch keine Bewertungen
- Propofol Infusion SyndromeDokument7 SeitenPropofol Infusion SyndromewadejackNoch keine Bewertungen
- SenokotDokument1 SeiteSenokotKatie McPeek100% (1)
- PASSIVE MOVEMENT TECHNIQUESDokument58 SeitenPASSIVE MOVEMENT TECHNIQUESabdulahNoch keine Bewertungen
- Yes, it hurts here.Roxana: I'm going to give you an injection to numb the area. Now I'm going to check the tooth with the probe again. Does it still hurtDokument5 SeitenYes, it hurts here.Roxana: I'm going to give you an injection to numb the area. Now I'm going to check the tooth with the probe again. Does it still hurtCristian IugaNoch keine Bewertungen
- Head Eyes: Head To Toe AssessmentDokument2 SeitenHead Eyes: Head To Toe AssessmentVijungco88% (8)
- Rotationof 180 Degreesof Bilateral Mandibular First Molarsin Pediatric Patient ACase ReportDokument5 SeitenRotationof 180 Degreesof Bilateral Mandibular First Molarsin Pediatric Patient ACase Reportsaja IssaNoch keine Bewertungen
- Kala-Azar (Leishmaniasis) Symptoms, Signs, DiagnosisDokument36 SeitenKala-Azar (Leishmaniasis) Symptoms, Signs, Diagnosisatulbd2006Noch keine Bewertungen
- Autism AlarmDokument2 SeitenAutism AlarmUmair KaziNoch keine Bewertungen
- Appendicitis and Crohn's Disease GuideDokument11 SeitenAppendicitis and Crohn's Disease GuideJa DimasNoch keine Bewertungen
- DiagramDokument12 SeitenDiagramJessica CindyNoch keine Bewertungen
- Chapter 33 Prescott Innate Immunity PDFDokument7 SeitenChapter 33 Prescott Innate Immunity PDFneeru.bhagatNoch keine Bewertungen
- Managing Pain After AppendectomyDokument2 SeitenManaging Pain After AppendectomyChatoh SanaoNoch keine Bewertungen
- Electo Homeopathy MedicinesDokument3 SeitenElecto Homeopathy MedicinesKoushik MaitraNoch keine Bewertungen
- E NihssDokument5 SeitenE NihssNayeli SánchezNoch keine Bewertungen
- F 16 CLINNeurologicalObservationChartDokument2 SeitenF 16 CLINNeurologicalObservationChartRani100% (1)
- Comparative Efficacy of SPONTANEOUS BREATHING TRIAL Techniques in Mechanically Ventilated Adult Patients A ReviewDokument6 SeitenComparative Efficacy of SPONTANEOUS BREATHING TRIAL Techniques in Mechanically Ventilated Adult Patients A ReviewInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Afterword by Ilyene BarskyDokument5 SeitenAfterword by Ilyene Barskykkleiman_ppscNoch keine Bewertungen
- CL (Mr. Von) Mathematics (Mr. Ryan) : Trivia QuestionsDokument2 SeitenCL (Mr. Von) Mathematics (Mr. Ryan) : Trivia QuestionsRichard Andrew Abratique DandanNoch keine Bewertungen
- CEMONCDokument10 SeitenCEMONCApril GuiangNoch keine Bewertungen
- Peds Shelf NotesDokument88 SeitenPeds Shelf Notesskeebs23100% (8)
- Androgenetic Alopecia and Current Methods of TreatmentDokument4 SeitenAndrogenetic Alopecia and Current Methods of TreatmentPamela TrujilloNoch keine Bewertungen
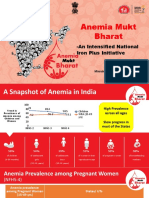
- Anemia Mukt Bharat: - An Intensified National Iron Plus InitiativeDokument23 SeitenAnemia Mukt Bharat: - An Intensified National Iron Plus InitiativeAnggun100% (1)
- Artificial MethodsDokument23 SeitenArtificial MethodsJanna Broqueza RodriguezNoch keine Bewertungen
- Nigeria Essential MedicinesDokument57 SeitenNigeria Essential MedicinesportosinNoch keine Bewertungen
- Plant Disease ResistanceDokument35 SeitenPlant Disease ResistanceAnuraj DaheriyaNoch keine Bewertungen