Beruflich Dokumente
Kultur Dokumente
Risk Factor
Hochgeladen von
HamtaroHedwig0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
3 Ansichten2 SeitenThis study evaluated the risk factors for neonatal seizures in a cohort of over 2 million California births. The risk was higher for males, infants of mothers over age 40, nulliparous mothers, and those with diabetes, fever, infection or late delivery. Maternal race/ethnicity was also associated with risk, with lower risk for Hispanic and Asian infants compared to Caucasian and African American infants. Identifying antenatal and intrapartum risk factors may help lower infant neurological morbidity and mortality from seizures.
Originalbeschreibung:
Risk factor
Originaltitel
Risk factor
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenThis study evaluated the risk factors for neonatal seizures in a cohort of over 2 million California births. The risk was higher for males, infants of mothers over age 40, nulliparous mothers, and those with diabetes, fever, infection or late delivery. Maternal race/ethnicity was also associated with risk, with lower risk for Hispanic and Asian infants compared to Caucasian and African American infants. Identifying antenatal and intrapartum risk factors may help lower infant neurological morbidity and mortality from seizures.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
3 Ansichten2 SeitenRisk Factor
Hochgeladen von
HamtaroHedwigThis study evaluated the risk factors for neonatal seizures in a cohort of over 2 million California births. The risk was higher for males, infants of mothers over age 40, nulliparous mothers, and those with diabetes, fever, infection or late delivery. Maternal race/ethnicity was also associated with risk, with lower risk for Hispanic and Asian infants compared to Caucasian and African American infants. Identifying antenatal and intrapartum risk factors may help lower infant neurological morbidity and mortality from seizures.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 2
enzymes may result in neuronal cell damage after febrile seizures.
That febrile seizures may
be less benign than generally assumed, as suggested by this study, is also apparent from a
recent report of MRI abnormalities that followed both simple and complex febrile seizures
(Hesdorffer DC et al. Epilepsia 2008;49:765-771), and an increased risk of sudden
unexpected death during 2 years after a first febrile seizure (Vestergaard M et al, Lancet
2008;372:457-463) (Ped Neur Briefs 2008;22:47-48 and 68-69). Recommendations for the
management of febrile seizures are outlined in a report of the Italian League Against
Epilepsy (Epilepsia Jan 2009;50(Suppl 1):2-6), with reference to the AAP Guidelines 1996,
1999, and to Fukuyama Y et al. Brain Dev 18:479-484. The possible benefits of prolonged
antiepileptic therapy to prevent recurrence of febrile seizures must be weighed against the
reported adverse cognitive effects. Currently, chronic prophylactic treatment is usually
discouraged, except in some patients with recurrent complex febrile seizures. More effective
antipyretic treatment, rapid viral testing and antiviral therapy should provide a more specific
approach to the prevention of recurrence of febrile seizures (Millichap JJ et al. J Infect Dis
2008;198:1093-4).
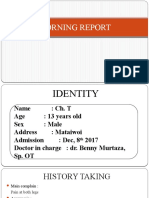
RISK FACTORS FOR NEONATAL SEIZURES
The association between maternal characteristics and birth admission seizures in a
cohort of 2.3 million California children born at >36 weeks’ gestation between 1998 and
2002 was evaluated using database statistics at the University of California San Francisco
and Davis, CA. The incidence of birth admission seizures was 0.95/1000 live births. The risk
of seizures was higher in male infants. Women age 40 years and older who were nulliparous,
had diabetes mellitus, intrapartum fever, or infection (chorioamnionitis) or delivered at >42
weeks had an increased risk of delivering an infant with seizures. Maternal/race ethnicity was
significantly associated with seizures, with a lower risk in infants of Hispanic and Asian
compared with Caucasian and African–American mothers. Identifying antenatal and
intrapartum risk factors for neonatal seizures might lower infant neurological morbidity and
mortality. Late delivery is one risk factor that might be avoided. (Glass HC, Pham TN,
Danielsen B, Towner D, Glidden D, Wu YW. Antenatal and intrapartum risk factors for
seizures in term newborns: a population-based study, California 1998-2002. J Pediatr Jan
2009;154:24-28). (Reprints: Hannah C Glass, University of California San Francisco,
Department of Neurology Box 0663, 521 Parnassus Ave, C-215, San Francisco, CA 94143.
E-mail: Hannah.Glass@ucsf.edu.).
COMMENT. Previous reports found a higher incidence of neonatal seizures, from 1
to 3.5 per 1000 in term infants, but other studies included seizures up to 28 days of life. The
increased risk of seizures at birth with maternal intrapartum fever and infection remains
elevated even when meningitis or neonatal infection is excluded. The risk is higher in febrile
multiparous compared to nulliparous women. A higher risk of seizures in infants born by
cesarean section during night hours is unexplained.
Unexplained seizures in an infant. A girl born by cesarean section at 38 weeks after
placental detachment developed generalized tonic-clonic seizures and tremors at 2 months.
Blood tests, EEG and MRI were normal. The mother was receiving amitriptyline for
postnatal depression and tension headache. The infant was treated with phenobarbital but
Pediatric Neurology Briefs 2009 3
seizures recurred, even during hospitalization. Metabolic studies were considered. At one
hospital stay, the seizure was complicated by ventricular tachycardia and fibrillation. After
transfer to intensive-care for resuscitation, she was comatose and hypotonic, her pupils were
dilated but reactive, and she was ventilated mechanically. She rapidly recovered
consciousness, breathed independently, and moved all limbs. Mother was unimpressed and
denied improvement in her child’s condition. Toxicological studies obtained because of
mother’s incongruous response disclosed serum concentrations of amitryptyline 350 mcg/L.
Mother admitted that she had administered amitryptyline drops to the infant for the past
month. When removed to live with maternal grandmother, the child remained well and
without seizures. The child was a victim of the factitious disorder, Munchausen’s syndrome
by proxy (Astuto M et al. Lancet Jan 3, 2009;373:94).
MRI FINDINGS AND SEIZURE OUTCOMES COMPARED IN FOCAL
CORTICAL DYSPLASIAS TYPES I AND II
Preoperative clinical, neuropsychological, EEG, and imaging features and surgical
outcomes of focal cortical dysplasias (FCD) types I and II were compared in 40 children with
refractory epilepsy and histopathologically confirmed FCD subtypes, in a study at Charles
University, Prague, Czech Republic and centers in Germany. FCD type I was identified in 24
and FCD type II in 16 patients. Seizure types were secondarily generalized tonic-clonic in
54% of FCDI and 37% FCDII; and infantile spasms in 21% of FCDI and 12% FCDII
patients. Status epilepticus occurred in 4% of FCDI and 12% of FCDII patients. Multilobar
involvement was found in 92% patients with FCDI and in 50% of FCDII patients. FCD type
I MRI findings include white matter signal changes on T2 images and/or FLAIR, and
reduction of white matter volume. FCD type II MRI showed increased cortical thickness,
transmantle sign, gray-white matter junction blurring, fluid-attenuated inversion recovery
(FLAIR) and proton density (PD) gray and white matter signal changes. Hippocampal
atrophy occurred in only 1 patient of each type. Patients with FCD type I showed EEG
continuous slowing more commonly; they had lower IQ levels and more behavioral
disorders. Postsurgical seizure freedom occurred in 21% FCD type I and in 75% FCD type II
patients (P<0.001). (Krsek P, Pieper T, Karimeier A et al. Different presurgical
characteristics and seizure outcomes in children with focal cortical dysplasia type I or II.
Epilepsia Jan 2009;50:125-137). (Respond: Pavel Krsek MD PhD, Department of Pediatric
Neurology, Charles University, Second Medical School, Motol University Hospital, V Uvalu
84, CZ 15006 Prague 5, Czech Republic. E-mail:pavel.krsek@post.cz).
COMMENT. FCD is reported in up to 25% of surgical patients with intractable
epilepsy and 5-10% of epilepsies. FCD Ia and Ib, and FCD IIa and IIb are classified
histopathologically. Type IIa is distinguished by dysmorphic, and IIb by balloon cells. FCD
type I patients present within the first year of life, and have multilobar involvement, high
seizure frequency, more complications, and a worse prognosis than FCD type II patients.
FCDI is more frequently associated with mental retardation and behavioral disorders, more
difficult to localize by EEG and MRI, and has less favorable surgical outcome. The authors
consider surgery except for hemispherectomy is frequently palliative in FCDI cases. FCD
type I should be considered a distinct entity.
Pediatric Neurology Briefs 2009 4
Das könnte Ihnen auch gefallen
- Europeanjournalofpaediatricneurology S SDokument1 SeiteEuropeanjournalofpaediatricneurology S SSeptianaNoch keine Bewertungen
- Tuberculous Meningitis With Initial Manifestation of Isolated Oculomotor Nerve PalsyDokument3 SeitenTuberculous Meningitis With Initial Manifestation of Isolated Oculomotor Nerve PalsyRakasiwi GalihNoch keine Bewertungen
- Anti-N-methyl-D-aspartate Receptor (NMDAR) Encephalitis: A Series of Ten Cases From A University Hospital in MalaysiaDokument6 SeitenAnti-N-methyl-D-aspartate Receptor (NMDAR) Encephalitis: A Series of Ten Cases From A University Hospital in MalaysiaAbhishek KayalNoch keine Bewertungen
- Encefalitis Autoinmune 2011 PDFDokument11 SeitenEncefalitis Autoinmune 2011 PDFDiana Vanessa SuarezNoch keine Bewertungen
- Stroke JounalDokument7 SeitenStroke JounalTony HermawanNoch keine Bewertungen
- Acute Hypotonia in An Infant (2017)Dokument3 SeitenAcute Hypotonia in An Infant (2017)nikos.alexandrNoch keine Bewertungen
- Incidence and Risk Factors For Seizures in Central Nervous System Infections in ChildhoodDokument6 SeitenIncidence and Risk Factors For Seizures in Central Nervous System Infections in ChildhoodLiani Toniaço BellesNoch keine Bewertungen
- Failure To ThriveDokument3 SeitenFailure To ThrivefernandoNoch keine Bewertungen
- Caso de EncefalitisDokument4 SeitenCaso de EncefalitisJonathan CuevaNoch keine Bewertungen
- Acute Disseminated Encephalomyelitis in Chicken Pox: Case ReportDokument2 SeitenAcute Disseminated Encephalomyelitis in Chicken Pox: Case ReportCorneliu VladNoch keine Bewertungen
- Clinical Reasoning: A Young Man With Recurrent Paralysis, Revisable White Matter Lesions and Peripheral Neuropathy Word Count: 945Dokument13 SeitenClinical Reasoning: A Young Man With Recurrent Paralysis, Revisable White Matter Lesions and Peripheral Neuropathy Word Count: 945aileenzhongNoch keine Bewertungen
- Casereport: Vishal Jain, MD, Anagha Deshmukh, MD, Stephen Gollomp, MDDokument4 SeitenCasereport: Vishal Jain, MD, Anagha Deshmukh, MD, Stephen Gollomp, MDlionkingNoch keine Bewertungen
- Holguin1967 MigraineDokument8 SeitenHolguin1967 MigraineArif Erdem KöroğluNoch keine Bewertungen
- Infectious Dan Autoantibody Associated EncephalitisDokument13 SeitenInfectious Dan Autoantibody Associated EncephalitisAyudiah ParamitaNoch keine Bewertungen
- Prion Disease: Kelly J. Baldwin, MD Cynthia M. Correll, MDDokument12 SeitenPrion Disease: Kelly J. Baldwin, MD Cynthia M. Correll, MDMerari Lugo Ocaña100% (1)
- Post-Traumatic Epilepsy (JNCN 2014-Summer)Dokument6 SeitenPost-Traumatic Epilepsy (JNCN 2014-Summer)skyclad_21Noch keine Bewertungen
- 278 977 1 SMDokument2 Seiten278 977 1 SMMohamed MukhrizNoch keine Bewertungen
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Dokument3 SeitenP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Aulia CandraNoch keine Bewertungen
- 1 s2.0 S1875957210600198 MainDokument9 Seiten1 s2.0 S1875957210600198 MainTaddesse taddesse Taddesse taddesseNoch keine Bewertungen
- Caso NeuroDokument12 SeitenCaso NeuroKaren Tapia ClarosNoch keine Bewertungen
- Cerebral Malaria-Research Desk by Ebenisha MajataDokument20 SeitenCerebral Malaria-Research Desk by Ebenisha MajataMedtalk ZambiaNoch keine Bewertungen
- Inflammatorybiomarkers Ofbirthasphyxia: Lina F. ChalakDokument10 SeitenInflammatorybiomarkers Ofbirthasphyxia: Lina F. ChalakRaul Morales VillegasNoch keine Bewertungen
- Epilepsy: New Advances: Journal ReadingDokument29 SeitenEpilepsy: New Advances: Journal Readingastra yudhaTagamawanNoch keine Bewertungen
- 2750-Article Text-14541-1-10-20231222Dokument4 Seiten2750-Article Text-14541-1-10-20231222Asti NuriatiNoch keine Bewertungen
- Clinical Approach to Sudden Cardiac Death SyndromesVon EverandClinical Approach to Sudden Cardiac Death SyndromesRamon BrugadaNoch keine Bewertungen
- Acute Disseminated Encephalomyelitis After Rabies Vaccination: One Case ReportDokument4 SeitenAcute Disseminated Encephalomyelitis After Rabies Vaccination: One Case ReportIJAR JOURNALNoch keine Bewertungen
- 1 Neuro A) IIHDokument3 Seiten1 Neuro A) IIHLoren boidNoch keine Bewertungen
- Encefalitis NmdaDokument9 SeitenEncefalitis Nmdamariafernandasv98Noch keine Bewertungen
- Version of Record:: ManuscriptDokument7 SeitenVersion of Record:: ManuscriptFlavia ChNoch keine Bewertungen
- Stroke in Children: Eview RticleDokument11 SeitenStroke in Children: Eview RticleÁgnes GedőNoch keine Bewertungen
- FTPDokument2 SeitenFTPDesta FransiscaNoch keine Bewertungen
- Adem LikeDokument4 SeitenAdem LikeRodrigo AriasNoch keine Bewertungen
- Idiopathic Intracranial Hypertension (By Dr. Rakshay)Dokument51 SeitenIdiopathic Intracranial Hypertension (By Dr. Rakshay)Rakshay KaulNoch keine Bewertungen
- Case Vignette. EpilepsyDokument8 SeitenCase Vignette. EpilepsyAizel ManiagoNoch keine Bewertungen
- Non Traumatic ComaDokument8 SeitenNon Traumatic ComasuyalamitNoch keine Bewertungen
- Prevention, Treatment, and Monitoring of Seizures in The Intensive Care UnitDokument17 SeitenPrevention, Treatment, and Monitoring of Seizures in The Intensive Care Unitanggi abNoch keine Bewertungen
- Educational Case: Brain Abscess: PMC DisclaimerDokument13 SeitenEducational Case: Brain Abscess: PMC DisclaimerANISA RIFKA RIDHONoch keine Bewertungen
- Winawer Et Al-2018-Annals of NeurologyDokument14 SeitenWinawer Et Al-2018-Annals of NeurologyAndoingNoch keine Bewertungen
- Clinical Outcomes of Neonatal Hypoxic Ischemic Encephalopathy Evaluated With Diffusion-Weighted Magnetic Resonance ImagingDokument6 SeitenClinical Outcomes of Neonatal Hypoxic Ischemic Encephalopathy Evaluated With Diffusion-Weighted Magnetic Resonance ImagingDrsandy SandyNoch keine Bewertungen
- Case ReportDokument3 SeitenCase ReportNeilavery WindaNoch keine Bewertungen
- JurnalDokument9 SeitenJurnalMelita Amalia AyubaNoch keine Bewertungen
- A Pain in The Butt - A Case Series of Gluteal Compartment Syndrome - PMCDokument6 SeitenA Pain in The Butt - A Case Series of Gluteal Compartment Syndrome - PMCchhabraanNoch keine Bewertungen
- The Dangers of PRESDokument5 SeitenThe Dangers of PRESShahnaaz ShahNoch keine Bewertungen
- Steroid Pulse Therapy in Herpes Simplex Encephalitis: Neurosciences July 2013Dokument3 SeitenSteroid Pulse Therapy in Herpes Simplex Encephalitis: Neurosciences July 2013Dwi KurniawanNoch keine Bewertungen
- Progressive Multifocal Leukoencephalopathy - A Case: Ovidiu Rosca, Elena-Cecilia Rosca, Lucian NegrutiuDokument5 SeitenProgressive Multifocal Leukoencephalopathy - A Case: Ovidiu Rosca, Elena-Cecilia Rosca, Lucian Negrutiunoorhadi.n10Noch keine Bewertungen
- Enterovirus ImagingDokument7 SeitenEnterovirus ImagingMomeneo NeoNoch keine Bewertungen
- Mitochondrial Case Studies: Underlying Mechanisms and DiagnosisVon EverandMitochondrial Case Studies: Underlying Mechanisms and DiagnosisRussell SanetoNoch keine Bewertungen
- CaseDokument24 SeitenCasecintaNoch keine Bewertungen
- A 5 Year Old Boy With Super Refractory Status Epilepticus and RANBP2 Variant WarrantingDokument8 SeitenA 5 Year Old Boy With Super Refractory Status Epilepticus and RANBP2 Variant WarrantingAlice MaulisovaNoch keine Bewertungen
- Fosnight S. Delirium in ElderlyDokument24 SeitenFosnight S. Delirium in ElderlyAnnisa MardhiyahNoch keine Bewertungen
- P71 NEJM DeliriumDokument10 SeitenP71 NEJM DeliriumGabriel CampolinaNoch keine Bewertungen
- Thijs 2019Dokument13 SeitenThijs 2019Priska CrisnandaNoch keine Bewertungen
- European Journal of Medical GeneticsDokument6 SeitenEuropean Journal of Medical GeneticsLarissa DmtNoch keine Bewertungen
- Magnetic Resonance Imaging Findings in Cerebral Palsy: R Yin, Ds Reddihough, MR Ditchfield and KJ CollinsDokument6 SeitenMagnetic Resonance Imaging Findings in Cerebral Palsy: R Yin, Ds Reddihough, MR Ditchfield and KJ CollinsKriti ShuklaNoch keine Bewertungen
- Pe 07070Dokument4 SeitenPe 07070Mich KingsNoch keine Bewertungen
- 453 Full PDFDokument5 Seiten453 Full PDFTank TankNoch keine Bewertungen
- 1536 FullDokument7 Seiten1536 FullJosue LayedraNoch keine Bewertungen
- Auto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementVon EverandAuto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementPetros EfthimiouNoch keine Bewertungen
- HI HA Syndrome JPEM Publicación Diciembre 2022Dokument5 SeitenHI HA Syndrome JPEM Publicación Diciembre 2022Boris FogelNoch keine Bewertungen
- Faktor Resiko Kejang PDFDokument10 SeitenFaktor Resiko Kejang PDFHamtaroHedwigNoch keine Bewertungen
- Asthma & Inhaled Corticosteroids (ICS) : Recommended Medications by Level of SeverityDokument2 SeitenAsthma & Inhaled Corticosteroids (ICS) : Recommended Medications by Level of SeverityHamtaroHedwigNoch keine Bewertungen
- LeucogenDokument2 SeitenLeucogenHamtaroHedwigNoch keine Bewertungen
- Larynx - Anatomy of LarynxDokument31 SeitenLarynx - Anatomy of LarynxHamtaroHedwigNoch keine Bewertungen
- Contoh Soal Fisika Berbahasa Inggris..Dokument5 SeitenContoh Soal Fisika Berbahasa Inggris..HamtaroHedwigNoch keine Bewertungen
- Subarachnoid Hemorrhage: Continuumaudio Interview Available OnlineDokument35 SeitenSubarachnoid Hemorrhage: Continuumaudio Interview Available OnlineJose DavidNoch keine Bewertungen
- Cancer Colon and Rectum (Wardah)Dokument23 SeitenCancer Colon and Rectum (Wardah)WardahAliNoch keine Bewertungen
- MethottexateDokument104 SeitenMethottexateFarha Elein KukihiNoch keine Bewertungen
- BrochureDokument2 SeitenBrochureapi-460857910Noch keine Bewertungen
- 2023 ACG Acute Liver FailureDokument26 Seiten2023 ACG Acute Liver FailuremohamedelsayedelmenyawyNoch keine Bewertungen
- Chap 26 - Assessing Male Genitalia (Interview Guide)Dokument3 SeitenChap 26 - Assessing Male Genitalia (Interview Guide)Mary Cielo DomagasNoch keine Bewertungen
- Nursing Care Plan #1: Assessment Diagnosis (NANDA-based) Planning Implementation Rationale EvaluationDokument9 SeitenNursing Care Plan #1: Assessment Diagnosis (NANDA-based) Planning Implementation Rationale EvaluationJoe RealNoch keine Bewertungen
- Shiki - Volume 01BDokument358 SeitenShiki - Volume 01BAmonNoch keine Bewertungen
- General Transfusion Practice Quiz For Rotating Medical StaffDokument3 SeitenGeneral Transfusion Practice Quiz For Rotating Medical StaffaymenNoch keine Bewertungen
- Pneumoslide LiteratratureDokument23 SeitenPneumoslide LiteratratureGREENCROSS PALDINoch keine Bewertungen
- Journal of Affective Disorders: Giulio Perugi, Elie Hantouche, Giulia Vannucchi, Olavo PintoDokument15 SeitenJournal of Affective Disorders: Giulio Perugi, Elie Hantouche, Giulia Vannucchi, Olavo PintoLuigi Maria PandolfiNoch keine Bewertungen
- Guillain-Barré Syndrome (GBS) : Prepared by Dr. Madiha Anees PT Asst. Prof/VP RCRS MS-PT, BS-PTDokument26 SeitenGuillain-Barré Syndrome (GBS) : Prepared by Dr. Madiha Anees PT Asst. Prof/VP RCRS MS-PT, BS-PTaneelala kanwal kanwalNoch keine Bewertungen
- Gas GangreneDokument16 SeitenGas GangreneGAURAVNoch keine Bewertungen
- Lombok Immunizationand Traveller231017-Dr - Agus SomiaDokument63 SeitenLombok Immunizationand Traveller231017-Dr - Agus Somiarinaldy IX9Noch keine Bewertungen
- Multipel Vulnus IncisivumDokument11 SeitenMultipel Vulnus IncisivumDeaz CressendoNoch keine Bewertungen
- Guidelines For Competency Based Postgraduate Training Programme For MD in PaediatricsDokument18 SeitenGuidelines For Competency Based Postgraduate Training Programme For MD in PaediatricsMohammed ameen mohammed AljabriNoch keine Bewertungen
- Date / Time Cues Nee D Nursing Diagnosis Patient Outcome Nursing Interventions Implemen Tation EvaluationDokument3 SeitenDate / Time Cues Nee D Nursing Diagnosis Patient Outcome Nursing Interventions Implemen Tation EvaluationJennifer Davis Condiman100% (1)
- Hip Arthroplasty in Lokoja PPT 2Dokument16 SeitenHip Arthroplasty in Lokoja PPT 2asi basseyNoch keine Bewertungen
- Abnormal GaitDokument14 SeitenAbnormal GaitAbolfazlNoch keine Bewertungen
- Crohns Disease Ebp Case Study PresentationDokument23 SeitenCrohns Disease Ebp Case Study Presentationapi-253093073Noch keine Bewertungen
- Life-Saving Esophageal Intubation in Neonate With Undiagnosed Tracheal Agenesis (A & A Case Reports, Vol. 9, Issue 1) (2017) DGDFGDokument2 SeitenLife-Saving Esophageal Intubation in Neonate With Undiagnosed Tracheal Agenesis (A & A Case Reports, Vol. 9, Issue 1) (2017) DGDFGMahdi WashahaNoch keine Bewertungen
- Abdominal Examination: OSCE ChecklistDokument2 SeitenAbdominal Examination: OSCE ChecklistWafa Abdalla100% (2)
- Reducción de Uratos y ERC NEJM 2020Dokument2 SeitenReducción de Uratos y ERC NEJM 2020Gabriel VargasNoch keine Bewertungen
- Art LineDokument10 SeitenArt LinerinamandarinaNoch keine Bewertungen
- Globus PharyngusDokument10 SeitenGlobus PharyngusamalNoch keine Bewertungen
- Piriformis SyndromeDokument8 SeitenPiriformis SyndromelewienNoch keine Bewertungen
- COVID-19 Vaccine Breakthrough Case Investigation: Information For Public Health, Clinical, and Reference LaboratoriesDokument2 SeitenCOVID-19 Vaccine Breakthrough Case Investigation: Information For Public Health, Clinical, and Reference LaboratoriesMarcusNoch keine Bewertungen
- Pregnant Women With UtiDokument9 SeitenPregnant Women With UtiJULIANNE BAYHONNoch keine Bewertungen
- Weather The Storm With Homeopathy - Homeopathy - Modern MedicineDokument4 SeitenWeather The Storm With Homeopathy - Homeopathy - Modern MedicineShubhankar BhowmickNoch keine Bewertungen
- Midwives Board Malaysia-Code of Professional Conduct and Practice of A MidwifeDokument8 SeitenMidwives Board Malaysia-Code of Professional Conduct and Practice of A MidwifeWei XinNoch keine Bewertungen