Beruflich Dokumente
Kultur Dokumente
Ignorance of Nutrition Is No Longer Defensible
Hochgeladen von
crackintheshatOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Ignorance of Nutrition Is No Longer Defensible
Hochgeladen von
crackintheshatCopyright:
Verfügbare Formate
Opinion
LESS IS MORE
PERSPECTIVE
Ignorance of Nutrition Is No Longer Defensible
Neal D. Barnard, MD It was the middle of the night, and the patient’s intra- A patient with diabetes receives a few obligatory
Adjunct Faculty, George venous (IV) line was clogged. Having refused the rec- diet-planning sessions shortly after diagnosis but is never
Washington University ommended foot amputation, the patient was receiving again asked about diet, even as the patient’s insulin doses
School of Medicine and
IV antibiotics to fight a festering infection, a complica- escalate and complications worsen.
Health Sciences,
Washington, DC; tion of longstanding diabetes. A patient with a heart complication is told that butter and
Physicians Committee During the few minutes it took to replace the IV cath- eggs have been exonerated in cardiovascular disease risk,
for Responsible eter, the patient let me know that whatever pride I held
Medicine, Washington, understands this to mean that diet does not matter, and
DC; and Barnard
in my phlebotomy skills was unjustified and that my ends up with progressive artery damage.
Medical Center, needle sticks only added to the misery of hospital life.
A patient with breast cancer saw a prior physician who
Washington, DC. Each time I was called to replace the IV during the pa-
mistakenly conveyed that soy products increase the risk
tient’s hospital stay, I found myself thinking, “Why not
of dying of cancer, and the patient avoids them despite
just get the amputation over with?” It seemed that the
compelling evidence that the reverse is true.
patient was only delaying the inevitable. But I was wrong.
This is not to suggest that physicians are not
The patient eventually left the hospital, foot still
interested in nutrition. A 2012 survey of primary care
attached.
physicians3 showed strong support for additional train-
My guess is that the patient eventually lost the
ing to improve care of obese patients. In 2018, the
battle, and it was not until much later in my career that
2 most-read articles in JAMA Internal Medicine related
it struck me that I and other members of the patient’s
to nutrition issues—one on the associations between cof-
clinical team were wrong in a much bigger way. As mag-
fee use and health outcomes4 and the other on the
netic resonance spectroscopy has elegantly demon-
potential benefits of organic produce and cancer risk.5
strated, the insulin resistance that is fundamental to type
But the curiosity about nutrition that physicians share
2 diabetes begins with the buildup of lipid particles in-
with the general public does not equate to clinical com-
side muscle and liver cells, interfering with insulin sig-
petence. In a 2018 survey,6 61% of internal medicine resi-
naling and pushing blood glucose values skyward. These
dents reported having little or no training in nutrition.6
intramyocellular and hepatocellular lipids come from
Physician inattention to nutrition is not only a function
food. With a sufficient change in the diet, they can di-
of insufficient training, but also of physicians’ own health
minish, and insulin resistance and diabetes itself can im-
and dietary practices. A 2012 study7 demonstrated that
prove and sometimes even disappear. Complications, like
physicians were less likely to record an obesity diagno-
the neuropathy that leads to foot ulcers and amputa-
sis (7% vs 93%; P < .001) when their own body weight
tions, can improve too.1
was higher than their estimate of the patient’s weight.
During the patient’s entire stay, no one on the medi-
There is no need to argue that medical schools need
cal staff had talked with the patient about the fundamen-
to teach nutrition—obviously, they do. Many medical
tal cause of the problem. Even though the roots of type 2
students can do little more than cough up the words
diabetes are in the everyday food choices that lead to obe-
“scurvy” or “cyanocobalamin” for a nutrition board
sityandinsulinresistance,wewerereadytoamputate,but
examination. Here is what I suggest as more immediate
never started a discussion about improving diet.
steps:
We might have been forgiven for ignoring diet’s role.
1. Nutrition should be a required part of continuing
Its importance was only gradually becoming clear. A few
medical education (CME) for physicians every-
years later, I had the opportunity to interview patients
where. It need not take the form of additional CME
with coronary artery disease participating in a clinical trial
hours but should be part of the hours currently
testing a nutrition and lifestyle intervention.2 Over the
required.
course of the trial, their chest pains had remitted, their
clinical status had greatly improved, and they were very 2. Physicians should work with registered dietitians.
appreciative. One participant, however, was angry. Pre- Physicians do not need to do their own diet
vious physicians, the patient said, had been ready to per- counseling, any more than they need to perform their
Corresponding form open heart surgery, but no one had communi- own radiographs or laboratory assays. But they must
Author: Neal D. cated that diet changes might be able to fix the problem recognize the role nutrition plays in disease, commu-
Barnard, MD, nicate it clearly to the patient, and refer the patient
Physicians Committee
much more easily.
for Responsible Overwhelming evidence has established the role of appropriately.
Medicine, 5100 nutrition in the pathogenesis of diabetes, cardiovascu- 3. Electronic medical record services should include
Wisconsin Ave, Ste customizable nutrition questions and handouts,
lar disease, obesity, hypertension, lipid disorders, can-
400, Washington, DC
20016 (nbarnard@ cer, and other health problems. Even so, the following facilitating both education and research on the
pcrm.org). clinical scenarios are not unheard of: effect of nutrition interventions.
jamainternalmedicine.com (Reprinted) JAMA Internal Medicine Published online July 1, 2019 E1
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 07/02/2019
Opinion Perspective
4. Physicians are role models and should embrace that fact. Just as a 5. Beyond medical practice, there is also a need for healthier foods
visible pack of cigarettes in a shirt pocket will erode their medical in schools, hospitals, and the workplace, as well as better gov-
credibility, the same is true for an inability to answer common nu- ernmental food policies. The medical community can support all
trition questions. So, as physicians learn to talk with patients about of these.
nutrition, they must also practice what they preach. To different au- Rather than allowing nutritional ignorance to fester like a gan-
thorities that means different things, but evidence would argue for grenous sore, the medical community can take advantage of
a low-fat, plant-based diet for both doctor and patient. current knowledge for patient benefit, as well as their own.
Published Online: July 1, 2019. 2. Barnard ND, Scherwitz LW, Ornish D. Adherence 5. Baudry J, Assmann KE, Touvier M, et al.
doi:10.1001/jamainternmed.2019.2273 and acceptability of a low-fat, vegetarian diet Association of frequency of organic food
Conflict of Interest Disclosures: Dr Barnard among patients with cardiac disease. J Cardiopulm consumption with cancer risk: findings from the
serves, without financial compensation, as Rehabil. 1992;12:423-431. doi:10.1097/00008483- NutriNet-Sante prospective cohort study. JAMA
president of the Physicians Committee for 199211000-00009 Intern Med. 2018;178(12):1597-1606. doi:10.1001/
Responsible Medicine and Barnard Medical Center, 3. Bleich SN, Bennett WL, Gudzune KA, Cooper LA. jamainternmed.2018.4357
both of which are nonprofit organizations providing National survey of US primary care physicians’ 6. Khandelwal S, Zemore SE, Hemmerling A.
education, research, and medical care related to perspectives about causes of obesity and solutions Nutrition education in internal medicine residency
nutrition. He has also authored books and given to improve care. BMJ Open. 2012;2(6):e001871. programs and predictors of residents' dietary
lectures related to nutrition and health, and has doi:10.1136/bmjopen-2012-001871 counseling practices. J Med Educ Curric Dev. 2018:
received royalties and honoraria from these 4. Loftfield E, Cornelis MC, Caporaso N, Yu K, Sinha 21(5):2382120518763360. doi:10.1177/
sources. R, Freedman N. Association of coffee drinking with 2382120518763360.
1. Bunner AE, Wells CL, Gonzales J, Agarwal U, mortality by genetic variation in caffeine 7. Bleich SN, Bennett WL, Gudzune KA, Cooper LA.
Bayat E, Barnard ND. A dietary intervention for metabolism: findings from the UK Biobank. JAMA Impact of physician BMI on obesity care and beliefs.
chronic diabetic neuropathy pain: a randomized Intern Med. 2018;178(8):1086-1097. doi:10.1001/ Obesity (Silver Spring). 2012;20(5):999-1005. doi:
controlled pilot study. Nutr Diabetes. 2015;5:e158. jamainternmed.2018.2425 10.1038/oby.2011.402
doi:10.1038/nutd.2015.8
E2 JAMA Internal Medicine Published online July 1, 2019 (Reprinted) jamainternalmedicine.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 07/02/2019
Das könnte Ihnen auch gefallen
- Casa Er 2014Dokument10 SeitenCasa Er 2014Siti HajarNoch keine Bewertungen
- Malnutrition Diagnoses in Hospitalized Patients: United States, 2010Dokument10 SeitenMalnutrition Diagnoses in Hospitalized Patients: United States, 2010MichealNoch keine Bewertungen
- Evans 2015Dokument7 SeitenEvans 2015Dr. Jaydeep MalakarNoch keine Bewertungen
- Research Agenda For Medical Cannabis in Palliative CareDokument3 SeitenResearch Agenda For Medical Cannabis in Palliative CarejclamasNoch keine Bewertungen
- Jco 2004 02 166Dokument4 SeitenJco 2004 02 166Cecilia ArgañarazNoch keine Bewertungen
- Jamainternal Heger 2023 PP 230001 1681398072.43626Dokument2 SeitenJamainternal Heger 2023 PP 230001 1681398072.43626Paola Cristini Gama SilvaNoch keine Bewertungen
- Postsepsis MorbidityDokument1 SeitePostsepsis MorbidityDaniel Enrique RubioNoch keine Bewertungen
- Hemoderivados en Cuidado CríticoDokument6 SeitenHemoderivados en Cuidado CríticoIvan Mauricio Palma BarraganNoch keine Bewertungen
- SUPER - Recom - Vaccin-ESRD-AJKD-2019Dokument9 SeitenSUPER - Recom - Vaccin-ESRD-AJKD-2019Ioana PanculescuNoch keine Bewertungen
- Improving End of Life CareDokument9 SeitenImproving End of Life CareM_LXNoch keine Bewertungen
- Improving Care For Overweight and Obese PatientsDokument5 SeitenImproving Care For Overweight and Obese PatientsJoshua DiaoNoch keine Bewertungen
- The Importance of Diagnosing and Managing ICU DeliriumDokument13 SeitenThe Importance of Diagnosing and Managing ICU DeliriumPablo RamirezNoch keine Bewertungen
- 1 - Educación Nutricional en La Escuela de MedicinaDokument2 Seiten1 - Educación Nutricional en La Escuela de MedicinakbuhringNoch keine Bewertungen
- JA A D: Saabg@health - Missouri.eduDokument3 SeitenJA A D: Saabg@health - Missouri.eduValentina AdindaNoch keine Bewertungen
- The AIDS Fighters - Brighthope, Ian Fitzgerald, PeterDokument196 SeitenThe AIDS Fighters - Brighthope, Ian Fitzgerald, Peterpdf ebook free download100% (1)
- Managing a Patient With Recurrent Gout AttacksDokument10 SeitenManaging a Patient With Recurrent Gout AttacksJesús Evangelista GomerNoch keine Bewertungen
- What'S The: Verdict?Dokument3 SeitenWhat'S The: Verdict?Cathy GabroninoNoch keine Bewertungen
- Protein and Calorie Requirements Associated With The Presence of ObesityDokument8 SeitenProtein and Calorie Requirements Associated With The Presence of ObesityRaman ChaudharyNoch keine Bewertungen
- 336.nut in Clin Prac - 2017 - Dickerson - Protein and Calorie Requirements Associated With The Presence of ObesityDokument8 Seiten336.nut in Clin Prac - 2017 - Dickerson - Protein and Calorie Requirements Associated With The Presence of ObesitytereNoch keine Bewertungen
- Journal: in This IssueDokument20 SeitenJournal: in This IssueLaura ZahariaNoch keine Bewertungen
- Kleinsinge 2018 - No AdherenciaDokument3 SeitenKleinsinge 2018 - No AdherenciaJuan camiloNoch keine Bewertungen
- Kleinsinge 2018 - No AdherenciaDokument3 SeitenKleinsinge 2018 - No AdherenciaJuan camiloNoch keine Bewertungen
- Precision Obesity Care On The Horizon: CirculationDokument3 SeitenPrecision Obesity Care On The Horizon: CirculationCarlosMoscosoNoch keine Bewertungen
- 1 s2.0 S2405457720301169 MainDokument16 Seiten1 s2.0 S2405457720301169 MainjvracuyaNoch keine Bewertungen
- 727 Outcomes of Antibiotic Use in Ischemic ColitisDokument2 Seiten727 Outcomes of Antibiotic Use in Ischemic ColitisDonNoch keine Bewertungen
- WischmeyerSurgNutritPOET20 tcm1423-138070Dokument12 SeitenWischmeyerSurgNutritPOET20 tcm1423-138070ckg5r6ykncNoch keine Bewertungen
- Harrisons Principles of Internal Medicine 21st Edition Vol 1 Vol Split PDF 1694700703964Dokument73 SeitenHarrisons Principles of Internal Medicine 21st Edition Vol 1 Vol Split PDF 1694700703964Clorinda RodriguezNoch keine Bewertungen
- Hospitalistas y Medicos de Familia, EditorialDokument1 SeiteHospitalistas y Medicos de Familia, EditorialJuan pablo Lopez MuñosNoch keine Bewertungen
- Jamainternal Gupta 2024 Oi 240004 1710785795.21061Dokument9 SeitenJamainternal Gupta 2024 Oi 240004 1710785795.21061Jose Artur AlbuquerqueNoch keine Bewertungen
- Williams 2020, Tutorial Devolopment and Implementation of A Multidisciplinary Preoperative Nutrition Optimization ClinicDokument12 SeitenWilliams 2020, Tutorial Devolopment and Implementation of A Multidisciplinary Preoperative Nutrition Optimization Clinicdiana perezNoch keine Bewertungen
- J Parenter Enteral Nutr - 2021 - Compher - Guidelines For The Provision of Nutrition Support Therapy in The AdultDokument30 SeitenJ Parenter Enteral Nutr - 2021 - Compher - Guidelines For The Provision of Nutrition Support Therapy in The AdultPabloNoch keine Bewertungen
- Nutrition Status and Risk Factors Associated With Length of Hospital Stay For Surgical PatientsDokument8 SeitenNutrition Status and Risk Factors Associated With Length of Hospital Stay For Surgical PatientsFarida MufidatiNoch keine Bewertungen
- ASPEN - Suplemental Parenteral Nutrition - Review of The Literature and Current Nutriton GuidelinesDokument11 SeitenASPEN - Suplemental Parenteral Nutrition - Review of The Literature and Current Nutriton GuidelinesRoberto Cárdenas GarcíaNoch keine Bewertungen
- J Parenter Enteral Nutr - 2021 - Compher - Guidelines For The Provision of Nutrition Support Therapy in The AdultDokument30 SeitenJ Parenter Enteral Nutr - 2021 - Compher - Guidelines For The Provision of Nutrition Support Therapy in The Adultsulemi castañonNoch keine Bewertungen
- International Journal of Gerontology: Thiago J. Avelino-Silva, Omar JaluulDokument6 SeitenInternational Journal of Gerontology: Thiago J. Avelino-Silva, Omar JaluulKaye Antonette AntioquiaNoch keine Bewertungen
- LRDokument22 SeitenLRمالك مناصرةNoch keine Bewertungen
- Obesity ManagentDokument54 SeitenObesity ManagentHugo David CoronelNoch keine Bewertungen
- Aspen Guidelines SurgicalDokument10 SeitenAspen Guidelines SurgicalJeshuanna DelgadoNoch keine Bewertungen
- Author Reply: BJU Int 2011 108 (Suppl 2)Dokument1 SeiteAuthor Reply: BJU Int 2011 108 (Suppl 2)Selliana Maretha Wijaya KusumaNoch keine Bewertungen
- NEJM Journal Watch Year in Review 2021Dokument20 SeitenNEJM Journal Watch Year in Review 2021Jaime DehaisNoch keine Bewertungen
- Acute Renal FailureDokument54 SeitenAcute Renal FailureNiala Almario100% (1)
- 1252-Article Text-5341-2-10-20200212Dokument6 Seiten1252-Article Text-5341-2-10-20200212Lizette AntonioNoch keine Bewertungen
- Competencies in Palliative Care For Cardiology FellowsDokument4 SeitenCompetencies in Palliative Care For Cardiology Fellowsandrey prawiroNoch keine Bewertungen
- Addressing Medicine's Bias Against Patients Who Are OverweightDokument3 SeitenAddressing Medicine's Bias Against Patients Who Are OverweightSean ChoNoch keine Bewertungen
- ARM en ICDokument11 SeitenARM en ICxLarcXDNoch keine Bewertungen
- 2011 Corrigan - Nutrition in Stroke PatientsDokument11 Seiten2011 Corrigan - Nutrition in Stroke PatientsAmy100% (1)
- Commentary: Nutritional Assessment and Length of Hospital StayDokument2 SeitenCommentary: Nutritional Assessment and Length of Hospital StayNjeodoNoch keine Bewertungen
- Medical Nutrition Therapy in Chronic Renal Disease: A Case StudyDokument6 SeitenMedical Nutrition Therapy in Chronic Renal Disease: A Case StudysarahNoch keine Bewertungen
- clinical nursing judgementDokument5 Seitenclinical nursing judgementapi-740444719Noch keine Bewertungen
- Carroll2017 PDFDokument1 SeiteCarroll2017 PDFLuisNoch keine Bewertungen
- Advantages of EnteralDokument11 SeitenAdvantages of EnteralClarestaNoch keine Bewertungen
- Vitamin C Deficiency in A University Teaching2008Dokument7 SeitenVitamin C Deficiency in A University Teaching2008Rossmery Mirella Vera PadillaNoch keine Bewertungen
- Geriatric Preoperative Optimization: A ReviewDokument10 SeitenGeriatric Preoperative Optimization: A Reviewalejandro montesNoch keine Bewertungen
- 2nd PeritonitisDokument11 Seiten2nd PeritonitisqweqweqwNoch keine Bewertungen
- Nutritional Assessment of The Critically Ill PatientDokument8 SeitenNutritional Assessment of The Critically Ill PatientDevani Bagus Aprinda0% (1)
- Stage III-B Cervical-Cancer of Young Age in Medical, Bioethics and Clinical Ethics PerspectivesDokument6 SeitenStage III-B Cervical-Cancer of Young Age in Medical, Bioethics and Clinical Ethics PerspectivesmusdalifahNoch keine Bewertungen
- s13054 017 1690 5Dokument16 Seitens13054 017 1690 5Anonymous SvlxqQeiNoch keine Bewertungen
- 2007 Pharmacy Times Inpatientglucosecontrol Szumita Greenwood Anger PendergrassDokument12 Seiten2007 Pharmacy Times Inpatientglucosecontrol Szumita Greenwood Anger Pendergrassnia rahayu wNoch keine Bewertungen
- Antibiotic Prophylaxis For Infective Endocarditis: CirculationDokument3 SeitenAntibiotic Prophylaxis For Infective Endocarditis: Circulationjagjit singhNoch keine Bewertungen
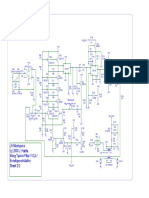
- JH Minotaurus Schematic p2 - Moog Taurus Filter VCA ENV EmulatorDokument1 SeiteJH Minotaurus Schematic p2 - Moog Taurus Filter VCA ENV EmulatorcrackintheshatNoch keine Bewertungen
- JH Minotaurus Schematic p1 - Moog Taurus Filter VCA ENV EmulatorDokument1 SeiteJH Minotaurus Schematic p1 - Moog Taurus Filter VCA ENV EmulatorcrackintheshatNoch keine Bewertungen
- Eviews F HerapeuticsDokument17 SeitenEviews F HerapeuticscrackintheshatNoch keine Bewertungen
- LVL - LOK-500 v1.13 SWITCH WIRINGDokument1 SeiteLVL - LOK-500 v1.13 SWITCH WIRINGcrackintheshatNoch keine Bewertungen
- Moog MF-101 LPF SchematicsDokument5 SeitenMoog MF-101 LPF SchematicscrackintheshatNoch keine Bewertungen
- Buddha CompDokument1 SeiteBuddha CompcrackintheshatNoch keine Bewertungen
- Match Transistors for Circuits with <40mΩ MismatchDokument5 SeitenMatch Transistors for Circuits with <40mΩ MismatchcrackintheshatNoch keine Bewertungen
- MF 101Dokument14 SeitenMF 101Kara JohnstonNoch keine Bewertungen
- Analysis of the SMR-4 VCF/VCA BoardDokument10 SeitenAnalysis of the SMR-4 VCF/VCA BoardcrackintheshatNoch keine Bewertungen
- Ladder Filter Design, Fabrication, & Measurement - EECS 142 Lab 3 Background ReadingDokument27 SeitenLadder Filter Design, Fabrication, & Measurement - EECS 142 Lab 3 Background ReadingcrackintheshatNoch keine Bewertungen
- LVL - Lok-500 v1.13 SchematicDokument1 SeiteLVL - Lok-500 v1.13 SchematiccrackintheshatNoch keine Bewertungen
- Russian FET CompressorDokument15 SeitenRussian FET CompressorcrackintheshatNoch keine Bewertungen
- LVL - LOK-500 v1.13 BOMDokument1 SeiteLVL - LOK-500 v1.13 BOMcrackintheshatNoch keine Bewertungen
- EHX Black Finger PDFDokument1 SeiteEHX Black Finger PDFГеоргий Ельцов100% (1)
- Electronics Today Magazine - January 1985 (ETI)Dokument76 SeitenElectronics Today Magazine - January 1985 (ETI)crackintheshat100% (1)
- Basic Transformer Hook Up DataDokument2 SeitenBasic Transformer Hook Up DatacrackintheshatNoch keine Bewertungen
- Pirani Gauge JST - 20131220Dokument9 SeitenPirani Gauge JST - 20131220crackintheshatNoch keine Bewertungen
- EC445 Final - Paper1Dokument22 SeitenEC445 Final - Paper1crackintheshatNoch keine Bewertungen
- EnigmaDokument2 SeitenEnigmaDwight JonesNoch keine Bewertungen
- Outcome of A Histamine-Restricted Diet Based On Chart Audit - JANICE M. VICKERSTAFF JONEJA PHD RDNDokument15 SeitenOutcome of A Histamine-Restricted Diet Based On Chart Audit - JANICE M. VICKERSTAFF JONEJA PHD RDNcrackintheshatNoch keine Bewertungen
- Summary of Terrorist Attacks of September 11, 2001Dokument6 SeitenSummary of Terrorist Attacks of September 11, 2001ShaktikumarNoch keine Bewertungen
- Barriga de Trigo - William DavisDokument19 SeitenBarriga de Trigo - William Davisfilipecosta1993Noch keine Bewertungen
- Amplifier Classification and Op-Amp ECG ApplicationDokument60 SeitenAmplifier Classification and Op-Amp ECG ApplicationcrackintheshatNoch keine Bewertungen
- Histamine and Histamine Intolerance1 3 Laura Maintz and Natalija Novak Znu00507001185 PDFDokument12 SeitenHistamine and Histamine Intolerance1 3 Laura Maintz and Natalija Novak Znu00507001185 PDFcrackintheshatNoch keine Bewertungen
- MIT Op-Amp Lab ReportDokument20 SeitenMIT Op-Amp Lab ReportcrackintheshatNoch keine Bewertungen
- Lab 06 - Mosfet & JfetsDokument64 SeitenLab 06 - Mosfet & JfetscrackintheshatNoch keine Bewertungen
- GP6 Users Manual enDokument61 SeitenGP6 Users Manual enJosé Antonio TapiaNoch keine Bewertungen
- Lab 2 - Transistor BiasDokument12 SeitenLab 2 - Transistor Biascrackintheshat100% (1)
- Lab 07 - Op-AmpsDokument49 SeitenLab 07 - Op-AmpscrackintheshatNoch keine Bewertungen
- Lab 05 - 3 Stage AmpliferDokument47 SeitenLab 05 - 3 Stage AmplifercrackintheshatNoch keine Bewertungen
- Diagnostic Diabetes: Diagnosing Maturity-Onset Diabetes of The Young (MODY)Dokument32 SeitenDiagnostic Diabetes: Diagnosing Maturity-Onset Diabetes of The Young (MODY)Christian SalimNoch keine Bewertungen
- Erectile Dysfunction Cure - How To Cure ED Naturally & Quickly & Enjoy Your Intimate Life (Jelqing, Male Enhancement, ED Cure, Erectile Dysfunction, Infertility) PDFDokument97 SeitenErectile Dysfunction Cure - How To Cure ED Naturally & Quickly & Enjoy Your Intimate Life (Jelqing, Male Enhancement, ED Cure, Erectile Dysfunction, Infertility) PDFWaleedNoch keine Bewertungen
- Diabetes and Gum Disease: Does Oral Health Matter?: Imogen Midwood, Penny HodgeDokument4 SeitenDiabetes and Gum Disease: Does Oral Health Matter?: Imogen Midwood, Penny HodgeNovena DpNoch keine Bewertungen
- International Nursing Conference Abstracts - AINEC 2018Dokument42 SeitenInternational Nursing Conference Abstracts - AINEC 2018Rika Fatmadona100% (1)
- Diabetic Retinopathy by-DuaneBryantMDDokument7 SeitenDiabetic Retinopathy by-DuaneBryantMDduanebryantmdNoch keine Bewertungen
- Social Orientation and Diabetes Distress in Japanese and American PatientsDokument7 SeitenSocial Orientation and Diabetes Distress in Japanese and American PatientsDebby Syahru RomadlonNoch keine Bewertungen
- Raymond Lo - The Year of The RatDokument4 SeitenRaymond Lo - The Year of The Ratay2004janNoch keine Bewertungen
- Ispad 2014Dokument290 SeitenIspad 2014Sheyla Alegre Pariona100% (1)
- Funda (Course Audit)Dokument16 SeitenFunda (Course Audit)Kath-Kath Cubillan RanayNoch keine Bewertungen
- Animal Aloksan PDFDokument14 SeitenAnimal Aloksan PDFTrias Ilmi PramudikaNoch keine Bewertungen
- Evaluation of Protective Effects of Euphorbia thymifolia Linn against Streptozotocin induced Diabetic Neuropathy in RatsDokument12 SeitenEvaluation of Protective Effects of Euphorbia thymifolia Linn against Streptozotocin induced Diabetic Neuropathy in Ratsrr48843Noch keine Bewertungen
- Basal Bolus InsulinDMT22009Dokument92 SeitenBasal Bolus InsulinDMT22009scribdNoch keine Bewertungen
- Current Challenges in Non-Invasive Insulin Delivery Systems A Comparative ReviewDokument26 SeitenCurrent Challenges in Non-Invasive Insulin Delivery Systems A Comparative Reviewridley45Noch keine Bewertungen
- FructosuriaDokument2 SeitenFructosuriaKaranja GitauNoch keine Bewertungen
- UntitledDokument54 SeitenUntitledapi-198310771Noch keine Bewertungen
- Non Communicable DiseasesDokument13 SeitenNon Communicable Diseaseszzzsubedi100% (1)
- GlimepirideDokument12 SeitenGlimepirideMobahil AhmadNoch keine Bewertungen
- Shoulder DystociaDokument13 SeitenShoulder Dystociarolla_hiraNoch keine Bewertungen
- 07 NovDokument32 Seiten07 NovEditorial TeamNoch keine Bewertungen
- Laboratory Tests To Evaluate Fluid StatusDokument52 SeitenLaboratory Tests To Evaluate Fluid StatusLester Exconde Alfonso0% (1)
- AMC MCQ Exam 2 Questions & Answer KeyDokument38 SeitenAMC MCQ Exam 2 Questions & Answer KeyVasile Rusnac100% (4)
- The Social Psychology of Exercise and Sport 2005 (For LydiaDokument280 SeitenThe Social Psychology of Exercise and Sport 2005 (For LydiaStephen Ladiator Cooper Shirley100% (1)
- Natural Medicines Used in The Traditional Chinese Medical System For Therapy of Diabetes MellitusDokument21 SeitenNatural Medicines Used in The Traditional Chinese Medical System For Therapy of Diabetes MellitusparibashaiNoch keine Bewertungen
- David Perlmutter Focus Autoimmune PDFDokument23 SeitenDavid Perlmutter Focus Autoimmune PDFutpal_thakar100% (6)
- Anatomia SufletuluiDokument1 SeiteAnatomia SufletuluiAlexandrina DeaşNoch keine Bewertungen
- Other Health Impairment Fact SheetDokument8 SeitenOther Health Impairment Fact SheetNational Dissemination Center for Children with DisabilitiesNoch keine Bewertungen
- Dka and HonkDokument30 SeitenDka and HonkignasachyntiaNoch keine Bewertungen
- Nutrition ManualDokument405 SeitenNutrition ManualRaghavendra Prasad100% (1)
- Management of Diabetes: DR Rukman Mecca M I 51 ST Batch Calicut Med CollegeDokument47 SeitenManagement of Diabetes: DR Rukman Mecca M I 51 ST Batch Calicut Med CollegeRukman MeccaNoch keine Bewertungen
- DietandCVDriskfactorsinBotswana Kwape PhDthesis2012 (1) (001-025)Dokument25 SeitenDietandCVDriskfactorsinBotswana Kwape PhDthesis2012 (1) (001-025)Indri Reskiawanti GalibNoch keine Bewertungen
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 5 von 5 Sternen5/5 (4)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyVon EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyBewertung: 5 von 5 Sternen5/5 (1)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsVon EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsBewertung: 4 von 5 Sternen4/5 (49)
- Proteinaholic: How Our Obsession with Meat Is Killing Us and What We Can Do About ItVon EverandProteinaholic: How Our Obsession with Meat Is Killing Us and What We Can Do About ItBewertung: 4.5 von 5 Sternen4.5/5 (19)
- The Fast800 Diet: Discover the Ideal Fasting Formula to Shed Pounds, Fight Disease, and Boost Your Overall HealthVon EverandThe Fast800 Diet: Discover the Ideal Fasting Formula to Shed Pounds, Fight Disease, and Boost Your Overall HealthBewertung: 5 von 5 Sternen5/5 (37)
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthVon EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthNoch keine Bewertungen
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisVon EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisBewertung: 3 von 5 Sternen3/5 (2)
- Forever Strong: A New, Science-Based Strategy for Aging WellVon EverandForever Strong: A New, Science-Based Strategy for Aging WellNoch keine Bewertungen
- Allen Carr's Easy Way for Women to Lose Weight: The original Easyway methodVon EverandAllen Carr's Easy Way for Women to Lose Weight: The original Easyway methodBewertung: 4.5 von 5 Sternen4.5/5 (18)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeVon EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNoch keine Bewertungen
- Glucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingVon EverandGlucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingBewertung: 5 von 5 Sternen5/5 (59)
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouVon EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouNoch keine Bewertungen
- Happy Gut: The Cleansing Program to Help You Lose Weight, Gain Energy, and Eliminate PainVon EverandHappy Gut: The Cleansing Program to Help You Lose Weight, Gain Energy, and Eliminate PainBewertung: 3.5 von 5 Sternen3.5/5 (6)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeVon EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeBewertung: 4 von 5 Sternen4/5 (3)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeVon EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeBewertung: 5 von 5 Sternen5/5 (1)
- Summary of Mary Claire Haver's The Galveston DietVon EverandSummary of Mary Claire Haver's The Galveston DietBewertung: 5 von 5 Sternen5/5 (1)
- Keto Friendly Recipes: Easy Keto For Busy PeopleVon EverandKeto Friendly Recipes: Easy Keto For Busy PeopleBewertung: 2 von 5 Sternen2/5 (1)
- Power Souping: 3-Day Detox, 3-Week Weight-Loss PlanVon EverandPower Souping: 3-Day Detox, 3-Week Weight-Loss PlanBewertung: 3.5 von 5 Sternen3.5/5 (3)
- The Longevity Plan: Seven Life-Transforming Lessons from Ancient ChinaVon EverandThe Longevity Plan: Seven Life-Transforming Lessons from Ancient ChinaNoch keine Bewertungen
- The Raw Food Detox Diet: The Five-Step Plan for Vibrant Health and Maximum Weight LossVon EverandThe Raw Food Detox Diet: The Five-Step Plan for Vibrant Health and Maximum Weight LossBewertung: 4 von 5 Sternen4/5 (22)
- The Toxin Solution: How Hidden Poisons in the Air, Water, Food, and Products We Use Are Destroying Our Health—AND WHAT WE CAN DO TO FIX ITVon EverandThe Toxin Solution: How Hidden Poisons in the Air, Water, Food, and Products We Use Are Destroying Our Health—AND WHAT WE CAN DO TO FIX ITBewertung: 5 von 5 Sternen5/5 (1)
- Lose Weight by Eating: 130 Amazing Clean-Eating Makeovers for Guilt-Free Comfort FoodVon EverandLose Weight by Eating: 130 Amazing Clean-Eating Makeovers for Guilt-Free Comfort FoodBewertung: 2 von 5 Sternen2/5 (1)
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreVon EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreBewertung: 5 von 5 Sternen5/5 (17)
- Ultrametabolism: The Simple Plan for Automatic Weight LossVon EverandUltrametabolism: The Simple Plan for Automatic Weight LossBewertung: 4.5 von 5 Sternen4.5/5 (28)
- Think Yourself Thin: A 30-Day Guide to Permanent Weight LossVon EverandThink Yourself Thin: A 30-Day Guide to Permanent Weight LossBewertung: 4.5 von 5 Sternen4.5/5 (22)
- The Ultimate Volumetrics Diet: Smart, Simple, Science-Based Strategies for Losing Weight and Keeping It OffVon EverandThe Ultimate Volumetrics Diet: Smart, Simple, Science-Based Strategies for Losing Weight and Keeping It OffNoch keine Bewertungen