Beruflich Dokumente
Kultur Dokumente
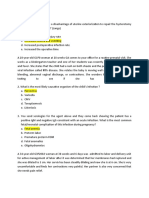
HANDOUT Chapter 11 Promoting Fetal and Maternal Health
Hochgeladen von
Eula ReyesOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
HANDOUT Chapter 11 Promoting Fetal and Maternal Health
Hochgeladen von
Eula ReyesCopyright:
Verfügbare Formate
Chapter 11
Assessing Fetal and Maternal Health
Health Promotion during pregnancy
Purposes of prenatal care:
Establish a baseline of present health
Determine gestational age of the fetus
Monitor fetal devt and maternal wellbeing
Identify women @ risk for complications
Minimize the risk of possible complications by anticipating and preventing probs before they
occur
Provide time for education about pregnancy, lactation and newborn care
Prenatal Management
1st prenatal visit
As soon as mother missed a menstrual period when pregnancy is suspected
Major causes of death for pregnancy:
Ectopic pregnancy, HPN, hemorrhage, embolism, anesthesia-relate complications
(intrapartum cardiac arrest)
Schedule of prenatal visits
Once a month: up to 1st 32 weeks
2 x a month (q 2 weeks): 32 – 36 weeks
4 x a month (q week): 36 – 40 weeks
Presence of danger signals of pregnancy – mother shd be instructed to report promptly for
evaluation
Conduct of initial visit
Baseline data collection
Basis for comparison
To screen for high-risk factors
OB history
Menstrual hx – menarche (onset, regularity, duration, frequency, character)
LMP, sexual hx, methods of contraception
PMP – menstrual period before the LMP
Conduct of Initial visit
Medical and surgical hx
Past illnesses and surgical procedures, current drugs used
Family hx
To detect illnesses or conditions that are transmittable
Current problems
ADL, discomforts, danger signs
Initial and subsequent visits
Vital signs
Temperature
rate: plus 10 – 15 bpm
RR: tend to be rapid and deep (16/min)
BP: tends to be hypotensive w/ supine position
Elevated BP = PIH
Do roll-over test in 1st trimester – for early detection of developing PIH by 20 – 24
weeks
Roll-Over Test
Procedure:
Place mother on LLR
Check BP until stable, may take 10 – 15 mins
Roll to supine
Check BP right away
Wait for 5 mins
Check BP again. Compare w/ 2nd diastolic reading
Interpretation:
Positive: in diastolic pressure greater than 20 mmHG; woman @ risk
Negative: in diastolic pressure less than 20 mmHG
Dyana M M Saplan, RN Phd 2019 1
Initial and subsequent visits
Weight
Checked in q visit
1st trimester: 1 lb/ mo (3 – 4 lb total)
2nd trimester: 0.9 – 1 lb/week to about 10 – 12 lb
3rd trimester: 0.5 – 1 lb/week 8 – 11 lb*
Weight is a measue of health of a mother
Urine testing for albumin and sugar
Sugar – ideally not more than 1+
Albumin – negative; nephritis
Fetal growth and devt assessment
Fundal height
FHT/FHR
Abdominal palpation
Quickening – 1st plus subsequent movements
Initial and subsequent visits
OB history
4-Point system: past pregnancies and perinatal outcomes (FPAL)
5-Point System: GFPAL
Estimates in Pregnancy
EDC/EDD
Naegele’s Rule
Mittendorf’s Rule
Date of Quickening
Fundic Height
AOG
McDonald’s Rule (2nd and 3rd trimester)
Bartholomew’s Rule of Fours
Estimated fetal weight (EFW)
Johnson’s Rule
Estimated fetal height in cm (EFL)
Haase’s Rule
Complete physical Examination
Includes internal gynecologic and bimanual examinations
Internal examination (IE)
Detects early signs of pregnancy
Chadwick’s, Goodell’s, and Hegar’s signs
Preparations for IE
Explanation
Void before
Proper positioning:
Draping
Instructions:
DON’Ts:
Complete physical Examination
Impt. Concerns of PE:
Breasts: look for changes, adequacy of breasts for breastfeeding, abnormal signs
Abdomen: Fundic height; Leopold’s
Pelvic measurements: done in the 3rd trimester to determine CPD (cephalo-pelvic
disproportions)
Extremities:
Discomforts: leg cramps, varicosities, pedal edema
Danger signs: + Homan’s sign = thrombophlebitis
Laboratory Tests
Blood studies
Complete blood count (CBC)
Hgb: 12 – 16g/dL
Hct: 37 – 47%
Leucocytosis – elevated WBC; normal
– Pregnancy: 5,500 – 11,500/mm3
– Labor: 20,000/mm3
– Postpartum: 25,000/mm3
Dyana M M Saplan, RN Phd 2019 2
Blood typing and Rh determination
Accdg to institution protocol, Serology for:
Syphylis (VDRL)
Rubella antibody titer
HIV
Alpha-fetoprotein (AFP) screening @ 16 – 18 weeks’ gestation to rule out neural
defects
Urine Test
Tested for sugar
Bacteria – asymptomatic bareriuria w/c can result in abortion in early pregnancy, and
premature labor, late in pregnancy
Laboratory Tests
Pelvic Lab tests
Collection of pelvic cultures
Pap test, culture for gonorrhea and Chlamydia
Bimanual examination
Usually last part of the initial PE
To identify cervical and uterine changes
Detect uterine size
Assess for deviation in expected shape and size
In all the necessary, prepare the client thru the ff steps:
Providing an explanation of the procedure
Physical prep specific to procedure
Provision of support to client and spouse; encouraging verbalization of concerns
Monitoring of client and fetus after procedure
Documentation prn
Assignment:
Rules in the different estimates in Pregnancy
Discomforts in pregnancy and management/relief measures for each discomfort (Tabulated)
Nutritional considerations:
Nutritional profile: pre-pregnant and current nutritional status
What is Pica?
What are some physical findings indicative of poor nutritional status? (@ least 5)
Factors/ conditions requiring special attention (@ least 5)
Nutrient needs:
Calories
Protein
Carbohydrates
Fiber
Fats
Essential minerals: Iron, calcium, sodium, folic acid, vitamins
Daily food needs/servings (Tabulated)
Food:
Number of servings each
Chapter 12
Promoting Fetal and Maternal Health
Health promotion during pregnancy begins with reviewing self-care
Self-Care Needs
Because pregnancy is not an illness, few special care measures other than common sense about self-
care are required
Average woman needs some help separating fact from fiction so that she can enjoy her pregnancy
unhampered by unnecessary restrictions
Be alert to the common misunderstandings, misconceptions, or inappropriate information of pregnancy
Bathing
Misconceptions:
Dyana M M Saplan, RN Phd 2019 3
Tub baths restricted @ one time – water would enter the vagina and cervix and contaminate
the uterine contents
Hot water touching the abdomen might initiate labor
Truths:
Normally vagina is in a closed position – danger of tub bath entering the cervix is minimal
Water temperature has no documented effect on initiating labor
During pregnancy, sweating tends
to because woman excretes Daily tub baths and
waste products for herself and showers are now
the fetus recommended
Vaginal discharge ed
As pregnancy advances – woman may have difficulty maintaining her balance when getting in
and out of a bath tub – change to showering or sponge bathing for her own safety
If membranes rupture or vaginal bleeding present – tub baths contraindicated because of
danger of contamination of uterine contents
During last month of pregnancy, when uterine cervix may begin to dilate – some health care
providers restrict tub bathing
Breast Care
Woman shd wear a firm, supportive bra w/ wide straps to spread weight across the shoulders
May need to buy a larger bra halfway through pregnancy – to accommodate ed breast size
If plans to breastfeed – choose bras suitable for breast-feeding so she can continue to use them after
baby’s birth
16th week of pregnancy – colostrum secretion begins in the breast
Sensation of a fluid discharge can be frightening unless woman is warned that this is a
possibility
Instruct to wash her breasts w/ clear tap water daily no soap coz it could be drying) – to
remove colostrums and reduce risk of infection
Dry her nipples well by patting them
If colostruman secretion is profuse – need to place gauze or breast pads inside her bra,
change frequently – to maintain dryness = constant moisture next to nipple can cause
excoriation, pain, and fissuring
Dental Care
Gingival tissue hypertrophy during pregnancy
Unless woman brushes well, pockets of plaque form readily bet. enlarged gumline and teeth
Encourage to see dentist regularly for routine examination and cleaning – 9 months is a
fairly long time to be w/o preventive dental care
Woman should question the need for x-rays during pregnancy – if necessary, abdomen should be
shielded w/ a lead apron
Tooth decay occurs from the action of bacteria on sugar = lowers pH of the mouth, creating an acid
medium etching or destruction of the enamel of teeth
Encourage to snack on nutritious foods – fresh fruits and vegetables (apples, carrots) to
avoid sugar coming in contact w/ teeth
If w/ trouble avoiding sweet snacks – suggest those that dissolve easily (chocolate bar) to
minimize the level of sugar in the mouth
Perineal Hygiene
Douching is contraindicated – force of irrigating fluid could enter cervix and lead to infection
Douching alters pH of the vagina = ed risk of bacterial growth
Dyana M M Saplan, RN Phd 2019 4
Dressing
Avoid:
o Garters May impede
o extremely firm girdles w/ panty legs lower extremity
o knee-high stockings circulation
Suggest: shoes w/ moderate to low heel – to minimize pelvic tilt and backache
Sexual Activity
Many need information to refute some myths about sexual relations in pregnancy that still exists, such
as:
o Coitus on expected date of period will initiate labor
o Orgasm will initiate labor; sexual relations w/o orgasm will not cause labor
o Coitus during fertile days of a cycle will cause a 2nd pregnancy or twins
o Coitus might cause rupture of membranes
Asking a woman @ a prenatal if she has any questions about sexual activity – allows her to voice
concerns; nurse can help dispel myths
Coitus is contraindicated in the ff. conditions:
o Hx of spontaneous miscarriage
o Ruptured membranes
o Vaginal spotting
o Deeply engaged presenting part
Advise caution about male oral – female genital contact = accidental air embolism has been reported
from this act during pregnancy
Couple shd be advised to find a comfortable position for intercourse
w/ non-monogamous sexual partner – partner needs to use a condom to prevent STIs during
pregnancy
women may use female condom throughout pregnancy
Sex in moderation is permitted but not during the last 6 weeks of pregnancy – increase incidence of
postpartum infection in women who engage in sex during the last 6 weeks
Exercises
Important during pregnancy to prevent circulatory stasis in the lower extremities and to strengthen the
muscles used in labor and delivery; it also offer a general feeling of well-being
Should be done in moderation
Exercise Programs:
o Exercises that target large muscle groups rhythmically – e.g. walking, are best
o Intensity of exercise program depends on the woman’s cardiopulmonary fitness
o Before any exercise program – woman must consult her physician or nurse-midwife
o If any complication of pregnancy occurs – e.g. bleeding or PIH – discontinue until she rechecks
w/ primary health care provider about continuing
Exercise shd be individualized – accdng to age; physical condition; customary amount of exercise (e.g.
swimming, tennis), not C/I unless done the first time; stage of pregnancy
Swimming may help relieve backache
o Membranes shd be intact
Dyana M M Saplan, RN Phd 2019 5
Recommended exercises:
1. Squatting and tailor-sitting
help stretch and strengthen perineal muscles
increases circulation in the perineum
make pelvic joints more pliable/flexible
when standing from the squatting position – raise buttocks first before raising head to
prevent postural hypotension
2. Pelvic rock
maintain good posture
relieves abdominal pressure and low backaches
strengthen abdominal muscles following delivery
3. Modified knee-chest position
Relieves pelvic pressure and cramps in the thighs and buttocks
4. Shoulder circling
Strengthens the muscles of the chest
5. Walking – BEST EXERCISE
Shd be encouraged to take daily walks unless bad weather, many levels of stairs or unsafe
neighborhood will not permit
6. Kegel
Relieves congestion and discomfort in pelvic region
Tones up pelvic floor muscles
Sleep
The optimal condition for body growth occurs when growth hormone secretion is @ its highest level –
that is, during sleep
This, plus overall increased metabolic demand of pregnancy – appears to be the physiologic reason
pregnant women need an ed amount of sleep or @ least rest to build new body cells during pregnancy
Pregnant women rarely have difficulty falling asleep @ night
o Trouble falling asleep – drink a glass of warm milk may help
o Relaxation techniques – lying quietly, systematically relaxing neck muscles, shoulder muscles,
arm muscles, and so on = may also be effective
Late in pregnancy – awakening @ short, frequent intervals by the activity of the fetus
o Leads to loss of REM sleep
o On rising, may feel anxious or not well-rested
May also awaken w/ pyrosis or dyspnea, if she has been lying flat – sleeping on 2 pillows or on a
couch w/ an armrest may be helpful
Rest period during the afternoon and full night of sleep – needed to obtain enough sleep and rest
during pregnancy
Modified Sim’s position w/ top leg forward – good resting or sleeping position
o Puts weight of the fetus on the bed, not on the woman, and allows good circulation in the lower
extremities
Avoid resting in a supine position – prevent supine hypotension syndrome
Avoid resting w/ knees sharply bent either when sitting or lying down – minimize risk of venous stasis
below the knee
Employment
Not C/I unless it entails:
exposure to toxic substances
Dyana M M Saplan, RN Phd 2019 6
lifting heavy objects
other kinds of physical strains
long periods of standing
or having to maintain body balance
Advise to walk about every few hours to break long periods of standing or sitting to promote circulation
Travel
Early in a normal pregnancy – no travel restriction
o Susceptible to motion sickness – shd not take any medication unless specifically prescribed or
approved by physician or nurse-midwife
Late in pregnancy – travel plans shd take into consideration the possibility of early labor, requiring birth
@ a strange setting where woman’s health history will be unknown
Advise a woman taking long trip by automobile:
o Plan for frequent rest or stretch periods q hour
o Q 2h, shd get out of the car and walk short distance – relieve stiffness and muscle ache; improve
lower extremity circulation = preventing varicosities, hemorrhoids and thrombophlebitis
Traveling by plane – not C/I; as long as plane has a well-pressurized cabin
o Some airline do not permit women who are more than 7 months pregnant
o Others require written permission from woman’s primary care provider
o Advise to inquire about these restrictions by calling airline
Advise additional immunizations (cholera vaccines) if traveling internationally
o All live virus vaccines (measles, mumps, rubella, yellow fever) – C/I during pregnancy, and shd
not be administered unless risk of disease outweighs risk to the pregnancy
Dyana M M Saplan, RN Phd 2019 7
Das könnte Ihnen auch gefallen
- Pregnancy Series I: All You Need to Know About Antenatal CareVon EverandPregnancy Series I: All You Need to Know About Antenatal CareNoch keine Bewertungen
- HANDOUT Chapter 11 Promoting Fetal and Maternal HealthDokument7 SeitenHANDOUT Chapter 11 Promoting Fetal and Maternal HealthClouiseNoch keine Bewertungen
- Antenatal CareDokument29 SeitenAntenatal Careعبدالكريم الاسدNoch keine Bewertungen
- HX and PX Obstetrics and GynecologyDokument21 SeitenHX and PX Obstetrics and GynecologyTadesse MuhammedNoch keine Bewertungen
- Antenatal Principles of Antenatal Care 2017Dokument60 SeitenAntenatal Principles of Antenatal Care 2017JanielWright100% (3)
- OBGYNE Must-KnowsDokument10 SeitenOBGYNE Must-KnowsPigwet KwisNoch keine Bewertungen
- Antenatal CareDokument21 SeitenAntenatal CareMariahNoch keine Bewertungen
- Prenatal Care Lecture Notes and Health TeachingsDokument12 SeitenPrenatal Care Lecture Notes and Health Teachingswanda100% (2)
- Antenatal CareDokument29 SeitenAntenatal CareFelaih Binasoy Dela Cruz100% (1)
- Assessing Fetal and Maternal Health: Prenatal Care: Health Promotion During PregnancyDokument8 SeitenAssessing Fetal and Maternal Health: Prenatal Care: Health Promotion During PregnancyMIKAELA DAVIDNoch keine Bewertungen
- Antenatal Care-Ova Emilia (2016)Dokument45 SeitenAntenatal Care-Ova Emilia (2016)Dwi WiraNoch keine Bewertungen
- ANC SreelakshmiDokument22 SeitenANC SreelakshmiEmyNoch keine Bewertungen
- High Risk PregnancyDokument113 SeitenHigh Risk PregnancyVivian Lajara100% (2)
- Antenatal CareDokument46 SeitenAntenatal CareKIPA SHRESTHANoch keine Bewertungen
- Ante PartumDokument49 SeitenAnte PartumNikhil TyagiNoch keine Bewertungen
- Process Flow of Clinical Service Antenatal Care: Information AreaDokument4 SeitenProcess Flow of Clinical Service Antenatal Care: Information ArearonronNoch keine Bewertungen
- Antenatal CareDokument30 SeitenAntenatal CareSheila WilsonNoch keine Bewertungen
- NCM 107 Lesson 9Dokument18 SeitenNCM 107 Lesson 9eirelav0902Noch keine Bewertungen
- OB ATI Study Guide: Initial Prenatal VisitDokument26 SeitenOB ATI Study Guide: Initial Prenatal Visitxoxo318Noch keine Bewertungen
- Maternal and Child Nursing Module 5Dokument4 SeitenMaternal and Child Nursing Module 5Ezekiel John GarciaNoch keine Bewertungen
- I Think I Am Pregnant?: Hawler Medical University Collage of Medicine OBGYN Department DR Trifa Y. MuttalibDokument18 SeitenI Think I Am Pregnant?: Hawler Medical University Collage of Medicine OBGYN Department DR Trifa Y. MuttalibZahraa HasanNoch keine Bewertungen
- Anc 1 2 1Dokument22 SeitenAnc 1 2 1Lemma AbishaNoch keine Bewertungen
- Highrisk RHDDokument9 SeitenHighrisk RHDmedzmedina2Noch keine Bewertungen
- Antenatal AssessmentDokument40 SeitenAntenatal Assessmentmanjuvm91% (11)
- ANTENATAL CARE Translate GooglingDokument26 SeitenANTENATAL CARE Translate GooglingLutfi ari206100% (2)
- Care of The Mother and The Fetus During The Perinatal PeriodDokument22 SeitenCare of The Mother and The Fetus During The Perinatal PeriodRoshin Tejero100% (1)
- Maternal and Fetal Wellbeing AssessmentDokument46 SeitenMaternal and Fetal Wellbeing AssessmentmariaNoch keine Bewertungen
- Antenatal Care AssessmentDokument67 SeitenAntenatal Care Assessmenthiral mistry100% (2)
- Abc Ob 2010Dokument351 SeitenAbc Ob 2010anjilozanoNoch keine Bewertungen
- Obstetrics and Gynecology Clerkship OverviewDokument16 SeitenObstetrics and Gynecology Clerkship Overviewselvie8750% (2)
- History TakingDokument26 SeitenHistory TakingShauie CayabyabNoch keine Bewertungen
- Teenage PregnancyDokument9 SeitenTeenage PregnancyRexelle RamosNoch keine Bewertungen
- Serdang Protocol ObgynDokument152 SeitenSerdang Protocol ObgynNadhirah ZulkifliNoch keine Bewertungen
- Gamo - Case Write-Up (TMC OB - Pre-LR 1)Dokument7 SeitenGamo - Case Write-Up (TMC OB - Pre-LR 1)JUAN VICTOR GAMONoch keine Bewertungen
- Prenatal Care: Muthia MutmainnahDokument77 SeitenPrenatal Care: Muthia MutmainnahBima NetNoch keine Bewertungen
- 2.1 Antenatal CareDokument27 Seiten2.1 Antenatal CaredeepaNoch keine Bewertungen
- Everything You Need to Know About Antenatal Care (ANCDokument42 SeitenEverything You Need to Know About Antenatal Care (ANCGamer StarNoch keine Bewertungen
- l5 Maternal HealthDokument34 Seitenl5 Maternal HealthNur AinaaNoch keine Bewertungen
- GRP Fritz Antepartal PeriodDokument7 SeitenGRP Fritz Antepartal PeriodthecoffeemugNoch keine Bewertungen
- Maternity Ati Key PointsDokument28 SeitenMaternity Ati Key PointsVin Lorenzo Campbell100% (2)
- Obsterics History C-I (Edited)Dokument14 SeitenObsterics History C-I (Edited)Tamam JamalNoch keine Bewertungen
- Importance of Prenatal CareDokument12 SeitenImportance of Prenatal CarePinkymekala HasanparthyNoch keine Bewertungen
- Antenatal Care EssentialsDokument6 SeitenAntenatal Care EssentialsadiNoch keine Bewertungen
- Antenatal CareDokument23 SeitenAntenatal Caremalaika khanNoch keine Bewertungen
- Antenatal CareDokument27 SeitenAntenatal CareFelaih Binasoy Dela CruzNoch keine Bewertungen
- Prenatal CareDokument40 SeitenPrenatal CareREVATHI H KNoch keine Bewertungen
- OB-GYN Soap NoteDokument9 SeitenOB-GYN Soap Notealex MusingilaNoch keine Bewertungen
- Antenatal AssessmentDokument40 SeitenAntenatal AssessmentKailash NagarNoch keine Bewertungen
- Antenatal Assessment of Foetal Wellbeing.Dokument30 SeitenAntenatal Assessment of Foetal Wellbeing.Kavya S MohanNoch keine Bewertungen
- Protocol Book For OBGYNDokument41 SeitenProtocol Book For OBGYNShabir BadakhshNoch keine Bewertungen
- Antenatal Care Guidelines for Pregnancy Screening and Risk FactorsDokument81 SeitenAntenatal Care Guidelines for Pregnancy Screening and Risk FactorsDorjee SengeNoch keine Bewertungen
- Maternal Measures and Prenatal Counselling AssessmentDokument13 SeitenMaternal Measures and Prenatal Counselling Assessmentvikas tak100% (1)
- Prenatal MGTDokument16 SeitenPrenatal MGTClairie Jhane ClaorNoch keine Bewertungen
- Diagnostic TestDokument5 SeitenDiagnostic TestCielo Alyssa IglianeNoch keine Bewertungen
- The High Risk Prenatal ClientDokument46 SeitenThe High Risk Prenatal ClientPaul Albert Agunod100% (2)
- Antenatal Care Maa PresentationDokument20 SeitenAntenatal Care Maa PresentationGaurav AcharyaNoch keine Bewertungen
- Role of nurse in prenatal careDokument40 SeitenRole of nurse in prenatal carejuanamay30gmailcomNoch keine Bewertungen
- Pre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandPre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- NSMDokument22 SeitenNSMNajj HasanNoch keine Bewertungen
- NCM TheoristsDokument21 SeitenNCM TheoristsEula ReyesNoch keine Bewertungen
- CH 15 Labor and Birth Part 1 HANDOUTDokument5 SeitenCH 15 Labor and Birth Part 1 HANDOUTEula ReyesNoch keine Bewertungen
- Blood Services Act of 1994Dokument2 SeitenBlood Services Act of 1994Eula ReyesNoch keine Bewertungen
- Nutrients: On The Reporting of Odds Ratios and Risk RatiosDokument2 SeitenNutrients: On The Reporting of Odds Ratios and Risk Ratiosfatihatus siyadaNoch keine Bewertungen
- 5.2 Intersectoral ApproachDokument55 Seiten5.2 Intersectoral ApproachShivangi SharmaNoch keine Bewertungen
- Plumbing Analysis SBDokument2 SeitenPlumbing Analysis SBCaryll BuenaluzNoch keine Bewertungen
- Xdeed3qtt - 1 - Concepts in The Care of at Risk and Sick Adult ClientsDokument14 SeitenXdeed3qtt - 1 - Concepts in The Care of at Risk and Sick Adult ClientsCamille GuintoNoch keine Bewertungen
- Statistics and Propaganda: by Jon RappoportDokument6 SeitenStatistics and Propaganda: by Jon RappoportSkogspilen Sprett100% (1)
- Workplace Safety and Health Management IssuesDokument2 SeitenWorkplace Safety and Health Management IssuesIsusiubestemoldovaNoch keine Bewertungen
- Cancer Prevention & Screening GuideDokument56 SeitenCancer Prevention & Screening Guidenoorulzaman84Noch keine Bewertungen
- Final DraftDokument5 SeitenFinal Draftapi-451064930Noch keine Bewertungen
- MRSA Care Plan 2011Dokument7 SeitenMRSA Care Plan 2011Adrian SavastitaNoch keine Bewertungen
- DR Ward ClassDokument36 SeitenDR Ward ClassChristy Mutia AlumbroNoch keine Bewertungen
- Oman's Oral Health and Dental Workforce IssuesDokument27 SeitenOman's Oral Health and Dental Workforce IssuesDivitNoch keine Bewertungen
- Workplace Hazards: Dr. Ardini S Raksanagara, dr.,MPH. Public Health Department Faculty of MedicineDokument31 SeitenWorkplace Hazards: Dr. Ardini S Raksanagara, dr.,MPH. Public Health Department Faculty of MedicinePutri Widya AndiniNoch keine Bewertungen
- 1421-PQ Contract 1 WSS Cahul Urban-Publication-201008-VvjDokument2 Seiten1421-PQ Contract 1 WSS Cahul Urban-Publication-201008-VvjLuminita NeteduNoch keine Bewertungen
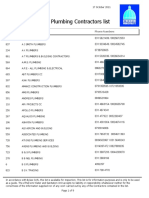
- Registered Plumbing ContractorsDokument9 SeitenRegistered Plumbing ContractorsviveknayeeNoch keine Bewertungen
- Letter Explanation To DoctorDokument1 SeiteLetter Explanation To DoctorDonnaNoch keine Bewertungen
- College of Nursing, Institute of Liver and Biliary Sciences (Ilbs)Dokument1 SeiteCollege of Nursing, Institute of Liver and Biliary Sciences (Ilbs)MoonNoch keine Bewertungen
- Pengobatan Ispa Dalam Jurnal PenelitianDokument6 SeitenPengobatan Ispa Dalam Jurnal PenelitianEzy RizkiNoch keine Bewertungen
- Detection & Treatment Training Flier - 04-20-12Dokument1 SeiteDetection & Treatment Training Flier - 04-20-12catholicpeepNoch keine Bewertungen
- Fetal risks of macrosomia in diabetic pregnanciesDokument27 SeitenFetal risks of macrosomia in diabetic pregnanciesIful SaifullahNoch keine Bewertungen
- By:-Firoz Qureshi Dept. Psychiatric NursingDokument46 SeitenBy:-Firoz Qureshi Dept. Psychiatric NursingrajeshwariNoch keine Bewertungen
- Widal Test - Introduction, Principle and Procedure - Metropolis BlogsDokument9 SeitenWidal Test - Introduction, Principle and Procedure - Metropolis BlogsinfoankitksNoch keine Bewertungen
- Case Presentation: Typhoid FeverDokument16 SeitenCase Presentation: Typhoid FeverCalingalan Hussin CaluangNoch keine Bewertungen
- Kualitas Bakteriologis Dan Higiene Sanitasi Pada Depot Air Minum Isi Ulang Di Wilayah Kerja Puskesmas II Denpasar BaratDokument6 SeitenKualitas Bakteriologis Dan Higiene Sanitasi Pada Depot Air Minum Isi Ulang Di Wilayah Kerja Puskesmas II Denpasar BaratCV KARYA BERSAMANoch keine Bewertungen
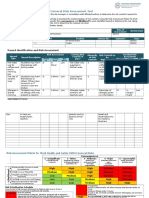
- Risk Assessment Grandparents DayDokument5 SeitenRisk Assessment Grandparents Dayapi-436147740Noch keine Bewertungen
- A social history of the science of food analysis and the control of adulteration, Atkins, P.J. (2013), pp 97-108 in Murcott, A., Belasco, W. and Jackson, P. (Eds) The Handbook of Food Research Oxford: BergDokument12 SeitenA social history of the science of food analysis and the control of adulteration, Atkins, P.J. (2013), pp 97-108 in Murcott, A., Belasco, W. and Jackson, P. (Eds) The Handbook of Food Research Oxford: BergPeter J. AtkinsNoch keine Bewertungen
- HFMD Parent Orientation Narrative ReportDokument7 SeitenHFMD Parent Orientation Narrative ReportGerald CiudadNoch keine Bewertungen
- Endometritis History: Disorder Signs and Symptom ManagementDokument8 SeitenEndometritis History: Disorder Signs and Symptom ManagementLourdes Angelie G. VirayNoch keine Bewertungen
- Tobacco Control Needs AssessmentDokument7 SeitenTobacco Control Needs AssessmentIndonesia TobaccoNoch keine Bewertungen
- LabCorp+Virology+Report+Quantitative+RNA CDokument5 SeitenLabCorp+Virology+Report+Quantitative+RNA CSooah ParkNoch keine Bewertungen
- Safety and Clinical Management in Clinical Microscopy SectionDokument21 SeitenSafety and Clinical Management in Clinical Microscopy SectionTom Anthony TonguiaNoch keine Bewertungen