Beruflich Dokumente
Kultur Dokumente
Coulter AC.T 5 Diff Procedure
Hochgeladen von
Luis Ferdinand Dacera-Gabronino Gamponia-NonanOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Coulter AC.T 5 Diff Procedure
Hochgeladen von
Luis Ferdinand Dacera-Gabronino Gamponia-NonanCopyright:
Verfügbare Formate
Procedure: Coulter AC.
T 5 Diff Cap Pierce (CP) Operations Procedure
Non-SMILE created resources
Author: N/A Document Number: Equ27-01
Effective (or Post) Date: 17 July 2008
Document Origin: MU-JHU Research Company: MU-JHU
Collaboration Laboratory (Uganda)
SMILE Approved by: Jo Shim
Review by Heidi Hanes Review date 9-Feb-12
SMILE Comments: This document is provided as an example only. It must be revised to accurately reflect your lab’s
specific processes and/or specific protocol requirements. Users are directed to countercheck facts when considering
their use in other applications. If you have any questions contact SMILE.
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
ROCHE COBAS-INTEGRA 400 PLUS CHEMISTRY – OPERARTION SOP
Effective Date: Revision #1.0 Supersedes Rev#
14 Jun, 2005 0.0
Approved By Signature Date
Laboratory Medical Director
Laboratory Administrator
Annual Review By Signature Date
(Lab Supervisor/Lab Management)
Revised/Prepared By Signature Date
March 2005 Rev# 1.0 Page 2 of 12
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
1. Principle
Complete blood count is performed on patients to identify normal and abnormal blood parameter results,
which guide the physician/clinician on the appropriate course of therapeutic management to the patients
and also to identify patient results that require additional studies.
The Coulter AC.T 5diff Cap Pierce (CP) hematology analyzer is a 26-parameter, fully automated
hematology analyzer, including a five-part leukocyte differential counter, capable of analyzing samples
in a closed vial mode. The instrument consists of the Analyzer, the Workstation, a barcode wand, the
printer and a software kit.
The Beckman-Coulter 5AcT diff analyzer is a quantitative, automated hematology analyzer for in-vitro
diagnostic use in clinical laboratories. It utilizes Coulter method to count and size Red Blood Cell
(RBC), and Platelet (Plt) RBC/Plt dilution and White Blood Cell (WBC)/Baso dilution. To perform a
complete leukocyte differential, the Absorbance Cytochemistry Technology (AcV) and WBC/BASO
methodology are used in the AcT5 diff analyzer.
The analyzer uses Acv (Absorbance Cytochemistry and volume) technology, which is used to analyze the
final RBC/Plt dilution and the WBC/BASO dilution. This electronic method of counting and sizing
particles is based on the fact that cells, which are poor conductors of electricity, will interrupt a current
flow. The impedance variation generated by the passage of non-conductive cells through a small,
calibrated aperture is used to determine the count (number of particles) and size (volume) of the particles
passing through the aperture within a given time period.
.
2. Specimen Collection and Handling
2.1. The required sample is EDTA (K2, K3 salt) whole blood.
2.2. The blood proportion to anticoagulant should be as specified by the tube manufacturer.
2.3. EDTA vacutainer tubes (3-7 mL) with total sample volume of < 1 mL will be noted as ‘short
sample’.
2.4. EDTA vacutainer tubes (3-7 mL) with total sample volume of < 0.5 mL should not be used due to
possible anticoagulant dilution effect on the results.
2.5. Minimum sample size is 53 uL from a well-mixed EDTA whole blood sample of adequate total
volume.
2.6. Samples should be stored/analyzed at room temperature (16 to 35 0C).
2.7. Samples should be analyzed within 24 hours of collection.
2.7.1. Samples > 24 hours old but <48 hours old may be analyzed if sample replacement is not
possible. Note “sample x hours old” under sample comments.
2.8. Do not refrigerate samples for platelet and differential counts.
2.9. If necessary, samples should be brought to room temperature (16 to 35 0C) before analyzing.
2.10. Unacceptable samples
2.10.1. Clotted samples
2.10.2. Samples with 3-4+ hemolysis
2.10.3. Samples >48 hours old
Note: Document unacceptable sample under sample comments on requisition and on
computer report. Notify study/clinic as soon as possible so that the sample may be replaced
in a timely manner.
3. Materials & Equipments Required
3.1. AC.T 5diff CP Coulter Analyzer
3.2. AC.T 5diff Coulter analyzer hardware/software
3.2.1. Hewlett Packard Monitor
3.2.2. Hewlett Packard Deskjet Printer
3.3. AC.T Tm 5diff Diluent Solution
3.4. AC.TTm 5diff Fix
March 2005 Rev# 1.0 Page 3 of 12
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
. m
3.5. AC TT 5diff WBC Lyse
3.6. AC.TTm 5diff Hgb Lyse
3.7. AC.TTm 5diff Rinse
3.8. AC.TTm 5diff Control Plus for Low, Normal and High levels
3.9. Personal Protective Equipments (i.e., Gloves , Splash protection)
4. Reagent Preparation
4.1. No reagent preparation is required for the Ac.T 5 diff reagents or AC.TTm 5diff Control Plus.
4.2. Refer to ‘Changing Reagents’ SOP for further instructions.
5. Storage and Stability
5.1. AC.T Tm 5diff Diluent, AC.TTm 5diff Fix, AC.TTm 5diff WBC Lyse, and AC.TTm 5diff Rinse are stored
at 2-30 0C. Opened container stability is per expiration dating listed on the containers.
5.2. AC.TTm 5diff Hgb Lyse is stored at 2- 25 0C. Opened container stability is 90 days.
5.3. AC.TTm 5diff Control Plus is stored at 2- 8 0C and is stable per the expiration dating listed on the
vials.
6. Calibration
6.1. Calibration is performed under the following conditions:
6.1.1. Every six (6) months
6.1.2. Whenever any instrument component involving primary measurement characteristics (such
as an aperture) is replaced.
6.1.3. Whenever the quality control program results suggest a calibration problem.
6.2. Refer to the Act 5diff Calibration SOP for calibration instructions.
7. Quality Control – Internal
7.1. AC.TTm 5diff Control Plus (low, normal, high) or equivalent will be run every 8 hours (each day of
use).
7.2. Controls must be run prior to running any patient samples.
7.3. Make sure the controls are run in the correct level.
7.3.1. If a control is run in the wrong level, delete the result and make a note in the daily QC log.
7.3.2. If the control result is not deleted before running the next sample it will become part of the
statistical database for the lot.
7.4. All control values must be within the expected ranges.
7.5. If any control value is outside the expected range, repeat the control once.
7.5.1. If the control value comes in on repeat, note it on the daily QC log and continue.
7.5.2. If the control value does not come in on the repeat, consult the laboratory supervisor (LS) or
Team Lead (TL) for further action.
7.6. Review the Levey-Jennings graphs for potential QC problems. Use the Westgard Multi-rule
technique along with the data patterns presented on the Levey-Jennings graphs as indicators of
possible problems. Notify the Lab Supervisor immediately if any of the following QC problems
are noted or suspected
7.6.1. Trends
7.6.2. Shifts
7.6.3. Bias
7.6.4. Precision
7.6.5. Control degradation
7.6.6. Excessive notes in the daily QC log regarding instrument or control performance (i.e.
more than 1 entry per week or more than 1 entry for the same problem in one month).
7.7. If the instrument-reagent-control system appears to be running as expected and the controls are
running within 2SD, the Levey-Jennings graphs may be printed and reviewed with the laboratory
March 2005 Rev# 1.0 Page 4 of 12
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
Team Lead or supervisor (at least Monthly). If problems are suspected, print the L-J’s charts
daily for review until resolved.
7.8. All unexpected results must be documented on the daily QC log along with action taken and final
resolution.
7.9. Refer to the ‘AC.TTm 5diff Control Plus’ SOP for information on changing control lots.
8. Quality Control – IQAP
8.1. Beckman-Coulter IQAP program provides peer comparison for the ‘AC.TTm 5diff Control Plus’
results.
8.2. At the end of each ‘AC.TTm 5diff Control Plus’ lot, the lab data will be submitted to the IQAP
program for additional analysis and peer comparison.
8.3. The LS/TL will review and sign the IQAP reports. Any potential problems will be addressed in a
timely manner.
8.4. The IQAP reports will be kept as part of the CoreLab External QC program.
8.5. Refer to the ‘AC.TTm 5diff Control Plus’ SOP for information on submission of results to IQAP.
9. Procedure – Start-Up
9.1. General Rules:
9.1.1. Only personnel trained on the machine should handle /operate Ac.T Coulter Analyzer.
9.1.2. All Coulter Counter Users must sign the Log Sheet before and after use.
9.1.3. Always check the reagents levels before startup according to procedure for changing
reagents.
9.1.4. Operating the instrument with the doors and/or covers open can cause personal injury. When
you operate the instrument, be sure all covers and door are closed. Note: There is a risk of
breaking the probe if this is neglected.
9.1.5. Only anti-coagulated blood samples are to be analyzed using this machine.
9.1.6. Make sure the sample tube matches the correct position on the tube holder in place.
[Example: 2ml EDTA Vacuette sample tube is placed in position 1]
9.1.7. In case of any difficulty with the software, please always ask for assistance from your
supervisor who will then report this in the Coulter Log Sheet.
Note: Never attempt to troubleshoot a noted machine technical error. Report to your supervisor
who should inform the Manufacturer’s technical staff for appropriate plan of action.
Note: Risk of instruments damage and/or erroneous results if you install additional software onto
the personal computer or if you use the personal computer for anything other than stated
within this documentation
9.2. Start Up (overview)
9.2.1. If the automatic startup feature is enabled, Start Up is automatically run when the instrument
is turned on. This Start Up cycle gives the background counts. If the background counts are
not within the acceptable limits, the instrument automatically performs a repeat Start Up, up
to two more times.
Note: If startup fails after the third attempt, A STARTUP FAILED message appears on the screen
and on the report.
9.2.2. Background limits are fixed and cannot be changed, therefore DO NOT attempt to correct.
The acceptable background limits are:
March 2005 Rev# 1.0 Page 5 of 12
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
WBC ≤ 0.3 x 103/µL3
RBC ≤ 0.03 x 106/µL3
Hgb ≤ 0.3 g/dL
Plt ≤ 7.0 x 103/µL3
.
9.3. Power Up the System
9.3.1. To ensure the correct operation of the system, it is important that the “Power Up” and
“Power Down” sequences are done in the proper order.
9.3.1.1. Check the waste container to determine if it needs to be replaced.
9.3.1.2. Verify that the Printer is ready and has paper
9.3.1.3. Verify that the analyzer’s ac power cord is plugged in the power source
9.3.1.4. Turn the workstation computer on:
Turn the PC ON.
Turn the Monitor ON.
Allow sufficient time for the computer to complete its internal checks.
9.3.2. At the analyzer: Turn the power on. Verify that the red LED (in front) remains illuminated.
9.3.3. Log on to the workstation:
Type your user name, and press TAB
Type your password.
Press ENTER or OK to log on
9.3.4. At the workstation:
Wait for the Analyzer /logs window to appear.
Wait about 30 seconds for the Analyzer to communicate and to connect.
9.3.5. Verify that the Analyzer and Workstation connection is made:
Verify that appears in the lower right corner of the screen.
Note: indicates that the analyser and workstation connection is
not made.
9.3.6. If the Analyser and Workstation connection fail, repeat steps 9.3.2 through 9.3.5. Starting with:
Verify that the green LED is illuminated (Ready).
9.3.7. Allow Start Up to finish.
9.3.8. Review the Start Up results status:
If “Failed” appears, tab StartUp log and evaluate the numeric results.Then Start Up
to initiate another Start Up routine.
If “Passed” appears, Start Up log automatically prints ( in tabular form) If auto print is
enabled.
March 2005 Rev# 1.0 Page 6 of 12
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
9.3.9. Add comments to the Start Up log if desired.
If the Add comments box appeared automatically, type your comments.
To access the Add comments box, tab the Startup log then select Add comments
button, then type your comments.
Click to save your comments.
Note: If the system has remained idle for a longer period of time you will be prompted to do
a Start Up or a Mini Prime.
9.4 Power Down the System
9.4.1 . Before performing certain replacement procedures or at the end of the day, you
will be instructed to power down the system to prevent personal injury from electric shock.
Follow this sequence:
a) Click Yes to confirm that you want to logoff.
b) Wait while the Workstation closes its program
c) When the Begin Log Box appears simultaneously press: Ctrl +Alt +Delete
d) Choose Shut Down
e) Verify that only Shut Down is selected. Click OK “It is now safe to turn off your
computer” Appears.
f) Turn off the Workstation. Do not Restart
g) Turn off the Analyzer
Note: Remember that all Coulter Counter Users must sign the Log Sheet before and after
use.
10. Running Patient Samples using the Work-list.
10.1. Autonumbering Off: If auto numbering is disabled on your system, you must manually enter the
sample ID (up to 16 characters) by typing it at the keyboard or by scanning it using the barcode
reader (if available)
Note: Beckman Coulter recommends that you verify each barcode reading to ensure correct
sample identification.
10.2. Prepare the Workstation for sample processing:
10.2.1. Click the Results button.
10.2.2. Verify that the active archive is open (white background on Worklist and Results
list) If an old archive is open (green background) click File >>>Close Archive.
10.2.3. Every Monday, the previously opened archive should be closed and a new archive opened
by >>>File >>>New Archive
Note: You cannot create a new archive until any previous opened archive, if any, is
closed.
March 2005 Rev# 1.0 Page 7 of 12
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
10.2.4. Click + to open the Add/Edit Worklist window
10.2.5. Scan the sample ID from the barcode label on the sample tube as follows:
Position the barcode reader over the barcode label.
Squeeze the trigger button. If the barcode is successfully read, the reader beeps, the
LED of the reader illuminates, and the cursor advances to the next field.
Verify the barcode reading to ensure that the Sample ID in the Sample
ID Next field is correct.
10.2.6. Select CBC/DIFF as the panel of analysis.
10.2.7. Select the appropriate Flagging Set, based on age and sex of the patient.
10.2.8. Enter the Date and Time the specimen was collected
10.2.9. Type your comments e.g., xxxx (Optional)*
10.2.10.Move to the Patient ID field and fill the dialog boxes with relevant information.
10.2.11.Click to save the information and clear the box for the additional entries.
10.2.12.When the last entry is added, Click to save and exit the window.
10.3. Running the Sample
10.3.1. Click the Run tab. The Sample ID for the next sample to be processed is identified in the
Next Sample ID field.
10.3.2. Mix the specimen gently and thoroughly by inversion up to four times
10.3.3. If the specimen tube does not have a pierceable stopper, remove the stopper.
10.3.4. Verify that the Sample ID in the Sample ID Next field matches the sample to be processed.
10.3.5. Insert the tube into the correct position of the correct tube holder. (Check the guide next to
the machine).
10.3.6. Close the tube holder door to begin analysis.
10.3.7. Remove the tube when the tube holder door automatically opens (after aspiration). The red
LED is still illuminated, which means the Analyzer is busy processing the sample.
10.3.8. Wait for the green LED to illuminate, which indicates the system, is ready for the next
sample. Information for the next sample is displayed in the sample ID Next field.
10.3.9. Verify that the current sample results appear in the Run Window.
10.3.10.A copy of the results prints automatically (Auto-print function is enabled).
10.3.11.Verify that the sample ID for the next sample is correct.
10.3.12.Repeat steps 10.3.2 through 10.3.11 until all the samples are analyzed.
10.4. Rerunning samples
10.4.1. There may be instances when you will want to repeat a sample. For example you want to
rerun a sample to confirm a suspect result. Due to duplicate ID feature, rerunning a sample
requires using the system’s Rerun feature. From the Run screen, you can indicate you want
to rerun the last sample.
March 2005 Rev# 1.0 Page 8 of 12
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
10.4.2. Locate the results of the sample you want to rerun
Click The system automatically places the Sample ID onto the work list and allows it
to be processed as a “rerun”. A red square, indicating that the sample is a rerun, appears at
the top right of the screen if you are in the Detailed Results view.
10.4.3. Click the Run tab.
10.4.4. Verify that the correct sample ID is displayed.
10.4.5. Mix the specimen gently by inversion four times.
10.4.6. If the specimen tube does not have a pierceable stopper, remove the stopper.
10.4.7. Verify that the sample ID in the sample ID Next field matches the sample to be processed.
10.4.8. Insert the tube into the correct position of the tube holder.
10.4.9. Close the tube holder door to begin analysis.
10.4.10.Remove the tube when the tube holder door automatically opens.
10.4.11.Review the sample’s results.
10.4.12.Verify the Sample ID and results before reporting the results.
10.4.13.A copy prints automatically (If Auto-print function is enabled).
11. Manual Blood Film Review
11.2. If MCV is >125fL, exclude pseudomacrocytosis due to micro clots or rouleaux.
11.3. If MCV is <55fL, exclude schistocytes, helmet cells. Confirm extreme microcytosis.
11.4. If WBC count is >30,000 cells/uL, exclude platelet agglutination, giant platelets, nucleated
erythrocytes or megakaryocytes.
11.5. If MCHC>36.5 g/dL, check for spherocytosis. .
11.6. If MCHC <31.0 g/dL, check for low MCV/severe iron deficiency anemia.
12. ERROR MESSAGES
12.2. As the ACT 5 diff machine is not perfect, there are some occasions when samples must be re-run
and/or a manual count and blood smear must be evaluated.
12.3. See Error Messages Guidelines (below) for error message constituting re-run, and manual
differential comments. When these messages appear, the sample should be re-run on the Act 5.
If the message still appears, perform the action listed in the table. (for additional information
refer to Coulter Act %Diff Operator Guide- Section 9.3)
12.4. The most recent ACT5 results or the one with the least flags should be signed off and reported.
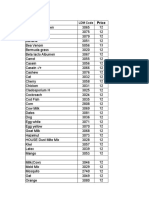
ERROR MESSAGES/CORRECTIVE ACTIONS GUIDELINES
ACTION
PLT Manual
Error message Parameter
Estimate differential
WBC
“Leukocytosis” or “Leukopenia” Low <2 (103/l YES
Hi> 30 (103/l)
March 2005 Rev# 1.0 Page 9 of 12
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
NE Abs count
“Neutropenia” YES
Low< 0.7 (103/l)
LY Abs Count
“Lymphopenia” YES
Low <0.5 (103/l)
PLT
“Thrombocytopenia” YES
Low <100
“MACROYTOSIS” or
“MICROYTOSIS” with “R” next to RBC YES
PLT value
“DIFF +” or “DIFF –“ DIFFS YES
“WBC Interp Not Possible” WBC YES
PLT Interp Not possible PLT YES
PLT Aggregates
PLT YES
and PLT < 100
“*WBC” WBC YES
“BASO +” BASO YES
“Reject” ANY YES
Any values missing ANY YES
13. Cold agglutinins
13.2.1. If MCV is >125fL and manual blood film does not support macrocytosis, micro clots or
rouleaux, warm tube at 36+ 20C for 15 minutes and re-run the sample.
13.2.2. If the MCV is normal after warming, report ‘possible cold agglutinin’ under sample
comments and report the warmed CBC Hemogram
14. Clot check
14.1. Check the sample for clots if results for multiple parameters look depressed.
15. Calculations – dilutions, nRBCs, corrections
15.1. Calculations are required under the following conditions:
15.1.1. Linear limit is exceeded and a sample dilution is required
15.1.2. The automatic differential voted out and a manual differential was performed – calculate the
absolute count.
15.1.3. Nucleated erythrocytes >8 per 100 WBC’s; correct WBC count and recalculate granulocyte,
lymphocyte and monocyte absolute count.
15.1.4. MCV was above or below the operating range resulting in no values reported for Hct or
MCHC.
15.2. Dilutions (linear limit exceeded)
15.2.1. Make a 1:2 dilution with a precision pipette using 1 part well mixed sample plus 1 part
normal saline (0.85-0.9% NaCl) in a 12x75 tube (or similar container). Sample and saline
volume of 100 uL is adequate.
15.2.2. Run the diluted sample in open mode.
15.2.3. Check the diluted results by comparing one of the parameters that was not above linear
limits to its diluted final result.
15.2.3.1. The results should be comparable.
15.2.3.2. If not the dilution may be erroneous. Remake the dilution and run again.
15.2.4. Correct the diluted result by multiplying by 2 (dilution factor). Report the corrected diluted
result along with the other undiluted parameters that are within linear limits.
March 2005 Rev# 1.0 Page 10 of 12
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
15.2.5. Do not report corrected diluted results for parameters that are within linear limits.
15.2.6. Example:
Parameter Undiluted Diluted x2 Report
RBC 7.2 3.7 7.4 (3.7 x 2)
Hgb 20.8 10.8 20.8
HCT 59.6 21.2 59.6
Plt 214 110 214
Note agreement between diluted x2 and undiluted parameters for Hgb, HCT and Plt verifying
dilution accuracy. Note only RBC value has been corrected since the remaining parameters were
within linear limits on undiluted sample.
16. Calculation of absolute leukocytes per category:
16.1. Absolute count (103 cells/uL) = (%count/100) x WBC count
16.2. Example:
WBC = 7.8 x 103 cells/uL
% lymphocytes = 48%
Absolute Lymphocyte Count (Ly#) = (48/100) x 7.8 = 3.744 x 103 cells/uL
16.3. Correction for >8 nucleated erythrocytes (nRBCs) per 100 WBC’s
(Refer to Nucleated Erythrocytes SOP for details)
16.3.1. Total WBC count correction
Uncorrected total WBC count
------------------------------------- X 100
100 + #nRBCs per 100 WBC’s
Example: 23.8 x 103 cells/uL
----------------------------------- X 100 = 21.8 x 103 cells/uL
100 + 9nRBC’s per 100 WBC’s
16.3.2. Calculation of absolute WBC counts by category
(% count/100) X corrected WBC count
Example: corrected WBC count = 21.8 x 103 cells/uL
% lymphocytes (or granulocytes or monocytes) = 45%
(45/100) x 21.8 = 9.81 x 103 cells/uL
17. Linear Range (or Analytical Measurement Range AMR)
17.1. The Analytical Measurement Range (AMR) or linear range is the range of analyte values that a
method can directly measure on the specimen without any dilution, concentration, or other
pretreatment not part of the usual assay process
Analytical Measurement Range (AMR)
Parameter
March 2005 Rev# 1.0 Page 11 of 12
Coulter AC.T 5 Diff Cap Pierce (CP) Operations SOP
WBC, x 103 cells/uL 0.4 – 91.3
RBC, x 109 cells/uL 0.23 – 7.70
HGB, g/dL 0.0 – 22.0
PLT, x 103 cells/uL 3.3 – 1017
18. Limitations of the Procedure (Interfering substances)
18.1. Refer to the Interfering Substances chart in the appendix for a list of possible interfering
agents and conditions.
19. REFERENCE
19.1. Beckman Coulter Operator’s Guide.
20. APPENDICES
20.1. AcT 5 Daily Operation Log.
20.2. AcT 5 Users Log-sheet.
March 2005 Rev# 1.0 Page 12 of 12
Das könnte Ihnen auch gefallen
- Cobas e 411Dokument2 SeitenCobas e 411Santos CruzNoch keine Bewertungen
- Siemens 500. GasometríaDokument14 SeitenSiemens 500. GasometríaPablo FerreiraNoch keine Bewertungen
- Performa II 07022590005Dokument180 SeitenPerforma II 07022590005Rodney Vitorino DiasNoch keine Bewertungen
- Beckman Coulter Manual ProcDokument14 SeitenBeckman Coulter Manual ProcWihadi Santoso Indra SusenoNoch keine Bewertungen
- IPP-LB-HEM-01-01-LH 750 Analyzer and Coulter Gen's SystemDokument13 SeitenIPP-LB-HEM-01-01-LH 750 Analyzer and Coulter Gen's SystemMaria Francesca MapaNoch keine Bewertungen
- IPM for CentrifugesDokument8 SeitenIPM for Centrifugesadmin ptkmiNoch keine Bewertungen
- Clinical Laboratories Point of Care Testing: Rev 2, Ver 1, 6/2013Dokument22 SeitenClinical Laboratories Point of Care Testing: Rev 2, Ver 1, 6/2013Inês PimentaNoch keine Bewertungen
- Performance Qualification and MaintenanceDokument19 SeitenPerformance Qualification and MaintenanceApoloTrevinoNoch keine Bewertungen
- Pro64-A-03 - Processing - A - CBC - CNT - SOPDokument7 SeitenPro64-A-03 - Processing - A - CBC - CNT - SOPBassam AlharaziNoch keine Bewertungen
- Prof. Aw Tar Choon - Quality Management Inf Point of Care Blood Gas TestingDokument70 SeitenProf. Aw Tar Choon - Quality Management Inf Point of Care Blood Gas TestingTaufan LutfiNoch keine Bewertungen
- ChillerDokument25 SeitenChillerZebi DiansNoch keine Bewertungen
- SOP For Alpha SpectrometerDokument8 SeitenSOP For Alpha SpectrometerajwolfeNoch keine Bewertungen
- Pneumatic TestDokument6 SeitenPneumatic TestShrichand G. BathvNoch keine Bewertungen
- 939-528 201301A ABL800 FLEX Operator Training Guide - en - LowDokument20 Seiten939-528 201301A ABL800 FLEX Operator Training Guide - en - LowTomas Fernandez100% (1)
- Market Review Blood Gas Analyser S 2010Dokument43 SeitenMarket Review Blood Gas Analyser S 2010Fercalo AndreiNoch keine Bewertungen
- Laboratory Procedure Manual: Alanine Amino Transferase (ALT) Refrigerated SerumDokument9 SeitenLaboratory Procedure Manual: Alanine Amino Transferase (ALT) Refrigerated Serumحيدر كاملNoch keine Bewertungen
- Husmhema-Upt STM R1Dokument7 SeitenHusmhema-Upt STM R1zakwanmustafaNoch keine Bewertungen
- Bowen AutoverificationDokument12 SeitenBowen AutoverificationDustin BradleyNoch keine Bewertungen
- Sysmex Calibrator ChartDokument2 SeitenSysmex Calibrator ChartDinil Kannur50% (2)
- GemPremier3000 ManualDokument24 SeitenGemPremier3000 ManualAlina OpreaNoch keine Bewertungen
- Manuel Utilisation Ac Performa 2015-06 PDFDokument196 SeitenManuel Utilisation Ac Performa 2015-06 PDFHisham ElsayedNoch keine Bewertungen
- PH SystemsDokument12 SeitenPH Systemslux0008Noch keine Bewertungen
- PH ControlDokument10 SeitenPH Controllux0008Noch keine Bewertungen
- 08 Cpv-IspeDokument35 Seiten08 Cpv-IspeschumonNoch keine Bewertungen
- 1220Infinity-Infinity2-LC Preventive Maintenance ChecklistDokument8 Seiten1220Infinity-Infinity2-LC Preventive Maintenance ChecklistYudi - PT. Laborindo SaranaNoch keine Bewertungen
- Process Performance Qualification Protocol For Autoclave - Pharmaceutical Guidelines 2Dokument12 SeitenProcess Performance Qualification Protocol For Autoclave - Pharmaceutical Guidelines 2MykolaNoch keine Bewertungen
- Strategies of Succesful Distillation Equipment Revamps PDFDokument6 SeitenStrategies of Succesful Distillation Equipment Revamps PDFJose DavalilloNoch keine Bewertungen
- Hematology Chemistry CoagulationDokument29 SeitenHematology Chemistry Coagulationdrafq2000Noch keine Bewertungen
- Eqp.005 Centrifuge CalibrationDokument7 SeitenEqp.005 Centrifuge CalibrationakelloNoch keine Bewertungen
- Handling of Oot ResultsDokument5 SeitenHandling of Oot ResultstghonsNoch keine Bewertungen
- Hematology Gain CalculatorDokument15 SeitenHematology Gain Calculatorابكر ابو ميلادNoch keine Bewertungen
- Use and Maintenance of The Milli-Q Integral 3 Water SystemDokument10 SeitenUse and Maintenance of The Milli-Q Integral 3 Water Systemsupermansam2Noch keine Bewertungen
- Auditing The Microbiology LaboratoryDokument68 SeitenAuditing The Microbiology LaboratoryMohammed Yousffi94% (18)
- Guidelines For Determining Interfering Element Corrections On ICAP 6000-7000 Series Running ITEVADokument5 SeitenGuidelines For Determining Interfering Element Corrections On ICAP 6000-7000 Series Running ITEVAGaetanoNoch keine Bewertungen
- PKG 14 BA-3301 A-B Performance & NPSH TestDokument6 SeitenPKG 14 BA-3301 A-B Performance & NPSH Testfiguev2208Noch keine Bewertungen
- Lab Policies Roche Cobas 6000 Routine Operation La Crosse Lab 4009Dokument4 SeitenLab Policies Roche Cobas 6000 Routine Operation La Crosse Lab 4009Hoàng Hà NguyễnNoch keine Bewertungen
- Poloroid ReportDokument7 SeitenPoloroid ReportKevin RenellNoch keine Bewertungen
- Sah Contingency Plan in Case of Equipment BreakdownDokument3 SeitenSah Contingency Plan in Case of Equipment BreakdownRazel Ann Elagio100% (2)
- Agilent Openlab Intelligent Reporter: Report CompendiumDokument34 SeitenAgilent Openlab Intelligent Reporter: Report CompendiumfabianNoch keine Bewertungen
- Manual de Uso Accu-Chekr Performa PDFDokument180 SeitenManual de Uso Accu-Chekr Performa PDFgilberto espinosaNoch keine Bewertungen
- NEOPRSP011 - Rev. 00 - Pages 11 - Plant Operation Quality Assurance ProcedureDokument13 SeitenNEOPRSP011 - Rev. 00 - Pages 11 - Plant Operation Quality Assurance Procedurealialharbi021Noch keine Bewertungen
- 11-Psa TotalDokument7 Seiten11-Psa TotalprityNoch keine Bewertungen
- Chemical Process Control Laboratory Manual: Department of Chemical Engineering 1999Dokument66 SeitenChemical Process Control Laboratory Manual: Department of Chemical Engineering 1999Łuis MTNoch keine Bewertungen
- Manual 7-Addendum Central Laboratory Procedures: June 22, 2011 - Version 1.0Dokument42 SeitenManual 7-Addendum Central Laboratory Procedures: June 22, 2011 - Version 1.0Arnold HarfiansyahNoch keine Bewertungen
- The Instrument Name and DescriptionDokument9 SeitenThe Instrument Name and DescriptionMakmal FarmaseutikalNoch keine Bewertungen
- Pharmaceutical Master Validation Plan GuideDokument3 SeitenPharmaceutical Master Validation Plan GuideDandung RuskarNoch keine Bewertungen
- Equ10-04 Micro QC - Eqpt Maint SOPDokument7 SeitenEqu10-04 Micro QC - Eqpt Maint SOPpokhara144Noch keine Bewertungen
- 2414 IEC 61850 SEL Conformance Certs 20081125Dokument3 Seiten2414 IEC 61850 SEL Conformance Certs 20081125Augusto César MarianoNoch keine Bewertungen
- LM-80 - OSLON SQUARE - GW CSSRM1.PC - 5000K - 1000ma - 10,000h - 150416W1Dokument15 SeitenLM-80 - OSLON SQUARE - GW CSSRM1.PC - 5000K - 1000ma - 10,000h - 150416W1Shadi Abdelsalam100% (1)
- Control Charts in Statistical Quality ControlDokument19 SeitenControl Charts in Statistical Quality Controlanon_785745540Noch keine Bewertungen
- Process Control Laboratory-Student's ManualDokument105 SeitenProcess Control Laboratory-Student's ManualAnonymous 8pCXXsNoch keine Bewertungen
- Controls - DraftDokument2 SeitenControls - DraftJanine Anne JuyoNoch keine Bewertungen
- Technical Bulletin: i-STATDokument9 SeitenTechnical Bulletin: i-STATJubelly AmarilesNoch keine Bewertungen
- Blood Gas Analyser With Electrolyte SpecificationsDokument3 SeitenBlood Gas Analyser With Electrolyte Specificationsrk927Noch keine Bewertungen
- Il Gem 4000 Operating and Maintenance ProcedureDokument15 SeitenIl Gem 4000 Operating and Maintenance ProcedureHfsh OmerNoch keine Bewertungen
- Roche Cobas-Integra 400 Plus Chemistry - Operartion Sop Non-SMILE Created Resources Author: N/ADokument12 SeitenRoche Cobas-Integra 400 Plus Chemistry - Operartion Sop Non-SMILE Created Resources Author: N/AMona-Lisa DoneaNoch keine Bewertungen
- Advanced Temperature Measurement and Control, Second EditionVon EverandAdvanced Temperature Measurement and Control, Second EditionNoch keine Bewertungen
- Diagnosis and Robust Control of Complex Building Central Chilling Systems for Enhanced Energy PerformanceVon EverandDiagnosis and Robust Control of Complex Building Central Chilling Systems for Enhanced Energy PerformanceNoch keine Bewertungen
- Reliability Prediction from Burn-In Data Fit to Reliability ModelsVon EverandReliability Prediction from Burn-In Data Fit to Reliability ModelsBewertung: 3 von 5 Sternen3/5 (2)
- Thermal Power Plant: Pre-Operational ActivitiesVon EverandThermal Power Plant: Pre-Operational ActivitiesBewertung: 4 von 5 Sternen4/5 (4)
- ChemDokument1 SeiteChemLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- ChessDokument3 SeitenChessLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- MicroDokument1 SeiteMicroLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Troponin I Normal RangeDokument1 SeiteTroponin I Normal RangeLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Alfa Test ProfilesDokument1 SeiteAlfa Test ProfilesLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- MicroDokument4 SeitenMicroLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Single AllergenDokument2 SeitenSingle AllergenLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- How to Play ChessDokument22 SeitenHow to Play Chessraj202987_47312067Noch keine Bewertungen
- Microalbumin EvaluationDokument2 SeitenMicroalbumin EvaluationLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Toshiba Canvio BasicsDokument201 SeitenToshiba Canvio BasicsMattiaVNoch keine Bewertungen
- Haematology Analyser Comparison 2019+Dokument2 SeitenHaematology Analyser Comparison 2019+Luis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Kumon'S Recommended Reading List - Level 7A Level 3ADokument6 SeitenKumon'S Recommended Reading List - Level 7A Level 3ALuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- The Aggressive Strength Solution by Mike MahlerDokument124 SeitenThe Aggressive Strength Solution by Mike Mahlermirocvet100% (3)
- Parameters LDM Machine Print Out CAP Result Ref Range Proficiency MIC Pol 2Dokument3 SeitenParameters LDM Machine Print Out CAP Result Ref Range Proficiency MIC Pol 2Luis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- OEC Exemption 2019Dokument1 SeiteOEC Exemption 2019Luis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- The Vert Specific Conditioning Guide : How Hard Can You Go and For How Long?.Dokument20 SeitenThe Vert Specific Conditioning Guide : How Hard Can You Go and For How Long?.Luis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Jose CapangyarihanDokument1 SeiteJose CapangyarihanLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Team THUMP Txtbook PDFDokument20 SeitenTeam THUMP Txtbook PDFLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- 8 Metabolic Conditioning Workouts MMA FightersDokument5 Seiten8 Metabolic Conditioning Workouts MMA FightersLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Chest Day: Gaspari Nutrition: 7 Day Split Workout Workout Example 1Dokument3 SeitenChest Day: Gaspari Nutrition: 7 Day Split Workout Workout Example 1Luis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Genetics For Dummies, 2nd Edition - WikispacesDokument23 SeitenGenetics For Dummies, 2nd Edition - WikispacesSundas ZahraNoch keine Bewertungen
- Troponin I Normal RangeDokument1 SeiteTroponin I Normal RangeLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Formaldehyde MSDS Mallinckrodt PDFDokument8 SeitenFormaldehyde MSDS Mallinckrodt PDFLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- MicroDokument1 SeiteMicroLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Dr. Fooke SOPDokument1 SeiteDr. Fooke SOPLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Confirmed Result First Batch Urine CultureDokument4 SeitenConfirmed Result First Batch Urine CultureLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Microbiology Urine Culture 2019 2Dokument1 SeiteMicrobiology Urine Culture 2019 2Luis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Dhoha R. HDokument1 SeiteDhoha R. HLuis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- Title: Microbiology Urine Screening Effective Date: 05/08/2013Dokument14 SeitenTitle: Microbiology Urine Screening Effective Date: 05/08/2013Luis Ferdinand Dacera-Gabronino Gamponia-NonanNoch keine Bewertungen
- PPAP ManualDokument102 SeitenPPAP Manualsuresh196950% (2)
- Imagery in Spenser's Amoretti PDFDokument16 SeitenImagery in Spenser's Amoretti PDFIms AliNoch keine Bewertungen
- Onion Model of CommunicationDokument4 SeitenOnion Model of CommunicationpjspickNoch keine Bewertungen
- Wall-Mounted King Shell Temperature and Humidity Transmitter User ManualDokument6 SeitenWall-Mounted King Shell Temperature and Humidity Transmitter User ManualTrung Trần HữuNoch keine Bewertungen
- Metabolic AdaptationDokument17 SeitenMetabolic AdaptationMozil Fadzil KamarudinNoch keine Bewertungen
- Soil Classification PDFDokument12 SeitenSoil Classification PDFbishry ahamedNoch keine Bewertungen
- Method Statement - 23apr18Dokument5 SeitenMethod Statement - 23apr18hinitahNoch keine Bewertungen
- Top 77 Similar Websites Like Examveda - Com and AlternativesDokument23 SeitenTop 77 Similar Websites Like Examveda - Com and AlternativesAbdul WahabNoch keine Bewertungen
- Prize List 2017Dokument6 SeitenPrize List 2017magmileNoch keine Bewertungen
- TLE-MAJOR-TEST-SET-010-Basic-electricity-1Dokument9 SeitenTLE-MAJOR-TEST-SET-010-Basic-electricity-1edsonlligananNoch keine Bewertungen
- The Philippine Tourism Master Plan 1991-2010Dokument7 SeitenThe Philippine Tourism Master Plan 1991-2010Zcephra MalsiNoch keine Bewertungen
- Descriptive ParagraphDokument25 SeitenDescriptive Paragraphabdishakuur272Noch keine Bewertungen
- Astm D-3300Dokument4 SeitenAstm D-3300Ovi Nafisa Zabeen OviNoch keine Bewertungen
- Stages of Growth and DevelopmentDokument32 SeitenStages of Growth and DevelopmentAaron Manuel MunarNoch keine Bewertungen
- Automating Network Slicing Operations in The 5G Core With OrchestrationDokument18 SeitenAutomating Network Slicing Operations in The 5G Core With OrchestrationmorganNoch keine Bewertungen
- Pressure Tech PDFDokument12 SeitenPressure Tech PDFThamaraikani ManiNoch keine Bewertungen
- Twilio Best Practices Sample ChapterDokument36 SeitenTwilio Best Practices Sample ChapterPackt Publishing100% (1)
- Approved) Approve Extension of Extended Waranties - W 40Dokument3 SeitenApproved) Approve Extension of Extended Waranties - W 40solorzanomercador2Noch keine Bewertungen
- Inglés Nivel San Marcos - Sem - 14Dokument12 SeitenInglés Nivel San Marcos - Sem - 14Luis Eduardo Escudero QuispeNoch keine Bewertungen
- Salesforce CRMDokument22 SeitenSalesforce CRMkrishna_mf01Noch keine Bewertungen
- Culligan o Ring DirectoryDokument30 SeitenCulligan o Ring DirectoryCarl Schleif0% (1)
- Sajjad Hussain Sociology 2021 Iiui IsbDokument323 SeitenSajjad Hussain Sociology 2021 Iiui IsbTaskeen MansoorNoch keine Bewertungen
- Instructions Before Starting The Test: WWW - Cuims.inDokument3 SeitenInstructions Before Starting The Test: WWW - Cuims.inYogeshNoch keine Bewertungen
- Poetry Potion 09 Infinite WondersDokument86 SeitenPoetry Potion 09 Infinite WondersBlack-Letter-MediaNoch keine Bewertungen
- Email Security StandardsDokument2 SeitenEmail Security StandardsPeng GuinNoch keine Bewertungen
- Flexfiled Oracle FaqDokument14 SeitenFlexfiled Oracle Faq$!@#$%!@#$%Noch keine Bewertungen
- GS1 Global Traceability StandardDokument58 SeitenGS1 Global Traceability StandardmindtrussNoch keine Bewertungen
- Industrial Gases and AcidsDokument5 SeitenIndustrial Gases and AcidscarlNoch keine Bewertungen
- Chap 011 NotesDokument10 SeitenChap 011 Notesfree50Noch keine Bewertungen
- Chapter 12 - Europe TextbookDokument16 SeitenChapter 12 - Europe Textbooktoasted breadNoch keine Bewertungen