Beruflich Dokumente
Kultur Dokumente
HEYER Scalis - User Manual en 1.1
Hochgeladen von
kalandorka92Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
HEYER Scalis - User Manual en 1.1
Hochgeladen von
kalandorka92Copyright:
Verfügbare Formate
Operating Instructions
Rev. 1.1 – 01/13
I NNOVATIONS AS S ERVICE TO THE P ATIENT
INTELLECTUAL PROPERTY STATEMENT
Copyright
HEYER Medical AG
VERSION: 1.1
RELEASE DATE: 01.2013
MODEL: Scalis 7, 12, 15
Declaration
HEYER Medical AG (hereinafter referred to as “HEYER”) owns the intellectual property rights
to this product and this manual. This manual may refer to information protected by copyrights
or patents and does not convey any license under the patent rights of HEYER or the rights of
others. HEYER does not assume any liability arising from any infringements of patents or
other rights of third parties.
HEYER intends to maintain the contents of this manual as confidential information. Disclosure
of the information in this manual in any manner whatsoever without the written permission of
HEYER is strictly forbidden. Release, amendment, reproduction, distribution, rent, adaption
and translation of this manual in any manner whatsoever without the written permission of
HEYER is strictly forbidden.
The contents of this manual are subject to change without prior notice.
Manufacturer’s Responsibility
All information contained in this manual is believed to be correct. HEYER shall not be liable for
errors contained herein or for incidental or consequential damages in connection with the
supply, performance or use of this manual.
HEYER is responsible for the safety, reliability and performance of this product only on the
condition that:
• all installation, additions, changes, modifications and repairs of this product are conducted
personnel authorized by HEYER; and,
• the electrical fittings of the relevant room comply with the applicable national and local
requirements; and,
• this product is operated under strict compliance with the instructions of this manual.
HEYER Scalis - Patient Monitor - Instruction Manual Rev. 1.1 I
Note
This equipment cannot be used at home.
Warning
In order to use this device safely, you must follow the instructions listed. This manual is not
intended to replace proper medical instruction of the user.
• Do not rely on the audible alarm alone to monitor patient. During patient monitoring, selecting
a very low volume or completely muting the sound may have catastrophic results for the
patient. The most reliable way to monitor the patient is to perform manual monitoring in parallel
to the correct use of monitoring equipment.
• This multi-parameter patient monitor is intended for use only by medical professionals in
healthcare establishments.
• To avoid electrical shock, do not open any covers by yourself. Service must be carried out by
qualified personnel.
• Use of this device may cause interference on the screens of ultrasound equipment. This
monitor and any ultrasound imaging equipment must be kept as far apart as possible.
• It is dangerous to expose the electrical contacts and connectors to normal saline, other liquids
or conductive adhesives. Electrical contacts and connectors, such as cable connectors, power
supply and parameter module socket inlet and frame must be kept clean and dry. These parts
must be dried thoroughly if they come into contact with any liquid. If further eradication is
required, please contact your biomedical department or manufacturer.
Warning
This is not a treatment device.
If the hospital or establishment responsible for using this instrument does not establish an
appropriate maintenance schedule, this may result in abnormal equipment failure, thus
endangering human health.
For device components identified in this manual as appropriate for repair by the user, HEYER will
provide circuit diagrams, calibration methods and any other information requested by the user, in
order to facilitate repair by appropriately qualified technical personnel on behalf of the user.
HEYER Scalis - Patient Monitor - Instruction Manual Rev. 1.1 II
Contact Information
HEYER Medical AG
Carl-Heyer-Str. 1/3
D-56130 Bad Ems – Germany
Tel.: +49 2603 791 3
Fax: +49 2603 70424
Email: info@heyermedical.de
www.heyermedical.de
HEYER Scalis - Patient Monitor - Instruction Manual Rev. 1.1 III
Contents
Contents
Page
Chapter 1. Overview .............................................................................................. 1
1.1 Overview ........................................................................................................ 1
1.2 Safety information .......................................................................................... 1
1.3 Device Labels................................................................................................. 3
1.4 Intended Use.................................................................................................. 4
1.5 Introduction to screen layouts......................................................................... 5
1.5.1 Information section .......................................................................... 5
1.5.2 Parameters section.......................................................................... 6
1.5.3 Waveform section ............................................................................ 6
1.5.4 Menu section ................................................................................... 6
1.6 Alarms............................................................................................................ 7
1.7 Control panel.................................................................................................. 7
1.8 Menu .............................................................................................................. 7
1.8.1 Patient management........................................................................ 7
1.8.2 History review .................................................................................. 8
1.8.3 Settings............................................................................................ 8
1.8.4 Alarm limit...................................................................................... 11
1.8.5 Service .......................................................................................... 12
1.9 Sensor socket .............................................................................................. 14
1.10 External interface ......................................................................................... 15
1.11 Networks ...................................................................................................... 15
1.12 Built-in rechargeable battery......................................................................... 15
1.13 Installation.................................................................................................... 16
1.13.1 Open the box and check ................................................................ 16
1.13.2 Connect the power cables ............................................................. 16
1.14 Turning on the monitor ................................................................................. 17
1.15 Connect patient sensors............................................................................... 17
1.16 Check the recorder....................................................................................... 17
Chapter 2. Alarms ................................................................................................ 18
2.1 Alarms overview........................................................................................... 18
2.1.1 Types of alarm ............................................................................... 18
2.1.2 Alarm levels ................................................................................... 18
2.1.3 Alarm modes ................................................................................. 18
2.2 Pausing the alarms ...................................................................................... 19
2.3 Silencing the alarms ..................................................................................... 19
2.4 Alarm Setting................................................................................................ 19
2.5 Alarm limits .................................................................................................. 20
2.5.1 ECG Alarm Limit ............................................................................ 21
2.5.2 SpO2 Alarm Limit ........................................................................... 21
2.5.3 NIBP Alarm Limit ........................................................................... 22
2.5.4 Resp Alarm Limit ........................................................................... 22
2.5.5 Temp Alarm Limit........................................................................... 23
2.5.6 Load Default Alarm Limit................................................................ 23
2.6 Patient alarm information ............................................................................. 23
2.7 Technical alarm information ......................................................................... 25
Chapter 3. Recording........................................................................................... 28
3.1 Record settings ............................................................................................ 28
3.2 Record type.................................................................................................. 28
HEYER Scalis - Patient Monitor - Instruction Manual Rev. 1.1 IV
Contents
3.2.1 Real-time recording ....................................................................... 28
3.2.2 Auto record .................................................................................... 29
3.3 Record content............................................................................................. 29
Chapter 4. Admit/Discharge Patient ................................................................... 30
4.1 Admit patient ................................................................................................ 30
4.2 Discharge patient ......................................................................................... 30
Chapter 5. ECG Monitoring ................................................................................. 32
5.1 Connecting ECG electrodes ......................................................................... 32
5.2 ECG electrode placement ............................................................................ 32
5.3 Connecting ECG leads for surgical patients ................................................. 33
5.4 ECG settings................................................................................................ 35
Chapter 6. Respiration Monitoring ..................................................................... 37
6.1 Principles of respiration measurement.......................................................... 37
6.2 Placing the electrodes .................................................................................. 37
6.3 Respiration settings...................................................................................... 37
Chapter 7. SpO2 Monitoring ................................................................................ 39
7.1 Monitoring procedure ................................................................................... 39
7.1.1 Neonatal SpO2 plethysmography measurements........................... 40
7.1.2 Placement of the neonatal oxygen probe ....................................... 41
7.2 Measurement restrictions ............................................................................. 42
7.3 SpO2 settings ............................................................................................... 43
Chapter 8. NIBP monitoring ................................................................................ 45
8.1 NIBP measurement procedure ..................................................................... 45
8.2 NIBP measurement limitations ..................................................................... 47
8.3 NIBP settings ............................................................................................... 47
8.4 Blood pressure calibration ............................................................................ 48
8.5 Checking for leaks........................................................................................ 48
Chapter 9. Temperature Monitoring ................................................................... 50
9.1 Steps for temperature measurement ............................................................ 50
9.2 Temperature settings menu.......................................................................... 50
Chapter 10. History Review................................................................................... 51
10.1 Trend Graph................................................................................................. 51
10.1.1 Select parameters.......................................................................... 51
10.1.2 Set period ...................................................................................... 52
10.1.3 Adjust observation time.................................................................. 52
10.2 Trend table................................................................................................... 52
10.2.1 Set period ...................................................................................... 53
10.2.2 Adjust observation time.................................................................. 53
10.3 Alarm review ................................................................................................ 53
10.3.1 Alarm Type .................................................................................... 54
10.3.2 Choose Alarm event ...................................................................... 54
10.3.3 Select wave ................................................................................... 54
10.3.4 Record........................................................................................... 54
10.4 NIBP Review ................................................................................................ 55
10.5 Wave review ................................................................................................ 55
10.5.1 Select waveform ............................................................................ 56
10.5.2 Adjust observation time.................................................................. 56
Chapter 11. Drug Calculation................................................................................ 57
11.1 Drug Calculation........................................................................................... 57
HEYER Scalis - Patient Monitor - Instruction Manual Rev. 1.1 V
Contents
11.2 Operating procedures................................................................................... 58
11.3 Titration table ............................................................................................... 58
Chapter 12. Maintenance and Cleaning................................................................ 60
12.1 System Check .............................................................................................. 60
12.2 General Cleaning ......................................................................................... 60
12.3 Cleaning Agents........................................................................................... 61
12.4 Sterilization .................................................................................................. 61
12.5 Disinfection .................................................................................................. 62
Chapter 13. Patient Safety..................................................................................... 63
13.1 Environment ................................................................................................. 63
13.2 Power Requirements.................................................................................... 63
13.3 Grounding .................................................................................................... 63
13.4 Equipotential grounding................................................................................ 64
13.5 Condensation ............................................................................................... 64
Chapter 14. EMC .................................................................................................... 65
Chapter 15. Appendix - Product Specifications................................................... 69
15.1 Classification................................................................................................ 69
15.2 Applicable Standards ................................................................................... 69
15.3 Size and weight............................................................................................ 69
15.4 Power Supply ............................................................................................... 70
15.5 Battery.......................................................................................................... 70
15.6 Signal Interface ............................................................................................ 70
15.7 Storage ........................................................................................................ 70
15.8 Environment ................................................................................................. 70
15.9 ECG ............................................................................................................. 70
15.9.1 Heart rate calculation method ........................................................ 70
15.9.2 Heart rate meter accuracy and arrhythmia response ..................... 71
15.9.3 Lead mode..................................................................................... 71
15.9.4 Gain............................................................................................... 72
15.9.5 Sweep speed ................................................................................. 72
15.9.6 Heart rate....................................................................................... 72
15.9.7 Sensitivity ...................................................................................... 72
15.9.8 Differential Input Impedance .......................................................... 72
15.9.9 Bandwidth...................................................................................... 72
15.9.10 CMRR............................................................................................ 72
15.9.11 Electrode offset potential ............................................................... 72
15.9.12 Input dynamic range ...................................................................... 72
15.9.13 Pacing pulse suppression .............................................................. 73
15.9.14 QRS wave amplitude and period range between ........................... 73
15.9.15 Line frequency voltage tolerance ................................................... 73
15.9.16 Drift tolerance ................................................................................ 73
15.9.17 Baseline stability ............................................................................ 73
15.9.18 System noise ................................................................................. 74
15.9.19 Multi-channel crosstalk .................................................................. 74
15.9.20 Electrosurgery interference suppression ........................................ 74
15.9.21 Pace pulse display capabilities ...................................................... 74
15.9.22 Heart rate response time ............................................................... 74
15.9.23 Baseline Recovery......................................................................... 74
15.9.24 Signal Range ................................................................................. 74
15.9.25 Calibration Signal........................................................................... 75
15.10 Respiration................................................................................................... 75
HEYER Scalis - Patient Monitor - Instruction Manual Rev. 1.1 VI
Contents
15.10.1 Method .......................................................................................... 75
15.10.2 Respiration Impedance Range....................................................... 75
15.10.3 Base Impedance Range ................................................................ 75
15.10.4 Bandwidth...................................................................................... 75
15.10.5 Gain............................................................................................... 75
15.10.6 Respiration Rate ............................................................................ 75
15.10.7 Apnea Alarm.................................................................................. 75
15.11 NIBP ............................................................................................................ 76
15.11.1 Method .......................................................................................... 76
15.11.2 Measure mode............................................................................... 76
15.11.3 Measure Interval in AUTO Mode.................................................... 76
15.11.4 Measure Period in STAT Mode...................................................... 76
15.11.5 Pulse Rate Range.......................................................................... 76
15.11.6 Measure and Alarm Range ............................................................ 76
15.11.7 Static pressure accuracy................................................................ 76
15.11.8 Resolution...................................................................................... 76
15.11.9 Accuracy........................................................................................ 77
15.11.10 Overpressure Protection ................................................................ 77
15.12 SpO2 ............................................................................................................ 77
15.12.1 Measurement Range ..................................................................... 77
15.12.2 Resolution...................................................................................... 77
15.12.3 Accuracy........................................................................................ 77
15.12.4 Pulse Rate ..................................................................................... 77
15.13 Temperature ................................................................................................ 77
15.14 Recorder (optional – only SCALIS 12 + 15).................................................. 77
15.15 Accessories List ........................................................................................... 78
Chapter 16. Warranty............................................................................................. 79
List of Figures
Fig. 1-1: demo of monitor interface................................................................... 5
Fig. 1-2: Patient management............................................................................ 7
Fig. 1-3: History review ...................................................................................... 8
Fig. 1-4: Setting .................................................................................................. 8
Fig. 1-5: Screen layouts ..................................................................................... 9
Fig. 1-6: Adjust time......................................................................................... 10
Fig. 1-7: Miscellaneous settings ..................................................................... 10
Fig. 1-8: Load default settings......................................................................... 11
Fig. 1-9: Alarm Limit......................................................................................... 12
Fig. 1-10: Service ............................................................................................... 12
Fig. 1-11: ECG calibration.................................................................................. 12
Fig. 1-12: Temp Sensor Type ............................................................................ 13
Fig. 1-13: Sensor socket .................................................................................... 14
Fig. 2-1: Alarm settings.................................................................................... 20
Fig. 2-2: Alarm Limit......................................................................................... 21
Fig. 2-3: ECG Alarm Limit ................................................................................ 21
Fig. 2-4: SpO2 Alarm Limit ............................................................................... 22
Fig. 2-5: NIBP Alarm Limit ............................................................................... 22
Fig. 2-6: Resp Alarm Limit ............................................................................... 22
Fig. 2-7: Temp Alarm Limit .............................................................................. 23
Fig. 2-8: Load Default Alarm Limit .................................................................. 23
HEYER Scalis - Patient Monitor - Instruction Manual Rev. 1.1 VII
Contents
Fig. 3-1: Record settings ................................................................................. 28
Fig. 4-1: Admit new patient.............................................................................. 30
Fig. 4-2: Discharge patient .............................................................................. 30
Fig. 5-1: Positioning of electrodes .................................................................. 32
Fig. 5-2: Standard ECG wave........................................................................... 34
Fig. 5-3: ECG settings menu ........................................................................... 35
Fig. 6-1: Resp settings..................................................................................... 37
Fig. 7-1: Finger sensor placement .................................................................. 39
Fig. 7-2: Neonatal arterial oxygen probe (1) ................................................... 40
Fig. 7-3: Neonatal arterial oxygen probe (2) ................................................... 40
Fig. 7-4: Placement of the neonatal oxygen probe ........................................ 41
Fig. 7-5: SpO2 settings ..................................................................................... 43
Fig. 8-1: Applying the cuff ............................................................................... 46
Fig. 8-2: NIBP settings ..................................................................................... 47
Fig. 9-1: Temperature settings ........................................................................ 50
Fig. 10-1: Trend Graph....................................................................................... 51
Fig. 10-2: Trend table menu............................................................................... 52
Fig. 10-3: Alarm review ...................................................................................... 54
Fig. 10-4: NIBP measurement review................................................................ 55
Fig. 10-5: Wave review ....................................................................................... 56
Fig. 11-1: Dose calculation ................................................................................ 57
Fig. 11-2: Titration table..................................................................................... 58
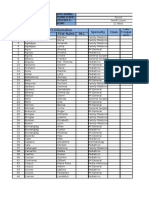
List of Tables
Table 14-1: Guidance and HEYER declaration — electromagnetic
emissions........................................................................................... 65
Table 14-2: Guidance and HEYER declaration — electromagnetic
immunity ............................................................................................ 66
Table 14-3: Guidance and HEYER declaration — electromagnetic
immunity ............................................................................................ 67
Table 14-4: Recommended separation distances between portable and
mobile RF communication and the monitor .................................... 68
HEYER Scalis - Patient Monitor - Instruction Manual Rev. 1.1 VIII
Chapter 1. Overview
1.1 Overview
This monitor is suitable for adult, pediatric and neonatal patients and can be used to
monitor physical parameters such as electrocardiograph (ECG), noninvasive blood
pressure (NIBP), oxygen saturation (SpO2), respiration rate (Resp) and body
temperature (Temp). It can display a maximum of 8 waveforms and all information
about the parameters being monitored on the same screen.
The monitoring functions of this monitor are listed below:
1) Electrocardiograph (ECG), including: heart rate, 6-channel ECG waveforms, ST
segment analysis and arrhythmia analysis.
2) Oxygen saturation (SpO2), including: oxygen saturation, pulse rate, pulse wave.
3) Noninvasive blood pressure (NIBP), including: systolic pressure, diastolic pressure,
mean pressure.
4) Body temperature (Temp): 2-channel body temperature data.
5) Respiration (Resp): respiratory rate, respiration waveform.
1.2 Safety information
NOTE Points to be noted.
CAUTION Points to be noted to avoid damage to the equipment.
WARNING Points to be noted to avoid injury to the patient and the operator.
Warnings
• Do not rely on the audible alarm alone to monitor patient. During patient monitoring,
selecting a very low volume or completely muting the sound may have catastrophic
results for the patient. The most reliable way to monitor the patient is to perform
manual monitoring in parallel to the correct use of monitoring equipment.
• This multi-parameter patient monitor is intended for use only by medical professionals
in healthcare establishments.
• To avoid electrical shock, do not open any covers by yourself. Service must be carried
out by qualified personnel.
• Use of this device may cause interference on the screens of ultrasound equipment.
This monitor and any ultrasound imaging equipment must be kept as far apart as
possible.
• It is dangerous to expose the electrical contacts and connectors to normal saline, other
liquids or conductive adhesives. Electrical contacts and connectors, such as cable
connectors, power supply and parameter module socket inlet and frame must be kept
clean and dry. These parts must be dried thoroughly if they come into contact with any
liquid. If further eradication is required, please contact your biomedical department or
manufacturer.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 1
Warnings
• This device can only monitor one patient at a time.
• There is the risk of electrical shock if the monitor casing is opened. All servicing and
future upgrading to this equipment must be carried out by personnel trained and
authorized by the manufacturer.
• Always ensure that the device and accessories can function safely and normally before
use.
• Possible explosion hazard if used in the presence of flammable anesthetics or other
flammable substances in combination with air, oxygen-enriched environments, or
nitrous oxide.
• You must customize the alarm setups according to the individual patient situation and
make sure that the alarm sound can be activated when an alarm is triggered.
• Do not touch the patient, operating table, bed or the device during defibrillation.
• Do not use cellular phones in the vicinity of this device. High-level electromagnetic
radiation emitted from such devices may greatly affect the performance of the monitor.
• Devices connected to the monitor shall form an equipotential system (protectively
earthed).
Connect the grounding wire to the equipotential grounding terminal on the main
system. If it is not evident from the instrument specifications whether a particular
instrument combination is hazardous or not, for example due to summation of leakage
currents, the user should consult the manufacturers concerned or an expert in the field
to ensure that the necessary safety of all instruments concerned will not be impaired by
the proposed combination.
• When used with electrosurgery equipment, the doctor or nurse must give top priority to
patient safety.
• Do not place the monitor or external power supply in any position that might cause it to
fall onto the patient. Do not lift the monitor by the power supply cord or patient cable;
use only the handle on the monitor.
• Consult IEC-601-1-1 for system interconnection guidance. The specific requirements
for system interconnection are dependent upon the devices connected to the monitor,
the relative distance of each device from the patient, and the location of the connected
device within the medically-used room containing the monitor. In all circumstances, the
monitor must be connected to a grounded AC power supply. The monitor is referred to
as an IEC 601/F device in the summary of situations table contained in IEC 601-1-1.
• Dispose of the packaging material in accordance with the applicable waste control
regulations, and keep out of reach of children.
• Grounding:
Connect the monitor only to a three-wire, grounded, hospital-grade socket. The three-
pin plug must be inserted into a properly wired three-wire socket; if a three-wire socket
is not available, a qualified electrician must install one in accordance with the
applicable electrical code.
Do not under any circumstances remove the grounding conductor from the power plug.
Do not use extension cords or adapters of any type. The power cord and plug must be
intact and undamaged.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 2
Warnings
If there is any doubt about the integrity of the protective earthing arrangement, operate
the monitor on internal battery power until the protective earthing of the AC power
supply is fully functional.
• For this equipment to be used safely, it is necessary to follow these instructions.
However, the instructions listed in this manual in no way supersede established
medical practices concerning patient care.
• It is important for the hospital or establishment using this equipment to enforce a
reasonable maintenance schedule. Neglect of this may result in machine breakdown or
injury to human health.
Caution
If you have any doubt about the earthing layout and its performance, you must use the
built-in battery to power the monitor.
1.3 Device Labels
This symbol means “BE CAREFUL”. Refer to the manual.
Caution: alerts users that failure to follow the instructions may cause damage to
the equipment or affect the test results.
Note: indicates important information. It is also used to describe some special
techniques.
Warning: warns users of potential dangers. Failure to follow the instructions may
result in personal injury.
This symbol indicates that the instrument is IEC 60601-1 Type CF equipment.
The unit displaying this symbol contains an F-Type isolated (floating) patient
applied part providing a high degree of protection against shock and is suitable
for use during defibrillation.
Equipotential grounding system.
Protective earth ground.
Power On/Off
AC power
This symbol indicates that the instrument is IEC 60601-1 Type CF equipment.
The unit displaying this symbol contains an F-Type isolated (floating) patient
applied part providing a high degree of protection against shock and is suitable
for use during defibrillation.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 3
This symbol indicates that the instrument is IEC 60601-1 Type CF equipment.
The unit displaying this symbol contains an F-Type isolated (floating) patient
applied part providing a high degree of protection against shock and is suitable
for use during defibrillation.
This symbol indicates that the instrument is IEC 60601-1 Type BF equipment.
1.4 Intended Use
The intended use of SCALIS is to monitor physiological data in a single adult, pediatric
or neonatal patient. Physiological data includes but is not restricted to:
electrocardiogram, noninvasive blood pressure, pulse oximetry, pulse, temperature,
respiration. These data can be displayed, trended, stored and printed.
SCALIS is designed as a bedside portable monitor that can operate in all professional
medical facilities, including but not restricted to: emergency department, operating
room, post-anesthesia recovery, critical care, surgical intensive care, respiratory
intensive care, medical intensive care, pediatric intensive care and neonatal intensive
care. SCALIS cannot be used on helicopters. SCALIS is intended strictly to monitor a
single patient at any one time.
Warning
This is not a therapeutic device
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 4
1.5 Introduction to screen layouts
The screen is divided into four sections: 1 – information section; 2 – waveform section;
3 – parameters section; 4 – menu section (as shown in Fig. 1-1).
Fig. 1-1: demo of monitor interface
1.5.1 Information section
The information section is at the top of the screen. It displays the current conditions of
the monitor and the patient. The information provided is as follows (from left to right):
“patient information”, “technical alarm information”, “physiological alarm information”,
“date and time” , “network connection status” and “battery status”.
1) Patient information:
Bed number (refers to the hospital bed number of patient monitored);
Type of patient (“Adult”, “Pediatric” or “Neonate”);
Name of patient (if operator does not input a patient name, this position will display
“NO NAME”);
2) Technical alarm information:
Reports the current condition of the monitor or sensors; this section will display
alarm information;
3) Physiological alarm information:
If the patient's physiological parameters exceed the alarm limit, this section will
display alarm information;
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 5
4) Date and time:
Updates current date and time every second;
5) Network connection status;
6) Battery status:
Current battery capacity or its condition.
1.5.2 Parameters section
Heart rate: heart rate (unit: beats per minute, bpm)
ST: ST segment (unit: millivolt, mV)
PVCs: number of premature ventricular contractions (unit: times/minute)
NIBP: From right to left: systolic pressure, diastolic pressure, mean
pressure (unit: millimeter of mercury (mmHg) or kilopascal (kPa))
SpO2: oxygen saturation SpO2 (unit: %), pulse rate (unit: pulses /minute)
Respiration rate: respiration rate (unit: breaths per minute, BrPM)
Temperature: body temperature (unit: centigrade (°C ) or Fahrenheit (°F))
The user may change the settings of the monitored parameters mentioned above. This
will be described in detail in later chapters.
1.5.3 Waveform section
The waveform section displays 7 waveforms in standard screen layout. From top to
bottom, these are: ECG1 waveform, ECG2 waveform, pulse wave, respiration
waveform. A total of 8 waveforms can be displayed if “ECG Full Lead” screen layout is
selected.
The name appears in upper left side of each waveform. The ECG waveform gain and
filter mode will be also displayed beside the ECG wave name. On the right side of the
ECG waveform is a mark demonstrating the unit of 1 mV. The gain setting of the
respiration waveform is displayed on the right side of the name of respiration wave.
When the user pushes the keys on the patient monitor, a window may pop up in the
waveform section. The waveform section will return to normal after the window is
minimized.
1.5.4 Menu section
At the bottom of the screen, there are 5 menu items: “Patient”, “Review”, “Settings”,
“Alarm Limit” and “Service”. When no windows are displayed on the screen, the user
may scroll through these menus by turning the knob. When one of these menu items is
highlighted, sublevel menus will pop up. If the user presses down the knob again, the
corresponding dialog window will pop up, and the user can change the settings in the
dialog window.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 6
1.6 Alarms
When an alarm is triggered, the warning light will flash or light up; the color represents
the alarm level. For a detailed explanation, please refer to Chapter 2 "Alarms".
1.7 Control panel
The control panel is on the front panel. All keys are listed below (from left to right):
1) Power key: to turn the power on and off.
2) Silence key: if this key is pressed, the alarm sound will be deactivated and “ALARM
SILENCE” will be displayed in the information section; other sounds (key sounds,
palpitation sounds and so on) will not be affected. Pressing the key again will
restore all alarms.
3) Pause key: if this key is pressed, the alarm may suspended for 2 minutes (“1
minute”, “2 minute” and “3 minute” optional are available), and “ALARM PAUSE”
will be displayed in the information section. All alarms will be restored if this key is
pressed again.
4) Freeze key: in normal mode, all waveforms on screen will be frozen if this key is
pressed. Pressing the key once again will release the frozen waveforms.
5) NIBP key: if this key is pressed, the cuff will start to inflate and measure blood
pressure. Pressing the key once again will cancel the measurement.
6) Record/Stop key: if the monitor has a recording device, pressing this key will start
recording the real-time waveforms. Pressing the key again will stop recording.
7) Main menu key: press this key to return to the main menu.
8) Knob key: the user can use this key to scroll through the menus and enter windows
in order to change the monitor settings.
1.8 Menu
1.8.1 Patient management
By selecting the “Patient” tab, the user may choose to enter the “Admit New Patient”,
“Discharge Current Patient” or “Dose Calculation” window. Please refer to Chapter 4
"Admit/Discharge Patient" for detailed instructions.
Fig. 1-2: Patient management
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 7
1.8.2 History review
By selecting the “Review” tab, the user may choose to enter the “Trend Graph”, “Trend
Table”, “Alarm Review”, “NIBP Review” or “Wave Review” window. Please refer to
Chapter 10 "History Review" for detailed instructions.
Fig. 1-3: History review
1.8.3 Settings
By selecting the “Setting” tab, the user may choose to enter the “Alarm Setting”,
“Record Setting”, “Screen Layout”, “Adjust Time”, “Miscellaneous”, “ECG Setting”, “ST
Setting”, “SpO2 Setting”, “NIBP Setting”, “Resp Setting”, “Temp Setting”, or “Load
Default” windows.
Fig. 1-4: Setting
1.8.3.1 Alarm Settings
Please refer to Chapter 2 "Alarms" for detailed instructions.
1.8.3.2 Record Settings
Please refer to Chapter 3 "Recording" for detailed instructions
1.8.3.3 Screen Layout
After entering the “Screen Layout” window, the user can change the current display
interface by selecting from 6 different layout options: “Standard”, “ECG Full Lead”, “Big
Font”, “OxyCRG”, “NIBP Trend”, “Trend Table”. The user can also choose to turn on or
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 8
off various parameters or waveforms in the boxes “Parameter Switch” and “Wave
Switch”.
If the screen layout is set to “Trend Table”, the user can change time intervals for the
trend analysis from “1 min” to “60 min” by adjusting the “Trend Time”.
The following figure shows the “Screen Layout” menu:
Fig. 1-5: Screen layouts
1.8.3.4 Screen Layout
Big Font Standard ECG Full Lead
OxyCRG Trend Table NIBP Trend
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 9
1.8.3.5 Adjust Time
By entering the “Adjust Time” window, the user can select the date format and adjust
the current date and time, as shown below:
Fig. 1-6: Adjust time
1.8.3.6 Miscellaneous
By entering the “Miscellaneous” window, the user can change the key volume and the
screen brightness. Key volume can be set at any level from 0 to 10 (0 represents
mute). Screen brightness settings range from 1 to 10 (10 representing the maximum
brightness). If “Wave Smooth” is set to “On”, the wave will be displayed in smooth
mode.
Fig. 1-7: Miscellaneous settings
1.8.3.7 ECG Settings
Please refer to Chapter 5 "ECG Monitoring" for detailed instructions about ECG
settings.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 10
1.8.3.8 ST Settings
Please refer to Chapter 6 "Respiration Monitoring" for detailed instructions about ST
settings.
1.8.3.9 Resp Settings
Please refer to Chapter 6 "Respiration Monitoring" for detailed instructions about
Resp settings.
1.8.3.10 SpO2 Settings
Please refer to Chapter 7 "SpO2 Monitoring" for detailed instructions about SpO2
monitoring.
1.8.3.11 NIBP Settings
Please refer to Chapter 8 "NIBP monitoring" for detailed introductions about
noninvasive blood pressure settings.
1.8.3.12 Temperature Settings
Please refer to Chapter 9 "Temperature Monitoring" for detailed introductions about
body temperature settings.
1.8.3.13 Load Default Setting
The following graphic shows the “Load Default” window:
Fig. 1-8: Load default settings
If “Yes” is chosen, then the current settings will be replaced with the default settings.
1.8.4 Alarm limit
By selecting the “Alarm Limit” tab, the user can choose to enter the “ECG Alarm Limit”,
“SpO2 Alarm Limit”, “NIBP Alarm Limit”, “Resp Alarm Limit”, “Temp Alarm Limit”, or
“Load default Alarm Limit” windows. Please refer to Chapter 2 "Alarms" for more
detailed information.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 11
Fig. 1-9: Alarm Limit
1.8.5 Service
By selecting the “Service” tab, the user can choose to enter the “ECG Calibrate”,
“Temp Sensor Type”, “NIBP Pneumatic Test”, “NIBP Calibration”, “NIBP reset”, “Demo
Mode”, “Version Info”, “User Setting” and “Factory Service” windows, and so on.
Fig. 1-10: Service
1.8.5.1 ECG calibration
By entering the “ECG Calibrate” window, the user can turn ECG calibration on or off, as
shown below:
Fig. 1-11: ECG calibration
1.8.5.2 Temp Sensor Type
By entering the “Temp Sensor Type” window, the user may select the type of body
temperature sensor: 10K or 2.25K, as shown below:
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 12
Fig. 1-12: Temp Sensor Type
1.8.5.3 NIBP Pneumatic Test
By selecting “NIBP Pneumatic Test”, the user can check the blood pressure
measurement apparatus for air leaks.
When the blood pressure cuff is connected, the user can start the air leakage test by
selecting this option. The test will determine whether condition of the gas tubes and
apparatus is airtight or not. The test results will be displayed as follows:
If the air leakage test is passed, the system will not make any prompts.
If the test result is a fail, the corresponding failure prompts will be displayed in the
screen segment providing information about noninvasive blood pressure.
For detailed instructions, please refer to Chapter 8.5 "Checking for leaks".
1.8.5.4 NIBP Calibration
By selecting the “NIBP Calibration”, the user enters the calibration mode. In this mode,
the user can calibrate pressure measurement using a pressure gauge (or mercury
sphygmomanometer) with a tolerance greater than 1 mmHg after calibration. If the
“Measure blood pressure” key is pressed down during the calibration, the system will
stop calibrating. For detailed instructions, please refer to Chapter 8.4 "Blood
pressure calibration".
1.8.5.5 NIBP reset
By selecting “NIBP reset”, the user can restore the blood pressure module to its initial
settings.
If the blood pressure measurement is abnormal but the monitor does not signal any
prompts to suggest the cause of the problem, we suggest using this option. If the BP
module functions abnormally, resetting it may resolve the error.
1.8.5.6 Demo mode
If the user inputs the correct password, the monitor will enter demo mode. “DEMO” will
be displayed in large font in the centre of the screen. The demo mode is a special
function intended solely for demonstrating how the machine operates and to help carry
out device training. This function is forbidden in actual clinical use, as it may result in
medical staff mistaking demo waveforms for patient waveforms and parameters, thus
affecting patient monitoring.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 13
1.8.5.7 Version information
By selecting “Version Info”, the user can review information about the version of the
software installed on the monitor.
1.8.5.8 User settings
The user can carry out user maintenance in the “User Setting” menu by inputting the
password. This option is only available to the service technician appointed by the
manufacturer.
1.8.5.9 Factory service
The user cannot implement service functions. This option is only available to the
service technician appointed by the manufacturer.
1.9 Sensor socket
Fig. 1-13: Sensor socket
The sensor sockets are labeled as follows:
TEMP1: Temperature channel 1 sensor socket
TEMP2: Temperature channel 2 sensor socket
SpO2: Oxygen saturation sensor socket
NIBP: Noninvasive blood pressure cuff socket
ECG: ECG cable socket
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 14
1.10 External interface
: This symbol means “BE CAREFUL”. Please refer to the manual.
VGA: VGA output. For connection to a VGA monitor.
NET: RJ45 net socket.
: Equipotential earthing system.
Warning
Accessory equipment connected to the analog and digital interfaces must be certified
according to the respective IEC standards (e.g. IEC 60950 for data processing equipment
and IEC 60601-1 for medical equipment). Furthermore all configurations must comply with
the valid version of the system standard IEC 60601-1-1. Everybody who connects
additional equipment to the signal input part or signal output part is configuring a medical
system and is therefore responsible for ensuring that the system complies with the
requirements of the valid version of the system standard IEC 60601-1-1. If in doubt,
please consult the technical service department or your local representative.
1.11 Networks
The network port on the monitor is a standard RJ45 network interface and can be used
to communicate with the central station through an Ethernet cable to enable remote
monitoring. In the top right corner of the screen is a network icon which depicts the
current network status. If the network cable is disconnected, the following network
status icon is shown “ ”. Once the monitor has established connection with the
central station, the following icon is shown “ ”. If the monitor is communicating
normally with the central monitoring system, the following icon is shown “ ”.
1.12 Built-in rechargeable battery
The monitor is equipped with a built-in rechargeable battery. The battery symbol
(“ “) in the top right corner of the screen indicates the status of the battery
capacity. The green bars indicate the battery level. When the battery is being charged,
an animated battery charging icon will appear. When the battery is fully charged, this
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 15
will be indicated using the following symbol: “ ”. If the monitor is not fitted with a
built-in battery, the symbol shows as “ ”, indicating no battery.
When operating on battery power, the monitor measures the battery level and triggers
an alarm when the battery level is insufficient; the prompt “BAT LOW” appears in the
information section. If this happens, the AC power cable should be plugged in; this will
immediately start to charge the battery before it can deplete. If battery continues to be
used as the power supply, the monitor will power off automatically when the battery is
exhausted.
Warning
If you have any doubts about the earthing arrangement or its performance, you must use
the built-in battery to power the monitor.
1.13 Installation
1.13.1 Open the box and check
Open the box and take out the monitor and accessories carefully. Keep the box for
possible future transportation or storage. Check the components against the packing
list.
• Check for any mechanical damage.
• Check all cables, modules and accessories.
If there is any problem, contact the distributor immediately.
1.13.2 Connect the power cables
Connection procedure for the AC power cable:
• Make sure the AC power supply complies with following specifications: 100-240
VAC, 50/60 Hz.
Connect the power cable provided to the monitor. Plug the power cable to the
INPUT socket on the monitor. Connect the other end of the power cable to an
earthed 3-phase power output.
Note
Connect the power cable to a hospital-grade socket.
• Connect to the ground line if necessary. Refer to the Chapter 13 "Patient Safety"
for details.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 16
1.14 Turning on the monitor
Press the power switch to turn on the monitor. The company logo will appear on the
screen. After approximately 15 seconds, during with the system performs a self-test,
the normal monitoring screen will appear. Monitoring can now commence as normal.
During the self-test, the model code will be displayed.
Notes
If the monitor finds any fatal errors during the self-test, it will trigger an alarm.
Check all functions that are to be used during monitoring, and make sure that the monitor
is operating normally.
The battery must be recharged to full capacity after each use to ensure adequate electrical
back-up.
Warning
If any signs of damage are detected, or if the monitor displays any error messages, do not
use it on any patients. Contact the biomedical engineer in the hospital or HEYER
Customer Service Center immediately.
Note
The interval between two presses of the POWER button must be more than 1 minute.
1.15 Connect patient sensors
Connect all necessary patient sensors between the monitor and the patient.
Note
For information on correct connection, please refer to the relevant chapter
(Chapters 5-11).
1.16 Check the recorder
If your monitor is equipped with a recorder, open the recorder door to check that the
paper is correctly loaded in the output slot. If no paper is present, please refer to the
Chapter 3 "Recording" for details.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 17
Chapter 2. Alarms
2.1 Alarms overview
2.1.1 Types of alarm
The alarms can be divided into two types: patient alarms and technical alarms.
Patient alarms: triggered if the patient's physiological parameters exceed the set limits,
e.g. patient’s body temperature exceeds the temperature alarm limit.
Technical alarms: triggered by an abnormality in a certain monitoring function or by a
distortion of monitoring results caused by a failure of the system or sensors, e.g.
disconnection of ECG leads.
2.1.2 Alarm levels
The alarms have three levels: high, medium and low.
The monitor has set levels for technical alarms and patient alarms.
2.1.3 Alarm modes
When an alarm is triggered, the monitor signals the alarm in three ways: audible alarm,
alarm light and descriptive alarm message.
The audible alarms are emitted by the speaker, the visible alarms occur at the LEDs,
and the alarm descriptions are displayed on the screen. The patient alarm is displayed
in the patient alarm information section, while technical alarms are displayed in the
monitor alarm information section.
When a patient alarm is triggered (caused by a measurement parameter exceeding the
alarm limit), the respective alarm limit that has been breached will light up on the
screen. This is in addition to the three means of alarm prompting mentioned above.
If there is “*” in the technical or physiological information section, this means a low-level
alarm. “**” means a medium-level alarm, and the background color of the relevant
section will turn yellow. “***” means a high-level alarm, and the background color of the
relevant section will turn red. For example: “** HR TOO HIGH” indicates a medium-
level alarm.
Patient alarms have 2 kinds of alarm mode: LATCH or Non Latch. LATCH means that
once an alarm has been triggered, the system will continue to indicate the alarm until
manual intervention (such as pushing the “SILENCE” button on the panel). Non Latch
means that the system will stop signaling an alarm once the condition that triggered the
alarm is no longer applicable.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 18
There are three alarm levels: high, medium and low. These are indicated by using
different lights and sounds, as demonstrated in the following table:
Alarm level Alarm light Characteristics of the audible alarm
High Alarm light flashes red with The audible alarm pattern “honk - honk - honk----
rapid frequency --honk - honk, honk - honk - honk------honk -
honk” sounds every 8 seconds
Medium Alarm light flashes yellow The alarm pattern “honk - honk - honk” sounds
with slow frequency every 25 seconds
Low Alarm light is yellow and The alarm pattern “honk” sounds every
continuous 25 seconds
2.2 Pausing the alarms
If the “PAUSE” key on the control panel is pressed, all audible alarms, alarm lights and
alarm messages are paused. The system enters a suspended alarm state. A
countdown is displayed in the technical alarm section to indicate how much longer the
alarm will be suspended.
Three options can be set for the alarm suspension time: 1 minute, 2 minutes and
3 minutes. To select the desired time, the user must enter the “Alarm Setting” window
and select the suspension time accordingly. If the “PAUSE” key is pressed again, the
system will restore to the normal state.
2.3 Silencing the alarms
Pressing the “SILENCE” key on the control panel will silence the audible alarm and
suspend the alarm light. Pressing the “SILENCE” key again will cancel this silencing of
the alarm, and the audible alarm and alarm lights will be reactivated accordingly,
returning to normal alarm conditions.
If an alarm state still exists while the alarm is silenced, the information segment on the
screen will display this alarm information.
If there is no alarm state triggered while the alarm is silenced, all alarms will be
cancelled.
Attention
When the system is operating in “SILENCE” mode, any newly triggered alarms will cause
the monitor to exit silence mode, and the system will return to normal alarm conditions.
2.4 Alarm Setting
The options below can be set by entering the “Alarm Setting” window:
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 19
1) Alarm Volume: The range is 1 - 10 (10 is the maximum volume).
2) Suspend Time: 1 minute, 2 minutes, 3 minutes.
3) Flash: If “On” is selected and there is patient alarm, the corresponding parameter
value will flash on screen to indicate that the parameter has triggered an alarm.
4) Para Alarm: 2 option - LATCH or Non Latch. LATCH means that once an alarm has
been triggered, the system will continue to indicate the alarm until manual
intervention (such as pushing the “SILENCE” button on the panel). Non Latch
means that the system will stop signaling an alarm once the condition that triggered
the alarm is no longer applicable.
5) Alarm Record: If “On” is selected, the recorder will record the alarm event when a
patient alarm occurs; recording will not take place if “Off” is selected.
6) Voice Alarm: If “On” is selected and an alarm is triggered, a human voice alarm will
continuously notify the user; no human voice alarm will be triggered if “Off” is
selected.
Fig. 2-1: Alarm settings
2.5 Alarm limits
Patient alarms are triggered according to the set limits. Various parameter limits are
show in a dark color in the upper left corner of the parameter segment. If the parameter
exceeds these limits, this triggers a patient alarm and the relevant limit value appears
in bright color. For example: the lower limit for heart rate is set at 80. If, like in our
example, the heart rate is 60 bpm, this triggers the alarm “HR TOO LOW”, and the
lower limit of the heart rate (in this case “80”) will appear in a bright color. The
parameter segment will appear as follows:
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 20
Fig. 2-2: Alarm Limit
2.5.1 ECG Alarm Limit
Select ECG alarm limits by entering the “ECG Alarm Limit” window:
Fig. 2-3: ECG Alarm Limit
The adjustment range for heart rate is listed below:
Patient type Adult Pediatric Neonate
HR high limit 300 350 350
HR low limit 15 15 15
The adjustment range for ST: -2.00mV – 2.00mV
The adjustment range for PVCs: 0 – 10
2.5.2 SpO2 Alarm Limit
Select SpO2 alarm limits by entering the “SpO2 Alarm Limit” window:
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 21
Fig. 2-4: SpO2 Alarm Limit
The adjustment range for SpO2 is: 0 – 100
The adjustment range for pulse rate is: 20 – 300.
2.5.3 NIBP Alarm Limit
Select the NIBP alarm limits by entering the “NIBP Alarm Limit” window:
Fig. 2-5: NIBP Alarm Limit
The adjustment range for NIBP alarm limits is as follows:
Patient type Adult Pediatric Neonate
Systolic pressure high limit 280 220 135
Systolic pressure low limit 40 40 40
Diastolic pressure high limit 220 160 100
Diastolic pressure low limit 10 10 10
Mean pressure high limit 240 170 110
Mean pressure low limit 20 20 20
2.5.4 Resp Alarm Limit
Select respiration alarm limits by entering the “Resp Alarm Limit” window:
Fig. 2-6: Resp Alarm Limit
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 22
The adjustment range for respiration rate limits is: 7 – 120
Patient type Adult Pediatric Neonate
RR high limit 120 150 150
RR low limit 7 7 7
2.5.5 Temp Alarm Limit
Select temperature alarm limits by entering the “Temp Alarm Limit” window:
Fig. 2-7: Temp Alarm Limit
The adjustment range for temperature alarm limits is: 0 – 50°C (32 – 122°F).
2.5.6 Load Default Alarm Limit
To restore the default alarm limits, enter the “Load Default Alarm limit” window:
Fig. 2-8: Load Default Alarm Limit
Selecting “Yes” will cancel all current alarm limit settings and restore the default alarm
limit settings.
2.6 Patient alarm information
The table below lists the alarm messages for all patient alarms:
Alarm message Trigger Condition
***ASYSTOLE Over 4 seconds with no heartbeat signals
*** APNEA No breaths recorded within the set time
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 23
Alarm message Trigger Condition
*** NO PULSE Over 15 seconds without a pulse signal
** HR TOO HIGH Heart rate has exceeded the upper alarm limit
** HR TOO LOW Heart rate has dropped below the lower alarm limit
** ST-I TO HIGH ST value in lead I has exceeded the upper alarm limit
** ST-I TOO LOW ST value in lead I has dropped below the lower alarm limit
** ST-II TO HIGH ST value in lead II has exceeded the upper alarm limit
** ST-II TOO LOW ST value in lead II has dropped below the lower alarm limit
** ST-III TO HIGH ST value in lead III has exceeded the upper alarm limit
** ST-III TOO LOW ST value in lead III has dropped below the lower alarm limit
** ST-AVR TOO HIGH ST value in lead AVR has exceeded the upper alarm limit
** ST-AVR TOO LOW ST value in lead AVR has dropped below the lower alarm limit
** ST-AVL TOO HIGH ST value in lead AVL has exceeded the upper alarm limit
** ST-AVL TOO LOW ST value in lead AVL has dropped below the lower alarm limit
** ST-AVF TOO HIGH ST value in lead AVF has exceeded the upper alarm limit
** ST-AVF TOO LOW ST value in lead AVF has dropped below the lower alarm limit
** ST-V TOO HIGH ST value in lead V has exceeded the upper alarm limit
** ST-V TOO LOW ST value in lead V has dropped below the lower alarm limit
** PVCs TOO HIGH The number of PVCs has exceeded the upper alarm limit
** SPO2 TOO HIGH Oxygen saturation has exceeded the upper alarm limit
** SPO2 TOO LOW Oxygen saturation has dropped below the lower alarm limit
** Pulse rate TOO HIGH Pulse rate has exceeded the upper alarm limit
** Pulse rate TOO LOW Pulse rate has dropped below the lower alarm limit
**NIBP SYS TOO HIGH NIBP systolic pressure has exceeded the upper alarm limit
**NIBP SYS TOO LOW NIBP systolic pressure has dropped below the lower alarm limit
**NIBP MEAN TOO HIGH NIBP mean pressure has exceeded the upper alarm limit
**NIBP MEAN TOO LOW NIBP mean pressure has dropped below the lower alarm limit
**NIBP DIA TOO HIGH NIBP diastolic pressure has exceeded the upper alarm limit
**NIBP DIA TOO LOW NIBP diastolic pressure has dropped below the lower alarm limit
** RR TOO HIGH Respiration rate has exceeded the upper alarm limit
** RR TOO LOW Respiration rate has dropped below the lower alarm limit
** TEMP1 TOO HIGH Body temperature in channel 1 has exceeded the upper alarm
limit
** TEMP1 TOO LOW Body temperature in channel 1 has dropped below the lower
alarm limit
** TEMP2 TOO HIGH Body temperature in channel 2 has exceeded the upper alarm
limit
** TEMP2 TOO LOW Body temperature in channel 2 has dropped below the lower
alarm limit
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 24
2.7 Technical alarm information
The table below lists the alarm messages for all patient alarms:
Alarm message Trigger condition Action required
** ECG LEAD OFF RL lead or more than 2 ECG Check the ECG lead connection.
leads become detached
** ECG LEAD RA OFF RA lead becomes detached Check the ECG lead connection.
** ECG LEAD LA OFF LA lead becomes detached Check the ECG lead connection.
** ECG LEAD LL OFF LL lead becomes detached Check the ECG lead connection.
** ECG LEAD V OFF V lead becomes detached Check the ECG lead connection.
** MODULE INIT ERR Error in the module self-test Restart the machine. If error is
still present, contact the factory
service.
***MODULE COMM The module and the main board Restart the machine. If error is
STOP communication have the problem still present, contact the factory
service.
** MODULE COMM The module and the main board Restart the machine. If error is
ERR communication have the problem still present, contact the factory
service.
** PARA ALARM LMT The parameter of the alarm limit Contact the factory service.
ERR has been modified by the
accident
** RANGE EXEED The observed value has Contact the factory service.
exceeded the measurement
range which the system can
carry out
** SpO2 SENSOR OFF SpO2 sensor not connected Check SpO2 sensor connection.
** SpO2 FINGER OFF The SpO2 sensor has fallen of Check SpO2 sensor is on finger.
the patient’s finger
SEARCHING SpO2 sensor connection is poor Check SpO2 sensor connection
PULSE... or the patient has move his/her and patient's current condition.
arm
** Temp1 SENSOR Body temperature channel 1 Check temperature sensor
OFF sensor not connected connection.
** Temp2 SENSOR Body temperature channel 2 Check temperature sensor
OFF sensor not connected connection.
** WATCHDOG ERR System monitoring (watch-dog) Restart the machine. If error is
by the main board has still present, contact the factory
malfunctioned service.
** SYSTEM TIME The system clock has not been Set the system time to the
LOST set current time. If error persists,
inform factory service.
** 12V HIGH The 12V voltage test exceeds the Restart the machine. If error is
normal voltage range still present, contact the factory
service.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 25
Alarm message Trigger condition Action required
** 12V LOW The 12V voltage test is lower Restart the machine. If error still
than the normal voltage range present, contact the factory
service.
** 3.3V HIGH The 3.3V voltage test exceeds Restart the machine. If error is
the normal voltage range still present, contact the factory
service.
** 3.3V LOW The 3.3V voltage test is lower Restart the machine. If error is
than the normal voltage range still present, contact the factory
service.
**BAT HIGH The battery voltage test exceeds Restart the machine. If error is
the normal voltage scope still present, contact the factory
service.
**BAT LOW Battery capacity is insufficient Connect to A/C current
immediately to carry on charging
the battery.
* NIBP LOOSE CUFF The cuff has not been connected Reconnect the blood pressure
cuff.
* NIBP AIR LEAK The cuff has not been connected Check the tube connection or
properly or there is a leak in the replace the cuff. If the error still
tubes exists, please contact the factory
service.
* NIBP DEFLATE ERR Problem when the blood Check the tube connection or
pressure cuff is deflating replace the cuff. If the error still
exists, please contact the factory
service.
* NIBP WEAK SIGNAL During blood pressure Ensure that patient type is set
measurement, the pulse signal correctly. Check the tube
too weak to be able to calculate connection or replace cuff. If the
blood pressure error still exists, please contact
the factory service.
* NIBP OUT OF During blood pressure Check the tube connection or
RANGE measurement, the blood replace the cuff. If the error still
pressure or the pulse signal exists, please contact the factory
exceeds the normal range and service.
the monitor is unable to carry out
the measurement
* NIBP MOVEMENT Patient has moved arm Check the patient positioning or
replace cuff. If the error still
exists, please contact the factory
service.
** NIBP OVER The pressure value exceeds the Check the tube connection or
PRESSURE measurement range replace the cuff. If the error still
exists, please contact the factory
service.
* NIBP SATURATE During blood pressure Check the patient positioning or
measurement, the pulse signal replace cuff. If the error still
exceeds the normal range and exists, please contact the factory
the monitor is unable to carry out service.
the measurement
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 26
Alarm message Trigger condition Action required
* NIBP PNEUMATIC The cuff has not been connected Check the tube connection or
FAIL properly or there is a leak in the replace the cuff. If the error still
air course exists, please contact the factory
service.
** NIBP SYSTEM ERR Blood pressure system self-test Restart the machine. If error is
error still present, contact the factory
service
** NIBP TIME OUT Blood pressure measurement Restart the machine. If error is
overtime still present, contact the factory
service
** NIBP CUFF TYPE Patient type set at adult when the Check the patient type or replace
WRONG neonate cuff has been used cuff. If the error is still present,
please contact the factory
service.
** NIBP MEASURE It has not been possible to Check the patient positioning or
FAIL calculate the blood pressure replace cuff. If the error still
exists, please contact the factory
service.
** NIBP RESET ERR Blood pressure measurement Restart the machine. If error is
has reset incorrectly still present, contact the factory
service.
Attention
1. When different levels of alarm are triggered simultaneously, the audible alarm emitted
corresponds to the highest level alarm.
2. While the alarm is paused, monitoring will not process any alarm information.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 27
Chapter 3. Recording
3.1 Record settings
Fig. 3-1: Record settings
1) Record wave 1, Record wave 2: there are five wave options to choose from: Off,
ECG1, ECG2, Pulse wave, Respiratory wave. The user may choose to record two
waves simultaneously or select the recording of one wave while recording of the
other wave is set to “Off”.
2) Record length: there are two options: “continuous” and “8 seconds”. “Continuous”
means that wave output is recorded continuously until the “RECORD” key is
pressed down again.
3) Record period: the time interval between two record outputs. There are 10 options:
Off, 10 minutes, 20 minutes, 30 minutes, 40 minutes, 50 minutes, 1 hour, 2 hours, 3
hours and 4 hours. The recording length is 8 seconds.
4) Record speed: there are two options: “25.0mm/s” and “50.0mm/s”.
5) Record grid: “Off” means non- grid output. “On” means grid output.
3.2 Record type
The monitor can carry out several kinds of types of recording: continuous real-time
recording; 8-second real-time recording; automatic 8-second recording.
3.2.1 Real-time recording
This means that real-time recording of the wave starts when the recording key is
pressed down and stops when the recording key is pressed down again during the
recording process .
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 28
3.2.2 Auto record
The monitor can trigger record output according to the time interval set. The recording
length is 8 seconds.
3.3 Record content
The record output includes the following information: recording type, patient
information, parameter table, recording time, wave name, wave amplitude and the
wave itself.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 29
Chapter 4. Admit/Discharge Patient
4.1 Admit patient
The steps for receiving anew patient are as follows:
Enter the “Patient Info” window by choosing the “Admit new patient” menu, and input
the patient information (see graphic below).
Fig. 4-1: Admit new patient
Select the “Ok” button to quit; the patient’s information will be accepted.
4.2 Discharge patient
Enter the “Discharge patient” window by selecting the ”Discharge patient” menu, as
shown in the following graphic.
Fig. 4-2: Discharge patient
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 30
Perform the following operations to discharge the patient:
1) Clear all patient information;
2) Clear all history data (including trend graphs, trend tables, blood pressure review,
wave review data).
Note
If do not discharge a patient first before admitting a new patient, the new patient’s
measurement data will be saved with the preceding patient's data. The monitor cannot
distinguish the new patient’s data from the data of the previous patient.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 31
Chapter 5. ECG Monitoring
The ECG measures the electrical activity of the heart and depicts this electrical activity
in wave-form on the monitor, together with the heart rate.
5.1 Connecting ECG electrodes
1) Prepare the patient’s skin before placing the electrode. A good signal at the
electrode provides the monitor with valid information for ECG data processing.
Clean the skin with soap and water (do not use ether and pure alcohol because this
can increase skin impedance) and wipe the skin dry vigorously to increase capillary
blood flow and remove dead skin and fat. If necessary, shave the hairs from the
area to which the electrode is to be attached.
2) Place the electrode on the patient’s body.
3) Connect the ECG lead to the patient cable.
5.2 ECG electrode placement
The positions for ECG electrode placement are as follows:
The RA (right arm) electrode — place in the subclavian area near the right shoulder.
The LA (left arm) electrode — place in the subclavian area near the left shoulder.
The LL (left leg) electrode — place under the left abdomen.
The RL (right leg) electrode — place under the right abdomen.
The V (chest) electrode — place on the chest.
Fig. 5-1: Positioning of electrodes
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 32
Warnings
• When connecting the cables and electrodes, make sure no conductive parts are in
contact with the ground. Verify that all ECG electrodes, including neutral electrodes,
are securely attached to the patient.
• Verify lead fault detection before start of monitoring. Unplug the ECG cable from the
socket, the screen will display the error message “ECG LEAD OFF” and the audible
alarm is activated.
• Use five lead wires. Use only silver/silver chloride (Ag/AgCl) ECG electrodes and
cables that meet AAMI standards.
• The following table shows the standard lead names and colors for Europe and the
United States.
United states Europe
Name of the lead Color Name of the lead Color
RA White R Red
LA Black L Yellow
LL Red F Green
RL Red N or RF Black
V Brown C White
5.3 Connecting ECG leads for surgical patients
The placing of the ECG leads will depend on the type of surgery that is being
performed. For example, with open chest surgery the electrodes may be placed
laterally on the chest or on the back. In the operating room, artifacts can sometimes
affect the ECG waveform due to the use of ESU (Electro Surgical Unit). To reduce this
effect, you can place the electrodes on the right and left shoulders and on the left side
of hypogastrium. Avoid placing the electrodes on the upper arms; otherwise the ECG
waveform will be too weak.
A good ECG wave is characterized as follows:
The QRS wave height is great and narrow with no notches.
The R wave height is big and located completely above the baseline or under.
The amplitude of the P wave and the T wave is smaller than 0.2mV.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 33
Fig. 5-2: Standard ECG wave
Warnings
• Do not touch the patient, table, bed or the equipment during defibrillation.
• Use only the recommended manufacturer ECG cable for monitoring. Other ECG cables
and leads may cause improper performance and/or provide inadequate protection
during defibrillation.
Note
Interference from a non-earthed device near the patient and ESU interference can cause
inaccuracy of the waveform.
Warning
When using ESU equipment, leads should be placed in a position at equal distance from
ESU electrotome and the grounding plate to avoid cautery. ESU equipment wire and ECG
cable must not be tangled up.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 34
5.4 ECG settings
Enter the “ECG setting” window by selecting the “ECG Setting” menu, which can be
seen in the following graphic:
Fig. 5-3: ECG settings menu
1) Pacemaker: When it is turned on, the pacing signal is shown as a vertical line
above ECG wave l; when it is turned off, the pacing signal will not be detected.
2) Channel 1 lead, Channel 2 lead: There are 7 leads: I, II, III, AVR, AVL, AVF, V.
3) Channel 1 size, Channel 2 size: There are four sizes: “×0.25”, “×0.5”, “×1”, “×2”.
A 1 millivolt scale is displayed to the right of the ECG wave, the height of which is
in direct ratio with the wave amplitude.
4) Notch: work frequency suppression switch; when it is “On”, it will filter the AC
interference of the ECG signal.
5) Filter: There are 3 filter modes: diagnostic, monitor and surgery.
In “Diagnostic” mode, the ECG wave without filtering is displayed;
In “Monitor” mode, the artifact which causes the false alarm is filtered out;
In “Surgery” mode, artifacts and the interference caused by electrosurgical
equipment can be reduced.
The filter modes are displayed above the ECG wave.
6) Heart volume: the range is from 0 to 10, “0” means that the sound of the
heartbeat is muted, “10” means it is on the maximum volume.
7) Wave speed: There are three levels of the ECG waveform tracing speed to be
chosen: 12.5, 25.0 and 50.0 mm/s.
8) HR source the options are “Auto”, “ECG”, “SpO2”. When “ECG” is selected, HR
and heart sound are from ECG; when “SpO2”is selected, HR and heart sound are
from SpO2; when “Auto” is selected, the patient monitor will automatically detect
the ECG and SpO2 signal. HR will come from ECG when and ECG signal exists,
otherwise it will come from SpO2.
9) ST switch: When it is “On”, ST analysis will be performed; otherwise it will not.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 35
10) ARR (arrhythmia) switch: When it is “On”, arrhythmia analysis is performed, which
shows the PVC parameters in the parameter area; otherwise, the arrhythmia
analysis isn’t performed, and the PCV parameters are not shown.
Note
When the “Pace” is turned on, arrhythmia related to PVC Premature Ventricular
Contractions (including the PVCs computation), will not be detected; simultaneously, ST
section analysis will not be performed
Warning
Do not touch the patient or the monitor during defibrillation.
In order to ensure patient safety, all leads must be connected to the patient.
When the electrosurgical (ES) equipment is used, position the ECG lead in the middle of
both the ES ground plate and the ES to avoid burning. The cable of the electrosurgical
equipment must not twist with the ECG cable.
When electrosurgical (ES) equipment is used, do not place the electrode on the ground
plate near the electrosurgical equipment. Otherwise, the ECG signal will be disturbed.
If monitoring a patient with a pacemaker, set “Pace” to “On”. If monitoring a patient without
pacemaker, set “Pace” to “Off”.
Regarding pacemaker patients, the pacing switch must be “On”; otherwise, it may
consider the pacing pulse as the normal QRS.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 36
Chapter 6. Respiration Monitoring
6.1 Principles of respiration measurement
When the human body breathes, chest impedance changes along with the breath. The
monitor receives the breath signal from the chest impedance values from the RA and
LL electrodes on the chest. After amplifying the signal of the impedance between the
electrodes (as a result of the thoracic activity), the breath wave will be displayed on the
screen.
6.2 Placing the electrodes
Connect the electrodes like the way that the heart electrodes are connected in
Chapter 5.1.
6.3 Respiration settings
Choose the “Resp Setting” menu and enter the “Resp Setting” window.
Fig. 6-1: Resp settings
1) Apnea time: This is an alarm to indicate when the patient is not breathing. The
apnea time (time between breaths) can be set between 10 seconds and 40
seconds. If the setting is set to ”Off”, this means that the apnea alarm is off.
2) Wave speed: you can set the wave speed to 6.25mm/s, 12.5mm/s or 25.0 mm/s.
3) Wave size: The user may set the wave amplitude enlargement factor. There are a
total of 5 levels: ×0.25, ×0.5, ×1, ×2, ×4.
4) RR Source: when “ECG” is selected, RR is from ECG leads; when “CO2” is
selected, RR is from the CO2 module and AwRR is displayed in the parameter
area.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 37
Notes
• Respiration monitoring is not recommended on a patient who moves a lot, as this may
trigger a false alarm.
• Place the RA and LL electrodes on opposite sides of the patient’s body in order to
obtain the best respiration wave. Avoid the liver area and the ventricles of the heart in
the line between the RESP electrodes to prevent cardiac overlay or artifacts from
pulsating blood flow. This is particularly important in neonates.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 38
Chapter 7. SpO2 Monitoring
Oxygen saturation (SpO2) is the measurement of oxygen saturation in arterial blood; it
is the percentage of hemoglobin bound to oxygen. For example, if 97% of hemoglobin
in arterial red blood cells is bound to oxygen, then this blood has 97% oxygen
saturation and the value reading on the monitor should be 97%.
7.1 Monitoring procedure
Fig. 7-1: Finger sensor placement
1. Switch on the monitor.
2. Attach the sensor to the appropriate site on the patient’s finger.
3. Plug the connector of the sensor extension cable into the SpO2 socket.
Note
Place the SpO2 sensor cable along the back of the patient’s hand. Make sure the
fingernail is just opposite to the light emitted from the sensor.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 39
7.1.1 Neonatal SpO2 plethysmography measurements
The neonatal SpO2 sensor consists of a Y-shaped SpO2 sensor and its sheath. Insert
the LED and PD ends of the Y-shape SpO2 sensor respectively into the upper and
lower grooves on the sheath (Fig. 7-2: Neonatal arterial oxygen probe (1)Fig. 7-2).
Fig. 7-3 shows the neonatal SpO2 sensor after insertion.
Y-shaped oxygen probe
Fig. 7-2: Neonatal arterial oxygen probe (1)
Fig. 7-3: Neonatal arterial oxygen probe (2)
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 40
7.1.2 Placement of the neonatal oxygen probe
Wind the SpO2 sensor around a hand or foot of a neonatal patient. Hold the sensor,
pull the belt and fit one of its sides with “V” edge into the “V” groove on the
corresponding side of the sheath. Appropriately elongate the belt to about 20mm, and
fit the “V” edge of the other side of the belt into the “V” groove of the other side of the
sheath. Then, loosen the belt. After the “V” edges of the two sides of the belt fit well
into the “V” grooves on the two sides of the sheath, put the belt into the first lock bar to
fasten the belt. See Fig. 7-4. If the belt is too long, you can put it into the second lock
bar. You must position the SpO2 sensor in this way so as to make the photoelectric
component face the correct position. Do not lengthen the belt too much, as this may
lead to inaccurate measurement and severely block blood circulation.
Fig. 7-4: Placement of the neonatal oxygen probe
Note
If the sensor cannot be positioned accurately, this may result in an inaccurate SpO2
reading, or it may even mean that the SpO2 cannot be measured because no pulse is
detected. If this is true, you must position the sensor again.
Excessive patient movement may result in an inaccurate reading. In this situation, you
must keep the patient still or change the site for monitoring in order to reduce the adverse
influence of excessive movement.
Warning
In the event of prolonged and continuous monitoring, you should check the peripheral
circulation and the skin every 2 hours. If any adverse changes take place, you should
change the measurement position in time.
In the event of prolonged and continuous monitoring, you should periodically check the
positioning of the sensor. If the positioning of the sensor moves during monitoring, the
measurement accuracy may be affected.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 41
7.2 Measurement restrictions
During operation, the following factors may affect the accuracy of the oxygen saturation
measurement:
1) High-frequency electrical jam, such as the interference which is produced by the
monitoring system itself or resulting, for example, from interference from
electrosurgery instruments connected with the system.
2) The blood oxymeter and the blood oxygen sensor must never be used during a
magnetic resonance imaging (MRI) scan, as the induced current may cause
burning;
3) Intravenous contrast agent;
4) Patient moving too frequently;
5) External illumination (such as typical office lighting);
6) Sensor installed incorrectly or in contact with the incorrect location on the object;
7) Body temperature (best body temperature should in 28°C - 42 C);
8) Placement of the sensor on an extremity that has a blood pressure cuff, arterial
catheter, or intravascular line
9) Density of the non-functional hemoglobin, such as carbooxyhemoglobin (COHb)
and methemoglobin (MetHb) and so on;
10) Loss of pulse signal can occur when
• The patient is in cardiac arrest or in shock.
• The patient has hypotension, severe vasoconstriction, severe anemia, or
hypothermia.
• There is arterial occlusion proximal to the sensor
11) Significant concentrations of dysfunctional hemoglobin, such as
carboxyhemoglobin and methemoglobin or
12) Injection of intravascular dye such as indocyanine green or methylene blue.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 42
7.3 SpO2 settings
Select the “SpO2 Setting” menu and enter the “SpO2 Setting” window.
Fig. 7-5: SpO2 settings
1) Pulse volume: the volume range is 0 to 10. 0 shows that pulse sound is muted; 10
is the maximum volume.
2) Sensitivity: the sensitivity for measuring the oxygen saturation value has three
option: “high”, “medium” and “low”.
3) Wave Speed: the wave scanning velocity has two options to choose between: 12.5
and 25mm/s.
4) Pulse Rate: when se to “On”, the parameter area will show the pulse rate;
otherwise the pulse rate will not be displayed.
5) Wave Mode: when “Line” is selected, the monitor will use line mode to draw the
pleth wave; when “Fill” is selected, the monitor will use fill mode to draw the pleth
wave.
Warning
1) In the presence of carbooxyhemoglobin, methemoglobin or dye dilution chemicals, the
oxygen saturation value may not be accurate.
2) The electric cables of electrosurgical equipment must not become entangled with the
sensor cable in the same place.
3) Do not use the sensor on extremities with arterial catheter or venous syringe
4) Make sure the nail covers the light window. The wire should be on the backside of the
hand.
5) Do not perform SPO2 and NIBP measuring in same arm simultaneously; because
obstruction of blood flow during NIBP measuring may adversely affect the SPO2 value.
6) Prolonged and continuous monitoring may increase jeopardy of unexpected change of
dermal condition such as abnormal sensitivity, erythema, vesicles, pressure necrosis,
and so on. It is especially important to check the sensor placement of neonate and
patient of poor perfusion or immature dermis by light collimation and proper attaching
strictly according to changes of the skin. Check per 2-3 hours the sensor placement
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 43
Warning
and move it when the skin deteriorates. More frequent examinations may be required
for different patients.
7) In the event of prolonged continuous monitoring, inspect the SpO2 measurement, the
peripheral circulation and the condition of the skin about every 2 hours. If the
discovered changes are not good, you should change the SpO2 measurement
promptly. At the same time, check periodically to ensure that the sensor is secure; this
is to avoid changes in the sensor fastness situation caused by the moving and so on,
as such factors can affect the accuracy of the measurement.
8) Inaccurate measurement can be caused by incorrect application or use of an SPO2
sensor; in case of lost measurement sensor has to be relocated.
9) Excessive movement during measurement of SpO2 may result in an inaccurate
measurement. In this case, the patient must be calmed down, and the measurement
sensor must be replaced.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 44
Chapter 8. NIBP monitoring
8.1 NIBP measurement procedure
Warnings
• Use accessories specified by HEYER only, otherwise the device may not function •
normally.
• Before starting a measurement, verify that you have selected a setting appropriate for
your patient (adult, pediatric or neonatal)
• Do not apply the cuff to a limb that has an intravenous infusion or catheter in place.
This could cause tissue damage around the catheter when the infusion is slowed or
blocked during cuff inflation.
• Make sure that the air tube connecting the blood pressure cuff and the monitor is
neither blocked nor tangled.
Notes
• If blood pressure measurement is to be used as the basis for establishing therapy, this
must be obtained using a different blood pressure measurement method, such as the
cuff/stethoscope auscultation method. Accordingly, the doctor must note that the
values obtained using other methods may differ from those obtained sing the SCALIS.
• NIBP monitoring uses the oscillometric method of measurement. Blood pressure
measurements obtained with this device are equivalent to those obtained by a trained
clinician using the cuff/stethoscope auscultation method and an intra-arterial blood
pressure measurement device, within the limits prescribed by the ANSI/AAMI SP10.
• This equipment is suitable for use in the presence of electrosurgical devices.
1) Insert the gas tube into the blood pressure socket of the monitor;
2) Place the blood pressure cuff around the patient’s upper arm or the thigh;
3) Use a suitable size cuff for the patient. Make sure that the symbol Ф is located over
a suitable artery. Make sure that the cuff is not too tight; otherwise this may cause
the limb periphery to change color, or it can even cut off blood supply;
4) Check that the edges of the cuff fall in the range marked <->.If not, swap for a more
appropriate cuff;
5) Make sure that the cuff is deflated completely;
6) Attach the cuff to the gas tube. The body part which is to be measured should
placed at the same horizontal level as the patient’s heart. If this is not possible, use
the following adjustment method to revision the measurement result:
If the cuff is at a higher horizontal level than the heart, add 0.75mmHg (0.10kPa) for
each centimeter difference.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 45
If the cuff is at a lower horizontal level than the heart, reduce the reading by
0.75mmHg (0.10kPa) for each centimeter difference.
7) Make sure that the patient type is correct (the patient type is displayed in the
information panel on the monitor, to the right side of the bed number).If it is
necessary to change the patient type, please enter the “Patient Information”
window and change the “Patient type”.
8) Press down the blood pressure measurement button on the front panel to start the
blood pressure measurement.
Fig. 8-1: Applying the cuff
Notes
• The width of the cuff should be either 40% of the limb circumference (50% for
neonates) or 2/3 of the upper arm length. The inflatable part of the cuff should be long
enough to encircle 50-80% of the limb. The wrong size of cuff can cause erroneous
readings. If there are any doubts about the cuff size, then use a larger cuff.
• For neonatal measurements, the maximum pressure of the cuff is 147mmHg. The
maximum pressure is 140mmHg when the cuff is used normally. The initial inflating
pressure of the cuff is 70mmHg during measurement.
Size of reusable cuff for neonates/children/adults
Patient Type Limb circumference Cuff width Tube
Neonate 10 -19 cm 8 cm 1.5 m or 3 m
Pediatric 18 - 26 cm 10.6 cm
Adult 1 25 - 35 cm 14 cm
Adult 2 33 - 47 cm 17 cm
Thigh 46 - 66 cm 21 cm
Size of disposable cuff for neonates/children/adults
Size No. Limb circumference Cuff width Hose
1 3.1 - 5.7 cm 2.5 cm 1.5 m or 3 m
2 4.3 - 8.0 cm 3.2 cm
3 5.8 - 10.9 cm 4.3 cm
4 7.1 - 13.1 cm 5.1 cm
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 46
8.2 NIBP measurement limitations
This device uses the oscillometric method for NIBP measurement. This kind of
measurement technique has certain limitations. The user should realize in the following
situations, the measured value may be unreliable, or the time required to measure
pressure may increase, or it may be impossible to perform the measurement.
1) Patient movement: If the patient is moving, trembles or experiences convulsions;
2) Arrhythmia: irregular heart beat caused by arrhythmia;
3) Heart-lung machine: if the patient is connected to a heart-lung machine;
4) Pressure fluctuations: for example, the patient’s blood pressure changes rapidly
while the blood pressure measurement is being performed;
5) Severe shock: for example, the patient is in severe shock or hypothermia;
6) Heart rate very high or low: if the heart rate is lower than 40bpm (heart beat/minute)
or higher than 240bpm (heart beat/minute), it is not possible to perform the blood
pressure measurement;
7) Obese patient: an excessively thick layer of fat can reduce the accuracy of the
measurement, because the fat can prevent the arterial pulse signal from reaching
the cuff.
8.3 NIBP settings
Fig. 8-2: NIBP settings
1) Unit: select the unit of pressure from the options “mmHg” or “kPa”.
2) Mode: there are 3 kinds of measurement mode: manual, automatic, STAT.
In the manual measurement mode, pressing down the blood pressure
measurement button on the control panel will result in a single manual
measurement of blood pressure;
In the automatic measurement mode, pressing down the blood pressure
measurement button on the control panel will result in a single immediate blood
pressure measurement, followed by automatic measurements initiated by the
monitor after a defined period;
In the STAT measurement mode, pressing down the blood pressure measurement
button on the control panel will start continuous measurement for 5 minutes.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 47
While measuring blood pressure, the user can stop the current blood pressure
measurement at any time by pressing down the blood pressure measurement
button on the control panel.
3) Period: This defines the automatic measurement interval. If the measurement mode
it set to “automatic”, then it will be possible to select a value in the “Period” field.
The following period options are available: 1 minute, 2 minutes, 3 minutes,
4 minutes, 5 minutes, 10 minutes, 15 minutes, 30 minutes, 60 minutes, 90 minutes,
2 hours, 3 hours, 4 hours, 8 hours.
After selecting the time interval, pressing down the blood pressure measurement
button will start the first automatic measurement. In order to stop automatic
measurement, select the “Manual” mode during the interval between measurement.
8.4 Blood pressure calibration
To perform calibration, use a pressure gauge (or mercury sphygmomanometer) with a
tolerance above 1 mmHg after calibration. Select “Noninvasive blood pressure
calibration” in the the “Maintenance” menu to start calibration. If the blood pressure
measurement button is pressed down during calibration, then the system will stop
calibrating.
Connect the pressure gauge and the cuff via a 3-way tube to the blood pressure
trachea jack on the monitor. Set the monitor to the “Calibration” mode, then inflate the
cuff using an air pump. First increase the pressure to 250 mmHg, then slowly deflate.
When the monitor display 200, 150 and 50 mmHg, the disparity between the standard
pressure gauge value and the monitor pressure value should be less than 3 mmHg. If
the value exceeds 3 mmHg, please contact our company’s service technician.
Note
The cuff has to be wrapped around a cylinder of an appropriate size.
Warning
You should calibrate NIBP measurements once every two years (or as required in your
hospital’s maintenance regulations). You should monitor performance according to the
following information.
8.5 Checking for leaks
When the cuff is connected, you can use this function to start inflating the air tubes to
discover whether the airway is in airtight condition or not. If the test is passed, the
system will not give any prompts. If the test is not passed, then a corresponding fault
prompt will appear in the noninvasive blood pressure parameter area.
The air leakage examination process:
1) Connect the cuff to the blood pressure socket on the monitor;
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 48
2) Wrap the cuff around a suitable cylinder;
3) Select “NIBP Pneumatic Test” in the “Service” menu. The noninvasive blood
pressure parameter area will display “Pneumatic test......”, indicating that the
system is starting to carry out a test for air leaks.
4) After about 20 seconds, the system will turn on the valve automatically, indicating
that the test for air leaks is complete;
5) If no prompt appears in the noninvasive blood pressure parameter area, this
indicates that the system does not leak air. If “Pneumatic leak!” is displayed, this
indicates that the air course possibly leaks air. The operator should check for loose
conditions and perform the air leakage test again after confirming that all
connections are OK.
Warning
1) Do not perform noninvasive blood pressure measurement on patients who have the
sickle cell anemia or damaged skin or this will result in injury.
2) Patients with susceptible to blood clots must be clinically assessed before deciding
whether to carry out the automatic blood pressure measurement, because there is a
risk of haematoma at the place where the body and the cuff rub together.
3) Before starting the measurement, you must confirm that the patient type is correct
(adult, pediatric, neonate).
4) Do not attach the cuff to a limb where there is an inravenous infusion or an inserted
syringe driver, as this may cause damage around the syringe driver when the
transfusion reduces speed or stops while cuff if inflating.
5) If noninvasive blood pressure measurement is used on automatic mode for too long,
then the limb with the cuff attached may develop purpura, lack of blood flow and
neuralgia. When monitoring the patient, it is necessary to check the luster, warmth and
sensitivity of limb periphery frequently. If any abnormalities are observed, please stop
the blood pressure measurement immediately.
6) Calibration of the noninvasive blood pressure measurement is supposed to be carried
out one time every year. (Or according to the maintenance regulations of your
hospital).
7) The cuff width should be 40% of the limb circumference (50% for neonates) or the 2/3
of the upper arm length. The length of the cuff inflation part should long enough to
surround 50-80% of the limb. A cuff of inappropriate size can result in an incorrect
reading. If there are any doubt about the cuff size, a bigger cuff should be used in order
to reduce errors.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 49
Chapter 9. Temperature Monitoring
9.1 Steps for temperature measurement
1) Insert temperature sensor directly into the socket.
2) Turn patient monitor on.
9.2 Temperature settings menu
Select the “Temperature setting” menu and enter the “Temp Setting” window:
Fig. 9-1: Temperature settings
Unit: Choose the unit of temperature °C or °F.
Warning
Before starting to use temperature measurement, please check whether the sensor cable
is normal. Unplug the temperature sensor cable from the socket: the screen will display
the error message “Temp sensor off” and emit an audible alarm.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 50
Chapter 10. History Review
The monitor can store 72 hours of trend data for all of the monitored parameters, and it
can store noninvasive blood pressure measurement data for 1,000 readings. The
monitor collects parameter data every minute and saves it in trend data. The user may
choose a trend graph or trend table to examine the trend data. Every time a
noninvasive blood pressure measurement value is obtained, it is stored in the
noninvasive blood pressure trend data. The user can choose noninvasive blood
pressure review to look over the noninvasive blood pressure trend data.
10.1 Trend Graph
The trend graph allows the use to view the stored trend data in graph mode. The most
recent 72 hours of trend data is displayed as a trend curve with a resolution of
1 second, 5 seconds, 1 minute, 2 minutes, 3 minutes, 4 minutes or 5 minutes.
Choosing “Trend Graph” in the “Review” menu will open the following window:
Fig. 10-1: Trend Graph
In the Trend Graph window, the time is shown underneath the X axis, with the most
recent time displayed on the nearest right side. The value ranges for the various
parameters is displayed on left side of the Y axis.
10.1.1 Select parameters
By selecting the “Parameter” box with cursor, the user may select the parameter trend
that is to be displayed. When the desired parameter appears, its trend graph will be
shown in the window by pressing down the revolving button.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 51
10.1.2 Set period
By selecting the “Period” option, the user may choose a period of 1 second, 5 seconds,
1 minute, 2 minutes, 3 minutes, 4 minutes or 5 minutes.
10.1.3 Adjust observation time
With the button “ ” and “ ”, the operator may move the time of trend graph a forward
or backward by one second (current period). With the button “ ” and “ ”, the
operator may move the time of trend graph a page forward or backward. By selecting
the button “ ” the operator may move the time of trend graph 72 hours backward, and
“ ” to current time.
10.2 Trend table
The trend table allows the operator to observe the trend data in tabular mode. The
most recent 72 hours trend data is displayed as a trend curve with a resolution of
1 minute, 2 minutes, 3 minutes, 4 minutes, 5 minutes, 10 minutes, 15 minutes,
30 minutes or 60 minutes.
Choosing “Trend Table” in the “Review” menu will open the following window:
Fig. 10-2: Trend table menu
In “Trend Table” window, the time shows underneath the parameter columns: the most
recent time is displayed on the nearest right side; the parameter name and the unit are
displayed in the first column.
Alarm events can also be observed in the trend table: The time of any triggered alarms
is also saved in the trend data. If a parameter triggers an alarm, the trend data in the
corresponding alarm time period will be displayed with a yellow background color.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 52
10.2.1 Set period
By selecting the “Period” option with the cursor, the operator may choose a period of
1 minute, 2 minutes, 3 minutes, 4 minutes, 5 minutes, 10 minutes, 15 minutes,
30 minutes or 60 minutes.
10.2.2 Adjust observation time
With the buttons “ ” and “ ”, the operator may move the time of trend graph a step
forward or backward (current period). With the buttons “ ” and “ ”, the operator may
move the time of trend graph a page forward or backward. By selecting the button “ ”,
the operator may move the time of trend graph 72 hours backwards, and “ ” to the
current time.
10.3 Alarm review
When a patient alarm occurs, the monitor will save all the parameters and a 16-second
wave in the alarm event database. The monitor can display 200 alarm events in the
alarm review.
Selecting “Alarm Review” in the “Review” menu will display recent alarm event
information, just as the following chart shows:
• Sequence number: format is I/N whereby I means the index of alarm event and N
means the total number of alarm events in the database, as shown in Fig. 10-3. The
most recent alarm has the smallest number, e.g. No 1 means the most recent alarm.
• Alarm event time;
• Alarm event type;
• Parameters when alarm occurs;
• 2 wave channels, 16 seconds for each channel;
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 53
Fig. 10-3: Alarm review
10.3.1 Alarm Type
There are 6 types of alarm event: “All”, “ECG”, “NIBP”, “SpO2”, “RESP”, “TEMP”, “All”
means all parameters. User can select which parameter’s alarm event to view.
10.3.2 Choose Alarm event
The user may use the “ “ and “ “ buttons to choose an alarm event. By selecting
the “ “ button, the previous event will be displayed. By selecting the “ “ button, the
next event will be displayed,
10.3.3 Select wave
With the buttons “ “ and “ “, the operator may move the alarm wave a page forward or
backward.
10.3.4 Record
The recorder will print out the current alarm event if the user presses the ”Record”
button.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 54
10.4 NIBP Review
The monitor can display the 1000 most recent pieces of noninvasive blood pressure
measurement data in the NIBP review.
Selecting “NIBP Review” in the “Review” menu will display the results and the times of
the 10 most recent pieces of noninvasive blood pressure measurement data, just as
the following window shows:
Fig. 10-4: NIBP measurement review
The data is arranged in order according to the time. The most recent measurement
data is displayed at the top. 10 lines of measurement data can be displayed on the
screen at a time. The buttons “ ” and “ ”can display the previous or the next
measurement data. With the buttons “ ” and “ ”, the operator can move the review
table a page forward or backward. By selecting the button “ ”, the operator may see
the earliest measurement data, and “ ”the most recent.
10.5 Wave review
The monitor can display 1 hour of wave data in the wave review.
Selecting “Wave Review” in the “History Review” menu will display the most recent
wave data, just as the following chart shows:
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 55
Fig. 10-5: Wave review
The section above the wave shows the related information: wave scanning velocity,
current review time, and a table of the measured parameters.
10.5.1 Select waveform
By selecting “Wave1” and “Wave2” with the cursor, the operator may choose the wave
that he wants to observe: ECG1, ECG2, pulse wave and resp wave.
10.5.2 Adjust observation time
With the buttons “ “ and “ “, the operator may move the wave a page forward or
backward. With the buttons “ “ and “ “, the operator may move the wave one minute
forward or backward. By selecting the button “ “, the operator may move the
waveform time one hour backward, and “ “ will jump to the current time.
Note
Trend data can be stored for 720 hours after turning off of the monitor. If the monitor is
turned on after more than 720 hours without power, the trend data will be erased.
Wave review data can be stored for 2 hours after turning off the monitor. If the monitor is
turned on after more than 2 hours without power, the wave review data will be deleted.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 56
Chapter 11. Drug Calculation
This monitor provides the function of dose calculation for 21 kinds of medicines and the
titration table.
11.1 Drug Calculation
The kinds of medicine that can be calculated include: AMINOPHYLLIN,
DOBUTAMINE, DOPAMINE, EPINEPHRINE, HEPARIN, ISUPREL, INOCOR,
INSULIN, INSUPREL, LIDOCAINE, NIPRIDE, NITROGLYCERIN,
NOREPINEPHRINE, PITOCIN, PROCAINAMIDE, VASOPRESIN. DRUG A, DRUG B,
DRUG C, DRUG D, DRUG E have been provided in addition to easily replace any kind
of medicine.
Selecting “Dose Calculation” in the menu will open the window as shown in the
following graphic:
Fig. 11-1: Dose calculation
Dose calculation can apply the following formulas:
Concentration = Amount/volume
Inf rate = Dose / Concentration
Duration = Amount / Dose
Dose = Inf rate × Concentration
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 57
11.2 Operating procedures
In the Dose Calculation window, the operator should first choose the name of the drug
that is to be calculated, then confirm the patient’s weight, and input other values that
are already known.
Rotate the knob and move the cursor to each calculation item in the formula
separately. Press down and rotate the knob, select the calculation values. After
selection, the value of the calculated item will be displayed in the corresponding place.
Drug name selection: move the cursor to ”drug name”, rotate the knob. It is possible to
choose from 21 kinds of medicines, AMINOPHYLLIN, DOBUTAMINE, DOPAMINE,
EPINEPHRINE, HEPARIN, ISUPREL, INOCOR, INSULIN, INSUPREL, LIDOCAINE,
NIPRIDE, NITROGLYCERIN, NOREPINEPHRINE, PITOCIN, PROCAINAMIDE,
VASOPRESIN, DRUG A, DRUG B, DRUG C, DRUG D, DRUG E. Only one type of
medicine can be calculated at a time.
11.3 Titration table
Select “Titration Table” in the “Dose calculation” menu to switch to the titration table
function.
The following graphic shows the titration table function:
Fig. 11-2: Titration table
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 58
1) Move the cursor to the “DoseType” option; press down the knob to choose dosage
unit.
2) Move the cursor to the “Item” option, then press down the knob to choose “Dose” or
“Inf Rate”. Selecting “Dose” will calculate the infusion rate taking the dose as the
basis of calculation. Selecting “Inf Rate” will calculate the dose taking infusion rate
as the basis of calculation.
3) Move the cursor to the “Step” option; press down the knob to choose the number of
steps. The range of options is 1 - 10.
4) With the buttons “ ” and “ ”, the operator may move the titration table a step
backward or forward. With the buttons “ ” and “ ”, the operator may move the
table a page forward or backward. By selecting the button “ ”, the operator may
display the minimum titration table data, and “ ” the maximum.
5) The recorder will print out the current titration table if the “Record” button is
pressed.
6) Move the cursor to the “Return” button and press down the knob to get back to the
“Dose calculation” menu.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 59
Chapter 12. Maintenance and Cleaning
12.1 System Check
Before using the monitor, you must:
• Check if there is any mechanical damage;
• Check that all external cables, inserted modules and accessories are in good
condition;
• Check that all monitoring functions of the monitor are working normally so as to
make sure that the monitor is in good condition.
If you find any damage on the monitor, stop using the monitor on the patient and
contact the biomedical engineer of the hospital or the HEYER Customer Service
Department immediately.
A complete check of the monitor, including the functional safety check, must be
performed by qualified personnel once every 6 to 12 months or each time after repair.
All checks that require the casing of the monitor to be opened must be performed by
qualified service personnel. Safety and maintenance checks can also be conducted by
HEYER personnel. You can obtain information about the customer service contract
from your local HEYER office.
HEYER provides all SCALIS circuit diagrams, parts lists and standard instructions.
Warning
If the hospital or agency that using the monitor does not follow a satisfactory maintenance
schedule, the monitor may become invalid, and human health may be endangered.
12.2 General Cleaning
Warning
Turn off the power and disconnect the power line before cleaning the monitor or the
sensor/probe.
The SCALIS Multi-Parameter Patient Monitor must be kept dust-free.
It is recommended that you should clean the outside surface of the monitor casing and
the display screen regularly. Only use non-caustic detergents such as soap and water
to clean the monitor casing.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 60
Caution
Pay special attention to the following to avoid damaging the SCALIS monitor:
1. Avoid using ammonia-based or acetone-based cleaners such as acetone.
2. Most cleaning agents must be diluted before use. Dilute the cleaning agent as per the
manufacturer's instructions.
3. Do not use abrasive material, such as steel wool etc.
4. Do not let the cleaning agent enter the monitor. Do not immerse any part of the system
into liquid.
5. Do not leave cleaning agents on any part of the equipment.
12.3 Cleaning Agents
Apart from the cleaning agents specified in the above “Caution”, you can use any of
the solutions listed below as the cleaning agent.
• Diluted ammonia water
• Diluted sodium hypochlorite (bleach).
Note
Diluted sodium hypochlorite from 500ppm (1:100 diluted bleach) to 5000ppm (1:10 bleach)
is very effective. The concentration of the diluted sodium hypochlorite depends on how
many organisms (blood, mucus) are left on the surface of the casing.
• Diluted formaldehyde 35% -- 37%
• Hydrogen peroxide 3%
• Alcohol
• Isopropanol
Notes
• You can use hospital-grade ethanol to clean the SCALIS monitor and its sensor/probe.
Leave it to dry naturally or use a clean cloth to dry it.
• HEYER bears no responsibility for the effectiveness of controlling infectious disease
using these chemical agents. Please contact infectious disease experts in your hospital
for details.
12.4 Sterilization
To avoid extensive damage to the equipment, sterilization is only recommended when
stipulated as necessary in the Hospital Maintenance Schedule. Sterilization facilities
must be cleaned first.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 61
Recommended sterilization materials: ethylate and acetaldehyde.
Appropriate sterilization materials for ECG leads and blood pressure cuffs are
mentioned in the chapters “ECG Monitoring”, “Respiration Monitoring” and “NIBP
Monitoring” respectively.
Caution
• Follow the manufacturer’s instructions to dilute the solution, or use the lowest possible
concentration.
• Do not let liquid enter the monitor.
• Do not immerse any part of the monitor in liquid.
• Do not pour liquid onto the monitor during sterilization.
• Use a moistened cloth to wipe off any agent remaining on the monitor
12.5 Disinfection
To avoid extensive damage to the equipment, disinfection is only recommended when
stipulated as necessary in the Hospital Maintenance Schedule. Disinfection facilities
should be cleaned first.
Appropriate disinfection materials for the ECG lead, SpO2 sensor, blood pressure cuff
and TEMP probe are introduced in the relevant chapters.
Caution
Do not use EtO gas or formaldehyde to disinfect the monitor.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 62
Chapter 13. Patient Safety
The Patient Monitor is designed to comply with the International National Safety
requirements for medical electrical equipment, IEC60601-1, EN60601-2-27 and
EN60601-2-30. This device has floating inputs and is protected against the effects of
defibrillation and electrosurgery. If the correct electrodes are used and applied in
accordance with the manufacturer’s instructions (see Chapters ECG/RESP
Monitoring), the system can restore screen display within 10 seconds of defibrillation.
This symbol indicates that the instrument is IEC60601-1 Type CF
equipment. The unit displaying this symbol contains an F-Type isolated
(floating) patient applied part providing a high degree of protection against
shock, and is suitable for use during defibrillation.
Warning
Do not come into contact with patients, beds or the monitor during defibrillation.
13.1 Environment
Follow the instructions below to ensure complete and safe electrical installation. The
environment where the PM-5000 Multi-Parameter Patient Monitor will be used should
be reasonably free from vibration, dust, corrosive or explosive gases, extremes of
temperature, humidity, and so on. For cabinet-mounted installation, allow sufficient
room at the front for operation and sufficient room at the rear for servicing with the
cabinet access door open.
The Patient Monitor operates within specifications at ambient temperatures between
0°C and 40°C. Ambient temperatures that exceed these limits may affect the accuracy
of the instrument and cause damage to the modules and circuits. Allow at least
2 inches (5cm) clearance around the instrument for proper air circulation.
13.2 Power Requirements
See Chapter 15 "Appendix - Product Specifications".
13.3 Grounding
To protect the patient and hospital personnel, the casing of the Patient Monitor must be
grounded. Accordingly, the Patient Monitor is equipped with a detachable 3-pin cable
which grounds the instrument to the power line ground (protective earth) when plugged
into an appropriate 3-pin socket. If a 3-pin socket is not available, consult the hospital
electrician.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 63
Warning
Do not use a 3-pin to 2-pin adapter with this device.
To protect the patient and hospital personnel, the case of patient monitor must be
grounded. If after consulting the instrument specifications the user is confused as to
whether a particular combination of equipment is dangerous, the user should consult
the manufacturer or other experts in this field to ensure that all instruments which
require security will not be damaged by the proposed combination.
13.4 Equipotential grounding
Protection class I instruments are already included in the protective grounding
(protective earth) system of the room by way of grounding contacts in the power plug.
For internal examinations on the heart or the brain, the portable Patient Monitor must
have a separate connection to the equipotential grounding system. One end of the
equipotential grounding cable (potential equalization conductor) is connected to the
equipotential grounding terminal on the rear panel of the monitor and the other end to
one point of the equipotential grounding system.
The equipotential grounding system is for the safety function of the protective
grounding conductor if ever there is a break in the protective grounding system.
Examinations in or on the heart (or brain) should only be carried out in medically used
rooms incorporating an equipotential grounding system. Check each time before use
that the instrument is in perfect working order.
13.5 Condensation
When the equipment is moved from one room to another, condensation may form. This
is because the equipment may be exposed to humid air and temperature differences,
among other reasons.
Warning
If there are places where flammable anesthetics are used, there will be a risk of explosion.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 64
Chapter 14. EMC
The monitor meets the requirements of IEC 60601-1-2:2001
Caution
The use of unapproved accessories may diminish the monitor performance.
Notes
The monitor should not be used adjacent to or stacked upon other equipment. If adjacent
or stacked use is necessary, the monitor should be observed to verify normal operation in
the configuration in which it will be used.
The monitor needs special precautions regarding EMC and needs to be installed and put
into service according to the EMC information provided below.
Portable and mobile RF communications equipment can affect this monitor. See tables
14-1, 14-2, 14-3, and 14-4 below.
Table 14-1: Guidance and HEYER declaration — electromagnetic emissions
The monitor is intended for use in the electromagnetic environment specified below. The
customer or the user of the monitor should assure that it is used in such an environment.
Emissions test Compliance Electromagnetic environment — guidance
RF emissions Group1 The monitor uses RF energy only for its internal
CISPR 11 function. Therefore, its RF emissions are very low and
are not likely to cause any interference with nearby
electronic equipment.
RF emissions Class A The monitor is suitable for use in all establishments
CISPR 11 other than domestic and those directly connected to
the public low-voltage power supply network that
supplies buildings used for domestic purposes
Harmonic Class A
Emissions
IEC61000-3-2
Voltage Compliance
Fluctuations/
Flicker
Emissions IEC
61000-3-3
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 65
Table 14-2: Guidance and HEYER declaration — electromagnetic immunity
The monitor is intended for use in the electromagnetic environment specified below.
The customer or the user of the monitor should assure that it is used in such an environment.
Immunity test IEC 60601 Compliance level Electromagnetic environment —
Test level guidance
Electrostatic ±6 kV contact ±6 kV contact Floors should be wood, concrete
Discharge ±8 kV air ±8 kV air or ceramic tile. If floors are
(ESD) covered with synthetic material,
IEC 61000-4-2 the relative humidity should be at
least 30%.
Electrical Fast ±2 kV for power ±2 kV for power Mains power quality should be
Transient/Burst supply lines ±1 kV supply lines ±1 kV that of a typical commercial or
IEC 61000-4-4 for input/output for input/output hospital environment.
lines (>3m). lines (>3m).
Surge ±1 kV differential ±1 kV different Mains power quality should be
IEC 61000-4-5 mode ±2 kV mode ±2 kV that of a typical commercial or
common mode common mode hospital environment.
Voltage dips, <5% UT <5% UT Mains power quality should be
Short (>95% dip in UT) (>95% dip in UT) that of a typical commercial or
interruptions and for 0.5 cycle for 0.5 cycle hospital environment. If the user
voltage variation of our product requires continued
on power supply 40% UT 40% UT operation during power mains
input lines (60% dip in UT) for (60% dip in UT) for interruptions, it is recommended
IEC 61000-4-11 5 cycle 5 cycle that our product be powered from
an uninterruptible power supply or
70% UT 70% UT a battery.
(30% dip in UT) for (30% dip in UT) for
25 cycle 25 cycle
<5% UT <5% UT
(>95% dip in UT) (>95% dip in UT)
for 5 sec for 5 sec
Power 3 A/m 3 A/m Power frequency magnetic fields
frequency should be at levels characteristic
(50/60 HZ) of a typical location in a typical
magnetic field commercial or hospital
IEC 61000-4-8 environment.
UT is the AC mains voltage prior to application of the test level.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 66
Table 14-3: Guidance and HEYER declaration — electromagnetic immunity
The monitor is intended for use in the electromagnetic environment specified below. The
customer or the user of the monitor should assure that it is used in such an environment
Immunity test IEC 60601 Compliance Electromagnetic environment — guidance
Test level level
Portable and mobile RF communications
equipment should be used no closer to any
part of the monitor, including cables, than the
recommended separation distance
calculated from the equation applicable to
3 Vrms the frequency of the transmitter.
Conducted RF
150kHz to 3 Vrms
IEC 61000-4-6
80MHz Recommended separation distance
d = 1.2 x P
d = 1.2 x P 80 MHz to 800 MHz
d = 2.3 x P 800 MHz to 2.5GHz
where P is the maximum output power rating
of the transmitter in watts (W) according to
the transmitter manufacturer and d is the
recommended separation distance in meters
(m).
Radiated RF 3 V/m 80MHz Field strengths from fixed RF transmitters,
to 2.5 GHz 3V/m as determined by an electromagnetic site
IEC 61000-4-3 a
survey, should be less than the
compliance level in each frequency range
b
Interference may occur in the vicinity of
equipment marked with the following
symbol:
Note — At 80 MHz and 800 MHz, the higher frequency range applies.
Note — These guidelines may not apply in all situations. Electromagnetic propagation is
affected by absorption and reflection from structures, objects and people.
a
Field strengths from fixed transmitters, such as base stations for radio (cellular/cordless)
telephones and land mobile radios, amateur radio, AM and FM radio broadcast and TV
broadcast cannot be predicted theoretically with accuracy. To assess the electromagnetic
environment due to fixed RF transmitters, an electromagnetic site survey should be
considered. If the measured field strength in the location in which the monitor is used
exceeds the applicable RF compliance level above, the monitor should be observed to verify
normal operation. If abnormal performance is observed, additional measures may be
necessary, such as reorienting or relocating the monitor.
b
Over the frequency ranges 150kHz to 80MHz, field strengths should be less than 3V/m.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 67
Table 14-4: Recommended separation distances between portable and mobile RF
communication and the monitor
The monitor is intended for use in an electromagnetic environment in which radiated RF
disturbance is controlled. The customer or the user of the monitor can help prevent
electromagnetic interference by maintaining a minimum distance between portable and mobile
RF communication equipment (transmitters) and the monitor as recommended below, according
to the maximum output power of the communication equipment.
Rated Maximum Separation Distance According to Frequency of Transmitter
Output power of M (Meters)
Transmitter W 150kHz -2MHz 80MHz -800MHz 800MHz -2.5GHz
(Watts)
d = 1.2 P d = 1.2 P d = 2.3 P
0.01 0.12 0.12 0.23
0.1 0.37 0.37 0.74
1 1.17 1.17 2.34
10 3.69 3.69 7.38
100 11.67 11.67 23.34
For transmitters at a maximum output power not listed above, the recommended separation
distance in meters (m) can be determined using the equation applicable to the frequency of the
transmitter, where P is the maximum output power rating of the transmitter in watts (W)
according to the transmitter manufacturer.
Note — At 80 MHz and 800 MHz, the separation distance for the higher frequency range
applies.
Note — These guidelines may not apply in all situations. Electromagnetic propagation is
affected by absorption and reflection from structures, objects and people.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 68
Chapter 15. Appendix - Product Specifications
Warning
The patient monitor may not meet its performance specifications if stored or used outside
the manufacturer’s specified temperature and humidity range.
15.1 Classification
Item Specification
MDD classification Class IIb
Anti-electroshock degree Class I equipment with internal power supply
TEMP/SpO2/NIBP: BF
Anti-electroshock degree
ECG/RESP CF
Explosion proof level Ordinary equipment. without explosion proof
Harmful liquid proof degree Ordinary equipment, without liquid proof
Working system Continuous running equipment
15.2 Applicable Standards
Medical Device Directive 93/42/EEC
EN60601-1+A1+A2 or IEC60601-1+A1+A2, Medical Electrical Equipment, Part 1:
General Requirements for Safety
EN60601-1-1 or IEC60601-1-1, Medical Electrical Equipment- Part 1-1: General
Requirements for Safety - Collateral Standard: Safety Requirements for Medical
Electrical Systems
IEC60601-1-4, Medical Electrical Equipment- Part 1-4: General Requirements for
Safety - Collateral Standard: Programmable Electrical Medical Systems
IEC60601-2-49 Medical Electrical Equipment-Part 2-49: Particular Requirements for
the Safety of Multifunction Patient Monitoring Equipment
IEC 60601-1-2:2007, Electromagnetic Compatibility – Medical Electrical Equipment
15.3 Size and weight
Size 368 × 345 × 187 mm
Weight 5 kg
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 69
15.4 Power Supply
a.c. 100V~240 V, 50Hz/60 Hz, Pmax=90VA, Fuse T1.5AL 250V
15.5 Battery
2.3 Ah 12V rechargeable battery
Operating time after full charge is more than 1 hour
Operating time after the first alarm of low battery will be about 5 minutes
Maximum charging time is less than 6 hours.
15.6 Signal Interface
Network interface standard RJ45 Socket
15.7 Storage
Trend 720 hours
NIBP review 1000 NIBP events
Wave review 2 hours
Alarm review 200 alarm events
All storage data are non volatile.
15.8 Environment
Temperature
Working 0 - 40°C
Storage -20 - 50°C
Humidity
Working 15% - 90 %
Storage 15% - 90 % (no coagulation)
Atmospheric pressure
Working 86.0 kPa - 106.0kPa;
Storage 86.0 kPa - 106.0kPa
15.9 ECG
15.9.1 Heart rate calculation method
The average of the last 4 R-to-R intervals, when last 3 R-to-R intervals > 1200msec.
Otherwise, the average of the last 12 R-to-R intervals, minus the maximum and
minimum values. The update rate of the Heart Rate on the display is once per second.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 70
15.9.2 Heart rate meter accuracy and arrhythmia response
After 20s stable time, the monitor will display a): heart rate display 40bpm ± 5bpm; b):
heart rate display 30bpm ±5bpm; c): heart rate display 120bpm±5bpm; d): heart rate
display 45bpm±5bpm.
a) Couplet rhythm — two waves of duration is 1500ms; if calculate all the QRS
complex, heart rate is 80bpm, if only calculate large R wave or S-wave, the heart
rate is 40bpm.
b) Slow change couple rhythm — if calculate all the QRS complex, heart rate is
60bpm, if only calculate large waves, heart rate is 30bpm.
c) Fast couple rhythm — if the calculate all the QRS complex, heart rate is 120bpm.
d) bi-directional contraction — if calculate all the QRS complex, heart rate is 90bpm, if
only large waves, heart rate is 45bpm.
15.9.3 Lead mode
5 Leads: RA, LA, LL, RL, V; lead mode: I, II, III, AVR, AVL, AVF, V
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 71
15.9.4 Gain
x2.5mm/mV, 5.0mm/mV, 10mm/mV, 20mm/mV
15.9.5 Sweep speed
12.5mm/s, 25mm/s, 50mm/s
15.9.6 Heart rate
Measurement range:
Adult 15 - 300 bpm
Neonatal/Pediatric 15 - 350 bpm
Accuracy ± 1%
Resolution 1 bpm
15.9.7 Sensitivity
> 200 µV P-P
15.9.8 Differential Input Impedance
> 5 M ohm
15.9.9 Bandwidth
Surgery 1 - 20 Hz
Monitor 0.5 - 40 Hz
Diagnostic 0.05 - 130 Hz
15.9.10 CMRR
Diagnostic Mode >90 dB
Monitor Mode >110 dB
Surgery Mode >110 dB
15.9.11 Electrode offset potential
±300mV
15.9.12 Input dynamic range
The device shall be capable of responding to and displaying differential voltages of
±5 mV varying at a rate up to 320 mV/s from a dc offset voltage in the range of
-300 mV to +300 mV, when applied to any lead. The time-varying output signal
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 72
amplitude shall not change by more than ±10 percent over the specified range of dc
offset.
15.9.13 Pacing pulse suppression
When the pace switch is “On”, the patient monitor can inhibit pace pulse without affect
heart rate calculation: ± 2 mV - ± 700mV, width: 0.1ms - 2ms, rise time: 10µs - 100µs
normal QRS wave single pulse without overshoot pacing pulse.
When the pace switch is “On”, the patient monitor can inhibit pace pulse without affect
heart rate calculation: ± 2 mV - ± 5mV, width: 0.5ms - 2ms, rise time: 10µs - 100µs
single pulse overshoot normal QRS waves of pacing pulses.
Overshoot (a0) range should 0.025ap to 0.25ap range, independent of the choice of
time constant, but not more than 2mV;
When the pace switch is “On”, pace pulse inhibition of rapid ECG signal to 1V / s RTI
minimum input slew rate.
15.9.14 QRS wave amplitude and period range between
The minimum range of QRS amplitude (ar + as) is 0.5 mV to 5 mV, and the duration of
the QRS wave is between 70 ms and 120 ms (40 ms and 120 ms for neonatal/pediatric
monitors). For monitors set for adult patients, the heart rate meter shall not respond to
signals having a QRS amplitude of 0.15 mV or less, or a duration of 10 ms or less with
an amplitude of 1 mV. Response to either or both of these types of signals is permitted
in monitors set for neonatal/pediatric patients.
15.9.15 Line frequency voltage tolerance
The maximum line frequency peak-to-valley sinusoidal voltage amplitude that can be
superimposed on a series of QRS signals without exceeding the error limits of ±10%
for indicated heart rate accuracy shall be no less than 100 µV p-v. The QRS signal
shall have an amplitude of 0.5 mV, a duration of 100 ms, and a repetition rate of
80 bpm.
15.9.16 Drift tolerance
The monitor shall indicate the heart rate within the error limits of 80bpm ± 8bpm when a
0.1 Hz triangular wave of 4 mV p-v amplitude is superimposed on a train of QRS
signals of 0.5 mV amplitude, 100 ms duration, and 80 bpm repetition rate.
15.9.17 Baseline stability
Reset: reset recovery time is not greater than 3s;
Baseline Stability: After boot, 10s baseline drift in the output rate should not exceed
10µV / s RTI;
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 73
After boot, 1h, total drift should not exceed 500µV / s RTI;
Working temperature should not exceed 50µV / °C
15.9.18 System noise
No more than 30µV (p-v RTI)
15.9.19 Multi-channel crosstalk
Any input signal limited in amplitude and rate of change as per 14.7.12, applied to any
one lead of a multi-channel monitor, and with all unused inputs connected to patient
reference through a 51 kilohm resistor in parallel with a 47 nF capacitor, shall not
produce an unwanted output greater than 5% of the applied signals (multiplied by the
gain) in those channels where no signal is applied.
15.9.20 Electrosurgery interference suppression
The heart rate shall not change by more than ±10 percent of the rate before
electrosurgical interference was activated while the interference is applied for less than
10s.
15.9.21 Pace pulse display capabilities
An indication of the pacemaker pulse shall be visible on the display with an amplitude
of no less than 0.2 mV RTI.
15.9.22 Heart rate response time
The maximum response time is less than 10 s, for step change of heart rate from
80bpm to 120bpm;
The maximum response time is less than 10 s , for step change of heart rate from
80bpm to 40bpm;
15.9.23 Baseline Recovery
< 3 s after defibrillation.
15.9.24 Signal Range
± 8 mV p-p
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 74
15.9.25 Calibration Signal
1 mV p-p, ± 5% accuracy
15.10 Respiration
15.10.1 Method
Impedance between RA-LL
15.10.2 Respiration Impedance Range
0.3-3Ω
15.10.3 Base Impedance Range
200Ω-4000Ω
15.10.4 Bandwidth
0.3 - 2.5 Hz
15.10.5 Gain
x0.25, x0.500, x1, x2, x4
15.10.6 Respiration Rate
Measurement Range
Adult 0 - 120 BrPM
Neonatal / Pediatric 0 - 150 BrPM
Resolution 1 BrPM
Accuracy 0-6 BrPM: unspecified
7-150 BrPM: ±2 BrPM
15.10.7 Apnea Alarm
10 - 40 s
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 75
15.11 NIBP
15.11.1 Method
Oscillometry
15.11.2 Measure mode
Manual, Auto, STAT
15.11.3 Measure Interval in AUTO Mode
1, 2, 3, 4, 5, 10, 15, 30, 60, 90, 120, 180, 240, 480 min
15.11.4 Measure Period in STAT Mode
5 min
15.11.5 Pulse Rate Range
40 - 240 bpm
15.11.6 Measure and Alarm Range
Adult Mode
SYS 40 - 280 mmHg
DIA 10 - 220 mmHg
MEAN 20 - 240 mmHg
Pediatric Mode
SYS 40 - 220 mmHg
DIA 10 - 160 mmHg
MEAN 20 - 170 mmHg
Neonatal Mode
SYS 40 - 135 mmHg
DIA 10 - 100 mmHg
MEAN 20 - 110 mmHg
15.11.7 Static pressure accuracy
±3mmHg
15.11.8 Resolution
1mmHg
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 76
15.11.9 Accuracy
Maximum Mean error ±5mmHg
Maximum Standard deviation 8mmHg
15.11.10 Overpressure Protection
Adult 300 mmHg
Pediatric 240 mmHg
Neonatal 150 mmHg
15.12 SpO2
15.12.1 Measurement Range
0 - 100 %
15.12.2 Resolution
1%
15.12.3 Accuracy
70% - 100% ±2 %
<69% unspecified
15.12.4 Pulse Rate
Measure and Alarm Range 20-250bpm
Resolution 1bpm
Accuracy 3bpm
15.13 Temperature
Channel 2
Measure and Alarm Range 0 - 50°C
Resolution 0.1°C
Accuracy (no sensor) ± 0.1°C (0°C – 50°C)
15.14 Recorder (optional – only SCALIS 12 + 15)
Paper width 48 mm
Speed 25/50 mm/s
Wave channel 3 channels
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 77
15.15 Accessories List
Type Supplier
NIBP Cuff Y000T1 Shenzhen Med-link electronic co., Ltd.
ECG cable 3 meter Shenzhen Med-link electronic co., Ltd.
SpO2 Sensor S0044B-S Shenzhen Med-link electronic co., Ltd.
Temp Sensor W0001A Shenzhen Med-link electronic co., Ltd.
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 78
Chapter 16. Warranty
Warranty declaration by HEYER Medical AG
In addition to the legal warranty acc. to HBG §377, HEYER MEDICAL AG shall grant a
warranty of 12 months for the purchase of a new apparatus from the HEYER product
range. The warranty period begins with the date of invoice and is subject to the
following conditions:
1. Within the warranty period we will remedy free of charge any defects or damages on the device
that are shown to be caused by a manufacturing or material error. The warranty does not include
easily breakable parts, e.g. glass or consumable parts.
2. Warranty services can only be claimed upon submission of a delivery note (bill of delivery or
invoice); the type and method of damage remedy (repair or replacement) shall be at the
discretion of HEYER MEDICAL AG. Warranty services do not result in an extension of the
warranty period, nor do they entail a new warranty being granted. There is no independent
warranty period for installed spare parts.
3. Excluded from the warranty are: Damages caused by improper use, operating errors, mechanical
stress or non-observance of the operating instructions, as well as damages caused by force
majeure or by extraordinary environmental conditions.
4. Warranty services may only be claimed if proof is submitted to confirm that all service and
maintenance work has been carried out by authorized staff.
5. The warranty includes all faults that impair a faultless functioning of the device on the basis of
technical defects of individual components. The warranty obligation can only be recognized by us
if the device has been used properly and according to its intended use and no repair attempts
have been undertaken by the client himself or by third parties. The warranty claim does not
include faults caused by mechanical damages or if the device is being operated with accessories
originating from third parties.
6. The warranty is also void if changes, alterations or repairs are made to the device by persons not
authorized to do this.
7. The warranty claim only applies to customers of HEYER MEDICAL AG; it cannot be transferred to
third parties.
8. The rejected device is to be shipped back to our plant postage free. In case of a request by our
customer service department, the costs for shipping to the plant are in general to be initially borne
by the customer. After successful repair, we will send the device back freight collect. If HEYER
MEDICAL AG confirms the existence of a warranty claim, the customer will receive
reimbursement for the costs of delivery and/or transport of the apparatus. Repair parts that do not
fall under the warranty claim will be billed by us. The shipping of the device to us always counts
as a complete assignment to eliminate all faults and/or replace missing parts, unless the
customer expressly excludes partial services. Additional claims to transfer or reduce and replace
damages of any kind in particular also of damages not incurred on the object of delivery itself are
excluded.
Our service address: HEYER Medical AG
Carl-Heyer-Straße 1-3
D-56130 Bad Ems - Germany
Tel.: (02603)791-3
Fax: (02603)70 424
Subject to technical changes!
Rev. no.: 1.0 of 01.2013
HEYER Scalis – Patient Monitor – Operation Manual Rev. 1.1 79
Carl-Heyer-Str. 1/3
D-56130 Bad Ems - Germany
Phone: +49 (0) 2603 / 791-3
Fax: +49 (0) 2603 / 70424
E-mail: info@HeyerMedical.de
www.HeyerMedical.de
Das könnte Ihnen auch gefallen
- HEYER Scalis - Product List Spare Parts - en 0914Dokument2 SeitenHEYER Scalis - Product List Spare Parts - en 0914kalandorka92Noch keine Bewertungen
- HEYER Vizor - Standard Scope of Delivery 052014Dokument1 SeiteHEYER Vizor - Standard Scope of Delivery 052014kalandorka92Noch keine Bewertungen
- HEYER Scalis M - Product List - 1015Dokument2 SeitenHEYER Scalis M - Product List - 1015kalandorka92Noch keine Bewertungen
- HEYER VizOR - Product List - en 0314 2Dokument7 SeitenHEYER VizOR - Product List - en 0314 2kalandorka92Noch keine Bewertungen
- HEYER Scalis - Product List - en 0314 2Dokument4 SeitenHEYER Scalis - Product List - en 0314 2kalandorka92Noch keine Bewertungen
- HEYER Scalis M - Product List Spare Parts - en 0914Dokument2 SeitenHEYER Scalis M - Product List Spare Parts - en 0914kalandorka92Noch keine Bewertungen
- HEYER VizOR - Product List - 1015Dokument7 SeitenHEYER VizOR - Product List - 1015kalandorka92Noch keine Bewertungen
- HEYER Scalis M - Operation Manual 1.0 en 1112Dokument138 SeitenHEYER Scalis M - Operation Manual 1.0 en 1112kalandorka92Noch keine Bewertungen
- Heyer Vizor 15 - Manual 1.0 enDokument88 SeitenHeyer Vizor 15 - Manual 1.0 enkalandorka92100% (1)
- HEYER VizOR 6 - Manual 1.0 EN PDFDokument128 SeitenHEYER VizOR 6 - Manual 1.0 EN PDFkalandorka92Noch keine Bewertungen
- HEYER Scalis M - Standard Scope of Delivery 052014Dokument1 SeiteHEYER Scalis M - Standard Scope of Delivery 052014kalandorka92Noch keine Bewertungen
- Heyer Vizor - Sales - 022012Dokument10 SeitenHeyer Vizor - Sales - 022012kalandorka92Noch keine Bewertungen
- HEYER Scalis - Standard Scope of Delivery 052014Dokument1 SeiteHEYER Scalis - Standard Scope of Delivery 052014kalandorka92Noch keine Bewertungen
- HEYER Medical AG - Monitoring Sales PresentationDokument10 SeitenHEYER Medical AG - Monitoring Sales Presentationkalandorka92Noch keine Bewertungen
- HEYER VizOR 6 - Manual 1.0 EN PDFDokument128 SeitenHEYER VizOR 6 - Manual 1.0 EN PDFkalandorka92Noch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Rehabilitation Exercises To Induce Balanced Scapular Muscle Activity in An Anti-Gravity PostureDokument4 SeitenRehabilitation Exercises To Induce Balanced Scapular Muscle Activity in An Anti-Gravity PostureSAMNoch keine Bewertungen
- Ocular LithiasisDokument2 SeitenOcular LithiasisMiranti Dwi HartantiNoch keine Bewertungen
- Caustinerf Deciduous Bahan Devital Desidui PDFDokument1 SeiteCaustinerf Deciduous Bahan Devital Desidui PDFNuri AugustiniNoch keine Bewertungen
- Toacs Surgical Trainees 2009 ADokument15 SeitenToacs Surgical Trainees 2009 AAnonymous bzHRfZzv100% (1)
- Where To Turn Sept 2009 - Complete DirectoryDokument326 SeitenWhere To Turn Sept 2009 - Complete DirectoryinfolineNoch keine Bewertungen
- CAMERON Current Surgical Therapy, Thirteenth EditionDokument1.667 SeitenCAMERON Current Surgical Therapy, Thirteenth Editionniberev100% (2)
- Kee: Pharmacology, 6th Edition: Test Bank Chapter 4: Medications and Calculations Short AnswerDokument39 SeitenKee: Pharmacology, 6th Edition: Test Bank Chapter 4: Medications and Calculations Short Answerthu_vu_2983% (6)
- Ahuja Phase 2 Fact SheetDokument2 SeitenAhuja Phase 2 Fact SheetWKYC.comNoch keine Bewertungen
- Clusivol DropsDokument3 SeitenClusivol DropsShermina Maruji PuttoNoch keine Bewertungen
- Master ListDokument100 SeitenMaster ListAris GonzalesNoch keine Bewertungen
- WMC Abbtt MbbsDokument8 SeitenWMC Abbtt MbbsMIR JALALNoch keine Bewertungen
- Formula FeedsDokument35 SeitenFormula FeedsrandoNoch keine Bewertungen
- Achilles Tendon ProtocolDokument6 SeitenAchilles Tendon Protocolomad pendaftaranPPDSNoch keine Bewertungen
- LorazepamDokument14 SeitenLorazepamJuan PerezNoch keine Bewertungen
- NCM 118Dokument5 SeitenNCM 118lalaine nadulpitNoch keine Bewertungen
- Impetigo in NeonatusDokument5 SeitenImpetigo in Neonatusasep budiyantoNoch keine Bewertungen
- Glenn - Urologic Surgery 5th EdDokument648 SeitenGlenn - Urologic Surgery 5th EdCristina Giurgiu100% (2)
- DVT Care PlanDokument13 SeitenDVT Care Planafeather8490100% (2)
- A Shade Selection TechniqueDokument4 SeitenA Shade Selection TechniqueKirti JajooNoch keine Bewertungen
- Practice Manager ResumeDokument2 SeitenPractice Manager Resumevictorryancastro95Noch keine Bewertungen
- Copyofuntitleddocument 1Dokument7 SeitenCopyofuntitleddocument 1api-352688085Noch keine Bewertungen
- Psicosis Atípica MitsudaDokument6 SeitenPsicosis Atípica MitsudaRoberth SanchezNoch keine Bewertungen
- l4 Clinical Intensive I Summative Evaluation 1Dokument6 Seitenl4 Clinical Intensive I Summative Evaluation 1api-396278555Noch keine Bewertungen
- Two Flap Palatoplasty Vanderbilt Cleft Care Meeting GC AllenDokument17 SeitenTwo Flap Palatoplasty Vanderbilt Cleft Care Meeting GC AllenkaarlaamendezNoch keine Bewertungen
- Luka Bakar Poster PDFDokument1 SeiteLuka Bakar Poster PDFnurisumirizqiNoch keine Bewertungen
- Tracheoesophageal FistulaDokument6 SeitenTracheoesophageal FistulaPankaj SinghNoch keine Bewertungen
- A Class I Incisor Relationship Is Defined by The British Standards Incisor Classification As FollowsDokument2 SeitenA Class I Incisor Relationship Is Defined by The British Standards Incisor Classification As Followsغسن سمن المدنNoch keine Bewertungen
- The Exorcist 2ooo: Dialogue ListDokument73 SeitenThe Exorcist 2ooo: Dialogue ListJunior TribbianiNoch keine Bewertungen
- Obladen 2010Dokument7 SeitenObladen 2010Barna ÉvaNoch keine Bewertungen
- Collet Gps DNP FNP Copy With Grades Blacked OutDokument4 SeitenCollet Gps DNP FNP Copy With Grades Blacked Outapi-251653314Noch keine Bewertungen