Beruflich Dokumente
Kultur Dokumente
Diuretic Agents Carbonic Anhydrase Inhibitors
Hochgeladen von
Amanda0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
18 Ansichten5 SeitenThis document summarizes different classes of diuretic and urinary tract agents. It discusses carbonic anhydrase inhibitors, potassium-sparing diuretics, and osmotic diuretics as mild diuretics that work through different mechanisms. It also covers urinary tract anti-infectives like fosfomycin and nitrofurantoin that treat UTIs, as well as urinary tract antispasmodics like trospium and mirabegron that relieve spasms by blocking parasympathetic activity. Each drug class is described in terms of indications, pharmacokinetics, contraindications, adverse effects, and important drug interactions.
Originalbeschreibung:
pharmacology, drugs, pharma, renal system
Originaltitel
Pharma Summary
Copyright
© © All Rights Reserved
Verfügbare Formate
ODT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenThis document summarizes different classes of diuretic and urinary tract agents. It discusses carbonic anhydrase inhibitors, potassium-sparing diuretics, and osmotic diuretics as mild diuretics that work through different mechanisms. It also covers urinary tract anti-infectives like fosfomycin and nitrofurantoin that treat UTIs, as well as urinary tract antispasmodics like trospium and mirabegron that relieve spasms by blocking parasympathetic activity. Each drug class is described in terms of indications, pharmacokinetics, contraindications, adverse effects, and important drug interactions.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als ODT, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
18 Ansichten5 SeitenDiuretic Agents Carbonic Anhydrase Inhibitors
Hochgeladen von
AmandaThis document summarizes different classes of diuretic and urinary tract agents. It discusses carbonic anhydrase inhibitors, potassium-sparing diuretics, and osmotic diuretics as mild diuretics that work through different mechanisms. It also covers urinary tract anti-infectives like fosfomycin and nitrofurantoin that treat UTIs, as well as urinary tract antispasmodics like trospium and mirabegron that relieve spasms by blocking parasympathetic activity. Each drug class is described in terms of indications, pharmacokinetics, contraindications, adverse effects, and important drug interactions.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als ODT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 5
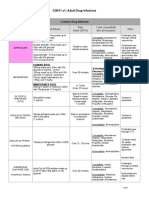
Diuretic Agents
Carbonic Anhydrase Inhibitors
✔ relatively mild diuretics
✔ agents include acetazolamide (Diamox) and methazolamide (generic)
A) Therapeutic Actions and Indications
• enzyme carbonic anhydrase is a catalyst for formation of sodium bicarbonate, which is
stored as the alkaline reserve in the renal tubule, and for the excretion of hydrogen, which
results in slightly acidic urine
• diuretics that block the effects of carbonic anhydrase slow down the movement of hydrogen
ions resulting in more sodium and bicarbonate loss in urine
B) Pharmacokinetics
• these drugs are rapidly absorbed and widely distributed
• acetazolamide is available orally and for IV use
• they peak in 2-4 hours and 6-12 hour duration
• excreted in urine
• some agents are associated with fetal abnormalities therefore should not be used during
pregnancy
C) Contraindications and Cautions
• contraindicated in px with allergy to drugs or to antibacterial sulfonamides or thiazides, or
in px with chronic noncongestive angle-closur glaucoma
• routine use during pregnancy is inappropriate
• caution in px who have fluid or electrolyte imbalances, renal or hepatic disease,
adrenocortical insufficiency, respiratory acidosis, or COPD
D) Adverse Effects
• disturbances in acid-base and electrolyte balances
• metabolic acidosis is a relatively common and potentially dangerous effect that occurs when
bicarbonate is lost
• hypokalemia is also common
• px also complain of paresthesias of extremities, confusion, and drowsiness
E) Clinically Important Drug-Drug Interaction
• increased excretion of salicylates and lithium if they are combined with these drugs
Potassium-Sparing Diuretics
✔ not as powerful as loop diuretics, but retains K instead of wasting them
✔ drugs include amiloride (Midamor), spironolactone (Aldactone), and triamterene (Dyrenium)
A) Therapeutic Actions and Indications
• cause loss of sodium while promoting the retention of K
• spironolactone acts as an aldosterone antagonist, blocking the actions of aldosterone in
distal tubule
• amiloride and triamterene block K secretion through the tubule
• the diuretic effect of these drugs comes from the balance achieved in losing sodium to offet
the K retained
B) Pharmacokinetics
• well absorbed after oral administration, protein bound and widely distributed
• metabolized in liver and excreted in urine
C) Contraindications and Cautions
• contraindicated for use in px with allergy to the drug, and hyperkalemia, renal diseas, or
anuria
• routine use during pregnncy is not appropriate
D) Adverse Effects
• most common: hyperkalemia, which can cause lethargy, confusion, ataxia, muscle cramps,
and cardiac arrhytmias
• px should be evaluated regularly for signs of increased potassium
• hirsutism, gynecomastia, deepening of voice, and irregular menses
E) Clinically Important Drug-Drug Interaction
• diuretic effect decreases if ptassium-sparing diuretics are combined with salicylates
Osmotic Diuretics
✔ pull water into the renal tubule without sodium loss
✔ only available is mannitol (Osmitrol)
A) Therapeutic Actions and Indications
• some nonelectrolytes are used IV to increase the volume of fluid produced by the kidneys
• mannitol is a sugar that is not well absorbed by the tubules; it acts to pull large amounts of
fluid into urine due to osmotic pull exerted by the large sugar molecule
• because the tubules is not able to reabsorb all of the sugar pulled into it, large amount of
fluid are lost in the urine
B) Pharmacokinetics
• only available for IV use
• freely filtered at the renal glomerulus, poorly reabsorbed by the renal tubule, not secreted by
the tubule, and resistant to metabolism
• action depends on concentration of osmotic activity in the solution
• not known if it causes fetal harm
C) Contraindications and Cautions
• contraindicated in px with renal disease and anuria from severe renal disease, pulmonary
congestion, intracranial bleeding, dehydration, and HF
• routine use for pregnancy is not appropriate
D) Adverse Effects
• most common: sudden drop in fluid levels
• nausea, vomiting, hypotension, light-headedness, confusion, and headache can be
accompanied by cardiac decompensation and even shock
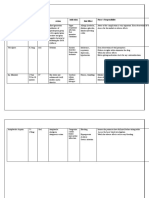
Drugs Affecting the Urinary Tract and Bladder
Conditions affecting the Urinary Tract and Bladder
• UTI
• bladder spasm
• bladder pain
• benign prostatic hyperplasia
Urinary Tract Anti-Infectives
✔ has two types
1. The antibiotics which particularly effective against the gram negative bacteria that cause the
most UTIs. These include fosfomycin (Monurol), and nitrofurantoin (Furadantin).
2. The other types works to acidify the urine, killing bacteria that might be in the bladder. This
includes methenamine (Hiprex) and methylene blue (Urolene Blue).
A) Therapeutic Actions and Indications
• act specifically within the urinary tract to destroy bacteria, either through direct antibiotic
effect (drugs interfere with reproduction of gram negative bacteria and cause bacterial cell
death) or through acidification of urine (produce an environment that is not conducive to
bacterial survival, leading to bacterial cell death)
• they are used to treat chronic UTIs, as adjunctive therapy in acute cystitis and
pyelonephritis, and as prophylaxis with urinary tract anatomical abnormalities and residual
urine disorders
B) Pharmacokinetics
• Fosfomycin – taken orally, one-time dose, not recommended for children under 18, rapidly
absorbed, undergoes slow hepatic metabolism, excreted in urine and feces, drug of choice
for cystitis during pregnancy or lactation
• Nitrofurantoin – old drug, very short half-life (20-60mins), not as effective as new ones,
successfully used for suppression therapy for children and adults with chronic UTIs, well
absorbed orally, metabolized in liver, and excreted in urine
• Methenamine – taken orally, well absorbed, metabolized in liver, excreted in urine
• Methylene blue – well absorbed orally, widely distributed, metabolized in tissues, and
excreted in urine, bile, and feces
C) Contraindications and Cautions
• contraindicated in presence of any known allergy to any of these drugs to prevent
hypersensitivity reactions
• should be used with caution in the presence of renal dysfuntion, pregnancy and lactation
D) Adverse Effects
• nausea, vomiting, diarrhea, anorexia, bladder irritation, and dysuria
• infrequent symptoms include pruritus, urticaria, headache, dizziness, nervousness, and
confusion
E) Clinically Important Drug-Drug Interaction
• consult a nursing drug guide for specific interactions since these drugs are from several
different chemical classes
Urinary Tract Antispasmodics
✔ they block the spasm of urinary tract muscles caused by various conditions
A) Therapeutic Actions and Indications
• the urinary tract antispasmodics relieve the spasms by blocking parasympathetic activity,
thus suppressing overactivity, which leads to relaxation of the detrusor and other urinary
tract muscles
• because parasympathetic system uses acetylcholine to cause its effects, these drugs are
called anticholinergic drugs
• Trospium – specifically blocks muscarinic receptors and reduces the muscle tone of bladder,
specifically indicated for treatment of overactive bladder with symptoms of urinary
incontinence, urgency, and urinary frequency
• Mirabegron – treats overactive bladder, beta-agonist and stimulates sympathetic nerves in
bladder which leads to detrudor muscle relaxation
B) Pharmacokinetics
• all agents are administered orally except oxybutynin (orally, dermal patch, topical gel)
• rapidly absorbed, slow onset of action (6-12hrs), metabolized in liver, excreted in urine
• Oxybutynin when given transermally lasts 96 hours
C) Contraindications and Cautions
• contraindicated in presence of any known allergy to any of these drugs, with pyloric or
duodenal obstruction or recent surgery, with obstructive urinary tract problems, and with
glaucoma, myasthenia gravis or acute haemorrhage
• caution in patients with acute renal or hepatic dysfuntion, and in pregnantand lactating
mothers
• Mirabegron must be used with caution in presence of hypertension
D) Adverse Effects
• nausea, vomiting, dry mouth, nervousness, tachycardia, and vision changes
• Flaxovate – associated with CNS effects
• Oxybutynin – has anticholinergic effects
• Mirabregon – stimulates sympathetic system and may cause hypertension and urinary
retention
E) Clinically Important Drug-Drug Interaction
• Oxybutynin + phenothiazines and haloperidol = decreased effectiveness
• Darifenacin or fesoterodine + antifungals or antiviral agents = toxic effects
• Solifenacin + antihistamines or antipsychotics = risk of increased QT intervals and serious
cardiac arrythmias
• Solifenacin + ketoconazole or other cytochrome P-450 (CYP) 3A4 inhibitors = risk of
increased serum levels and toxic effects
• Tolterodine + CYP2D6 inhibitors = increased toxicity
• Trospium can interfere with excretion of drugs by tubular secretion, leading to increased
serum levels f those drugs
• Mirabegron should not be combined with drugs that are metabolized by CYP2D6 system as
it inhibits that system
Other Drugs Affecting the Urinary Tract and Bladder
✔ Urinary Tract Analgesics – a dye used to decrease pain
A) Therapeutic Actions and Indications
• Phenazopyridine exerts a direct, topical analgesic effect on the urinary tract mucosa
• it is used to relieve symptoms related to urinary tract irritation from infection, surgery,
or trauma
B) Pharmacokinetics
• Phenazopyridine – available for oral use, rapid onset of action, widely distributed,
crossing placenta and entering breastmilk, metabolized in liver, and excreted in urine
C) Contraindications and Cautions
• contraindicated in presence of known allergy to drug, and with serious renal dysfuntion
• should be avoided during pregnancy and lactation
D) Adverse Effects
• GI upset, headache, rash, and reddish-orange coloring of urine
• potential for renal or hepatic toxicity
• using drugs for longer than 2 days increases risk of toxic effects
E) Clinically Important Drug-Drug Interaction
• risk of toxic effects increases when combined with antibacterial agents
✔ Bladder Protectant – used to coat or adhere to bladder mucosal wall to prevent irritation
A) Therapeutic Actions and Indications
• has anticoagulant and fibrinolytic effects
• the drug adheres to the bladder wall to act a buffer to control cell permeability,
preventing irritating solutes in urine from reaching the bladder wall cells
• used specifically to decrease pain and discomfort
B) Pharmacokinetics
• administered orally and only 3% is absorbed
• distributed to GI tract, liver, spleen, kin, bone marrow, and periosteum
• undergoes metabolism in liver and spleen and is excreted in urine
• has a half-life of 4.8 hours
C) Contraindications and Cautions
• should not be used with any condition that involved increased risk of bleeding
• contraindicated in presence of a history of heparin-induced thrombocytopenia
• caution in patients with hepatic or splenic dysfunction
D) Adverse Effects
• bleeding that may progress to hemorrhage, headache, alopecia, and GI disturbances
E) Clinically Important Drug-Drug Interaction
• potential of increased bleeding risks if combined with anticoagulants, aspirin, or
nonsteroidal anti-inflammatory drugs
Drugs for Treating Benign Prostatic Hyperplasia
✔ also called benign prostatic hypertrophy or enlarged prostate
✔ common problem in men and increases in incidence with age
✔ the prostate completely encircles the urethra
✔ two types of drugs are used to relieve the symptoms of BPH: the alpha-adrenergic blockers
doxazosin (Cardura), tamsulosin (Flomax), alfuzosin (Uroxatral), silodosin (Rapaflo), and
terazosin (generic) and drugs that block testosterone production like finasteride (Proscar) and
dutasteride (Avodart)
A) Therapeutic Actions and Indications
• prostate enlargement must be benign and not caused by cancer, infection, stricture, or
hypotonic bladder
• patients receiving long-term therapy must be reassessed periodically
• alpha-adrenergic blockers block postsynaptic alpha-adrenergic receptors, which results in a
dilation of arterioles and veins and a relaxation of sympathetic effects of bladder and urinary
tract
• drugs that block testosterone production inhibit the intracellular enzyme that converts
testosterone to potent androgen dihydrotes-testosterone, which the proostate gland depends
for its development and maintenance
B) Pharmacokinetics
• alpha, selective adrenergic blocking agents are well absorbed after oral administration,
reaching peak levels in 2-8 hours and undergo extensive hepatic metabolism
• excreted in urine
• finasteride and dutasteride are rapidly absorbed from GI tract after oral administration,
undergo hepatic metabolism, and are excreted in feces and urine
C) Contraindications and Cautions
• contraindicated in patient who are allergic to drugs
• caution should be used in patients with hepatic or renal dysfunction
• adrenergc blockers should be used with caution in px with heart failure or known coronary
disease
• finasteride and dutasteride have no inications for women and are rated pregnancy X
• women must not touch finasteride or dutasteride tablets
D) Adverse Effects
• headache, fatigue, diziness, postural diziness, lethargy, tachycardia, hypotension, GI upset,
and sexul dysfuntion
• finasteride and dutasteride are associated with decreased libido,impotence, an sexual
dysfunction
• px using finasteride or dutasteride can’t donate blood for 6months after last dose
E) Clinically Important Drug-Drug Interaction
• alpha-adrenergic blockers + antihypertensives, nitrates, or erectile dysfunction drugs =
increased antihypertensive effects
Das könnte Ihnen auch gefallen
- PDF Module 10 Urinary System DrugsDokument7 SeitenPDF Module 10 Urinary System DrugsAJ VitangculNoch keine Bewertungen
- Lec (10) Word G I TDokument9 SeitenLec (10) Word G I TAhmed EngNoch keine Bewertungen
- Drugs Acting On G I System: Mr. Dipti SorteDokument65 SeitenDrugs Acting On G I System: Mr. Dipti Sortesandeepv08Noch keine Bewertungen
- GI DrugsDokument35 SeitenGI DrugsIconMaicoNoch keine Bewertungen
- Pharmacology of The GIT System: CIC Ragasa, RN-MDDokument70 SeitenPharmacology of The GIT System: CIC Ragasa, RN-MDCarmencita Ileen Ragasa - AhmedNoch keine Bewertungen
- GI DrugsDokument79 SeitenGI DrugsreecoleNoch keine Bewertungen
- Drugs Affecting The Gi Tract: Myla M - Guadiz, R.N., M.A.NDokument37 SeitenDrugs Affecting The Gi Tract: Myla M - Guadiz, R.N., M.A.NRachel CabiguenNoch keine Bewertungen
- Drugs Used in The Treatment of Gastrointestinal DiseasesDokument52 SeitenDrugs Used in The Treatment of Gastrointestinal DiseasesWidia Isa Aprillia SujanaNoch keine Bewertungen
- Gastrointestinal Agents & Antiulcer Drugs: MedanDokument56 SeitenGastrointestinal Agents & Antiulcer Drugs: MedanSartika NapitupuluNoch keine Bewertungen
- Parathyroid AgentsDokument36 SeitenParathyroid AgentsGlaiza Joves EncarnacionNoch keine Bewertungen
- Drugs For Diarrhea and ConstipationDokument24 SeitenDrugs For Diarrhea and ConstipationFaddi BoyNoch keine Bewertungen
- Drugs Acting On The Intestinal Tract1Dokument53 SeitenDrugs Acting On The Intestinal Tract1Isheanesu MugwisiNoch keine Bewertungen
- 15th November 2016 - Phar01 - Drugs For The Gastrointestinal SystemDokument47 Seiten15th November 2016 - Phar01 - Drugs For The Gastrointestinal SystemRjDNoch keine Bewertungen
- Lec 2 - GIT DrugsDokument68 SeitenLec 2 - GIT DrugsAiqa QaziNoch keine Bewertungen
- Gastrointestinal Tract DisordersDokument4 SeitenGastrointestinal Tract DisordersCarissa Mae Tapec EstradaNoch keine Bewertungen
- Drugs For Constipation, AntiEmetics and Emetics Daniel Chans AUG 2022Dokument80 SeitenDrugs For Constipation, AntiEmetics and Emetics Daniel Chans AUG 2022kerenpatience7Noch keine Bewertungen
- Peptic Ulcer Sec4Dokument12 SeitenPeptic Ulcer Sec4Roro RageyNoch keine Bewertungen
- Anti DiarrheaDokument40 SeitenAnti DiarrheaNofilia Citra CandraNoch keine Bewertungen
- Parathyroid AgentsDokument33 SeitenParathyroid AgentsFaith madayagNoch keine Bewertungen
- Urinary Tract Antiseptics: AntimicrobialDokument13 SeitenUrinary Tract Antiseptics: AntimicrobialZaim Ul Hassan ZaimNoch keine Bewertungen
- Pharma Review FinalsDokument31 SeitenPharma Review FinalsLanz Andrei MatociñosNoch keine Bewertungen
- Medications Used in DiarrhoeaDokument25 SeitenMedications Used in Diarrhoeagitama9904Noch keine Bewertungen
- Drugs Acting On GitDokument119 SeitenDrugs Acting On GitNathaniel Mbiu Tim100% (1)
- Pharmacology of GITDokument29 SeitenPharmacology of GITMohammed Bahnasy100% (1)
- Drugs Used in Gastrointestinal TractDokument111 SeitenDrugs Used in Gastrointestinal TractIsaacNoch keine Bewertungen
- Pharmagout 190907102528Dokument42 SeitenPharmagout 190907102528AugustinoNoch keine Bewertungen
- Printed Material Module 7 Gastrointestinal System Drugs - PDFDokument45 SeitenPrinted Material Module 7 Gastrointestinal System Drugs - PDFShang MacarayonNoch keine Bewertungen
- Gastrointestinal DrugsDokument45 SeitenGastrointestinal DrugsCindy MaslagNoch keine Bewertungen
- Food-Drug InteractionsDokument67 SeitenFood-Drug InteractionsMadeleine Mourad RouchdyNoch keine Bewertungen
- Interaksi ObatDokument83 SeitenInteraksi ObatGeronimouzt LoverzNoch keine Bewertungen
- Gastrointestinal Medicines MBCHB II - 2023 NdlovuDokument31 SeitenGastrointestinal Medicines MBCHB II - 2023 NdlovuKeamogetswe Zwane100% (1)
- Nichols GI 09Dokument59 SeitenNichols GI 09marviecute22Noch keine Bewertungen
- Esomeprazole MagnesiumDokument3 SeitenEsomeprazole Magnesiumapi-3797941100% (1)
- Drugs Affecting Gastrointestinal (GI) Secretions: CUIZON, Ariel GONZALES, Claire Marie PLAZA, GabrielDokument29 SeitenDrugs Affecting Gastrointestinal (GI) Secretions: CUIZON, Ariel GONZALES, Claire Marie PLAZA, GabrielKay GonzalesNoch keine Bewertungen
- Drug Therapy For GI Disorders PDFDokument5 SeitenDrug Therapy For GI Disorders PDFmeeraNoch keine Bewertungen
- Drugs Act On Hyper AcidityDokument33 SeitenDrugs Act On Hyper AcidityAzifah IbrahimNoch keine Bewertungen
- Antidiarrhoeals and Laxatives PDFDokument34 SeitenAntidiarrhoeals and Laxatives PDFKumar SaurabhNoch keine Bewertungen
- Lecture 21 Drugs Against GI DisordersDokument40 SeitenLecture 21 Drugs Against GI DisordershamzabhayatNoch keine Bewertungen
- Antacids Are Used To Chemically React With and NeuDokument4 SeitenAntacids Are Used To Chemically React With and Neunipheyy dananNoch keine Bewertungen
- GastrointestinaldrugsDokument30 SeitenGastrointestinaldrugsmayaNoch keine Bewertungen
- Drugs Acting On Gastrointestinal SystemDokument41 SeitenDrugs Acting On Gastrointestinal SystemDivya JoyNoch keine Bewertungen
- W11 & W12 - Medication For Gastrointestinal SystemDokument18 SeitenW11 & W12 - Medication For Gastrointestinal SystemAkari ChanNoch keine Bewertungen
- DiureticsDokument42 SeitenDiureticsKeziah TampusNoch keine Bewertungen
- ANTIEMETICSDokument26 SeitenANTIEMETICSkhurshidghorihumaNoch keine Bewertungen
- Continence Tools For Residential Aged Care: An Education GuideDokument27 SeitenContinence Tools For Residential Aged Care: An Education GuideAlfred SamuelNoch keine Bewertungen
- Antibiotik Dan Antiseptik Saluran KemihDokument14 SeitenAntibiotik Dan Antiseptik Saluran KemihPuterinugraha Wanca ApatyaNoch keine Bewertungen
- Bulk Stimulants Lubricants Other Laxatives GI StimDokument5 SeitenBulk Stimulants Lubricants Other Laxatives GI Stimrosita d. ramosNoch keine Bewertungen
- PCL 302 Lecture DiureticsDokument7 SeitenPCL 302 Lecture DiureticsZayyanu AminuNoch keine Bewertungen
- GI Tract - Nutrition/EliminationDokument51 SeitenGI Tract - Nutrition/Eliminationnick_nock08Noch keine Bewertungen
- Non Steroid Antiinflammatory Drugs & Drugs Use in The Treatment of GoutDokument28 SeitenNon Steroid Antiinflammatory Drugs & Drugs Use in The Treatment of GoutVevi VarcetyNoch keine Bewertungen
- Pharmacotherapy of DiarhheaDokument29 SeitenPharmacotherapy of DiarhheaFahril LabuduNoch keine Bewertungen
- Drugs Used in GoutDokument19 SeitenDrugs Used in GoutSamah AbboNoch keine Bewertungen
- GI Drug-I & IIDokument29 SeitenGI Drug-I & IIapi-3699361Noch keine Bewertungen
- Git PharmacologyDokument73 SeitenGit PharmacologyShehu Baba AbdullahiNoch keine Bewertungen
- Drug CardsDokument16 SeitenDrug Cardsp_dawg100% (7)
- Drugs Affecting The Renal System I. Diuretics II. Parenteral Fluids (Video) III. Electrolytes (Video)Dokument44 SeitenDrugs Affecting The Renal System I. Diuretics II. Parenteral Fluids (Video) III. Electrolytes (Video)Juliene Hannah FloresNoch keine Bewertungen
- DrugDokument36 SeitenDruggecalian100% (1)
- Drugs Used in The Treatment of Gastrointestinal Diseases - 2Dokument63 SeitenDrugs Used in The Treatment of Gastrointestinal Diseases - 2Varunavi SivakanesanNoch keine Bewertungen
- The Complete Guide to Chronic Constipation: Symptoms, Risks, Treatments & CuresVon EverandThe Complete Guide to Chronic Constipation: Symptoms, Risks, Treatments & CuresNoch keine Bewertungen
- Handbook of Drug Interaction and the Mechanism of InteractionVon EverandHandbook of Drug Interaction and the Mechanism of InteractionBewertung: 1 von 5 Sternen1/5 (1)
- Community Health NursingDokument3 SeitenCommunity Health NursingAmandaNoch keine Bewertungen
- NCM118-FNCP & LetterDokument6 SeitenNCM118-FNCP & LetterAmandaNoch keine Bewertungen
- N118 0XYGEN Checklist FinalDokument7 SeitenN118 0XYGEN Checklist FinalAmandaNoch keine Bewertungen
- Drugs Affecting The Renal SystemDokument8 SeitenDrugs Affecting The Renal SystemAmandaNoch keine Bewertungen
- Activity 2 Biochemical ProcessesDokument13 SeitenActivity 2 Biochemical ProcessesAmandaNoch keine Bewertungen
- NAPLEX Pass Rates 2016 2017 and 2018Dokument14 SeitenNAPLEX Pass Rates 2016 2017 and 2018Lorena CalderonNoch keine Bewertungen
- Nurdr Practice QuestionsDokument6 SeitenNurdr Practice QuestionsSHEENA MAE DE LOS REYESNoch keine Bewertungen
- OptumRx Prescription Reimbursement Request FormDokument3 SeitenOptumRx Prescription Reimbursement Request FormBennyNoch keine Bewertungen
- R A No 9165 Powerpoint PresentationDokument30 SeitenR A No 9165 Powerpoint Presentationmina villamorNoch keine Bewertungen
- Hyg 062Dokument5 SeitenHyg 062verneck silvaNoch keine Bewertungen
- Dispensary APTsDokument12 SeitenDispensary APTsTewodros TafereNoch keine Bewertungen
- 75 Target Controlled Infusions in Anaesthetic PracticeDokument10 Seiten75 Target Controlled Infusions in Anaesthetic PracticeadamkurniawandanaNoch keine Bewertungen
- 04 - Extravascular Administration (Oral)Dokument41 Seiten04 - Extravascular Administration (Oral)Prasanna PappuNoch keine Bewertungen
- Instructions To Author-REACH2020Dokument2 SeitenInstructions To Author-REACH2020pharma xlNoch keine Bewertungen
- Chapter 19Dokument8 SeitenChapter 19madhushaNoch keine Bewertungen
- Pharmaceutics Sem 1 SyllabusDokument3 SeitenPharmaceutics Sem 1 SyllabusHILAL AHMAD DASSNoch keine Bewertungen
- Medication AdministrationDokument586 SeitenMedication AdministrationJa DaNoch keine Bewertungen
- AntipyreticsDokument14 SeitenAntipyreticsRadianty Haengbog Daeng FrederichaNoch keine Bewertungen
- Practice Math For Nursing 333Dokument6 SeitenPractice Math For Nursing 333nicoleb777100% (1)
- May 20151Dokument17 SeitenMay 20151Hany Rasheed Mohamed50% (2)
- 2022-OXFORD-HANDBOOK-OF-ANAESTHESIA-Oxford-Press-5th-Edition ExportDokument4 Seiten2022-OXFORD-HANDBOOK-OF-ANAESTHESIA-Oxford-Press-5th-Edition ExportHany ElbarougyNoch keine Bewertungen
- OET:Writing TipsDokument2 SeitenOET:Writing Tipsfernanda1rondelliNoch keine Bewertungen
- Drug Doses Frank Shann - PDFDokument49 SeitenDrug Doses Frank Shann - PDFAgustina Permata Sari100% (1)
- Phar 1000 AssignmentDokument5 SeitenPhar 1000 AssignmentSandeep Kumar BNoch keine Bewertungen
- PCOG Questions Unit IDokument7 SeitenPCOG Questions Unit IManjusha KondepudiNoch keine Bewertungen
- Advanced Marketing Strategy: ZantacDokument6 SeitenAdvanced Marketing Strategy: ZantacAALOK SINGLANoch keine Bewertungen
- Peptide DrugDokument17 SeitenPeptide DrugNADIA INDAH FITRIA NINGRUM -100% (1)
- JP Farm As Igg 160029Dokument5 SeitenJP Farm As Igg 160029Lia Alizia HafitriNoch keine Bewertungen
- Defekta PEMDA 13 09 2021Dokument13 SeitenDefekta PEMDA 13 09 2021k24 bambukuningNoch keine Bewertungen
- CG011.v1: Adult Drug Infusions: Drug Dose and Diluent Rate (Note UNITS) Y Site Compatibility (Not All-Inclusive) OtherDokument8 SeitenCG011.v1: Adult Drug Infusions: Drug Dose and Diluent Rate (Note UNITS) Y Site Compatibility (Not All-Inclusive) OtheriqbalNoch keine Bewertungen
- Treatment For My Patient: Drug Dose Route Action Indication Side Effect Nurse's ResponsibilityDokument2 SeitenTreatment For My Patient: Drug Dose Route Action Indication Side Effect Nurse's ResponsibilityValarmathiNoch keine Bewertungen
- Common Ophthalmic DrugsDokument3 SeitenCommon Ophthalmic DrugsBadr DihamNoch keine Bewertungen
- Key Topics - Bioequivalence - 13-April-2017.ppt'Dokument36 SeitenKey Topics - Bioequivalence - 13-April-2017.ppt'Md TayfuzzamanNoch keine Bewertungen
- ETIKET BOX OBAT PATEN Box BesarDokument5 SeitenETIKET BOX OBAT PATEN Box Besarbabas basriNoch keine Bewertungen
- Pharma PrelimDokument8 SeitenPharma PrelimNom NomNoch keine Bewertungen