Beruflich Dokumente
Kultur Dokumente
DD - Ultrasound Guided
Hochgeladen von
eko donnyOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
DD - Ultrasound Guided
Hochgeladen von
eko donnyCopyright:
Verfügbare Formate
The British Journal of Radiology, 81 (2008), 154–163
PICTORIAL REVIEW
Ultrasound-guided thrombin injection of iatrogenic groin
pseudoaneurysm: Doppler features and technical tips
1 2
J M HANSON, FFRRCSI, FRCR, M ATRI, MD, FRCP(C) and 3N POWER, FRCR, MRCPI
1
Department of Rodiology, Our Lady of Lourdes Hospital, Drogheda, Co. Louth, Ireland, 2Abdominal Imaging, Princess
Margaret Hospital, 610 University Avenue, Toronto, ON M5G 2MG, Canada and 3Department of Medical Imaging, St
Bartholomew’s Hospital, West Smithfield, London ECIA 7BE, UK
ABSTRACT. The practice of angiographic procedures is increasing and, concomitantly,
there has been an increase in the incidence of iatrogenic femoral pseudoaneurysms Received 13 January 2006
(PA). Ultrasound-guided thrombin injection is becoming the accepted gold standard in Revised 16 May 2006
the treatment of PA. It is a cost-effective, safe and efficacious treatment that requires a Accepted 6 June 2006
short learning curve. The aim of this pictorial review is to demonstrate the Doppler and
DOI: 10.1259/bjr/52029321
ultrasound features used to diagnose PA and those that help differentiate it from
alternative diagnoses, and to describe the procedure of thrombin injection, ’ 2008 The British Institute of
highlighting technical tips and ways to avoid potential complications. Radiology
Pseudoaneurysms (PAs) occur after incomplete hae- immunogenic complications in the literature [8]. Another
mostasis of a punctured artery. The resulting continued consequence of bovine thrombin exposure is the potential
extravasation of blood into the subcutaneous tissues is development of antibodies to human clotting proteins and
contained within a pseudocapsule of fibrous tissue thrombin, in particular factor V, resulting in a coagulo-
within the adjacent soft tissue. PAs are becoming pathy and excessive bleeding [9]. Such complications are
increasingly prevalent with the widespread use of not seen with newer human-derived thrombin. This is
endovascular procedures. Incidence rates vary and are taken from pooled blood products and, therefore, there is
quoted between 0.05% and 4%, and as high as 16% [1]. theoretical possibility of infection from such human blood
Patients present with a range of signs and symptoms products. All of the immunogenic and infective risks can
including pain, pulsatile mass and rapidly enlarging be avoided by the autologous use of thrombin. A sufficient
mass. Some PAs are subclinical and resolve sponta- sample of thrombin can be isolated from a 50 ml sample of
neously [2], but there is always a risk of growth and a patient’s own blood in a straightforward procedure of
rupture, overlying skin necrosis, distal embolus and less than 1 h [10]. Thrombin injection has largely been used
neurological symptoms owing to compression. Although in the treatment of lower limb PA. Cases describing
it is difficult to predict spontaneous closure, low flow in aneurysms of the upper limb and mesenteric arterial tree
the aneurysm suggests potential for spontaneous closure as well as the thoracic aorta have been noted in the
[3]. Despite the surgical approach being simple, it often literature [11–14].
requires general anaesthesia. The surgical approach has In this pictorial essay, we present a brief description of
been replaced in the last two decades by compression the US-guided compression procedure, emphasizing the
under US guidance. This treatment is often a lengthy role of Doppler ultrasound in the diagnosis and
procedure and may fail because of patient discomfort, treatment of iatrogenic PA of the groin.
patient obesity and anticoagulation. Success rates for
compression of PA range from 30% to 62% for patients
on anticoagulation and from 74% to 95% when not on Diagnosis of pseudoaneurysm using
anticoagulation [4, 5]. The larger the PA, the less likely ultrasound
compression will be efficacious.
The diagnosis of a PA is based on a triad of ultrasound
Operators have shown success with thrombin injection
findings:
of PA. The reported success rates range from 90% to 100%
[1, 6]. Complications are rare. In one literature review, (1) a hypoechoic sac in the vicinity of the parent vessel;
3/319 complications have been documented [7]. These (2) swirling high resistance flow on Doppler ultra-
were all thrombotic complications, which required surgi- sound within this mass;
cal repair in one case. Bovine thrombin is highly (3) ‘‘to and fro’’ type waveform in the neck or in the
immunogenic. There are case reports describing the sac close to the neck (Figure 1).
This waveform may be dampened in the periphery of
Address correspondence to: Dr John M Hanson, Consultant
Radiologist, Medical Imaging, Our Lady of Lourdes Hospital, larger PA sacs, where it may be confused with that of a
Drogheda, Co. Louth, Louth, Ireland. E-mail: maryjohnny@ venous waveform [15]. The ‘‘to and fro’’ flow pattern is
eircom.net synchronous with the cardiac cycle.
154 The British Journal of Radiology, February 2008
Pictorial review: Ultrasound-guided thrombin injection of iatrogenic groin pseudoaneurysm
(a) (b) (c)
Figure 1. Typical example of a pseudoaneurysm. In (a), transverse view, there is a short-necked pseudoaneurysm (PA) with spiral
flow within the aneurysm sac (arrowheads). The high-resistance flow pattern is demonstrated in (b). In (c), a post-thrombin
injection image, the PA is thrombosed and the cavity is now echogenic (arrows).
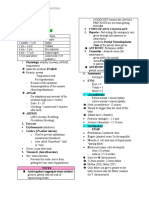
Table 1. Procedure summary and technical tips
1. Evaluate the shape of the PA: single lobe vs multilobed. Lack of recognition of multilocularity may result in failure of the
procedure (Figure 9).
2. Acknowledge the contraindications to treatment; superficial infection; co-existent AVF.
3. Identify the neck of the aneurysm by looking for the ‘‘to and fro’’ waveform in the connection between the aneurysm and
the native artery. If the neck is not clearly visible, the location of the maximal ‘‘to and fro’’ waveform in the aneurysm would
help identify the neck. This reduces the risk of embolization of thrombin by injecting close to the neck.
4. When there is difficulty demonstrating the connecting tract in deeper lesions, use of a lower MHz probe helps identify the
tract or exclude a PA (Figure 7).
5. The presence of forward diastolic flow in the aneurysm suggests an associated AVF (Figure 4). Lack of communication
between the PA and vein should be established before injecting the aneurysm, as existence of an AVF is a contraindication to
thrombin injection (Figures 3 and 4).
6. When there is more than one lobe, it is best to inject the lobe closest to the neck first as the thrombus formed can propagate
to involve the entire PA, precluding the need for individual lobar injections. Injection should be performed under real-time
grey-scale and with intermittent colour Doppler US guidance.
7. Complete thrombosis should be confirmed immediately after injection to determine the need for continuous or re-injection.
Early clot may be hypo- or anechoic so its presence is established by colour Doppler (Figure 11). In some cases, injection in the
non-thrombosed portion of the aneurysm is required since clot surrounding the first injection site prevents extension of
thrombin to the non-thrombosed portion.
8. The native artery and vein should be examined at the completion of the procedure to document their patency. Ankle pulses
should be checked at the end of a procedure.
AVF, arteriovenous fistula; PA, pseudoaneurysm.
The British Journal of Radiology, February 2008 155
J M Hanson, M Atri and N Power
Figure 2. Tissue vibration around the neck of a pseudoaneur-
ysm. Tissue vibration is an indication of underlying high-velocity
flow. On this transverse image, there is vibration artefact
surrounding the neck of the pseudoaneurysm (PA) (arrow).
(a) (b) (c)
Figure 3. Arteriovenous fistula. In (a), there is tissue vibration artefact (arrows) surrounding the femoral vein. This should be an
alarming finding for the existence of a high-velocity flow. The low-resistance arterial flow with high diastolic component is seen
at the fistulous site in (b) and in (c), pulsatile flow is shown in the femoral vein downstream from the fistula.
156 The British Journal of Radiology, February 2008
Pictorial review: Ultrasound-guided thrombin injection of iatrogenic groin pseudoaneurysm
(a) (b)
Figure 4. Pseudoaneurysm (PA) and arteriovenous fistula (AVF). This is an absolute contraindication to thrombin injection. Note
the low-resistance arterial flow pattern in the aneurysm in (a) and in (b) there is low resistance and high velocity across the
arterial connection of this aneurysm on spectral Doppler instead of the expected ‘‘to and fro’’ pattern.
The British Journal of Radiology, February 2008 157
J M Hanson, M Atri and N Power
(a)
Figure 5. Pulsatile flow in a groin vein after angiography. As
a consequence of transmission of flow from the adjacent
artery, pulsatile flow is seen in a groin vein after angio-
graphy. The two are compressed by surrounding oedema
and haematoma. This should not be confused with the
appearance of the draining vein of an AVF.
Figure 6. An example of a lymph node. In (a), the feeding
artery of a lymph node (curved arrow) could be confused for
the neck of an aneurysm. However, it has a normal low-
resistance arterial flow pattern on spectral Doppler, and in
(b) the hypoechoic node does not demonstrate the high-
resistance flow expected in a PA.
(b)
158 The British Journal of Radiology, February 2008
Pictorial review: Ultrasound-guided thrombin injection of iatrogenic groin pseudoaneurysm
(a) (b)
Figure 7. The role of a low-frequency probe. In (a), a low-frequency probe shows a small PA lying between the artery and the
vein (arrows). This was difficult to see using a high-frequency probe. The neck of the PA is seen with a ‘‘to and fro’’ Doppler
waveform in image (b).
(a) (b)
Figure 8. Pseudoneck: sagittal views. (a) A typical example of a PA (arrowheads) prior to treatment. In (b), the post-thrombin
injection, there is a branch artery adjacent to the haematoma (arrow), demonstrating a low-resistance arterial flow pattern that
is often seen after angiography because of hyperaemia. This flow pattern helps differentiating this from a true neck.
The British Journal of Radiology, February 2008 159
J M Hanson, M Atri and N Power
(a) (b) (c)
Figure 9. An example of a tri-lobed PA: transverse views. In (a), on grey-scale US, the larger more anterior distal lobe was
spontaneously thrombosed (white arrows). The smaller proximal lobes were patent (white arrowheads). In (b), a neck is
demonstrated between proximal and middle PAs with ‘‘to and fro’’ waveform (black arrow). These aneurysms were thrombosed
following thrombin injection of the proximal lobe of the aneurysm in (c).
(a) (b)
Figure 10. PA treated with a single injection of thrombin followed by a brief period of compression (sagittal views). In (a), there
is minimal filling of a PA (arrows) after injection, and in (b) a small clot (curved arrow) is demonstrated adherent to the site of
the neck of the PA within the parent vessel. This was non-consequential.
160 The British Journal of Radiology, February 2008
Pictorial review: Ultrasound-guided thrombin injection of iatrogenic groin pseudoaneurysm
Thrombin works in the final common pathway of the
clotting cascade and therefore bypasses the factors
influenced by heparin and Coumadin. The procedure is
relatively straightforward and requires a short learning
curve. Patients usually require no preparation, sedation or
long post-procedure hospital stay [6]. Prior to and after the
procedure, distal pedal pulses are examined. Initially, the
morphology of the PA is studied. If there is more than one
lobe, each lobe may have to be considered for injection
separately if injection in one lobe does not thrombose the
entire aneurysm. A low-frequency probe is helpful when
characterizing deeper aneurysms and their necks
(Figure 7). The injection should be done as far from the
PA neck as possible. Position of the maximum ‘‘to and fro’’
waveform in the PA helps in localizing the adjacent neck of
the aneurysm. The operator should be cautious that the
surrounding vessels are not mistaken for the neck of the
PA (Figure 8). Needle sizes for the injection of thrombin
range from 19 to 25 gauge. We use a 1 ml tuberculin
syringe and a 25-gauge needle. Doses as high as 1000 IU
were initially used in the treatment of PA, although
concentrations have been reduced with more experience.
Taylor et al [20] have successfully treated PAs with
Figure 11. PA requiring multiple injections; transverse view.
Follow-up US at 24 h shows a large component of aneurysm concentrations as low as 100 IU. We have successfully
thrombosed (arrows) with persistent PA filling centrally treated PAs with doses as low as 20 IU of thrombin.
(arrowheads). This responded to a repeat injection of 500 Thrombin injection is performed under real-time grey-
units of thrombin. scale US guidance to quantify the necessary amount of
thrombin needed as most aneurysms thrombose imme-
High-velocity flow across the neck can cause vibration diately. Grey-scale and colour Doppler are intermittently
of the adjacent soft tissues. This vibration artefact is used to confirm thrombosis, since, occasionally, acute
seen as a speckling artefact on colour Doppler (Figure 2) thrombus can be hypoechoic and not clearly visible on
and is helpful in locating the neck. The velocity of grey-scale imaging. Documenting the complexity of a
high-resistance flow within the aneurysm is diminished multilobar aneurysm is important, as the knowledge of
in aneurysms that are imminently closing. the number and location of the various lobes will
increase the success rate of thrombosis. With multilobar
aneurysms, injection of the lobe closest to the parent
artery may result in subsequent thrombosis of more
Differential diagnosis of pseudoaneurysm distal lobes by stopping the flow to those distal
The diagnosis of PA can be confused with lymph components (Figure 9) [15, 18, 21]. Sheiman and
node, arteriovenous fistula, haematoma, abscess, lym- Mastromatteo [22] and Brophy et al [17] suggest the less
phocoele, deep venous thrombosis (DVT) and a femoral efficacious method of injecting the distal lobe first to
hernia [15, 16]. However, most of these conditions are reduce the risk of injecting thrombin into the parent
easily differentiated from PA using colour and pulsed vessel. All of their failed procedures were multicompart-
Doppler (Figures 3–6). mental PAs [21]. Compression following incomplete
closure of the aneurysm may be effective (Figure 10).
This should not be encouraged owing to the risk of
forcing thrombin from the PA into the native vessel. We
Thrombin injection prefer to reinject because of the danger of expelling a
PAs can have a benign course and have been treated thrombus into the native artery with compression
expectantly [2]. They may remain static in size, regress or (Figure 11). Multiple injections are uncommonly needed
even thrombose spontaneously. Therefore, if the aneurysm and procedure failure is rare (Figure 12). Those unre-
is small or is mostly thrombosed and shows little flow, it sponsive to percutaneous thrombin injection would
can potentially be observed, and a repeat Doppler require surgical intervention, as a parent vessel lacera-
ultrasound needs to be performed if there has been a delay tion is a likely cause of PA reperfusion. PAs from vessel
between the diagnostic scan and possible intervention [17– lacerations will not respond to thrombin injection and
19]. In a small study sample, Kent et al [19] saw that PAs usually require surgical repair [22] (Figure 12).
with a mean size of less than 1.8 cm would thrombose After thrombin injection, distal pedal pulses should be
spontaneously. The mean time for this was 22 days (3– palpated to assess parent vessel patency. Initial reports
34 days). The skin overlying the proposed injection site of this procedure had insisted on bed rest for a fixed
should be intact and free of infection as this is a period of time but, as confidence has increased, it is
contraindication to percutaneous injection. Because of the increasingly performed as an outpatient procedure
risk of thrombin leakage into the venous circulation, the without the need for conscious sedation or bed rest [6].
presence of a coexistent arteriovenous fistula (AVF) is an Grewe et al [23] injected ultrasound contrast media
absolute contraindication to thrombin injection (Figure 3). into PAs prior to treatment and noted leakage into the
The British Journal of Radiology, February 2008 161
J M Hanson, M Atri and N Power
(a) (b)
(c) (d)
Figure 12. Procedure failure in a deep aneurysm; (a) and (b) sagittal US views; (c) and (d) axial enhanced CT examination
images. In (a) a large short-necked PA (arrows) arising from the distal external iliac artery is seen. The ‘‘to and fro’’ flow pattern
across the neck is documented in (b). (c) Despite three injections, there was persistent filling of the aneurysm (arrows) as shown
on a CT scan after thrombin injection. (d) There is an associated large retroperitoneal haematoma (arrows).
parent artery in 58% of initial needle placements. A small of Doppler features of PAs is important for proper
leak of thrombin into the parent vessel usually presents diagnosis, treatment and differentiation from its mimickers.
no sequelae as thrombin loses efficacy in rapid-flowing The procedure is relatively simple with a short learning
vessels and it is deactivated by circulating anti-thrombin curve.
III as was noted in one of our patients (Figure 10) [20].
Table 1 shows the steps to take to maximize the
success of this procedure and prevent complication. References
1. Olsen DM, Rodriguez JA, Vranic M, Ramaiah V, Ravi R,
Diethrich EB, et al. A prospective study of ultrasound
Conclusions injection of femoral pseudoaneurysm: a trend toward
minimal medication. J Vasc Surg 2002;36:779–82.
US-guided thrombin injection is now an established 2. Toursarkissian B, Allen BT, Petrinec D, Thompson RW,
treatment of iatrogenic groin PAs. However, the knowledge Rubin BG, Reilly JM, et al. Spontaneous closure of selected
162 The British Journal of Radiology, February 2008
Pictorial review: Ultrasound-guided thrombin injection of iatrogenic groin pseudoaneurysm
iatrogenic pseudoaneurysms and arteriovenous fistulae. J pseudoaneurysm complicated by transient ischemic attack
Vasc Surg 1997;25:803–8. and rescued with systemic abciximab. J Vasc Surg
3. Maleux G, Hendrickx S, Vaninbroukx J, Lacroix H, Thijs M, 2001;34:939–42.
Desmet W, et al. Percutaneous injection of human thrombin 14. Clark TWI, Abraham RJ. Thrombin injection for treatment
to treat iatrogenic femoral pseudoaneurysms: short and of brachial artery pseudoaneurysm at the site of a
midterm ultrasound follow-up. Eur Radiol 2003;13:209–12. hemodialysis fistula: report of two patients. Cardiovasc
4. Coley BD, Roberts AC Fellmeth BD, Valji K, Bookstein JJ, Intervent Radiol 2000;23:389–402.
Hye RJ. Postangiographic femoral artery pseudoaneurysms: 15. Middleton WD, Daysam A, Teefey S. Diagnosis and
further experience with US-guided compression repair. treatment of iatrogenic femoral artery pseudoaneurysms.
Radiology 1995;194:307–11. Ultrasound Q 2005;21:3–17.
5. Eisenberg L, Paulson EK, Kliewer MA, Hudson MP, Delong 16. Trigaux J-P, Daube A, De Wispelaere J-F, Van Beers B.
DM, Carroll BA. Sonographically guided compression Differential diagnosis and repair of femoral artery pseu-
repair of pseudoaneurysms: further experience from a doaneurysms: report of clinical experience using colour
single institution. AJR Am J Roentgenol 1999;173:1567–73. Doppler imaging. JBR-BTR 1994;77:111–15.
6. Sultan S, Nicholls S, Madhavan P, Colgan MP, Moore D, 17. Brophy DP, Sheiman RG, Amatulle P, Akbari CM. Iatrogenic
Shanik DG. Ultrasound guided human thrombin injection. A femoral pseudoaneurysms: thrombin injection after failed
new modality in the management of femoral artery pseudo- US-guided compression. Radiology 2000;214:278–82.
aneurysms. Eur J Vasc Endovasc Surg 2001;22:542–5.
18. Kruger K, Zahringer M, Franz-Dietmar S, Gossman A,
7. Powell A, Benenati JF, Becker GJ, Katzen BT, Zemel G.
Schulte O, Feldmann C, et al. Femoral pseudoaneurysms:
Percutaneous ultrasound-guided thrombin injection for the
management with percutaneous thrombin injections –
treatment of pseudoaneurysms. J Am Coll Surg
success rates and effects on systemic coagulation.
2002;194:S53–7.
Radiology 2003;226:452–8.
8. Pope M, Johnson KW. Anaphylaxis after thrombin injection
of a femoral pseudoaneurysm: recommendations for pre- 19. Kent KC, McArdle CR, Kennedy B, Baim DS, Anninos E,
vention. J Vasc Surg 2000;32:190–1. Skillman JJ. A prospective study of the clinical outcome of
9. Muntaen W, Zenz W, Edlinger G. Severe bleeding due to femoral pseudoaneurysms and arteriovenous fistulas
factor V inhibitor after repeated operations using fibrin induced by arterial puncture. J Vasc Surg 1993;17:125–33.
sealant containing bovine thrombin. Thromb Haemost 20. Taylor BS, Rhee RY, Muluk S, Trachtenberg J, Walters D,
1997;77:1223. Steed DL, et al. Thrombin injection versus compression of
10. Engelke C, Quarmby J, Ubhayakar G, Morgan R, Holmes K, femoral artery pseudoaneurysms. J Vasc Surg
Belli AM. Autologous thrombin: a new embolization 1999;30:1052–9.
treatment for intrasplenic pseudoaneurysm. J Endovasc 21. Bloom AI, Sheiman RG, Brophy DP. Iatrogenic femoral
Ther 2002;9:29–35. pseudoaneurysms. Radiology 2002;222:292–3.
11. Owen RJT, Jackson R, Loose HW, Lees TA, et al. 22. Sheiman RG, Mastromatteo M. Iatrogenic femoral pseu-
Percutaneous ablation of an internal iliac aneurysm using doaneurysms that are unresponsive to percutaneous
tissue adhesive. Cardiovasc Intervent Radiol 2000;23:389–91. thrombin injection: potential causes. AJR Am J Roentgenol
12. Sparrow P, Asquith J, Chalmers N. Ultrasonic-guided 2003;181:1301–4.
percutaneous injection of pancreatic pseudoaneurysm with 23. Grewe PH, Mugge A, Germig A, Harrer E, Baberg H,
thrombin. Cardiovasc Intervent Radiol 2003;26:312–15. Hanefeld C, et al. Occlusion of pseudoaneurysms using
13. Lin PH, Bush RL, Tong FC, Chaikof E, Martin LG, Lumsden human or bovine thrombin using contrast-enhanced ultra-
AB. Intra-arterial thrombin injection of an ascending aortic sound guidance. Am J Cardiol 2004;93:1540–2.
The British Journal of Radiology, February 2008 163
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Janet Belsky's Experiencing The Lifespan: Later Life: Cognitive and Socio-Emotional DevelopmentDokument28 SeitenJanet Belsky's Experiencing The Lifespan: Later Life: Cognitive and Socio-Emotional Developmentmia cokleyNoch keine Bewertungen
- Retina As Window To CNS Disorders - Eye Based Diagnosis of CNS - MS & ALZHEIMER DISEASE - ARDY GISNAWAN (ARD)Dokument8 SeitenRetina As Window To CNS Disorders - Eye Based Diagnosis of CNS - MS & ALZHEIMER DISEASE - ARDY GISNAWAN (ARD)UNHAS OphthalmologyNoch keine Bewertungen
- Handbook of Urology Diagnosis and Therapy (3rd Ed.) - Lippincott Williams & WilkinsDokument556 SeitenHandbook of Urology Diagnosis and Therapy (3rd Ed.) - Lippincott Williams & WilkinsdimasNoch keine Bewertungen
- Common DrugsDokument15 SeitenCommon DrugsKate Penelope DalidNoch keine Bewertungen
- Infectious Diseases Pharmacotherapy: Lesson 5 Central Nervous System InfectionDokument63 SeitenInfectious Diseases Pharmacotherapy: Lesson 5 Central Nervous System Infectionbest batiNoch keine Bewertungen
- Stroke Syndromes and Localization 2007Dokument56 SeitenStroke Syndromes and Localization 2007SaintPaul Univ100% (1)
- Gerontology and Geriatrics: Dr. Bernardo D. Morantte JRDokument9 SeitenGerontology and Geriatrics: Dr. Bernardo D. Morantte JRRenz Francis SasaNoch keine Bewertungen
- Reports of DeathsDokument86 SeitenReports of Deathsjeff.aufderheide2634Noch keine Bewertungen
- Historical Profile of Harold G WolffDokument2 SeitenHistorical Profile of Harold G WolffBarry BrantonNoch keine Bewertungen
- Vitamin B12 DeficiencyDokument6 SeitenVitamin B12 DeficiencyDzuljuniaf JaafarNoch keine Bewertungen
- Canine Elbow Dysplasia: Heidi Reuss-Lamky, LVT, VTS (Anesthesia)Dokument6 SeitenCanine Elbow Dysplasia: Heidi Reuss-Lamky, LVT, VTS (Anesthesia)Katarina SimicicNoch keine Bewertungen
- 23rd of DecemberDokument48 Seiten23rd of Decemberْ ّNoch keine Bewertungen
- Documentation of The Medical HistoryDokument5 SeitenDocumentation of The Medical Historyadultmedicalconsultants100% (1)
- Gingival Hyperplasia: Interaction Between Cyclosporin A and Nifedipine?Dokument3 SeitenGingival Hyperplasia: Interaction Between Cyclosporin A and Nifedipine?RamonaNoch keine Bewertungen
- 1 - FMGE Dec GH VersionDokument14 Seiten1 - FMGE Dec GH VersionHarshit SharmaNoch keine Bewertungen
- A. List Names of Antipsychotic Medications and Their Usual Range of Daily Dose For AdultsDokument7 SeitenA. List Names of Antipsychotic Medications and Their Usual Range of Daily Dose For AdultsAbbie_Borromeo_1036Noch keine Bewertungen
- Diabetes Mellitus in PediatricsDokument22 SeitenDiabetes Mellitus in PediatricsKermaigne MirandaNoch keine Bewertungen
- UCDokument6 SeitenUCapiv2010_808955526Noch keine Bewertungen
- Krimigranthi (Blepharitis) : Dr. Preeti PatelDokument24 SeitenKrimigranthi (Blepharitis) : Dr. Preeti PatelPreeti PatelNoch keine Bewertungen
- INSTRUMENTS For UGDokument22 SeitenINSTRUMENTS For UGPugazhenthi CNoch keine Bewertungen
- Grand Rounds PresentationDokument40 SeitenGrand Rounds Presentationapi-610941700Noch keine Bewertungen
- Generic Name: Brand Name: Drug Class: Chemical Structure:: Atorvastatin Lipitor StatinsDokument3 SeitenGeneric Name: Brand Name: Drug Class: Chemical Structure:: Atorvastatin Lipitor StatinsnivraeNoch keine Bewertungen
- Drug Study Module 4Dokument6 SeitenDrug Study Module 4Hannah Angelu CabadingNoch keine Bewertungen
- CH 1 - Cell Injury III Subcellular Responses To Injury - PPT (Compatibility Mode)Dokument7 SeitenCH 1 - Cell Injury III Subcellular Responses To Injury - PPT (Compatibility Mode)sultan khabeebNoch keine Bewertungen
- Care of Clients With Problems in OxygenationDokument8 SeitenCare of Clients With Problems in OxygenationRed StohlNoch keine Bewertungen
- Pedia TranscriptDokument18 SeitenPedia TranscriptUma CrespoNoch keine Bewertungen
- Case Report: Reynolds SyndromeDokument2 SeitenCase Report: Reynolds SyndromePeertechz Publications Inc.Noch keine Bewertungen
- Combination Estrogem ProgestinDokument8 SeitenCombination Estrogem ProgestinUdsanee SukpimonphanNoch keine Bewertungen
- ITE Crash Course - CardiologyDokument260 SeitenITE Crash Course - CardiologyDre2323Noch keine Bewertungen
- Delayed Acute Myocarditis and COVID 19 Relatedmultisystem in Ammatory SyndromeDokument6 SeitenDelayed Acute Myocarditis and COVID 19 Relatedmultisystem in Ammatory SyndromedrKranklNoch keine Bewertungen