Beruflich Dokumente
Kultur Dokumente
Infectious Myelopathies: Review Article
Hochgeladen von
night.shadowOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Infectious Myelopathies: Review Article
Hochgeladen von
night.shadowCopyright:
Verfügbare Formate
Infectious Myelopathies REVIEW ARTICLE
By Marie F. Grill, MD C O N T I N U UM A U D I O
I NT E R V I E W A V A I L AB L E
ONLINE
ABSTRACT
PURPOSE OF REVIEW: This article reviews bacterial, viral, fungal, and parasitic
pathogens associated with myelopathy. Infectious myelopathies may
be due to direct infection or parainfectious autoimmune-mediated
mechanisms; this article focuses primarily on the former.
RECENT FINDINGS: Some microorganisms exhibit neurotropism for the spinal
cord (eg, enteroviruses such as poliovirus and flaviviruses such as West
Nile virus), while others are more protean in neurologic manifestations (eg,
herpesviruses such as varicella-zoster virus), and others are only rarely
reported to cause myelopathy (eg, certain fungal and parasitic infections).
Individuals who are immunocompromised are at increased risk of
disseminated infection to the central nervous system. Within the last few
years, an enterovirus D68 outbreak has been associated with cases of
acute flaccid paralysis in children, and emerging Zika virus infection has
been concurrent with cases of acute flaccid paralysis due to Guillain-Barré
syndrome, although cases of myelitis have also been reported. Associated
pathogens differ by geographic distribution, with myelopathies related
to Borrelia burgdorferi (Lyme disease) and West Nile virus more commonly
seen in the United States and parasitic infections encountered more often
in Latin America, Southeast Asia, and Africa. Characteristic CSF and MRI
patterns have been identified with many of these infections.
SUMMARY: A myriad of pathogens are associated with infectious
myelopathies. Host factors, geographic distribution, clinical features,
CSF profiles, and MRI findings can assist in formulating the differential
CITE AS:
diagnosis and ultimately guide management. CONTINUUM (MINNEAP MINN)
2018;24(2, SPINAL CORD DISORDERS):
441–473.
INTRODUCTION Address correspondence to
I
Dr Marie F. Grill, Mayo Clinic,
nfectious myelopathies can result from direct viral invasion or can occur as 13400 E Shea Blvd, Scottsdale,
a parainfectious immune-mediated process. Acute inflammation results in AZ 85259, Grill.Marie@mayo.edu.
varying degrees of motor and sensory impairment, as well as bowel/bladder
RELATIONSHIP DISCLOSURE:
and other autonomic dysfunction, ultimately determined by the extent of Dr Grill reports no disclosure.
segmental involvement as well as the potential predilection for certain spinal
UNLABELED USE OF
cord regions. The microorganisms associated with myelopathy are many and
PRODUCTS/INVESTIGATIONAL
include bacteria, viruses, fungi, and parasites. Pathogens from each of these USE DISCLOSURE:
microbial groups will be highlighted in this article and are summarized in Dr Grill discusses the
unlabeled/investigational use
TABLE 4-1. Epidemiologic risk factors, clinical characteristics, CSF profiles, and
of IV immunoglobulin for the
imaging features may assist in the approach to differential diagnosis for infectious treatment of infectious
myelopathies. Treatment includes antimicrobial therapy (extrapolating myelopathies.
recommendations for meningitis management as specific recommendations © 2018 American Academy
for myelitis are lacking in most cases) with or without concomitant steroids; of Neurology.
CONTINUUMJOURNAL.COM 441
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
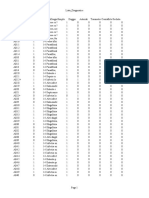
TABLE 4-1 Pathogens Associated With Infectious Myelopathies
Bacterial Infections
u Pyogenic: paraspinous infections/abscesses
u Tuberculosis/mycobacterial
u Borrelia species (Lyme disease)
u Treponema pallidum (syphilis)
u Brucella species
u Mycoplasma pneumoniae
Viral Infections
u DNA viruses
⋄Herpesviruses
→ Herpes simplex virus type 1
→ Herpes simplex virus type 2
→ Varicella-zoster virus
→ Epstein-Barr virus
→ Cytomegalovirus
⋄Human herpesvirus 6
⋄Human herpesvirus 7
⋄JC virus
u RNA viruses
⋄Enteroviruses
→ Poliovirus
→ Enterovirus 71
→ Enterovirus D68
→ Echovirus
→ Coxsackievirus A16, B2, B4, A9
⋄Flaviviruses
→ West Nile virus
→ St. Louis encephalitis virus
→ Japanese encephalitis virus
→ Tick-borne encephalitis virus
→ Dengue virus
→ Zika virus
⋄Hepatitis C
⋄Retroviruses
→ Human immunodeficiency virus
→ Human T-cell lymphotropic virus type I
CONTINUED ON PAGE 443
442 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
CONTINUED FROM PAGE 442
⋄Rabies
⋄Hepatitis A
⋄Hepatitis E
⋄Influenza A
⋄Paramyxoviruses
→ Measles
→ Mumps
Fungal Infections
u Endemic mycoses/dimorphic fungi
⋄Coccidioides immitis/Coccidioides posadasii
⋄Histoplasma capsulatum
⋄Blastomyces dermatitidis
u Yeasts
⋄Cryptococcus neoformans
u Yeastlike fungi
⋄Candida species
u Molds
⋄Septate mycetes
→ Aspergillus species
⋄Nonseptate mycetes
→ Zygomycetes, eg, Mucor
Parasitic Infections
u Taenia solium (neurocysticercosis)
u Echinococcus species
u Schistosoma species
u Toxoplasma gondii
u Plasmodium species (malaria)
u Gnathostoma spinigerum
u Toxocara canis
u Strongyloides stercoralis
u Paragonimus
u Angiostrongylus cantonensis
DNA = deoxyribonucleic acid; RNA = ribonucleic acid.
CONTINUUMJOURNAL.COM 443
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
KEY POINTS IV immunoglobulin (IVIg), other immunomodulatory treatments, and
neurosurgical interventions may also be appropriate in certain settings.
● Differential diagnosis of
infectious myelopathies
should be tailored based on DIAGNOSTIC PRINCIPLES
patients’ risk factors and Patient-specific epidemiologic risk factors should be identified and include
exposures. environmental exposures and travel history as well as immunologic status (eg,
history of diabetes mellitus, use of immunosuppressant medications, or disorders
● MRI of the spinal cord
with contrast is the gold of cell-mediated or humoral immunodeficiency). The duration of symptoms
standard for imaging in the should be ascertained as the differential diagnosis is influenced by whether the
diagnosis of infectious myelopathy is acute, subacute, or chronic. Examination will show varying
myelopathies. Specific MRI findings based on the site of spinal cord pathology and can assist in localizing the
patterns of abnormality
include extramedullary, disease process as well as identifying patterns that may be suggestive of specific
centromedullary, eccentric neurotropism (eg, acute flaccid paralysis from enteroviruses such as poliovirus
tract-specific, ventral horn, and West Nile virus due to tropism for motor neurons of spinal cord). Laboratory
and irregular/masslike investigations should include testing for selected pathogens including bacteria,
presentations. Notably,
imaging studies may also
viruses, fungi, and parasites (TABLE 4-2).
be normal. MRI of the spine with and without contrast is the gold standard for imaging in
the diagnosis of infectious myelopathies. Patterns of abnormality on spinal cord
● Pyogenic infections may MRI include extramedullary, centromedullary (eg, segmental or longitudinally
cause myelitis due to the
extensive transverse myelitis), eccentric tract-specific (eg, lateral columns, posterior
contiguous spread of a
nearby infection, such columns), ventral horn, and irregular/masslike presentations and may help to
as in association with narrow the differential diagnosis. Overlapping imaging patterns may be seen,
spondylodiscitis, or and, in some cases, the MRI may be normal. Brain MRI should also be obtained to
less commonly, by
assess for other areas of central nervous system (CNS) dissemination; for example,
hematogenous spread.
some pathogens may have accompanying meningitis with complications such as
● Staphylococcus aureus is hydrocephalus. Assuming no contraindications to lumbar puncture are present,
the most common cause of CSF studies (TABLE 4-3)1 should be pursued and should include opening pressure,
pyogenic infectious myelitis. cell count with differential, protein, glucose, Gram stain and culture, acid-fast
smear and culture, fungal stain and culture, and specific serologic-based as well as
polymerase chain reaction (PCR)-based testing for suspected pathogens.
BACTERIAL INFECTIONS
Bacterial causes of infectious myelopathies include pyogenic infections that carry
the potential for significant morbidity and mortality, as well as atypical bacterial
infections such as Lyme disease and syphilis.
Pyogenic Infections
Bacterial causes of infectious myelitis include pyogenic infections (ie, paraspinal
infections) due to hematogenous spread in the setting of bacteremia and, more
commonly, by direct inoculation and contiguous spread from nearby infection,
as seen with nearby spondylodiscitis or meningitis.2 Patients with myelopathy
associated with epidural abscess or spondylodiscitis typically present with back
pain and fever. Presentation may be acute, as when myelopathy occurs in
association with bacterial meningitis, or may be more chronic (eg, 2 to 12 weeks),
as occurs in association with spondylodiscitis. Spine MRI should be obtained
emergently and demonstrates an extramedullary pattern, given the abundant
vascular supply to the epidural region and associated spondylodiscitis (most
commonly within the lumbar region), facet arthropathy, or other paraspinous
infection. The involved spinal cord demonstrates less hyperintensity on
T2-weighted imaging than edema; varying intensities of contrast enhancement
444 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
are seen.3 Associated leptomeningitis, epidural fluid collection, or spinal cord
abscess may be seen. Staphylococcus is the most commonly implicated pathogen
(methicillin-resistant Staphylococcus aureus followed by methicillin-sensitive S.
aureus and methicillin-resistant Staphylococcus epidermidis); other pathogens
include Streptococcus agalactiae (group B streptococcus), Streptococcus viridans,
methicillin-sensitive S. epidermidis, Enterococcus faecalis, and Gram-negative
bacilli (eg, Escherichia coli, Klebsiella pneumoniae, and Enterobacter cloacae).4
Selected Diagnostic Studies to be Considered in the Evaluation of TABLE 4-2
Infectious Myelopathies
Blood Work
u Bacterial
⋄Blood cultures
⋄Rapid plasma reagin (RPR)/syphilis IgG
⋄Borrelia burgdorferi antibodies
⋄Mycoplasma pneumoniae antibodies
⋄QuantiFERON Gold (tuberculosis)
⋄Brucella agglutination titers
u Viral
⋄Human immunodeficiency virus
⋄Arboviral antibody panel
⋄Cytomegalovirus IgM and IgG
⋄Anti–hepatitis C antibody
⋄Human T-cell lymphotropic virus types I and II antibodies
u Fungal
⋄Fungal cultures
⋄Cryptococcal antigen
⋄Fungal pathogen-specific serologies
⋄β- -glucan
D
u Parasitic
⋄Peripheral blood smear
⋄Parasite-specific serologies
Other Studiesa
u CSF cell count with differential, protein, glucose, pathogen-specific antibodies, polymerase
chain reactions (PCRs), and cultures
u Bronchoalveolar lavage/sputum culture
u Nasopharyngeal swab for respiratory virus polymerase chain reaction (PCR) panel/culture
u Stool ova and parasite testing, cultures
CSF = cerebrospinal fluid; IgG = immunoglobulin G; IgM = immunoglobulin M.
a
CSF studies are listed in more detail in TABLE 4-3.
CONTINUUMJOURNAL.COM 445
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
Even in the absence of cord compromise from spinal abscess or epidural
hematoma, spinal cord ischemia may also occur in bacterial meningitis
due to hypotension in the setting of shock or due to vasculitis (with or
without associated arachnoiditis). Longitudinally extensive (typically
centromedullary) myelitis has also been reported as a rare phenomenon in
the setting of bacterial meningitis.5 Implicated pathogens include Neisseria
meningitidis and Streptococcus pneumoniae. If lumbar puncture can be
safely performed (eg, meningomyelitis without extrinsic fluid collection
such as an epidural abscess), CSF studies will characteristically show
polymorphonuclear-predominant pleocytosis and hypoglycorrhachia,
although CSF cultures may be sterile, underscoring the importance of
obtaining blood cultures. Biopsy of affected disk/bone may be considered
if cultures are negative. Erythrocyte sedimentation rate and C-reactive
protein can also be helpful both at diagnosis as well as in follow-up to assess
treatment response. Antibiotic treatment is tailored to the specific bacterial
TABLE 4-3 Characteristic Infectious Cerebrospinal Profiles and Testsa
Normal Bacterial Viral Fungal Tuberculosis
Opening pressure 180 Elevated, 200–500 Normal Normal to slightly Elevated
(mm H20) elevated
White blood cell <5 (lymphocytes 1000–5000 (range Lymphocyte 20–500, 10–500,
count (cells/μL) and monocytes) 100–10,000), predominant, lymphocyte lymphocyte
polymorphonuclear some initially predominant predominant
cells predominant polymorphonuclear
cells predominant
Protein (mg/dL) 45–50 Elevated, >45 (90%) Normal to slightly Elevated Elevated
elevated (100–500)
Glucose (mg/dL) 45–80 (65% of Decreased, <40 Normal Decreased Decreased
serum glucose) (50–60%)
Gram stain/ Positive Gram stain Viral culture Fungal culture Mycobacterium
culture (60–90%), bacterial tuberculosis
culture culture
Other Polymerase chain Viral PCRs and India ink stain Acid-fast smear;
reactions (PCRs): reverse and culture, M. tuberculosis
broad range 16S transcriptase PCRs cryptococcal PCR
ribosomal DNA and (eg, enterovirus), antigen, fungal-
specific pathogen pathogen-specific specific antigens/
serologies antibodies
DNA = deoxyribonucleic acid.
a
Data from Roos KL, Continuum (Minneap Minn).1
446 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
microorganism; empiric KEY POINT
therapy includes third- or
● Tuberculosis-related
fourth-generation cephalosporin spinal complications include
and vancomycin for at least spinal tuberculomas,
several weeks (duration vertebral tuberculosis/
determined by extent of spondylitis, spinal abscesses,
syringomyelia, and myelitis,
infection). Emergent surgical as well as associated
drainage is indicated in the radiculitis or arachnoiditis.
case of spinal epidural abscess
given that neurologic deficits
may remain permanent
(FIGURE 4-1).
Atypical Bacteria
Mycobacterium tuberculosis, Lyme
disease, syphilis, and brucellosis
are some of the atypical bacterial
diseases associated with
infectious myelopathies.
MYCOBACTERIUM TUBERCULOSIS.
The nervous system is among
the more common sites of
extrapulmonary dissemination
of tuberculous infection, which
most commonly manifests as
meningitis. A variety of spinal
FIGURE 4-1
cord pathologies associated with Large thoracic epidural abscess (arrows) as seen
tuberculous meningitis have on spine MRI on sagittal T2-weighted (A),
been reported, including spinal sagittal postcontrast T1-weighted (B), and axial
tuberculomas, vertebral T2-weighted (C) sequences. Abscess extends
superiorly to approximately the T2-T3 level;
tuberculosis/spondylitis (ie, Pott
note the corresponding effacement of the dorsal
disease), spinal abscesses, thecal sac with mild cord flattening.
syringomyelia (more commonly
seen as a later complication),
arachnoiditis, as well as myelitis
more frequently (although not exclusively) with concomitant radiculitis.6
The clinical presentation is often more insidious than some other infectious
myelopathies. The MRI pattern for M. tuberculosis spinal cord infection is
typically extramedullary. The genesis of pathologic mechanisms is found
in the posteriorly predominant thick inflammatory exudates characteristically
produced by the bacilli of M. tuberculosis. Thoracic segments are most often
affected, followed by cervical regions, and while most involve greater than
one spinal segment, longitudinally extensive myelitis is much less frequent.
More than 50% of myelitis cases are associated with arachnoiditis. In cases
of myeloradiculitis, cauda equina or conus medullaris syndromes may be
clinically evident given the predilection for lumbosacral nerve root
involvement.2 In addition to focal inflammation within the spinal cord
parenchyma, vasculitis of spinal blood vessels may also occur and lead to cord
ischemia (meningovascular disease).
CONTINUUMJOURNAL.COM 447
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
CSF classically demonstrates lymphocytic-predominant pleocytosis with
hypoglycorrhachia and significant protein elevation (at times reflective of
spinal block, which can be seen in fungal as well as mycobacterial infections).
Mycobacterial culture should be obtained as this is the gold standard for
diagnosis; M. tuberculosis PCR test in the CSF is also available as a more rapid
diagnostic tool, although it also has a variable range of sensitivity7; adjunctive
pulmonary testing (ie, bronchoalveolar lavage/sputum samples) can be helpful
in addition to chest imaging (preferably CT chest as chest x-ray may be
unremarkable). Assuming no drug resistance is present, treatment consists
of an intensive four-drug regimen (rifampin, isoniazid, pyrazinamide, and
ethambutol) for at least 2 months followed by two-drug therapy (isoniazid
and rifampin) for an additional 7 to 10 months. While not studied specifically
in the setting of myelitis, adjunctive high-dose corticosteroids (dexamethasone
or prednisolone tapered over 6 to 8 weeks) are recommended for tuberculous
meningitis and may be used in the setting of tuberculous myelitis.8 Paradoxical
reactions may occur several months after initiation of therapy for tuberculosis,
as seen in tuberculosis-associated immune reconstitution inflammatory syndrome
(IRIS). Surgery, such as shunt placement for patients with syringomyelia and
neurologic decline, may be appropriate. Atypical/nontuberculous mycobacteria
may also potentially be associated with myelitis, although the literature is scant;
case reports have suggested Mycobacterium avium complex and Mycobacterium
kansasii as potential nontuberculosis candidates, with an immune-mediated
mechanism suspected in the setting of primary pulmonary infection at least
in the case of M. kansasii.9
NEUROBORRELIOSIS (LYME DISEASE). Lyme disease is the most common tick-borne
infection in the United States and is transmitted by Ixodes species carrying the
spirochete Borrelia burgdorferi; borreliosis is also found in Europe (most
frequently non-Lyme Borrelia garinii). Neurologic manifestations are many and
include cranial nerve palsies, radiculitis, peripheral neuropathy, meningitis, and
encephalitis, in addition to myelitis (overlap in phenotypic features may be
seen); CNS involvement (and specifically myelitis) is much less frequently seen
than peripheral complications such as radiculitis and neuropathies.10 The clinical
presentation may be acute or subacute and typically presents early in the
infection rather than as a late complication. Spine MRI typically demonstrates a
centromedullary pattern of spinal cord involvement but may also be normal;
midthoracic and lumbar levels are most frequently involved, and patchy cord
enhancement may be present in addition to variable longitudinally extensive or
segmental inflammatory cord lesions.3 A poliomyelitislike syndrome with
corresponding signal abnormalities of the anterior horn cells has also been
described.11 CSF typically shows a mononuclear cell increase with elevated
protein and normal glucose. A gold standard diagnostic tool is lacking (likely in
part because bacterial concentration in CSF is very low), and Lyme IgG
CSF/blood index may initially be negative, so treatment should be initiated and
testing repeated if suspicion for Lyme disease exists. Serum and CSF Lyme
antibody titers need to be obtained to calculate the CSF index in order to confirm
intrathecal antibody production and distinguish it from passive antibody
transfer. Note also that false positives can occur given cross-reactivity with
Treponema pallidum; thus, CSF Venereal Disease Research Laboratory (VDRL)
test should additionally be obtained. The recommended treatment for
448 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
parenchymal Lyme disease is IV ceftriaxone (IV penicillin G and IV cefotaxime KEY POINTS
as alternatives) for a 14-day to 28-day course.12 That said, given the excellent CNS
● Treatment of tuberculous
penetration of doxycycline, this may be a reasonable alternative to parenteral meningitis consists of a
therapy (at least for Borrelia species in Europe) even for CNS infections, as four-drug antituberculosis
suggested by a European nonrandomized observational study.13 regimen of rifampin,
isoniazid, pyrazinamide, and
ethambutol as well as
NEUROSYPHILIS. Neurosyphilis encompasses a myriad of neurologic
consideration of
manifestations caused by the spirochete T. pallidum, given its protean nature, adjunctive steroids.
and while tertiary manifestations are much less common in the postantibiotic Tuberculosis immune
era, syphilitic myelitis should be considered within the differential for myelitis. reconstitution inflammatory
syndrome may be seen
Tabes dorsalis refers to a late (tertiary) manifestation of neurosyphilis that
several months after
typically occurs decades after primary infection; patients characteristically initiation of tuberculosis
present with progressive gait abnormalities. antimicrobial therapy.
More specific spinal cord MRI findings may include a “candle guttering”
appearance (seen on sagittal sequences) and “flip-flop” signs (hyperintensity on ● Central nervous system
complications of Lyme
contrast-enhanced T1-weighted sequences and hypointensity on T2-weighted disease are less common
images).14 Myelitis may present as cord swelling involving central cord than peripheral nervous
parenchyma and extending over multiple levels longitudinally, as seen in system complications and
meningomyelitis, although may also include meningovascular cord disease typically occur in the early
rather than the late stages
(secondary to ischemia), as well as osteitis and gumma, which may present as of infection.
intramedullary lesions and can also cause cord compression. A tract-specific
pattern on spinal cord MRI consisting of nonenhancing longitudinally extensive ● Recommended treatment
T2-hyperintense signal changes in the dorsal columns, often with associated cord for parenchymal Lyme
disease consists of IV
atrophy, may be seen in tabes dorsalis.3
ceftriaxone for a minimum
Diagnostic laboratory tests include positive serum rapid plasma reagin (RPR) 14-day course.
test; an RPR titer of at least 1:32 is associated with an increased likelihood of
neurosyphilis in patients both with and without human immunodeficiency virus ● Tabes dorsalis is a
(HIV), with an even higher risk in the latter group.15 CSF typically shows a manifestation of tertiary
neurosyphilis, and MRI may
lymphocytic-predominant pleocytosis with an elevated protein and positive show longitudinally
VDRL or treponemal-specific antibody testing. Parenteral penicillin G for 10 to extensive hyperintensities
14 days is the recommended treatment16; systemic steroids have not been found within the dorsal columns.
to be effective in neurosyphilis but have been used in some myelitis cases for
● Neurobrucellosis is a
cord edema and prevention of Jarisch-Herxheimer reactions.17 Recovery is often
zoonotic infection that may
suboptimal, particularly in cases with cord ischemia. uncommonly manifest as
myelitis; some cases may be
NEUROBRUCELLOSIS. Brucellosis is a zoonotic infection caused by aerobic, autoimmune mediated.
Gram-negative coccobacilli; cattle and goats are particularly important sources
of the infection, and related occupational exposures and consumption of
unpasteurized dairy products confer risk. Brucellosis is most commonly seen in
Middle Eastern, Mediterranean, and Latin American countries but can also be
found in the United States, particularly among immigrants.
Neurobrucellosis more commonly manifests as meningoencephalitis
(often chronic or undulating in its course), although rarely can have a
myelitic presentation.18 One case report details a longitudinally extensive
T2-hyperintense lesion with some minimal associated enhancement.18 Suspected
postinfectious Brucella-related myelitis has also been reported, as described
in one case of recurrent myelitis at the same spinal cord segment following
intracranial Brucella infection.19 Of interest, this case responded to
immunomodulatory treatment (cyclophosphamide and plasma exchange) and
was therein supportive of an autoimmune-driven pathogenesis. CSF typically
CONTINUUMJOURNAL.COM 449
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
demonstrates lymphocytic-predominant pleocytosis with decreased glucose
and elevated protein. Brucella agglutination titers can be obtained in serum
and in CSF; cultures have lower sensitivity in CSF than in blood.20 First-line
antimicrobial therapy typically consists of ceftriaxone in combination with
rifampin and doxycycline as well as consideration of an adjunctive short
course of high-dose steroids for spinal cord involvement.
MYCOPLASMA PNEUMONIAE. Mycoplasma pneumoniae is much more commonly
reported in the pediatric population and causes a neurologic syndrome that is
more than likely parainfectious, ie, immune-mediated, in nature along the
spectrum of acute disseminated encephalomyelitis. In the majority of reported
cases, M. pneumoniae–specific antibodies were positive by serologic testing,
which is how the diagnosis is typically established, while CSF PCR testing was
often negative, lending support to a parainfectious/postinfectious entity
rather than a myelitis mediated by direct infection. Coinfection with other
pathogens may also play a role in pathogenesis. Spinal cord MRI demonstrates
nonspecific T2 hyperintensity that may be longitudinally extensive; the thoracic
region is most commonly involved.21 Treatment includes macrolides or
doxycycline (the latter is preferred because of superior CNS penetration),
although it is unclear how effective antimicrobials or adjunctive corticosteroids
are in this setting; additional immunotherapy may also be considered.
OTHER BACTERIA. Burkholderia pseudomallei (melioidosis), an emerging pathogen
in Southeast Asia, has been implicated as a putative cause of myelitis.22
Additional bacterial infections that have been reported in association with
myelitis include Tropheryma whipplei (as a cause of chronic myelitis),23
Listeria monocytogenes, Rickettsia species (Rickettsia rickettsii and Rickettsia
tsutsugamushi), Chlamydia pneumoniae, and Bartonella henselae.24
VIRAL INFECTIONS
Viral causes of infectious myelitis are many, although herpesviruses, flaviviruses,
and enteroviruses are the more commonly causative pathogens given their
neurotropic character. The retroviruses human T-cell lymphotropic virus type I
(HTLV-I) and HIV are associated with chronic myelopathies.
Deoxyribonucleic Acid Viruses
DNA viruses, the Herpesviridae family (double-stranded DNA viruses), are most
commonly associated with infectious myelopathy.
HERPESVIRUSES. Human herpesviruses, of the Herpesviridae family, include
herpes simplex virus types 1 and 2 (HSV-1 and HSV-2), varicella-zoster virus
(VZV), Epstein-Barr virus (EBV), cytomegalovirus (CMV), and, less
commonly, human herpesviruses 6 and 7 (HHV-6 and HHV-7). These viruses
can be causes of infectious myelitis; respective PCR testing can be obtained in
the CSF in addition to serologies.
HERPES SIMPLEX VIRUSES TYPES 1 AND 2. In the adult population, HSV-2 is more
commonly associated with myelitis than HSV-1. Reactivation of herpesvirus
in sacral dorsal root ganglia can result in myeloradiculitis, secondary to
inflammation of the corresponding dorsal root and adjacent spinal cord (Elsberg
syndrome refers to the combination of myelitis and acute lumbosacral radiculitis
preceded by herpes virus infection).25 Extension into the cervicothoracic
450 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
region may be seen on imaging studies. Encephalomyeloradiculitis has also been KEY POINTS
reported as both an infectious and parainfectious entity,26 underscoring the fact
● In adults, herpes simplex
that HSV disease can manifest itself ubiquitously throughout both the CNS virus type 2 is more
and peripheral nervous system. HSV myelitis may be acute or subacute in onset commonly associated with
and may present in an ascending fashion. Imaging findings in some cases have myelitis than herpes simplex
been suggestive of hemorrhagic necrosis of the cord.27 Recommended treatment virus type 1, as seen in
radiculomyelitis with
is IV acyclovir with consideration of high-dose adjunctive corticosteroids as this
reactivation of herpesvirus
may reduce the risk of ascending myelitis28; recovery ranges from permanent in the sacral dorsal
disability to complete resolution. root ganglia.
VARICELLA-ZOSTER VIRUS. VZV is also quite protean in its neurologic ● Varicella-zoster virus is
manifestations, and while myelitis is not one of the more frequently encountered one of the more common
causes of infectious myelitis
complications of VZV, it is, in fact, one of the more common causes of infectious
and is typically subacute
myelitis. Typical clinical symptoms manifest as asymmetric weakness with in presentation.
sensory impairment preferentially involving pain and temperature modalities,
with subacute onset ranging from days to weeks; it is often monophasic. VZV ● In suspected varicella-
myelitis often occurs in the absence of rash (zoster sine herpete). In individuals zoster virus myelitis, CSF
varicella-zoster virus IgG
who are immunocompromised, the presentation may be insidious and more antibody should also be
severe.29 Imaging characteristically demonstrates T2 hyperintensities of the obtained, as the CSF
ipsilateral dorsal horns and columns along with pathologic enhancement polymerase chain reaction
reflecting the path of reactivation of latent virus, most commonly in the thoracic for this agent may be
negative.
region; centromedullary cord involvement and longitudinally extensive lesions
are less common.3 Enhancement and thickening of the nerve roots and
inflammation within brain parenchyma may be seen in cases with accompanying
radicular and encephalitic involvement, respectively. CSF shows mild
pleocytosis, although it often can be normal. VZV IgG should also be obtained in
the CSF as this can be supportive of VZV disease even with negative PCR testing,
particularly in those with latency for weeks to months after the rash, or in cases
of zoster sine herpete.29 Treatment consists of IV acyclovir. Adjunctive steroids
may be considered and are recommended with concomitant vasculopathy.
EPSTEIN-BARR VIRUS. EBV myelitis may be preceded by mononucleosis with the
development of myelitis symptoms several weeks later, although EBV can also
occur synchronously with mononucleosis. Clinical symptoms include varying
patterns of sensory, motor, and bladder dysfunction depending on the degree of
cord involvement. EBV myelitis may be associated with meningitis, encephalitis,
or radiculitis.30 Imaging most commonly demonstrates longitudinally extensive
lesions in a centromedullary pattern and cord expansion with or without
associated enhancement.3 CSF typically shows mononuclear-predominant
pleocytosis, elevated protein, and normal glucose. CSF EBV PCR should be
obtained along with IgM and IgG (ie, positive IgM antibodies to capsid antigen
and negative IgG to nuclear antigens) as well as corresponding serologic testing
within blood as false-positive CSF EBV PCRs can occur with passive transfer
to the CSF (traumatic lumbar puncture). IV acyclovir or ganciclovir and steroids
are used in the management of EBV-associated myelitis, although data are
lacking for efficacy of antiviral therapy.31
CYTOMEGALOVIRUS. CMV is almost exclusively seen in patients who are
immunocompromised, such as in patients who experience reactivation of latent
virus in the setting of acquired immunodeficiency syndrome (AIDS) and solid
organ and hematopoietic stem cell transplantation. Clinically, patients typically
CONTINUUMJOURNAL.COM 451
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
present with acute radicular pain followed by ascending weakness and urinary
retention. It should be noted that MRI may be normal in up to 50% of cases32;
thus, the clinician must maintain a strong index of suspicion in individuals
who are immunocompromised and present with a myelitic syndrome. When
abnormal imaging is present, pathologic enhancement and nerve root
thickening with predilection for the ventral roots of the cauda equina may
be seen; arachnoiditis has also been described.3 CSF may demonstrate a
neutrophilic predominance and mild hypoglycorrhachia. The presence of
CMV PCR in the CSF provides diagnostic confirmation. Treatment consists
of IV ganciclovir.
HUMAN HERPESVIRUS 6. HHV-6 is most commonly reported in allogeneic
hematopoietic stem cell transplant recipients (highest risk in cord blood
transplantation); use of mycophenolate mofetil may be an independent risk
factor for HHV-6 myelitis in this population. Accompanying symptoms
include pain and generalized pruritus.33 Treatment consists of antiviral
therapy with ganciclovir or foscarnet (extrapolated from the management of
HHV-6 encephalitis).
HUMAN HERPESVIRUS 7. Rare case reports exist of reactivation of HHV-7 infection
causing acute myelitis, including one case that occurred in a patient following
bone marrow transplantation and one in the setting of HIV infection
(interestingly, with a CD4 count of more than 500 and an undetectable viral
load).34,35 Treatment consists of foscarnet.
Ribonucleic Acid Viruses
RNA viruses are usually single stranded and include enteroviruses, flaviviruses,
and hepatitis C virus.
ENTEROVIRUSES. Enteroviruses belonging to the Picornaviridae family are
transmitted primarily via fecal-oral transmission and are recognized as an
emerging pathogen in children, as well as in adults who are immunocompromised.
Enteroviruses implicated in myelitis include enterovirus 71, coxsackieviruses
(A16, B2, B4, A9), echovirus, and poliovirus and have a predilection for
anterior horn cell involvement. Thus, MRI findings typically manifest as
abnormal signal within the ventral nerve roots (unilateral or bilateral). High
fevers often occur along with neurologic symptoms. CSF pleocytosis may
be polymorphonuclear predominant in the first 72 hours and is otherwise
characteristically lymphocytic predominant; CSF protein is commonly elevated.
Enterovirus PCR in the CSF should be used for disease confirmation, and
specific serologies may be obtained (eg, poliovirus-specific IgM). Enterovirus
may also be isolated from stool samples or nasopharyngeal swabs. While a
specific antienteroviral agent is not presently available, IVIg may be
considered as a treatment option for severe neuroinvasive disease in
affected individuals.
POLIOVIRUS. Poliovirus is considered the prototype for myelitis and is
characterized clinically by acute flaccid paralysis due to infection of the anterior
horn cells. This disorder is much less frequently encountered in the age of the
poliovirus vaccination; however, poliomyelitis has not been eradicated and
remains endemic in areas where vaccination accessibility is impaired, such as in
452 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Nigeria. Poliomyelitis typically presents as acute to subacute asymmetric KEY POINTS
weakness; the lower extremities are more commonly affected than the upper
● Cytomegalovirus myelitis
extremities, and bulbar involvement may also occur in addition to autonomic is almost exclusively seen
dysfunction. Myalgias and muscle spasms frequently occur, and muscle atrophy in patients who are
may be noted after several weeks. immunocompromised. MRI
On examination, tone is flaccid, and hyperreflexia is present initially, may show thickening and
enhancement of the ventral
although deep tendon reflexes are eventually absent in the involved regions. nerve roots of the cauda
Abnormal cord signal changes within the ventral horns may be seen on MRI equina but may be normal in
in the acute to subacute stages. Serologies such as CSF IgM for poliovirus as up to 50% of cases.
well as stool cultures can be used to confirm the diagnosis. Treatment
● Enteroviruses have a
is supportive. predilection for anterior
Postpolio syndrome is characterized by progressive weakness, atrophy, pain, horn cell involvement.
and fatigue decades after poliovirus infection. Specific MRI abnormalities are
● Poliovirus is characterized
lacking for this syndrome.36
by acute flaccid paralysis
due to infection of the
ENTEROVIRUS 71. Enterovirus 71 is most commonly associated with anterior horn cells.
hand-foot-and-mouth disease and herpangina; however, it has become
well-recognized in its tropism for motor neurons of the brainstem and spinal ● Postpolio syndrome is
characterized by
cord. Numerous outbreaks have been reported including epidemics in progressive weakness,
Southeast Asia.37 atrophy, pain, and fatigue
Clinically, patients present with an acute flaccid paralysis typically within 2 to and occurs decades after
3 weeks of inoculation; tremor, ataxia, or myoclonus may precede the onset poliovirus infection.
of acute flaccid paralysis. Spinal cord MRI typically shows segmental or ● A cluster of acute flaccid
longitudinally extensive increased T2 signal concentrated in the ventral horns; paralysis cases were
associated enhancement may also be seen. A centromedullary pattern of reported during an outbreak
longitudinally extensive transverse myelitis may also be seen less frequently of enterovirus D68, therein
supporting an association
and portends a worse prognosis.3 Abnormal signal may also be observed in between the conditions.
the dorsal medulla and pons on MRI (rhombencephalitis). As with other
enteroviruses, no specific antiviral therapy exists, although IVIg is sometimes
used. Significant motor and autonomic dysfunction may be seen in long-term
follow-up and does not necessarily correlate with severity of disease at onset
or with use of IVIg.38
ENTEROVIRUS D68. Cases of acute flaccid paralysis were reported during an
outbreak of enterovirus D68 respiratory illnesses (ranging from pharyngitis to
severe pneumonia with respiratory failure) initially in Colorado and later
reported in nearby states in the spring and summer of 2014; thus, while direct
causation was not established, this cluster of cases supports an association
between enterovirus D68 and acute flaccid paralysis.39 This was further
supported by findings of nasopharyngeal swabs positive for enterovirus D68 in
almost half of the affected patients. In these cases, spinal cord MRI demonstrated
confluent longitudinally extensive T2 hyperintensity of the cord gray matter,
most commonly affecting cervical regions. Abnormalities also included
brainstem lesions of the motor nuclei (eg, dorsal pontine tegmentum and ventral
pons). Enterovirus D68–associated MRI findings also include thickening and
enhancement of the nerve roots and a centromedullary pattern.3 In the review of
US cases of acute flaccid myelitis from 2012 to 2015, the majority of cases were in
the pediatric population, with a reported median age of 7.1 years (range of
5 months to 73 years of age); and a minority of patients (n = 9; 15%) were older
CONTINUUMJOURNAL.COM 453
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
than 21 years of age.39 Apart from one case in which enterovirus D68 was
identified in bloody CSF, no other infectious agents were isolated from the CSF,
and identification of respiratory viruses (which also include respiratory syncytial
virus, adenovirus, rhinovirus, influenza virus, and parainfluenza virus) was
made from respiratory specimens.39 IVIg, corticosteroids, and plasma exchange
have been used as treatment in these cases.
FLAVIVIRUSES. Flaviviruses are arthropod-borne RNA viruses, and while they are
more commonly associated with encephalitis, they can also be associated with
myelitis, namely in association with acute flaccid paralysis. Given the limitations in
treatment, focus is on prevention of disease transmission through mosquito bites
(and tick bites in the case of tick-borne encephalitis virus).
WEST NILE VIRUS. West Nile virus is carried by the Culex species of mosquitoes
and is now considered endemic in the United States. While neuroinvasive
disease is uncommon, when it does occur, meningitis and encephalitis are the
typical manifestations. An estimated 5% to 10% of neuroinvasive disease cases
are associated with myelitis, specifically, a poliolike illness characterized by
acute flaccid paralysis. Antecedent clinical symptoms often include fever, rash,
and myalgias, as well as meningitis/encephalitis, followed (usually within 24
to 48 hours) by relatively abrupt rapidly progressive asymmetric
flaccid weakness.
Examination characteristically shows diminished to absent reflexes; bowel
and/or bladder dysfunction may also be present. Respiratory distress may
develop as a consequence of lower brainstem motor nuclei involvement and
often portends a worse prognosis; patients with other bulbar symptoms such
as dysphagia and dysarthria are more likely to develop respiratory compromise.
West Nile virus has a predilection for anterior horn cell involvement that is
reflected in diagnostic studies, with spinal cord MRI typically demonstrating
abnormal signal centered within the ventral cord (sometimes with associated
ventral nerve root enhancement), and nerve conduction study and EMG
showing motor axonopathy with relatively minimal (if any) sensory
abnormalities.40,41 Of note, spinal cord MRI may also be unremarkable; thus, a
high index of clinical suspicion should be maintained even in the absence of
abnormal MRI findings. In the majority of cases, CSF demonstrates a pleocytosis
that may be neutrophil-predominant initially, in addition to mildly elevated
protein and normal glucose levels. Serologic testing should be obtained in both
blood and CSF. Although CSF West Nile virus PCR has 100% specificity, CSF
West Nile virus IgM is more sensitive. It should be noted that patients are
typically no longer viremic by the time they present with neuroinvasive disease;
therefore, the utility of nucleic acid amplification testing is limited. IgM
antibodies can persist for prolonged periods of time (months, even longer
than 1 year); thus, paired acute and convalescent IgM and IgG antibody titers
are necessary to establish acute infection. Testing should be repeated after
1 week of symptom onset if West Nile virus is suspected clinically to increase
testing yield.
As with other flavivirus infections, no specific antiviral treatment is known,
and supportive care remains the mainstay of treatment (CASE 4-1). Prior
randomized trials of pooled donor high-titer West Nile virus–specific IVIg
454 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
formulation failed to show efficacy, although trials were significantly limited KEY POINT
by challenges in recruitment. Anecdotal reports in the literature suggest that ● Japanese encephalitis
IVIg use may be beneficial, particularly in the case of individuals who are virus is the most common
immunocompromised (eg, patients who have undergone a transplant) given the cause of acute flaccid
coexistent increased morbidity and mortality,42 and the thought is that West Nile paralysis in children
in Vietnam.
virus–specific immunoglobulins would be included within the US donor
pool given that West Nile virus is considered endemic in the United States.
Interferon-alfa-2b has also been shown to possess some in vitro anti–West Nile
virus activity, although further evidence is lacking.41
ST. LOUIS ENCEPHALITIS VIRUS. St. Louis encephalitis virus is similar to West Nile
virus in its clinical manifestations; thus, St. Louis encephalitis virus should be
considered within the differential diagnosis whenever West Nile virus is
suspected. A concurrent West Nile virus and St. Louis encephalitis virus outbreak
was first reported in Arizona in 2015.43 Cross-reactivity in antibody testing
may occur given that the viruses are closely related within the Flaviviridae
family; therefore, confirmatory neutralization antibody testing via the local
department of health or Centers for Disease Control and Prevention is necessary
to establish the diagnosis. Similar to West Nile virus, some have used IVIg
with or without concomitant interferon-alfa for St. Louis encephalitis virus
neuroinvasive disease.
JAPANESE ENCEPHALITIS VIRUS. Japanese encephalitis virus is an important global
neurotropic flavivirus, with areas of endemicity that include countries
throughout Asia and the Western Pacific. It is transmitted by the Culex species of
mosquitoes and represents the leading cause of vaccine-preventable encephalitis
in these areas, as well as the most common cause of acute flaccid paralysis in
children in Vietnam. Serologic studies should be obtained in both blood and
CSF as DNA testing may be negative by the time the patient presents (as with
other flavivirus infections). Case reports of immune-mediated acute transverse
myelitis following Japanese encephalitis virus infection (ie, 3 weeks after
signs and symptoms consistent with Japanese encephalitis virus–related
encephalitis) can also be found in the literature; IV steroids were used in at
least one case.44,45
TICK-BORNE ENCEPHALITIS VIRUS. Tick-borne encephalitis virus is another
flavivirus transmitted in many areas of Europe (especially central), Siberia,
far-eastern Russia, and Asia. Illness is biphasic, with fevers and rash occurring
4 to 28 days (median of 8 days) following ixodid (hard) tick bite, and neurologic
manifestations typically occur after a period of defervescence. Myelitis most
often occurs in association with meningoencephalitis, although it has also been
reported as an isolated syndrome. This virus also has a predilection for ventral
cord involvement and therefore should be considered within the differential for
acute flaccid paralysis. Spinal cord MRI may be unremarkable. Serologic testing
should be obtained in both serum and CSF.46 The mainstay of treatment is
supportive care.
DENGUE VIRUS. Dengue is transmitted by Aedes aegypti and Aedes albopictus
mosquitoes. It is estimated that 40% of the world’s population reside in endemic
areas, which include countries in the Americas, the Caribbean, Africa, Asia,
and the Pacific. Dengue fever and shock are commonly encountered clinical
CONTINUUMJOURNAL.COM 455
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
manifestations, although rare cases of dengue-associated transverse myelitis
have been reported.47 These patients are typically managed with supportive care.
ZIKA VIRUS. Zika virus is an emerging flavivirus also transmitted by the A. aegypti
and A. albopictus mosquitoes. Zika has quickly established a reputation for
neurotropism, with increased reports of acute flaccid paralysis thought to be
secondary to Guillain-Barré syndrome and of microcephaly due to congenital
Zika infection.48 Several cases of myelitis secondary to Zika infection have also
been reported; in at least one case, MRI demonstrated nonspecific abnormal cord
signal.49 Steroids have been used in at least one of these cases.49
Hepatitis C Virus
Hepatitis C virus is an RNA virus belonging to the Flaviviridae family and is
well-established as a cause of hepatitis, which may be acute or may develop into a
chronic infection. Extrahepatic manifestations include rare reports of associated
acute or subacute myelopathy. Transaminitis may not necessarily be present,
therein underscoring the importance of checking for hepatitis C (serum
CASE 4-1 A 55-year-old man with no significant past medical history presented to
the emergency department during the summer with symptoms of fever,
chills, malaise, dull headache, and weakness that he had experienced
over several days. He was admitted for further evaluation, and his
weakness progressed overnight.
Neurologic examination demonstrated lethargy, dysarthria, tremor, and
left greater than right weakness involving the extremities, with diminished
tone. Initial CSF profile showed a neutrophil-predominant pleocytosis with
mildly elevated protein. MRI of the cervical spine (FIGURE 4-2) showed
longitudinally extensive T2 hyperintensity involving the ventral horns.
West Nile virus IgM in the CSF was negative, although CSF West Nile virus
polymerase chain reaction (PCR) was positive.
His weakness progressed, and he required ventilatory support.
Following a prolonged stay in the intensive care unit, he ultimately was
discharged to a rehabilitation facility, and in follow-up several months
later, he had some residual weakness and cognitive symptoms.
COMMENT Most cases of West Nile virus occur in the summer and fall when mosquitoes
are most active. West Nile virus is a poliolike virus with a predilection for
anterior horn cell involvement and presents as asymmetric acute flaccid
paralysis. The pleocytosis in arboviral infections like West Nile virus may be
polymorphonuclear predominant early in infection (typically for the first
72 hours, but may persist for as long as 1 week). West Nile virus IgM antibody
may not be positive for up to 7 days after symptom onset; CSF West Nile
virus PCR has lower sensitivity than antibody testing. Repeat lumbar
puncture should be performed if the initial lumbar puncture was performed
early in the course of infection. Persistent cognitive symptoms are
commonly reported in patients with neuroinvasive West Nile virus.
456 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
anti–hepatitis C antibody) even in the absence of abnormal liver function tests.
The specific time course is variable as cases of myelitis have been reported to
occur more than 10 years following initial infection (this likely has to do with the
chronic nature of this virus).50 Accompanying spinal cord MRIs demonstrate
longitudinally extensive nonenhancing centromedullary T2 hyperintensity
typically involving the cervical and thoracic regions, although enhancement and
lumbar involvement have also been reported; MRI may also be normal.3 As
with other pathogens, it is unclear whether this results from direct viral
load–related mechanisms or indirect immune-mediated pathology. While it is of
interest that hepatitis C virus RNA has been isolated in the CSF in several of these
cases, it should also be noted that this can be identified in at least half of
patients with hepatitis C virus infection even in the absence of myelitis or
other CNS pathology.50 Steroids with or without IVIg have been used as
treatment in these cases with improvement noted, particularly in the acute
phase. Given the suspected immune-mediated mechanism, antiviral therapy is
not helpful for acute attacks but may potentially reduce the risk and frequency
of relapses.51
FIGURE 4-2
Cervical spine MRI of the patient in CASE 4-1 with West Nile virus myelitis demonstrating
hyperintensity bilaterally within the ventral horns on sagittal T2-weighted (A) and axial
gradient recalled echo (B) sequences.
CONTINUUMJOURNAL.COM 457
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
KEY POINTS Retroviruses
Retroviruses are RNA viruses named for using their own reverse transcriptase
● Zika virus has been
associated with acute
to produce DNA from an RNA genome. HTLV-I, HTLV-II, and HIV (previously
flaccid paralysis thought to referred to as HTLV-III in earlier iterations) belong to this class of viruses.
be secondary to Guillain-Barré Infection may be acquired via vertical transmission (eg, breast-feeding), shared
syndrome, although IV drug needles, blood transfusion, or sexual transmission.
several cases of myelitis
have also been reported.
HUMAN IMMUNODEFICIENCY VIRUS. The differential for myelitis in individuals
● Vacuolar myelopathy with HIV includes opportunistic infections such as VZV, CMV, toxoplasmosis,
related to human syphilis, and tuberculosis. HIV belongs to the Lentivirus genus and is itself also
immunodeficiency virus and directly associated with myelopathy. Vacuolar myelopathy is the classic
acquired immunodeficiency
spinal cord pathology associated with AIDS and parallels the AIDS dementia
syndrome preferentially
involves the posterior complex spectrum, ie, seen in later stages of the disease. The pathologic
columns of the thoracic hallmark is macrophage infiltration and vacuolization of the lateral and
cord. Patients typically posterior columns of the thoracic spinal cord. Postmortem studies suggest that
present with slowly
greater than one-third of patients with AIDS have these findings, although a
progressive spastic
paraparesis with impaired smaller proportion are symptomatic; thus, the degree of vacuolization is
sensation and bladder severe by the time of presentation.52 Clinically, patients present with a slowly
dysfunction. progressive spastic paraparesis, impaired vibratory and position sense, and
urinary urgency; erectile dysfunction may be an earlier sign. Spinal cord MRI
● Human T-cell
lymphotropic virus is a demonstrates symmetric nonenhancing increased T2 signal within the posterior
classic chronic viral columns (thoracic cord). Other infectious, metabolic, and neoplastic causes
myelopathy. Affected of myelopathy need to be excluded. Apart from antiretroviral drugs for HIV
individuals present with a infection, no specific treatment is known, and severe paraparesis resulting in
slowly progressive lower
extremity spastic the inability to walk and loss of sphincter control are seen as the disease
paraparesis, sensory progresses. HIV myelitis may also occur as a manifestation of acute HIV
impairment, and urinary infection. IV corticosteroids may be used for treatment in this setting with
incontinence. good response.53
● The paralytic form of
HUMAN T-CELL LYMPHOTROPIC VIRUS. HTLV-I belongs to the oncovirus subgroup
rabies virus infection, in
which many of the more of retroviruses and, as such, is associated with adult T-cell leukemia/lymphoma;
classic rabies symptoms additionally, this virus is the cause of HTLV-associated myelopathy/tropical
may be lacking, can be spastic paraparesis (HAM-TSP) (CASE 4-2). Endemic areas include the
associated with myelitis.
Caribbean, Melanesia, Brazil, Africa, and Japan. HTLV-II is found in North and
South America and parts of Asia. The association between myelitis and HTLV-II
is not as clear as the well-established association between myelitis and HTLV- I,
which has a much higher incidence. The latent period between infection and
symptom onset may be years. HAM-TSP is the classic chronic viral myelopathy.
It is suspected to be immunologically mediated and occurs more commonly in
women. Affected individuals present with a slowly progressive lower extremity
spastic paraparesis, sensory impairment, and urinary incontinence.54 Spinal cord
MRI typically shows cord atrophy; cord edema and longitudinally extensive T2
hyperintensity also occur less commonly.3 HTLV-I– and HTLV-II–specific
antibody titers can be obtained in both blood and CSF. Data for effective
treatment have been lacking overall (interferon-alfa has been used, although it
has not conclusively been shown as effective long-term). That said, a recent
study suggests benefit of steroids, specifically low-dose continuous
administration of prednisolone, in slowing disease progression.55 Symptomatic
treatments include pulsed IV methylprednisolone for pain and danazol for
bladder dysfunction.54,56
458 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Lyssaviruses
Lyssaviruses are RNA viruses that cause rabies in both humans and adults.
RABIES. Rabies transmission to humans is typically via a rabid animal bite
(including wild animals such as bats, raccoons, skunks, foxes, and coyotes, as
well as domestic animals such as dogs and cats) and less commonly via saliva
from a rabid animal entering a wound or the eyes, nose, or mouth. The paralytic
form, which includes approximately 20% of cases, versus the classic form, may
be associated with myelitis and should be considered in the differential diagnosis
A 48-year-old woman from the CASE 4-2
Caribbean presented with a
several-year history of gradually
progressive lower extremity weakness
and gait disturbance. She also noted
some recent increased urinary
urgency. Neurologic examination
showed spasticity of the lower
extremities, brisk deep tendon
reflexes with ankle clonus, and
bilateral Babinski signs. MRI of the
thoracic spine (FIGURE 4-3)
showed longitudinally extensive
T2-hyperintense signal with no
associated enhancement. Serum was
positive for human T-cell
lymphotropic virus
type I (HTLV-I).
FIGURE 4-3
Sagittal T2-weighted thoracic spine
MRI of the patient in CASE 4-2 with
human T-cell lymphotropic virus type
I infection demonstrating abnormal
intramedullary T2 hyperintensity
(arrow) of the distal spinal cord and
conus medullaris (T10 through L1).
This case highlights the chronic presentation of HTLV-I–associated COMMENT
myelopathy, also known as tropical spastic paraparesis. The disease is
considered endemic in the Caribbean, Japan, and regions in Africa; cases
may also be associated with a history of blood transfusion. Abnormalities
on MRI include abnormal T2 hyperintensity (often involving the lateral
columns) and cord atrophy, although imaging findings are variable and may
often be normal.
CONTINUUMJOURNAL.COM 459
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
of encephalomyelitis. It should be noted that in this paralytic form, some of the
more classic rabies symptoms such as hydrophobia and autonomic dysfunction
may not be present. The disease is rapidly progressive, and death typically
occurs within 5 to 10 days; this is a distinguishing feature of rabies myelitis in
contrast to other myelopathies. MRI characteristics include longitudinally
extensive T2 hyperintensity with accompanying edema and preferential
involvement of gray matter (ie, ventral cord) with relative sparing of white
matter.57 Several tests are required for confirmation including antibody testing in
serum and CSF, antigen testing in cutaneous nerves at hair follicle bases via skin
biopsy, and virus isolation or reverse transcriptase PCR testing in saliva. No
treatments have been found to be effective, although some clinicians still
consider the Milwaukee protocol (therapeutic coma with ketamine, ribavirin,
and amantadine) despite this.58
Other Viruses
Cases of myelitis have also been reported in association with hepatitis A,59
hepatitis E,60 influenza A,61 measles,62 mumps,63 and JC virus64 infections.
FUNGAL INFECTIONS
Fungal infections of the CNS are typically associated with increased morbidity
and mortality in comparison to bacterial, viral, and parasitic infections, although
spinal fungal infections typically confer a better prognosis than intracranial
extension. The route of infection is characteristically via inhalation of aerosolized
fungi into the lungs or paranasal sinuses and is most often self-limited, although
it can disseminate to the CNS, albeit infrequently. Immunocompromised
populations are at increased risk. Any part of the spine/spinal cord may be
affected, although the upper thoracic region is more often involved in endemic
mycotic infections, ie, Coccidioides and Aspergillus, due to contiguous spread
from the lungs. Less commonly, spinal infection may result from hematogenous
dissemination, ie, Candida. Fungal spinal infections may parallel mycobacterial
infections insofar as granulomatous or osteolytic lesions may be seen, although
without relative sparing of posterior elements as may be seen in M. tuberculosis.65
CSF characteristically shows a lymphocytic-predominant pleocytosis,
hypoglycorrhachia, and a significantly elevated protein; opening pressure
is also commonly elevated; testing for b-D-glucan and fungus-specific
antigens/antibodies can also be helpful.
Pseudomycetes/Yeast and Endemic Mycotic Infections
Endemic mycoses are found in specific ecologic/geographic regions and are
dimorphic fungi that form under the influence of environmental factors such
as temperature.
COCCIDIOIDES IMMITIS AND COCCIDIOIDES POSADASII. Coccidioidomycosis is a fungal
infection endemic to the Southwest United States characteristically associated
with pulmonary infection (also known as valley fever); Coccidioides immitis is
found primarily in the San Joaquin Valley in California, while Coccidioides
posadasii is found in the desert regions of Arizona, Utah, New Mexico, and west
Texas, in addition to parts of Mexico, Central America, and South America.
While dissemination is uncommon, when it occurs, at least one-third of cases
are associated with CNS involvement, specifically coccidioidomycosis
meningitis, which presents as chronic meningitis that may be complicated by
460 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
hydrocephalus. Spinal involvement more frequently manifests as osseous KEY POINT
involvement, although myelitis may occur. This is quite often in association
● Coccidioidomycosis is a
with spinal block given the altered CSF dynamics that result from the presence mycotic infection endemic
of thick gelatinous exudate characteristic of fungal infections such as these. to the Southwest
MRI of the spine may demonstrate leptomeningeal enhancement (FIGURE 4-4) United States. Patients
and thickening of the nerve roots; myelitis may be complicated by syrinx with central nervous system
involvement should remain
formation.3
on lifelong antifungal
Coccidioides-specific antigen and antibody testing should be obtained in serum therapy.
and CSF. Treatment consists of azole therapy, eg, fluconazole; if inadequate
response is seen, an alternative azole should be used (eg, voriconazole or
posaconazole), and intrathecal administration of amphotericin B should be
considered.66 Patients with CNS involvement should be maintained on lifelong
antifungal therapy. Although data are lacking, a short course of pulse steroids
may be appropriate for associated cord edema. Neurosurgical intervention
should be considered in cases of associated osteomyelitis, particularly when
evidence of spinal column instability is seen and also in refractory cases requiring
surgical debridement.67
HISTOPLASMA CAPSULATUM. Histoplasma capsulatum is a dimorphic fungus found
in Central and South America, Asia, Africa, and Australia; in the United States, it
is endemic in the Ohio and the Mississippi River valleys of the southeastern,
mid-Atlantic, and central states. H. capsulatum is associated with birds and bats
whose respective excrement accelerates sporulation in the soil (common
reported exposures include bird droppings, caves, and chicken coops).
Extrapulmonary infection is uncommon, but when it occurs, it can disseminate
FIGURE 4-4
Sagittal T2-weighted cervical spine MRI of a patient with coccidioidomycosis meningitis
complicated by myelitis. Images demonstrate cord signal abnormality from approximately C7
through T2 (A) with associated enhancement on postcontrast T1-weighted sequences
(B, arrow).
CONTINUUMJOURNAL.COM 461
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
to the CNS and should be considered in the differential diagnosis of chronic
meningitis and, rarely, myelitis. Extrapulmonary infection has been reported as a
phenomenon compartmentalized to the CNS (leptomeningeal enhancement of
brain and cord).68 Diagnosis can be quite challenging as none of the
pathogen-specific tests are highly sensitive; performing multiple large-volume
lumbar punctures can help increase the diagnostic yield of fungal cultures;
serologic testing should be performed in blood and CSF, in addition to obtaining
a urine antigen test. Recommended treatment for CNS histoplasmosis is
liposomal amphotericin B, followed by itraconazole for at least 1 year and until
normalization of CSF and negative Histoplasma antigen testing.69 As this is the
typical regimen for meningitis, modifications may be needed, such as
incorporating serial imaging into monitoring of disease activity. Voriconazole is
often used clinically as an alternative given its superior CNS penetration in
comparison to itraconazole. Surgery is rarely necessary, although it should be
considered if spinal cord compression is present.
BLASTOMYCES DERMATITIDIS. Blastomyces dermatitidis is a dimorphic fungus found
in soil (often forest soil) in Europe, Africa, Asia, and the Americas; in the
United States, it is endemic in states bordering the Mississippi and Ohio rivers
and the Midwest and southern Canadian provinces bordering the Great Lakes,
with the most cases reported in Wisconsin. Hunters, farmers, and manual
laborers are those most commonly affected. Cutaneous granulomatous disease
is often seen in the form of cutaneous fistulae. As with the other endemic
mycotic infections, most cases are asymptomatic or consist of self-limited
pulmonary infection; however, cases of dissemination to the CNS are seen,
typically in the form of chronic meningitis or brain abscess. Spinal cord
involvement is most frequently described in pediatric and immunocompromised
populations. MRI may demonstrate an isolated intramedullary or extradural
focal blastomycosis lesion in the spinal cord. Serologic testing for B. dermatitidis
should be obtained in both CSF and blood; cross-reactivity may occur with
other endemic mycotic infections, such as histoplasmosis. Surgical resection of
lesions may be indicated.70 Recommended treatment consists of liposomal
amphotericin B followed by a prolonged course of azole therapy (1 year
minimum) with a preference for voriconazole given its good CNS penetration
and reported fluconazole failures.71
Yeasts
Pathogenic yeast associated with spinal cord infection consists primarily of
Cryptococcus species.
CRYPTOCOCCUS NEOFORMANS. Cryptococcus is a yeastlike round fungus found in
soil globally with a pulmonary route of transmission; those with compromised
cell-mediated immunity are more susceptible to infection/disseminated disease,
although individuals who are immunocompetent may be affected. In fact,
Cryptococcus gattii, a newer variant found in Vancouver and the northwestern
United States, preferentially affects individuals who are immunocompetent.
Cryptococcus is a neurotropic fungus and most commonly manifests as a subacute
meningitis or meningoencephalitis, although cases of cryptococcal spinal cord
disease have also been reported, sometimes as vertebral osteomyelitis resulting
in spinal cord syndromes. Clinically, patients can present with a subacute
incomplete transverse myelitis, and MRI is often normal in these cases.72
462 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Cryptococcal antigen (both CSF and blood) is highly sensitive in diagnosis, KEY POINTS
and India ink stain is also helpful; fungal cultures are less sensitive. Treatment
● Histoplasmosis and
consists of liposomal amphotericin B in combination with flucytosine (or blastomycosis are other
fluconazole if flucytosine is unavailable) for 4 to 6 weeks as induction therapy.73 endemic mycotic infections
that may disseminate to the
Nonseptate Mycetes/Yeastlike central nervous system.
These fungi exist primarily as yeast, although they are partly hyphaelike; Azole therapy and liposomal
amphotericin B are used
Candida infection may cause spinal cord pathology.
for treatment.
CANDIDA SPECIES. Candida albicans and other Candida species are larger fungi
● Cryptococcal infection
that often manifest as cerebral abscesses and granulomas. Ischemia may result most commonly occurs in
from occlusion of arterioles. Risk factors include an immunocompromised status individuals who are
and indwelling lines and other medical devices. When present, spinal meningeal immunocompromised,
although it can occur even in
infection is typically associated with osteomyelitis; intradural extramedullary
immunocompetent settings.
lesions secondary to Candida infection have also been reported.74 Treatment Cryptococcal antigen (in
consists of antifungal therapy (ie, amphotericin B with or without flucytosine); both the serum and CSF) is
azoles may also be used. Echinocandins such as caspofungin have suboptimal highly sensitive.
CNS penetration, although they may be included as adjunctive therapy in cases
not responsive to other antifungal treatment. Neurosurgical intervention such as
decompression may also be needed.
MOLDS. The human pathogens in this group are represented by Aspergillus species
(septate mycetes) and zygomycetes such as Mucor species.
ASPERGILLUS SPECIES. Aspergillus is an opportunistic pathogen in individuals with
bone marrow failure, AIDS, chronic granulomatous disease, chronic steroid use,
underlying structural lung disease (and even asthma), and in recipients of
solid organ and hematopoietic transplants. Aspergillus often occurs in association
with chronic paranasal sinusitis. Myelitis is an uncommon manifestation of
disseminated CNS infection.75 Myelopathic syndromes may occur as a result
of compression from granulomata, intramedullary abscess, or from fungal
myelitis. Aspergillus causes a necrotizing myelitis and spinal cord infarction,
which highlights the angioinvasive nature of this fungus; neuropathologic
studies demonstrate nonhemorrhagic infarction. CSF findings are typically
nondiagnostic; pathologic studies may be necessary for confirmation.
Antifungals are the mainstay of treatment, although these infections are
challenging to treat as amphotericin B may not be effective.
ZYGOMYCETES. Mucor species, while more commonly associated with rhinocerebral
disease, have also rarely been reported as causes of infectious myelopathy.76
Risk factors include immunocompromised status, neutropenia, chronic steroid
use, and diabetes mellitus. Antifungals such as amphotericin B are used
for treatment.
Parasitic Infections
Infectious myelopathies associated with parasitic pathogens are more frequently,
although not exclusively, encountered in the tropics.77 CSF eosinophilia or
peripheral eosinophilia may be found in parasitic infections.
TAENIA SOLIUM (NEUROCYSTICERCOSIS). Taenia solium is a cestode parasitic
tapeworm infection that humans can acquire by consuming larvae in undercooked
pork. It is endemic throughout Latin America, parts of Asia (eg, Indonesia,
CONTINUUMJOURNAL.COM 463
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
India, China), Africa, and Eastern Europe (the Balkans). Cases may be seen in
parts of the United States (particularly southern states) due to immigration.
Neurocysticercosis (acquired by ingestion of tapeworm eggs, typically via the
fecal-oral route, and subsequent hematogenous dissemination) is considered to
be the parasitic infection that most frequently involves the CNS. Serologic testing
should be obtained; Western blot enhances specificity as cross-reactivity can
occur with other parasitic infections. Brain imaging may be helpful in identifying
parenchymal (potentially calcified) nodules, which may be asymptomatic
or epileptogenic.
Spinal lesions occur much less commonly and are manifest on spine MRI as
complex enhancing cysts (cystic fluid is isointense to CSF). Leptomeningeal
(extramedullary) cysts occur more frequently than intramedullary lesions, the
latter of which are most often found in the thoracic region. The spinal cord may
appear enlarged; in which case, it may be difficult to distinguish from other mass
lesions such as ependymomas.78 Spinal lesions may be treated with steroids as
well as albendazole; subarachnoid lesions may require surgical removal.79
ECHINOCOCCUS SPECIES. Echinococcus is another cestode tapeworm parasite
transmitted by ingestion of eggs from carrier animal (canines and livestock)
feces or from contaminated food or water; most commonly, infections are caused
by the species Echinococcus granulosus. The liver and lungs are typically affected,
and spinal involvement is quite rare. On MRI, hydatid cysts are characteristically
described as dumbbell-shaped (less frequently spherical) with a hypointense thin
cyst wall on both T1-weighted and T2-weighted imaging, hyperintense cyst
contents, and absent intraluminal debris. Diagnosis is made by histopathologic
confirmation of cyst contents (presence of protoscolices or hydatid membranes);
serologic testing (enzyme-linked immunosorbent assay [ELISA], Western
blot) can additionally support characteristic radiographic findings. Surgery is
recommended for management of hydatid cysts, with care to avoid rupture
(high risk of spread of infection, anaphylaxis to cyst contents), in addition to
albendazole treatment.80
SCHISTOSOMA SPECIES. Schistosomiasis is caused by the parasites platyhelminthes,
which are endemic to South America, the Caribbean, Africa (especially southern
and sub-Saharan and Nile valley regions), the Middle East, and Asia; humans
may be infected while swimming in fresh water when larvae enter the skin. The
most common species associated with spinal cord involvement are Schistosoma
mansoni and Schistosoma haematobium, and manifestations most commonly
include acute transverse myelitis and subacute myeloradiculitis. Spinal MRI may
show enlargement of patchy, masslike multinodular enhancing intramedullary
lesions in the T11 through L1 regions; thickening and enhancement of the
cauda equina and conus medullaris regions may also be seen. Diagnostic
studies include serologic testing and stool studies, although histopathologic
confirmation is required for definitive diagnosis. Treatment consists of oral
praziquantel and steroids; occasionally, surgical debridement may be
necessary, particularly in the event of granuloma formation or if any
medullary compression is present.81
TOXOPLASMA GONDII. Toxoplasma gondii is a protozoan parasite transmitted
via ingestion of oocytes in cat feces or undercooked meat (usually beef or pork
in the United States and Western Europe); pregnant women/fetuses and
464 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
immunocompromised hosts are considered vulnerable populations. T. gondii is, KEY POINTS
in fact, the most common cause of opportunistic intracranial lesions in
● Neurocysticercosis is the
individuals with AIDS. Rarely, toxoplasmosis may also affect the spinal cord and most common parasitic
present as a transverse myelitis, with MRI demonstrating expansive enhancing central nervous system
intramedullary lesions. Serologies and PCR testing in blood and CSF can aid in infection and most
diagnosis, although visualization of bradyzoites or tachyzoites within biopsied commonly manifests as
brain parenchymal lesions,
tissue is necessary for definitive diagnosis. Treatment consists of pyrimethamine,
although cystic lesions may
sulfadiazine, and leucovorin. A suspected case of IRIS was reported in an be seen in the spine and are
individual with AIDS who experienced paradoxical worsening symptoms more commonly located
posttreatment for myelopathy (and myopathy) secondary to T. extramedullary than
intramedullary.
gondii infection.82
● The most common species
PLASMODIUM SPECIES (MALARIA). Plasmodium species belong to the Apicomplexa
of Schistosoma associated
protozoal group; infection is transmitted via mosquito bites. Plasmodium with spinal cord involvement
falciparum is the species most frequently implicated in symptomatic malarial are Schistosoma mansoni and
cases, followed by Plasmodium vivax. The largest burden of disease is in Africa, Schistosoma haematobium,
and manifestations most
although malaria is also found throughout Southeast Asia and parts of Central
commonly include acute
America and South America. Cerebral malaria is the most common CNS transverse myelitis and
manifestation; immunologically mediated acute disseminated encephalomyelitis subacute myeloradiculitis.
(ADEM) has also been reported following malarial infection. Rare case reports
exist of suspected infectious myelitis due to P. falciparum, P. vivax, or mixed ● Toxoplasmosis is the
most common cause of
infection; resolution of initial presenting malarial fever following antiparasitic opportunistic intracranial
therapy lends support to malarial infection as a putative direct cause rather lesions in patients with
than an immune-mediated pathology. MRI demonstrates hyperintense T2 human immunodeficiency
spinal cord lesions preferentially involving the dorsal columns.83 Diagnostic virus and acquired
immunodeficiency
studies include peripheral thick blood smears to evaluate for parasitemia as syndrome, although
well as rapid antigen and antibody detection tests. Treatment consists of a toxoplasmosis may rarely
combination of corticosteroids and antimalarial therapy (typically quinine manifest as myelitis
based). In most of these cases, complete recovery was reported with a corresponding
centromedullary pattern of
following treatment.
abnormality on spinal cord
imaging.
GNATHOSTOMA SPINIGERUM. Gnathostoma spinigerum is a helminthic parasite
endemic in Asia and Latin America (although almost all neurologic cases are
reported in Thailand) and is acquired by consumption of undercooked food
(eg, raw fish, frogs, or poultry) containing larvae. While the disease is typically
gastroenterologic and cutaneous, when neurologic spread occurs, the spinal cord
is the most frequently affected site. In neurognathostomiasis involving the spinal
cord, MRI demonstrates multisegmental T2 hyperintensity within the cord with
associated edema involving cervical and thoracic regions and mild postcontrast
enhancement. Additionally, conus medullaris involvement (conus enlargement on
imaging with clinical correlate of radicular pain) was reported in almost half of
patients in a case series.84 Lesions were of varying extension, although at least one
longitudinally extensive lesion extended from C2 to the conus medullaris. Several
were reported as having normal spinal cord imaging. Brain imaging may show
intracranial hemorrhage, and CSF xanthochromia has been commonly described
in addition to eosinophilic pleocytosis.84,85 Serum antibody testing is used for
diagnosis. Albendazole has been used concomitantly with corticosteroids for
treatment, although efficacy remains unclear.
TOXOCARA CANIS.Toxocara canis is a roundworm typically found in dogs.
Humans may be infected via consumption of dog feces–contaminated produce
CONTINUUMJOURNAL.COM 465
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
or contaminated meat (eg, rabbit, pork, beef, poultry). CNS involvement of
T. canis is rare, but when it occurs, may manifest as a subacute or chronic,
relapsing-remitting, or progressive myelitis. MRI typically demonstrates a single
lesion with fusiform enlargement with a smaller area of nodular enhancement
(in posterior horns, usually posteromarginal nucleus) on postcontrast sequences.
T. canis serologies should be obtained in blood and CSF; accompanying
eosinophilia may also be seen (more commonly in blood than CSF). Treatment
consists of albendazole with or without steroids (one case series reported that no
TABLE 4-4 Geographic Distribution and Transmission for Selected Pathogens
Associated With Infectious Myelopathya
Pathogen Geography Transmission
Bacteria
Borrelia burgdorferi United States (New England, Atlantic Tick-borne: Ixodes species (eg, Ixodes
coast, northern Midwest, Pacific scapularis, Ixodes pacificus)
Northwest), Europe
Borrelia garinii Europe Tick-borne: Ixodes species (eg, Ixodes ricinus)
Brucella species Middle East, Mediterranean, Latin Hosts include cattle and goats, risks with
America, Western Asia related occupations and consumption of
unpasteurized milk from infected animals
Viruses
West Nile virus United States, Europe, Middle East, Mosquito-borne; Culex species (eg, Aedes
Africa, Western Asia aegypti, Aedes albopictus)
Poliovirus Nigeria, Pakistan, Afghanistan Fecal-oral transmission; areas of poor
sanitation, limited vaccine availability
Japanese encephalitis virus Asia, Western Pacific Mosquito-borne: Culex species (eg, Culex
tritaeniorhynchus)
Tick-borne encephalitis virus Europe, former Soviet Union, Asia Tick-borne: Ixodes species; also risk with
consumption of unpasteurized milk from
infected animals
Zika virus Central America, South America, Mosquito-borne: Culex species, eg, A.
Caribbean, Pacific Islands, Asia, Africa aegypti, A. albopictus; also congenital
infection and sexual transmission
Human T-cell lymphotropic Caribbean, South America, Africa, Vertical transmission (eg, breast-feeding),
virus type I Japan sexual transmission, blood exposure (eg,
blood transfusion, shared needles)
CONTINUED ON PAGE 467
466 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
patients improved with steroids until antihelminthic therapy was initiated)
and is associated with good recovery.86
OTHER. Other parasitic pathogens that have been rarely associated with spinal
cord infection include Strongyloides stercoralis,87 Paragonimus (manifests as
intraspinal extradural granuloma),88 and Angiostrongylus cantonensis.89
TABLE 4-4
90,91
summarizes the geographic distribution and transmission for
selected pathogens associated with infectious myelopathy, and TABLE 4-592,93
CONTINUED FROM PAGE 466
Pathogen Geography Transmission
Fungi
Coccidioides immitis, United States (Southwest, recently Inhalation of spores (dust exposure)
Coccidioides posadasii south-central Washington), Mexico,
Central America, South America
Histoplasma capsulatum United States (central and eastern, Inhalation of spores, especially soil containing
especially Ohio and Mississippi River bird, bat droppings; other exposures in caves,
valleys), Central America, South chicken coops
America, Asia, Africa, and Australia
Blastomyces dermatitidis United States (Ohio and Mississippi Inhalation of spores (moist soil,
River valleys, Midwest, Great Lakes decomposing matter)
region especially Wisconsin), southern
Canadian provinces, Europe, Africa, Asia
Parasites
Taenia solium Latin America, Asia (eg, Indonesia, Tapeworm egg ingestion, typically via
India, China), Africa, and Eastern fecal-oral route
Europe (the Balkans), United States
(states with immigrants from endemic
areas)
Echinococcus granulosus Africa, Europe, Asia, Middle East, Tapeworm infection transmitted by ingestion
Central America, South America, of eggs from carrier animal (canines and
Canada, United States (Alaska, cases livestock) feces or from contaminated food or
in Arizona and New Mexico in water; uncontrolled livestock slaughter,
sheep-raising areas; immigrants poor sanitation
from endemic areas)
Schistosoma mansoni, South America, Africa (southern and Skin contact when swimming in contaminated
Schistosoma haematobium sub-Saharan, Nile River valley), Middle fresh water
East, Caribbean (low risk)
Plasmodium species Africa, Southeast Asia, Central Mosquito-borne: Anopheles species
America, South America
Gnathostoma spinigerum Latin America, Asia (most neurologic Consumption of undercooked contaminated
cases reported in Thailand) foods (eg, fish, frogs, poultry)
a
Data from the Centers for Disease Control and Prevention, cdc.gov,90 and the World Health Organization, who.int/en.91
CONTINUUMJOURNAL.COM 467
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
TABLE 4-5 Pathogen-Specific Infectious Myelopathy Treatmenta
Pathogen Treatment
Bacteria
Pyogenic Empiric antibiotics: third- or fourth-generation cephalosporin (ie, ceftriaxone), plus
vancomycin; specific antibiotics dictated by culture results
Mycobacterium tuberculosis Four-drug regimen (rifampin, isoniazid, pyrazinamide, ethambutol) for 2 months,
two-drug regimen (isoniazid, rifampin) for 7–10 additional months minimum; plus
high-dose corticosteroids
Borrelia species IV ceftriaxone (2 g/d) or IV penicillin G (18–24 million units IV daily divided over every
4 hours) or IV cefotaxime (2 g every 8 hours) for 14–28 days;11 oral doxycycline may be an
alternative (European studies)
Treponema pallidum IV penicillin G (18–24 million units daily administered as 3–4 million units every 4 hours or
continuous infusion) for 10–14 days; with or without steroids
Brucella species IV ceftriaxone 2 g/d IV in combination with rifampin 600 mg orally once daily and doxycycline
100 mg orally twice daily; consider adjunctive short course of high-dose steroids
Mycoplasma pneumoniae Doxycycline 100 mg orally twice daily for 10–14 days (erythromycin, azithromycin,
clarithromycin, levofloxacin, moxifloxacin are alternatives; tetracyclines and
quinolones preferred for superior central nervous system penetration); plus
adjunctive steroids; consider additional immunotherapy
Viruses
Herpes simplex virus types 1 and 2 IV acyclovir 10 mg/kg every 8 hours for minimum of 7 days (longer if
immunocompromised92); consider adjunctive steroids
Varicella-zoster virus IV acyclovir 10 mg/kg every 8 hours for minimum of 7 days (longer if
immunocompromised92); consider adjunctive steroids (oral prednisone, 1 mg/kg/d for
5 days without taper, recommended in setting of varicella-zoster virus vasculopathy)
Epstein-Barr virus IV acyclovir or ganciclovir (data lacking for benefit); steroids
Cytomegalovirus IV ganciclovir 5 mg/kg every 12 hours for induction, followed by 5 mg/kg every 24 hours
for maintenance92; or valganciclovir
Human herpesvirus 6 IV ganciclovir or foscarnet
Human herpesvirus 7 IV foscarnet
Poliovirus Supportive care
Enterovirus 71 Supportive care; consider IV immunoglobulin (IVIg)
Enterovirus D68 Supportive care; consider IVIg, steroids, plasma exchange
West Nile virus Supportive care; consider IVIg, interferon-alfa (data lacking for benefit)
Japanese encephalitis virus Supportive care
Tick-borne encephalitis virus Supportive care
Dengue virus Supportive care; consider adjunctive steroids (in parainfectious setting93)
Zika virus Supportive care, consider steroids
CONTINUED ON PAGE 469
468 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
CONTINUED FROM PAGE 468
Pathogen Treatment
Hepatitis C Steroids; consider IVIg, antiviral medications (not helpful acutely but may have
long-term benefit in reducing relapses)
Human immunodeficiency virus (HIV) Antiretroviral treatment; adjunctive steroids in setting of acute HIV infection
Human T-cell lymphotropic virus Supportive care; consider steroids; consider interferon-alfa (data lacking for benefit)
types I and II (HTLV-I/II)
Rabies virus Supportive care; consider Milwaukee protocol (therapeutic coma with ketamine,
ribavirin, and amantadine), although controversial (and of questionable efficacy)58
Fungi
Coccidioides immitis, Coccidioides Fluconazole (minimum of 400–800 mg/d, recommend starting at 800 mg IVb);
posadasii alternative azole (eg, voriconazole, posaconazole) with or without intrathecal or IV
amphotericin B if inadequate response; consider short course of adjunctive steroids
Histoplasma capsulatum Liposomal amphotericin B (5.0 mg/kg/d for a total of 175 mg/kg given over 4–6 weeks),
followed by itraconazole (200 mg 2–3 times daily) for 1 year minimum and until
normalization of CSF and negative Histoplasma antigen testing
Blastomyces dermatitidis Liposomal amphotericin B for 4–6 weeks, followed by azole (preferably voriconazole)
therapy for 1 year minimum
Cryptococcus neoformans Liposomal amphotericin B plus flucytosine (or fluconazole as alternative) for 4–6 weeks
as induction therapy
Aspergillus species Liposomal amphotericin B
Candida species Liposomal amphotericin B with or without flucytosine; voriconazole; consider
caspofungin as adjunctive therapy although suboptimal central nervous
system penetration
Parasites
Taenia solium Albendazole, adjunctive steroids
Echinococcus species Albendazole, surgical removal of hydatid cysts
Schistosoma species Praziquantel 60 mg/kg divided in 3 doses for 1 day with adjunctive steroids
(prednisone 60–80 mg/d, taper over 6 months) (controversial and no formal
guidelines92); possible surgical intervention
Toxoplasma gondii Pyrimethamine, sulfadiazine, and leucovorin
Plasmodium species Steroids plus quinine-based antimalarial drugs
Gnathostoma spinigerum Albendazole plus steroids
CSF = cerebrospinal fluid; IV = Intravenous.
a
Formal guidelines are lacking for the majority of pathogen-specific infectious myelopathies; therefore, treatment is often extrapolated from
antimicrobial recommendations for nonmyelitis cases and case reports in the literature.
b
This author advocates using no less than 800 mg once daily for the initial treatment of coccidioidal meningitis.
CONTINUUMJOURNAL.COM 469
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
provides a summary of the treatments of the major pathogens associated with
infectious myelopathy.
CONCLUSION
A variety of bacterial, viral, fungal, and parasitic pathogens can be associated with
infectious myelopathies, either via direct infection or via an infection-triggered
immune-mediated response. Host factors including immune status and
geographic and occupational exposures, time course, and CSF profiles should be
considered when approaching the differential diagnosis. Neuroimaging patterns
of abnormality can also be helpful in the diagnostic approach, although
sometimes MRI may be normal, therein underscoring the importance of
maintaining a high index of suspicion in patients presenting with a clinical
syndrome consistent with myelopathy. The general treatment approach includes
use of targeted antimicrobial therapy when available and indicated, with or
without adjunctive corticosteroids; use of other immunotherapies if a
postinfectious autoimmune-mediated process is suspected; and neurosurgical
intervention in certain settings such as cord compression.
REFERENCES
1 Roos KL. Bacterial infections of the central 9 Case records of the Massachusetts General
nervous system. Continuum (Minneap Minn) Hospital. Weekly clinicopathological exercises.
2015;21(6 Neuroinfectious Disease):1679–1691. Case 33–2001. A 33-year-old man with a rash,
doi: 10.1212/CON.0000000000000242. pulmonary infection, and neurologic disorder.
N Engl J Med 2001;345(17):1263–1269. doi:10.
2 Tali ET, Oner AY, Koc AM. Pyogenic spinal
1056/NEJMcpc332001.
infections. Neuroimaging Clin N Am 2015;25(2):
193–208. doi:10.1016/j.nic.2015.01.003. 10 Halperin JJ. Neuroborreliosis. J Neurol 2017;
264(6):1292–1297. doi:10.1007/s00415-016-8346-2.
3 Talbott J, Narvid J, Chazen J, et al. An
imaging-based approach to spinal cord 11 Charles V, Duprez TP, Kabamba B, et al.
infection. Semin Ultrasound CT MR 2016;37(5): Poliomyelitis-like syndrome with matching
411–430. doi:10.1053/j.sult.2016.05.006. magnetic resonance features in a case of Lyme
4 Yoon SH, Chung SK, Kim KJ, et al. Pyogenic neuroborreliosis. BMJ Case Rep 2009;2009. pii:
vertebral osteomyelitis: identification of bcr07.2008.0527. doi:10.1136/bcr.07.2008.0527.
microorganism and laboratory markers used to 12 Halperin JJ, Shapiro ED, Logigian E, et al. Practice
predict clinical outcome. Eur Spine J 2010;19(4): parameter: treatment of nervous system Lyme
575–582. doi:10.1007/s00586-009-1216-1. disease (an evidence based review): report of
5 Kastenbaer S, Winkler F, Fesl G, et al. Acute the Quality Standards Subcommittee of the
severe spinal cord dysfunction in bacterial American Academy of Neurology. Neurology
meningitis in adults: MRI findings suggest 2007;69(1):91–102. doi:10.1212/01.wnl.0000265517.
extensive myelitis. Arch Neurol 2001;58(5): 66976.28.
806–810. doi:10.1001/archneur.58.5.806. 13 Bremell D, Dotevall L. Oral doxycycline for Lyme
6 Garg RK, Malhotra HS, Gupta R. Spinal cord neuroborreliosis with symptoms of encephalitis,
involvement in tuberculous meningitis. Spinal myelitis, vasculitis or intracranial hypertension.
Cord 2015;53(9):649–657. doi:10.1038/sc.2015.58. Eur J Neurol 2014;21(9):1162–1167. doi:10.1111/
ene.12420.
7 Takahashi T, Tamura M, Takasu T. The PCR-based
diagnosis of central nervous system tuberculosis: 14 He D, Jiang B. Syphilitic myelitis: magnetic
up to date. Tuberc Res Treat 2012;2012:831292. resonance imaging features. Neurol India 2014;
doi:10.1155/2012/831292. 62(1):89–91. doi:10.4103/0028-3886.128347.
8 Nahid P, Dorman SE, Alipanah N, et al. Official 15 Marra CM, Maxwell CL, Smith SL, et al.
American Thoracic Society/Centers for Disease Cerebrospinal fluid abnormalities in patients with
Control and Prevention/Infectious Diseases Society syphilis: association with clinical and laboratory
of America Clinical Practice Guidelines: treatment of features. J Infect Dis 2004;189(3):369–376.
drug-susceptible tuberculosis. Clin Infect Dis 2016;63 doi:10.1086/381227.
(7):e147–e195. doi:10.1093/cid/ciw376.
470 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
16 Workowski KA, Berman S; Centers for Disease 31 Sanefuji M, Ohga S, Kira R, et al. Epstein-Barr
Control and Prevention (CDC). Sexually virus-associated meningoencephalomyelitis:
transmitted diseases treatment guidelines, intrathecal reactivation of the virus in an
2010. MMWR Recomm Rep 2010;59(RR-12):1–110. immunocompetent child. J Child Neurol 2008;
23(9):1072–1077. doi:10.1177/0883073808315414.
17 Chilver-Stainer L, Fischer U, Hauf M, et al.
Syphilitic myelitis: rare, nonspecific, but 32 Tselis AC. Cytomegalovirus infections of the
treatable. Neurology 2009;72(7):673–675. adult human nervous system. Handb Clin
doi:10.1212/01.wnl.0000342460.07764.5c. Neurol 2014;123:307–318. doi:10.1016/
B978-0-444-53488-0.00014-6.
18 Onder H, Gocmen R, Inkaya AC, et al. A rare case
of longitudinal Brucella myelitis. Spine J 2015;15 33 Miyashita N, Endo T, Onozawa M, et al. Risk
(7):1689–1690. doi:10.1016/j.spinee.2015.03.002. factors of human herpesvirus 6 encephalitis/
myelitis after allogeneic hematopoietic stem cell
19 Krishnan C, Kaplin AI, Graber JS, et al. Recurrent
transplantation. Transpl Infect Dis 2017;19(3).
transverse myelitis following neurobrucellosis:
doi:10.1111/tid.12682.
immunologic features and beneficial response
to immunosuppression. J Neurovirol 2005;11(2): 34 Escobar-Villalba A, Sainz dela Maza S, Pérez
225–231. doi:10.1080/13550280590922801. Torre P, et al. Acute myelitis by human herpes
virus 7 in an HIV-infected patient. J Clin Virol
20 Guven T, Ugurlu K, Ergonul O, et al.
2016;77:63–65. doi:10.1016/j.jcv.2016.02.001.
Neurobrucellosis: clinical and diagnostic
features. Clin Infect Dis 2013;56(10):1407–1412. 35 Ward KN, White RP, Mackinnon S, Hanna M.
doi:10.1093/cid/cit072. Human herpesvirus-7 infection of the CNS with
acute myelitis in an adult bone marrow recipient.
21 Tsiodras S, Kelsidis T, Kelesidis I, et al.
Bone Marrow Transplant 2002;30(12):983–985.
Mycoplasma pneumoniae-associated myelitis: a
doi:10.1038/sj.bmt.1703774.
comprehensive review. Eur J Neurol 2006;13(2):
112–124. doi:10.1111/j.1468-1331.2006.01174.x. 36 Kidd D, Williams AJ, Howard RS. Poliomyelitis.
Postgrad Med J 1996;72(853):641–647.
22 Nandasiri S, Wimalaratna H, Manjula M, Corea E.
Transverse myelitis secondary to melioidosis: 37 Palacios G, Oberste MS. Enteroviruses as agents
a case report. BMC Infect Dis 2012;12:232. of emerging infectious diseases. J Neurovirol
doi:10.1186/1471-2334-12-232. 2005;11(5):424–433. doi:10.1080/13550280591002531.
23 Schröter A, Brinkhoff J, Günthner-Lengsfeld T, et al. 38 Lee HF, Chi CS. Enterovirus 71 infection-associated
Whipple's disease presenting as an isolated lesion acute flaccid paralysis: a case series of long-term
of the cervical spinal cord. Eur J Neurol 2005;12(4): neurologic follow-up. J Child Neurol 2014;29(10):
276–279. doi:10.1111/j.1468-1331.2004.01035.x. 1283–1290. doi:10.1177/0883073813516193.
24 Mihai C, Jubelt B. Infectious myelitis. Curr Neurol 39 Messacar K, Schreiner TL, Maloney JA, et al.
Neurosci Rep 2012;12(6):633–641. doi:10.1007/ A cluster of acute flaccid paralysis and cranial
s11910-012-0306-3. nerve dysfunction temporally associated with
an outbreak of enterovirus D68 in children
25 Savoldi F, Kaufmann TJ, Flanagan EP, et al. Elsberg in Colorado, USA. Lancet 2015;385(9978):
syndrome: a rarely recognized cause of cauda 1662–1671. doi:10.1016/S0140-6736(14)62457-0.
equina syndrome and lower thoracic myelitis.
Neurol Neuroimmunol Neuroinflamm 2017; 40 Davis LE, DeBiasi R, Goade DE, et al. West Nile
4(4):e355. doi:10.1212/NXI.0000000000000355. virus neuroinvasive disease. Ann Neurol 2006;
60(3):286–300. doi:10.1002/ana.20959.
26 Kusuhara T, Nakajima M, Inoue H, et al.
41 Sejvar JJ. Clinical manifestations and outcomes
Parainfectious encephalomyeloradiculitis
of West Nile virus infection. Viruses 2014;6(2):
associated with herpes simplex virus 1 DNA in
606–623 doi:10.3390/v6020606.
cerebrospinal fluid. Clin Infect Dis 2002;34(9):
1199–1205. doi:10.1086/339811. 42 Yango AF, Fischbach BV, Levy M, et al. West
Nile virus infection in kidney and pancreas
27 Nakajima H, Furutama D, Kimura F, et al. Herpes
transplant recipients in the Dallas-Fort Worth
simplex virus myelitis: clinical manifestations
Metroplex during the 2012 Texas epidemic.
and diagnosis by the polymerase chain reaction
Transplantation 2014;97(9):953–957. doi:
method. Eur Neurol 1998;39(3):163–167.
10.1097/01.TP.0000438621.81686.ab.
28 Berger J, Houff S. Neurological complications of
43 Venkat H, Krow-Lucal E, Hennessey M, et al.
herpes simplex virus type 2 infection. Arch Neurol
Concurrent outbreaks of St. Louis encephalitis virus
2008;65(5):596–600. doi:10.1001/archneur.65.5.596.
and West Nile virus disease – Arizona, 2015. MMWR
29 Nagel MA, Gilden D. Neurological complications Morb Mortal Wkly Rep 2015;64(48):1349–1350.
of varicella zoster virus reactivation. Curr Opin doi:10.15585/mmwr.mm6448a5.
Neurol 2014;27(3):356–360 doi:10.1097/
44 Solomon T, Kneen R, Dung NM, et al.
WCO.0000000000000092.
Poliomyelitis-like illness due to Japanese
30 Majid A, Galetta SL, Sweeney CJ, et al. encephalitis virus. Lancet 1998;351(9109):
Epstein-Barr virus myeloradiculitis and 1094–1097. doi:10.1016/
encephalomyeloradiculitis. Brain 2002;125(pt 1): S0140-6736(97)07509-0.
159–165.
CONTINUUMJOURNAL.COM 471
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
INFECTIOUS MYELOPATHIES
45 Verma R, Praharai HN, Patil TB, Giri P. Acute 59 Chonmaitree P, Methawasin K. Transverse
transverse myelitis following Japanese myelitis in acute hepatitis A infection: the rare
encephalitis viral infection: an uncommon co-occurrence of hepatology and neurology.
complication of a common disease. BMJ Case Rep Gastroenterol 2016;10(1):44–49.
Case Rep 2012;2012. pii:bcr2012007094. doi:10.1159/000444013.
doi:10.1136/bcr-2012-007094.
60 Sarkar P, Morgan C, Ijaz S. Transverse myelitis
46 Zambito Marsala S, Francavilla E, Gioulis M, et al. caused by hepatitis E: previously undescribed
Isolated polio-like syndrome after tick-borne in adults. BMJ Case Rep 2015;2015. pii:
encephalitis presenting with acute hyperckemia. bcr2014209031. doi:10.1136/bcr-2014-209031.
Neurol Sci 2012;33(3):669–672. doi:10.1007/
61 Xia JB, Zhu J, Hu J, et al. H7N9 influenza A-induced
s10072-011-0834-7.
pneumonia associated with acute myelitis in an
47 Mota MT, Estofolete CF, Zini N, et al. Transverse adult. Intern Med 2014;53(10):1093–1095.
myelitis as an unusual complication of dengue
fever. Am J Trop Med Hyg 2017;96(2):380–381. 62 van der Heijden LB, Janse AJ. Transverse myelitis
doi:10.4269/ajtmh.16-0284. in measles. Pediatr Neurol 2015;52(1):132.
doi:10.1016/j.pediatrneurol.2014.09.018.
48 Araujo AQ, Silva MT, Araujo AP. Zika virus-associated
neurological disorders: a review. Brain 2016;139 63 Savaş L, Arlier Z, Akçali A, et al. Full recovered
(pt 8):2122–2130. doi:10.1093/brain/aww158. meningoencephalomyelitis caused by mumps
virus. Eur J Neurol 2004;11(9):639–640.
49 Mécharles S, Herrmann C, Poullain P, et al.
Acute myelitis due to Zika virus infection. 64 Stich O, Herpers M, Keil A, et al. JC virus myelitis
Lancet 2016;387(10026):1481. doi:10.1016/ without cerebral involvement in acute myeloid
S0140-6736(16)00644-9. leukemia. Eur J Neurol 2011;18(11):e143–e144.
doi:10.1111/j.1468-1331.2011.03480.x.
50 Suzuki K, Takao M, Katayama Y, Mihara B.
Acute myelitis associated with HCV infection. 65 Raman Sharma R. Fungal infections of the
BMJ Case Rep 2013;2013. pii:bcr2013008934. nervous system: current perspective and
doi:10.1136/bcr-2013-008934. controversies in management. Int J Surg 2010;
8(8):591–601. doi:10.1016/j.ijsu.2010.07.293.
51 Stübgen JP. Immune-mediated myelitis
associated with hepatitis virus infections. 66 Galgiani JN, Ampel NM, Blair JE, et al. Executive
J Neuroimmunol 2011;239(1–2):21–27. doi:10.1016/ Summary: 2016 Infectious Diseases Society of
j.jneuroim.2011.09.001. America (IDSA) Clinical Practice Guideline for
the Treatment of Coccidioidomycosis. Clin
52 Di Rocco A. Diseases of the spinal cord in human Infect Dis 2016;63(6):717–722. doi:10.1093/cid/
immunodeficiency virus infection. Semin Neurol ciw538.
1999;19(2):151–155. doi:10.1055/s-2008-1040832.
67 Kakarla UK, Kalani MY, Sharma GK, et al. Surgical
53 Andrade P, Figueiredo C, Carvalho C, et al. management of coccidioidomycosis of the
Transverse myelitis and acute HIV infection: a spine: clinical article. J Neurosurg Spine 2011;
case report. BMC Infect Dis 2014;14:149. 15(4):441–446. doi:10.3171/2011.5.SPINE10596.
doi:10.1186/1471-2334-14-149.
68 Eid AJ, Leever JD, Husmann K. Compartmentalized
54 Recommendations for counseling persons Histoplasma capsulatum infection of the central
infected with human T-lymphotrophic virus, types I nervous system. Case Rep Infect Dis 2015;2015:
and II. Centers for Disease Control and Prevention 581415. doi:10.1155/2015/581415.
and U.S. Public Health Service Working Group.
MMWR Recomm Rep 1993;42(RR-9):1–13. 69 Wheat LJ, Musial CE, Jenny-Avital E. Diagnosis
and management of central nervous system
55 Coler-Reilly ALG, Sato T, Matsuzaki T, et al. histoplasmosis. Clin Infect Dis 2005;40(6):
Effectiveness of daily prednisolone to slow 844–852. doi:10.1086/427880.
progression of human T-lymphotropic virus type
1-associated myelopathy/tropical spastic 70 Parr AM, Fewer D. Intramedullary blastomycosis
paraparesis: a multicenter retrospective cohort in a child: case report. Can J Neurol Sci 2004;
study. Neurotherapeutics 2017. doi:10.1007/ 31(2):282–285.
s13311-017-0533-z.
71 Bariola JR, Perry P, Pappas PG, et al.
56 Buell KG, Puri A, Demontis MA, et al. Effect of Blastomycosis of the central nervous system: a
pulsed methylprednisolone on pain, in patients multicenter review of diagnosis and treatment in
with HTLV-1-associated myelopathy. PLoS One the modern era. Clin Infect Dis 2010;50(6):
2016;11(4):e0152557. doi:10.1371/journal. 797–804. doi:10.1086/650579.
pone.0152557.
72 Gumbo T, Hakim JG, Mielke J, et al. Cryptococcus
57 Vaish AK, Jain N, Gupta LK, Verma SK. Atypical myelitis: atypical presentation of a common
rabies with MRI findings: clue to the diagnosis. infection. Clin Infect Dis 2001;32(8):1235–1236.
BMJ Case Rep 2011;2011. pii:bcr0520114234. doi:10.1086/319749.
doi:10.1136/bcr.05.2011.4234.
73 Mitchell TG, Perfect JR. Cryptococcosis in the
58 Jackson AC. Human rabies: a 2016 update. Curr era of AIDS—100 years after the discovery of
Infect Dis Rep 2016;18(11):38. doi:10.1007/s11908- Cryptococcus neoformans. Clin Mircobiol Rev
016-0540-y. 1995;8(4):515–548.
472 APRIL 2018
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
74 Merwick Á, Minhas Z, Curtis C, et al. Intradural 84 Kanpittaya J, Sawanyawisuth K, Intapan PM, et al.
extramedullary spinal candida infection. Pract A comparative study of neuroimaging features
Neurol 2015;15(5):400–404. doi:10.1136/ between human neuro-gnathostomiasis and
practneurol-2014-001052. angiostrongyliasis. Neurol Sci 2012;33(4):
893–898. doi:10.1007/s10072-011-0864-1.
75 Kleinschmidt-DeMasters BK. Central nervous
system aspergillosis: a 20-year retrospective 85 Katchanov J, Sawanyawisuth K, Chotmongkoi V,
series. Hum Pathol 2002;33(1):116–124. et al. Neurognathostomiasis, a neglected
parasitosis of the central nervous system. Emerg
76 Suzuki G, Kurosawa M, Takanashi Y, et al. Infect Dis 2011;17(7):1174–1180. doi:10.3201/
Transverse lesion of the spinal cord due to eid1707.101433.
mucormycosis in an AML patient [in Japanese].
Rinsho Ketsueki 1996;37(8):694–700. 86 Jabbour RA, Kanj SS, Sawaya RA, et al. Toxocara
canis myelitis: clinical features, magnetic
77 Román GC. Tropical myelopathies. Handb Clin resonance imaging (MRI) findings, and treatment
Neurol 2014;121:1521–1548. doi:10.1016/ outcome in 17 patients. Medicine (Baltimore)
B978-0-7020-4088-7.00102-4. 2011;90(5):337–343. doi:10.1097/MD.
0b013e31822f63fb.
78 García HH, Del Brutto OH. Imaging findings
in neurocysticercosis. Acta Trop 2003;87(1): 87 Hénon H, Vermersch P, Dutoit E, et al.
71–78. Strongyloides stercoralis myelitis [in French].
Rev Neurol (Paris) 1995;151(2):139–141.
79 Hernández RD, Durán BB, Lujambio PS. Magnetic
resonance imaging in neurocysticercosis. 88 Qin Y, Cai J. MRI findings of intraspinal extradural
Top Magn Reson Imaging 2014;23(3):191–198. paragonimiasis granuloma in a child. Pediatr
doi:10.1097/RMR.0000000000000026. Radiol 2012;42(10):1250–1253. doi:10.1007/
s00247-012-2408-0.
80 Secer HI, Anik I, Celik E, et al. Spinal hydatid
cyst mimicking arachnoid cyst on magnetic 89 Al Hammoud R, Nayes SL, Murphy JR, et al.
resonance imaging. J Spinal Cord Med Angiostrongylus cantonensis meningitis and
2008;31(1):106–108. doi:10.1080/ myelitis, Texas, USA. Emerg Infect Dis 2017;23(6):
10790268.2008.11753990. 1037–1038. doi:10.3201/eid2306.161683.
81 Ross AG, McManus DP, Farrar J, et al. 90 Centers for Disease Control and Prevention.
Neuroschistosomiasis. J Neurol 2012;259(1): cdc.gov. Accessed January 4, 2018.
22–32. doi:10.1007/s00415-011-6133-7. 91 World Health Organization. who.int/en.
82 Kung DH, Hubenthal EA, Kwan JY, et al. Accessed January 4, 2018.
Toxoplasmosis myelopathy and myopathy 92 Auwaeter P. Myelitis. Johns Hopkins ABX Guide.
in an AIDS patient: a case of immune hopkinsguides.com/hopkins/view/Johns_
reconstitution inflammatory syndrome? Hopkins_ABX_Guide/540374/all/Myelitis.
Neurologist 2011;17(1):49–51. doi:10.1097/ Accessed January 4, 2018.
NRL.0b013e3181d35c62.
93 de Sousa AM, Alvarenga MP, Alvarenga RM. A
83 Moulick A, Maitra S, Sarkar BS, et al. Vivax malaria cluster of transverse myelitis following dengue
presenting with myelitis: a rare complication. virus infection in the Brazilian Amazon region.
J Clin Diagn Res 2013;7(5):914–916. doi:10.7860/ Trop Med Health 2014;42(3):115–120. doi:10.2149/
JCDR/2013/5251.2974. tmh.2014-06.
CONTINUUMJOURNAL.COM 473
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- s40136-022-00431-4Dokument10 Seitens40136-022-00431-4night.shadowNoch keine Bewertungen
- Pediatric Central NervousDokument22 SeitenPediatric Central Nervousnight.shadowNoch keine Bewertungen
- Clinically Isolated Syndrome and Early Relapsing Multiple SclerosisDokument19 SeitenClinically Isolated Syndrome and Early Relapsing Multiple Sclerosisnight.shadowNoch keine Bewertungen
- EEG in Epilepsy EvaluationDokument23 SeitenEEG in Epilepsy Evaluationnight.shadowNoch keine Bewertungen
- Multiple Sclerosis Risk Factors and Pathogenesis PDFDokument15 SeitenMultiple Sclerosis Risk Factors and Pathogenesis PDFnight.shadowNoch keine Bewertungen
- Epilepsy Emergencies - Status Epilepticus, Acute Repetitite Seizures, and Autoimmune EncephalitisDokument23 SeitenEpilepsy Emergencies - Status Epilepticus, Acute Repetitite Seizures, and Autoimmune Encephalitisnight.shadowNoch keine Bewertungen
- Management of Multiple SclerosisDokument15 SeitenManagement of Multiple Sclerosisnight.shadowNoch keine Bewertungen
- Monitoring, Switching, and Stopping Multiple Sclerosis Disease-Modifying TherapiesDokument21 SeitenMonitoring, Switching, and Stopping Multiple Sclerosis Disease-Modifying Therapiesnight.shadowNoch keine Bewertungen
- Neuromyelitis Optica Spectrum DIsorder and Other Non-Multiple Sclerosis Central Nervous System Inflammatory DIseasesDokument30 SeitenNeuromyelitis Optica Spectrum DIsorder and Other Non-Multiple Sclerosis Central Nervous System Inflammatory DIseasesnight.shadow100% (1)
- Management - ComorbiditiesDokument20 SeitenManagement - Comorbiditiesnight.shadowNoch keine Bewertungen
- Highly Agressive Multiple Sclerosis PDFDokument26 SeitenHighly Agressive Multiple Sclerosis PDFnight.shadowNoch keine Bewertungen
- Diagnosis, Differential Diagnosis, And.5Dokument25 SeitenDiagnosis, Differential Diagnosis, And.5Rahul RaiNoch keine Bewertungen
- Counseling and Management of The RIskis of Living With EpilepsyDokument15 SeitenCounseling and Management of The RIskis of Living With Epilepsynight.shadowNoch keine Bewertungen
- Epilepsy Overview and Revised Classification of Seizures and Epilepsies PDFDokument16 SeitenEpilepsy Overview and Revised Classification of Seizures and Epilepsies PDFnight.shadowNoch keine Bewertungen
- Treatment of Women With EpilepsyDokument23 SeitenTreatment of Women With Epilepsynight.shadowNoch keine Bewertungen
- Nonepileptic Episodic EventsDokument16 SeitenNonepileptic Episodic Eventsnight.shadowNoch keine Bewertungen
- Identification and Treatment of Drug-Resistent EpilepsyDokument19 SeitenIdentification and Treatment of Drug-Resistent Epilepsynight.shadowNoch keine Bewertungen
- Optimizing Management of Medically Responsive EpilepsyDokument19 SeitenOptimizing Management of Medically Responsive Epilepsynight.shadowNoch keine Bewertungen
- Evaluation of Seizure Etiology From Routine Testing To Genetic EvaluationDokument21 SeitenEvaluation of Seizure Etiology From Routine Testing To Genetic Evaluationnight.shadowNoch keine Bewertungen
- Antiepileptic Drug Treatment of Epilepsy in ChildrenDokument27 SeitenAntiepileptic Drug Treatment of Epilepsy in Childrennight.shadowNoch keine Bewertungen
- Zika Virus and Other Emerging Arboviral Central Nervous System InfectionsDokument23 SeitenZika Virus and Other Emerging Arboviral Central Nervous System Infectionsnight.shadowNoch keine Bewertungen
- Lewy Body DementiasDokument19 SeitenLewy Body Dementiasnight.shadowNoch keine Bewertungen
- Neuroborreliosis and NeurosyphilisDokument20 SeitenNeuroborreliosis and Neurosyphilisnight.shadowNoch keine Bewertungen
- Central Nervous System Infections Complicating Immunosuppression and TransplantationDokument27 SeitenCentral Nervous System Infections Complicating Immunosuppression and Transplantationnight.shadowNoch keine Bewertungen
- Tuberculosis of The Central Nervous SystemDokument17 SeitenTuberculosis of The Central Nervous Systemnight.shadowNoch keine Bewertungen
- Acute Bacterial MeningitisDokument20 SeitenAcute Bacterial Meningitisnight.shadowNoch keine Bewertungen
- Helminthic Infections of The Central Nervous SystemDokument23 SeitenHelminthic Infections of The Central Nervous Systemnight.shadowNoch keine Bewertungen
- Tetanus, Botulism, and DiphtheriaDokument30 SeitenTetanus, Botulism, and Diphtherianight.shadowNoch keine Bewertungen
- Brain and Spinal Epidural AbscessDokument22 SeitenBrain and Spinal Epidural Abscessnight.shadowNoch keine Bewertungen
- Neurologic Complications of Human Immunodeficiency Virus InfectionDokument25 SeitenNeurologic Complications of Human Immunodeficiency Virus Infectionnight.shadowNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- C-Reactive Protein Test for Beckman AnalyzersDokument3 SeitenC-Reactive Protein Test for Beckman AnalyzersYến Minh NguyễnNoch keine Bewertungen
- Hematologic Complications in Patients Hospitalized With COVID 19 InfectionDokument7 SeitenHematologic Complications in Patients Hospitalized With COVID 19 Infectionedson floresNoch keine Bewertungen
- Hematopoiesis - The Process of Blood Cell ProductionDokument64 SeitenHematopoiesis - The Process of Blood Cell Productionmatthew deguzman100% (1)
- Case Report Tinea Corporis - Salsabilla Sahara - 22004101052Dokument25 SeitenCase Report Tinea Corporis - Salsabilla Sahara - 22004101052Salsabilla SaharaNoch keine Bewertungen
- Spleen Histology and Hematology of Mice after E. coli Infection and Humic Acid AdministrationDokument9 SeitenSpleen Histology and Hematology of Mice after E. coli Infection and Humic Acid AdministrationMyusik ZNoch keine Bewertungen
- Origin, Transmission, Diagnosis and Management of Coronavirus Disease 2019 (COVID-19)Dokument6 SeitenOrigin, Transmission, Diagnosis and Management of Coronavirus Disease 2019 (COVID-19)Alfitrah NurjayaNoch keine Bewertungen
- Lista DiagnosticeDokument566 SeitenLista DiagnosticeGeanina MireaNoch keine Bewertungen
- Emailing DOC-20221210-WA0012.Dokument1 SeiteEmailing DOC-20221210-WA0012.JAHIR HASANNoch keine Bewertungen
- Anthrax Black LegDokument20 SeitenAnthrax Black LegCary PriceNoch keine Bewertungen
- Introduction To Microbiology Lecture 01 INSDokument27 SeitenIntroduction To Microbiology Lecture 01 INSsa72562624742Noch keine Bewertungen
- BIOL3403 Immunology Syllabus 2021Dokument1 SeiteBIOL3403 Immunology Syllabus 2021SnowyNoch keine Bewertungen
- IJP - Volume 11 - Issue 4 - Pages 17583-17589Dokument7 SeitenIJP - Volume 11 - Issue 4 - Pages 17583-17589NidaSofianaNoch keine Bewertungen
- ADA en TBCDokument6 SeitenADA en TBCNorma Ruth Aguilar CarbajalNoch keine Bewertungen
- Reducing Malaria Infections in Sub-Saharan AfricaDokument2 SeitenReducing Malaria Infections in Sub-Saharan AfricaStansa SeniaNoch keine Bewertungen
- Difference Between Plasma and SerumDokument4 SeitenDifference Between Plasma and SerumQuraishi SahbNoch keine Bewertungen
- Gram-Positive Cocci and Rods: Key Features, Diseases, and TreatmentsDokument27 SeitenGram-Positive Cocci and Rods: Key Features, Diseases, and TreatmentsDjdjjd SiisusNoch keine Bewertungen
- Principles of Immunodetection 2Dokument59 SeitenPrinciples of Immunodetection 2Martha RetnaningtyasNoch keine Bewertungen
- Blood: Muhammad Iqbal Lecturer KMUDokument40 SeitenBlood: Muhammad Iqbal Lecturer KMUKomal NayabNoch keine Bewertungen
- Workplace AIDS PolicyDokument2 SeitenWorkplace AIDS Policyhai phamNoch keine Bewertungen
- Open Vial Policy - MoHFW - Sep2015Dokument6 SeitenOpen Vial Policy - MoHFW - Sep2015SaumyaNoch keine Bewertungen
- CompleteBloodCounts NORMAL VALUEDokument4 SeitenCompleteBloodCounts NORMAL VALUEWoro Hapsari Wahyuningrum100% (1)
- DengueDokument5 SeitenDengueSam Angelo EstrellaNoch keine Bewertungen
- Lecture Notes On Disease and EpidemiologyDokument4 SeitenLecture Notes On Disease and EpidemiologyDiane Princess SultanNoch keine Bewertungen
- Chapter 8..... HypersensitivityDokument6 SeitenChapter 8..... HypersensitivityShama AftabNoch keine Bewertungen
- Blood Cell Formation (Hematopoiesis) : Senin, 12 Januari 2004Dokument42 SeitenBlood Cell Formation (Hematopoiesis) : Senin, 12 Januari 2004nurliah armandNoch keine Bewertungen
- Risk Factors For Pneumonia in NeonatesDokument20 SeitenRisk Factors For Pneumonia in NeonatesPaula Andrea Perdomo SalamancaNoch keine Bewertungen
- Ken's Thesis Chapter 1-6 Main WK Final Final For PrintDokument56 SeitenKen's Thesis Chapter 1-6 Main WK Final Final For PrintCallumNoch keine Bewertungen
- Rulebook Simpic2018Dokument17 SeitenRulebook Simpic2018Troy FengNoch keine Bewertungen
- Francisco GS Conference March 2022Dokument69 SeitenFrancisco GS Conference March 2022SamuelNoch keine Bewertungen
- Urinary System Test BankDokument30 SeitenUrinary System Test BankVinz TombocNoch keine Bewertungen