Beruflich Dokumente
Kultur Dokumente
KJR 7 1
Hochgeladen von
Azka Rizky HidayatOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
KJR 7 1
Hochgeladen von
Azka Rizky HidayatCopyright:
Verfügbare Formate
Differentiation of Acute Myocardial
Infarction from Chronic Myocardial
Scar with MRI
Byoung Wook Choi, MD
Department of Radiology, Yonsei University, College of Medicine, Severance Hospital, Seoul 120-752, Korea
T
he coherent steady-state free precession the T1 SI. However, the low SI of the infarcted
(SSFP) pulse sequence is increasingly being myocardium that was seen in the chronic MI of this study
used in cine imaging for evaluating the is in disagreement with those findings of Abdel-Aty et al.,
cardiac function. Compared to the spoiled gradient echo in which the T2 SI of the infarcted myocardium in chronic
MRI, which has usually been performed for cardiac cine MI showed as isosignal intensity compared to the non-
imaging, the SSFP imaging sequence provides a higher infarcted myocardium (4). This discrepancy may be due to
signal-to-noise ratio (SNR) by recycling the residual the usage of contrast-enhancement in Kim et al’s study.
transverse magnetization, and there is less of an inflow Hyperenhancement of infarcted myocardium on the
effect by using a very short repetition time. A few studies delayed contrast-enhanced (DCE) MRI has been well
have recently reported that contrast-enhanced (CE) cine- established for evaluating an infarct’s location and size.
SSFP imaging could be used for estimating the viability of However, there is the same degree of hyperenhancement
infarcted myocardium with or without the simultaneous of the infarcted myocardium on the DCE MRI regardless of
evaluation of the ventricular function (1). Since the the infarct’s age. The low SI of infarcted myocardium in
contrast of the SSFP sequence imaging is based on the ratio chronic MI could be accounted for by the slow enhance-
of T2 to T1, T1-shortening contrast-enhancement is shown ment of fibrosis in the relatively early phase compared to
as hyperenhancement, which is similar to that in the the DCE, which occurred two minutes after contrast
delayed-enhanced T1-imaging. In this issue of the Korean administration in Kim’s study, as contrasted with the
Journal of Radiology, Kim et al. (2) have reported that the enhancement of the surrounding normal myocardium.
CE-cine-SSFP sequence could be used for differentiating Although the concept of early enhancement, which is
the acutely infarcted myocardium from chronic myocardial different from the first-pass perfusion, has not been well
scar with a sensitivity of 95.8%. This was a new approach established in cardiac imaging, dynamic enhancement has
for evaluating the age of myocardial infarction (MI) by already been used as a diagnostic imaging technique for
using MRI. the radiological examination for various pathologies; this
The most important pathologic changes of infarcted was recently recognized to be different from the delayed
myocardium that influence the signal intensities (SI) on the
T1- and T2-weighted imaging (WI) are the edema in acute
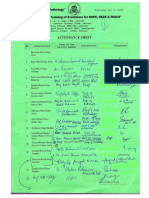
Table 1. T1- and T2-Relaxation Times and the Degree of
MI and the fibrosis in chronic MI. The T1 and T2 Enhancement in Acute and Chronic Myocardial
relaxation times are directly correlated with the water Infarction
content and they are inversely correlated with the collagen
Non Infarcted
content (3) (Table 1). The abnormal signal intensity of Acute MI* Chronic MI
Myocardium
infarcted myocardium on the T2-WI is usually conspicuous
T1 relaxation time Increase (11) Decrease Reference
compared to that on the T1-WI. Therefore, to evaluate the
T2 relaxation time Increase (12) Decrease Reference
age of an infarct, the T2-WI could be added to the infarct
T2/T1 Signal High Iso or low Iso
MRI (4). T2-WI reveals a high signal intensity of edema, Early Enhancement (+++) (+) (++)
which inevitably accompanies acutely infarcted Delayed Enhancement (+++) (+++) (+)
myocardium and it is intensified by reperfusion therapy.
* : Myocardial infarction
The abnormal signal intensity of infarcted myocardium on : Grade of enhancement: +++; strong, ++; moderate, +; mild
the cine-SSFP images should reflect the T2 SI more than : Grade of enhancement: +++; strong, ++; moderate, +; mild
Korean J Radiol 7(1), March 2006 1
Choi
enhancement in cardiac imaging and this has been applied From a practical point of view, is differentiating acute MI
to amyloid cardiomyopathy (5). from chronic MI clinically important? The authors suggest
We can suggest another possible explanation for the low that localizing the acute infarcted myocardium would be
SI of infarcted myocardium in chronic MI on the CE-cine- difficult when there is a preexisting chronic myocardial
SSFP imaging: it is a fat tissue related artifact from the infarction, and ECG and coronary angiography are not
lipomatous metaplasia of chronic scar (6). In one study, able to localize the acute lesion. How many patients with
large amounts of adipose tissue were demonstrated on the MI have difficulty with the treatment planning and follow-
histology of 4- to 18-month old transmural infarcts that up after treatment due to the coexistence of acute MI and
were experimentally produced in dog hearts (7). In chronic MI at the first diagnosis? In a discussion on this
addition, considering the frequent findings of profound matter, Sechtem et al. (10) commented that differentiation
hypo-SI of thin infarcted scars on the cine-SSFP imaging of acute and chronic MI had a limited application for those
without contrast-enhancement, a fat tissue related artifact patients with multiple previous ischemic events in rare
is more likely to induce the hypo-SI rather than the low- instances when catheter identification of the culprit lesion
degree enhancement during the early phase of the CE- was not possible. Even though the differentiation is not so
cine-SSFP imaging. The shape and degree of hypo-SI of the clinically significant, it is true that the CE-cine-SSFP pulse
infarcted scar in this study strongly suggested a phase sequence provides information about T2/T1 SI, the
cancellation artifact in the cine imaging with a low spatial contrast-enhancement, the wall motion and the wall
resolution, which can be seen at any interface containing thickness all at once, and it may be possible to substitute
both fat and water regardless of the encoding direction. To this for the T2-WI for differentiating acute MI from chronic
exclude artifacts due to fat tissue, fat suppression MI as a time-effective method.
techniques, swapping encoding directions or increasing the
receiver bandwidth can be tried. The pre- and early post- References
contrast enhanced imagings should be compared to 1. Laissy JP, Hyafil F, Huart V, Serfaty JM, Chillon S, Schouman-
Claeys E, et al. Value of contrast-enhanced, balanced cine-MR
elucidate what the SI change in the CE-cine-SSFP imaging
sequences in the assessment of apparent infarct size after acute
is, in addition to performing T1-and T2-WI for further myocardial infarction: a prospective comparison with delayed-
explanation. enhancement sequences. J Magn Reson Imaging 2005;22:765-
In this study, the high sensitivity of the CE-cine-SSFP 771
imaging for differentiating acute MI from chronic MI was 2. Kim KA, Seo JB, Do KH, Heo J-N, Lee YK, Song JW, et al.
Differentiation of recently infarcted myocardium from chronic
in contrast with the low sensitivity of measuring the end-
myocardial scar: the value of contrast-enhanced SSFP-based
diastolic wall thickness (EDWT), which was done for the cine MR imaging. Korean J Radiol 2006;7:14-19
same purpose. Wall thinning is a result of remodeling of 3. Cutillo AG, Chan PH, Ailion DC, Watanabe S, Rao NV, Hansen
the infarcted myocardium, and it is a manifestation of CB, et al. Characterization of bleomycin lung injury by nuclear
chronic MI. An EDWT < 6 mm, which was used as a cut- magnetic resonance: correlation between NMR relaxation times
and lung water and collagen content. Magn Reson Med 2002;
off value for the diagnosis of chronic MI in this study, was
47:246-256
originally obtained from the measurement of chronic 4. Abdel-Aty H, Zagrosek A, Schulz-Menger J, Taylor AJ,
transmural scar done at autopsy. A study showed that a Messroghli D, Kumar A, et al. Delayed enhancement and T2-
EDWT < 5.5 mm on the MRI obtained with the gradient weighted cardiovascular magnetic resonance imaging differenti-
echo sequence, which was calculated as the mean minus ate acute from chronic myocardial infarction. Circulation 2004;
109:2411-2416
2.5 standard deviations (SDs) of a healthy control group,
5. Wassmuth R, Bohl S, Dietz R, Schulz-Menger J. Combined
was a useful cut-off value for the diagnosis of non-viable early and delayed myocardial contrast enhancement in cardiac
myocardium (8). When comparing the cine-SSFP sequence amyloidosis. J Cardiovasc Magn Reson 2006;8:33-34
to the cine turbo gradient echo sequence, the ‘mean-2.5 6. Baroldi G, Silver MD, De Maria R, Parodi O, Pellegrini A.
SDs’ of the EDWT was 3.8 and 5.3 mm, respectively (9). Lipomatous metaplasia in left ventricular scar. Can J Cardiol
1997;13:65-71
Theoretically, 3.8 mm of EDWT with the cine-SSFP
7. Ursell PC, Gardner PI, Albala A, Fenoglio JJ Jr, Wit AL.
imaging can be tried as a cut-off value for the diagnosis of Structural and electrophysiological changes in the epicardial
viability. This accounts for why the sensitivity of the 6 mm border zone of canine myocardial infarcts during infarct healing.
cut-off value was that low. In addition, wall thinning had Circ Res 1985;56:436-451
been used as an index for the determination of viability, 8. Baer FM, Voth E, Schneider CA, Theissen P, Schicha H,
Sechtem U. Comparison of low-dose dobutamine-gradient-echo
and not for the differentiation of acute MI from chronic
magnetic resonance imaging and positron emission tomography
MI, because chronic MI confined to the subendocardial with [18F]fluorodeoxyglucose in patients with chronic coronary
layer does not necessarily demonstrate wall thinning. artery disease. A functional and morphological approach to the
2 Korean J Radiol 7(1), March 2006
Acute Myocardial Infarction versus Chronic Myocardial Scar at MRI
detection of residual myocardial viability. Circulation 1995; infarction? Nat Clin Pract Cardiovasc Med 2004;1:22-23
91:1006-1015 11. Wisenberg G, Prato FS, Carroll SE, Turner KL, Marshall T.
9. Plein S, Bloomer TN, Ridgway JP, Jones TR, Bainbridge GJ, Serial nuclear magnetic resonance imaging of acute myocardial
Sivananthan MU. Steady-state free precession magnetic infarction with and without reperfusion. Am Heart J 1988;
resonance imaging of the heart: comparison with segmented k- 115:510-518
space gradient-echo imaging. J Magn Reson Imaging 2001; 12. Higgins CB, Herfkens R, Lipton MJ, Sievers R, Sheldon P,
14:230-236 Kaufman L, et al. Nuclear magnetic resonance imaging of acute
10. Sechtem U, Mahrholdt H. Can delayed enhancement and T2- myocardial infarction in dogs: alterations in magnetic relaxation
weighted imaging distinguish acute from chronic myocardial times. Am J Cardiol 1983;52:184-188
Korean J Radiol 7(1), March 2006 3
Das könnte Ihnen auch gefallen
- Music Production EngineeringDokument1 SeiteMusic Production EngineeringSteffano RebolledoNoch keine Bewertungen
- 5 Ways To Foster A Global Mindset in Your CompanyDokument5 Seiten5 Ways To Foster A Global Mindset in Your CompanyGurmeet Singh KapoorNoch keine Bewertungen
- Economics Exam Technique GuideDokument21 SeitenEconomics Exam Technique Guidemalcewan100% (5)
- API RP 7C-11F Installation, Maintenance and Operation of Internal Combustion Engines.Dokument3 SeitenAPI RP 7C-11F Installation, Maintenance and Operation of Internal Combustion Engines.Rashid Ghani100% (1)
- E Voting PPT - 1Dokument11 SeitenE Voting PPT - 1madhu100% (2)
- 15 Miscellaneous Bacteria PDFDokument2 Seiten15 Miscellaneous Bacteria PDFAnne MorenoNoch keine Bewertungen
- Collecting, Analyzing, & Feeding Back DiagnosticDokument12 SeitenCollecting, Analyzing, & Feeding Back DiagnosticCaroline Mariae TuquibNoch keine Bewertungen
- Ryct 2019190010Dokument8 SeitenRyct 2019190010Deepak BhatNoch keine Bewertungen
- Pathophysiology of LV Remodeling in Survivors of STEMI: in Ammation, Remote Myocardium, and PrognosisDokument11 SeitenPathophysiology of LV Remodeling in Survivors of STEMI: in Ammation, Remote Myocardium, and PrognosisEDIY SANTOSANoch keine Bewertungen
- Imaging of Myocardial Fibrosis and ItsDokument9 SeitenImaging of Myocardial Fibrosis and ItsGaal PinNoch keine Bewertungen
- Leong2015 Hub Total Waktu Iskemik LVMD Dan AritmiaDokument8 SeitenLeong2015 Hub Total Waktu Iskemik LVMD Dan AritmiaauliaNoch keine Bewertungen
- Patterns of Myocardial Late Enhancement: Typical and Atypical FeaturesDokument9 SeitenPatterns of Myocardial Late Enhancement: Typical and Atypical FeaturesRicardo VallejoNoch keine Bewertungen
- MI LABS ExplainedDokument3 SeitenMI LABS Explainedjrubin83669Noch keine Bewertungen
- Leukositosis Ami 1Dokument6 SeitenLeukositosis Ami 1moonchae1989Noch keine Bewertungen
- Kharel - Implications of Localized ST Depression in A Vascular Territory and Altered Precordial T-Wave Balance in Ischemic Heart DiseaseDokument6 SeitenKharel - Implications of Localized ST Depression in A Vascular Territory and Altered Precordial T-Wave Balance in Ischemic Heart DiseaseM. PurnomoNoch keine Bewertungen
- Qualitative and Quantitative Comparison of Tgrappa and Tsense Real Time Cine Techniques During Deep BreathingDokument316 SeitenQualitative and Quantitative Comparison of Tgrappa and Tsense Real Time Cine Techniques During Deep BreathingRadhaRajasekaranNoch keine Bewertungen
- 2016-02 Imaging in ACS, FinalDokument27 Seiten2016-02 Imaging in ACS, FinalMakhyan JibrilNoch keine Bewertungen
- 2021 Article 1975Dokument6 Seiten2021 Article 1975melon segerNoch keine Bewertungen
- MRI STEMI PerazzoloDokument12 SeitenMRI STEMI PerazzoloBenjamin GonzalezNoch keine Bewertungen
- EAT STEMI Volume Gohbara2016Dokument7 SeitenEAT STEMI Volume Gohbara2016Wyah MpNoch keine Bewertungen
- 1 SMDokument9 Seiten1 SMaris hidayatul mNoch keine Bewertungen
- ST Elevation After Myocardial Infarction: What Does It Mean?Dokument2 SeitenST Elevation After Myocardial Infarction: What Does It Mean?IqbalDzakyNoch keine Bewertungen
- Adverse Diastolic Remodeling After Reperfused ST-elevation Myocardial Infarction: An Important Prognostic IndicatorDokument11 SeitenAdverse Diastolic Remodeling After Reperfused ST-elevation Myocardial Infarction: An Important Prognostic IndicatorCatia MoraesNoch keine Bewertungen
- Seems Basic-2011-Journal - of - Magnetic - Resonance - ImagingDokument7 SeitenSeems Basic-2011-Journal - of - Magnetic - Resonance - ImagingRaiyanNoch keine Bewertungen
- Jurnal Kedokteran Dan Kesehatan IndonesiaDokument7 SeitenJurnal Kedokteran Dan Kesehatan IndonesiaAlfix AnugrahNoch keine Bewertungen
- Bidirectional VTDokument4 SeitenBidirectional VTbgusjklNoch keine Bewertungen
- Muser2017 LVMD Dan CMRDokument7 SeitenMuser2017 LVMD Dan CMRauliaNoch keine Bewertungen
- Association Between Pasma Big Endothelin 1 Level and The Severity of CoronaryDokument9 SeitenAssociation Between Pasma Big Endothelin 1 Level and The Severity of Coronaryfernanda souzaNoch keine Bewertungen
- Differential Diagnosis of Elevated Troponins: Susanne Korff, Hugo A Katus, Evangelos GiannitsisDokument7 SeitenDifferential Diagnosis of Elevated Troponins: Susanne Korff, Hugo A Katus, Evangelos GiannitsisSurya M. TiyantaraNoch keine Bewertungen
- Dogan 2012Dokument7 SeitenDogan 2012Davy JonesNoch keine Bewertungen
- It Is Myocardial Infarction With Non-Obstructive Coronary Arteries: A Myth or Reality?Dokument4 SeitenIt Is Myocardial Infarction With Non-Obstructive Coronary Arteries: A Myth or Reality?asclepiuspdfsNoch keine Bewertungen
- Whole Body Dengan Iodine Kontras Terlihat Adanya Filling Defect Pada AnteroseptalDokument2 SeitenWhole Body Dengan Iodine Kontras Terlihat Adanya Filling Defect Pada AnteroseptalrandulNoch keine Bewertungen
- Relationship Between Myocardial Blush GRDokument9 SeitenRelationship Between Myocardial Blush GRNiñaNoch keine Bewertungen
- Role of Exercise Treadmill Testing in The Assessment of Coronary Microvascular Disease - LopezDokument10 SeitenRole of Exercise Treadmill Testing in The Assessment of Coronary Microvascular Disease - LopezM. PurnomoNoch keine Bewertungen
- Dasar Dasar MriDokument15 SeitenDasar Dasar MriEsa Fitriani AzizahNoch keine Bewertungen
- 35 NS Shear Stress PatternsDokument2 Seiten35 NS Shear Stress PatternsCarol Artigas GómezNoch keine Bewertungen
- ST-segment Depression: All Are Not Created Equal!Dokument6 SeitenST-segment Depression: All Are Not Created Equal!asclepiuspdfsNoch keine Bewertungen
- Journal of Cardiovascular Magnetic ResonanceDokument13 SeitenJournal of Cardiovascular Magnetic ResonanceKrombaNoch keine Bewertungen
- Exertionallegpain: Sathish Rajasekaran,, Jonathan T. FinnoffDokument29 SeitenExertionallegpain: Sathish Rajasekaran,, Jonathan T. FinnoffjohanesNoch keine Bewertungen
- Brain Sciences: Brain Abscess Masquerading As Brain InfarctionDokument6 SeitenBrain Sciences: Brain Abscess Masquerading As Brain Infarctiondaniela ivanNoch keine Bewertungen
- Dijagnoza 1 PDFDokument6 SeitenDijagnoza 1 PDFSemir1989Noch keine Bewertungen
- Eht 179Dokument10 SeitenEht 179fauzibigbossNoch keine Bewertungen
- Basra 2014Dokument18 SeitenBasra 2014Pratama InsaniNoch keine Bewertungen
- Cardiac MR With Late Gadolinium Enhancement in Acute Myocarditis With Preserved Systolic FunctionDokument11 SeitenCardiac MR With Late Gadolinium Enhancement in Acute Myocarditis With Preserved Systolic FunctionAnca NegrilaNoch keine Bewertungen
- A Case of Atypical Presentation and Valuable Lesson To LearnDokument1 SeiteA Case of Atypical Presentation and Valuable Lesson To LearnJonah SeeniNoch keine Bewertungen
- Right Ventricular Injury in ST-Elevation Myocardial InfarctionDokument9 SeitenRight Ventricular Injury in ST-Elevation Myocardial InfarctionRismarini AsantiNoch keine Bewertungen
- 2016 Article 173Dokument4 Seiten2016 Article 173Alfeus GradyNoch keine Bewertungen
- MRI in NSTEMI N STEMIDokument11 SeitenMRI in NSTEMI N STEMIBenjamin GonzalezNoch keine Bewertungen
- Truncation in Myocardial Perfusion SPECT ImagingDokument6 SeitenTruncation in Myocardial Perfusion SPECT ImagingSEP-PublisherNoch keine Bewertungen
- Jkms 35 E24Dokument9 SeitenJkms 35 E24Defriyan RamziNoch keine Bewertungen
- 0068KJR - KJR 11 571Dokument3 Seiten0068KJR - KJR 11 571Indra dig DrNoch keine Bewertungen
- 1 s2.0 S1936878X19307259 MainDokument21 Seiten1 s2.0 S1936878X19307259 MainFredognes PastorNoch keine Bewertungen
- Cardiovascular Magnetic Resonance Evaluation of The Patient With Known or Suspected Coronary Artery DiseaseDokument7 SeitenCardiovascular Magnetic Resonance Evaluation of The Patient With Known or Suspected Coronary Artery DiseaseJosep Melero FerrerNoch keine Bewertungen
- Muscular Weakness and Muscle Wasting in The Critically IllDokument14 SeitenMuscular Weakness and Muscle Wasting in The Critically IllpamelaNoch keine Bewertungen
- SNH CraniotomyDokument8 SeitenSNH CraniotomyxshreNoch keine Bewertungen
- Ryct 2021200378Dokument14 SeitenRyct 2021200378Vimal NishadNoch keine Bewertungen
- RRC Art-1aqDokument12 SeitenRRC Art-1aqCristi AlexandruNoch keine Bewertungen
- Deep Learning For Detecting and Locating Myocardial Infarction by Electrocardiogram - A Literature ReviewDokument28 SeitenDeep Learning For Detecting and Locating Myocardial Infarction by Electrocardiogram - A Literature ReviewSathvick BatchuNoch keine Bewertungen
- Diagnosis of Acute Myocardial InfarctDokument5 SeitenDiagnosis of Acute Myocardial InfarctOscar SanNoch keine Bewertungen
- Ersboll LVMD For Early Echocardiographic Prediction of Aritmia and SCDDokument10 SeitenErsboll LVMD For Early Echocardiographic Prediction of Aritmia and SCDauliaNoch keine Bewertungen
- Kontny 1993Dokument4 SeitenKontny 1993sssNoch keine Bewertungen
- Lupus Myocarditis Presenting As Acute Congestive Heart FailureDokument3 SeitenLupus Myocarditis Presenting As Acute Congestive Heart FailurehafifanisaNoch keine Bewertungen
- David N.2007Dokument7 SeitenDavid N.2007Giulia AndreeaNoch keine Bewertungen
- FCVM 08 691665Dokument9 SeitenFCVM 08 691665orhanmuratgursonNoch keine Bewertungen
- Cu 19 7Dokument6 SeitenCu 19 701-13-07 G.Noch keine Bewertungen
- Chyu Shah 2022 Electrocardiograms in Critical Care CardiologyDokument5 SeitenChyu Shah 2022 Electrocardiograms in Critical Care Cardiologytegar ksatriaNoch keine Bewertungen
- W7-8.0-8.1-10 KeysDokument6 SeitenW7-8.0-8.1-10 KeysAjhuCostaNoch keine Bewertungen
- W7-8.0-8.1-10 KeysDokument6 SeitenW7-8.0-8.1-10 KeysAjhuCostaNoch keine Bewertungen
- 3858 9727 1 PBDokument9 Seiten3858 9727 1 PBAzka Rizky HidayatNoch keine Bewertungen
- Prof Zullies. Paper1Dokument6 SeitenProf Zullies. Paper1Azka Rizky HidayatNoch keine Bewertungen
- Annurev-Ecolsys-040212-092530 (2) - 2Dokument24 SeitenAnnurev-Ecolsys-040212-092530 (2) - 2Azka Rizky HidayatNoch keine Bewertungen
- 1b - Diagnosis of Smear Positive Pulmonary TB PDFDokument5 Seiten1b - Diagnosis of Smear Positive Pulmonary TB PDFAzka Rizky HidayatNoch keine Bewertungen
- Pantone PDFDokument53 SeitenPantone PDF2dlmediaNoch keine Bewertungen
- Corelink Mmu600ae TRM 101412 0100 00 enDokument194 SeitenCorelink Mmu600ae TRM 101412 0100 00 enLv DanielNoch keine Bewertungen
- Learning English Through The Educational Games of Wordwall Website For Elementary Students by Group 1 (R4E)Dokument6 SeitenLearning English Through The Educational Games of Wordwall Website For Elementary Students by Group 1 (R4E)NurulNoch keine Bewertungen
- Dist - Propor.danfoss PVG32Dokument136 SeitenDist - Propor.danfoss PVG32Michal BujaraNoch keine Bewertungen
- Subeeka Akbar Advance NutritionDokument11 SeitenSubeeka Akbar Advance NutritionSubeeka AkbarNoch keine Bewertungen
- Caroline Coady: EducationDokument3 SeitenCaroline Coady: Educationapi-491896852Noch keine Bewertungen
- Work Sample 2 - Eoc and CrucibleDokument35 SeitenWork Sample 2 - Eoc and Crucibleapi-259791703Noch keine Bewertungen
- Index: © Christopher Pitt 2018 C. Pitt, The Definitive Guide To AdonisjsDokument5 SeitenIndex: © Christopher Pitt 2018 C. Pitt, The Definitive Guide To AdonisjsZidi BoyNoch keine Bewertungen
- 3) Uses and Gratification: 1) The Hypodermic Needle ModelDokument5 Seiten3) Uses and Gratification: 1) The Hypodermic Needle ModelMarikaMcCambridgeNoch keine Bewertungen
- Not CE 2015 Version R Series 1t-3.5t Operating Manua 2015-08Dokument151 SeitenNot CE 2015 Version R Series 1t-3.5t Operating Manua 2015-08hocine gherbiNoch keine Bewertungen
- PathologyDokument31 SeitenPathologyStudy Usmle100% (1)
- Air Blower ManualDokument16 SeitenAir Blower ManualshaiknayeemabbasNoch keine Bewertungen
- 2010 Information ExchangeDokument15 Seiten2010 Information ExchangeAnastasia RotareanuNoch keine Bewertungen
- Chapter 30 - HypertensionDokument70 SeitenChapter 30 - HypertensionSakaC.TanayaNoch keine Bewertungen
- Flipkart Labels 06 Jul 2022 09 52Dokument37 SeitenFlipkart Labels 06 Jul 2022 09 52Dharmesh ManiyaNoch keine Bewertungen
- Ethical Hacking IdDokument24 SeitenEthical Hacking IdSilvester Dian Handy PermanaNoch keine Bewertungen
- Localization On ECG: Myocardial Ischemia / Injury / InfarctionDokument56 SeitenLocalization On ECG: Myocardial Ischemia / Injury / InfarctionduratulfahliaNoch keine Bewertungen
- 1572 - Anantha Narayanan FFS CalculationDokument1 Seite1572 - Anantha Narayanan FFS CalculationAnantha NarayananNoch keine Bewertungen
- Fortnite Task Courier Pack 1500 V Bucks - BuscarDokument1 SeiteFortnite Task Courier Pack 1500 V Bucks - Buscariancard321Noch keine Bewertungen
- FINAL VERSION On Assessment Tool For CDCs LCs Sept. 23 2015Dokument45 SeitenFINAL VERSION On Assessment Tool For CDCs LCs Sept. 23 2015Edmar Cielo SarmientoNoch keine Bewertungen
- Capgemini - 2012-06-13 - 2012 Analyst Day - 3 - Michelin - A Better Way ForwardDokument12 SeitenCapgemini - 2012-06-13 - 2012 Analyst Day - 3 - Michelin - A Better Way ForwardAvanish VermaNoch keine Bewertungen
- Session 10. Value Proposition.Dokument69 SeitenSession 10. Value Proposition.Bibhu R. TuladharNoch keine Bewertungen
- ABBindustrialdrives Modules en RevBDokument2 SeitenABBindustrialdrives Modules en RevBMaitry ShahNoch keine Bewertungen