Beruflich Dokumente
Kultur Dokumente
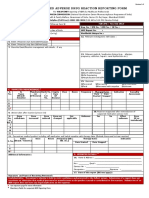
Doh 694
Hochgeladen von
János JuhászOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Doh 694
Hochgeladen von
János JuhászCopyright:
Verfügbare Formate
Hospital and Community
NEW YORK STATE DEPARTMENT OF HEALTH
OHSM-Division of Quality and Surveillance for Nursing Homes and ICFs/MR Patient Review Instrument (HC-PRI)
RUG II Group (print name)
RHCF Level of Care:
� HRF � SNF
Use with separate Hospital and Community PRI Instructions
I. ADMINISTRATIVE DATA
1. OPERATING CERTIFICATE NUMBER 2. SOCIAL SECURITY NUMBER
(1-8)
(9-17) - -
3. OFFICIAL NAME OF HOSPITAL OR OTHER AGENCY/FACILITY COMPLETING THIS REVIEW
4A. PATIENT NAME (AND COMMUNITY ADDRESS IF REVIEWED IN 11A. DATE OF HOSPITAL ADMISSION OR INITIAL AGENCY VISIT
COMMUNITY)
(49-56) - -
4B. COUNTY OF RESIDENCE MO DAY YEAR
5. DATE OF PRI COMPLETION 11B. DATE OF ALTERNATE LEVEL OF CARE STATUS IN HOSPITAL
(IF APPLICABLE)
(18-25) - - (57-64) - -
MO DAY YEAR
MO DAY YEAR
6. MEDICAL RECORD NUMBER/CASE NUMBER 12. MEDICAID NUMBER
(65-75)
(26-34)
7. HOSPITAL ROOM NUMBER 13. MEDICARE NUMBER
(35-39) (76-85)
8. NAME OF HOSPITAL UNIT/DIVISION/BUILDING 14. PRIMARY PAYOR (86)
1=Medicaid
2=Medicare
3= Other
9. DATE OF BIRTH 15. REASON FOR PRI COMPLETION (87)
(40-47) - - 1. RHCF Application from Hospital
MO DAY YEAR 2. RHCF Application from Community
3. Other (Specify: )
10. SEX (48) 1=Male
2=Female
II. MEDICAL EVENTS
16. DECUBITUS LEVEL: ENTER THE MOST SEVERE 18. MEDICAL TREATEMENTS: READ THE INSTRUCTIONS FOR
LEVEL (0-5) AS DEFINED IN THE INSTRUCTIONS. THE QUALIFIERS.
1=YES
2=NO
17. MEDICAL CONDITIONS: DURING THE PAST WEEK. READ THE A. Trachesotomy Care/Suctioning
INSTRUCTIONS FOR SPECIFIC DEFINITIONS (Daily—Exclude self-care)
1=YES
2=NO
A. Comatose B. Suctioning-General (Daily)
B. Dehydration C. Oxygen (Daily)
C. Internal Bleeding D. Respiratory Care (Daily)
D. Stasis Ulcer E. Nasal Gastric Feeding
E. Terminally Ill F. Parenteral Feeding
F. Contractures G. Wound Care
G. Diabetes Mellitus H. Chemotherapy
H. Urinary Tract Infection I. Transfusion
I. HIV Infection Symptomatic J. Dialysis
J. Accident K. Bowel and Bladder Rehabilitation (SEE INSTRUCTIONS)
K. Ventilator Dependent L. Catheter (Indwelling or External)
M. Physical Restraints (Daytime Only)
DOH-694 (12/05) Page 1 of 4
III. ACTIVITIES OF DAILY LIVING (ADLs)
Measure the capability of the patient to perform each ADL 60% or more of the time it is performed during the past week (7 days). Read the
Instructions for the Changed Condition Rule and the definitions of the ADL terms.
19. EATING: PROCESS OF GETTING FOOD BY ANY MEANS FROM THE RECEPTACLE INTO THE BODY (FOR EXAMPLE: 19.
PLATE, CUP, TUBE) (113)
1=Feeds self without supervision or physical assistance. May use 3= Requires continual help (encouragement/teaching/physical assistance)
adaptive equipment. with eating or meal will not be completed.
2=Requires intermittent supervision (that is, verbal 4=Totally fed by hand, patient does not manually participate
encouragement/guidance) and/or minimal physical assistance with
minor parts of eating, such as cutting food, buttering bread or 5=Tube or parenteral feeding for primary intake of food. (Not just for
opening milk carton. supplemental nourishments)
20. MOBILITY: HOW THE PATIENT MOVES ABOUT 20.
(114)
1=Walks with no supervision or human assistance. May require 3= Walks with constant one-to-one supervision and/or constant physical
mechanical device (for example, a walker), but not a wheelchair. assistance.
2=Walks with intermittent supervision (that is, verbal cueing and 4= Wheels with no supervision or assistance, except for difficult maneuvers
observation). May require human assistance for difficult parts of (for example, elevators, ramps). May actually be able to walk, but generally
walking (for example, stairs, ramps). does not move.
5= Is wheeled, chairfast or bedfast. Relies on someone else to move
about, if at all.
21. TRANSFER: PROCESS OF MOVING BETWEEN POSITIONS, TO/FROM BED, CHAIR, STANDING, (EXCLUDE 21.
(115)
TRANSFERS TO/FROM BATH AND TOILET).
1=Requires no supervision or physical assistance to complete 3=Requires one person to provide constant guidance, steadiness and/or
necessary transfers. May use equipment, such as railings, trapeze. physical assistance. Patient may participate in transfer.
2=Requires intermittent supervision (that is, verbal cueing, guidance) 4=Requires two people to provide constant supervision and/or physically lift.
and/or physical assistance for difficult maneuvers only. May need lifting equipment.
5=Cannot and is not gotten out of bed.
22. TOILETING: PROCESS OF GETTING TO AND FROM A TOILET (OR USE OF OTHER TOILETING EQUIPMENT, SUCH AS 22.
(116)
BEDPAN). TRANSFERRING ON AND OFF TOILET, CLEANSING SELF AFTER ELIMINATION AND ADJUSTING CLOTHES.
1=Requires no supervision or physical assistance. May require 3=Continent of bowel and bladder. Requires constant supervision and/or
special equipment, such as a raised toilet or grab bars. physical assistance with major/all parts of the task, including appliances (i.e.,
colostomy, ileostomy, urinary catheter).
2=Requires intermittent supervision for safety or encouragement, or 4=Incontinent of bowel and/or bladder and is not taken to a bathroom.
minor physical assistance (for example, clothes adjustment or 5=Incontinent of bowel and/or bladder, but is taken to a bathroom every two
washing hands). to four hours during the day and as needed at night.
IV. BEHAVIORS
23. VERBAL DISRUPTION: BY YELLING, BAITING, THREATENING, ETC. 23.
(117)
1=No known history 4=Unpredictable, recurring verbal disruption at least once during the past
2=Known history or occurrences, but not during the past week (7 week (7 days) for no foretold reason
days)
3=Short-lived or predictable disruption regardless of frequency (for 5=Patient is at level #4 above, but does not fulfill the active treatment and
example, during specific care routines, such as bathing.) assessment qualifiers (in the instructions)
24. PHYSICAL AGGRESSION: ASSAULTIVE OR COMBATIVE TO SELF OR OTHERS WITH INTENT FOR INJURY. (FOR 24.
(118)
EXAMPLE, HITS SELF, THROWS OBJECTS, PUNCHES, DANGEROUS MANEUVERS WITH WHEELCHAIR)
1=No known history. 4=Unpredictable, recurring aggression at least once during the past week (7
2=Known history or occurrences, but not during the past week (7 days) for no apparent or foretold reason (that is, not just during specific care
days). routines or as a reaction to normal stimuli).
3=Predictable aggression during specific care routines or as a 5=Patient is at level #4 above, but does not fulfill the active treatment and
reaction to normal stimuli (for example, bumped into), regardless of assessment qualifiers (in the instructions).
frequency. May strike or fight.
DOH-694 (12/05) Page 2 of 4
25. DISRUPTIVE, INFANTILE OR SOCIALLY INAPPROPRIATE BEHAVIOR: CHILDISH, REPETITIVE OR ANTISOCIAL 25.
PHYSICAL BEHAVIOR WHICH CREATES DISRUPTION WITH OTHERS. (FOR EXAMPLE, CONSTANTLY UNDRESSING SELF, (119)
STEALING, SMEARING FECES, SEXUALLY DISPLAYING ONESELF TO OTHERS). EXCLUDE VERBAL ACTIONS. READ THE
INSTRUCTIONS FOR OTHER EXCLUSIONS.
1=No known history 4=Occurences of this disruptive behavior at least once during the past week
2=Displays this behavior, but is not disruptive to others (for example, (7 days)
rocking in place).
3=Known history or occurrences, but not during the past week (7 5=Patient is at level #4 above, but does not fulfill the active treatment and
days). psychiatric assessment qualifiers (in instructions).
26. HALLUCINATIONS: EXPERIENCED AT LEAST ONCE DURING THE PAST WEEK. VISUAL, AUDITORY OR TACTILE 26.
(120)
PERCEPTIONS THAT HAVE NO BASIS IN EXTERNAL REALITY.
1=Yes 2=No 3=Yes, but does not fulfill the active treatment
and psychiatric assessment qualifiers (in the
instructions)
V. SPECIALIZED SERVICES
27. PHYSICAL AND OCCUPATIONAL THERAPIES: READ INSTRUCTIONS AND QUALIFIERS. EXCLUDE REHABILITATIVE NURSES AND
OTHER SPECIALIZED THERAPISTS (FOR EXAMPLE, SPEECH THERAPIST). ENTER THE LEVEL, DAYS AND TIME (HOURS AND MINUTES)
DURING THE PAST WEEK (7 DAYS).
A. Physical Therapy (P.T.) P.T. Level
(121)
P.T. Days
(122)
P.T. Time
(123-126) HOURS MIN/WEEK
B. Occupational Therapy (O.T.) O.T. Level
(127)
O.T. Days
(128)
O.T. Time
(129-132) HOURS MIN/WEEK
LEVEL 3=Restorative Therapy-Requires and is currently receiving physical and/or
1=Does not receive. occupational therapy for the past week.
2= Maintenance program-Requires and is currently receiving 4=Receives therapy, but does not fulfill the qualifiers stated in the
physical and/or occupational therapy to help stabilize or slow instructions. (For example, therapy provided for only two days).
functional deterioration.
DAYS AND TIME PER WEEK: ENTER THE CURRENT NUMBER OF DAYS AND TIME (HOURS AND MINUTES) DURING THE PAST WEEK (7
DAYS) THAT EACH THERAPY WAS PROVIDED. ENTER ZERO IF AT #1 LEVEL ABOVE. READ INSTRUCTIONS AS TO QUALIFIERS IN
COUNTING DAYS AND TIME.
28. NUMBER OF PHYSICIAN VISITS: DO NOT ANSWER THIS QUESTION FOR HOSPITALIZED PATIENTS, (ENTER ZERO), 28.
(133-134)
UNLESS ON ALTERENATE LEVEL OF CARE STATUS. ENTER ONLY THE NUMBER OF VISITS DURING THE PAST WEEK
THAT ADHERED TO THE PATIENT NEED AND DOCUMENTATION QUALIFIERS IN THE INSTRUCTIONS. THE PATIENT
MUST BE MEDICALLY UNSTABLE TO ENTER ANY PHYSICIAN VISITS, OTHERWISE ENTER A ZERO.
VI. DIAGNOSIS
29. PRIMARY PROBLEM: THE MEDICAL CONDITION REQUIRING THE LARGEST AMOUNT OF NURSING TIME IN THE HOSPITAL OR
CARE TIME IF IN THE COMMUNITY. (FOR HOSPITALIZED PATIENTS THIS MAY OR MAY NOT BE THE ADMISSION DIAGNOSIS).
ICD-9 Code of medical problem 29. -
(135-139)
If code cannot be located, print medical name here:
DOH-694 (12/05) Page 3 of 4
VII. PLAN OF CARE SUMMARY
This section is to communicate to providers any additional clinical information, which may be needed for their preadmission review of the
patient. It does not have to be completed if the information below is already provided by your own form, which is attached to this H/C-PRI.
30. DIAGNOSES AND PROGNOSES: FOR EACH DIAGNOSIS, DESCRIBE THE PROGNOSIS AND CARE PLAN IMPLICATIONS.
Primary Prognosis
1.
Secondary (Include Sensory Impairments)
1.
2.
3.
4.
31. REHABILITATION POTENTIAL (INFORMATION FROM THERAPISTS)
A. POTENTIAL DEGREE OF IMPROVEMENT WITH ADLs WITHIN SIX MONTHS (DESCRIBE IN TERMS OF ADL LEVELS ON THE HC-PRI):
B. CURRENT THERAPY CARE PLAN: DESCRIBE THE TREATMENTS (INCLUDING WHY) AND ANY SPECIAL EQUIPMENT REQUIRED.
32. MEDICATIONS
NAME DOSE FREQUENCY ROUTE DIAGNOSIS REQUIRING
EACH MEDICATION
33. TREATMENTS: INCLUDE ALL DRESSINGS, IRRIGATIONS, WOUND CARE, OXYGEN.
A. TREATMENTS DESCRIBE WHY NEEDED FREQUENCY
B. NARRATIVE: DESCRIBE SPECIAL DIET, ALLERGIES, ABNORMAL LAB VALUES, PACEMAKER.
34. RACE/ETHNIC GROUP: ENTER THE CODE WHICH BEST DESCRIBES THE PATIENT’S RACE OR ETHNIC GROUP 34.
1=White 4=Black/Hispanic 7=American Indian or Alaskan Native
2=White/Hispanic 5=Asian or Pacific Islander 8=American Indian or Alaskan Native/Hispanic
3=Black 6=Asian or Pacific Islander/Hispanic 9=Other
35. QUALIFIED ASSESSOR: I HAVE PERSONALLY OBSERVED/INTERVIEWED THIS PATIENT AND COMPLETED THIS H/C PRI.
YES NO
I CERTIFY THAT THE INFORMATION CONTAINED HEREIN IS A TRUE ABSTRACT OF THE PATIENT’S CONDITION AND MEDICAL RECORD.
___________________________________ IDENTIFICATION NO.
SIGNATURE OF QUALIFIED ASSESSOR
DOH-694 (12/05) Page 4 of 4
Das könnte Ihnen auch gefallen
- Weekly Report Feb. 2-8, 2024Dokument8 SeitenWeekly Report Feb. 2-8, 2024vandiemagallanesNoch keine Bewertungen
- Cioms FormDokument2 SeitenCioms Formnaura_farrelNoch keine Bewertungen
- Case Study FormatDokument4 SeitenCase Study FormatLuiezt BernardoNoch keine Bewertungen
- Case Study Format 1Dokument4 SeitenCase Study Format 1Michelle Rose RodaviaNoch keine Bewertungen
- Brief Description of The Disease/statistical IncidenceDokument2 SeitenBrief Description of The Disease/statistical IncidenceLeanne Princess Gamboa100% (1)
- Health Emergency Preparedness Response and Recovery PlanDokument11 SeitenHealth Emergency Preparedness Response and Recovery PlanReslyn YanocNoch keine Bewertungen
- Pedia Case Study FormatDokument4 SeitenPedia Case Study FormatJohn Carlo B. Dungca100% (1)
- CBAHI and JCI Common Asked Questions. 2023Dokument5 SeitenCBAHI and JCI Common Asked Questions. 2023Rini NoviantiNoch keine Bewertungen
- Head Nursing: University of Cebu - BaniladDokument30 SeitenHead Nursing: University of Cebu - BaniladVjay DingNoch keine Bewertungen
- Lic 602 ADokument6 SeitenLic 602 ALm RappeportNoch keine Bewertungen
- Check List For SNCUDokument5 SeitenCheck List For SNCUpriyahospitalNoch keine Bewertungen
- GNO Medication ReviewDokument18 SeitenGNO Medication ReviewCHARLENE MAY PANDINONoch keine Bewertungen
- Case Study FormatDokument4 SeitenCase Study FormatKOBE TOMAGANNoch keine Bewertungen
- Medical Plan ICS 206Dokument3 SeitenMedical Plan ICS 206RexNoch keine Bewertungen
- Medical Record Dept.Dokument32 SeitenMedical Record Dept.Kool KingNoch keine Bewertungen
- VBA-21-0960G-4-ARE Intestinal Surgery PDFDokument3 SeitenVBA-21-0960G-4-ARE Intestinal Surgery PDFCombat CraigNoch keine Bewertungen
- Perioperative Pre-Class Mini-Lecture - CH 17-19Dokument22 SeitenPerioperative Pre-Class Mini-Lecture - CH 17-19Marcel YoungNoch keine Bewertungen
- Duty NotesDokument4 SeitenDuty NotesjustinjareddNoch keine Bewertungen
- 9 Caf001diDokument1 Seite9 Caf001diwhite304Noch keine Bewertungen
- Clinical Case Study Format General Ward 1Dokument3 SeitenClinical Case Study Format General Ward 1Fita ClanNoch keine Bewertungen
- DJPRH Processes and ProceduresDokument289 SeitenDJPRH Processes and ProceduresjeffaguilarNoch keine Bewertungen
- Medical Plan ICS 206Dokument3 SeitenMedical Plan ICS 206Leo ConstantinoNoch keine Bewertungen
- Signed DOH-DBM Joint Circular On One COVID-19 Allowance (OCA) OCA Information System (OCAIS)Dokument35 SeitenSigned DOH-DBM Joint Circular On One COVID-19 Allowance (OCA) OCA Information System (OCAIS)genNoch keine Bewertungen
- Project Proposal: Code of 1991 Mandates The Local Government Units To Provide Basic FacilitiesDokument4 SeitenProject Proposal: Code of 1991 Mandates The Local Government Units To Provide Basic Facilitiescasagantm-1Noch keine Bewertungen
- VA Housebound Form VBA-21-2680Dokument2 SeitenVA Housebound Form VBA-21-2680tom2susanNoch keine Bewertungen
- Medical and Social Examination of DisabilityDokument20 SeitenMedical and Social Examination of DisabilityashighaNoch keine Bewertungen
- Health Record GuidelinesDokument18 SeitenHealth Record GuidelinesragNoch keine Bewertungen
- Source NP%Dokument10 SeitenSource NP%Ima Leigh RubioNoch keine Bewertungen
- Dictation Discharge Summary TemplateDokument19 SeitenDictation Discharge Summary TemplateBobby ReddyNoch keine Bewertungen
- Grand Case Presentation FormatDokument7 SeitenGrand Case Presentation FormatRENEROSE TORRESNoch keine Bewertungen
- Quiz Hospital DocumentationDokument5 SeitenQuiz Hospital DocumentationJessica EdiosNoch keine Bewertungen
- Customer Satisfction - Quarter ReportDokument3 SeitenCustomer Satisfction - Quarter Reportjimelyquinones78Noch keine Bewertungen
- Surgical Case Presentation SchemeDokument4 SeitenSurgical Case Presentation SchemeVasilescu LauraNoch keine Bewertungen
- New Assessment Tool For Hospitals (Repaired)Dokument60 SeitenNew Assessment Tool For Hospitals (Repaired)Ana dominique Hernandez100% (1)
- 2021 AMR - CoacoDokument11 Seiten2021 AMR - CoacoAngelo MojicaNoch keine Bewertungen
- Far Eastern University Institute of Nursing: Individual/ Group Nursing Process FormatDokument8 SeitenFar Eastern University Institute of Nursing: Individual/ Group Nursing Process FormatAbie Jewel Joy RoqueNoch keine Bewertungen
- Medical-Surgical Nursing Knowledge & Skills ChecklistDokument3 SeitenMedical-Surgical Nursing Knowledge & Skills Checklistnorthweststaffing100% (1)
- Digital Learner'S Worksheet: Student Nameraphael Chino Aragon Date: InstitutionDokument67 SeitenDigital Learner'S Worksheet: Student Nameraphael Chino Aragon Date: InstitutionRAPHAEL CHINO ARAGONNoch keine Bewertungen
- Nurse Np1 Board CramsheetDokument8 SeitenNurse Np1 Board CramsheetZero TwoNoch keine Bewertungen
- Activity On Hospital Documentation - HospPharmLab Act 1Dokument4 SeitenActivity On Hospital Documentation - HospPharmLab Act 1Jan Aerielle AzulNoch keine Bewertungen
- 5 6212887793887085843 PDFDokument11 Seiten5 6212887793887085843 PDFeruditeNoch keine Bewertungen
- Missionary Recommendation Physician Dental FormDokument5 SeitenMissionary Recommendation Physician Dental FormdozieojiakuNoch keine Bewertungen
- VBA-21-0960J-3-ARE Prostate Cancer PDFDokument3 SeitenVBA-21-0960J-3-ARE Prostate Cancer PDFCombat CraigNoch keine Bewertungen
- Case Study FormatDokument2 SeitenCase Study Formatgrandpa12Noch keine Bewertungen
- West Visayas State University Medical Center E. Lopez St. Jaro Iloilo CityDokument7 SeitenWest Visayas State University Medical Center E. Lopez St. Jaro Iloilo CityRegine Marie EspañaNoch keine Bewertungen
- Safe HospitalDokument36 SeitenSafe HospitalSagrina BangunNoch keine Bewertungen
- Nursing Recruitment Skills Checklist: Guidance or DirectionDokument4 SeitenNursing Recruitment Skills Checklist: Guidance or DirectionKRIZZEL CATAMINNoch keine Bewertungen
- ALJ Decision Holy Cross 05-CA-182154 - 07212017Dokument30 SeitenALJ Decision Holy Cross 05-CA-182154 - 07212017David LublinNoch keine Bewertungen
- Hiv and Aids OrientationDokument56 SeitenHiv and Aids OrientationRufo JawaNoch keine Bewertungen
- ESR Follow-Up FormDokument2 SeitenESR Follow-Up FormAflkjael JamaelNoch keine Bewertungen
- ADRnewReporting Form 1.4Dokument2 SeitenADRnewReporting Form 1.4Sourabh kundara0% (1)
- Severe Acute Malnutrition Guidelines - PPD - CPDDokument7 SeitenSevere Acute Malnutrition Guidelines - PPD - CPDTamal Deb BarmaNoch keine Bewertungen
- Esr Summary 2023Dokument2 SeitenEsr Summary 2023Mohamed KamalNoch keine Bewertungen
- Health Facilities and Services Regulatory Bureau: Republic of The Philippines Department of HealthDokument60 SeitenHealth Facilities and Services Regulatory Bureau: Republic of The Philippines Department of HealthMichael Capuyan JrNoch keine Bewertungen
- NDRRMC - 206Dokument3 SeitenNDRRMC - 206Dexter Martije DescotidoNoch keine Bewertungen
- Nursing Health History FormatDokument7 SeitenNursing Health History FormatJasmine PonceNoch keine Bewertungen
- Nursing Health History FormatDokument7 SeitenNursing Health History Formatgeraldine suarezNoch keine Bewertungen
- Syllab Ccincommhealthcare-20042021Dokument23 SeitenSyllab Ccincommhealthcare-20042021Suresh JNoch keine Bewertungen
- Good Health in the Tropics: Advice to Travellers and SettlersVon EverandGood Health in the Tropics: Advice to Travellers and SettlersNoch keine Bewertungen
- Plant Disease: An Advanced Treatise: How Plants Suffer from DiseaseVon EverandPlant Disease: An Advanced Treatise: How Plants Suffer from DiseaseJames G. HorsfallNoch keine Bewertungen
- HL 2022 Sample PagesDokument14 SeitenHL 2022 Sample PagesJános JuhászNoch keine Bewertungen
- Mindmanager Enterprise: Promotes Collaborative Working Practices at ManeDokument2 SeitenMindmanager Enterprise: Promotes Collaborative Working Practices at ManeJose M. GuerreroNoch keine Bewertungen
- Lions Mane Ultimate Guide 00Dokument1 SeiteLions Mane Ultimate Guide 00János JuhászNoch keine Bewertungen
- Ps 2Dokument6 SeitenPs 2János JuhászNoch keine Bewertungen
- Fen-11 User ManualDokument40 SeitenFen-11 User ManualJuan Jiménez GamezNoch keine Bewertungen
- Manual Nintendo64 SinAndPunishment ENDokument11 SeitenManual Nintendo64 SinAndPunishment ENJános JuhászNoch keine Bewertungen
- En FEN 01 Um CDokument32 SeitenEn FEN 01 Um CJános JuhászNoch keine Bewertungen
- SYLLABUS For JEE (Main) - 2021 Syllabus For Paper-1Dokument19 SeitenSYLLABUS For JEE (Main) - 2021 Syllabus For Paper-1HrishiNoch keine Bewertungen
- Pri PDFDokument5 SeitenPri PDFAnonymous dyqQV3Noch keine Bewertungen
- D2.2a Poor FenDokument9 SeitenD2.2a Poor FenJános JuhászNoch keine Bewertungen
- Human MAIT Cells Are Devoid of Alloreactive Potential: Prompting Their Use As Universal Cells For Adoptive Immune TherapyDokument34 SeitenHuman MAIT Cells Are Devoid of Alloreactive Potential: Prompting Their Use As Universal Cells For Adoptive Immune TherapyJános JuhászNoch keine Bewertungen
- Check MAIT: References Cites 53 ArticlesDokument7 SeitenCheck MAIT: References Cites 53 ArticlesJános JuhászNoch keine Bewertungen
- Ids High-Leit Flyer enDokument8 SeitenIds High-Leit Flyer enJános JuhászNoch keine Bewertungen
- Ding Dong Merrily On HighDokument1 SeiteDing Dong Merrily On Highpfr31430Noch keine Bewertungen
- Cancers: MAIT Cells: Partners or Enemies in Cancer Immunotherapy?Dokument23 SeitenCancers: MAIT Cells: Partners or Enemies in Cancer Immunotherapy?János JuhászNoch keine Bewertungen
- BasicRiderCourse HandbookDokument84 SeitenBasicRiderCourse HandbookKonstantinos AirmanNoch keine Bewertungen
- The RISC Algorithm Language (RISCAL)Dokument155 SeitenThe RISC Algorithm Language (RISCAL)János JuhászNoch keine Bewertungen
- Giuseppe Verdi - Aida MARCIA TRIONFALEDokument38 SeitenGiuseppe Verdi - Aida MARCIA TRIONFALEJános JuhászNoch keine Bewertungen
- Prupersonal Accident EBrochure EnglishDokument6 SeitenPrupersonal Accident EBrochure EnglishJános JuhászNoch keine Bewertungen
- PRI FrenchEnergyTransitionLawDokument16 SeitenPRI FrenchEnergyTransitionLawJános JuhászNoch keine Bewertungen
- SAMv 1Dokument21 SeitenSAMv 1János JuhászNoch keine Bewertungen
- PumpingStationOne20140628 Real TimeProgrammingWithBeagleBonePRUsDokument37 SeitenPumpingStationOne20140628 Real TimeProgrammingWithBeagleBonePRUsJános JuhászNoch keine Bewertungen
- INVM11630Dokument36 SeitenINVM11630János JuhászNoch keine Bewertungen
- A Step-By-Step Guide To The Prufund Smoothing ProcessDokument6 SeitenA Step-By-Step Guide To The Prufund Smoothing ProcessJános JuhászNoch keine Bewertungen
- Pru Ar2016 FullDokument412 SeitenPru Ar2016 FullEsplanadeNoch keine Bewertungen
- PRU Assembly Instruction User GuideDokument50 SeitenPRU Assembly Instruction User GuideJános JuhászNoch keine Bewertungen
- The Prufund Range of Funds: An Introduction ToDokument24 SeitenThe Prufund Range of Funds: An Introduction ToJános JuhászNoch keine Bewertungen
- INVB6572Dokument24 SeitenINVB6572János JuhászNoch keine Bewertungen
- CV 2017 VirginiaDokument4 SeitenCV 2017 Virginiaapi-353693776Noch keine Bewertungen
- Porcelain Veneer Preparations PDFDokument3 SeitenPorcelain Veneer Preparations PDFSamah FadelNoch keine Bewertungen
- Diagnosis and Management of Meniscal Injury: PresentationDokument4 SeitenDiagnosis and Management of Meniscal Injury: PresentationemilyNoch keine Bewertungen
- Echo Facts IndexDokument3 SeitenEcho Facts Indexs336336anl100% (1)
- NCP Acute PainDokument2 SeitenNCP Acute PainNecheal BaayNoch keine Bewertungen
- Valleylab ForceTriad - User Manual PDFDokument100 SeitenValleylab ForceTriad - User Manual PDFPaulina LekszyckaNoch keine Bewertungen
- InjectionsDokument26 SeitenInjectionsNotInterested100% (3)
- Psych Units 11-13 Cheat SheetDokument1 SeitePsych Units 11-13 Cheat SheetTalia ShumanNoch keine Bewertungen
- Failure Mode and Effect Analysis (FMEA) Sanglah General Hospital 2012Dokument28 SeitenFailure Mode and Effect Analysis (FMEA) Sanglah General Hospital 2012ferekonstantinusNoch keine Bewertungen
- Pe StressDokument50 SeitenPe StressAngelica OrbizoNoch keine Bewertungen
- Tourette Syndrome Script FinalDokument5 SeitenTourette Syndrome Script Finalapi-439171422Noch keine Bewertungen
- 02 Full Crown PreparationDokument35 Seiten02 Full Crown PreparationSurgaBetariJelita100% (1)
- Drug Interactions Results - MICROMEDEX®Dokument3 SeitenDrug Interactions Results - MICROMEDEX®Kike MenesesNoch keine Bewertungen
- Emergency Protocol ProcedureDokument14 SeitenEmergency Protocol Procedurejmmos207064Noch keine Bewertungen
- Hystori of EndoskopikDokument3 SeitenHystori of Endoskopiksmansa123Noch keine Bewertungen
- Skin Care PowerpointDokument52 SeitenSkin Care Powerpointisapatrick812667% (3)
- Smaple Case Study - Virginia's Henderson Need Theory PDFDokument8 SeitenSmaple Case Study - Virginia's Henderson Need Theory PDFEduardo AnerdezNoch keine Bewertungen
- Nursing Care Plan Breast-CancerDokument2 SeitenNursing Care Plan Breast-CancerGreg Llandelar100% (2)
- Trauma Wajah Tutorial - PPTX RevDokument49 SeitenTrauma Wajah Tutorial - PPTX RevShinta Andi SarasatiNoch keine Bewertungen
- Adl IadlDokument20 SeitenAdl IadlKrisna Eka Yudha100% (1)
- Pharyngeal ReflexDokument3 SeitenPharyngeal ReflexAyra Nakrish AlvarezNoch keine Bewertungen
- Kyp Ho Scoliosis 1Dokument70 SeitenKyp Ho Scoliosis 1Tias DiahNoch keine Bewertungen
- Chronic Kidney Disease in Children Clinical PresentationDokument4 SeitenChronic Kidney Disease in Children Clinical PresentationJendriella LaaeeNoch keine Bewertungen
- Insulin Adjustment Workbook CompleteDokument53 SeitenInsulin Adjustment Workbook CompleteDiabestes-stuff100% (1)
- Suggamadex Remifentanyl PalonosetronDokument28 SeitenSuggamadex Remifentanyl PalonosetronSai TejeswiNoch keine Bewertungen
- RETDEM TEMPLATE AutoRecoveredDokument5 SeitenRETDEM TEMPLATE AutoRecoveredAlexa Gwen Agnila BihagNoch keine Bewertungen
- How To Perform A Head To Toe AssessmentDokument2 SeitenHow To Perform A Head To Toe AssessmentLalaine RomeroNoch keine Bewertungen
- NaloxoneDokument3 SeitenNaloxoneTracyNoch keine Bewertungen
- Fibrous Dysplasia of BoneDokument31 SeitenFibrous Dysplasia of Bonet.babyNoch keine Bewertungen
- Understanding Neurology - A Problem-Orientated Approach PDFDokument241 SeitenUnderstanding Neurology - A Problem-Orientated Approach PDFAshabul AnharNoch keine Bewertungen