Beruflich Dokumente
Kultur Dokumente
Disease of Immune System
Hochgeladen von
Yuvraj Chauhan0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
12 Ansichten29 SeitenHow immune system works when we encountered a foreign objects.
Originaltitel
Disease of immune system
Copyright
© © All Rights Reserved
Verfügbare Formate
DOCX, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenHow immune system works when we encountered a foreign objects.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
12 Ansichten29 SeitenDisease of Immune System
Hochgeladen von
Yuvraj ChauhanHow immune system works when we encountered a foreign objects.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 29
TODAY’ TOPICS:
Normal Immune Response
a. Innate Immunity
b. Adaptive Immunity
Cells of the Immune System
Lymphocyte Diversity
T-Lymphocytes
B- Lymphocytes
Dendritic Cells
Macrophages
Natural Killer Cells
Innate Lymphoid Cells (ILC’s)
Tissues of the Immune System
Generative Lymphoid Organs
Peripheral Lymphoid Organs
Lymphocyte Recirculation
The Immune System
The immune system is vital for survival, because
it protects us from infectious pathogens that
abound in the environment. Predictably, immune
deficiencies render individuals easy prey to
infections. But the immune system is itself
capable of causing tissue injury and disease.
Examples of disorders caused by immune
responses include allergies and reactions
against an individual’s own tissues and cells
(autoimmunity).
The Normal Immune Response
The classic definition of immunity is protection
from infectious pathogens, and the normal
immune response is best understood in this
context. The mechanisms of defense against
microbes fall into two broad categories . Innate
immunity (also called natural, or native,
immunity) refers to the mechanisms that are
ready to react to infections even before they
occur, and that have evolved to specifically
recognize and combat microbes. Adaptive
immunity (also called acquired, or specific,
immunity) consists of mechanisms that are
stimulated by (“adapt to”) microbes and are
capable of recognizing microbial and
nonmicrobial substances. Innate immunity is the
first line of defense. It is mediated by cells and
molecules that rec- ognize products of microbes
and dead cells and induce rapid protective host
reactions. Adaptive immunity develops later,
after exposure to microbes and other foreign
substances, and is even more powerful than
innate immunity in combating infections. By
convention, the term immune response usually
refers to adaptive immunity.
Innate Immunity
Innate immunity is always present, ready to
provide defense against microbes and to
eliminate damaged cells. The receptors and
components of innate immunity have evolved to
serve these purposes. Innate immunity functions
in stages: recognition of microbes and damaged
cells, activation of various mechanisms, and
elimination of the unwanted substances.
Components of Innate Immunity
The major components of innate immunity are
epithelial barriers that block entry of microbes,
phagocytic cells (mainly neutrophils and
macrophages), dendritic cells, natural killer (NK)
cells, and several plasma proteins, including the
proteins of the complement system.
• Epithelia of the skin and gastrointestinal and
respiratory tracts provide mechanical barriers to
the entry of microbes from the external
environment. Epithelial cells also produce
antimicrobial molecules such as defensins, and
lymphocytes located in the epithelia combat
microbes at these sites. If microbes do breach
epithelial boundaries, other defense mechanisms
are called in.
• Monocytes and neutrophils are phagocytes in
the blood that can rapidly be recruited to
any site of infection; monocytes that enter
the tissues and mature are called
macrophages. All tissues contain resident
macrophages, the professional phagocytes
of the body. These cells not only sense the
presence of microbes and other offending
agents, but also ingest (phagocytose) these
invaders and destroy them. Macrophages
are the dominant cells of chronic
inflammation.
• Dendritic cells are a specialized cell population
present in epithelia, lymphoid organs, and
most tissues. They capture protein antigens
and display peptides for recognition by T
lymphocytes. In addition to their antigen
presenting function, dendritic cells are
endowed with a rich collection of receptors
that sense microbes and cell damage and
stimulate the secretion of cytokines,
mediators that play critical roles in
inflammation and anti-viral defense. Thus,
dendritic cells are involved in the initiation
of innate immune responses, but, unlike
macrophages, they are not key participants
in the destruction of microbes and other
offending agents.
• Natural killer cells provide early protection
against many viruses and intracellular
bacteria.
• Several other cell types can sense and react to
microbes. These include mast cells, which
are capable of producing many mediators of
inflammation , and even epithelial and
endothelial cells.
In addition to these cells, several soluble
proteins play important roles in innate immunity.
The proteins of the complement system, are
plasma proteins that are activated by microbes
using the alternative and lectin pathways in
innate immune responses; in adaptive immunity
it is activated by antibodies using the classical
pathway. Other circulating proteins of innate
immunity are mannose-binding lectin and C-
reactive protein, both of which coat microbes
and promote phagocytosis. Lung surfactant is
also a component of innate immunity, providing
protection against inhaled microbes.
Cellular Receptors for Microbes, Products of
Damaged Cells, and Foreign Substances
Cells that participate in innate immunity are
capable of recognizing certain microbial
components that are shared among related
microbes and are often essential for infectivity
(and thus cannot be mutated to allow the
microbes to evade the defense mechanisms).
These microbial structures are called pathogen-
associated molecular patterns. Leukocytes also
recognize molecules released by injured and
necrotic cells, which are called damage-
associated molecular patterns. Collectively, the
cellular receptors that recognize these
molecules are often called pattern recognition
receptors. Pattern recognition receptors are
located in all the cellular compartments where
microbes may be present: plasma membrane
receptors detect extracellular microbes,
endosomal receptors detect ingested microbes,
and cytosolic receptors detect microbes in the
cytoplasm
Toll-Like Receptors. The best known of the
pattern recognition receptors are the Toll-like
receptors (TLRs), whose founding member, Toll,
was discovered in Drosophila. A family of related
proteins was later shown to be essential for host
defense against microbes. There are 10 TLRs in
mammals, and each recognizes a different set of
microbial molecules. The TLRs are present in the
plasma membrane and endosomal vesicles . All
these receptors signal by a common pathway
that culminates in the activation of two sets of
transcription factors: (1) NF-κB, which stimulates
the synthesis and secretion of cytokines and the
expression of adhesion molecules, both of which
are critical for the recruitment and activation of
leukocytes , and (2) interferon regulatory factors
(IRFs), which stimulate the production of the
antiviral cytokines, type I interferons. Germline
loss-of-function mutations affecting TLRs and
their signaling pathways are associated with
rare but serious immunodeficiency syndromes.
NOD-Like Receptors and the Inflammasome.
NOD-like receptors (NLRs) are cytosolic
receptors named after the founding member
NOD-2. They recognize a wide variety of
substances, including products of necrotic cells
(e.g., uric acid and released ATP), ion
disturbances (e.g., loss of K+), and some
microbial products. How this family of sensors is
capable of detecting so many, quite diverse,
signs of danger or damage is not known. Several
of the NLRs signal via a cytosolic multiprotein
complex called the inflammasome, which
activates an enzyme (caspase-1) that cleaves a
precursor form of the cytokine interleukin-1 (IL-
1) to generate the biologically active form. IL-1
is a mediator of inflammation that recruits
leukocytes and induces fever. Gain-of-function
mutations in one of the NLRs result in periodic
fever syndromes, called autoinflammatory
syndromes (to be distinguished from
autoimmune diseases, which result from T and B
lympho- cyte reactions against self antigens).
The autoinflammatory syndromes respond very
well to treatment with IL-1 antagonists. The
NLR-inflammasome pathway may also play a role
in many common disorders. For example,
recognition of urate crystals by a class of NLRs
underlies the inflammation associated with gout.
These receptors may also be capable of
detecting lipids and cholesterol crystals that are
deposited in abnormally large amounts in
tissues, and the resulting inflammation may
contribute to obesity-associated type 2 diabetes
and atherosclerosis, respectively.
Other Receptors for Microbial Products. C-type
lectin receptors (CLRs) expressed on the plasma
membrane of macrophages and dendritic cells
detect fungal glycans and elicit inflammatory
reactions to fungi. RIG-like receptors (RLRs),
named after the founding member RIG-I, are
located in the cytosol of most cell types and
detect nucleic acids of viruses that replicate in
the cytoplasm of infected cells. These receptors
stimulate the production of antiviral cytokines. G
protein–coupled receptors on neutrophils,
macrophages, and most other types of
leukocytes recognize short bacterial peptides
containing N-formylmethionyl residues. Because
all bacterial proteins and few mammalian
proteins (only those synthesized within
mitochondria) are initiated by N-
formylmethionine, this receptor enables
neutrophils to detect bacterial proteins and
stimulate chemotactic responses of the cells.
Mannose receptors recognize microbial sugars
(which often contain terminal mannose residues,
unlike mammalian glycoproteins) and induce
phagocytosis of the microbes.
Reactions of Innate Immunity
The innate immune system provides host
defense by two main reactions.
• Inflammation. Cytokines and products of
complement activation, as well as other
mediators, are produced during innate immune
reactions and trigger the vascular and cellular
components of inflammation. The recruited
leukocytes destroy microbes and ingest and
eliminate damaged cells.
• Antiviral defense. Type I interferons produced
in response to viruses act on infected and
uninfected cells and activate enzymes that
degrade viral nucleic acids and inhibit viral
replication, inducing what has been called an
antiviral state.
• In addition to these defensive functions, innate
immunity provides the danger signals that
stimulate the subsequent more powerful
adaptive immune response.
Innate immunity, unlike adaptive immunity, does
not have memory or fine antigen specificity. It is
estimated that innate immunity uses about 100
different receptors to recognize 1,000 molecular
patterns. In contrast, adaptive immunity uses
two types of receptors (antibodies and T-cell
receptors, ), each with millions of variations, to
recognize millions of antigens.
Adaptive Immunity
The adaptive immune system consists of
lymphocytes and their products, including
antibodies. The lymphocytes of adaptive
immunity use highly diverse receptors to
recognize a vast array of foreign substances.
There are two types of adaptive immunity:
humoral immunity, which protects against
extracellular microbes and their toxins, and cell-
mediated (or cellular) immunity, which is
responsible for defense against intracellular
microbes. Humoral immunity is mediated by B
(bone marrow–derived) lymphocytes and their
secreted products, antibodies (also called
immunoglobulins, Ig), and cellular immunity is
mediated by T (thymus-derived) lymphocytes.
Both classes of lymphocytes express highly
specific receptors for a wide variety of
substances, which are called antigens.
Cells of the Immune System
Although T and B lymphocytes and their subsets
are morphologically unimpressive and appear
quite similar to one another, they are actually
remarkably heterogeneous and specialized in
molecular properties and functions.
Lymphocytes and other cells involved in
immune responses are not fixed in particular
tissues (as are cells in most of the organs of the
body) but constantly circulate among lymphoid
and other tissues via the blood and the
lymphatic circulation. This feature promotes
immune surveillance by allowing lymphocytes to
home to any site of infection. In lymphoid
organs, different classes of lymphocytes are
anatomically segregated in such a way that they
interact with one another only when stimulated
to do so by encounters with antigens and other
stimuli. Mature lymphocytes that have not
encountered the antigen for which they are
specific are said to be naive (immunologically
inexperienced). After they are activated by
recognition of antigens and other signals
described later, lymphocytes differentiate into
effector cells, which perform the function of
eliminating microbes, and memory cells, which
live in a state of heightened awareness and are
able to react rapidly and strongly to combat the
microbe in case it returns.
Lymphocyte Diversity
Lymphocytes specific for a large number of
antigens exist before exposure to antigen, and
when an antigen enters, it selectively activates
the antigen-specific cells. This fundamental
concept is called clonal selection. According to
this hypothesis, lymphocytes express specific
receptors for antigens and mature into
functionally competent cells before exposure to
antigen. Lymphocytes of the same specificity
are said to constitute a clone; all the members
of one clone express identical antigen receptors,
which are different from the receptors in all
other clones. There are about 1012 lymphocytes
in a healthy adult, and it is estimated that these
are capable of recognizing 107 to 109 different
antigens. It follows that the number of cells
specific for any one antigen is very small,
probably less than 1 in 100,000 to 1 in 1 million
lymphocytes. It is remarkable that so few cells
with a particular specificity can accomplish the
difficult task of combating various microbes; the
immune system has developed many
mechanisms for optimizing reactions to
microbial antigens. It is also remarkable that the
system is capable of producing so many
receptors, far more than could be individually
encoded in the genome. The mechanisms by
which this happens are now well understood.
Antigen receptor diversity is generated by
somatic recombination of the genes that encode
the receptor proteins. All cells of the body,
including lymphocyte progenitors, contain
antigen receptor genes in the germline
(inherited) configuration, in which the genes
encoding these receptors consist of spatially
separated segments that cannot be expressed
as proteins. During lymphocyte maturation (in
the thymus for T cells and the bone marrow for B
cells), these gene segments recombine in
random sets and variations are introduced at the
sites of recombination, forming many different
genes that can be transcribed and translated
into functional antigen receptors. The enzyme in
developing lymphocytes that mediates
recombination of these gene segments is the
product of RAG-1 and RAG-2 (recombination
activating genes); inherited defects in RAG
proteins result in a failure to generate mature
lymphocytes. It is important to note that
germline antigen receptor genes are present in
all cells in the body, but only T and B cells
contain recombined (also called rearranged)
antigen receptor genes (the T-cell receptor
[TCR] in T cells and immunoglobulin [Ig] in B
cells). Hence, the presence of recombined TCR
or Ig genes, which can be demonstrated by
molecular analysis, is a marker of T- or B-lineage
cells. Furthermore, because each T or B cell and
its clonal progeny have a unique DNA
rearrangement (and hence a unique antigen
receptor), it is possible to distinguish polyclonal
(nonneoplastic) lymphocyte proliferations from
monoclonal (neoplastic) lymphoid tumors. Thus,
analysis of antigen receptor gene
rearrangements is a valuable assay for detecting
tumors derived from lymphocytes.
T Lymphocytes
There are three major populations of T cells,
which serve distinct functions.
Helper T lymphocytes stimulate B lymphocytes
to make antibodies and activate other
leukocytes (e.g., phagocytes) to destroy
microbes; cytotoxic T lymphocytes (CTLs) kill
infected cells; and regulatory T lymphocytes
limit immune responses and prevent reactions
against self antigens.
T lymphocytes develop in the thymus from
precursors that arise from hematopoietic stem
cells. Mature T cells are found in the blood,
where they constitute 60% to 70% of
lymphocytes, and in T-cell zones of peripheral
lymphoid organs . Each T cell recognizes a
specific cell-bound antigen by means of an
antigen-specific TCR. In approximately 95% of T
cells, the TCR consists of a disulfide-linked
heterodimer made up of an α and a β polypeptide
chain , each having a variable (antigen-binding)
region and a constant region. The αβ TCR
recognizes peptide antigens that are presented
by major histocompatibility complex (MHC)
molecules on the surfaces of antigen-presenting
cells. By limiting the specificity of T cells for
peptides displayed by cell surface MHC
molecules, called MHC restriction, the immune
system ensures that T cells see only cell-
associated antigens (e.g., those derived from
microbes in cells or from proteins ingested by
cells).
Each TCR is noncovalently linked to six
polypeptide chains, which form the CD3 complex
and the ζ chain dimer (Fig. 6-5). The CD3 and ζ
proteins are invariant (i.e., identical) in all T
cells. They are involved in the transduction of
signals into the T cell that are triggered by
binding of antigen to the TCR. Together with the
TCR, these proteins form the TCR complex.
A small population of mature T cells expresses
another type of TCR composed of γ and δ
polypeptide chains. The γδ TCR recognizes
peptides, lipids, and small molecules, without a
requirement for display by MHC proteins. γδ T
cells tend to aggregate at epithelial surfaces,
such as the skin and mucosa of the
gastrointestinal and urogenital tracts,
suggesting that these cells are sentinels that
protect against microbes that try to enter
through epithelia. However, the functions of γδ T
cells are not established. Another small subset
of T cells expresses markers that are also found
on NK cells; these cells are called NK-T cells.
NK-T cells express a very limited diversity of
TCRs, and they recognize glycolipids that are
displayed by the MHC- like molecule CD1. The
functions of NK-T cells are also not well defined.
In addition to CD3 and ζ proteins, T cells express
several other proteins that assist the TCR
complex in functional responses. These include
CD4, CD8, CD28, and integrins. CD4 and CD8 are
expressed on two mutually exclusive subsets of
αβ T cells. Approximately 60% of mature T cells
are CD4+ and about 30% are CD8+. Most CD4+ T
cells function as cytokine-secreting helper cells
that assist mac- rophages and B lymphocytes to
combat infections. Most CD8+ cells function as
cytotoxic (killer) T lymphocytes (CTLs) to
destroy host cells harboring microbes. CD4 and
CD8 serve as coreceptors in T-cell activation, so
called because they recognize a part of the
same ligand that the antigen receptor sees.
During antigen recognition, CD4 molecules bind
to class II MHC molecules that are display- ing
antigen (Fig. 6-5), and CD8 molecules bind to
class I MHC molecules, and the CD4 or CD8
coreceptor initiates signals that are necessary
for activation of the T cells. Because of this
requirement for coreceptors, CD4+ helper T cells
can recognize and respond to antigen displayed
only by class II MHC molecules, whereas CD8+
cytotoxic T cells recognize cell-bound antigens
only in association with class I MHC molecules;
this segregation is described later. Integrins are
adhesion molecules that promote the
attachment of T-cells to APCs.
To respond, T cells have to recognize not only
antigen- MHC complexes but additional signals
provided by anti- gen-presenting cells. This
process, in which CD28 plays an important role,
is described later, when the steps in cell-
mediated immune responses are summarized.
B Lymphocytes
B lymphocytes are the only cells in the body
capable of producing antibody molecules, the
mediators of humoral immunity. B lymphocytes
develop from precursors in the bone marrow.
Mature B cells constitute 10% to 20% of the
circulating peripheral lymphocyte population and
are also present in peripheral lymphoid tissues
such as lymph nodes, spleen, and mucosa-
associated lymphoid tissues. B cells recognize
antigen via the B-cell antigen receptor complex.
Membrane-bound antibodies of the IgM and IgD
isotypes, present on the surface of all mature,
naive B cells, are the antigen-binding component
of the B-cell receptor complex . After stimulation
by antigen and other signals (described later), B
cells develop into plasma cells, veritable protein
factories for antibodies. It is estimated that a
single plasma cell can secrete hundreds to
thousands f antibody molecules per second, a
remarkable measure of the power of the immune
response for combating pathogens. Antibody-
secreting cells are also detected in human
peripheral blood; these are called plasmablasts.
In addition to membrane Ig, the B-cell antigen
receptor complex contains a heterodimer of two
invariant proteins called Igα and Igβ. Similar to
the CD3 and ζ proteins of the TCR complex, Igα
(CD79a) and Igβ (CD79b) are essential for signal
transduction through the antigen receptor. B
cells also express several other molecules that
are essential for their responses. These include
the type 2 complement receptor (CR2, or CD21),
which recognizes complement products
generated during innate immune responses to
microbes, and CD40, which receives signals from
helper T cells. CR2 is also used by the Epstein-
Barr virus (EBV) as a receptor to enter and infect
B cells.
Dendritic Cells
Dendritic cells (sometimes called interdigitating
dendritic cells) are the most important antigen-
presenting cells for initiating T-cell responses
against protein antigens. These cells have
numerous fine cytoplasmic processes that
resemble dendrites, from which they derive their
name. Several features of dendritic cells
account for their key role in antigen
presentation. First, these cells are located at the
right place to capture antigens—under epithelia,
the common site of entry of microbes and
foreign antigens, and in the interstitia of all
tissues, where antigens may be produced.
Immature dendritic cells within the epidermis
are called Langerhans cells.
Second, dendritic cells express many receptors
for capturing and responding to microbes (and
other antigens), including TLRs and lectins.
Third, in response to microbes, dendritic cells
are recruited to the T-cell zones of lymphoid
organs, where they are ideally located to present
antigens to T cells.
Fourth, dendritic cells express high levels of
MHC and other molecules needed for presenting
antigens to and activating T cells.
A second type of cell with dendritic morphology
is present in the germinal centers of lymphoid
follicles in the spleen and lymph nodes and is
called the follicular dendritic cell. These cells
bear Fc receptors for IgG and receptors for C3b
and can trap antigen bound to antibodies or
comple- ment proteins. Such cells play a role in
humoral immune responses by presenting
antigens to B cells and selecting the B cells that
have the highest affinity for the antigen, thus
improving the quality of the antibody produced.
Macrophages
Macrophages are a part of the mononuclear
phagocyte system.
• Macrophages that have phagocytosed microbes
and protein antigens process the antigens
and present peptide fragments to T cells.
Thus, macrophages function as antigen-
presenting cells in T-cell activation.
• Macrophages are key effector cells in certain
forms of cell-mediated immunity, the
reaction that serves to eliminate
intracellular microbes. In this type of
response, T cells activate macrophages and
enhance their ability to kill ingested
microbes .
Macrophages also participate in the effector
phase of humoral immunity. Macrophages
efficiently phagocytose and destroy microbes
that are opsonized (coated) by IgG or C3b.
Natural Killer Cells The function of NK cells is
to destroy irreversibly stressed and abnormal
cells, such as virus-infected cells and tumor
cells. NK cells make up approximately 5% to
10% of peripheral blood lymphocytes. They do
not express TCRs or Ig. Morphologically, NK
cells are somewhat larger than small
lymphocytes, and they contain abundant
azurophilic granules. NK cells are endowed with
the ability to kill a variety of virus-infected cells
and tumor cells, without prior exposure to or
activation by these microbes or tumors. This
ability makes NK cells an early line of defense
against viral infections and, perhaps, some
tumors. Two cell surface molecules, CD16 and
CD56, are commonly used to identify NK cells.
CD16 is an Fc receptor for IgG, and it confers on
NK cells the ability to lyse IgG-coated target
cells. This phenomenon is known as antibody-
dependent cell-mediated cytotoxicity (ADCC).
The function of CD56 is not known.
The functional activity of NK cells is regulated
by a balance between signals from activating
and inhibitory receptors . There are many types
of activating receptors, of which the NKG2D
family is the best character- ized. The NKG2D
receptors recognize surface molecules that are
induced by various kinds of stress, such as
infection and DNA damage. NK cell inhibitory
receptors recognize self class I MHC molecules,
which are expressed on all healthy cells. The
inhibitory receptors prevent NK cells from killing
normal cells. Virus infection or neoplastic
transformation often enhances expression of
ligands for activating receptors and at the same
time reduces the expression of class I MHC
molecules. As a result the balance is tilted
toward activation, and the infected or tumor cell
is killed.
NK cells also secrete cytokines such as
interferon-γ (IFN-γ), which activates
macrophages to destroy ingested microbes, and
thus NK cells provide early defense against
intracellular microbial infections. The activity of
NK cells is regulated by many cytokines,
including the interleukins IL-2, IL-15, and IL-12.
IL-2 and IL-15 stimulate proliferation of NK cells,
whereas IL-12 activates killing and secretion of
IFN-γ.
Innate Lymphoid Cells (ILCs)
Recent studies have identified populations of
lymphocytes that lack TCRs but produce
cytokines similar to those that are made by T
cells. NK cells are considered the first defined
ILC. Different subsets of ILCs produce IFN-γ, IL-5,
IL-17, and IL-22. The functions that have been
attributed to ILCs include:
• Early defense against infections
• Recognition and elimination of stressed cells
(so-called stress surveillance)
• Shaping the later adaptive immune response,
by pro- viding cytokines that influence the
differentiation of T lymphocytes.
Interest in these cells has been spurred by
the hypothesis that they are early
participants in inflammatory diseases,
primarily as a source of cytokines. However,
much remains to be learned about the
functions and roles of these cells in normal
and pathologic immune responses.
Tissues of the Immune System
The tissues of the immune system consist of the
generative (also called primary, or central)
lymphoid organs, in which T and B lymphocytes
mature and become competent to respond to
antigens, and the peripheral (or secondary)
lymphoid organs, in which adaptive immune
responses to microbes are initiated.
Generative Lymphoid Organs
The principal generative lymphoid organs are the
thymus, where T cells develop, and the bone
marrow, the site of production of all blood cells
and where B lymphocytes mature.
Peripheral Lymphoid Organs
The peripheral lymphoid organs—lymph nodes,
spleen, and the mucosal and cutaneous
lymphoid tissues—are organized to concentrate
antigens, antigen-presenting cells, and
lymphocytes in a way that optimizes interactions
among these cells and the development of
adaptive immune responses.
• Lymph nodes are nodular aggregates of
lymphoid tissues located along lymphatic
channels throughout the body . As lymph
slowly suffuses through lymph nodes,
antigen-presenting cells in the nodes are
able to sample the antigens of microbes that
may enter through epithelia into tissues and
are carried in the lymph. In addition,
dendritic cells pick up and transport
antigens of microbes from epithelia and
tissues via lymphatic vessels to the lymph
nodes. Thus, the antigens of microbes that
enter through epithelia or colonize tissues
become concentrated in draining lymph
nodes.
• The spleen is an abdominal organ that serves
the same role in immune responses to
bloodborne antigen as the lymph nodes do in
responses to lymph-borne antigens. Blood
entering the spleen flows through a network
of sinusoids. Bloodborne antigens are
trapped by dendritic cells and macrophages
in the spleen.
The cutaneous and mucosal lymphoid systems
are located under the epithelia of the skin and
the gastrointestinal and respiratory tracts,
respectively. They respond to antigens that
enter through breaches in the epithelium.
Pharyngeal tonsils and Peyer’s patches of the
intestine are two anatomically defined mucosal
lymphoid tissues. At any time, more than half the
body’s lymphocytes are in the mucosal tissues
(reflecting the large size of these tissues), and
many of these are memory cells.
Within the peripheral lymphoid organs, T
lymphocytes and B lymphocytes are segregated
into different regions . In lymph nodes the B cells
are concentrated in discrete structures, called
follicles, located around the periphery, or cortex,
of each node. If the B cells in a follicle have
recently responded to an antigen, this follicle
may contain a central region called a germinal
center. The T lymphocytes are concentrated in
the paracortex, adjacent to the follicles. The
follicles contain the follicular dendritic cells that
are involved in the activation of B cells, and the
paracortex contains the dendritic cells that
present antigens to T lymphocytes. In the
spleen, T lymphocytes are concentrated in
periarteriolar lymphoid sheaths surrounding
small arterioles, and B cells reside in the
follicles.
Lymphocyte Recirculation
Lymphocytes constantly recirculate between
tissues and home to particular sites; naive
lymphocytes traverse the peripheral lymphoid
organs where immune responses are initiated,
and effector lymphocytes migrate to sites of
infection and inflammation. This process of
lymphocyte recirculation is most important for T
cells, because naïve T cells have to circulate
through the peripheral lymphoid organs where
antigens are concentrated and effector T cells
have to locate and eliminate microbes at any
site of infection. In contrast, plasma cells remain
in lymphoid organs and the bone marrow and do
not need to migrate to sites of infection because
they secrete antibodies that are carried to
distant tissues.
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Outpatient Referral Guidelines: NeurosurgeryDokument11 SeitenOutpatient Referral Guidelines: NeurosurgeryYuvraj Chauhan100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Dustin & Baldari, 2017 - The Immune Synapse PDFDokument581 SeitenDustin & Baldari, 2017 - The Immune Synapse PDFjill142Noch keine Bewertungen
- Immnunology Notebook Chapter One: Innate ImmunityDokument45 SeitenImmnunology Notebook Chapter One: Innate ImmunityJavier Alejandro Daza GalvánNoch keine Bewertungen
- ImmunologyDokument80 SeitenImmunologyMaged HusseinNoch keine Bewertungen
- Understanding Toxic Epidermal NecrolysisDokument13 SeitenUnderstanding Toxic Epidermal NecrolysisHend AbdallaNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Basic ImmunologyDokument29 SeitenBasic ImmunologyHema Duddukuri0% (1)
- IMMUNITY: A Concise Guide to Innate and Acquired ImmunityDokument190 SeitenIMMUNITY: A Concise Guide to Innate and Acquired ImmunityFathima100% (1)
- Bispecific Antibodies - Kontermann (Ebook) PDFDokument363 SeitenBispecific Antibodies - Kontermann (Ebook) PDForkboss77100% (1)
- Topics For FinalsDokument3 SeitenTopics For FinalsYuvraj ChauhanNoch keine Bewertungen
- Neurosurgery Referral Guidelines for Valley Specialty CenterDokument8 SeitenNeurosurgery Referral Guidelines for Valley Specialty CenterYuvraj ChauhanNoch keine Bewertungen
- ASSIGNMENTDokument7 SeitenASSIGNMENTYuvraj ChauhanNoch keine Bewertungen
- Pathology Study GuideDokument1 SeitePathology Study GuideYuvraj ChauhanNoch keine Bewertungen
- Cardiac ArrhythmiaDokument101 SeitenCardiac ArrhythmiaYuvraj ChauhanNoch keine Bewertungen
- Pharmacology Topics 2020Dokument2 SeitenPharmacology Topics 2020Yuvraj ChauhanNoch keine Bewertungen
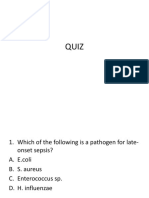
- Quiz on sepsis, apnea of prematurity, and neonatal conditionsDokument14 SeitenQuiz on sepsis, apnea of prematurity, and neonatal conditionsYuvraj ChauhanNoch keine Bewertungen
- Congenital Heart DiseasesDokument10 SeitenCongenital Heart DiseasesYuvraj ChauhanNoch keine Bewertungen
- Cancer ChemotherapyDokument64 SeitenCancer ChemotherapyYuvraj ChauhanNoch keine Bewertungen
- Types of VaccinesDokument220 SeitenTypes of VaccinesYuvraj ChauhanNoch keine Bewertungen
- Disease of Immune SystemDokument29 SeitenDisease of Immune SystemYuvraj ChauhanNoch keine Bewertungen
- PD QuestionsDokument8 SeitenPD QuestionsYuvraj ChauhanNoch keine Bewertungen
- FatigueDokument55 SeitenFatigueYuvraj ChauhanNoch keine Bewertungen
- What is Bioethics? Exploring its Origins, Scope and Controversial IssuesDokument19 SeitenWhat is Bioethics? Exploring its Origins, Scope and Controversial IssuesYuvraj ChauhanNoch keine Bewertungen
- 1Dokument19 Seiten1Yuvraj ChauhanNoch keine Bewertungen
- 1Dokument19 Seiten1Yuvraj ChauhanNoch keine Bewertungen
- BrainDokument1 SeiteBrainYuvraj ChauhanNoch keine Bewertungen
- File For SCRB To DownloadDokument1 SeiteFile For SCRB To DownloadYuvraj ChauhanNoch keine Bewertungen
- File For SCRB To DownloadDokument1 SeiteFile For SCRB To DownloadYuvraj ChauhanNoch keine Bewertungen
- BrainDokument2 SeitenBrainYuvraj ChauhanNoch keine Bewertungen
- I'm Reading "Chapter 6 - Immune Diseases (Part I) (Robbins and Cotran PathologicDokument1 SeiteI'm Reading "Chapter 6 - Immune Diseases (Part I) (Robbins and Cotran PathologicYuvraj ChauhanNoch keine Bewertungen
- IMTX PatentDokument72 SeitenIMTX PatentCharles GrossNoch keine Bewertungen
- J Exp Med 1991 Linsley 721 30Dokument10 SeitenJ Exp Med 1991 Linsley 721 30Fernanda RibeiroNoch keine Bewertungen
- Seminar 4 Prepoznavanje Antigena U Stečenoj ImunostiDokument28 SeitenSeminar 4 Prepoznavanje Antigena U Stečenoj ImunostidocaNoch keine Bewertungen
- 9700 s02 QP 2 PDFDokument12 Seiten9700 s02 QP 2 PDFIG UnionNoch keine Bewertungen
- Immunosero Trans4Dokument5 SeitenImmunosero Trans4Jan Francis Kevin YasisNoch keine Bewertungen
- Type 1 Diabetes Mellitus POSTERDokument1 SeiteType 1 Diabetes Mellitus POSTERLeandro FigueiraNoch keine Bewertungen
- 2018 - 05 IssuDokument188 Seiten2018 - 05 IssuEduardo RomeroNoch keine Bewertungen
- Major Histocompatibility Complex 12032018Dokument39 SeitenMajor Histocompatibility Complex 12032018Kelly YeowNoch keine Bewertungen
- Mouse Cell Surface MarkersDokument9 SeitenMouse Cell Surface Markersavalon784Noch keine Bewertungen
- Pathogenesis, Diagnosis and Treatment of Rasmussen EncephalitisDokument20 SeitenPathogenesis, Diagnosis and Treatment of Rasmussen Encephalitisidno1008Noch keine Bewertungen
- Mathematics in Modern ImmunologyDokument14 SeitenMathematics in Modern ImmunologyFeby ArdhaniNoch keine Bewertungen
- 9700 s02 QP 2Dokument12 Seiten9700 s02 QP 2wegdanNoch keine Bewertungen
- Immune Response Regulation by Antigen Receptors' Clone-Specific Nonself PartsDokument14 SeitenImmune Response Regulation by Antigen Receptors' Clone-Specific Nonself PartsMohammed R.HusseinNoch keine Bewertungen
- The Major Histocompatibility Complex of Genes: ©dr. Colin R.A. HewittDokument58 SeitenThe Major Histocompatibility Complex of Genes: ©dr. Colin R.A. HewittErmi WatiNoch keine Bewertungen
- Immunology First Exam..Dokument7 SeitenImmunology First Exam..Abdallah Essam Al-Zireeni100% (1)
- BMS2 Microbiology Innate ImmunityDokument40 SeitenBMS2 Microbiology Innate ImmunityAbd El-Rahman SalahNoch keine Bewertungen
- Novel VaccineDokument16 SeitenNovel Vaccineparam540Noch keine Bewertungen
- VMC Unit IV Notes 2017 BVSc&AH March 20 2019 PDFDokument99 SeitenVMC Unit IV Notes 2017 BVSc&AH March 20 2019 PDFAbhijith S. PNoch keine Bewertungen
- Human Leukocyte Antigen (HLA) System: Alkitab University College of Technology Medical Department of Medical AnalysisDokument4 SeitenHuman Leukocyte Antigen (HLA) System: Alkitab University College of Technology Medical Department of Medical AnalysisMohammed R.HusseinNoch keine Bewertungen
- Bizhub 163 211 SM Field ServiceDokument47 SeitenBizhub 163 211 SM Field ServiceRuben Troncoso100% (1)
- Cancer Inmunoterapia Rasl1Dokument13 SeitenCancer Inmunoterapia Rasl1missbearNoch keine Bewertungen
- Caps HTMLDokument152 SeitenCaps HTMLUchy Luph'milimiLy0% (1)
- Archives of Pathology & Laboratory Medicine Online - Acute Leukemia Immunohistochemistry - A Systematic Diagnostic ApproachDokument13 SeitenArchives of Pathology & Laboratory Medicine Online - Acute Leukemia Immunohistochemistry - A Systematic Diagnostic Approachpooo80Noch keine Bewertungen