Beruflich Dokumente
Kultur Dokumente
Therapy Studies What Question Did The Study Ask?: Centre For Evidence-Based Medicine, University of Oxford, 20101
Hochgeladen von
Apt RiskaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Therapy Studies What Question Did The Study Ask?: Centre For Evidence-Based Medicine, University of Oxford, 20101
Hochgeladen von
Apt RiskaCopyright:
Verfügbare Formate
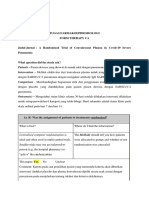
Critical Appraisal for Therapy Articles Worksheet
THERAPY STUDIES
What question did the study ask?
Patients – Intervention - Comparison - Outcome(s) –
Step 1: Are the results of the trial valid? (Internal Validity)
1a. R- Was the assignment of patients to treatments randomised?
What is best? Where do I find the information?
Centralised computer randomisation is ideal and often The Methods should tell you how patients were allocated
used in multi-centred trials. Smaller trials may use an to groups and whether or not randomisation was
independent person (e.g, hospital pharmacy) to “police” concealed.
the randomization.
This paper: Yes No Unclear
Comment:
1b. R- Were the groups similar at the start of the trial?
What is best? Where do I find the information?
If the randomisation process worked (that is, achieved The Results should have a table of "Baseline
comparable groups) the groups should be similar. The Characteristics" comparing the randomized groups on a
more similar the groups the better it is. number of variables that could affect the outcome (ie. age,
There should be some indication of whether differences risk factors etc). If not, there may be a description of group
between groups are statistically significant (ie. p values). similarity in the first paragraphs of the Results section.
This paper: Yes No Unclear
Comment:
2a. A – Aside from the allocated treatment, were groups treated equally?
What is best? Where do I find the information?
Apart from the intervention the patients in the different Look in the Methods section for the follow-up schedule,
groups should be treated the same, eg., additional and permitted additional treatments, etc and in Results for
treatments or tests. actual use.
This paper: Yes No Unclear
Comment:
2b. A – Were all patients who entered the trial accounted for? – and were they
analysed in the groups to which they were randomised?
What is best? Where do I find the information?
Losses to follow-up should be minimal – preferably less The Results section should say how many patients were
than 20%. However, if few patients have the outcome of andomised (eg., Baseline Characteristics table) and how
interest, then even small losses to follow-up can bias the many patients were actually included in the analysis. You
results. Patients should also be analysed in the groups to will need to read the results section to clarify the number
which they were randomised – ‘intention-to-treat analysis’. and reason for losses to follow-up.
This paper: Yes No Unclear
Comment:
3. M - Were measures objective or were the patients and clinicians kept “blind”
to which treatment was being received?
What is best? Where do I find the information?
It is ideal if the study is ‘double-blinded’ – that is, both First, look in the Methods section to see if there is some
patients and investigators are unaware of treatment mention of masking of treatments, eg., placebos with the
allocation. If the outcome is objective (eg., death) then same appearance or sham therapy. Second, the Methods
blinding is less critical. If the outcome is subjective (eg., section should describe how the outcome was assessed
symptoms or function) then blinding of the outcome and whether the assessor/s were aware of the patients'
assessor is critical. treatment.
This paper: Yes No Unclear
Comment:
Centre for Evidence-based Medicine, University of Oxford, 20101
Critical Appraisal for Therapy Articles Worksheet
Step 2: What were the results?
1. How large was the treatment effect?
Most often results are presented as dichotomous outcomes (yes or not outcomes that happen or don't
happen) and can include such outcomes as cancer recurrence, myocardial infarction and death.
Consider a study in which 15% (0.15) of the control group died and 10% (0.10) of the treatment group
died after 2 years of treatment. The results can be expressed in many ways as shown below.
What is the measure? What does it mean?
Relative Risk (RR) = risk of the outcome in the The relative risk tells us how many times more likely it is that
treatment group / risk of the outcome in the control an event will occur in the treatment group relative to the control
group. group. An RR of 1 means that there is no difference between the
two groups thus, the treatment had no effect. An RR < 1 means
that the treatment decreases the risk of the outcome. An RR > 1
means that the treatment increased the risk of the outcome.
In our example, the RR = 0.10/0.15 = 0.67 Since the RR < 1, the treatment decreases the risk of death.
Absolute Risk Reduction (ARR) = risk of the The absolute risk reduction tells us the absolute difference in the
outcome in the control group - risk of the outcome rates of events between the two groups and gives an indication
in the treatment group. This is also known as the of the baseline risk and treatment effect. An ARR of 0 means
absolute risk difference. that there is no difference between the two groups thus, the
treatment had no effect.
In our example, the ARR = 0.15 - 0.10 = 0.05 or 5% The absolute benefit of treatment is a 5% reduction in the death
rate.
Relative Risk Reduction (RRR) = absolute risk The relative risk reduction is the complement of the RR and is
reduction / risk of the outcome in the control group. probably the most commonly reported measure of treatment
An alternative way to calculate the RRR is to effects. It tells us the reduction in the rate of the outcome in the
subtract the RR from 1 (eg. RRR = 1 - RR) treatment group relative to that in the control group.
In our example, the RRR = 0.05/0.15 = 0.33 or 33% The treatment reduced the risk of death by 33% relative to that
Or RRR = 1 - 0.67 = 0.33 or 33% occurring in the control group.
Number Needed to Treat (NNT) = inverse of the The number needed to treat represents the number of patients
ARR and is calculated as 1 / ARR. we need to treat with the experimental therapy in order to
prevent 1 bad outcome and incorporates the duration of
treatment. Clinical significance can be determined to some
extent by looking at the NNTs, but also by weighing the NNTs
against any harms or adverse effects (NNHs) of therapy.
In our example, the NNT = 1/ 0.05 = 20 We would need to treat 20 people for 2 years in order to prevent
1 death.
2. How precise was the estimate of the treatment effect?
The true risk of the outcome in the population is not known and the best we can do is estimate the true risk based on the
sample of patients in the trial. This estimate is called the point estimate. We can gauge how close this estimate is to the
true value by looking at the confidence intervals (CI) for each estimate. If the confidence interval is fairly narrow then we
can be confident that our point estimate is a precise reflection of the population value. The confidence interval also
provides us with information about the statistical significance of the result. If the value corresponding to no effect falls
outside the 95% confidence interval then the result is statistically significant at the 0.05 level. If the confidence interval
includes the value corresponding to no effect then the results are not statistically significant.
Step 3: Will the results help me in caring for my patient?
(ExternalValidity/Applicability)
The questions that you should ask before you decide to apply the results of the study to your patient are:
Is my patient so different to those in the study that the results cannot apply?
Is the treatment feasible in my setting?
Will the potential benefits of treatment outweigh the potential harms of treatment for my patient?
Centre for Evidence-based Medicine, University of Oxford, 20102
Das könnte Ihnen auch gefallen
- RCT Appraisal Sheets 2005 EnglishDokument2 SeitenRCT Appraisal Sheets 2005 EnglishF NNoch keine Bewertungen
- Worksheet Therapy-CebmDokument3 SeitenWorksheet Therapy-Cebmteddy sNoch keine Bewertungen
- Worksheet Therapy CebmDokument3 SeitenWorksheet Therapy Cebmandynightmare97Noch keine Bewertungen
- Patients - Intervention - Comparison - Outcome(s)Dokument3 SeitenPatients - Intervention - Comparison - Outcome(s)Intan SetyadewiNoch keine Bewertungen
- RCT Appraisal Sheets 2005 EnglishDokument4 SeitenRCT Appraisal Sheets 2005 EnglishAmanda SoebadiNoch keine Bewertungen
- Centralised Computer Randomisation Is: Critical Appraisal For Therapy ArticlesDokument4 SeitenCentralised Computer Randomisation Is: Critical Appraisal For Therapy ArticleshadzaliegNoch keine Bewertungen
- Patients - Intervention - Comparison - Outcome(s) - Knowledge GapDokument4 SeitenPatients - Intervention - Comparison - Outcome(s) - Knowledge GapAmal NajiNoch keine Bewertungen
- Worksheet Appraisal AZALEADokument5 SeitenWorksheet Appraisal AZALEAArini NurlelaNoch keine Bewertungen
- (OBAT CINA) CAT TherapyDokument6 Seiten(OBAT CINA) CAT TherapyArga PRNoch keine Bewertungen
- RCT Appraisal Sheets 2005 English-2Dokument6 SeitenRCT Appraisal Sheets 2005 English-2tsyrahmaniNoch keine Bewertungen
- Referat Iktiosis PembahasanDokument4 SeitenReferat Iktiosis PembahasanPatih GajahmadaNoch keine Bewertungen
- RCT Appraisal Sheets 2005 English-1 1Dokument5 SeitenRCT Appraisal Sheets 2005 English-1 1api-479716004Noch keine Bewertungen
- Centralised Computer Randomisation IsDokument4 SeitenCentralised Computer Randomisation IsAhmad BukhariNoch keine Bewertungen
- Patients - Intervention - Comparison - Outcome(s)Dokument4 SeitenPatients - Intervention - Comparison - Outcome(s)Ainur 'iin' RahmahNoch keine Bewertungen
- RCT+Appraisal+sheets 2005Dokument3 SeitenRCT+Appraisal+sheets 2005Otty Mitha OctrizaNoch keine Bewertungen
- Patients - Intervention - Comparison - Outcome(s)Dokument4 SeitenPatients - Intervention - Comparison - Outcome(s)sahirbuleNoch keine Bewertungen
- CRITICAL APPRAISAL Mas WikoDokument10 SeitenCRITICAL APPRAISAL Mas WikoEliataMariaMahanaimNoch keine Bewertungen
- RCT Appraisal Sheets 2005 English-2Dokument3 SeitenRCT Appraisal Sheets 2005 English-2VeysusanNoch keine Bewertungen
- Therapy RCT Critical Appraisal Worksheet With ExplanationDokument2 SeitenTherapy RCT Critical Appraisal Worksheet With ExplanationAdwin AlamsyaputraNoch keine Bewertungen
- Randomised: Differences Between Groups Are Statistically Significant P ValuesDokument6 SeitenRandomised: Differences Between Groups Are Statistically Significant P ValuesArga PRNoch keine Bewertungen
- Critical Appraisal TafaDokument7 SeitenCritical Appraisal TafaFabric FameNoch keine Bewertungen
- Critical Appraisal Jurnal Asam Traneksamat Pada MelasmaDokument4 SeitenCritical Appraisal Jurnal Asam Traneksamat Pada MelasmaMsrirrrNoch keine Bewertungen
- Critical Appraisal For Therapy Articles: Are The Results of The Trial Valid? (Internal Validity)Dokument4 SeitenCritical Appraisal For Therapy Articles: Are The Results of The Trial Valid? (Internal Validity)Putri Widya AndiniNoch keine Bewertungen
- RCT Appraisal Sheets 2005 English-2Dokument4 SeitenRCT Appraisal Sheets 2005 English-2Mahardhika AcintyaNoch keine Bewertungen
- CA Therapy Artikel 09Dokument5 SeitenCA Therapy Artikel 09Christiana TrijayantiNoch keine Bewertungen
- Critical ApraisalDokument4 SeitenCritical Apraisalfauziah qurrota a'yuniNoch keine Bewertungen
- Kritisi Artikel - Ni Nengah Susilawati - 152191105 - BDokument5 SeitenKritisi Artikel - Ni Nengah Susilawati - 152191105 - BShilaNoch keine Bewertungen
- Tugas Farepid - CA - 198114152Dokument11 SeitenTugas Farepid - CA - 198114152JeanieNoch keine Bewertungen
- Telaah Kritis Jurnal 2Dokument9 SeitenTelaah Kritis Jurnal 2Ayu Vitha ViginiaNoch keine Bewertungen
- Presentation On TherapyDokument21 SeitenPresentation On TherapyMarjorie CepeNoch keine Bewertungen
- Critical Appraisal Therapy Study by DR BhismaDokument28 SeitenCritical Appraisal Therapy Study by DR BhismaAhmadAfiyyuddinNoch keine Bewertungen
- Worksheet Therapy CebmDokument5 SeitenWorksheet Therapy CebmZulfan RifqiawanNoch keine Bewertungen
- EBM Dan Critical AppraisalDokument7 SeitenEBM Dan Critical AppraisalNovia Ariani DewiNoch keine Bewertungen
- Therapystudy: Are The Results of The Trial Valid? (Internal Validity)Dokument6 SeitenTherapystudy: Are The Results of The Trial Valid? (Internal Validity)Sinta AgustinaNoch keine Bewertungen
- Crit AppDokument5 SeitenCrit AppdikkaNoch keine Bewertungen
- Critical Appraisal Checklist For An Article On Treatment or PreventionDokument4 SeitenCritical Appraisal Checklist For An Article On Treatment or PreventionSaina AbasNoch keine Bewertungen
- Critical Appraisal Checklist For An Article OnDokument4 SeitenCritical Appraisal Checklist For An Article OnTiaz DiniutamiNoch keine Bewertungen
- C - II - 3 - Critical AppraisalDokument10 SeitenC - II - 3 - Critical AppraisalWahyu NandaNoch keine Bewertungen
- Therapystudy: Are The Results of The Trial Valid? (Internal Validity)Dokument10 SeitenTherapystudy: Are The Results of The Trial Valid? (Internal Validity)WiraNoch keine Bewertungen
- RCT+Appraisal+sheets. TherapyDokument2 SeitenRCT+Appraisal+sheets. Therapydian_c87Noch keine Bewertungen
- Critical Appraisal of TherapyDokument34 SeitenCritical Appraisal of Therapyapi-19733840Noch keine Bewertungen
- Checklist RCTDokument5 SeitenChecklist RCTFajar SukmajayaNoch keine Bewertungen
- Anesthesiologists (ASA) I: THERAPY STUDY: Are The Results of The Trial Valid? (Internal Validity)Dokument4 SeitenAnesthesiologists (ASA) I: THERAPY STUDY: Are The Results of The Trial Valid? (Internal Validity)Sandra Lydiayana Aisyah AzharNoch keine Bewertungen
- Critical Appraisal of Articles On TherapyDokument46 SeitenCritical Appraisal of Articles On TherapyAditya Rachman Van Der ArjunaqueeNoch keine Bewertungen
- Angel Yudiakristi - Praktikum 5Dokument10 SeitenAngel Yudiakristi - Praktikum 5Angel MaharaniNoch keine Bewertungen
- Table 2A: Worksheet Critical Appraisal Article Therapy Questions Your AnswerDokument10 SeitenTable 2A: Worksheet Critical Appraisal Article Therapy Questions Your Answer7CANTIKA PRAMESWARI HANANTONoch keine Bewertungen
- EBM Worksheets (Therapy, Diagnosis, Prognosis, Economic, Guideline, Decision Making)Dokument15 SeitenEBM Worksheets (Therapy, Diagnosis, Prognosis, Economic, Guideline, Decision Making)Soffatul AzizahNoch keine Bewertungen
- Evaluating RCTs For PracticeDokument11 SeitenEvaluating RCTs For PracticeJoanna RiveraNoch keine Bewertungen
- (CPG) Philippine Periodic Health Examination Phase 1 - Evidence SummariesDokument159 Seiten(CPG) Philippine Periodic Health Examination Phase 1 - Evidence SummariesKaren Mae PadillaNoch keine Bewertungen
- A List A Statistical Definition For The CICM Fellowship ExamDokument5 SeitenA List A Statistical Definition For The CICM Fellowship ExamSimon WongNoch keine Bewertungen
- Critical AppraisalDokument71 SeitenCritical Appraisaloddone_outNoch keine Bewertungen
- Evidence-Based Medicine Therapy: Dr. Rina Amelia, MARSDokument43 SeitenEvidence-Based Medicine Therapy: Dr. Rina Amelia, MARSRezky IlhamNoch keine Bewertungen
- TherappraisalclrDokument5 SeitenTherappraisalclrMike CabotageNoch keine Bewertungen
- Critical Appraisal 2017Dokument65 SeitenCritical Appraisal 2017Fransiscus RivaldyNoch keine Bewertungen
- Critical Appraisal of An RCTDokument2 SeitenCritical Appraisal of An RCTomboNoch keine Bewertungen
- Evidence-Based Medicine Therapy: Dr. Dr. Rina Amelia, MARS Departemen Kedokteran Komunitas FK USUDokument40 SeitenEvidence-Based Medicine Therapy: Dr. Dr. Rina Amelia, MARS Departemen Kedokteran Komunitas FK USUSamuel TanNoch keine Bewertungen
- What Are Confidence Intervals and P-Values?Dokument8 SeitenWhat Are Confidence Intervals and P-Values?Mostafa Abdelrahman0% (1)
- Therapy Worksheet Title of Article: Authors: Journal: BackgroundDokument3 SeitenTherapy Worksheet Title of Article: Authors: Journal: BackgroundRandi Kosim SiregarNoch keine Bewertungen
- Multivariate Analysis – The Simplest Guide in the Universe: Bite-Size Stats, #6Von EverandMultivariate Analysis – The Simplest Guide in the Universe: Bite-Size Stats, #6Noch keine Bewertungen
- A Smart Pill For InsulinDokument2 SeitenA Smart Pill For InsulinApt RiskaNoch keine Bewertungen
- Tugas OEEDokument10 SeitenTugas OEEApt RiskaNoch keine Bewertungen
- Acute Decompensated Heart Failure: Inpatient ManagementDokument72 SeitenAcute Decompensated Heart Failure: Inpatient ManagementparahNoch keine Bewertungen
- Consensus AcutedecompensatedDokument19 SeitenConsensus AcutedecompensatedYoga RamadhanNoch keine Bewertungen
- Soal UjianDokument5 SeitenSoal UjianApt RiskaNoch keine Bewertungen
- 1 PBDokument7 Seiten1 PBApt RiskaNoch keine Bewertungen
- Skizofrenia CaseDokument338 SeitenSkizofrenia CaseApt RiskaNoch keine Bewertungen
- Pocket Guide To 2015 Beers Criteria PDFDokument7 SeitenPocket Guide To 2015 Beers Criteria PDFYuliEdySeringnyungsepNoch keine Bewertungen
- An Analysis of Seriousness Predictability and PrevDokument6 SeitenAn Analysis of Seriousness Predictability and PrevApt RiskaNoch keine Bewertungen
- STOPPSTART Criteria For Potentially Inappropriate - 1Dokument7 SeitenSTOPPSTART Criteria For Potentially Inappropriate - 1Apt RiskaNoch keine Bewertungen
- An Analysis of Seriousness Predictability and PrevDokument6 SeitenAn Analysis of Seriousness Predictability and PrevApt RiskaNoch keine Bewertungen
- Pocket Guide To 2015 Beers Criteria PDFDokument7 SeitenPocket Guide To 2015 Beers Criteria PDFYuliEdySeringnyungsepNoch keine Bewertungen
- Naranjo Causality ScaleDokument2 SeitenNaranjo Causality ScaleZamharira MuslimNoch keine Bewertungen
- STOPPSTART Criteria For Potentially Inappropriate - 1Dokument7 SeitenSTOPPSTART Criteria For Potentially Inappropriate - 1Apt RiskaNoch keine Bewertungen
- Pocket Guide To 2015 Beers Criteria PDFDokument7 SeitenPocket Guide To 2015 Beers Criteria PDFYuliEdySeringnyungsepNoch keine Bewertungen
- Guideline DM PDFDokument8 SeitenGuideline DM PDFApt RiskaNoch keine Bewertungen
- Ambulatory Blood Pressure JournalDokument7 SeitenAmbulatory Blood Pressure JournalApt RiskaNoch keine Bewertungen
- Essentials of Ambulatory Blood Pressure Monitoring (ABPM) : November 2017Dokument7 SeitenEssentials of Ambulatory Blood Pressure Monitoring (ABPM) : November 2017Apt RiskaNoch keine Bewertungen
- An Analysis of Seriousness Predictability and PrevDokument6 SeitenAn Analysis of Seriousness Predictability and PrevApt RiskaNoch keine Bewertungen
- Pocket Guide To 2015 Beers Criteria PDFDokument7 SeitenPocket Guide To 2015 Beers Criteria PDFYuliEdySeringnyungsepNoch keine Bewertungen
- Therapy Studies What Question Did The Study Ask?Dokument2 SeitenTherapy Studies What Question Did The Study Ask?Apt RiskaNoch keine Bewertungen
- An Analysis of Seriousness Predictability and PrevDokument6 SeitenAn Analysis of Seriousness Predictability and PrevApt RiskaNoch keine Bewertungen
- An Analysis of Seriousness Predictability and PrevDokument6 SeitenAn Analysis of Seriousness Predictability and PrevApt RiskaNoch keine Bewertungen
- Guideline DM PDFDokument8 SeitenGuideline DM PDFApt RiskaNoch keine Bewertungen
- Nstemi Acs EscDokument56 SeitenNstemi Acs EscRiuin23Noch keine Bewertungen
- Pembanding1 Phanthom ReproDokument13 SeitenPembanding1 Phanthom ReproEva SavitriNoch keine Bewertungen
- ConsultsDokument16 SeitenConsultsRaq KhoNoch keine Bewertungen
- Health and Wellness Calendar 2020Dokument1 SeiteHealth and Wellness Calendar 2020CHARMAINE ACEVEDONoch keine Bewertungen
- NCLEX Review Cardiovascular QuizDokument17 SeitenNCLEX Review Cardiovascular Quizdany tesemaNoch keine Bewertungen
- CV For Website 2019Dokument2 SeitenCV For Website 2019api-276874545Noch keine Bewertungen
- Case StudyDokument4 SeitenCase StudyTariq shahNoch keine Bewertungen
- Pathology MnemonicsDokument27 SeitenPathology MnemonicsdyaNoch keine Bewertungen
- 1 - Mattu, Amal ECGsDokument68 Seiten1 - Mattu, Amal ECGsKhan A Reh50% (2)
- Radiation Toxicity: 31.1 Principles of RadioactivityDokument9 SeitenRadiation Toxicity: 31.1 Principles of RadioactivityVarshith GandlaNoch keine Bewertungen
- HTTPSWWW - whc.SgDocumentsWH Allied20Health and Pharmacy PDFDokument5 SeitenHTTPSWWW - whc.SgDocumentsWH Allied20Health and Pharmacy PDFAndrew LimNoch keine Bewertungen
- Caring For The Client During Labor and Delivery2Dokument80 SeitenCaring For The Client During Labor and Delivery2wafflesNoch keine Bewertungen
- Unlock Listening and Speaking 4Dokument225 SeitenUnlock Listening and Speaking 4Amar AlmalkiNoch keine Bewertungen
- Osteovit: Collagen Matrix For Filling Bone DefectsDokument2 SeitenOsteovit: Collagen Matrix For Filling Bone DefectsAngga SaputraNoch keine Bewertungen
- Level 2 (Complete) Ppe Donning-Doffing ChecklistDokument2 SeitenLevel 2 (Complete) Ppe Donning-Doffing ChecklistALIMBOYOGUEN RexorNoch keine Bewertungen
- Engorgement & Mastitis MM RH SJDokument18 SeitenEngorgement & Mastitis MM RH SJbrown_chocolate87643Noch keine Bewertungen
- Chapter #5 - Summary Abnormal Psychology: An Integrative Approach Chapter #5 - Summary Abnormal Psychology: An Integrative ApproachDokument13 SeitenChapter #5 - Summary Abnormal Psychology: An Integrative Approach Chapter #5 - Summary Abnormal Psychology: An Integrative ApproachDjane VillarinNoch keine Bewertungen
- Hallucinations, Delusions and Paranoia: See The DoctorDokument3 SeitenHallucinations, Delusions and Paranoia: See The DoctorNyong FenNoch keine Bewertungen
- Dental Health: The ComponentDokument1 SeiteDental Health: The Componentmaddie g.Noch keine Bewertungen
- Oxygen TherapyDokument31 SeitenOxygen TherapyChayan BhowmikNoch keine Bewertungen
- Comparative Study: Formula Praktis Estimasi Laju: Filtrasi Glomerulus (LFG) Dengan Biomarker Kreatinin SerumDokument8 SeitenComparative Study: Formula Praktis Estimasi Laju: Filtrasi Glomerulus (LFG) Dengan Biomarker Kreatinin SerumAchmad ThoriqNoch keine Bewertungen
- Acutebrainfailure: Pathophysiology, Diagnosis, Management, and Sequelae of DeliriumDokument59 SeitenAcutebrainfailure: Pathophysiology, Diagnosis, Management, and Sequelae of DeliriumdarlingcarvajalduqueNoch keine Bewertungen
- The New Yorker - 14 09 2020Dokument80 SeitenThe New Yorker - 14 09 2020Dragoş Şerban PopNoch keine Bewertungen
- Test Questions CA1Dokument3 SeitenTest Questions CA1Gemery Jade ArtatesNoch keine Bewertungen
- GAD Aos 40 AnosDokument7 SeitenGAD Aos 40 AnosrafaelplNoch keine Bewertungen
- Brief Intervention: Mhgap-Ig Base Course - Field Test Version 1.00 - May 2012 1Dokument16 SeitenBrief Intervention: Mhgap-Ig Base Course - Field Test Version 1.00 - May 2012 1TEOFILO PALSIMON JR.Noch keine Bewertungen
- Chemotherapy Protocols V 101Dokument42 SeitenChemotherapy Protocols V 101Charm TanyaNoch keine Bewertungen
- JaundiceDokument19 SeitenJaundiceketsela12Noch keine Bewertungen
- Daftar PustakaDokument3 SeitenDaftar PustakaChalimatussa DiyahNoch keine Bewertungen
- Teleradiologi: Cross Reporting & Smart AssignDokument17 SeitenTeleradiologi: Cross Reporting & Smart Assignrafael100% (1)
- 0 - Review of Post Graduate Medical Entrance Examination (PGMEE) (AAA) (PDFDrive - Com) Export PDFDokument39 Seiten0 - Review of Post Graduate Medical Entrance Examination (PGMEE) (AAA) (PDFDrive - Com) Export PDFAbu ÂwŞmž100% (2)