Beruflich Dokumente
Kultur Dokumente
Ijwh 218933 Retained Placenta After Vaginal Delivery Risk Factors and M 2
Hochgeladen von
terry mutiaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Ijwh 218933 Retained Placenta After Vaginal Delivery Risk Factors and M 2
Hochgeladen von
terry mutiaCopyright:
Verfügbare Formate
International Journal of Women's Health Dovepress
open access to scientific and medical research
Open Access Full Text Article
REVIEW
Retained placenta after vaginal delivery: risk
factors and management
International Journal of Women's Health downloaded from https://www.dovepress.com/ by 182.1.8.221 on 03-Nov-2019
This article was published in the following Dove Press journal:
International Journal of Women's Health
Nicola C Perlman Abstract: Retained placenta after vaginal delivery is diagnosed when a placenta does not
Daniela A Carusi spontaneously deliver within a designated amount of time, variably defined as a period of
18–60 mins. It may also be diagnosed if a patient experiences significant hemorrhage prior to
Department of Obstetrics and
Gynecology, Brigham and Women’s delivery of the placenta. Normal placenta delivery requires adequate uterine contractions,
Hospital, Harvard Medical School, with shearing of the placenta and decidua from the uterine wall and expulsion of the tissue.
Boston, MA, USA
Thus, retained placenta can occur in the setting of significant uterine atony, abnormally
For personal use only.
adherent placenta, as with placenta accreta spectrum (PAS), or closure of the cervix prior to
placental expulsion. Risk factors for retained placenta parallel those for uterine atony and
PAS and include prolonged oxytocin use, high parity, preterm delivery, history of uterine
surgery, and IVF conceptions. History of a prior retained placenta and congenital uterine
anomalies also appear to be risk factors. Management entails manual removal of the placenta
with adequate analgesia, as medical intervention alone has not been proven effective.
Complications can include major hemorrhage, endometritis, or retained portions of placental
tissue, the latter of which can lead to delayed hemorrhage or infection. Prophylactic
antibiotics can be considered with manual placenta removal, though evidence regarding
effectiveness is inconsistent. If hemorrhage is encountered, deployment of a massive transfu-
sion protocol, uterine evacuation with suction, and use of intrauterine tamponade, as with an
intrauterine balloon, should be initiated immediately. When a separation plane between the
placenta and uterus is particularly difficult to create, PAS should be considered, and
preparations should be made for hemorrhage and hysterectomy. Patients with risk factors
for retained placenta should have a laboratory sample sent for blood type and antibody
screening on admission to labor and delivery, and plans should be made for appropriate
analgesia and preparations for hemorrhage if a retained placenta is encountered.
Keywords: retained placenta, manual removal of the placenta, postpartum hemorrhage,
placenta accreta spectrum
Introduction
Retained placenta after vaginal delivery, which occurs in around 1–3% of deliv-
eries, is a relatively common cause of obstetrical morbidity. This is typically
diagnosed when the placenta fails to spontaneously separate during the third stage
of labor when a patient experiences excessive bleeding in absence of placenta
Correspondence: Daniela A Carusi
Department of Obstetrics and separation or if there is confirmation of placenta tissue remaining after the
Gynecology, Brigham and Women’s majority of the placenta delivers spontaneously.1–3 Placentas that fail to sponta-
Hospital, Harvard Medical School, 75
Francis St, Boston, MA 02115, USA neously separate can be a cause of significant surgical and hemorrhagic
Tel +1 617 732 5452 morbidity.4,5 Untreated, retained placenta is considered the second leading cause
Fax +1 617 232 6346
Email dcarusi@bwh.harvard.edu of postpartum hemorrhage (PPH).5,6
submit your manuscript | www.dovepress.com International Journal of Women's Health 2019:11 527–534 527
DovePress © 2019 Perlman and Carusi. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/
terms.php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing
http://doi.org/10.2147/IJWH.S218933
the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed.
For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms (https://www.dovepress.com/terms.php).
Powered by TCPDF (www.tcpdf.org)
Perlman and Carusi Dovepress
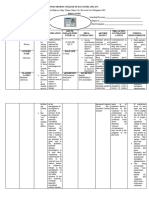
Although retained placenta is an obstetrical complica- Table 1 Risk factors for retained placenta
tion encountered relatively infrequently on the labor and Risk factors related to poor uterine contraction
delivery floor, recognizing patient risk factors and under-
High parity
standing management are important steps in mitigating
Prolonged use of oxytocin
this morbidity.
Risk factors related to abnormal placentation
Pathophysiology
International Journal of Women's Health downloaded from https://www.dovepress.com/ by 182.1.8.221 on 03-Nov-2019
History of uterine surgery
Normal placentation begins with blastocyst implantation into IVF conception
the maternal endometrium. In preparation for this implanta- Other risk factors
tion, the endometrium develops the decidua under the influ-
Preterm delivery
ence of progesterone and estrogen in early pregnancy. As the
Congenital uterine anomaly
blastocyst invades this decidua, the layer of cells forming the Prior history of retained placenta
surface of the blastocyst develops into the chorionic mem-
brane. Cytotrophoblast cells proliferate from the chorionic
membrane and form multinucleated aggregates called syncy- risk factors include prior retained placenta, preterm deliv-
tiotrophoblast cells. These cells form the placental villi, ery, prior uterine surgery, previous pregnancy termination,
allowing fetal–maternal interchange between the villi–decid- miscarriage or curettage, grand multiparity (greater than
ual interaction. With delivery of the infant, both a hormonal five prior deliveries), and congenital uterine anomalies
For personal use only.
cascade and uterine contractions allow for separation of these (often unrecognized prior to delivery).3,5,11
layers and expulsion of the placenta.7 Some studies have suggested that prolonged oxytocin
Retained placenta is generally attributed to one of three use could be a potentially modifiable risk factor for
pathophysiologies. First, an atonic uterus with poor con- retained placenta, with one study reporting that oxytocin
traction may prevent normal separation and contractile use for over 195 mins increased the odds ratio of the
expulsion of the placenta.2,8,9 Second, an abnormally retained placenta by 2.0, and oxytocin use over 415 mins
adherent or invasive placenta, as seen with placenta increased the odds ratio by 6.5.5 It is less clear whether
accreta spectrum (PAS), may be incapable of normal oxytocin is directly involved in placental retention, or if
separation. Finally, a separated placenta may be trapped the association is mediated by uterine atony or infection
or incarcerated due to closure of the cervix prior to deliv- due to prolonged labor.
ery of the placenta.2,8–10 Placental hypoperfusion disor- Placental under perfusion disorders have been impli-
ders, such as with preeclampsia, and infection have also cated as risk factors for retained placenta.11 In a case–
been proposed as mechanisms for retained placenta, control study of all singleton primiparous vaginal deliv-
although little is known about the specific mechanism.9,11 eries in Sweden between 1997 and 2009, the authors found
an increased association between placental under perfusion
Epidemiology disorders (such as preeclampsia, small for gestational age,
Estimates of retained placenta put the incidence at between and stillbirth) and retained placenta; however, they could
0.1% and 3%.5,8 Prospective investigations of retained pla- not designate a common pathophysiology.
centa confirm these estimates, with one study of >45,000 Some research suggests that women may be predis-
patients showing that overall for all gestational ages, retained posed to retained placenta. Retained placenta in a prior
placenta happened in about 3% of deliveries, with gestational delivery appears to be an important risk factor for recur-
ages of <26 weeks and <37 weeks having a significantly rence. In one study of over 280 women in Denmark,
increased risk of retained placenta requiring manual prevalence of retained placenta was found to be consistent
removal.1 Generally, incidence seems to be higher in devel- with previously reported numbers (approximately 3%)
oped countries where practices tend toward earlier manual using strict diagnostic criteria. The authors found that in
removal of the placenta in the third stage of labor.8,12 subsequent vaginal deliveries, the risk of recurrence was
substantially increased to about 25%.3 There has even
Risk factors been some suggestion that tendency toward retained pla-
Many studies have attempted to define risk factors for centa may even be inherited. In one study, authors used the
retained placenta, which are listed in Table 1. Established Swedish Medical Birth Register to identify women with
submit your manuscript | www.dovepress.com International Journal of Women's Health 2019:11
528
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Perlman and Carusi
retained placenta after 1992 whose mothers’ own birth If the placenta or pieces of the placenta remain in situ
records were also in the Register (after 1973). The authors following attempt at manual removal, a patient may
found that the risk of retained placenta increased if require surgical management. In a study of >20,000
retained placenta had occurred at the mother’s own birth patients in Norway, 3% of women requiring manual
(aOR 1.66 95% CI 1/52–1/82), at the birth of one of her removal of retained placenta needed additional surgical
siblings (aOR 1.58, 95% CI 1.43–1.76), or both (aOR management with dilation and curettage.17 Another case–
International Journal of Women's Health downloaded from https://www.dovepress.com/ by 182.1.8.221 on 03-Nov-2019
2.75, 95% CI 2.18–3.46).13 control study of 114 women found that cases required
Because of its relationship to PAS, assisted reproduc- more dilation and curettage than controls, although with
tive technologies (IVF or ICSI) have been proposed and their study number they could not confirm significance.18
studied as an additional risk factor for retained placenta.14 Occasionally portions of the placenta or membranes may
Elenis et al, in a 2015 study from Sweden, looked speci- remain in the uterus after manual extraction, leading to
fically at oocyte donation IVF and the risk of poor obste- delayed complications from retained products of concep-
trical outcomes in otherwise healthy women.15 The tion. These can include delayed postpartum hemorrhage or
authors found a positive association between retained pla- endomyometritis.
centa and oocyte donation, as well as between PPH and Evidence of infection risk, particularly endometritis,
oocyte donation.15 In another 2016 study by Aziz et al, following manual or surgical removal of retained placenta
seeking to determine whether or not length of third stage has been inconsistently demonstrated.20 A large 1995 ret-
was related to IVF, the authors concluded that cryopre- rospective cohort study at University of Iowa compared
For personal use only.
served embryo transfer (donated or autologous) without over 1000 patients requiring manual extraction after vagi-
controlled ovarian hyperstimulation was not related to nal delivery with those who did not.20 After controlling for
longer third stage, but did significantly increase the risk confounders, the authors found that manual removal of
for manual removal of the placenta.16 retained placenta was significantly associated with post-
partum endometritis.20 Alternatively, in the large cohort
study of >20,000 patients from Norway mentioned above,
Morbidity patients requiring intervention for retained placenta did not
Retained placenta requiring invasive procedures is associated show a significantly increased risk of infection, despite
with obstetrical morbidities. Of arguably greatest signifi- varying practices regarding antibiotic administration and
cance is the risk of postpartum hemorrhage, with retained timing.17 Other studies have similarly found a relationship
placenta the second leading cause of significant and even but could not prove a significant association between
fatal hemorrhage in the obstetric population.5,17 One group manual removal or surgical placental removal and
found that the odds ratio related to estimated blood loss endometritis.18,21 The discrepancies may in part be due
exceeding 500 mL, 1000 mL, and 2000 mL with retained to the lack of rigorous distinction between postpartum
placenta, respectively, is as high as 33.07 (95% CI 20.57– fever and true uterine infection.
53.16), 43.44 (95% CI 26.57–71.02), and 111.24 (95% CI
27.26–454.00).5 In another case–control study of 114 women Diagnosis
with manual removal for retained placenta, the authors found Retained placenta is clinically diagnosed when the pla-
that the case group required significantly more blood transfu- centa fails to spontaneously separate during the third
sions (13% in the case group versus 0% in the controls).18 stage of labor, with or without active management, or in
Large cohort studies have confirmed this elevated risk.17 the setting of severe bleeding in the absence of placental
Further research additionally suggests that the longer delivery.18,22 The first diagnostic criterion requires a time
the third stage of labor, the greater the risk of postpartum cutoff, though there is no uniform consensus as to timing
hemorrhage.19 A study by Dombrowski et al in 1995 tried for diagnosis of retained placenta in the third stage in the
to determine gestational age–specific data for the length of absence of postpartum hemorrhage. Selection of a clinical
the third stage, retained placenta, hemorrhage, and manual time definition can be based either on a population curve
removal. The authors found that both manual removal of of observed spontaneous placental delivery times or on a
the placenta and PPH decreased with increasing gesta- time at which morbidity significantly increases. Thirty
tional age, and that the two were related. However, causal minutes have been used as a loose guideline, which
association could not be determined.1 comes from a 1991 study by Combs et al.2 The researchers
submit your manuscript | www.dovepress.com
International Journal of Women's Health 2019:11 529
DovePress
Powered by TCPDF (www.tcpdf.org)
Perlman and Carusi Dovepress
found that the third stage had a log-normal distribution, At times the bulk of the placenta will deliver sponta-
with a mean length of 6.8 minutes, with only 3.3% of neously or manually, but small portions or an accessory
deliveries having greater a greater than 30 minutes third lobe may be retained. This may be suspected when the
stage. This timing has been supported by other studies as placenta appears fragmented after delivery or when there
well.8 Interestingly, the authors calculated that the inci- is ongoing heavy uterine bleeding. In this situation, the
dence of PPH, transfusion, and dilation and curettage uterine cavity may be evaluated with manual exploration
International Journal of Women's Health downloaded from https://www.dovepress.com/ by 182.1.8.221 on 03-Nov-2019
remained constant during this period, increasing only or with ultrasound. The utility of ultrasound in this situa-
after 30 minutes and plateauing at 75 minutes for both tion has yet to be established, with a focal endometrial
manually and spontaneously delivered placentas. Because mass, particularly with Doppler flow, being the findings of
PPH incidence did not increase until after 30 minutes, interest. In one study of routine ultrasound immediately
Combs et al recommended this timing for initiation of after vaginal delivery, the sensitivity for diagnosing
manual removal of the placenta. retained placental fragments was only 44% with a positive
However, this guidance is not uniformly supported. In a predictive value (PPV) of 58%.27 An alternate study
subsequent study by Deneux-Tharaux, surveys from 14 showed a 75–80% sensitivity of postpartum ultrasound,
European countries exhibited wide variations in wait time though the mean time for evaluation was 21 days post-
prior to manual placental removal, largely by country but partum, when less blood and decidua are expected to be
also by the hospital.23 In countries such as Finland and seen.28 While immediate ultrasound’s PPV will be higher
when there is clinical suspicion of retained POCs, a nega-
Denmark, obstetricians tended to wait 60 minutes or more
For personal use only.
tive ultrasound should not deter manual or suction curet-
prior to manual removal of the placenta, versus in countries
tage when there is a strong clinical suspicion, especially in
such as Spain and France, where providers removed the
the setting of hemorrhage.
placenta after 30 minutes. Practices also varied considerably
depending on whether or not the patient in question had prior
epidural anesthesia.23 National and worldwide guidelines
Management
After delivery of the infant and prior to diagnosis of
similarly have no consensus on when to intervene on an
retained placenta, active management is recommended to
undelivered placenta. For instance, the National Institute
facilitate spontaneous placental separation, including oxy-
for Health and Clinical Excellence suggests a wait time of
tocin, controlled cord traction, and uterine massage.4
30 minutes in the United Kingdom prior to manual removal
These maneuvers have been shown to decrease the risk
of the placenta,24 while the World Health Organization
of postpartum hemorrhage, though it has not been shown
guidelines propose a wait time of 60 minutes.12,25
that active management will prevent retained placenta.22
The most significant risk of waiting a prolonged
Once diagnosed, the placenta is usually manually
amount of time before removing the placenta is postpar-
extracted from the uterus.22,29 Table 2 lists items that
tum hemorrhage. In 2005, Magann and colleagues under-
should be readily available if needed during the extraction
took a prospective observational study in which all process. Because this procedure is painful, adequate
women delivering vaginally were assessed for analgesia should be achieved via epidural, conscious seda-
PPH.15 Using receiver operating characteristic curves, tion, or general anesthesia prior to an attempt at extraction.
the authors showed that 95% of normal placental delivery Once the patient is comfortable, she should be appropri-
occurs within 18 minutes, and that a third stage of labor ately positioned in lithotomy. A conical drape, preferably
longer than 18 minutes was associated with a significant one that is graduated and marked to allow for quantitative
risk of PPH.19 The authors followed up this paper in blood loss, should be placed under the patient’s buttocks.
2012 with a randomized controlled trial assigning vaginal The operator should make every attempt to wear gown and
deliveries to manual removal at either 10 or 15 minutes gloves and maintain sterility, both for personal and for
(as opposed to the traditional 30) if the placenta had not patient protection. The patient’s bladder should be drained.
yet spontaneously delivered.26 The findings supported the The provider should then use one hand to follow the
authors’ initial study, showing that removal at 15 minutes umbilical cord through the vagina and cervix until the
had a significantly greater likelihood of hemorrhage com- placenta is palpated. If the placenta is separated but not
pared to 10 minutes, opening up the discussion on earlier expelled, such as in the case of uterine atony, the tissue can
intervention.26 be firmly grasped and brought through the cervix.
submit your manuscript | www.dovepress.com International Journal of Women's Health 2019:11
530
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Perlman and Carusi
Table 2 Items that should be available for manual placental If placental removal is refractory or only partially
extraction successful (ie the placenta or parts of the placenta remain
Medications in the uterus), or if bleeding persists despite placental
delivery, often the next step is surgical management with
Analgesics or sedatives with appropriate monitoring equipment
Uterotonic agents curettage. This may be best achieved in an operating room,
Nitroglycerin with optimal access to surgical equipment, analgesia, and
International Journal of Women's Health downloaded from https://www.dovepress.com/ by 182.1.8.221 on 03-Nov-2019
patient resuscitation aids, if needed. Suction curettage is
Patient preparation
generally used, though a sharp curette may be needed to
Conical under-buttocks drape for blood collection facilitate a separation plane. Access to uterine tamponade
Bladder catheter
supplies with either a large intrauterine balloon or surgical
Surgical instruments packs should be immediately accessed in the event of
Sponge forceps for grasping tissue hemorrhage. Crossmatched blood products should be
Long curette made imminently available if placental separation is diffi-
cult or blood loss exceeds 1 L, and the care team should
Hemorrhage management
attend to uterotonic administration and attention to coagu-
Intrauterine balloon or uterine packing material lopathy as the extraction is performed.4
Availability of crossmatched blood
Due to the risk of endometritis, routine antibiotics are
Massive transfusion protocol
Equipment for quantitative blood loss measurement (volumetric or
generally administered just before or shortly after manual
For personal use only.
gravimetric) removal of the placenta.20 Prophylaxis can parallel cesar-
Available operating room with anesthesia equipment ean prophylaxis with a first-generation cephalosporin.
Suction curettage equipment Patients who are febrile at the time of extraction should
Laparotomy equipment be fully treated for chorioamnionitis with broad-spectrum
antibiotics.32 Despite these guidelines, few studies have
been undertaken examining the effectiveness of antibiotics
Uterotonic medications, such as oxytocin, methylergono-
in reducing infectious morbidity. A 2015 systematic
vine, carboprost, or other prostaglandins, should be given
review by Chibueze and colleagues attempted to summar-
to facilitate contraction once the placenta is removed.4
ize the literature on the efficacy of antibiotics for prevent-
Nitroglycerine (NTG) has been used to facilitate manual
ing adverse maternal outcomes related to manual placenta
extraction by relaxing uterine smooth muscle.30 This may be
removal following vaginal birth.21 The authors reported on
particularly helpful when the placenta is trapped behind a
three retrospective cohort studies examining endometritis
partially closed cervix, though the use of NTG alone does
and puerperal fever after manual extraction for retained
not appear to facilitate spontaneous placental expulsion.31 It
placenta. None of the three studies found evidence to
can be given as a 1 mg sublingual dose, or as sequential 50
suggest beneficial effects for routine antibiotic use in
mcg intravenous boluses, up to a total dose of 200 mcg. The women undergoing intervention for retained placenta.
medication can produce hypotension and tachycardia, which The authors concluded that further research is required to
can confound assessments of maternal stability. Once the adequately answer this question.21 Due to mixed data
placenta is delivered, uterotonics should be promptly given regarding prophylaxis, as well as the increasing risk of
to restore uterine tone and avoid significant atony. postpartum hemorrhage with prolonged third stage of
If the placenta remains attached to the uterine decidua, an labor, administration of antibiotics should not delay man-
attempt should be made to separate it manually. Using one ual removal of retained placenta.
hand to provide counter pressure on the fundus through the Occasionally, a portion of placental tissue may remain
maternal abdomen, the provider should then use the internal in the uterus, either knowingly or unbeknownst to the
hand to manually create a cleavage plane between the pla- providers. This can present as abnormal bleeding days to
centa with the attached decidua and the myometrium. Once weeks after delivery and should be suspected in the setting
separated, the placenta can be removed as described above. If of a delayed postpartum hemorrhage. Recently, studies
a separation plane cannot be created behind all or part of the have examined the usefulness of hysteroscopic morcella-
placenta, the provider should suspect a morbidly adherent tion devices in aiding with retained placenta left in situ
placenta (MAP) and prepare for potential hemorrhage. postpartum (Figure 1A [before] and B [after]). In a series
submit your manuscript | www.dovepress.com
International Journal of Women's Health 2019:11 531
DovePress
Powered by TCPDF (www.tcpdf.org)
Perlman and Carusi Dovepress
International Journal of Women's Health downloaded from https://www.dovepress.com/ by 182.1.8.221 on 03-Nov-2019
Figure 1 The photo on the left (A) shows a retained portion of placenta approximately 8 weeks after delivery. The photo on the right (B) shows the same uterus following
hysteroscopic morcellation of the retained placenta.
of case reports, Lee and colleagues reported a higher risk oxytocin either alone or in conjunction with intravenous
of complications with blind curettage compared to hys- oxytocin to reduce the need for manual removal of
teroscopic morcellation.33 They additionally reported com- retained placenta.36 While inexpensive and easy to do,
plete resection in 90% of hysteroscopic cases and the authors found that all well-designed randomized con-
reduction of both perforation and intrauterine adhesion trol trials showed no significant effect of umbilical vein
risk.33 In another randomized control trial by oxytocin on retained placenta.36
For personal use only.
Hamerlynck et al, the authors randomized patients to
undergo hysteroscopic resection of retained placenta with
either hysteroscopic morcellation versus loop resection
Morbidly adherent placenta
In the unusual event that manual extraction does not result
with rigid bipolar resectoscopes.34 These authors in com-
in delivery of the entire or partial placenta, MAP must be
parison found that when comparing the two modalities,
considered as an etiology. The PAS, which includes
complete resection was comparatively high in both groups,
accreta, increta, or percreta, can be causes of significant
and intrauterine adhesions were comparatively low.34 The
one significant difference between the two groups was that surgical and hemorrhagic morbidity on the labor and deliv-
the hysteroscopic group had significantly faster operative ery floor4,37 (Figure 2). While PAS is relatively rare,
times.34 The ability to perform hysteroscopic removal particularly in the absence of a placenta previa, it can
depends on the amount of active bleeding, with suction occur at vaginal delivery when there is no previa. Given
curettage often needed when bleeding is heavy.
Other studies have examined alternative, nonsurgical,
management for retained placenta, none of which have
been successful. In 2012, 99 women in a large teaching
hospital in the Netherlands with retained placenta (>60 mins
after delivery) were given either 800 mcg misoprostol or
placebo orally.35 The author’s primary outcomes were num-
ber of manual removals of retained placenta and blood loss.
The authors found that oral misoprostol reduced neither the
need for manual removal nor the overall amount of blood
loss. Both groups were observed for additional 45 mins
after administration of misoprostol or placebo. While the
authors found that 50% of remaining placentas at 60 mins
delivered in the intervening 45 mins, it came at the expense
of additional significant blood loss.35
For a time, umbilical vein oxytocin was thought to be a
promising alternative or adjunct to manual extraction of Figure 2 Magnetic resonance image showing a portion of retained placenta 6
weeks postpartum. The arrow indicates an area where the light-gray placenta is
the placenta. A 2011 Cochrane Review summarized avail-
deeply invasive into the darker-gray myometrium. Placenta accreta spectrum was
able data on the subject to assess the use of umbilical vein confirmed pathologically following hysterectomy.
submit your manuscript | www.dovepress.com International Journal of Women's Health 2019:11
532
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Perlman and Carusi
the excess morbidity, providers should consider this etiology. Regardless, prompt diagnosis and management
pathology when a placenta is retained in the setting of with appropriate personnel, access to blood for massive
significant PAS risk factors. These include prior uterine transfusion protocol, and surgical equipment such as uter-
surgeries, including hysteroscopic resections, IVF concep- ine suction and tamponade can be required to treat retained
tion, a history of intrauterine adhesions, or a prior history placenta and lessen its morbidity.
of MAP or pathologic findings of accreta.38,39
International Journal of Women's Health downloaded from https://www.dovepress.com/ by 182.1.8.221 on 03-Nov-2019
When a separation plane cannot be created or extraction Disclosure
attempts begin to invert the uterus, MAP should be sus- The authors report no conflicts of interest in this work.
pected. In this case, further attempts to extract the placenta
should cease, as forcible removal of a MAP can lead to
References
massive hemorrhage.40 At this point, consideration should
1. Dombrowski MP, Bottoms SF, Saleh AA, Hurd WW, Romero R.
be made for hysterectomy, which will be necessary if the Third stage of labor: analysis of duration and clinical practice. Am
patient has an undeliverable placenta with significant J Obstet Gynecol. 1995;172(4 Pt 1):1279–1284. doi:10.1016/0002-
hemorrhage. Alternative treatment has been described 9378(95)91493-5
2. Combs CA, Murphy EL, Laros RK. Factors associated with postpartum
including expectant management or uterine conservation.41 hemorrhage with vaginal birth. Obstet Gynecol. 1991;77(1):69–76.
Expectant management has been described in small studies 3. Nikolajsen S, Løkkegaard ECL, Bergholt T. Reoccurrence of retained
placenta at vaginal delivery: an observational study. Acta Obstet Gynecol
and refers to the placenta left in situ after diagnosis of Scand. 2013;92(4):421–425. doi:10.1111/j.1600-0412.2012.01520.x
PAS.38,41,42 Such management requires careful patient 4. American College of Obstetricians and Gynecologists. ACOG practice
For personal use only.
selection and counseling, as this risks delayed hemorrhage bulletin: clinical management guidelines for obstetrician-gynecologists
number 76, October 2006: postpartum hemorrhage. Obstet Gynecol.
or infection. Nevertheless, successful conservative manage- 2006;108(4):1039–1047. doi:10.1097/01.AOG.0000214671.19023.68
ment has been described, with placental expulsion, resorp- 5. Endler M, Grünewald C, Saltvedt S. Epidemiology of retained pla-
centa: oxytocin as an independent risk factor. Obstet Gynecol.
tion, or removal at a median of 3 months and up to 1 year 2012;119(4):801–809. doi:10.1097/AOG.0b013e31824acb3b
postpartum.43 6. Bateman BT, Berman MF, Riley LE, Leffert LR. The epidemiology
Uterine conservation with placental removal is an alter- of postpartum hemorrhage in a large, nationwide sample of deliv-
eries. Anesth Analg. 2010;110(5):1368–1373.
native technique that likewise has been described in only 7. Kraus FT, Redline RW, Gersell DJ, Nelson DM, Dicke JM. Placental
small studies. This refers to resection of the placental bed Pathology. American Registry of Pathology in collaboration with the
Armed Forces Institute of Pathology. Atlas Nontumor Pathol.
at the area of suspected PAS and requires conversion to 2004;1:10–16.
laparotomy after vaginal delivery.41 The resultant defect in 8. Urner F, Zimmermann R, Krafft A. Manual removal of the placenta
theory can be repaired via over-sewing and/or uterine after vaginal delivery: an unsolved problem in obstetrics. J
Pregnancy. 2014;2014:274651. doi:10.1155/2014/239406
repair or alternatively attempting tamponade with a Bakri 9. Greenbaum S, Wainstock T, Dukler D, Leron E, Erez O. Underlying
balloon. Only one small study has evaluated the latter in a mechanisms of retained placenta: evidence from a population based
cohort study. Eur J Obstet Gynecol Reprod Biol. 2017;216:12–17.
randomized control trial, and only with the lesser invasive doi:10.1016/j.ejogrb.2017.06.035
types of PAS.41,44 10. Kramer MS, Berg C, Abenhaim H, et al. Incidence, risk factors, and
temporal trends in severe postpartum hemorrhage. Am J Obstet
Gynecol. 2013;209(5):449.e1–7. doi:10.1016/j.ajog.2013.07.007
Conclusion 11. Endler M, Saltvedt S, Cnattingius S, Stephansson O, Wikström A-K.
Retained placenta after vaginal delivery can be a source of Retained placenta is associated with pre-eclampsia, stillbirth, giving
birth to a small-for-gestational-age infant, and spontaneous preterm
significant hemorrhagic and surgical morbidity to the birth: a national register-based study. BJOG Int J Obstet Gynaecol.
mother. In considering ways to lesson morbidity, the clin- 2014;121(12):1462–1470. doi:10.1111/1471-0528.12752
12. Joseph KS, Rouleau J, Kramer MS, et al. Investigation of an increase
ician should have a knowledge of risk factors for both
in postpartum haemorrhage in Canada. BJOG Int J Obstet Gynaecol.
retained placenta and MAP, allowing them to triage those 2007;114(6):751–759. doi:10.1111/j.1471-0528.2007.01316.x
patients most at risk of hemorrhage and prepare by ensur- 13. Endler M, Cnattingius S, Granfors M, Wikström A-K. The inherited risk
of retained placenta: a population based cohort study. BJOG Int J Obstet
ing blood products are easily available. When managing Gynaecol. 2018;125(6):737–744. doi:10.1111/1471-0528.14828
the patient with retained placenta, 30 minutes of elapsed 14. Esh-Broder E, Ariel I, Abas-Bashir N, Bdolah Y, Celnikier DH.
Placenta accreta is associated with IVF pregnancies: a retrospective
third stage have been traditionally used as a guideline for
chart review. BJOG Int J Obstet Gynaecol. 2011;118(9):1084–1089.
timing manual removal; however, recent research has sug- doi:10.1111/j.1471-0528.2011.02976.x
gested that shorter duration of third stage may in fact be 15. Elenis E, Svanberg AS, Lampic C, Skalkidou A, Åkerud H, Sydsjö G.
Adverse obstetric outcomes in pregnancies resulting from oocyte dona-
less morbid. Further research should be pursued to deter- tion: a retrospective cohort case study in Sweden. BMC Pregnancy
mine the best timing and infection prophylaxis for this Childbirth. 2015;8(15):247. doi:10.1186/s12884-015-0687-9
submit your manuscript | www.dovepress.com
International Journal of Women's Health 2019:11 533
DovePress
Powered by TCPDF (www.tcpdf.org)
Perlman and Carusi Dovepress
16. Aziz MM, Guirguis G, Maratto S, Benito C, Forman EJ. Is there an 29. Rogers MS, Yuen PM, Wong S. Avoiding manual removal of pla-
association between assisted reproductive technologies and time and centa: evaluation of intra-umbilical injection of uterotonics using the
complications of the third stage of labor? Arch Gynecol Obstet. Pipingas technique for management of adherent placenta. Acta Obstet
2016;293(6):1193–1196. doi:10.1007/s00404-015-3943-3 Gynecol Scand. 2007;86(1):48–54. doi:10.1080/00016340601088570
17. Tandberg A, Albrechtsen S, Iversen OE. Manual removal of the 30. Chedraui PA, Insuasti DF. Intravenous nitroglycerin in the manage-
placenta. Incidence and clinical significance. Acta Obstet Gynecol ment of retained placenta. Gynecol Obstet Invest. 2003;56(2):61–64.
Scand. 1999;78(1):33–36. doi:10.1080/j.1600-0412.1999.780108.x doi:10.1159/000072734
18. Titiz H, Wallace A, Voaklander DC. Manual removal of the placenta– 31. Abdel-Aleem H, Abdel-Aleem MA, Shaaban OM. Nitroglycerin for
a case control study. Aust N Z J Obstet Gynaecol. 2001;41(1):41–44. management of retained placenta. Cochrane Database Syst Rev.
International Journal of Women's Health downloaded from https://www.dovepress.com/ by 182.1.8.221 on 03-Nov-2019
doi:10.1111/ajo.2001.41.issue-1 2015;12(11):CD007708.
19. Magann EF, Evans S, Chauhan SP, Lanneau G, Fisk AD, Morrison 32. Committee on Obstetric Practice. Committee opinion no. 712: intra-
JC. The length of the third stage of labor and the risk of postpartum partum management of intraamniotic infection. Obstet Gynecol.
hemorrhage. Obstet Gynecol. 2005;105(2):290–293. doi:10.1097/01. 2017;130(2):e95–101. doi:10.1097/AOG.0000000000002236
AOG.0000159040.51773.bf 33. Lee MHM. Surgical management of retained placental tissue with the
20. Ely JW, Rijhsinghani A, Bowdler NC, Dawson JD. The association hysteroscopic morcellation device. Gynecol Minim Invasive Ther.
between manual removal of the placenta and postpartum endometritis 2019;8(1):33–35. doi:10.4103/GMIT.GMIT_66_18
following vaginal delivery. Obstet Gynecol. 1995;86(6):1002–1006. 34. Hamerlynck TWO, van Vliet HAAM, Beerens A-S, Weyers S, Schoot
doi:10.1016/0029-7844(95)00327-N BC. Hysteroscopic morcellation versus loop resection for removal of
21. Chibueze EC, Parsons AJQ, Ota E, Swa T, Oladapo OT, Mori R. placental remnants: a randomized trial. J Minim Invasive Gynecol.
Prophylactic antibiotics for manual removal of retained placenta 2016;23(7):1172–1180. doi:10.1016/j.jmig.2016.08.828
during vaginal birth: a systematic review of observational studies 35. van Stralen G, Veenhof M, Holleboom C, van Roosmalen J. No
reduction of manual removal after misoprostol for retained placenta:
and meta-analysis. BMC Pregnancy Childbirth. 2015;26(15):313.
a double-blind, randomized trial. Acta Obstet Gynecol Scand.
doi:10.1186/s12884-015-0752-4
2013;92(4):398–403. doi:10.1111/aogs.12065
22. Rogers J, Wood J, McCandlish R, Ayers S, Truesdale A, Elbourne D.
36. Nardin JM, Weeks A, Carroli G. Umbilical vein injection for management
For personal use only.
Active versus expectant management of third stage of labour: the
of retained placenta. Cochrane Database Syst Rev. 2011;11(5):CD001337.
Hinchingbrooke randomised controlled trial. Lancet Lond Engl.
37. Bjurström J, Collins S, Langhoff-Roos J, et al. Failed manual
1998;351(9104):693–699. doi:10.1016/S0140-6736(97)09409-9
removal of the placenta after vaginal delivery. Arch Gynecol Obstet.
23. Deneux-Tharaux C, Macfarlane A, Winter C, et al. Policies for
2018;297(2):323–332. doi:10.1007/s00404-017-4579-2
manual removal of placenta at vaginal delivery: variations in timing
38. Carusi DA. The placenta accreta spectrum: epidemiology and risk
within Europe. BJOG Int J Obstet Gynaecol. 2009;116(1):119–124.
factors. Clin Obstet Gynecol. 2018;61(4):733–742.
doi:10.1111/j.1471-0528.2008.01996.x
39. Roeca C, Little SE, Carusi DA. Pathologically diagnosed placenta accreta
24. National Collaborating Centre for Women’s and Children’s Health and hemorrhagic morbidity in a subsequent pregnancy. Obstet Gynecol.
(UK). Intrapartum Care: Care of Healthy Women and Their Babies
2017;129(2):321–326. doi:10.1097/AOG.0000000000001843
during Childbirth [internet]. London: RCOG Press; 2007 [cited Jun 40. Kayem G, Davy C, Goffinet F, Thomas C, Clément D, Cabrol D.
2, 2019] (National Institute for Health and Clinical Excellence: Conservative versus extirpative management in cases of placenta
Guidance). Available from: http://www.ncbi.nlm.nih.gov/books/ accreta. Obstet Gynecol. 2004;104(3):531–536. doi:10.1097/01.
NBK49388/. Accessed September 3, 2019. AOG.0000136086.78099.0f
25. Ronsmans C, Graham WJ; Lancet Maternal Survival Series steering 41. Placenta accreta spectrum. Obstetric care consensus no. 7. American
group. Maternal mortality: who, when, where, and why. Lancet Lond College of Obstetricians and Gynecologists. Obstet Gynecol.
Engl. 2006;368(9542):1189–1200. doi:10.1016/S0140-6736(06)69380-X 2018;132:e259–e275. doi:10.1097/AOG.0000000000002983
26. Magann EF, Niederhauser A, Doherty DA, Chauhan SP, Sandlin AT, 42. Fox KA, Shamshirsaz AA, Carusi D, et al. Conservative management
Morrison JC. Reducing hemodynamic compromise with placental of morbidly adherent placenta: expert review. Am J Obstet Gynecol.
removal at 10 versus 15 mins: a randomized clinical trial. Am J 2015;213(6):755–760. doi:10.1016/j.ajog.2015.04.034
Perinatol. 2012;29(8):609–614. doi:10.1055/s-0032-1311985 43. Sentilhes L, Ambroselli C, Kayem G, et al. Maternal outcome after
27. Carlan SJ, Scott WT, Pollack R, Harris K. Appearance of the uterus conservative treatment of placenta accreta. Obstet Gynecol. 2010;115
by ultrasound immediately after placental delivery with pathologic (3):526–534. doi:10.1097/AOG.0b013e3181d066d4
correlation. J Clin Ultrasound. 1997;25(6):301–308. doi:10.1002/ 44. Pala Ş, Atilgan R, Başpınar M, et al. Comparison of results of
(SICI)1097-0096(199707)25:6<301::AID-JCU3>3.0.CO;2-G Bakri balloon tamponade and caesarean hysterectomy in manage-
28. Durfee SM, Frates MC, Luong A, Benson CB. The sonographic and color ment of placenta accreta and increta: a retrospective study. J
Doppler features of retained products of conception. J Ultrasound Med Obstet Gynaecol J Inst Obstet Gynaecol. 2018;38(2):194–199.
Off J Am Inst Ultrasound Med. 2005;24(9):1181–6; quiz 1188–9. doi:10.1080/01443615.2017.1340440
International Journal of Women's Health Dovepress
Publish your work in this journal
The International Journal of Women’s Health is an international, peer- manuscript management system is completely online and includes a
reviewed open-access journal publishing original research, reports, very quick and fair peer-review system, which is all easy to use.
editorials, reviews and commentaries on all aspects of women’s Visit http://www.dovepress.com/testimonials.php to read real quotes
healthcare including gynecology, obstetrics, and breast cancer. The from published authors.
Submit your manuscript here: https://www.dovepress.com/international-journal-of-womens-health-journal
submit your manuscript | www.dovepress.com International Journal of Women's Health 2019:11
534
DovePress
Powered by TCPDF (www.tcpdf.org)
Das könnte Ihnen auch gefallen
- On Autumn's Wing, A Story of Birth Trauma, Brain Injury and Miracles.Von EverandOn Autumn's Wing, A Story of Birth Trauma, Brain Injury and Miracles.Noch keine Bewertungen
- Perlman 2019Dokument8 SeitenPerlman 2019Huy Nguyễn QuốcNoch keine Bewertungen
- Damage-Control Surgery For Maternal Near-Miss Cases of Placenta Previa and Placenta Accreta SpectrumDokument6 SeitenDamage-Control Surgery For Maternal Near-Miss Cases of Placenta Previa and Placenta Accreta SpectrumMuh AqwilNoch keine Bewertungen
- Placenta Previa, Accreta, & Vasa Previa 2006Dokument15 SeitenPlacenta Previa, Accreta, & Vasa Previa 2006Ika Agustin0% (1)
- Diagnosis and Management of Fetal DIstress - A Review Based On Modern Concept and Ancient Ayurvedic GranthasDokument3 SeitenDiagnosis and Management of Fetal DIstress - A Review Based On Modern Concept and Ancient Ayurvedic GranthasaginaNoch keine Bewertungen
- Jurnal PlacentaDokument13 SeitenJurnal Placentaoke boskuNoch keine Bewertungen
- Type and Location of Placenta Previa Afect Preterm Delivery Risk Related To Antepartum HemorrhageDokument7 SeitenType and Location of Placenta Previa Afect Preterm Delivery Risk Related To Antepartum HemorrhageRiskaSusila WijayantiNoch keine Bewertungen
- Common Side Effects of Oxytocin Include:: CNS: Maternal: COMADokument3 SeitenCommon Side Effects of Oxytocin Include:: CNS: Maternal: COMAann camposNoch keine Bewertungen
- Article Ejbps Volume 3 December Issue 12 1480826682Dokument4 SeitenArticle Ejbps Volume 3 December Issue 12 1480826682yenni anggrainiNoch keine Bewertungen
- Treatment of Vasa PreviaDokument5 SeitenTreatment of Vasa PreviaDewina Dyani Rosari IINoch keine Bewertungen
- Placenta Accreta Spectrum Disorders: Challenges, Risks, and Management StrategiesDokument13 SeitenPlacenta Accreta Spectrum Disorders: Challenges, Risks, and Management StrategiesRahmayantiYuliaNoch keine Bewertungen
- DR Ward ClassDokument36 SeitenDR Ward ClassChristy Mutia AlumbroNoch keine Bewertungen
- Article Ejbps Volume 3 December Issue 12 1480826682Dokument4 SeitenArticle Ejbps Volume 3 December Issue 12 1480826682kelompok5Noch keine Bewertungen
- Nejm 199604183341601Dokument6 SeitenNejm 199604183341601Simon ReichNoch keine Bewertungen
- Maternal and FDokument3 SeitenMaternal and FNununkNoch keine Bewertungen
- Type and Location of Placenta Previa Affect Preterm Delivery Risk Related To Antepartum HemorrhageDokument7 SeitenType and Location of Placenta Previa Affect Preterm Delivery Risk Related To Antepartum HemorrhageBuya TaftaNoch keine Bewertungen
- Recurrent Ectopic Pregnancy: Current Perspectives: BackgroundDokument4 SeitenRecurrent Ectopic Pregnancy: Current Perspectives: BackgroundRizkaNoch keine Bewertungen
- Vasa Previa ArticuloDokument7 SeitenVasa Previa ArticuloLupita torresNoch keine Bewertungen
- The Placenta Accreta Spectrum: Pathophysiology and Evidence-Based Anatomy For Prenatal Ultrasound ImagingDokument14 SeitenThe Placenta Accreta Spectrum: Pathophysiology and Evidence-Based Anatomy For Prenatal Ultrasound ImagingIriamana Liasyarah MarudinNoch keine Bewertungen
- Nursing-Care-Plans 211112 153011Dokument57 SeitenNursing-Care-Plans 211112 153011Zahraa AlTahanNoch keine Bewertungen
- Ncma219 Week 4Dokument9 SeitenNcma219 Week 4Aruxi YoshiNoch keine Bewertungen
- Effect of Placenta Previa On Fetal Growth: ObstetricsDokument5 SeitenEffect of Placenta Previa On Fetal Growth: ObstetricsAnonymous 4OpLzzt6Noch keine Bewertungen
- Failed Induction of Labor - 2022 - YmobDokument6 SeitenFailed Induction of Labor - 2022 - YmobMor OB-GYNNoch keine Bewertungen
- Retained Placenta and Associated Risk FactorsDokument3 SeitenRetained Placenta and Associated Risk Factorskenny stefanusNoch keine Bewertungen
- VASA Previa CaseDokument3 SeitenVASA Previa CasewijeNoch keine Bewertungen
- Cervical Evaluation ACOGDokument13 SeitenCervical Evaluation ACOGrgutierrez1722Noch keine Bewertungen
- (Australian and New Zealand Journal of ObstetricsDokument2 Seiten(Australian and New Zealand Journal of ObstetricsvvragkonNoch keine Bewertungen
- Cord ProlapseDokument7 SeitenCord ProlapseIwi DancelNoch keine Bewertungen
- Page 277-292 PlacentaDokument16 SeitenPage 277-292 PlacentaRaul DoctoNoch keine Bewertungen
- Protocol For A Systematic Review of "Lotus Birthing Method: Friend or Foe"Dokument4 SeitenProtocol For A Systematic Review of "Lotus Birthing Method: Friend or Foe"International Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- 157 FullDokument3 Seiten157 Fullnazanin zahra rezaeiNoch keine Bewertungen
- Multiple Gestation: Complications of Labor and Birth Problems With The PassengerDokument4 SeitenMultiple Gestation: Complications of Labor and Birth Problems With The PassengerAmethystNoch keine Bewertungen
- Persistent Occiput PosteriorDokument15 SeitenPersistent Occiput Posteriorm8wyb2f6ngNoch keine Bewertungen
- Drug Study Format 1Dokument3 SeitenDrug Study Format 1Janeenne Fe Nicole SilvanoNoch keine Bewertungen
- Placenta Previa: DefinitionDokument4 SeitenPlacenta Previa: DefinitionCT Johara MusorNoch keine Bewertungen
- Prevention of Preterm Delivery: Current Challenges and Future ProspectsDokument13 SeitenPrevention of Preterm Delivery: Current Challenges and Future ProspectsgalihNoch keine Bewertungen
- Placenta Accreta A Practical Review 2020Dokument6 SeitenPlacenta Accreta A Practical Review 2020Adriana MartínezNoch keine Bewertungen
- Safe Sleep and Skin-to-Skin Care in The Neonatal Period For Healthy Term NewbornsDokument12 SeitenSafe Sleep and Skin-to-Skin Care in The Neonatal Period For Healthy Term NewbornsKatherine Peña SánchezNoch keine Bewertungen
- Placenta Increta Concept MapDokument1 SeitePlacenta Increta Concept MapEkay OrsolinoNoch keine Bewertungen
- Prenatal DiagnosisDokument8 SeitenPrenatal DiagnosisEstefania GutierrezNoch keine Bewertungen
- Screening For Placenta Accreta at 11-14 Weeks of GestationDokument6 SeitenScreening For Placenta Accreta at 11-14 Weeks of Gestationjuljim01Noch keine Bewertungen
- Physiological Changes of The PuerperiumDokument6 SeitenPhysiological Changes of The PuerperiumBladimir CentenoNoch keine Bewertungen
- Emergency Delivery and Peripartum EmergenciesDokument20 SeitenEmergency Delivery and Peripartum EmergenciesRocky PangerapanNoch keine Bewertungen
- Plasenta Previa PDFDokument4 SeitenPlasenta Previa PDFZuriatun HasanahNoch keine Bewertungen
- DeafDokument9 SeitenDeafsagung93Noch keine Bewertungen
- Fetal SurgeryDokument27 SeitenFetal SurgeryFileScanNoch keine Bewertungen
- Revista CienciaDokument126 SeitenRevista CienciaMario SantayanaNoch keine Bewertungen
- I J V S: Nternational Ournal of Eterinary CienceDokument3 SeitenI J V S: Nternational Ournal of Eterinary CienceMarangga SarpakenakaNoch keine Bewertungen
- Journal Reading: Advisor: Dr. Ariawan Ditya, SP - OG Arranged byDokument18 SeitenJournal Reading: Advisor: Dr. Ariawan Ditya, SP - OG Arranged bydesti cahyantiNoch keine Bewertungen
- Placenta Accreta Spectrum: Risk Factors, Diagnosis and Management With Special Reference To The Triple P ProcedureDokument8 SeitenPlacenta Accreta Spectrum: Risk Factors, Diagnosis and Management With Special Reference To The Triple P Proceduremiss betawiNoch keine Bewertungen
- Management of Uterine Inversion: Operative TechniquesDokument4 SeitenManagement of Uterine Inversion: Operative TechniquesMuhammad AzkaNoch keine Bewertungen
- Artículo Redalyc 323449162009Dokument10 SeitenArtículo Redalyc 323449162009DesyHandayaniNoch keine Bewertungen
- VBACDokument8 SeitenVBACKukuh PrasetyoNoch keine Bewertungen
- The Pathology of Placenta Accreta, A Worldwide EpidemicDokument6 SeitenThe Pathology of Placenta Accreta, A Worldwide EpidemicYoga ParipurnaNoch keine Bewertungen
- Incompetent Department: CervixDokument5 SeitenIncompetent Department: CervixFaradiba NoviandiniNoch keine Bewertungen
- Vasa Praevia RCOG GTGDokument13 SeitenVasa Praevia RCOG GTGMariaBrincatNoch keine Bewertungen
- Green Olive Minimalis Modern Trip Promotion Trifold Brochure - 20240311 - 131605 - 0000Dokument3 SeitenGreen Olive Minimalis Modern Trip Promotion Trifold Brochure - 20240311 - 131605 - 0000Christie TirolNoch keine Bewertungen
- Palacios-Jaraquemada. Advantages of Individualizing The PAS Management. Frontiers 2023Dokument4 SeitenPalacios-Jaraquemada. Advantages of Individualizing The PAS Management. Frontiers 2023Devy JuárezNoch keine Bewertungen
- Placenta Previa: Distance To Internal Os and Mode of DeliveryDokument3 SeitenPlacenta Previa: Distance To Internal Os and Mode of DeliveryZEMENAY TRUNEHNoch keine Bewertungen
- Umbilical CordDokument6 SeitenUmbilical Cordterry mutiaNoch keine Bewertungen
- GGGDokument1 SeiteGGGterry mutiaNoch keine Bewertungen
- Cover Jurnal Obsos MUTDokument1 SeiteCover Jurnal Obsos MUTterry mutiaNoch keine Bewertungen
- As Long Ago As of A: 'OrrespondenceDokument6 SeitenAs Long Ago As of A: 'Orrespondenceterry mutiaNoch keine Bewertungen
- Factors Affecting Retained Fetal Membrane and Its Therapeutic Management in Dairy CowsDokument5 SeitenFactors Affecting Retained Fetal Membrane and Its Therapeutic Management in Dairy Cowsterry mutiaNoch keine Bewertungen
- Matsuzaki 2018Dokument28 SeitenMatsuzaki 2018terry mutiaNoch keine Bewertungen
- Hepatitis B in PregnancyDokument12 SeitenHepatitis B in PregnancyTasya Felicia MacellinNoch keine Bewertungen
- Hepatitis B in PregnancyDokument7 SeitenHepatitis B in Pregnancynino123456Noch keine Bewertungen
- Hepatitis B in Pregnancy and The Postnatal Period Clinical Guidelines Register No: 12004 Status: PublicDokument13 SeitenHepatitis B in Pregnancy and The Postnatal Period Clinical Guidelines Register No: 12004 Status: Publicterry mutiaNoch keine Bewertungen
- Infanticide AbortionDokument2 SeitenInfanticide AbortionDee LMNoch keine Bewertungen
- Breech Presentation - PPT (Read-Only)Dokument5 SeitenBreech Presentation - PPT (Read-Only)Nestor SantiagoNoch keine Bewertungen
- The Partograph: Dr. Udin Sabarudin, SpogDokument30 SeitenThe Partograph: Dr. Udin Sabarudin, SpogJenni Irmacikita Irawaty SanaanNoch keine Bewertungen
- STUDENT Tasks For NCM Culminating ProgramDokument4 SeitenSTUDENT Tasks For NCM Culminating ProgramLyra LorcaNoch keine Bewertungen
- Fertility HerbsDokument17 SeitenFertility HerbsKyle J. Norton100% (1)
- Chromium BrochureDokument2 SeitenChromium BrochurevietvuducNoch keine Bewertungen
- Prenatal Genetic DiagnosisDokument38 SeitenPrenatal Genetic DiagnosismaneshaputraNoch keine Bewertungen
- Assessment of Condom Use For Prevention of Hiv/Aids Among Jimma University Students, Jimmatown, South West EthiopiaDokument42 SeitenAssessment of Condom Use For Prevention of Hiv/Aids Among Jimma University Students, Jimmatown, South West EthiopiaFitalaBokaNoch keine Bewertungen
- OvulationDokument2 SeitenOvulationEarl CopeNoch keine Bewertungen
- Biology 10th Edition Mader Test BankDokument23 SeitenBiology 10th Edition Mader Test Bankphelanaletheaa7ye100% (33)
- Obs QNDokument15 SeitenObs QNAnurag AnupamNoch keine Bewertungen
- Obstetrics MCQDokument8 SeitenObstetrics MCQSandip Patil100% (6)
- Testicular BreathingDokument8 SeitenTesticular BreathingYCY57% (30)
- Premature Rupture of Membranes (Prom)Dokument12 SeitenPremature Rupture of Membranes (Prom)KABERA RENE50% (2)
- Menstrual HygieneDokument8 SeitenMenstrual HygieneManvendra Pratap SinghNoch keine Bewertungen
- Cognitive Behavioral Erectile Dysfunction TreatmeDokument11 SeitenCognitive Behavioral Erectile Dysfunction Treatmefunny_tricksterNoch keine Bewertungen
- Cudurada Kudhaca XoolahaDokument11 SeitenCudurada Kudhaca XoolahaAnonymous ZeRmTfJY83% (12)
- Wollo UniversityDokument14 SeitenWollo UniversityabdishakurNoch keine Bewertungen
- Female GenitaliaDokument96 SeitenFemale GenitaliaJopaii TanakaNoch keine Bewertungen
- Maternal and Child NursingDokument9 SeitenMaternal and Child NursingWarrenSandoval100% (12)
- C Section Step by StepDokument2 SeitenC Section Step by Stepj_nagelyNoch keine Bewertungen
- Nursing Process - Placenta PreviaDokument56 SeitenNursing Process - Placenta PreviaRicardo Robianes BautistaNoch keine Bewertungen
- Republic of The Philippines Vs CagandahanDokument3 SeitenRepublic of The Philippines Vs CagandahanSheng EyyNoch keine Bewertungen
- Code: VT802-KIT: DS WS1 WS2Dokument2 SeitenCode: VT802-KIT: DS WS1 WS2Sep NeufNoch keine Bewertungen
- GNRH - Gonadotropin Releasing HormoneDokument2 SeitenGNRH - Gonadotropin Releasing Hormonehaydunn55Noch keine Bewertungen
- Perineal CareDokument10 SeitenPerineal Careoxidalaj100% (11)
- 4 Male and Female Reproductive Organs PPTDokument71 Seiten4 Male and Female Reproductive Organs PPTDanica Marie Sibay100% (1)
- Human Reproduction PyqsDokument7 SeitenHuman Reproduction PyqsMrityunjay PandeyNoch keine Bewertungen
- OA 6 SeptDokument19 SeitenOA 6 Septstella pangestikaNoch keine Bewertungen
- Premature Rupture of MembranesDokument4 SeitenPremature Rupture of MembranesRobiyanti Nur Chalifah HattaNoch keine Bewertungen