Beruflich Dokumente
Kultur Dokumente
Mock Board Operative Section
Hochgeladen von
ahmadrid93Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Mock Board Operative Section
Hochgeladen von
ahmadrid93Copyright:
Verfügbare Formate
(University of Louisville School of Dentistry)
Candidate Manual
Mock Board Operative Dentistry Section:
Students must complete restorations as described in your clinical operative manual on
blackboard that is paraphrased below:
Each student is required to complete 3 (three) competency examinations on permanent vital teeth
on patients of record before the end of the spring semester senior year (clinical operative
dentistry II).
2 (two) direct posterior Class II preparation/restoration
o Must have at least one virgin proximal lesion or evidence of significant
clinical caries to the DEJ
o One (1) restored with amalgam
o One (1) restored with composite
1 (one) direct anterior Class III or IV preparation/restoration
o Must have at least one virgin proximal lesion or evidence of significant
clinical caries to the DEJ
o Restored with composite
One (1) of these competency examinations must be successfully completed prior to
participating in Mock Boards.
Two (2) of these competency examinations must be successfully completed as part of the Mock
Boards.
Mock Board Examination
The Mock Boards are designed to simulate actual testing situations on regional licensure
examinations. The Mock Board examination is an amalgamation of the regional WREBS, SRTA,
NERBS and ADEX examinations. It is NOT designed to mimic any one of the above listed
examinations to eliminate any bias. Students have the autonomy to take any regional
examination (if qualified) and should make themselves familiar with the selected testing format
and documentation.
The operative section of the mock boards must be successfully completed during the scheduled
examination time frame, or, in the event of a failure, successfully retaken on a later specified
date. Upon successful completion of both Mock Board indications, credit will be awarded
towards Clinical Operative Dentistry II. Upon unsuccessful completion of one or both Mock
Board indications, a formal remediation will be assigned as deemed appropriate by the Course
Director to improve deficient areas in operative dentistry.
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 1
Successful completion of the mock board operative section is mandatory to receive a final grade
in Clinical Operative Dentistry II and to graduate. You will not be given permission to register to
participate in any regional licensure examination until the operative section of the Mock Boards
is successfully completed. Additional detailed information will be forthcoming about Mock
Board Examinations in the spring semester as part of the Mock Board Manual.
Examination Guidelines
Once a student has been approved to begin the examination, the student must proceed and cannot
withdraw without penalty of failure.
Students are expected to provide compassionate and ethical care to their patients. Failure to do so
will result in failure of the examination.
Students are expected to communicate effectively with faculty, staff and patients. Failure to do
so will result in a significant reduction in grade.
The health history form as found in this manual must be completed for each patient. Failure to do
so will result in a significant reduction in grade.
Patient approval for a second operative procedure, if done on a different patient, will occur in the
scoring area. When you are ready, a runner will bring the patient with the instruments and
appropriate paperwork to the scoring area for a pre-op check.
If both operative procedures are to be done on the same patient, both lesions may be approved at
the same time. Both teeth may be prepped/ restored at the same time as long as they are in the
same arch and comfortably isolated and are not adjacent. If students decide to share a patient,
each student will complete separate paperwork and will submit separately from the other student.
Patients must be ambulatory and able to move about easily.
Patients requiring the administration of Nitrous Oxide will not be treated.
Students will receive no instructor input during the exam. Floor Examiners have been calibrated
to answer questions for modification requests and potential pulp exposures. Should faculty find it
necessary to intervene in patient treatment during the examination, this will result in failure of
the examination.
Two faculty members will grade each preparation and restoration independently consistent with
the grading rubric in your preclinical and clinical operative courses (below). A third examiner
will be consulted, if necessary, for a final decision in grading should it occur.
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 2
Grading Scale
The evaluation of the mock board examination preparation, restoration and overall performance
will be based on the following grading scale:
3= Superior; satisfies all criteria
2= Acceptable; could be improved with minor deficient area improvement
1= Marginal; needs major improvement in deficient areas
0= Unacceptable; unsatisfactory and serious remediation is required
The examiners of the mock board examination reserve the right to score in (.5) increments. The
following conversion of averaged points to a course letter grade will be employed by the Course
Director as graded by the two examiners:
2.50 – 3.00 = A
2.00 – 2.49 = B
1.50 – 1.99 = C
< 1.50 =F
Photographs may be taken (of preparations and restorations) which will be used for remediation/
teaching purposes and does not in itself constitute failure of the examination procedure.
Patient Selection: the patient can be:
Another dental student (1st, 2nd 3rd year)
A dental hygiene student
A ULSD staff member
A ULSD patient of record
Assistants are encouraged and can be another dental student: 1st, 2nd, 3rd year level ….however
the senior dental student taking the mock board exam is expected to perform the competency on
their own and without inappropriate assistance. Failure to do so will result in failure of the
examination.
The assigned Mock Board number must be written on the upper right side of the patient’s
UNSOILED napkin.
Radiographs: At pre-op: current radiographs (single PA and 1 bitewing radiographs) that reflect
the condition of the area to be restored as well as the contralateral side of the arch must be
evident. Radiographs also should have been taken within the last 6 months. If a student is using
a digital radiograph, the patient’s ID number/ name must be sent with the patient to the grading
area so that the radiograph can be pulled up in axium for evaluation.
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 3
Criteria for acceptance of a lesion radiographically and clinically are laid out in your clinical
operative manual on blackboard. A point of emphasis is that the mesial/occlusal surfaces of
#21 and #28 will NOT be accepted for this Mock Board Examination.
Critical errors (Automatic Failures) listed in your clinical operative manual on blackboard will
be the same critical errors/ automatic failures for the Mock Board examination (below).
Critical Errors
The following critical errors are considered below minimal competency standards and will result
in an unsatisfactory performance on the competency examination and recorded as a 0 (zero):
Inadequate anesthesia
Poor or no rubber dam isolation
Mechanical or carious pulpal exposure
Extremely over-extended preparation outline
Extremely under-extended preparation outline
o Preparation still in or partially in enamel
o Proximal contacts not broken
Incomplete caries removal
Incomplete removal of ALL previous restorative materials (including bases and liners)
Major damage to hard or soft tissue during preparation and/or finishing restoration
Inadequate proximal contact design (too open or too tight)
Significant overhang and/or flash over cavosurface margin
Open cavosurface margin or voids in the final restoration
Hyperocclusion
Significant over-carving with compromised anatomical form and function
Examination proposed or completed on non-vital tooth
Preparing the wrong tooth (one not pre-approved) or tooth surface(s) of approved tooth
Cracked or broken restorations
Poor time management/ Past time limit
Unprofessional/ unethical conduct towards examiners and/or patient
Receiving a zero (0) in any of the criteria categories
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 4
MOCK BOARD FORMS
OPERATIVE DENTISTRY SECTION
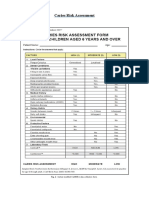
Health History Form
Form used and reproduced with permission of the Southern Regional Testing Agency (SRTA)
A completed Health History Form, current within 30 days, is required for each patient treated.
The patient’s blood pressure and pulse are taken and recorded on the Health History Form on the
day of the examination. No treatment will be allowed if the patient’s blood pressure is greater
than 160/100 the day of the examination. A patient may not be:
A dentist
Latex sensitive
A female in the first or third trimester of pregnancy
Receiving intravenous (IV), intramuscular (IM), or subcutaneous bisphosphonates, (Not
including oral bisphosphonates) in the past 18 months
The patient's health status must be acceptable for treatment. Any patient who presents with a
history of previous bacterial endocarditis, an artificial heart valve, a congenital heart defect that
has not been successfully repaired or a heart transplant must verify in writing on the Health
History Form that he/she has taken or has been released from taking the proper medication
prescribed by his/her physician, in compliance with the guidelines established in April 2007 by
the American Heart Association. This also holds true for patients who have a history of previous
orthopedic joint replacements. All questions on the Health History Form must be answered
“Yes” or “No” by the patient, including all questions in the shaded area. If the patient responds
“Yes” to any of the questions in the shaded area, a physician’s written verification of
acceptability for treatment is required and must be available to examiners during patient approval
or the patient will not be allowed to participate in the examination. A physician’s note is required
for patients with the following health history:
Cardiovascular disease, including angina pectoris, a previous heart attack, coronary
insufficiency, coronary occlusion, congestive heart failure, an internal cardiac defibrillator or
pacemaker, a previous transient ischemic attack (TIA)
Stroke (CVA)
Blood dyscrasias (hemophilia)
Active tuberculosis
Kidney/renal disease
Current epilepsy, seizure activity or fainting
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 5
This written clearance must be presented at registration with the Health History Form. An
acceptable medical clearance/statement includes
A statement from a physician written on his/her letterhead or prescription pad within 30
days of the examination
A statement of how the patient should be managed
The exact procedure that is to be performed (i.e., amalgam, composite)
The physician's clearly legible name, address and phone number
The Health History Form must be submitted at patient approval. Additional copies of the form
will be available at registration and from the Clinic Floor Coordinator.
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 6
Patient Acceptance/ Modification/ Limited Treatment Plan/ Anesthesia Record
Appendix I
Patient Acceptance/ Modification/ Limited Treatment Plan/ Anesthesia Record form is used to
qualify the proposed lesion for examination, record any major modification request, obtain
informed consent and document anesthesia use throughout the examination process. The
candidate must complete the information at the top of the page in ink and may place a 2nd or 3rd
indication for examination on the same patient. The candidate may receive a radiographic
DENTAL REJECTION NOTICE if the films are ≥ 6 months old, non-diagnostic and/or lesion
depth does not qualify. Additionally, the candidate may receive a DENTAL REJECTION
NOTICE clinically if the lesion is non-detectable with an explorer or the radiographs don’t
match the current clinical situation. A 2nd and 3rd indication may be requested on the same form
ON THE SAME PATIENT. Each new submission of a new patient gets a new form and will be
screened in the staging area. The accepting examiner will circle the approved lesion and place a
solid line in the boxes under “Dental Rejection Notice” for both radiograph and clinical
examination if no comments need to be made.
Should the need arise to make a major extension of a preparation, the candidate is required to
complete a Modification Request with written justification and the proposed treatment for any
major modification. Before proceeding with the procedure, the candidate must contact the
Clinic Floor Coordinator to clinically observe the stated need for the major modification.
The completion of a Modification Request does not constitute automatic authorization or
approval. The Clinic Floor Coordinator must record his/her approval or disapproval concerning
the candidate’s stated justification for the modification. The candidate will then forward the
Patient Acceptance Form (red) to the scoring area for use when the patient is sent for scoring.
Failure to obtain the Clinic Floor Coordinator's clinical observation will negatively impact the
candidate's score.
Example: The candidate is preparing a Class II Slot or Conventional Composite Preparation. In
the course of the procedure, the margins of the preparation have moved closer than 1 mm to the
CEJ, and decalcification is still present below the gingival margin. The candidate should
complete a Modification Form to indicate that he/she is requesting to change the preparation to a
Class II Amalgam procedure.
The candidate must complete a Modification Request when a pulp exposure occurs.
If the Clinic Floor Coordinator (CFC) feels that a candidate has presented a Modification
Request proposing excessive treatment or that the reason for modification demonstrates a lack of
professional judgment, the CFC will send the patient to the scoring area, where one examiner
will evaluate the candidate’s proposed modification. If the examiner agrees with the stated
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 7
modification, the candidate will be instructed to continue with the proposed treatment. If the
examiner disagrees with the stated modification, the candidate will fail that section of the
examination stating that the candidate has proposed excessive treatment or demonstrated a lack
of professional judgment.
The candidate modification request can be approved by the clinical floor coordinator or grading
examiners. Once any modifications are requested and/or performed, this form must
accompany the patient to the grading area with the preparation grading form. This will
allow the examiners to see any modification performed as part of the final preparation
evaluation.
ON THE REVERSE SIDE
The candidate must obtain informed consent by having the patient sign their limited treatment
plan as presented AFTER the patient is accepted. If the patient is NOT accepted, there will be
NO treatment rendered.
The candidate must record every aspect of anesthesia use during the examination. The candidates
will be provided with 2 carpules of 2% lidocaine with 1:100k epinephrine which must be
recorded. A request for additional anesthesia must be presented to the floor coordinators for
approval. Under no circumstances will a candidate receive more than 4 carpules of anesthesia
during any one procedure. Inability to achieve profound anesthesia will result in a failure for this
examination.
The Operative Discipline Coordinator will place the final grades on this sheet as part of your
final grade per performance recommendations by the clinical floor coordinators. PLEASE DO
NOT PLACE GRADES FOR YOURSELF.
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 8
Procedural Forms
Appendices II-III-IV
Four of the six below forms will be used depending on which indications are required to fulfill
your senior competencies as written in you clinical operative manual on blackboard (paraphrased
in yellow above).
Once the proposed patient has been approved on the “Patient Acceptance/ Modification Form”,
the appropriate indication must be completed on one of the above forms in ink for EACH
INDICATION (except the pass/fail area).
Class II Amalgam Preparation Evaluation Form (Appendix II)
This form is used when sending patient to staging area for class II amalgam preparation
evaluation. A grading scale is located in the bottom right hand corner and will follow the
grading rubric described in your clinical operative manual. Only this form is necessary
for grading if there have been no modification requests or potential pulp exposures. If
there has been modification/s approved and performed, please send the “Patient
Acceptance Form” along with the preparation evaluation form. If there is actual pulp
exposure or potential pulp exposure, please refer to the “Pulp Management” form for
detailed overview. In summary of the “Pulp Management Form” (pink), all actual pulp
exposures will be documented on the “Patient Acceptance Form” and sent to the staging
area for evaluation/treatment recommendations. All potential pulp exposures are a STOP
light for the student to show the floor coordinators their FINAL PREPARATION minus
the area of concern. The “Pulp Management Form” with this information certified by the
floor coordinator must be sent to the staging area.
You may get back from the grading area an “Instructions to the Candidate Form”
detailing areas of attention that must be approved before and after by the floor
coordinators via their initials before placing final restoration. Please see the section
detailing the “Instructions to the Candidate Form”.
Class II Amalgam Restoration Evaluation Form (Appendix II)
This form is used when sending a patient to the staging area for class II amalgam
restoration evaluation. A grading scale is located in the bottom right hand corner and will
follow the grading rubric described in your clinical operative manual. Only this form is
necessary for grading the final restoration.
You may get back from the grading area an “Instructions to the Candidate Form”
detailing areas of attention that must be approved before and after by the floor
coordinators via their initials before dismissing your patient. Please see the section
detailing the “Instructions to the Candidate Form”.
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 9
Class II Composite Preparation Evaluation Form (Appendix III)
Same as described above.
Class II Composite Restoration Evaluation Form (Appendix III)
Same as described above.
Class III Composite Preparation Evaluation Form (Appendix IV)
Same as described above.
Class III Composite Restoration Evaluation Form (Appendix IV)
Same as described above.
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 10
Pulp Management Form
Appendix V
The pulp management form is utilized in the situations where the vitality of the pulp may be
compromised. This form is completed when the candidate recognizes that the pulp may be
compromised BEFORE it is exposed. This form is a STOP LIGHT for treatment to allow the
floor coordinator to evaluate the FINAL PREPARATION minus the small area of concern. If the
floor coordinator is asked to look before the final preparation is complete, the candidate will fail
the examination due to poor clinical judgment. The floor coordinator will initial this form,
provide possible notes to the examiners and send to the grading area for evaluation. An
“Instructions to the Candidate Form” will return with treatment guidelines/ recommendations
from the grading examiners.
If an actual pulp exposure occurs, stop the examination procedure and complete a modification
request on the “Patient Acceptance Form” and request a floor coordinator attention for
evaluation. The floor coordinator will initial this form, provide possible notes to the examiners
and send to the staging area for evaluation. An “Instructions to the Candidate Form” will return
with treatment guidelines/ recommendations from the grading examiners.
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 11
Instruction to Candidate Form
Appendix VI
The Instruction to Candidate Form may be completed by the examiners in the scoring area to
notify the candidate that additional adjustments, removal of caries or postoperative care is
required. The “Instruction to the Candidate” form is also used to convey information to the
patient about follow-up care that may be needed.
This form is used only for certain errors that can be adjusted at the examination site or to inform
the patient that postoperative care is required. The form is not used to notify candidates of failure
of an examination section nor does it imply failure. Critical errors are described in the clinical
operative manual located on blackboard and the candidates should be familiar with them.
Examples (not all inclusive) of critical errors on the preparation procedures include:
Unsupported enamel
Preparation too shallow
Base placement required
Margins in defective tooth structure
Examples (not all inclusive) of critical errors on the restoration procedures include:
High occlusion
Overhang at the gingival margin that needs to be removed
Student Flow and Self-evaluation Form
Appendix VII
Students please score yourself on the Student Self Evaluation Form in all three areas via the
grading rubric in your candidate manuals. A separate grade for your preparation, restoration and
overall performance is required to receive a final grade for the mock board examination on each
lesion restored. Incomplete self-evaluation forms for each lesion will result in an overall failure
for the examination.
Mock Board Preparation Materials
Operative Dentistry Section, Candidate Manual
Page 12
Das könnte Ihnen auch gefallen
- PAPAYA Plus User's Manual Eng Ver 1.2Dokument102 SeitenPAPAYA Plus User's Manual Eng Ver 1.2Hostoben hospital100% (2)
- How To Argue and Win Every TimeDokument24 SeitenHow To Argue and Win Every TimeMeiHong Lynn Wong100% (1)
- BDA Consent 2016Dokument9 SeitenBDA Consent 2016KandiwapaNoch keine Bewertungen
- Moldova SMPhU 2014 DubaiDokument28 SeitenMoldova SMPhU 2014 DubaiIgor CemortanNoch keine Bewertungen
- OSCE - Health PromotionDokument13 SeitenOSCE - Health PromotionbabukanchaNoch keine Bewertungen
- Dscke 2015 - Sample Questions For Website - Revised February 2016 - English PDFDokument7 SeitenDscke 2015 - Sample Questions For Website - Revised February 2016 - English PDFBranko MaticNoch keine Bewertungen
- ADEA CAAPID InstructionsDokument10 SeitenADEA CAAPID Instructionsshyam05_narainNoch keine Bewertungen
- ACJ 2017 ProtocolDokument17 SeitenACJ 2017 ProtocollkjhgfdsalkNoch keine Bewertungen
- Essential Tissue Healing of the Face and NeckVon EverandEssential Tissue Healing of the Face and NeckBewertung: 5 von 5 Sternen5/5 (2)
- NATIONAL OPTOMETRY BOARDS (NOB) Part III PATIENT CARE: Passbooks Study GuideVon EverandNATIONAL OPTOMETRY BOARDS (NOB) Part III PATIENT CARE: Passbooks Study GuideNoch keine Bewertungen
- UAF References Style 2020Dokument8 SeitenUAF References Style 2020ahmadrid9333% (3)
- Os Roent PDFDokument87 SeitenOs Roent PDFTJ OberioNoch keine Bewertungen
- DENTAL AUXILIARY EDUCATION EXAMINATION IN DENTAL MATERIALS: Passbooks Study GuideVon EverandDENTAL AUXILIARY EDUCATION EXAMINATION IN DENTAL MATERIALS: Passbooks Study GuideNoch keine Bewertungen
- An Examiner’s Guide to Professional Plastic Surgery ExamsVon EverandAn Examiner’s Guide to Professional Plastic Surgery ExamsNoch keine Bewertungen
- What Is EBD?Dokument7 SeitenWhat Is EBD?RATHEESH M. S.Noch keine Bewertungen
- 2019 NBDHE Guide PDFDokument29 Seiten2019 NBDHE Guide PDFHosam MahmoudNoch keine Bewertungen
- Caries and Quality of Life in Portuguese Adolescents: Impact of Diet and Behavioural Risk FactorsDokument6 SeitenCaries and Quality of Life in Portuguese Adolescents: Impact of Diet and Behavioural Risk FactorsCristian OneaNoch keine Bewertungen
- NEW Online Exam Guideline 2020Dokument87 SeitenNEW Online Exam Guideline 2020arezooNoch keine Bewertungen
- Oral and Maxillofacial Surgery An Objective Based PDFDokument1 SeiteOral and Maxillofacial Surgery An Objective Based PDFRuhi AhmedNoch keine Bewertungen
- Reference Texts For The Advanced Dental Admissions Test (ADAT)Dokument6 SeitenReference Texts For The Advanced Dental Admissions Test (ADAT)SanNoch keine Bewertungen
- Treatment Planning 2Dokument7 SeitenTreatment Planning 2api-660191691Noch keine Bewertungen
- Dental InformaticsDokument13 SeitenDental Informaticsho laNoch keine Bewertungen
- Medical Emergencies in Dental OfficeDokument92 SeitenMedical Emergencies in Dental Officeapi-3704106100% (7)
- Infection Control BDADokument15 SeitenInfection Control BDAMariam WaseemNoch keine Bewertungen
- Dental MCQDokument22 SeitenDental MCQPinpointq0% (1)
- 3Dokument2 Seiten3imtiyazh85100% (1)
- Dental Assisting and Charting Course OutlineDokument4 SeitenDental Assisting and Charting Course OutlineShimika TennantNoch keine Bewertungen
- A Road To TOACSDokument33 SeitenA Road To TOACSSoha Jan KhuhawarNoch keine Bewertungen
- Dental Assistant Emergency CareDokument2 SeitenDental Assistant Emergency CareAshfahan Alam100% (1)
- Info Immediate DenturesDokument4 SeitenInfo Immediate DenturesDyah Wulan RamadhaniNoch keine Bewertungen
- Vodic Za Stomatologe DHADokument9 SeitenVodic Za Stomatologe DHAIvanaNoch keine Bewertungen
- Outpatient Care Facilities RegulationDokument68 SeitenOutpatient Care Facilities RegulationDzikri PutraNoch keine Bewertungen
- Partial Dentures PDFDokument1 SeitePartial Dentures PDFGabriela ArgeseanuNoch keine Bewertungen
- Dental Hygiene Portfolio GuideDokument12 SeitenDental Hygiene Portfolio GuideMostafa FayadNoch keine Bewertungen
- Syllabus 5k en ExamDokument2 SeitenSyllabus 5k en ExamVagelis RaftopoulosNoch keine Bewertungen
- Antibiotics in DentistryDokument3 SeitenAntibiotics in DentistrymanikantatssNoch keine Bewertungen
- Medical Problems in DentistryDokument13 SeitenMedical Problems in DentistryعصامالعبيديNoch keine Bewertungen
- Sample Questions MJDF Part 1 Sample Questions MJDF Part 1Dokument21 SeitenSample Questions MJDF Part 1 Sample Questions MJDF Part 1HarkanNoch keine Bewertungen
- Foreign Trained Dentists To US - FullDokument8 SeitenForeign Trained Dentists To US - Fullh20pologt100% (1)
- Dionne: Management of Pain Anxiety in The Dental OfficeDokument690 SeitenDionne: Management of Pain Anxiety in The Dental OfficeseveredtiesNoch keine Bewertungen
- RCDSO Infection ControlDokument56 SeitenRCDSO Infection ControlsnaniraqNoch keine Bewertungen
- Basics of EndodonticsDokument26 SeitenBasics of EndodonticsAreebaKhalidNoch keine Bewertungen
- Write Your Name On Your Scantron Scoring SheetDokument8 SeitenWrite Your Name On Your Scantron Scoring Sheetchakriy9Noch keine Bewertungen
- MJDF April 2019 PDFDokument16 SeitenMJDF April 2019 PDFsajna1980Noch keine Bewertungen
- ABCD PedodontiaDokument120 SeitenABCD Pedodontiahridarjunn100% (4)
- Systemic Diseases Manifested in The JawsDokument25 SeitenSystemic Diseases Manifested in The JawsTeguh Caninus100% (1)
- Dental Assisting ProgramsDokument4 SeitenDental Assisting ProgramsJuan EstebanNoch keine Bewertungen
- Adex Dental Exam Series: Fixed Prosthodontics and EndodonticsDokument36 SeitenAdex Dental Exam Series: Fixed Prosthodontics and EndodonticsmeethaileyyyNoch keine Bewertungen
- MJDF Part 1 OCTOBER 2019Dokument7 SeitenMJDF Part 1 OCTOBER 2019sajna1980Noch keine Bewertungen
- Structure of The Medical Prescription. Prescription WritingDokument8 SeitenStructure of The Medical Prescription. Prescription WritingAdelia Desti Endah SariNoch keine Bewertungen
- Anesthesia For Maxillofacial ProcedureDokument90 SeitenAnesthesia For Maxillofacial ProcedureAnirban Roy100% (1)
- 1000 MCQ For Emergency MedicineDokument161 Seiten1000 MCQ For Emergency MedicineAsif NewazNoch keine Bewertungen
- 13 Osha Infection ControlDokument78 Seiten13 Osha Infection ControlAnonymous c8G1bmIrNoch keine Bewertungen
- Webinar Course of Pediatric Dentistry November 30-December 1 PDFDokument11 SeitenWebinar Course of Pediatric Dentistry November 30-December 1 PDFLarisa Oros FulczNoch keine Bewertungen
- Periodicity DentalGuideDokument52 SeitenPeriodicity DentalGuideSalam BataienehNoch keine Bewertungen
- Oral Surgery - Treatment Planning GuidelinesDokument5 SeitenOral Surgery - Treatment Planning GuidelinesFaizal Prabowo KalimanNoch keine Bewertungen
- The Paediatric PatientDokument6 SeitenThe Paediatric PatientSueChen TanNoch keine Bewertungen
- 03 MFDS Regulations & Syllabus 2011Dokument15 Seiten03 MFDS Regulations & Syllabus 2011FarahMohammed1Noch keine Bewertungen
- Endodontics in Systemically Compromised PatientsDokument30 SeitenEndodontics in Systemically Compromised Patientscarolina pavezNoch keine Bewertungen
- Anesthesia and Extraction in Children: Dr. Masar MohammedDokument46 SeitenAnesthesia and Extraction in Children: Dr. Masar Mohammedscribfoerte100% (1)
- Geriatric Dentistry: Caring for Our Aging PopulationVon EverandGeriatric Dentistry: Caring for Our Aging PopulationNoch keine Bewertungen
- What After BDS Career OptionsDokument10 SeitenWhat After BDS Career OptionsDENTALORG.COM100% (1)
- Essentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly DifferentVon EverandEssentials for Practice of Medicine in the Frontline: From Tropical Africa; Pleasantly DifferentNoch keine Bewertungen
- Is VeryDokument1 SeiteIs Veryahmadrid93Noch keine Bewertungen
- Useful Downloads: The Centre For Teaching & LearningDokument1 SeiteUseful Downloads: The Centre For Teaching & Learningahmadrid93Noch keine Bewertungen
- Abstract Book PDFDokument80 SeitenAbstract Book PDFahmadrid93Noch keine Bewertungen
- Cur R Ent Year Licensed PR Ivate Schools Repor T: Name Administrator Mailing Address City State Zip CodeDokument3 SeitenCur R Ent Year Licensed PR Ivate Schools Repor T: Name Administrator Mailing Address City State Zip Codeahmadrid93Noch keine Bewertungen
- First Semester 2013/2014Dokument5 SeitenFirst Semester 2013/2014NourAldin AbuSalehNoch keine Bewertungen
- First Semester 2013/2014Dokument5 SeitenFirst Semester 2013/2014NourAldin AbuSalehNoch keine Bewertungen
- Calendar - 2014-2015 - ArDokument6 SeitenCalendar - 2014-2015 - Arahmadrid93Noch keine Bewertungen
- Materi Ajar D3 Kep - GigiDokument34 SeitenMateri Ajar D3 Kep - GigiMelysa SlebesNoch keine Bewertungen
- Dental Radiology An Adjunctive Aid in Age EstimationDokument5 SeitenDental Radiology An Adjunctive Aid in Age EstimationalyaNoch keine Bewertungen
- 3 Radiographic Dental Assessment For The Child Patient PDFDokument21 Seiten3 Radiographic Dental Assessment For The Child Patient PDFFamodimu Funbi SamuelNoch keine Bewertungen
- 4203 RHS Exam BlueprintDokument10 Seiten4203 RHS Exam BlueprintAliceNoch keine Bewertungen
- 125 Years of Developments in DentistryDokument4 Seiten125 Years of Developments in DentistryShoaib A. KaziNoch keine Bewertungen
- Tooth Detection From Panoramic Radiographs Using Deep LearningDokument11 SeitenTooth Detection From Panoramic Radiographs Using Deep LearningShweta ShirsatNoch keine Bewertungen
- 2022 @dentolib Antigoni Delantoni, Kaan Orhan Atlas of DentomaxillofacialDokument229 Seiten2022 @dentolib Antigoni Delantoni, Kaan Orhan Atlas of Dentomaxillofacialc8dqt289hfNoch keine Bewertungen
- BDA Advice Sheet A11Dokument12 SeitenBDA Advice Sheet A11soomro76134Noch keine Bewertungen
- Gendex Expert DC Dental X-Ray - User ManualDokument55 SeitenGendex Expert DC Dental X-Ray - User ManualENGBIONoch keine Bewertungen
- Radiographic Diagnosis of Dental Caries: S. Brent Dove, D.D.S., M.SDokument6 SeitenRadiographic Diagnosis of Dental Caries: S. Brent Dove, D.D.S., M.Saulia lubisNoch keine Bewertungen
- Procedure ListDokument20 SeitenProcedure ListsoyrolandoNoch keine Bewertungen
- Obtaining High Quality Dental Radiographs 45466 ArticleDokument6 SeitenObtaining High Quality Dental Radiographs 45466 ArticleMambaul IkhsanNoch keine Bewertungen
- Dental Radiography For The Pediatric Patient PedoDokument30 SeitenDental Radiography For The Pediatric Patient PedoFourthMolar.comNoch keine Bewertungen
- Xview TridentDokument8 SeitenXview TridentShathaNoch keine Bewertungen
- Effects of Herbal Lollipops On Streptococcus Mutans Levels and The Dental Caries Experience of Children With Asthma Taking B2-Adrenergic Agonish DrugsDokument23 SeitenEffects of Herbal Lollipops On Streptococcus Mutans Levels and The Dental Caries Experience of Children With Asthma Taking B2-Adrenergic Agonish Drugsinfo6680Noch keine Bewertungen
- PaX-i Insight Product DataDokument22 SeitenPaX-i Insight Product DataHichem BellaghaNoch keine Bewertungen
- Fixed Prosthodontics Clinic Manual 2015-2016Dokument73 SeitenFixed Prosthodontics Clinic Manual 2015-2016wendyjemmy8gmailcomNoch keine Bewertungen
- Nabh Application Dental ClinicDokument13 SeitenNabh Application Dental ClinicPriya HariNoch keine Bewertungen
- 2022-Pricelist Feb2022 PDFDokument2 Seiten2022-Pricelist Feb2022 PDFjackNoch keine Bewertungen
- FGDP X-Ray Book Web v2 PDFDokument190 SeitenFGDP X-Ray Book Web v2 PDFMariana IdorașiNoch keine Bewertungen
- Evans Et Al-2008-Australian Dental Journal PDFDokument10 SeitenEvans Et Al-2008-Australian Dental Journal PDFtea metaNoch keine Bewertungen
- User Manual: Portable Dental X-Ray SystemDokument46 SeitenUser Manual: Portable Dental X-Ray SystemOyster Labs Service EngineerNoch keine Bewertungen
- Planmeca ProMax 3D USER ManualDokument108 SeitenPlanmeca ProMax 3D USER ManualmigsayalNoch keine Bewertungen
- DMFR 20220335Dokument22 SeitenDMFR 20220335Albert CamusNoch keine Bewertungen
- X - Gen - Pano Block 11 - Unit 2 Dental Panoramic X-RayDokument8 SeitenX - Gen - Pano Block 11 - Unit 2 Dental Panoramic X-RayĐông PhùngNoch keine Bewertungen
- Dental Caries and Its ManagementDokument15 SeitenDental Caries and Its Managementpennyshevlin1Noch keine Bewertungen
- Wadia 2019 The Updated Periodontal ClassificationDokument4 SeitenWadia 2019 The Updated Periodontal ClassificationPatricia CastellanosNoch keine Bewertungen
- Dental Xray Film and It's Parts (2626)Dokument21 SeitenDental Xray Film and It's Parts (2626)AA HHNoch keine Bewertungen