Beruflich Dokumente
Kultur Dokumente
PPDS McDonald - Et - al-2015-BJOG: - An - International - Journal - of - Obstetrics - & - Gynaecology PDF
Hochgeladen von
Rommy Yorinda PutraOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
PPDS McDonald - Et - al-2015-BJOG: - An - International - Journal - of - Obstetrics - & - Gynaecology PDF
Hochgeladen von
Rommy Yorinda PutraCopyright:
Verfügbare Formate
DOI: 10.1111/1471-0528.
13263 General gynaecology
www.bjog.org
Dyspareunia and childbirth: a prospective cohort
study
EA McDonald,a D Gartland,a R Small,b SJ Browna,c
a
Healthy Mothers Healthy Families Research Group, Murdoch Childrens Research Institute, Melbourne, Vic., Australia b The Judith Lumley
Centre, La Trobe University, Melbourne, Vic., Australia c General Practice and Primary Health Care Academic Centre, The University of
Melbourne, Melbourne, Vic., Australia
Correspondence: EA McDonald, Healthy Mothers Healthy Families Research Group, Murdoch Childrens Research Institute, The Royal
Children’s Hospital, Flemington Road, Parkville, Vic. 3052, Australia. Email ellie.mcdonald@mcri.edu.au
Accepted 15 November 2014. Published Online 21 January 2015.
Objective To investigate the relationship between mode of perineum or unsutured tear, women who had an emergency
delivery, perineal trauma and dyspareunia. caesarean section (adjusted odds ratio [aOR] 2.41, 95% confidence
interval [95% CI] 1.4–4.0; P = 0.001), vacuum extraction (aOR
Design Prospective cohort study.
2.28, 95% CI 1.3–4.1; P = 0.005) or elective caesarean section
Setting Six maternity hospitals in Melbourne, Australia. (aOR 1.71, 95% CI 0.9–3.2; P = 0.087) had increased odds of
reporting dyspareunia at 18 months postpartum, adjusting for
Sample A total of 1507 nulliparous women recruited in the first
maternal age and other potential confounders.
and second trimesters of pregnancy.
Conclusions Obstetric intervention is associated with persisting
Method Data from baseline and postnatal questionnaires (3, 6, 12
dyspareunia. Greater recognition and increased understanding of
and 18 months) were analysed using univariable and multivariable
the roles of mode of delivery and perineal trauma in contributing
logistic regression.
to postpartum maternal morbidities, and ways to prevent
Main outcome measure Study-designed self-report measure of postpartum dyspareunia where possible, are warranted.
dyspareunia at 18 months postpartum.
Keywords Cohort studies, delivery obstetric, dyspareunia, pain,
Results In all, 1244/1507 (83%) women completed the baseline perineum, postpartum period, prospective studies, sexual intercourse.
and all four postpartum questionnaires; 1211/1237 (98%) had
Linked article This article is commented on by C Sakala, p. 680 in
resumed vaginal intercourse by 18 months postpartum, with 289/
this issue. To view this mini commentary visit http://dx.doi.org/
1211 (24%) women reporting dyspareunia. Compared with
10.1111/1471-0528.13264.
women who had a spontaneous vaginal delivery with an intact
Please cite this paper as: McDonald EA, Gartland D, Small R, Brown SJ. Dyspareunia and childbirth: a prospective cohort study. BJOG 2015;122:672–679.
nulliparous pregnancy cohort study.8 The primary objective
Introduction
of this paper was to investigate the contribution of obstet-
The relationship between obstetric risk factors including ric risk factors, including mode of delivery and perineal
mode of delivery and perineal trauma and dyspareunia is trauma, to postpartum dyspareunia. In addition, we aimed
not well characterised or understood.1–7 Previous studies to assess the influence of potential confounders, including
have suffered from several methodological limitations breastfeeding, maternal fatigue, maternal depression and
including cross-sectional study design,1–3,5,6 limited power intimate partner abuse.
to assess associations with obstetric risk factors1–7 and lack
of long-term follow up.1–7 Inferences drawn from the exist-
Methods
ing literature are limited by the failure of the studies to
consider prepregnancy dyspareunia2–7 and a range of post- Sample and participants
partum factors, such as breastfeeding and intimate partner Details regarding study eligibility and exclusion criteria and
abuse, that may confound associations.2–6 recruitment methods are available in a published study pro-
This study draws on data collected in the Maternal tocol.8 Briefly, women were recruited to the study between
Health Study, an Australian multicentre, prospective April 2003 and December 2005 from six metropolitan public
672 ª 2015 Royal College of Obstetricians and Gynaecologists
Dyspareunia and childbirth
maternity hospitals in Melbourne, Australia. We recruited proportions of women reporting symptoms divided by the
nulliparous women, aged over 18 years, in the first and total number of women who had resumed vaginal sex and
second trimesters of pregnancy. Women with poor Eng- had data available for the relevant period. Pain on first vag-
lish language literacy were excluded. inal sex is reported separately.
Risk factors for postpartum dyspareunia were investi-
Measures and definitions gated using univariable and multivariable logistic regres-
At recruitment, participants were asked to complete a sion. Logistic regression modelling was used to examine the
baseline questionnaire recording demographic and social association between mode of delivery and perineal trauma
characteristics, including age, country of birth and socio- (exposures of main interest) and dyspareunia at 18 months
economic status, and baseline measures of common maternal postpartum (primary outcome), taking into account poten-
morbidities, including dyspareunia before and during preg- tial confounders. Maternal age was included in modelling
nancy.1 Follow-up questionnaires were administered at 3, 6, analyses for a priori reasons. Other variables were included
12 and 18 months postpartum. Data regarding the mode of based on associations that were observed in univariable
delivery and degree of perineal trauma were collected in the analyses at 6 and/or 18 months postpartum. Data are pre-
3-month postpartum questionnaire and abstracted from sented as crude or adjusted odds ratios (ORs) with 95%
medical records for a subset of women. There was a high confidence intervals (95% CI).
degree of congruity between women’s own accounts of mode Ethical approval for the study was provided by La Trobe
of delivery and other obstetric events and data abstracted University (2002/38); Royal Children’s Hospital, Melbourne
from medical records.9,10 (27056A); Royal Women’s Hospital, Melbourne (2002/23);
Follow-up questionnaires included study-designed ques- Southern Health, Melbourne (2002-099B); and Angliss
tions regarding sexual health and dyspareunia drawing on Hospital, Melbourne (2002).
questions included in the Australian Longitudinal Women’s
Health Study11 and a study by Barrett et al.1 assessing
Results
women’s health after childbirth. Study questionnaires also
included validated measures of maternal depressive symp- Participants
toms (Edinburgh Postnatal Depression Scale)12 and inti- A total of 1507 women enrolled in the study. The mean
mate partner abuse (Composite Abuse Scale),13,14 and gestation of study participants at the time of enrolment
single item measures assessing maternal fatigue15 and infant was 15.0 weeks (range 6–24 weeks). We were unable to
feeding.16 Pretesting of the questionnaires, paying particu- determine a precise response fraction, but conservatively
lar attention to study-designed questions, was undertaken estimate that the response was between 1507/5400 (28%)
with a pilot sample of women recruited through participat- and 1507/4800 (31%). The follow-up response fractions
ing hospitals. The baseline Maternal Health Study ques- were 1431/1507 (95%), 1400/1507 (93%), 1387/1507
tionnaire is available on the study website.17 Postnatal (92%), 1326/1507 (88%) at 3, 6, 12 and 18 months post-
questionnaires can be made available by contacting the partum, respectively. In all, 1211/1239 (98%) participants
authors. were sexually active at 18 months postpartum.
Study participants were representative in relation to
Statistical analysis obstetric characteristics including mode of delivery and
Data were analysed using STATA version 13 (StataCorp., perineal trauma (see Table 1). Women born overseas in
College Station, TX, USA).18 Sample representativeness was countries where English is not the first language, and youn-
assessed by comparing data on social and obstetric charac- ger women were under-represented. Further information
teristics of participants with routinely collected perinatal regarding sociodemographic and reproductive characteris-
data for nulliparous women giving birth in the study per- tics of the sample and representativeness of study partici-
iod at the six participating hospitals, and at all public pants is available in previous papers.10,19 The 1244/1507
maternity hospitals in Victoria. (83%) women who completed all four follow-up question-
Analyses presented in the paper are restricted to women naires comprise the sample for the analyses in this paper
who completed the baseline questionnaire and all follow-up (Figure 1).
questionnaires. The proportions of women resuming vagi-
nal sex by 3, 6 and 12 months postpartum were calculated Birth outcomes
based on the proportion of women reporting resumption A total of 609/1244 (49.0%) women had a spontaneous
of sex divided by the total number of women with valid vaginal birth, two-thirds of whom (411/609, 67.5%) sus-
responses at each time point. tained a sutured tear and/or episiotomy; 134/1244 (10.8%)
The period prevalence of dyspareunia at 6 and had an operative vaginal birth assisted by vacuum extrac-
18 months postpartum was calculated based on the tion and 133/1244 (10.7%) gave birth assisted by forceps.
ª 2015 Royal College of Obstetricians and Gynaecologists 673
McDonald et al.
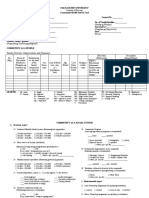
Table 1. Social characteristics of participants in the Maternal Health Study compared with Victorian Perinatal Data Collection Unit data
Maternal Health Nulliparous women Nulliparous women
Study participants ≥18 years giving ≥18 years giving
(n = 1507) birth in Victorian birth in the six
public hospitals participating
1/7/03 to 31/12/05 Victorian hospitals
(n = 40 905) 1/7/03 to 31/12/05
(n = 13 803)
n % n % n %
Maternal age at birth of first child
18–24 years 212 14.1 12 216 29.8 3813 27.6
25–29 years 437 29.0 13 802 33.7 4645 33.7
30–34 years 580 38.4 10 740 26.3 3769 27.3
35–39 years 236 15.7 3552 8.7 1319 9.6
≥40 years 42 2.8 595 1.5 257 1.9
Relationship status*
Married 914 60.7 22 790 56.0 8300 60.3
Unmarried 593 39.3 17 932 44.0 5469 39.7
Country of birth*
Australia 1115 74.4 29 791 73.3 8603 62.5
Overseas—English speaking 141 9.4 2109 5.2 905 6.6
Overseas—non-English speaking background 243 16.2 8738 21.5 4267 30.9
Mode of delivery*
Caesarean—no labour 140 9.8 3750 9.2 1237 9.0
Caesarean—laboured 292 20.4 7665 18.7 2587 18.7
Spontaneous vaginal birth 695 48.6 20 785 50.8 7000 50.7
Vaginal breech birth 5 0.3 182 0.4 95 0.7
Vaginal with forceps 150 10.5 3915 9.6 1426 10.3
Vaginal with vacuum extraction 149 10.4 4603 11.3 1457 10.6
Perineal trauma**
Intact perineum 595 41.7 19 805 48.4 6296 45.6
Unsutured laceration 72 5.0 n/a n/a n/a n/a
Sutured laceration 439 30.8 11 074 27.1 4221 30.6
Episiotomy 228 16.0 9068 22.2 3089 22.4
Episiotomy and tear 93 6.5 958 2.3 197 1.4
*Denominators vary due to missing values.
**Data collected by the Perinatal Data Collection Unit on perineal trauma does not include information regarding unsutured lacerations or
nonperineal lacerations, e.g. vaginal wall tears.
The majority of these women sustained a sutured tear and/ (44.7%) women at 3 months postpartum, 496/1144
or episiotomy (124/134, 92.5% and 129/133, 97.0%, respec- (43.4%) women at 6 months postpartum, 333/1184
tively). In all, 120/1244 (9.7%) were delivered by elective (28.1%) women at 12 months postpartum and 289/1236
caesarean section and 248/1244 (19.9%) were delivered by (23.4%) women at 18 months postpartum. Of the 496
emergency caesarean section. women who reported dyspareunia at 6 months postpartum,
one-third (162/496, 32.7%) reported persisting dyspareunia
Dyspareunia following childbirth at 18 months postpartum. In all, 338/1234 (27.4%) women
By 3 months postpartum, 970/1239 (78.3%) had resumed reported dyspareunia in the year prior to the index preg-
vaginal intercourse; 1165/1239 (94.0%) by 6 months post- nancy.
partum, 1202/1239 (97.0%) by 12 months postpartum and
1211/1239 (97.7%) by 18 months postpartum. Most of the Associations with dyspareunia
women who had resumed sex by 12 months postpartum The unadjusted odds of dyspareunia at 18 months postpar-
experienced pain during first vaginal sex after childbirth tum were higher in women who gave birth by vacuum
(961/1122, 85.7%). Dyspareunia was reported by 431/964 extraction (OR 2.01, 95% CI 1.2–3.5; P = 0.013),
674 ª 2015 Royal College of Obstetricians and Gynaecologists
Dyspareunia and childbirth
Q1: 1507 eligible participants
13 Withdrew
Q2: 1494 participants
1431 completed (95.0% of 1507 participants)
5 Withdrew
3 lost to follow up
Q3: 1486 participants
1400 completed (92.9% of 1507 participants)
16 Withdrew
6 lost to follow up
Q4: 1464 participants
1357 completed (90.0% of 1507 participants)
6 Withdrew
6 lost to follow up
Q5: 1452 participants
1327 completed (88.1% of 1507 participants)
Figure 1. Maternal Health Study participation flowchart to 18 months postpartum.
emergency caesarean section (OR 2.04, 95% CI 1.3–3.3; other variables in the model. Elective caesarean section was
P = 0.004) or elective caesarean section (OR 1.65, 95% CI also associated with increased odds of dyspareunia at
0.9–2.9; P = 0.090) compared with women who had a 18 months postpartum, although the confidence interval
spontaneous vaginal birth with an intact perineum. Youn- suggests borderline statistical significance.
ger women (OR 1.58, 95% CI 1.0–2.5; P = 0.057), women Similar patterns of association were found between
who experienced dyspareunia before the index pregnancy dyspareunia at 6 months postpartum, mode of delivery,
(OR 2.18, 95% CI 1.6–2.9; P = 0.000), women who perineal trauma and other maternal and postnatal factors
reported intimate partner abuse from birth to 12 months (Table 3). Women who had an operative vaginal delivery
postpartum (OR 1.84, 95% CI 1.3–2.6; P = 0.001), women (with forceps or vacuum extraction) had greater than a
who reported fatigue at 18 months postpartum (OR 1.65, three-fold increase in adjusted odds of dyspareunia at
95% CI 1.2–2.3; P = 0.002) and women who reported 6 months postpartum. Emergency caesarean section and
depressive symptoms at 18 months postpartum (OR 1.97, vaginal birth with a sutured tear and/or episiotomy were
95% CI 1.3–3.0; P = 0.002) also had increased odds of associated with a two-fold increase in odds of dyspareunia
reporting dyspareunia at 18 months postpartum. after taking into account other factors in the model.
To obtain more precise estimates of the association Women who had an elective caesarean section did not
between mode of delivery and dyspareunia at 18 months have raised odds of reporting dyspareunia at 6 months
postpartum, we developed a multivariable logistic regres- postpartum. Prepregnancy dyspareunia was associated with
sion model (Table 2). A composite variable combining data a two-fold increase in odds of dyspareunia at both 6 and
on mode of delivery and perineal trauma was the exposure 18 months postpartum. Observed associations with obstet-
of main interest. Maternal age was included in the model ric intervention in multivariable models were stronger
for a priori reasons based on previous research showing than associations with postnatal factors, including mater-
that younger women are more likely to experience dyspa- nal depressive symptoms, fatigue and intimate partner
reunia.20,21 Dyspareunia before pregnancy, maternal depres- abuse.
sion, maternal fatigue and intimate partner abuse were
included because of the significant associations with dyspa-
Discussion
reunia at 6 and/or 18 months postpartum noted in univari-
able analyses. Main findings
Women who gave birth by emergency caesarean section Almost all women experience some pain during sexual
or vacuum extraction and those who reported prepregnan- intercourse following childbirth. Our findings show that
cy dyspareunia had greater than a twofold increase in the extent to which women report dyspareunia at 6 and
adjusted odds of persisting dyspareunia at 18 months post- 18 months postpartum is influenced by events during
partum compared with women who had a spontaneous labour and birth. The odds of dyspareunia at 18 months
vaginal birth with an intact perineum after adjusting for were substantially higher in women who delivered by
ª 2015 Royal College of Obstetricians and Gynaecologists 675
McDonald et al.
Table 2. Adjusted odds of dyspareunia at 18 months postpartum associated with mode of delivery, perineal trauma and other risk factors*
Dyspareunia at 18 months Adjusted OR (95% CI) P values
postpartum
No Yes
n (%) n (%)
Mode of delivery and perineal trauma
Spontaneous vaginal birth
Intact perineum/unsutured tear 153 (83.2) 31 (16.8) 1.0 ref
Sutured tear/episiotomy 307 (80.2) 76 (19.8) 1.37 (0.8–2.2) 0.201
Caesarean section (intact perineum)
Elective 84 (75.0) 28 (25.0) 1.71 (0.9–3.2) 0.087
Emergency 157 (70.7) 65 (29.3) 2.41 (1.4–4.0) 0.001
Forceps (sutured tear/episiotomy) 95 (79.8) 24 (20.2) 1.56 (0.8–2.9) 0.156
Vacuum extraction (sutured tear/episiotomy) 86 (71.1) 35 (28.9) 2.28 (1.3–4.1) 0.005
Prepregnancy dyspareunia
No 679 (81.5) 154 (18.5) 1.0 ref
Yes 210 (66.9) 104 (33.1) 2.09 (1.5–2.8) 0.000
Maternal age at index birth
30–34 years 254 (78.9) 68 (21.1) 1.0 ref
18–24 years 85 (70.3) 36 (29.7) 1.45 (0.9–2.4) 0.165
25–29 years 366 (76.1) 115 (23.9) 1.10 (0.8–1.6) 0.602
35+ years 189 (81.8) 42 (18.2) 0.77 (0.5–1.2) 0.263
Highest educational qualification
University degree 436 (77.0) 130 (23.0) 1.0 ref
Certificate/diploma 226 (76.4) 70 (23.6) 0.91 (0.6–1.3) 0.620
Year 12 165 (81.3) 38 (18.7) 0.69 (0.4–1.1) 0.091
<Year 12 62 (73.8) 22 (26.2) 1.02 (0.6–1.8) 0.938
Maternal fatigue at 18 months postpartum
No 297 (83.0) 61 (17.0) 1.0 ref
Yes 592 (74.8) 200 (25.2) 1.51 (1.1–2.1) 0.018
EPDS ≥13 at 18 months postpartum
No 824 (78.8) 222 (21.2) 1.0 ref
Yes 68 (65.4) 36 (34.6) 1.27 (0.8–2.0) 0.318
Intimate partner abuse in first 12 months postpartum
No 766 (79.3) 200 (20.7) 1.0 ref
Yes 125 (67.6) 60 (32.4) 1.65 (1.1–2.4) 0.009
EPDS, Edinburgh Postnatal Depression Scale.
*Excludes women who report giving birth to second baby by 18 months postpartum and denominators vary due to missing values.
emergency caesarean section or vacuum extraction, and women reporting dyspareunia at 18 months postpartum is
somewhat higher for women who had an elective caesarean similar for women who had a spontaneous vaginal birth
section, compared with women who had a spontaneous with and without perineal damage.
vaginal birth with an intact perineum. At 6 months post- Other factors associated with dyspareunia at 18 months
partum, vaginal birth assisted with forceps was also associ- postpartum include prepregnancy dyspareunia, intimate
ated with dyspareunia, but elective caesarean section was partner abuse and maternal fatigue. These results suggest
not. These differences in the pattern of association with that clinicians should be alert to the possibility that inti-
mode of delivery may reflect limited study power for com- mate partner abuse is a potential underlying factor in per-
parisons of these subgroups. Alternatively, it is possible that sisting dyspareunia.
women recover more quickly from forceps than from vac- The finding that breastfeeding is associated with dyspa-
uum extraction, and that women having an elective caesar- reunia in the early postnatal period confirms previous
ean section that do experience postpartum dyspareunia are study findings.1 Women still breastfeeding at 6 months
slow to recover. It is noteworthy that the proportion of postpartum had a higher likelihood of experiencing
676 ª 2015 Royal College of Obstetricians and Gynaecologists
Dyspareunia and childbirth
Table 3. Adjusted odds of dyspareunia at 6 months postpartum associated with mode of delivery, perineal trauma and other risk factors*
Dyspareunia at 6 months Adjusted OR (95% CI) P values
postpartum
No Yes
Mode of delivery and perineal trauma
Spontaneous vaginal birth
Intact perineum/unsutured tear 130 (68.8) 59 (31.2) 1.0 ref
Sutured tear/episiotomy 201 (53.6) 174 (46.4) 2.32 (1.5–3.5) 0.000
Caesarean section (intact perineum)
Elective 72 (68.6) 33 (31.4) 0.76 (0.4–1.4) 0.387
Emergency 133 (59.4) 91 (40.6) 1.83 (1.2–2.9) 0.010
Forceps (sutured tear/episiotomy) 59 (48.0) 64 (52.0) 3.11 (1.9–5.2) 0.000
Vacuum extraction (sutured tear/episiotomy) 45 (40.5) 66 (59.5) 3.36 (2.0–5.8) 0.000
Prepregnancy dyspareunia
No 503 (60.8) 325 (39.2) 1.0 ref
Yes 140 (45.8) 166 (54.2) 1.91 (1.4–2.6) 0.000
Maternal age at index birth
30–34 years 203 (60.1) 135 (39.9) 1.0 ref
18–24 years 77 (59.2) 53 (40.8) 1.39 (0.9–2.3) 0.181
25–29 years 249 (53.4) 217 (46.6) 1.30 (0.9–1.8) 0.118
35+ years 119 (56.7) 91 (43.3) 1.25 (0.8–1.9) 0.293
Highest educational qualification
University degree 293 (53.5) 255 (46.5) 1.0 ref
Certificate/diploma 168 (56.2) 131 (43.8) 1.03 (0.7–1.4) 0.882
Year 12 122 (61.0) 78 (39.0) 0.81 (0.6–1.2) 0.286
<Year 12 62 (68.9) 28 (31.1) 0.61 (0.3–1.1) 0.102
Breastfeeding at 6 months postpartum
No 183 (62.0) 112 (38.0) 1.0 ref
Yes 373 (52.5) 337 (47.5) 1.55 (1.1–2.1) 0.007
Maternal fatigue at 6 months postpartum
No 283 (60.1) 188 (39.9) 1.0 ref
Yes 363 (54.4) 304 (45.6) 1.28 (1.0–1.7) 0.081
EPDS ≥13 at 6 months postpartum
No 598 (57.3) 445 (42.7) 1.0 ref
Yes 47 (48.5) 50 (51.5) 1.62 (1.0–2.7) 0.060
Intimate partner abuse in first 12 months postpartum
No 552 (57.1) 414 (42.9) 1.0 ref
Yes 94 (53.4) 82 (46.6) 1.26 (0.9–1.8) 0.237
EPDS, Edinburgh Postnatal Depression Scale.
*Denominators vary due to missing values.
dyspareunia at 6 months postpartum, even after adjusting on subsequent sex. Importantly for the analyses presented
for other maternal factors including mode of delivery and in this paper, the sample was representative in relation to
perineal trauma. mode of delivery.
The recruitment method did result in under-representa-
Strengths and limitations tion of younger women and women born overseas with a
Major strengths of this study are recruitment of a nullipa- non-English-speaking background. However, this is unlikely
rous pregnancy cohort in early pregnancy, frequent follow to have biased the results, as these social characteristics
up and high retention of participants to 18 months post- were unrelated to the primary outcomes reported in the
partum. All of these key features of the design of the study paper. The fact that recruitment was restricted to nullipa-
reduce the likelihood of recall bias, which is a major con- rous women, while very valuable in providing rich detail
cern in much of the previous literature. Additionally, the about the experiences of women having their first baby,
study was designed to facilitate ascertainment and differen- means that we are unable to comment on outcomes follow-
tiation of pain on first vaginal sex after childbirth and pain ing second and subsequent births.
ª 2015 Royal College of Obstetricians and Gynaecologists 677
McDonald et al.
Interpretation paper for publication. EM and DG were responsible for
The major contribution of this study is that it provides data management.
much more robust evidence than previously available about
the extent and persistence of postpartum dyspareunia, and Funding
associations with mode of delivery and perineal trauma. This research was supported by project grants from the
No other study has undertaken such detailed, frequent and Australian National Health and Medical Research Council
long-term follow up with a sufficiently large nulliparous (ID191222 and ID433006 Melbourne, Australia); a Vic-
cohort recruited in early pregnancy to assess associations Health Public Health Research Fellowship (2002–2006), a
with obstetric risk factors. National Health and Medical Research Council Career
The higher prevalence of persisting dyspareunia in Development Fellowship (ID491205, 2008–2011) and an
women who had an operative birth raises important ques- ARC Future Fellowship (2012–2015) awarded to SB; a La
tions about the longer-term impact of operative procedures Trobe University Postgraduate Scholarship awarded to EM,
on women’s health. Although in a study of this nature we and the Victorian Government’s Operational Infrastructure
cannot be confident in drawing causal inferences, the find- Support Programme.
ings raise important questions about the extent to which
obstetric procedures have long-term consequences for Acknowledgements
women’s health and wellbeing, and whether any of this We are grateful to members of the Maternal Health Study
morbidity could be prevented. It is striking that so few research team who have contributed to data collection and
prospective studies have collected data on the persistence coding (Maggie Flood, Ann Krastev, Renee Paxton, Susan
of dyspareunia beyond 6 months postpartum. The study Perlen, Martine Spaull, Hannah Woolhouse). &
findings highlight the importance of continuing efforts to
improve understanding of postpartum maternal morbidi-
References
ties, including factors that influence severity and persistence
of symptoms. The fact that dyspareunia persists for a sub- 1 Barrett G, Pendry E, Peacock J, Victor C, Thakar R, Manyonda I.
Women’s sexual health after childbirth. BJOG 2000;107:186–95.
stantial proportion of women also points to the need for
2 Brubaker L, Handa VL, Bradley CS, Connolly A, Moalli P, Brown MB,
focusing clinical attention on ways to help women experi- et al. Sexual function 6 months after first delivery. Obstet Gynecol
encing ongoing morbidity, and increased efforts to prevent 2008;111:1040–4.
postpartum morbidity whenever possible. 3 Buhling KJ, Schmidt S, Robinson JN, Klapp C, Siebert G,
Dudenhausen JW. Rate of dyspareunia after delivery in primiparae
according to mode of delivery. Eur J Obstet Gynecol Reprod Biol
Conclusions 2006;124:42–6.
4 Gjerdingen DK, Froberg DG, Chaloner KM, McGovern PM. Changes
The findings of this multicentre prospective cohort of nul- in women’s physical health during the first postpartum year. Arch
liparous women suggest that obstetric intervention—specif- Fam Med 1993;2:277–83.
ically vacuum extraction and caesarean section—contribute 5 Klein MC, Gauthier RJ, Robbins JM, Kaczorowski J, Jorgensen SH,
Franco ED, et al. Relationship of episiotomy to perineal trauma and
to persisting dyspareunia affecting a significant proportion
morbidity, sexual dysfunction, and pelvic floor relaxation. Am J
of women up to 18 months postpartum. Greater recogni- Obstet Gynecol 1994;171:591–8.
tion and better overall understanding of the role of obstet- 6 Signorello LB, Harlow BL, Chekos AK, Repke JT. Postpartum sexual
ric intervention in contributing to maternal postpartum functioning and its relationship to perineal trauma: a retrospective
morbidities, and ways to prevent postpartum dyspareunia cohort study of primiparous women. Am J Obstet Gynecol
2001;184:881–90.
where possible, are warranted.
7 Safarinejad MR, Kolahi AA, Hosseini L. The effect of the mode of
delivery on the quality of life, sexual function, and sexual
Disclosure of interests satisfaction in primiparous women and their husbands. J Sex Med
None disclosed. 2009;6:1645–67.
8 Brown S, Lumley J, McDonald E, Krastev A. Maternal Health Study:
a prospective cohort study of nulliparous women recruited in early
Contribution to authorship pregnancy. BMC Pregnancy Childbirth 2006;6:12.
EM planned and conducted the analyses and wrote the 9 Gartland D, Lansakara N, Flood M, Brown S. Assessing obstetric risk
paper. SB wrote the study protocol, took primary responsi- factors for maternal morbidity: congruity between medical records
bility for the design and conduct of the study, contributed and mothers’ reports of obstetric exposures. Am J Obstet Gynecol
2012;206:152.e1–e10.
to analysis and interpretation of data and contributed to
10 Brown S, Gartland D, Donath S, MacArthur C. Fecal incontinence
writing the paper. DG and RS contributed to interpretation during the first 12 months postpartum: complex causal pathways
of data and reviewed and commented on drafts of the and implications for clinical practice. Obstet Gynecol 2012;119:
paper. All authors have approved the final draft of the 1–10.
678 ª 2015 Royal College of Obstetricians and Gynaecologists
Dyspareunia and childbirth
11 Brown WJ, Bryson L, Byles JE, Dobson AJ, Lee C, Mishra G, et al. 17 Brown SB. Maternal Health Study. 2014 [www.mcri.edu.au/media/
Women’s Health Australia: recruitment for a national longitudinal 987190/031570_pregnancy_v10_f_a_.pdf]. Accessed 17 December
cohort study. Women Health 1999;28:23–40. 2014.
12 Cox J. Perinatal Mental Health: A Guide to the Edinburgh Postnatal 18 StataCorp. Stata Statistical Software: Release 13. College Station,
Depression Scale (EPDS). London: Gaskell, 2003. TX: StataCorp LP, 2013.
13 Hegarty K, Bush R, Sheehan M. The composite abuse scale: further 19 Brown S, Donath S, MacArthur C, McDonald E, Krastev A. Urinary
development and assessment of reliability and validity of a incontinence in nulliparous women before and during pregnancy:
multidimensional partner abuse measure in clinical settings. Violence prevalence, incidence, and associated risk factors. Int Urogynecol J
Vict 2005;20:529–47. 2010;21:193–202.
14 Hegarty KL, Sheehan M, Schonfeld C. A multidimensional definition 20 Richters J, Grulich AE, de Visser RO, Smith AMA, Rissel C. Sex in
of partner abuse: development and preliminary validation of the Australia: sexual difficulties in a representative sample of adults [The
Composite Abuse Scale. J Fam Violence 1999;14:399–414. Australian Study of Health and Relationships, a survey of 19,307
15 Woolhouse H, Gartland D, Perlen S, Donath S, Brown SJ. Physical people aged 16–59 years which had a broad focus across many
health after childbirth and maternal depression in the first 12 aspects of sexual and reproductive health.]. Aust N Z J Public Health
months post partum: results of an Australian nulliparous pregnancy 2003;27:164–70.
cohort study. Midwifery 2014;30:378–84. 21 Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United
16 McDonald E, Brown S. Does method of birth make a difference to States: prevalence and predictors. JAMA 1999;281:537–44.
when women resume sex after childbirth? BJOG 2013;120:823–30.
ª 2015 Royal College of Obstetricians and Gynaecologists 679
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Chapter 35 - Her Triplet Alphas - Novel SquareDokument5 SeitenChapter 35 - Her Triplet Alphas - Novel SquareeiseNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Family Structure, Characteristics and DynamicsDokument6 SeitenFamily Structure, Characteristics and DynamicsErilyn Leigh ManaloNoch keine Bewertungen
- (GYNE) 3.05 Gestational Trophoblastic Disease - Co-HidalgoDokument7 Seiten(GYNE) 3.05 Gestational Trophoblastic Disease - Co-HidalgoMeg MisaNoch keine Bewertungen
- DR Template - BeghDokument2 SeitenDR Template - BeghJayran Bay-an100% (1)
- Children and Adolescents of Lesbian and Gay ParentsDokument5 SeitenChildren and Adolescents of Lesbian and Gay ParentsshyznogudNoch keine Bewertungen
- Contraceptive SuppositoryDokument3 SeitenContraceptive SuppositoryMonica GereroNoch keine Bewertungen
- (#5) Benign and Malignant Ovariaan TumorsDokument35 Seiten(#5) Benign and Malignant Ovariaan Tumorsmarina_shawkyNoch keine Bewertungen
- Nutritional Strategies For Optimizing Reproductive Performance of SowDokument18 SeitenNutritional Strategies For Optimizing Reproductive Performance of Sowanon_151103933Noch keine Bewertungen
- BrochureDokument3 SeitenBrochureapi-218300213Noch keine Bewertungen
- The Controversy Over Stem Cell ResearchDokument4 SeitenThe Controversy Over Stem Cell ResearchGra BohórquezNoch keine Bewertungen
- Chapter 2 Lesson 1Dokument3 SeitenChapter 2 Lesson 1John Carldel VivoNoch keine Bewertungen
- Bsc1102 Lab Power PointDokument26 SeitenBsc1102 Lab Power PointKris StephensNoch keine Bewertungen
- CV European English Fabiana Interlandi 7Dokument3 SeitenCV European English Fabiana Interlandi 7Andrea VetranoNoch keine Bewertungen
- 2 Tumor Genital WanitaDokument115 Seiten2 Tumor Genital WanitaKhafidz Asy'ariNoch keine Bewertungen
- b1 ChecklistDokument2 Seitenb1 ChecklistRoryNoch keine Bewertungen
- Practice Bulletin: Vaginal Birth After Previous Cesarean DeliveryDokument14 SeitenPractice Bulletin: Vaginal Birth After Previous Cesarean DeliveryFernando González PeruggiNoch keine Bewertungen
- Sci5 q2 Mod1 Human Reproductive System Loida Pineda Revised Bgo v1Dokument20 SeitenSci5 q2 Mod1 Human Reproductive System Loida Pineda Revised Bgo v1Louie Raff Michael EstradaNoch keine Bewertungen
- Pollination and Its AgentsDokument6 SeitenPollination and Its AgentsdebbyhooiNoch keine Bewertungen
- Definition: Bilateral Tubal Ligation (BTL)Dokument5 SeitenDefinition: Bilateral Tubal Ligation (BTL)Reginald UyNoch keine Bewertungen
- Babson and Benda's ChartDokument10 SeitenBabson and Benda's ChartZasly WookNoch keine Bewertungen
- SampleDokument255 SeitenSampleshivaNoch keine Bewertungen
- SemenDokument6 SeitenSemenMarkNoch keine Bewertungen
- Ethical Issues IVFDokument1 SeiteEthical Issues IVFBasinga OkinamNoch keine Bewertungen
- Family Planning Service Record (Form 1)Dokument32 SeitenFamily Planning Service Record (Form 1)Kareen Xc Mae BerdosNoch keine Bewertungen
- Hormones FTMDokument16 SeitenHormones FTMapi-221867127Noch keine Bewertungen
- SDKI 2002 - Kuesioner PriaDokument19 SeitenSDKI 2002 - Kuesioner Priakiki rizkiNoch keine Bewertungen
- Communities WorksheetDokument2 SeitenCommunities WorksheetJamie MakrisNoch keine Bewertungen
- Uso Medicinal de Cordia LuteaDokument12 SeitenUso Medicinal de Cordia LuteaBelen GonzalezNoch keine Bewertungen
- Barr Body and HermaphroditismDokument41 SeitenBarr Body and HermaphroditismTamjid KhanNoch keine Bewertungen
- ALE 2014 Animal Science Autosaved - Docx 2003409664Dokument85 SeitenALE 2014 Animal Science Autosaved - Docx 2003409664Haifa KalantunganNoch keine Bewertungen