Beruflich Dokumente
Kultur Dokumente
CD Malaria Latest
Hochgeladen von
Miguel Cuevas DolotOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
CD Malaria Latest
Hochgeladen von
Miguel Cuevas DolotCopyright:
Verfügbare Formate
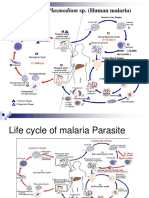
COMMUNICABLE DISEASES
Topic: MALARIA
Lecturer: Dr. Edwin Fortuno
MED BLOCK 1ST Sem – OLFU-COM Batch 2020
MALARIA
Malaria is a mosquito-borne infectious disease caused by a
eukaryotic protist of the genus Plasmodium.
MAL (BAD) + ARIA (AIR) = MALARIA (BAD AIR)
This “bad air” was believed to be the cause of the fever that
often developed in those who spent time around the swamps.
In fact, the illness, now known as malaria, was due to certain OVERVIEW OF MALARIA
protozoon present in the mosquitoes that bred around these • Most important parasitic disease in humans globally.
swamps, and which caused recurring feverish symptoms in • Causes a heavy burden among tropical countries.
those they bit. • Poses a threat to non – endemic countries.
• Poses a danger to international and local travelers
MALARIA
- disease caused by protozoan parasite called Plasmodium.
- It is usually transmitted through the bite of an infected female
Anopheles mosquito.
- Malaria may also be transmitted through the following:
• Transfusing blood that is positive for malaria
DISEASE OF THE TROPICS parasites
• Sharing of IV needles (especially among IV drug
users)
• Trans -placental (transfer of malaria parasites from
an infected mother to her unborn child)
A. Plasmodium falciparum (60-70%)
B. Plasmodium vivax (30-40%)
C. Plasmodium malariae
D. Plasmodium ovale
E. Plasmodium knowlesi affects H. sapiens and Macaca
fascicularis
MD2020 SECTION C – MED BLOCK 1OF7
Communicable Diseases: MALARIA
Characteristic P. falciparum P. vivax P ovale P. malariae
Duration of 5.5 8 9 15
intra – hepatic
phase
Number of 30,000 10,000 15,000 15,000
merozoites
released per
infected
erythrocyte
Duration of 48 48 50 72
erythroctic
cycle in hours
RBC Young but Reticulocytes Reticulocytes Older cells
preference can invade all and cells up
cell ages to 2 weeks
old
Morphology Ring forms, Irregular Infected Bands or
banana shaped large eryhrocytes, rectangular
shaped rings and enlarged and forms of
gametocytes trophozoites, oval with trophozoites
enlarged tufted ends,
Plasmodium knowlesi RBC, schuffer’s
schuffer’s dots
Molecular, entomological, and epidemiological data indicate dots
that human infections with P. knowlesi are not newly Pigment color Black Yellow brown Dark brown Brown black
Ability to NO YES YES NO
emergent cause relapse
Primarily a zoonotic form.
Potentially fatal, but if detected early enough, infections in A. Plasmodium falciparum 12 Days
humans are readily treatable. B. Plasmodium vivax 14 Days
C. Plasmodium malariae 30 Days
Plasmodium knowlesi D. Plasmodium ovale 14 Days
• Reports of its emergence from monkeys
• Isolated from Philippine macaques (Macaca fascicularis) in
1961
• Incriminated vector in Anopheles balabacensis
• Published reports of human infection
- 1965, 2004 Malaysia
- 2008 (Palawan) Phils : (2 cases)
- 2004 Thailand
- 2006 China
Presentation:
• Morphologically similar to P. malariae may be mistaken to be Parts of a mosquito:
P. falciparum because of abundant ring stages
• In Rhesus monkey studies
• High parasite densities is possible
• No significant sequestration in microcirculation
• In humans
Reported in children and relatively older adults
May present as mild form of malaria easily responding to
chloroquine but may also be severe and fatal
Fever, headaches, intermittent chills, abdominal pain,
sweating and malaise
Polymerase chain reaction is of value for diagnosis because
P. knowlesi infection is easily misdiagnosed as less
dangerous Plasmodium malariae infection with conventional
microscopy.
Do all mosquitoes carry the malaria parasite?
• No, not all mosquitoes carry the malaria parasite.
What are the common species of malaria parasites in the
• In the country, it is the adult female Anopheles mosquito that
Philippines?
can become infective and therefore carries the malaria
• Plasmodium falciparum and Plasmodium vivax are the
parasite after she bites a person infected with malaria.
common species of malaria parasites in the Philippines
• This anopheles mosquito bites from dusk to dawn and it
where 70% of malaria cases are P. falciparum while 29% are
breeds in clear, slow flowing streams that are found in
P. vivax.
mountainous/forested areas or in brackish water where salt
• There are also P. malariae cases but contributes to about <
and fresh water meet. This is usually found in coastal areas
1% of the total malaria cases.
MD2020 SECTION C – MED BLOCK 2OF7
Communicable Diseases: MALARIA
Can a person get malaria by drinking water in the streams with STATISTICS
mosquito eggs? THINK….. • P. falciparum and P. vivax – responsible for most new
infections.
VECTORS IN THE PHILIPPINES • No. The malaria parasite has to undergo development inside
• Anopheles sp. the adult female mosquito; therefore one cannot get malaria
o An. flavirostris from drinking water that has mosquito eggs in it.
o An. litoralis
o An. maculatus P. falciparum
o An. mangyanus • Causes severe malaria.
o An babacensis • Creates a high level of parasitemia and sequestration
causing end organ damage.
Who are at risk OF getting malaria? • Sequestration is a specific property.
• Children • Usually seen in the smears are younger forms before
• Pregnant women sequestration takes place.
• Indigenous peoples
• Forest workers, miners, soldiers RBC CHANGES
• Persons who are not from a malaria endemic area but travel • Once inside the cell, it consumes and degrades intracellular
to this area. proteins (hemoglobin).
• Alteration in RBC properties more irregular in shape and less
deformable.
• P. falciparum – causes appearances of knobs on the cell
surface.
– Mediates attachment to the capillary and venular
endothelium (cytoadherence).
• Rosette formation – infected RBCs may adhere to uninfected
RBC.
• Agglutination – infected RBCs adhere to other parasitized
RBCs.
SEQUESTRATION
• Contribute to mental changes and coma.
• End organs affected are:
– CNS, lungs and kidneys.
EPIDEMIOLOGY A combination of all these results in . . .
• Endemicity is defined as palpable spleen rates in children 2 – • Interference with microcirculatory circulation and metabolism
9 years old: especially in the brain
– < 10% - hypoendemic Other things noted in P. falciparum infection:
– 11-50% - mesoendemic • Hypoglycemia
– 51 – 75% - hyperendemic • Lactic acidosis
– > 75% - holoendemic • Severe anemia
• Africa and New Guinea • Multi - organ dysfunction secondary to hypoxia.
• Principal determinants are: • Usually occurs in travelers without immunity or young
– Biting habits children living in endemic areas.
– Density of the mosquito population
– Longevity of the anopheline mosquito INNATE IMMUNITY
• The lifecycle that takes place inside the • Depends on the host’s immunity.
mosquito is between 8 – 30 days. • P. falciparum usually results in death.
• Low temperatures are not conducive for PROTECTIVE GENETIC FACTORS
sporogony to take place. • Sickle cell disease
STABLE TRANSMISSION • Hemoglobinopathies
• Constant year round transmission. • Polymorphisms in the host’s Tumor Necrosis Factor (TNF).
• By adulthood would have achieved full immunity
CLINICAL MANIFESTATIONS
UNSTABLE TRANSMISSION
• Erratic transmission HISTORY
• Usually in hypoendemic areas • Most patients will present with fever and headache.
• Full protective immunity is not acquired • There is no neck stiffness or photophobia resembling
meningitis.
• Get a history of recent travel in those patients with high
grade fever.
• Malaria free areas:
MD2020 SECTION C – MED BLOCK 3OF7
Communicable Diseases: MALARIA
o Aklan, Albay, Batangas, Benguet, Biliran, Bohol, P. vivax and P. ovale
Camiguin, Capiz, Catandauanes, Cavite, Cebu, • Patient may relapse after long periods because of the
Eastern Samar, Guimaras, Ilo-Ilo, Leyte, hypnozoite stage in the liver.
Marinduque, Masbate, Northern Samar, Siquijor, • Can remain dormant for months to years before entering the
Sorsogon, Southern Leyte, Surigao del Norete, blood stream to produce symptoms.
Western Samar • Causes the benign form of tertian fever.
o Malaria areas in and near NCR: Fairview, Antipolo – (P. malariae causes the quartan fever.)
Malaria is a febrile illness characterized by fever and related PHYSICAL EXAMINATION
symptoms. • Most patients will have splenomegaly.
However, it is very important to remember that malaria is not a • Anemia
simple disease of fever, chills and rigors. • Thrombocytopenia
In fact, in a malaria prone area, it can present with such varied • MARF
and dramatic manifestations that malaria may have to be • Acute tubular necrosis secondary to hypovolemia,
considered as a differential diagnosis for almost all the ischemia, intravascular coagulation
clinical problems. • Parameters:
Malaria is a great imitator and trickster, particularly in areas • <1 ml/kg/hr.
where it is endemic. • Elevated creatinine
DIAGNOSTIC PROCEDURE
Since Charles Laveran first visualized the malaria parasite in blood in
1880, the main-stay of malaria diagnosis has been the microscopic
- rapidly rising fever with headache examination of blood.
- paroxysm with shaking chills
- profuse sweating Malarial Smear
- hepatosplenomegaly In this procedure, a film of blood is placed on a slide, stained, and
- myalgia (muscle pain) examined microscopically.
- orthostatic hypotension Peripheral smear examination for malarial parasite is the gold-
standard in confirming the diagnosis of malaria
• Severe anemia – usually associated with P. falciparum infections.
• May be secondary to RBC infection and a loss of infected RBC.
• Uninfected RBCs are inappropriately cleared and bone marrow
suppression may also be involved.
RENAL FAILURE
• Infected RBCs adhere to the microvasculature in the renal
cortex.
• Oliguric renal failure.
• Usually reversible.
• P. malariae can cause the nephrotic syndrome
RESPIRATORY SYMPTOMS
• Metabolic alkalosis and respiratory acidosis leading to
respiratory distress.
• Can develop pulmonary edema.
TYPICAL MANIFESTATIONS IN DIAGNOSING MALARIA
• Cerebral malaria – almost always due to P. falciparum
infections.
– Coma lasts more than 30 minutes.
MD2020 SECTION C – MED BLOCK 4OF7
Communicable Diseases: MALARIA
DEMONSTRATION OF THE PARASITE TREATMENT
• Must identify the asexual forms in the peripheral blood • 3 medical conditions associated with Plasmodium infection:
smear. – Uncomplicated
• Negative smears do not rule out malaria if there is a high – Treatment failure
degree of suspicion. Repeat. – Severe malaria
• Use the Giemsa stains at pH – 7.2
• Thick blood smear provides better sensitivity. UNCOMPLICATED MALARIA (falciparum, vivax)
• Thin blood smear provides better specificity and allows • Febrile
better identification of the species involved. • Parasites in blood
• Not so diagnostic in P. falciparum infections since • Absence of severe malaria and multi drug resistant P.
sequestration removes the RBCs out of the peripheral falciparum
circulation especially in the late stages. • Severe headache, chills
• Thick and thin smears done 12 – 24 hours apart at any time • Thrombocytopenia
of the infection.
•Day 0 – 2 Co Artem
THICK SMEARS • Given after high fat meals
• More sensitive than thin smears. • Contraindicated in pregnancy and lactation
• Can’t identify the species • Day 3 Primaquine
• Parasitemia can be calculated based on the number of » falciparum – gametocidal
infected RBC. » vivax – hypnozoiticidal
• Quantitative test. » Discharged if asexual forms are not seen in Day7
• Can concentrate the parasites increasing diagnostic then monitor once a week for a month.
sensitivity. Other Plasmodium parasites and mixed infections:
• P. malariae chloroquine; Primaquine
THIN SMEARS
• Less sensitive. Multi drug resistant P. falciparum and treatment failure
• Facilitate speciation • Ability of the parasite to survive and or multiply despite the
• Qualitative test administration and absorption of a drug given in the
recommended or higher dose but within the limits of
ALTERNATIVE TESTS tolerance of the patient.
• Quantitative buffy coat – as sensitive as a thick smear but • Basis:
must still do a thin smear. • Recrudescence of asexual parasitemia from 48
• (PfHRP2)Histidine rich protein - 2 ( the only approved rapid hours after treatment
test in the US. • No parasite clearance or reduction
Objectives:
Rapid Diagnostic Test (RDT) 1. cure the infection
This is a blood test for malaria. It can be conducted outside the 2. prevent the development of severe malaria
laboratory and inside the field. 3. prevent spread of drug resistant forms of the
It gives a result within 10 to 15 minutes. parasite
This is done to detect malarial parasite antigen in the blood.
SEVERE MALARIA
• Dysfunction of organ systems secondary to:
Effects of malaria toxins
Sequestration of infected RBC
Anemia
• Abnormal organ function tests
• Jaundice
• Hyperparasitemia (>2% parasitized RBC)
MALARIA SUSPECT • Severe anemia
• Patients with malaria like illness • Metabolic abnormalities
• With thrombocytopenia • Hemoglobinuria
• Relative lymphocytopenia
• Atypical lymphocytes Conditions:
• Elevated LDH • Seizures
• Impaired consciousness
OBJECTIVES FOR TREATMENT • Prostration/ weakness
• Treat the malaria • Poor urine output
• Prevent development and spread of anti malarial drug • Signs of pulmonary edema
resistance • Signs of DIC
• Abnormal spontaneous bleeding
MD2020 SECTION C – MED BLOCK 5OF7
Communicable Diseases: MALARIA
• US FDA and WHO: Artesunate IV BASIS FOR CHEMOPROPHYLAXIS
• DOH: may give Coartem • Each species has a specific incubation period.
– Quinine IV or artesunate IV plus treatment: • P. falciparum infection typically develops within a month of
• Quinine or artesunate + tetracycline + exposure. Rare cases have been reported up to a year
clindamycin later.
• Falciparum + either vivax or malariae • Hypnozoite form – P. vivax and P. ovale.
– CoArtem (falciparum) and Primaquine (vivax) – Parasite stays in the liver for months before
inducing initial infection.
P. vivax
• Day 0 – 2 chloroquine CHEMOPROPHYLAXIS
– No treatment failure reported yet • Doxycycline 100 mg daily for 2 – 3 days before going to an
• Days 3 – 17 primaquine endemic area, continue while in the endemic area and
continue for 4 more weeks after leaving the endemic area.
TREATMENT FAILURE
• Falciparum malaria - quinine and any of the three drugs: PERSONAL PROTECTION
doxycycline, tetracycline, clindamycin (QUININE • Reduce the frequency of mosquito bites.
PLUS) – Avoid the mosquito’s peak feeding hours.
• Vivax – CoArtem – DEET and picaridin
– If hypnozoites are suspected and fever recurs – Insecticide impregnated mosquito nets.
after 2 weeks primaquine
PREVENTION AND CONTROL
Treatment under special conditions: Malaria case should be reported.
• Pregnant women: A thorough screening of all infected person’s from
– Falciparum – oral quinine; Insulin secreting drug mosquitoes is important.
monitor blood sugar levels Mosquito breeding places must be destroyed.
– Vivax – chloroquine Homes should be sprayed with effective insecticides
which have residual actions on the wall.
QUININE Mosquito nets should be used especially when in infected
• No role in prophylaxis areas.
• Used with second agent in drug – resistant falciparum Insecticide Treated Bed Nets (ITN’s) have emerged as a
infections. very important tool in malaria control in endemic areas.
Insect repellents must be applied to the exposed portion of
FANSIDAR the body.
• Pyrimethamine –sulfadoxine o Permethrin
• Can also be used for treatment o DEET (N,N-diethyl-m-toluamide)
• Not anymore considered as a first line drug for prophylaxis o IR3535 (3-[N-acetyl-N-butyl]-aminopropionic acid
because of adverse drug reactions. ethyl ester)
o Bayrepel (1-piperidinecarboxylic acid, 2-(2-
MEFLOQUINE hydroxyethyl)-, 1-methylpropylester)
• Use of mefloquine for pregnant women in the second and Blood donors should be properly screened.
third trimester is sanctioned by the WHO and the CDC
allow the use of mefloquine even in the first trimester of MALARIA SITUATION IN THE PHILIPPINES
pregnancy. • Malaria is a rural disease
• one of the important mosquito-borne diseases affecting far-
SUPPORTIVE MANAGEMENT flung barangays of the country
• Cerebral malaria • Out of the 79 provinces nationwide, 57 are malaria endemic
– Unarousable coma not attributed to any other
cause and persists for > 30 minutes after a MALARIA ENDEMIC AREAS
seizure
• Treatment: fluid balance, hyperpyexia,
control seizures
– No mannitol, osmotic
diuretics, steroids
• Pulmonary edema
– Increased pulmonary capillary permeability
• Hypoglycemia
• Circulatory collapse/ shock
MD2020 SECTION C – MED BLOCK 6OF7
Communicable Diseases: MALARIA
MALARIA CONTROL PROGRAM
Vision: malaria-free Philippines by 2020.
STRATEGIES
1) Early diagnosis and prompt treatment;
2) Vector control – insecticide-treated mosquito net as main
vector control strategy, complemented by indoor residual
spraying;
3) early management and disease surveillance;
4) monitoring and evaluation
MD2020 SECTION C – MED BLOCK 7OF7
Das könnte Ihnen auch gefallen
- Bo Sanchez-Turtle Always Wins Bo SanchezDokument31 SeitenBo Sanchez-Turtle Always Wins Bo SanchezCristy Louela Pagapular88% (8)
- Understanding PumpDokument113 SeitenUnderstanding Pumpnyr1981_942955963100% (5)
- Motor BookDokument252 SeitenMotor BookKyaw KhNoch keine Bewertungen
- Turning The Mind Into An AllyDokument244 SeitenTurning The Mind Into An AllyNic Sosa67% (3)
- 30 Risk and InsuranceDokument4 Seiten30 Risk and InsuranceSiti Nur Ain RamliNoch keine Bewertungen
- Intern App PediatricsDokument36 SeitenIntern App PediatricsMiguel Cuevas Dolot100% (2)
- Homeopatia Vibracional RatesDokument45 SeitenHomeopatia Vibracional RatesAugusto Bd100% (4)
- Anesthesia Pocket Cards 7 18 18Dokument6 SeitenAnesthesia Pocket Cards 7 18 18Miguel Cuevas DolotNoch keine Bewertungen
- Anesthesia Pocket Cards 7 18 18Dokument6 SeitenAnesthesia Pocket Cards 7 18 18Miguel Cuevas DolotNoch keine Bewertungen
- Effectiveness of Transdermal MagnesiumDokument2 SeitenEffectiveness of Transdermal MagnesiumMiguel Cuevas Dolot100% (1)
- GTAG-14 Edited With Ad 05-20-20101 PDFDokument32 SeitenGTAG-14 Edited With Ad 05-20-20101 PDFpiornelNoch keine Bewertungen
- HandoutsDokument74 SeitenHandoutschayChay gapolNoch keine Bewertungen
- Introduction To: ParasitesDokument32 SeitenIntroduction To: ParasitesJaznMonNoch keine Bewertungen
- MalariaDokument102 SeitenMalariatummalapalli venkateswara rao100% (8)
- 1.introduction To ParasitologyDokument32 Seiten1.introduction To ParasitologyPallavi Uday Naik100% (1)
- MalariaDokument170 SeitenMalariatummalapalli venkateswara rao100% (4)
- The Sword and The Exquisiteness PDFDokument1.437 SeitenThe Sword and The Exquisiteness PDFTaruna UnitaraliNoch keine Bewertungen
- Burton's Microbiology For The Health Sciences: Chapter 21. Parasitic InfectionsDokument29 SeitenBurton's Microbiology For The Health Sciences: Chapter 21. Parasitic Infectionsmirai desu50% (2)
- MalariaDokument28 SeitenMalariaArie GradiyantoNoch keine Bewertungen
- Chapter 224 - MalariaDokument31 SeitenChapter 224 - MalariamnnicolasNoch keine Bewertungen
- Plasmodium. Leishmania, TripanosomaDokument48 SeitenPlasmodium. Leishmania, TripanosomaStefan SaerangNoch keine Bewertungen
- Microbio Act 05 10 2022Dokument2 SeitenMicrobio Act 05 10 2022Janna Niña ElementoNoch keine Bewertungen
- Lesson 5 - PlasmodiumDokument9 SeitenLesson 5 - PlasmodiumAnya IgnacioNoch keine Bewertungen
- PlasmodiumDokument25 SeitenPlasmodiumyt2zkpkphqNoch keine Bewertungen
- L09 MalariaDokument30 SeitenL09 MalariaS sNoch keine Bewertungen
- Disease Biology of Vector Borne Diseases: Malaria /dengueDokument135 SeitenDisease Biology of Vector Borne Diseases: Malaria /dengueMeenakshisundaram CNoch keine Bewertungen
- Introduction To Parasitology - B28Dokument23 SeitenIntroduction To Parasitology - B28Heswer RajNoch keine Bewertungen
- Kylie Malaria Report Final 2Dokument18 SeitenKylie Malaria Report Final 2Francine UriarteNoch keine Bewertungen
- Lesson 5 Plasmodium SPPDokument8 SeitenLesson 5 Plasmodium SPPAnya IgnacioNoch keine Bewertungen
- MALARIADokument7 SeitenMALARIAjeccomNoch keine Bewertungen
- 219 - MalariaDokument16 Seiten219 - Malaria4g8psyr2qfNoch keine Bewertungen
- Assingment of ParasateDokument36 SeitenAssingment of ParasateHibaaq AxmedNoch keine Bewertungen
- Plasmodium MalariaDokument18 SeitenPlasmodium Malariajahanvi vermaNoch keine Bewertungen
- SPOROZOADokument5 SeitenSPOROZOACDNoch keine Bewertungen
- DR - Nasser AL Amin Medical Resident, QCHDokument76 SeitenDR - Nasser AL Amin Medical Resident, QCHmohammednaNoch keine Bewertungen
- 2.4amalaria StrawberryDokument11 Seiten2.4amalaria StrawberrydeevoncNoch keine Bewertungen
- 1 Maisarah Repin© Group 531-FDokument4 Seiten1 Maisarah Repin© Group 531-FMaisarah RepinNoch keine Bewertungen
- Para Lect Prelims (Reviewer) : Lumbricoides Is An Example of A/anDokument17 SeitenPara Lect Prelims (Reviewer) : Lumbricoides Is An Example of A/anJ Pao Bayro - LacanilaoNoch keine Bewertungen
- PROTOZOADokument3 SeitenPROTOZOAMaria Jevica Barandon SolimanNoch keine Bewertungen
- Medical Parasitology A Self Instructional Text PDFDriveDokument60 SeitenMedical Parasitology A Self Instructional Text PDFDriveDenise Sta. AnaNoch keine Bewertungen
- Plasmodiumspp 230727053539 5ffdb015Dokument51 SeitenPlasmodiumspp 230727053539 5ffdb015راوند اعبيدNoch keine Bewertungen
- CDC - Malaria - About Malaria - BiologyDokument11 SeitenCDC - Malaria - About Malaria - Biologyselimamira018Noch keine Bewertungen
- 206 MalariaDokument3 Seiten206 MalariaQuang Huy PhạmNoch keine Bewertungen
- The Life Cycle & The Transmission Dynamic Versi 1Dokument14 SeitenThe Life Cycle & The Transmission Dynamic Versi 1rayNoch keine Bewertungen
- Malaria: Prof Dr. Hj. Wan Omar Abdullah, JSMDokument35 SeitenMalaria: Prof Dr. Hj. Wan Omar Abdullah, JSMMohd ZulhanafiNoch keine Bewertungen
- Unit 8Dokument6 SeitenUnit 8Tresha MadroñalNoch keine Bewertungen
- Malaria Powerpoint Slides PDF For Yunus-SinaDokument21 SeitenMalaria Powerpoint Slides PDF For Yunus-SinaSuzy SazaliNoch keine Bewertungen
- Malaria ىواسكرك كرابم ةلئان .د دادعاDokument87 SeitenMalaria ىواسكرك كرابم ةلئان .د دادعاkoncoerrorNoch keine Bewertungen
- Pneumocystis Carinii: Igm and Igg LevelsDokument8 SeitenPneumocystis Carinii: Igm and Igg LevelslyrojenNoch keine Bewertungen
- Plasmodium MP2 2020-21Dokument29 SeitenPlasmodium MP2 2020-21Reza YudiantoroNoch keine Bewertungen
- Malaria Prevention For Non-Immune: Level 2Dokument38 SeitenMalaria Prevention For Non-Immune: Level 2Victor SanchezNoch keine Bewertungen
- 9.parasit Filariasis-Amoeba (Rev 03.17)Dokument36 Seiten9.parasit Filariasis-Amoeba (Rev 03.17)maya dwiNoch keine Bewertungen
- Dr. Syeda Anjuman Nasreen Assistant Prof - MicrobiologyDokument52 SeitenDr. Syeda Anjuman Nasreen Assistant Prof - MicrobiologyTamzid Bin ShafiNoch keine Bewertungen
- Malaria FrancesDokument41 SeitenMalaria FrancesFrances Lau Yee ChinNoch keine Bewertungen
- Malaria: Causative OrganismsDokument5 SeitenMalaria: Causative OrganismsanreilegardeNoch keine Bewertungen
- (IM) 1.4b Malaria - Dra. CondeDokument14 Seiten(IM) 1.4b Malaria - Dra. CondeReggie Lyn BaricanNoch keine Bewertungen
- Protozoa. Sporozoa. Haemosporidia (The Malaria Parasites)Dokument22 SeitenProtozoa. Sporozoa. Haemosporidia (The Malaria Parasites)Sharan MurugaboopathyNoch keine Bewertungen
- BIO3242 - Lecture 3Dokument86 SeitenBIO3242 - Lecture 3NGOGA NISINGIZWE NESTORNoch keine Bewertungen
- Harrison MalariaDokument22 SeitenHarrison Malariahenath93Noch keine Bewertungen
- Major Bacteria Infecting The Hematology System 2. Major Parasites Infecting The Hematologic SystemDokument128 SeitenMajor Bacteria Infecting The Hematology System 2. Major Parasites Infecting The Hematologic SystemƯớc Của BếttingNoch keine Bewertungen
- Malaria: Dr. Niniek Burhan SP - PD-KPTI Divisi Tropik Infeksi Ilmu Penyakit Dalam Fkub - RssaDokument102 SeitenMalaria: Dr. Niniek Burhan SP - PD-KPTI Divisi Tropik Infeksi Ilmu Penyakit Dalam Fkub - RssaazizahNoch keine Bewertungen
- M6Dokument14 SeitenM6Julianne Marie LacsentoNoch keine Bewertungen
- MalariaDokument3 SeitenMalariaKrista CabelloNoch keine Bewertungen
- Major Bacteria Infecting The Hematology System 2. Major Parasites Infecting The Hematologic SystemDokument121 SeitenMajor Bacteria Infecting The Hematology System 2. Major Parasites Infecting The Hematologic SystemƯớc Của BếttingNoch keine Bewertungen
- Plasmodium PDFDokument10 SeitenPlasmodium PDFJarmy BjNoch keine Bewertungen
- Parasitology 2 Shifting Outline Plasmodium: Malaria-Leading Worldwide Parasitic Disease That CausesDokument13 SeitenParasitology 2 Shifting Outline Plasmodium: Malaria-Leading Worldwide Parasitic Disease That CausesAyaAlforqueNoch keine Bewertungen
- Malaria - Update: DR - Girish Vaswani (D.N.B. Med) Consulting Physician Bhatia Hospital Motiben Dalvi Kothari HospitalDokument38 SeitenMalaria - Update: DR - Girish Vaswani (D.N.B. Med) Consulting Physician Bhatia Hospital Motiben Dalvi Kothari HospitaldrdamsNoch keine Bewertungen
- Lec 9 MalariaDokument42 SeitenLec 9 MalariaMye AkmaNoch keine Bewertungen
- The Most Important Parasitic DiseaseDokument90 SeitenThe Most Important Parasitic DiseaseAminath MeesanNoch keine Bewertungen
- Lec 9 MalariaDokument42 SeitenLec 9 MalariaMye AkmaNoch keine Bewertungen
- Antimalarial DrugsDokument19 SeitenAntimalarial Drugspallavi DiwareNoch keine Bewertungen
- PSB 368Dokument6 SeitenPSB 368Miguel Cuevas DolotNoch keine Bewertungen
- Physical Examination in ENT: Ussana Promyothin, MDDokument60 SeitenPhysical Examination in ENT: Ussana Promyothin, MDMiguel Cuevas DolotNoch keine Bewertungen
- Physical Assessment: Ear, Nose, Mouth, and ThroatDokument59 SeitenPhysical Assessment: Ear, Nose, Mouth, and ThroatMiguel Cuevas DolotNoch keine Bewertungen
- Covid 19 PDFDokument18 SeitenCovid 19 PDFMiguel Cuevas DolotNoch keine Bewertungen
- Drug IndexDokument2 SeitenDrug IndexMiguel Cuevas DolotNoch keine Bewertungen
- Store Docket - Wood PeckerDokument89 SeitenStore Docket - Wood PeckerRakesh KumarNoch keine Bewertungen
- Instructional Decision MakingDokument5 SeitenInstructional Decision Makingapi-257693907Noch keine Bewertungen
- BROMINE Safety Handbook - Web FinalDokument110 SeitenBROMINE Safety Handbook - Web Finalmonil panchalNoch keine Bewertungen
- Factsheet AMRT 2023 01Dokument4 SeitenFactsheet AMRT 2023 01arsyil1453Noch keine Bewertungen
- TRUMPF Marking Laser BrochureDokument48 SeitenTRUMPF Marking Laser BrochureKKM SBNoch keine Bewertungen
- Atlantis Implant Compatibility Chart 79214-US-1107Dokument2 SeitenAtlantis Implant Compatibility Chart 79214-US-1107Jean-Christophe PopeNoch keine Bewertungen
- CHAPTER 2 (C) Innovation in EntrepreneurDokument36 SeitenCHAPTER 2 (C) Innovation in EntrepreneurHuiLingNoch keine Bewertungen
- Metro Depot: (Aar 422) Pre-Thesis SeminarDokument3 SeitenMetro Depot: (Aar 422) Pre-Thesis SeminarSri VirimchiNoch keine Bewertungen
- Case Study 1 HRM in PandemicDokument2 SeitenCase Study 1 HRM in PandemicKristine Dana LabaguisNoch keine Bewertungen
- To Word AkheebDokument31 SeitenTo Word AkheebDavid Raju GollapudiNoch keine Bewertungen
- Asian RegionalismDokument15 SeitenAsian RegionalismLiezel AalaNoch keine Bewertungen
- High School Department PAASCU Accredited Academic Year 2017 - 2018Dokument6 SeitenHigh School Department PAASCU Accredited Academic Year 2017 - 2018Kevin T. OnaroNoch keine Bewertungen
- Coastal Blue Carbon - Methods For Assessing Carbon Stocks and Emissions Factors in Mangroves Tidal Salt Marshes and Seagrass MeadowsDokument182 SeitenCoastal Blue Carbon - Methods For Assessing Carbon Stocks and Emissions Factors in Mangroves Tidal Salt Marshes and Seagrass Meadowsapi-245803001Noch keine Bewertungen
- Pamphlet On Arrangement of Springs in Various Casnub Trolleys Fitted On Air Brake Wagon PDFDokument9 SeitenPamphlet On Arrangement of Springs in Various Casnub Trolleys Fitted On Air Brake Wagon PDFNiKhil GuPtaNoch keine Bewertungen
- Serie10 User Man ProgDokument1.042 SeitenSerie10 User Man Progfahmi derbel100% (1)
- Data Abstraction and Problem Solving With C Walls and Mirrors 6th Edition Carrano Solutions ManualDokument36 SeitenData Abstraction and Problem Solving With C Walls and Mirrors 6th Edition Carrano Solutions Manualallocaturnonylgvtt100% (12)
- Estocell - Data Sheet - 14-07-06Dokument2 SeitenEstocell - Data Sheet - 14-07-06LeoRumalaAgusTatarNoch keine Bewertungen
- Decs vs. San DiegoDokument7 SeitenDecs vs. San Diegochini17100% (2)
- How To Spend An Hour A Day in Prayer - Matthew 26:40-41Dokument1 SeiteHow To Spend An Hour A Day in Prayer - Matthew 26:40-41Steve GainesNoch keine Bewertungen
- Calculating Staff Strength:: Find Latest Hospitality Resources atDokument8 SeitenCalculating Staff Strength:: Find Latest Hospitality Resources atPriyanjali SainiNoch keine Bewertungen
- Being Agile. Staying Resilient.: ANNUAL REPORT 2021-22Dokument296 SeitenBeing Agile. Staying Resilient.: ANNUAL REPORT 2021-22PrabhatNoch keine Bewertungen
- Electrostatics Practice ProblemsDokument4 SeitenElectrostatics Practice ProblemsMohammed Aftab AhmedNoch keine Bewertungen