Beruflich Dokumente
Kultur Dokumente
Vit D CKD
Hochgeladen von
umie khoirunCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Vit D CKD
Hochgeladen von
umie khoirunCopyright:
Verfügbare Formate
translational nephrology http://www.kidney-international.
org
& 2010 International Society of Nephrology
Use of vitamin D in chronic kidney disease patients
Anca Gal-Moscovici1 and Stuart M. Sprague2
1
Hebrew University of Jerusalem, Hadassah Hospital, Ein Keren, Jerusalem, Israel and 2NorthShore University HealthSystem and
University of Chicago Pritzker School of Medicine, Evanston, Illinois, USA
Chronic kidney disease (CKD) has been recognized as a Life expectancy in patients with chronic kidney disease (CKD)
significant public health problem, with 20 million Americans, is limited, in large part, by the high rate of cardiovascular
or 11% of the adult population, currently living with CKD. Life morbidity and mortality. The development of CKD and
expectancy in patients with CKD is limited by the mineral and bone disease with its associated disorders in
development of disturbances of mineral metabolism, which calcium and phosphorus homeostasis, vitamin D metabolism,
occurs in virtually all patients during the progression of their secondary hyperparathyroidism, metabolic changes in bone,
disease, and is associated with bone loss and fractures, and vascular calcification have been implicated in the patho-
cardiovascular disease, immune suppression, and increased genesis of this high mortality rate in patients with CKD.
mortality. As kidney disease develops, there is decreased The wide range of mineral and bone metabolic disorders
functional renal mass and a reduction in renal 1a-hydroxylase have become a diagnostic and therapeutic challenge in the
activity and thus in renal production of calcitriol at very day-to-day management of patients with CKD.
early CKD stages. Recently, a potentially important role
of vitamin D receptor activation (VDRa) in the survival of EPIDEMIOLOGICAL FACTORS
patients undergoing dialysis has been suggested. Beyond the Numerous epidemiologic studies have revealed a potentially
effect on parathyroid hormone suppression, the pleiotropic important role of the vitamin D receptor (VDR) in the survival
effect of vitamin D has been associated with improvement of of patients undergoing dialysis.1,2 Compared with the absence
cardiovascular risk factors, including increased renin activity, of any form of vitamin D therapy, treatment with vitamin D
hypertension, inflammation, insulin resistance, diabetes, and compounds that activate the VDR, the so-called VDR activators
albuminuria. However, the current K/DOQI and KDIGO (VDRa), have been associated with decreased mortality, with
recommendations limit the administration of VDRa agents for the newer VDRa analogs appearing to have a greater effect than
treatment of hyperparathyroidism only. The role of vitamin D calcitriol.1–3 As these agents have been administered primarily to
administration in the different CKD stages will be discussed treat secondary hyperparathyroidism, the most obvious explana-
in this review. tion for the observed benefits could be the result of lowering of
Kidney International (2010) 78, 146–151; doi:10.1038/ki.2010.113; parathyroid hormone (PTH) concentrations. Elevated PTH has
published online 26 May 2010 been shown to be associated with a number of cardiovascular
KEYWORDS: bone; chronic kidney disease; hyperparathyroidism; vascular (myocardial fibrosis, left ventricular hypertrophy, decreased
calcification; vitamin D myocardial contractility, increased vascular and valvular calci-
fication, and decreased vasodilatation),4,5 metabolic (decreased
insulin sensitivity and disorders of lipid metabolism),6–8 hemato-
logical (bone marrow fibrosis and decreased erythropoiesis),9,10
and immunological11 abnormalities. Treatment of secondary
hyperparathyroidism could thus improve or reverse a number
of these abnormalities, potentially translating into a better
survival. However, the survival benefit attributed to use of
VDRa agents was apparently independent of serum calcium,
phosphate, and PTH concentrations, suggesting that treat-
ment with a VDRa in advanced CKD to treat moderate and
severe secondary hyperparathyroidism has a survival benefit
beyond its role in suppressing PTH secretion.
Correspondence: Stuart M. Sprague, Division of Nephrology and Hyperten-
EXTRASKELETAL ROLE OF VITAMIN D
sion, NorthShore University HealthSystem, University of Chicago Pritzker
School of Medicine, 2650 Ridge Avenue, Evanston, Illinois 60201, USA. An increased understanding of the biologic role of vitamin D in
E-mail: stuartmsprague@gmail.com both bone and mineral metabolism, as well as its extraskeletal
Received 18 August 2009; revised 24 February 2010; accepted 2 March activity, supports its association with lower mortality. Vitamin D
2010; published online 26 May 2010 is a pleiotropic steroid hormone that binds to its intracellular
146 Kidney International (2010) 78, 146–151
A Gal-Moscovici and SM Sprague: Use of vitamin D in CKD patients translational nephrology
receptor to elicit a diverse genetic response.12 Part of the TREATMENT CONSIDERATIONS
difficulty in understanding the physiologic role of vitamin D In the light of these data, we believe that patients with CKD
sterols is confusion with nomenclature. For the purpose of should be treated similarly as the general population and
clarity in this paper, we are using the nomenclature and vitamin D therapy should be offered to every CKD patient
abbreviations as noted in Table 1. Experimental and epidemiologic who shows vitamin D deficiency. However, administration of
studies have connected lower 25-hydroxyvitamin D (25 Vit D) VDRa agents is limited by the current K/DOQI (Kidney Disease
and calcitriol concentrations with cardiovascular risk factors, Outcomes Quality Initiative) recommendations. In CKD patients
including increased renin activity, hypertension, inflamma- undergoing renal replacement therapy, it is recommended to
tion, insulin resistance, diabetes, and albuminuria.13–16 use VDRa therapy only for treatment of hyperparathyroidism.
The potential ameliorative effects of vitamin D on Furthermore, it is suggested that vitamin D therapy should be
cardiovascular risk factors include mechanisms related to stopped or not initiated when phosphate concentrations are
the development of vascular calcification and atherosclerosis. 45.5 mg/dl, when intact PTH concentrations areo150 pg/ml,
In this regard, VDRa was shown to inhibit activators of or when the calcium–phosphate product exceeds 55 mg2/dl2.29
vascular mineralization such as Cbfa1 (RUNX2), bone There is no comment on the use of vitamin D to correct the
morphogenic protein-2, type I collagen, interleukin-1b, vitamin D deficiency observed in these patients. In patients with
interleukin-6, and transforming growth factor-a, and to CKD stages 3 and 4, it is recommended to correct 25 Vit D
stimulate inhibitors of vascular mineralization such as matrix deficiency when hyperparathyroidism is present with the
Gla protein and osteopontin.17–22 Similarly, data are use of nutritional replacement with either ergocalciferol or
emerging supporting a potential role of VDRa in preventing cholecalciferol. Only if hyperparathyroidism persists, it is
or ameliorating the pathogenesis of atherosclerosis. Th1 recommended to use a VDRa for treatment.29
lymphocytes, which infiltrate the subendothelial cell in Whether any type of vitamin D therapy is beneficial in
response to oxidized low-density lipoprotein, secrete inter- CKD has created some controversy; in fact, a meta-analysis
feron-g that in turn suppresses the antiatherogenic Th2 by Palmer et al.30 suggested that there was no benefit of
lymphocytes. The favorable effect of VDRa on this process vitamin D therapy in patients with CKD. Synthesizing 76 trials,
may occur by enriching the Th2 cell population.23,24 the researchers suggested that vitamin D compounds do not
Other potential mechanisms in which VDRa may reduce the risk of death or vascular calcification, and when
ameliorate or prevent cardiovascular disease include its effect compared with placebo, calcitriol results in an increased risk
on the renin-angiotensin-aldosterone axis. Decreased VDR of hypercalcemia and hyperphosphatemia and did not show a
activity increases circulating renin levels and blood pressure consistent reduction in PTH concentrations. Other VDRas
and causes left ventricular and myocyte hypertrophy in were associated with hypercalcemia but not with hyperpho-
genetically manipulated mouse models.25 Treatment with sphatemia, and an effect on PTH was also not consistently
VDRa agents inhibits renin expression, normalizes blood reduced. The researchers concluded that vitamin D treatment
pressure, and reverses the cardiac hypertrophy.26,27 for CKD patients remains uncertain. Unfortunately, this
Vitamin D insufficiency and deficiency is widely prevalent analysis excluded a 220-patient 24-week placebo-controlled
in the general population. It has been estimated that 1 billion randomized trial, which found that paricalcitol suppressed
people worldwide have vitamin D insufficiency or defi- PTH by an average of 42%, and 90% of patients achieved at
ciency.12 Similar to the general population, vitamin D least a 30% suppression of PTH,31 and also a 266-patient
insufficiency and deficiency is widely prevalent in CKD. 32-week randomized controlled trial of calcitriol versus
Regardless of the geographic location in the United States, paricalcitol, in which 80 and 90% of patients, respectively,
low 25 Vit D concentrations are present in 71% of patients achieved 450% PTH suppression.32 Instead, the researchers
with stage 3 CKD and 83% of patients with stage 4 CKD. included studies from the 1980s in which PTH suppression
Suboptimal 25 Vit D levels can be found in up to 97% of was not the primary end point. For adverse outcomes such as
patients on maintenance hemodialysis.28 hypercalcemia, the results were driven by a single study,
which considered elevated calcium as acceptable and possibly
necessary. Numerous placebo-controlled studies show that
Table 1 | Vitamin D nomenclature
the newer VDRas do not result in significant hypercalcemia
Term Sterol Comment or hyperphosphatemia when compared with placebo. Thus,
Vitamin D Cholecalciferol D3 the conclusion that vitamin D is not useful in CKD cannot be
Ergocalciferol D2 ascertained from this study. Prospective studies are required
25 Vit D Calcidiol (25(OH)D3) D3
Ercalcidiol (25(OH)D2) D2
to address whether VDRa therapy should be initiated in any
VDRa Calcitriol (1,25(OH)2D3) D3; natural hormone stage of CKD to replace the calcitriol deficiency and whether
Alfacalcidol (1(OH)D3) D3; synthetic prohormonea such therapy would have physiologic benefit.
Doxercalciferol (1(OH)D2) D2; synthetic prohormone In most patients with early CKD, calcium and phosphate
Paricalcitol (19nor,1,25(OH)2D2) D2; synthetic analog
Maxacalcitol (22oxa,1,25(OH)2D3) D3; synthetic analog
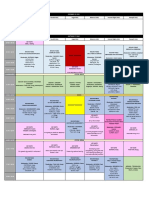
disorders are not evident until advanced stage 4 (Figure 1),
Abbreviations: VDRa, vitamin D receptor agonist; 25 Vit D, 25-hydroxyvitamin D.
and hence the high risk for cardiovascular events in this
a
Prohormone requires 25-hydroxylation by the liver to become an active analog. population could not be attributed solely to disturbances in
Kidney International (2010) 78, 146–151 147
translational nephrology A Gal-Moscovici and SM Sprague: Use of vitamin D in CKD patients
2000
Stage 1 Stage 2 Stage 3 Stage 4
50
FGF
200
Calcitriol (pg/ml)
FGF-23 (RU/ml)
40
Calcitriol
Intact PTH (pg/ml)
PTH
30 P < 0.01 150
20 100
10
100
50
P < 0.01
0
105 95 85 75 65 55 45 35 25 15
GFR (ml/min)
Figure 1 | Progression of changes in calcitriol, parathyroid hormone (PTH), and fibroblast growth factor-23 (FGF-23) with
chronic kidney disease (CKD). The early decrease in calcitriol with the increase of FGF-23 before the increase in PTH as CKD develops.
Adapted from references 28, 33, 38, and 39.
these minerals. However, calcitriol concentrations already Low doses of VDRa agents have recently been shown to be
decline to the lower limit of the normal in stage 2 CKD, and associated with a significantly better survival in pre-dialysis
progress to low and very low levels in patients with stages 3 patients.47,48 Shoben et al.47 reported a survival benefit of
and 4 CKD.28,33 Vitamin D deficiency is associated with therapy with calcitriol versus no therapy in patients with
increased mortality and cardiovascular morbidity in patients stages 3 and 4 CKD. To be eligible for the study, patients had
undergoing dialysis.34 Similar association may also be present to be calcitriol naive and have a PTH level of 70 pg/ml during
in patients with earlier stages of CKD.35–37 the year before starting therapy. Patients who were treated
The major determinant of low calcitriol levels is the with calcitriol had a 26% lower mortality compared with
reduction in renal mass with associated decreased 1a- those who were untreated. Survival benefit in patients treated
hydroxylase available for converting 25 Vit D by the proximal with calcitriol, despite the important limitation of the study,
tubular cells. 1a-hydroxylase is further suppressed by was not statistically different across baseline PTH levels,
fibroblast growth factor-23. The secretion of fibroblast including those with lower pretreatment PTH, greater risk of
growth factor-23 is stimulated by phosphate and its hypercalcemia, and higher phosphorus levels.47
concentrations are markedly increased in the early stages of Similar results have been reported by Kovesdy et al.48 in
CKD.38,39 Recently, it was shown that fibroblast growth 520 male US veterans outpatient population with CKD stages
factor-23 may also suppress the expression of PTH 3–5, showing that treatment of secondary hyperparathyroid-
mRNA40,41 as well as osteoblastic differentiation and bone ism with low doses of an oral nonselective activated vitamin
matrix maturation,42 in addition to its phosphaturic activity. D was associated with a significantly better survival. This
These findings might result in a delayed increase in PTH benefit was present in all the examined subgroups, including
concentrations and suppressed bone turnover, as an early patients with lower pretreatment PTH, higher calcium, and
presentation in CKD stages 2 and 3. They could also result in higher phosphorus levels. There are other potential benefits
the postponement of vitamin D treatment in early CKD regarding the treatment of patients with CKD stages 2–4 with
stages. Although these hypotheses should be further tested by VDRa agents, which include the renoprotective role in
clinical and laboratory research, several investigators have diabetic nephropathy and the amelioration of proteinuria of
found adynamic bone disease in pre-dialysis patients,43,44 and glomerular origin.49–51 An another important issue regarding
also in an animal model of CKD and metabolic syndrome, in low calcitriol levels in patients with CKD is the prevalence of
which adynamic bone develops in early renal insufficiency 25 Vit D deficiency in this population that is independent of
despite very mild secondary hyperparathyroidism.45 CKD staging.28,52,53 Interestingly, low substrate levels of 25
Usually the administration of VDRa in incipient CKD Vit D are associated with low calcitriol levels, except for those
with normal or slightly increased PTH concentration is with normal kidney function.54 Lower serum 25 Vit D levels
avoided because of the concern of oversuppression of the have been associated with impaired glucose tolerance and
parathyroid gland and development of adynamic bone. diabetes across diverse populations, and administration of
However, administration of small physiologic doses of VDRa vitamin D3 to deficient animals improves insulin secretion.55–57
agents in mild CKD was shown to normalize the bone The active form of vitamin D, calcitriol, is a potent
metabolism even in patients with low PTH and low-turnover inducer of the antimicrobial protein cathelicidin. In
bone disease.46 macrophages, this response is dependent on intracrine
148 Kidney International (2010) 78, 146–151
A Gal-Moscovici and SM Sprague: Use of vitamin D in CKD patients translational nephrology
synthesis of 1,25(OH)2D from precursor, catalyzed by the placebo with a tendency for improved bone histology,
enzyme 25-hydroxyvitamin D-1a-hydroxylase (CYP27B1). although adynamic bone was observed in some biopsies.
Low cathelicidin plasma level in patients undergoing dialysis There were two studies performed using VDRa prohor-
is predictive of increases in infectious disease mortality.58 mones, which required activation by the 25-hydroxlyase in
Treatment with 25 Vit D have been shown to improve the the liver. The study using alfacalcidol included 176 patients;
immune response.59 however, it was also conducted in 1995 and had some of the
Treatment with vitamin D (ergocalciferol or cholecalciferol) same problems as the study with calcitriol, and was
to raise 25 Vit D levels was shown to increase calcitriol in conducted with reference to the clinical practice at that
both stage 3 and 4 CKD, but lowered PTH only in CKD stage time.46 The study was designed to maintain calcium levels at
3, but not in stage 4 patients.60,61 Similar findings were noted the upper limit of the normal laboratory reference range.
with the use of cholecalciferol.62 The potential success of Compared with placebo, PTH levels fell significantly (28%)
ergocalciferol monotherapy might be limited, as cellular with improvement in bone turnover. The study evaluating
uptake of 25 Vit D may be dependent on combined therapy doxercalciferol included 55 patients, was performed with
with calcitriol.63 Consistent with this notion is the finding current clinical practice, and was designed to lower PTH
that VDRa treatment enhances megalin expression and that concentrations.67 Compared with placebo, PTH levels fell
megalin endocytosis of the 25 Vit D–vitamin D binding significantly (46%) and although no bone histology was
protein complex from the glomerular ultrafiltrate is the performed, bone-specific alkaline phosphatase levels fell
major mechanism for delivering 25 Vit D to the 1a- significantly in the treated subjects. However, no data for bone
hydroxylase enzyme in the proximal tubule.64,65 Thus, in alkaline phosphatase were provided for the placebo-treated
our opinion ergocalciferol or cholecalciferol should be used subjects. The most recently published study used paricalcitol
to correct 25 Vit D levels in patients with CKD, either before and included 220 patients.31 Similar to the PTH results with
or during active vitamin D therapy. Clearly, appropriate doxercalciferol, PTH concentrations fell significantly (42%) and
outcome studies are required to assess the role of vitamin D this was associated with a significant decrease in bone-specific
therapy on outcomes in all patients with CKD. alkaline phosphatase compared with placebo subjects.
Unfortunately, none of these studies provided other
TREATMENT IN CKD STAGES 3 AND 4 outcome information. In these studies, calcium levels trended
There are very little data to guide the use of VDRa agents in upward for paricalcitol and doxercalciferol, whereas they
CKD stages 3 and 4. Although there may be potential for increased significantly for calcitriol- and alfacalcidol-treated
improved outcomes with the use of VDRa agents in these subjects. Phosphate levels and the calcium–phosphorus
patients, therapy and recommendations have focused on product increased significantly for doxercalciferol, with an
treatment for hyperparathyroidism. There are four rando- upward trend for paricalcitol and alfacalcidol.
mized controlled trials that have assessed the use of
doxercalciferol, paricalcitol, alfacalcidol, or calcitriol with CONCLUSION
placebo (Table 2). The study using calcitriol included only 30 In conclusion, vitamin D deficiency develops very early in
patients and assessed laboratory values and bone histomor- the course of CKD. There is an increasing body of data
phometry.66 Unfortunately, this study was conducted in1988 suggesting that VDRa has a central role in lowering the
and the design of the study was to increase serum calcium morbidity and mortality observed in these patients through
and evaluate bone histology and was not specific for mechanism involving classical skeletal and non-classical
reduction in PTH concentrations. Furthermore, these data pathways. Thus, it is imperative that future studies are
may also be hard to interpret because of changes in clinical directed toward understanding the role of vitamin D and
practice and the common use of aluminum-based phosphate VDRa in maintaining health. Presently, the indication for
binders at that time. However, treatment with calcitriol did vitamin D and VDRa treatment in CKD is predicated on the
result in a significant decrease in PTH (26%) compared with serum or plasma PTH concentration. It is our opinion that,
Table 2 | Results of randomized controlled trials of VDRa versus placebo in non-dialysis CKD stage 3–5 patients
VDRa (final dose) Duration (months) (n) Outcome Results
66
Calcitriol (B0.5 mg/day) 8 (30) Bone biopsy Placebo; increase in bone formation
(many worsened)
Calcitriol; decrease in bone formation
(some better, few developed adynamic)
No difference in mineralization and volume
Change in PTH 26% reduction
Alfacalcidol46 (B0.4 mg/day) 24 (176) Bone biopsy Alfacalcidol tended to result in improved bone turnover
Change in PTH 28% reduction
Doxercalciferol67 (B1.6 mg/day) 6 (55) Change in PTH 46% reduction
Paricalcitol31 (B1.4 mg/day) 6 (220) Change in PTH 42% reduction
Abbreviations: CKD, chronic kidney disease; PTH, parathyroid hormone; VDRa, vitamin D receptor agonist.
Kidney International (2010) 78, 146–151 149
translational nephrology A Gal-Moscovici and SM Sprague: Use of vitamin D in CKD patients
consistent with K/DOQI and KDIGO (Kidney Disease: 20. Bostrom K, Watson KE, Horn S et al. Bone morphogenetic protein
expression in human atherosclerotic lesions. J Clin Invest 1993; 91:
Improving Global Outcomes) guidelines, current evidence 1800–1809.
supports treating all patients with vitamin D (either 21. Moe SM, Duan D, Doehle BP et al. Uremia induces the osteoblast
differentiation factor Cbfa1 in human blood vessels. Kidney Int 2003; 63:
ergocalciferol or cholecalciferol) to correct 25 Vit D 1003–1011.
deficiency. In the presence of hyperparathyroidism, VDRa 22. Jono S, Peinado C, Giachelli CM. Phosphorylation of osteopontin is
therapy should be strongly considered. However, until required for inhibition of vascular smooth muscle cell calcification. J Biol
Chem 2000; 275: 20197–20203.
appropriately designed outcome studies are performed, the 23. Staeva-Vieira TP, Freedman LP. 1,25-dihydroxyvitamin D inhibits IFN-g
use of VDRa therapy to replace hormonal calcitriol deficiency and IL-4 levels during in vitro polarization of primary murine CD4+ T cells.
is speculative and opinion based. J Immunol 2002; 168: 1181–1189.
24. Barrat FJ, Cua DJ, Boonstra A et al. In vitro generation of interleukin 10-
producing regulatory CD4+Tcells is induced by immunosuppressive
DISCLOSURE drugs and inhibited by T helper type 1 (TH1)- and TH2-inducing
SMS serves as a consultant and has received grants from Abbott, Amgen cytokines. J Exp Med 2002; 195: 603–616.
and Genzyme and AG-M declared no competing interests. 25. Xiang W, Kong J, Chen S et al. Cardiac hypertrophy in vitamin D
receptor knockout mice: role of the systemic and cardiac
renin–angiotensin systems. Am J Physiol Endocrinol Metab 2005; 228:
REFERENCES E124–E132.
1. Teng M, Wolf M, Lowrie E et al. Survival of patients undergoing 26. Bodyak N, Ayus JC, Achinger S et al. Activated vitamin D attenuates left
hemodialysis with paricalcitol or calcitriol therapy. N Engl J Med 2003; ventricular abnormalities induced by dietary sodium in Dahl salt-sensitive
349: 446–456. animals. Proc Natl Acad Sci USA 2007; 104: 16810–16815.
2. Teng M, Wolf M, Ofstun MN et al. Activated injectable vitamin D and 27. Li YC, Kong J, Wei M et al. 1,25-dihydroxyvitamin D is a negative
hemodialysis survival: a historical cohort study. J Am Soc Nephrol 2005; endocrine regulator of the renin-angiotensin system. J Clin Invest 2002;
16: 1115–1125. 110: 229–238.
3. Tentori F, Hunt WC, Stidley CA et al. Mortality risk among vitamin D 28. González EA, Sachdeva A, Oliver DA et al. Vitamin D insufficiency and
analog hemodialysis patients receiving different vitamin D analogs. deficiency in chronic kidney disease. A single center observational study.
Kidney Int 2006; 70: 1858–1865. Am J Nephrol 2004; 24: 503–510.
4. Massry SG, Smogorzewski M. Mechanisms through which parathyroid 29. Eknoyan G, Levin A, Levin NW. Clinical practice guidelines for bone
hormone mediates its deleterious effects on organ function in uremia. metabolism and disease in chronic kidney disease. Am J Kidney Dis 2003;
Semin Nephrol 1994; 14: 219–231. 42(Suppl 3): S1–S201.
5. Mazzaferro S, Coen G, Bandini S et al. Role of ageing, chronic renal failure 30. Palmer SC, McGregor DO, Macaskill P et al. Meta-analysis: vitamin D
and dialysis in the calcification of mitral annulus. Nephrol Dial Transplant compounds in chronic kidney disease. Ann Intern Med 2007; 147:
1993; 8: 335–340. 840–853.
6. Chiu KC, Chuang LM, Lee NP et al. Insulin sensitivity is inversely correlated 31. Coyne D, Acharya M, Qiu P et al. Paricalcitol capsule for the treatment of
with plasma intact parathyroid hormone level. Metabolism 2000; 49: secondary hyperparathyroidism in stages 3 and 4 CKD. Am J Kidney Dis
1501–1505. 2006; 47: 263–276.
7. Gadallah MF, el-Shahawy M, Andrews G et al. Factors modulating 32. Sprague SM, Llach F, Amdahl M et al. Paricalcitol versus calcitriol in the
cytosolic calcium. Role in lipid metabolism and cardiovascular morbidity treatment of secondary hyperparathyroidism. Kidney Int 2003; 63:
and mortality in peritoneal dialysis patients. Adv Perit Dial 2001; 17: 29–36. 1483–1490.
8. Wareham NJ, Byrne CD, Carr C et al. Glucose intolerance is associated 33. Levin A, Bakris GL, Molitch M et al. Prevalence of abnormal serum vitamin
with altered calcium homeostasis: a possible link between increased D, PTH, calcium, and phosphorus in patients with chronic kidney disease:
serum calcium concentration and cardiovascular disease mortality. results of the study to evaluate early kidney disease. Kidney Int 2007; 71:
Metabolism 1997; 46: 1171–1177. 31–38.
9. Meytes D, Bogin E, Ma A et al. Effect of parathyroid hormone on 34. Wolf M, Shah A, Gutierrez O et al. Vitamin D levels and early mortality
erythropoiesis. J Clin Invest 1981; 67: 1263–1269. among incident hemodialysis patients. Kidney Int 2007; 72: 1004–1013.
10. Rao DS, Shih MS, Mohini R. Effect of serum parathyroid hormone and 35. Barreto DV, Barreto FC, Liabeuf S et al. Vitamin D affects survival
bone marrow fibrosis on the response to erythropoietin in uremia. N Engl independently of vascular calcification in chronic kidney disease. Clin J
J Med 1993; 328: 171–175. Am Soc Nephrol 2009; 4: 1128–1135.
11. Massry SG, Alexiewicz JM, Gaciong Z et al. Secondary 36. Inaguma D, Nagaya H, Hara K et al. Relationship between serum 1,25-
hyperparathyroidism and the immune system in chronic renal failure. dihydroxyvitamin D and mortality in patients with pre-dialysis chronic
Semin Nephrol 1991; 11: 186–201. kidney disease. Clin Exp Nephrol 2008; 12: 126–131.
12. Holick MF. Vitamin D deficiency. N Engl J Med 2007; 357: 266–281. 37. Mehrotra R, Kermah DA, Salusky IB et al. Chronic kidney disease,
13. Li YC, Kong J, Wei M et al. 1,25-Dihydroxyvitamin D(3) is a negative hypovitaminosis D, and mortality in the United States. Kidney Int 2009; 76:
endocrine regulator of the renin-angiotensin system. J Clin Invest 2002; 977–983.
110: 229–238. 38. Larsson T, Nisbeth U, Ljunggren O et al. Circulating concentration of FGF-
14. Kuhlmann A, Haas CS, Gross ML et al. 1,25-Dihydroxyvitamin D3 23 increases as renal function declines in patients with chronic kidney
decreases podocyte loss and podocyte hypertrophy in the subtotally disease, but does not change in response to variation in phosphate
nephrectomized rat. Am J Physiol Renal Physiol 2004; 286: F526–F533. intake in healthy volunteers. Kidney Int 2003; 64: 2272–2279.
15. Oelzner P, Franke S, Muller A et al. Relationship between soluble markers 39. Gutierrez O, Isakova T, Rhee E et al. Fibroblast growth factor-23 mitigates
of immune activation and bone turnover in postmenopausal women hyperphosphatemia but accentuates calcitriol deficiency in chronic
with rheumatoid arthritis. Rheumatology (Oxford) 1999; 38: 841–847. kidney disease. J Am Soc Nephrol 2005; 16: 2205–2215.
16. Scragg R, Sowers M, Bell C. Serum 25-hydroxyvitamin D, diabetes, and 40. Krajisnik T, Björklund P, Marsell R et al. Fibroblast growth
ethnicity in the Third National Health and Nutrition Examination Survey. factor-23 regulates parathyroid hormone and 1alpha-hydroxylase
Diabetes Care 2004; 27: 2813–2818. expression in cultured bovine parathyroid cells. J Endocrinol 2007; 195:
17. Bellows CG, Reimers SM, Heersche JN. Expression of mRNAs for type I 125–131.
collagen, bone sialoprotein, osteocalcin and osteopontin at different 41. Galitzer H, Ben-Dov I, Lavi-Moshayoff V et al. Fibroblast growth factor 23
stages of osteoblastic differentiation and their regulation by 1,25 acts on the parathyroid to decrease parathyroid hormone secretion. Curr
dihydroxyvitamin D. Cell Tissue Res 1999; 297: 249–259. Opin Nephrol Hypertens 2008; 17: 363–367.
18. Speer MY, McKee MD, Guldberg RE et al. Inactivation of the osteopontin 42. Wang H, Yoshiko Y, Yamamoto R et al. Overexpression of fibroblast
gene enhances vascular calcification of matrix gla protein-deficient mice: growth factor 23 suppresses osteoblast differentiation and matrix
evidence for osteopontin as an inducible inhibitor of vascular calcification mineralization in vitro. J Bone Miner Res 2008; 23: 939–948.
in vivo. J Exp Med 2002; 196: 1047–1055. 43. Spasovski GB, Bervoets AR, Behets GJ et al. Spectrum of renal bone
19. Parhami F, Basseri B, Hwang J et al. High-density lipoprotein regulates disease in end-stage renal failure patients not yet on dialysis. Nephrol Dial
calcification of vascular cells. Circ Res 2002; 91: 570–576. Transplant 2003; 18: 1159–1166.
150 Kidney International (2010) 78, 146–151
A Gal-Moscovici and SM Sprague: Use of vitamin D in CKD patients translational nephrology
44. Coen G, Mazzaferro S, Ballanti P et al. Renal bone disease in 76 patients 56. Scragg R, Sowers M, Bell C. Serum 25-hydroxyvitamin D, diabetes, and
with varying degrees of predialysis chronic renal failure: a cross-sectional ethnicity in the Third National Health and Nutrition Examination Survey.
study. Nephrol Dial Transplant 1996; 11: 813–819. Diabetes Care 2004; 27: 2813–2818.
45. Davies MR, Lund RJ, Mathew S et al. Low turnover osteodystrophy and 57. Kadowaki S, Norman AW. Dietary vitamin D is essential for normal
vascular calcification are amenable to skeletal anabolism in an animal insulin secretion from the perfused rat pancreas. J Clin Invest 1984; 73:
model of chronic kidney disease and the metabolic syndrome. J Am Soc 759–766.
Nephrol 2005; 16: 917–928. 58. Gombart AF, Bhan I, Borregaard N et al. Low plasma level of cathelicidin
46. Hamdy NA, Kanis JA, Beneton MN et al. Effect of alfacalcidol on natural antimicrobial peptide (hCAP18) predicts increased infectious disease
course of renal bone disease in mild to moderate renal failure. BMJ 1995; mortality in patients undergoing hemodialysis. Clin Infect Dis 2009; 48:
310: 358–363. 418–424.
47. Shoben AB, Rudser KD, de Boer IH et al. Association of oral calcitriol with 59. Adams JS, Hewison M. Unexpected actions of vitamin D: new
improved survival in nondialyzed CKD. J Am Soc Nephrol 2008; 19: perspectives on the regulation of innate and adaptive immunity. Nat Clin
1613–1619. Pract Endocrinol Metab 2008; 4: 80–90.
48. Kovesdy CP, Ahmadzadeh S, Anderson JE et al. Association of activated 60. Zisman AL, Hristova M, Ho LT et al. Impact of ergocalciferol treatment of
vitamin D treatment and mortality in chronic kidney disease. Arch Intern vitamin D deficiency on serum parathyroid hormone concentrations in
Med 2008; 168: 397–403. chronic kidney disease. Am J Nephrol 2007; 27: 36–43.
49. Agarwal R, Acharya M, Tian J et al. Antiproteinuric effect of oral 61. Martin KJ, González EA. Vitamin D analogues for the management of
paricalcitol in chronic kidney disease. Kidney Int 2005; 68: 2823–2828. secondary hyperparathyroidism. Am J Kidney Dis 2001; 38(5 Suppl 5):
50. Kuhlmann A, Haas CS, Gross ML et al. 1,25-Dihydroxyvitamin D3 S34–S40.
decreases podocyte loss and podocyte hypertrophy in the subtotally 62. Andress DL, Coyne DW, Kalantar-Zadeh K et al. Management of
nephrectomized rat. Am J Physiol Renal Physiol 2004; 286: F526–F533. secondary hyperparathyroidism in stages 3 and 4 chronic kidney disease.
51. Fishbane S, Chittineni H, Packman M et al. Oral paricalcitol in the Endocr Pract 2008; 14: 18–27.
treatment of patients with CKD and proteinuria: a randomized trial. Am J 63. Gallieni M, Kamimura S, Ahmed A et al. Kinetics of monocyte 1a-
Kidney Dis 2009; 54: 647–652. hydroxylase in renal failure. Am J Physiol 1995; 268: F746–F753.
52. Nesby-O’Dell S, Scanlon KS, Cogswell ME et al. Hypovitaminosis D 64. Liu W, Yu WR, Carling T et al. Regulation of gp330/megalin expression by
prevalence and determinants among African American and white women vitamins A and D. Eur J Clin Invest 1998; 28: 100–107.
of reproductive age: Third National Health and Nutrition Examination 65. Nykjaer A, Dragun D, Walther D et al. An endocytic pathway essential for
Survey, 1988–1994. Am J Clin Nutr 2002; 76: 187–192. renal uptake and activation of the steroid 25(OH) vitamin D3. Cell 1999;
53. Holick MF. Vitamin D: importance in the prevention of cancers, type I 96: 507–515.
diabetes, heart disease, and osteoporosis. AmJ Clin Nutr 2004; 79: 66. Nordal KP, Dahl E. Low dose calcitriol versus placebo in patients
362–371. with predialysis chronic renal failure. J Clin Endocrinol Metab 1988; 67:
54. Papapoulos SE, Clemens TL, Fraher LJ et al. Metabolites of vitamin D in 929–936.
human vitamin D deficiency: effect of vitamin D3 or 1,25- 67. Coburn JW, Maung HM, Elangovan L et al. Doxercalciferol safely
ihydroxycholecalciferol. Lancet 1980; 2: 612–615. suppresses PTH levels in patients with secondary hyperparathyroidism
55. Baynes KC, Boucher BJ, Feskens EJ et al. Vitamin D, glucose tolerance and associated with chronic kidney disease stages 3 and 4. Am J Kidney Dis
insulinaemia in elderly men. Diabetologia 1997; 40: 344–347. 2004; 43: 877–890.
Kidney International (2010) 78, 146–151 151
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- 2019 J. Phys. Conf. Ser. 1381 011001 PDFDokument2 Seiten2019 J. Phys. Conf. Ser. 1381 011001 PDFumie khoirunNoch keine Bewertungen
- CMAM MHealth App Poster ACF Conf Nov 2016Dokument1 SeiteCMAM MHealth App Poster ACF Conf Nov 2016umie khoirunNoch keine Bewertungen
- Probability Distributions PDFDokument10 SeitenProbability Distributions PDFumie khoirunNoch keine Bewertungen
- Guideline EMR DesignDokument3 SeitenGuideline EMR Designumie khoirunNoch keine Bewertungen
- Sistem Tagihan RS Menggunakan AlgoritmaDokument20 SeitenSistem Tagihan RS Menggunakan Algoritmaumie khoirunNoch keine Bewertungen
- 0884533611431069Dokument1 Seite0884533611431069umie khoirunNoch keine Bewertungen
- Liberate Science Sustainable Science Symposium Ticket 1ZZF 1Dokument1 SeiteLiberate Science Sustainable Science Symposium Ticket 1ZZF 1umie khoirunNoch keine Bewertungen
- 2019 J. Phys. Conf. Ser. 1381 011001 PDFDokument2 Seiten2019 J. Phys. Conf. Ser. 1381 011001 PDFumie khoirunNoch keine Bewertungen
- 2019 J. Phys. Conf. Ser. 1381 011001 PDFDokument2 Seiten2019 J. Phys. Conf. Ser. 1381 011001 PDFumie khoirunNoch keine Bewertungen
- Practice Patterns Relating To The UseDokument5 SeitenPractice Patterns Relating To The Useumie khoirunNoch keine Bewertungen
- Skripsi Tanpa Bab PembahasanDokument103 SeitenSkripsi Tanpa Bab Pembahasanumie khoirunNoch keine Bewertungen
- Acta Medica IndonesianaDokument10 SeitenActa Medica Indonesianaumie khoirunNoch keine Bewertungen
- Practice Patterns Relating To The UseDokument5 SeitenPractice Patterns Relating To The Useumie khoirunNoch keine Bewertungen
- Nutrition PDFDokument16 SeitenNutrition PDFumie khoirunNoch keine Bewertungen
- PUB Box391498B PUBLIC PDFDokument107 SeitenPUB Box391498B PUBLIC PDFumie khoirunNoch keine Bewertungen
- Tinjauan Validity Dan Verfiikasi Berkas RMDokument6 SeitenTinjauan Validity Dan Verfiikasi Berkas RMumie khoirunNoch keine Bewertungen
- The Potential Use of Biomarkers in Predicting Contrast-Induced Acute Kidney InjuryDokument17 SeitenThe Potential Use of Biomarkers in Predicting Contrast-Induced Acute Kidney Injuryumie khoirunNoch keine Bewertungen
- Brosur Fikes 2019Dokument6 SeitenBrosur Fikes 2019umie khoirunNoch keine Bewertungen
- Maternal HealthDokument14 SeitenMaternal Healthumie khoirunNoch keine Bewertungen
- Maternal HealthDokument14 SeitenMaternal Healthumie khoirunNoch keine Bewertungen
- Acta Medica IndonesianaDokument10 SeitenActa Medica Indonesianaumie khoirunNoch keine Bewertungen
- FactorsaffectingPatientSatisfactionandHealthcareQualityInternationalJournalofHealthCareQualityAssuranceVol22No.4 2Dokument18 SeitenFactorsaffectingPatientSatisfactionandHealthcareQualityInternationalJournalofHealthCareQualityAssuranceVol22No.4 2umie khoirunNoch keine Bewertungen
- QultypaperwithAaron PDFDokument12 SeitenQultypaperwithAaron PDFumie khoirunNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Name_Naw Aung_La Mai Patient Focused ProceduresDokument2 SeitenName_Naw Aung_La Mai Patient Focused ProceduresEileenNoch keine Bewertungen
- Classifications of Pharmaceutical Drugs1Dokument24 SeitenClassifications of Pharmaceutical Drugs1RPh Krishna Chandra JagritNoch keine Bewertungen
- Dan Gelber Letter To Gov. Ron DeSantisDokument2 SeitenDan Gelber Letter To Gov. Ron DeSantisPeterBurkeNoch keine Bewertungen
- Makati Medical Center College of NursingDokument14 SeitenMakati Medical Center College of NursingEunice Angela FulguerasNoch keine Bewertungen
- Afterword by Ilyene BarskyDokument5 SeitenAfterword by Ilyene Barskykkleiman_ppscNoch keine Bewertungen
- Biochemistry Importance for NursesDokument15 SeitenBiochemistry Importance for NursesJulius Memeg PanayoNoch keine Bewertungen
- Gunshot Wound ScenariosDokument19 SeitenGunshot Wound Scenariossweetwaffle50% (2)
- Kala-Azar (Leishmaniasis) Symptoms, Signs, DiagnosisDokument36 SeitenKala-Azar (Leishmaniasis) Symptoms, Signs, Diagnosisatulbd2006Noch keine Bewertungen
- Understanding BenzodiazepinesDokument7 SeitenUnderstanding BenzodiazepinesChris Patrick Carias StasNoch keine Bewertungen
- 2019 International Symposium on Pediatric Audiology ScheduleDokument3 Seiten2019 International Symposium on Pediatric Audiology ScheduleEulalia JuanNoch keine Bewertungen
- Leucorrhea KnowledgeDokument3 SeitenLeucorrhea KnowledgeAnamika ChoudharyNoch keine Bewertungen
- DiagramDokument12 SeitenDiagramJessica CindyNoch keine Bewertungen
- CNS Microbiology MeningitisDokument26 SeitenCNS Microbiology MeningitisSaransh GhimireNoch keine Bewertungen
- Adel Elkady Sba PDFDokument290 SeitenAdel Elkady Sba PDFAsh Ame100% (2)
- Sonopuls 490 User ManualDokument57 SeitenSonopuls 490 User ManualMaryam BushraNoch keine Bewertungen
- ACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-nCoV InfectionDokument16 SeitenACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-nCoV InfectionSY LodhiNoch keine Bewertungen
- Apollo: Reliability Meets Realism For Nursing or Prehospital CareDokument2 SeitenApollo: Reliability Meets Realism For Nursing or Prehospital CareBárbara BabNoch keine Bewertungen
- NDT 3 429Dokument13 SeitenNDT 3 429Mohammed AldaffaieNoch keine Bewertungen
- Controversias en El Manejo de Las Fracturas Abiertas (2014)Dokument7 SeitenControversias en El Manejo de Las Fracturas Abiertas (2014)J. Adrian NogueraNoch keine Bewertungen
- Pharmaceutical Assasination (Partial)Dokument14 SeitenPharmaceutical Assasination (Partial)jamie_clark_2100% (2)
- Autism AlarmDokument2 SeitenAutism AlarmUmair KaziNoch keine Bewertungen
- Prospect Frisium in EnglezaDokument4 SeitenProspect Frisium in EnglezaTanasa AdrianNoch keine Bewertungen
- Text Book of Sarcoidosis With Homeopathy TreatmentDokument107 SeitenText Book of Sarcoidosis With Homeopathy TreatmentDr. Rajneesh Kumar Sharma MD Hom100% (4)
- 00300-2019 FullDokument10 Seiten00300-2019 FullFitrikarnoNoch keine Bewertungen
- NCP (Rheumatic Heart Disease)Dokument2 SeitenNCP (Rheumatic Heart Disease)Jenny Ajoc75% (4)
- Nutrients: Anemia of Chronic Diseases: Wider Diagnostics-Better Treatment?Dokument17 SeitenNutrients: Anemia of Chronic Diseases: Wider Diagnostics-Better Treatment?Gufront MustofaNoch keine Bewertungen
- FJMCW Lahore MbbsDokument9 SeitenFJMCW Lahore MbbsRayan ArhamNoch keine Bewertungen
- Androgenetic Alopecia and Current Methods of TreatmentDokument4 SeitenAndrogenetic Alopecia and Current Methods of TreatmentPamela TrujilloNoch keine Bewertungen
- Management of The Urologic Sepsis SyndromeDokument10 SeitenManagement of The Urologic Sepsis SyndromeNur Syamsiah MNoch keine Bewertungen
- HYPETHYROIDISM NURSING CARE PLANDokument6 SeitenHYPETHYROIDISM NURSING CARE PLANTrisha Joyce MadriagaNoch keine Bewertungen