Beruflich Dokumente
Kultur Dokumente
A Review of Root Resorption in Orthodontics PDF
Hochgeladen von
RahulLife'sOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
A Review of Root Resorption in Orthodontics PDF
Hochgeladen von
RahulLife'sCopyright:
Verfügbare Formate
Review articles Annals and Essences of Dentistry
10.5368/aedj.2015.7.1.4.2
A REVIEW OF ROOT RESORPTION IN ORTHODONTICS
1 1
Venkatesh Nettam Postgraduate student
2 2
Prasad Mandava Professor and Head
3 3
Gowri Sankar Singaraju Professor
4 4
Vivek Reddy Ganugapanta Senior lecturer
1-4
Department of Orthodontics, Narayana Dental College, Nellore, Andhra Pradesh, India.
ABSTRACT: Root resorption is unavoidable, unwanted and undesirable consequence of the orthodontic tooth movement.
This paper describes the various causes, types and classification of root resorption during orthodontic treatment
KEYWORDS: Orthodontics, Tooth Movement, Root resorption.
INTRODUCTION
Bone is not necessarily the only hard tissue The principle cellular elements in the PDL are
resorbed during orthodontic tooth movement. Root undifferentiated mesenchymal cells and their progeny in
resorption involving cementum and dentin can be an the form of fibroblasts and osteoblasts. Remodelling and
1
unfavourable sequel to orthodontic procedures . Apical recontouring of the bony socket and the cementum of the
root resorption is one of the most common iatrogenic root is also constantly being carried out, though on a
6
problems associated with orthodontic treatment. It is smaller scale, as a response to normal function .
becoming an increasingly more serious problem from a
2 6
medico legal stand point . Response to Normal Function : During masticatory
function, the teeth and periodontal structures are
Root shortening as a result of external resorption is a well- subjected to intermittent heavy forces. When a tooth is
documented possible side effect of orthodontic treatment. subjected to heavy loads of this type, quick displacement
It is irreversible, difficult to predict and can be sufficiently of the tooth within the PDL space is prevented by the
extensive to cast doubt on the overall benefit to the patient incompressible tissue fluid. Instead the force is transmitted
3
of an otherwise successful orthodontic treatment .Root to the alveolar bone, which bends in response. Bone
resorption is undesirable because it can affect the long- bending in response to normal function generates
term viability of the dentition, and reports in the literature piezoelectric currents, which appear to be an important
indicate that patients undergoing orthodontic treatment are stimulus to skeletal regeneration and repair. This is the
4
more likely to have severe apical root shortening . Bates mechanism by which bony architecture is adapted to
(1856) was the first person to discuss root resorption of functional demands. When pressure on tooth is applied
permanent teeth. Ottolengui (1914) related root resorption for a second, very little of the fluid within the PDL space
directly to orthodontic treatment and mentioned that gets squeezed out. However, if pressure against a tooth is
Schwarzkopf (1887) demonstrated resorbed roots in maintained, the fluid is rapidly expressed and the tooth
extracted permanent teeth. In 1927 root resorption of displaces within the PDL space, compressing the ligament
permanent teeth was a subject of major concern to the itself against adjacent bone. Although the PDL is
orthodontic field. Ketcham, demonstrated with beautifully adapted to resist forces of short duration, it
radiographic evidence, the differences between root shape rapidly loses its adaptive capability as the tissue fluids are
before and after orthodontic treatment. This observation squeezed out of its confined area. Prolonged force, even
initiated a research on histological, clinical and physiologic of low magnitude, produces a different physiologic
5
root resorption occurring during orthodontic treatment . response- remodelling of the adjacent bone. Orthodontic
tooth movement is made possible by the application of
Periodontal and bone response to normal prolonged forces.
function and orthodontic force 6
Effects Of Force Magnitude : When light but prolonged
Each tooth is attached to and separated from the adjacent force is applied to a tooth, blood flow through the partially
alveolar bone by a heavy collageneous supporting compressed PDL decreases as soon as fluids are
6
structure and the periodontal ligament (PDL) . expressed from the PDL space and the tooth moves in its
socket (i.e. in a few seconds). Within a few hours,
Vol. VII Issue 1 Jan– Mar 2015 23
Review articles Annals and Essences of Dentistry
resulting change in the chemical environment produces a PDL is marked by the contact and the clast cells attack
different pattern of cellular activity. Animal experiments this marked cementum when the PDL area is repaired.
indicate that increased levels of cyclic adenosine This observation helps explain why heavy continuous
monophosphate (AMP), the “second messenger” appear orthodontic force can lead to severe root resorption.
after about 4 hours of sustained pressure. If removable
appliances are worn less than 4 to 6 hours per day, it will PROCESS OF ROOT RESORPTION
produce no orthodontic effects.
Resorption of deciduous roots during permanent
Experiments have shown that prostaglandin and tooth eruption is a necessary process that eventually
interleukin –1 beta levels increase within the PDL within a results in the exfoliation of the deciduous tooth in
short time after the application of pressure, and it now anticipation of the arrival of its permanent successor.
seems clear that prostaglandin E is an important mediator However, root resorption that occurs in permanent teeth is
of the cellular response. Changes in cell shape probably an unwanted process and is considered pathologic (Bates
7
play a role. There is some evidence that prostaglandins 1856) . The publications of Wehrbein et al made
are released when cells are mechanically deformed. Since substantial contributions to the research concerning OIIRR
drugs of various types can affect both prostaglandin levels in humans. These authors discussed different grades of
and other potential chemical messengers, it is clear that root resorption in detail, mainly in terms of the close
pharmacologic modification of the response to orthodontic proximity of the root to the cortical nonmetaplastic bones,
force is more than just a theoretic possibility. as well as other pathologic phenomena such as
8
Prostaglandin E has the interesting property of stimulating dehiscence and fenestrations .
both osteoclastic and osteoblastic activity, making it 8
particularly suitable as a mediator of tooth movement. If The Cellular Process
parathyroid hormone is injected, osteoclasts can be
induced in only a few hours, but the response is much The studies in mice and rats conducted by Brudvik
slower when mechanical deformation of the PDL is the and Rygh confirmed that Orthodontically Induced
stimulus. The course of the events is different if the Inflammatory Root resorption (OIIR) is a part of the
sustained force against the tooth is great enough to totally hyaline zone elimination process. The first cells to be
occlude blood vessels and cut off the blood supply to an involved in this necrotic tissue removal are cells that are
area within the PDL, When this happens, rather than cells negative for tartrate resistance acid phosphatase (TRAP)
within the compressed area of the PDL being stimulated to and that have no ruffled borders. These are Macrophage-
develop into osteoclasts, a sterile necrosis starts within the like cells, which are most probably activated by signals
compressed area. Because of its histological appearance coming from the sterile necrotic tissue, the result of the
as the cells disappear; an avascular area in the PDL orthodontic force application. As described by Brudvik and
traditionally has been referred to as hyalinized. When this Rygh, the initial elimination process takes place at the
happens, remodeling of bone bordering the necrotic area periphery of the hyaline zone, where blood supply to the
of the PDL must be accomplished by cells derived from periodontal ligament exists is even increased. During
adjacent undamaged areas. After a delay of several days, removal of the hyaline zone, the nearby outer surface of
cellular elements begin to invade the necrotic (hyalinized) the root, which consists of the cementoblast layer covering
area. More importantly, osteoclasts appear within the the cementoid, can be damaged, thus exposing the
adjacent bone marrow spaces and begin an attack on the underlying highly dense mineralized cementum. It is
underside of the bone immediately adjacent to the necrotic possible that the orthodontic pressure itself directly
PDL area. This process is appropriately described as damages the outer root surface layers in such a way that
undermining resorption, since the attack is from the there is a need for their removal as well. The resorption
underside of the lamina dura. When hyalinization and process continues until no hyaline tissue is present and/or
undermining resorption occur, an unwanted delay in tooth the force level decreases. The extent of root resorption
movement results. This is caused first by a delay in was increased only when force reactivation was performed
stimulating differentiation of cells within the marrow at the peak presence of osteoclast count in the involved
spaces, and second because considerable thickness of region (day 4). Idiopathic root resorption is most frequently
bone must be removed from the underside before any found at the apex followed by mesial, buccal, distal and
tooth movement can take place. The PDL response is lingual surfaces. Small differences were noted between
determined not by force alone, but by force per unit area, right and left sides, or between mandibular and maxillary
or pressure. The different time course of tooth movement teeth. More resorption areas were seen on molars since
when frontal resorption is compared with undermining their total surface area is greater than that of other teeth.
resorption is shown in diagram(Fig 1).
Factors affecting root resorption
7 9
Effects On Root Structures:Thomas M. Graber has Naphtali Brezniak, Atalia Wasserstein (1993) have
mentioned that according to Rygh and his co-workers, described the following factors responsible for root
cementum adjacent to hyalinised (necrotic) areas of the resorption.
Vol. VII Issue 1 Jan– Mar 2015 24
Review articles Annals and Essences of Dentistry
9
I) BIOLOGIC FACTORS: NAPHTALI BREZNIAK ET AL have published three types
1) Individual susceptibility of external root resorption originally given by Andreasen:-
2) Genetics
3) Systemic factors i)Surface resorption: - Surface resorption is a self-limiting
4) Nutrition process, usually involving small outlining areas followed
5) Chronologic Age by spontaneous repair from adjacent intact parts of the
6) Dental age periodontal ligament.Root resorption after orthodontic
7) Gender treatment is surface resorption.
8) The presence of root resorption before
orthodontic treatment ii) Inflammatory resorption: In inflammatory resorption,
9) Habits initially root resorption occurs up to dentinal tubules of an
10) Tooth structure infected necrotic pulpal tissue or an infected leukocyte
11) Previously traumatized teeth zone.There are two types of inflammatory resorption.
12) Endodontically Treated Teeth
13) Alveolar bone density a) Transient inflammatory resorption
14) Types of malocclusion It occurs when the stimulation to the damage is
15) Specific tooth vulnerability to root resorption minimal and for a short period. This defect is
usually undetected radiographically and is repaired
II) MECHANICAL FACTORS by a cementum-like tissue.
1) Orthodontic appliances: -
A. Fixed versus removable b) Progressive inflammatory resorption
B. Begg versus edgewise When stimulation for damage is for longer period,
C.Magnets ankylosis occurs. Ankylosis is the result of an
D.Inter maxillary elastics extensive necrosis of the periodontal ligament with
2) Extraction versus nonextraction formation of bone into a denuded area of the root
3) Serial extractions surface. Since the tooth becomes a part of the
4) Other appliances bone, normal remodeling process will gradually
5) Types of orthodontic tooth movement lead to a complete destruction of the tooth by the
6) Orthodontic force bone.
7) Continuous versus intermittent force
8) Jiggling and occlusal trauma iii) Replacement resorption: - In replacement resorption,
9) The extent of tooth movement bone replaces the resorbed tooth material that leads to
III) BIOLOGIC AND MECHANICAL FACTORS:- ankylosis.Replacement resorption is rarely seen during or
after orthodontic treatment.
1) Treatment duration
2) Relapse
3) Root resorption after appliance removal
IV) OTHER CONSIDERATIONS:-
1) Teeth vitality.
2)Loss of crestal bone and tooth stability
CLASSIFICATION OF ROOT RESORPTION
10
ACCORDING TO SHAFER, HINE AND LEVY ,
resorption of root occurs in many circumstances other
than the normal process associated with shedding of
deciduous teeth. Resorption of root may occur either on
the external surface or internal surface of the root. Root
resorption is mainly of two types
1.External root resorption:- This resorption mainly
occurs as a result of a tissue reaction in the periodontal or
pericoronal tissues. Following are the few conditions: -
a. Periapical inflammation Fig. 1.Diagrammatic representation of the time
b. Reimplantation of teeth course of tooth movement with
c. Tumors or cysts frontal resorption vs. undermining resorption.
d. Excessive mechanical or occlusal forces
e. Impaction of teeth
f. Idiopathic
Vol. VII Issue 1 Jan– Mar 2015 25
Review articles Annals and Essences of Dentistry
incremental line is seen which is characterized by a slim
deposit of cellular cementum with a deficient width in
comparison with the sound width of all consecutive
incremental lines.
3) Peak phase (14 to 28 days): - This phase is seen with
successive first and second incremental lines because of
spurt in matrix formation as defined by an increase in
width. This phase is also characterized by initial
incorporation of periodontal fiber bundle into intrinsic
cementum matrix.
4) Steady phase (42 to 56 days): - This phase included
rest of the incremental lines which were of equal width,
indicating a steady deposit phase of mix fibrillar
cementum.
5) Retreating phase (70 days): - This phase was seen
1 2 3 4 during relapse period (after removal of retention
Fig 2:- Grading scale for apical root resorption.
appliance). In this phase only first and second incremental
lines were seen. This phase may be attributed to the
conversion of the former pressure site of active treatment
period into the tension side of the relapse period as a
2. Internal resorption: - consequence of appliance removal. This conversion led to
10
According to Shafer, Hine and Levy internal an increase in osteogenesis on the new tension site along
resorption mainly arises from inflammatory with a decrease in cementogenesis.
hyperplasia of pulp. This begins centrally within the
9
tooth. The cause of the pulpal inflammation and Naphtali Brezniak and Atlia Wasserstein have mentioned
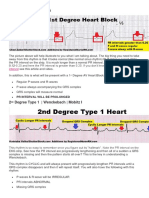
subsequent resorption of the root. David N. that according to Henry and Weinmann, repair can be
11
Ramingtonet al in 1989 described the following classified as,
grading scale for apical root resorption as shown in
Fig 2. 1) Anatomic repair: - In this type of repair the root
surface gets restored to its original contour.
Grade-0: Normal apical contour, same length as
- pretreatment. 2) Functional repair: - In this type of repair, a thin
Grade-1: Apical irregularity, same length as layer of repair cementum covers the exposed
- pretreatment. dentine, resulting in a deficient root outline. In
Grade-2: Apical root resorption of less than 2mm. both types, the periodontal ligament (PDL) was
- restored to its original width.
Grade-3: Apical root resorption more than 2mm,
- less than one third of original root DIAGNOSTIC AIDS
length. According to Naphtali Brezniak and Atalia
9 ,
Grade-4: Apical root resorption more than one Wasserstein (1993) radiographs are commonly used as a
- third of original root length diagnostic aid for investigating root resorption. Following
are the various radiographic techniques used as
REPAIR PROCESS OF ROOT RESORPTION diagnostic aids for assessing root resorption:
1) Periapical bisecting angle.
According to the appearance of these incremental lines, 2) Periapical paralleling.
histologicaly the repair process is divided into following 3) Orthopantomogram.
12
phases 4) Cephalogram.
5) Lamiogram.
1) Early lag phase: -In this phase no cementum 6) Computed tomography.
apposition was seen which can be explained by the
dissipation of residual forces and the replacement of A biochemical assay could potentially offer advantages of
clastic cell population by blastic cell population. 1) sensitivity, 2) non-invasiveness, 3) No radiation
exposure, 4) information on the stage of resorptive activity
2) Incipient phase (First 14 days): - This phase implies a and Severity, 5) possibly identifying at-risk individuals, 6)
transitional stage from no apposition (lag phase) to active reducing the time between clinical onset and Usual
deposition stages of repair cementum. In this phase, first clinical diagnosis and prognosis, 7) predicting subsequent
Vol. VII Issue 1 Jan– Mar 2015 26
Review articles Annals and Essences of Dentistry
clinical course and diagnosis 8) implementing alterations 7. Prakash A, Shanker DG, Adit A, Nitin D, and Sonali
in therapy, 9) assessment of the actual response to R. Burning of roots in orthodontics-reviewing every
13
treatment alterations. Balducciet al. (2006) explored the aspect. UnivJ Med Dent 2013;2: 1-9.
presence of dentine sialoprotein (DSP),dentine 8. Brezniak N, Wasserstein A. Orthodontically Induced
phosphoprotein (DPP), and dentine matrix protein-1 Inflammatory Root Resorption. Part I: The basic
(DMP-1) in the GCF, concluded that the use of DSP and science aspect. Angle Orthod 2002 ;72:175-9.
DPP as biomarkers were suitable alternatives for 9. Brezniak N, Wasserstein A. Root resorption after
monitoring root resorption during orthodontic tooth orthodontic treatment: part-2. Literature review. Am J
14
movement . RANKL and osteoprotegerin (OPG) in OrthodDentofacialOrthop 1993 ;103:138-46.
periodontal tissues are important determinants for the 10. Rajendran R, Sivapathasundharam B, Shafer WG,
regulation of bone remodelling as well as root resorption Hine MK, Levy BM. Shafer’s Textbook Of Oral
during orthodontic tooth movement. Pathology. Regressive alterations of the teeth.
Seventh edition.2012:571-90.
Zhang et al demonstrated that compressive force 11. Remington DN, Joondeph DR, Artun J, Riedel
stimulates gene expression in the IL-17 and IL-17 (IL-17R) RA, Chapko MK. Long-term evaluation of root
in MC3T3-E1 cells, and also results in the induction of resorption occurring during orthodontic treatment.
15
osteoclastogenesis. Immunoreactivities for interleukin-6 Am J OrthodDentofacialOrthop 1989;96:43-6.
and interleukin -17 were detected in gingival crevicular 12. Vardimon AD, Graber TM, Pitaru S. Repair process
16
fluid of subjects with severe root resorption. Hayashi et al of external root resorption subsequent to palatal
demonstrated that heavy orthodontic force induced expansion treatment. Am J
expression of Th17, IL-17 and IL-17R in rat root resorbed OrthodDentofacialOrthop 1993;103:120-30.
tissue on day7. Therefore, IL-17 and Th17 cells may 13. Tyrovola JB, Perrea D, Halazonetis DJ, Dontas
15
aggravate the process of OIIRR. I, Vlachos IS, Makou M.
Relation of soluble RANKL and osteoprotegerin level
CONCLUSION s in blood and gingival crevicular fluid to the degree
In post-orthodontic treatment, all permanent teeth of root resorption after orthodontic tooth movement. J
may show microscopic root resorption that is clinically Oral Sci 2010 ;52:299-311.
insignificant and radiographically undetected. Root 14. Estrela C, Bueno MR, De Alencar AH, Mattar
resorption of permanent teeth is a probable consequence R, ValladaresNeto J, Azevedo BC, De Araújo Estrela
of orthodontic force and active tooth movement. The CR. Method to evaluate inflammatory root
incidence of reported root resorption during orthodontic resorption by using cone beam computed
treatment varies widely among investigators. Most studies tomography. J Endod 2009 ;35:1491-7.
agree that the root resorption process ceases once the 15. Yamaguchi T, Nariyasu T, Hayashi N, Nakajima R,
active treatment is terminated. The question if there is any Fujita S, Yamaguchi M, And Kasai K. IL-6 and IL-17
ideal (optimal) force to move teeth without root resorption in Gingival Crevicular Fluid during Orthodontic Root
and whether root resorption is predictable remains Resorption. Int J Oral-Med Sci 2012; 10:247-54.
unanswered. 16. Rody WJ Jr, Holliday LS, McHugh KP, Wallet
SM, Spicer V, Krokhin O.
Mass spectrometry analysis of gingival crevicular flui
References d in the presence of external root resorption. Am J
OrthodDentofacialOrthop 2014; 145:787-98.
1. Harry MR, Sims MR. Root resorption in bicuspid
intrusion: A scanning electron microscope study.
Angle Orthod 1982;52:235-58. Corresponding Author
2. Copeland S, Green LJ. Root resorption in maxillary
central incisors following active orthodontic
treatment. Am J Orthod 1986;89:51-5.
3. Linge BO, Linge L. Apical root resorption in upper
Venkatesh Nettam
anterior teeth. Eur J Orthod 1983;5:173-83.
Post Graduate Student,
4. Weltman B, Vig KW, Fields HW, Shanker S, Kaizar
Department of Orthodontics, Narayana
EE. Root resorption associated with orthodontic tooth
Dental College, Nellore, Andhra
movement: A systematic review. Am J
Pradesh, India.
OrthodDentofacialOrthop 2010;137:462-76. Ph no. 9493223512
5. Brezniak N, Wasserstein A. Root resorption after e-mail: venkateshnettam@gmail.com
orthodontic treatment: Part-1.Literature review. Am J
OrthodDentofacialOrthop 1993;103:62-6.
6. Proffit WR, Fields HW Jr, Sarver DM and Ackerman
JL: Contemporary Orthodontics. The biologic basis
of orthodontic therapy. Fifth edition 2013:278-311.
Vol. VII Issue 1 Jan– Mar 2015 27
Das könnte Ihnen auch gefallen
- Cellular, Molecular, and Tissue-Level Reactions To Orthodontic ForceDokument32 SeitenCellular, Molecular, and Tissue-Level Reactions To Orthodontic Forcecarlina_the_bestNoch keine Bewertungen
- Oral Wound Healing: Cell Biology and Clinical ManagementVon EverandOral Wound Healing: Cell Biology and Clinical ManagementHannu LarjavaNoch keine Bewertungen
- Moving The TeethDokument117 SeitenMoving The TeethThirunavukkarasu Srinivasan100% (2)
- THE ORTHODONTICS EFFECTIVE ROLE IN PROSTHODONTIC FIELDDokument31 SeitenTHE ORTHODONTICS EFFECTIVE ROLE IN PROSTHODONTIC FIELDHamza BelhajNoch keine Bewertungen
- 18 Interrelationship of Orthodontics With Periodontics and Restorative DentistryDokument25 Seiten18 Interrelationship of Orthodontics With Periodontics and Restorative DentistrySriAduri100% (1)
- Efficient Treatment: Solutions ForDokument28 SeitenEfficient Treatment: Solutions ForRoss Sacravilca LaderaNoch keine Bewertungen
- Usefulness of Occlusal SplintsDokument12 SeitenUsefulness of Occlusal SplintsFransisca Dwi A PNoch keine Bewertungen
- January 2018 1516198794 146 PDFDokument1 SeiteJanuary 2018 1516198794 146 PDFGaby ZapataNoch keine Bewertungen
- Mandibular Incisor Extraction TherapyDokument10 SeitenMandibular Incisor Extraction TherapyLeonardo LamimNoch keine Bewertungen
- Ghafari (1997) Emerging Paradigms in Orthodontics - An EssayDokument8 SeitenGhafari (1997) Emerging Paradigms in Orthodontics - An EssayMaja Maja BułkaNoch keine Bewertungen
- Pain ManagementDokument44 SeitenPain ManagementSaherish FarhanNoch keine Bewertungen
- Diagnostic Limitations of Cephalometrics in OrthodonticsDokument6 SeitenDiagnostic Limitations of Cephalometrics in OrthodonticsDevata RaviNoch keine Bewertungen
- Principles of The Alexander DisciplineDokument5 SeitenPrinciples of The Alexander DisciplineSarah Fauzia SiregarNoch keine Bewertungen
- Orthodontics Food N DietDokument4 SeitenOrthodontics Food N DietnatashaNoch keine Bewertungen
- Activator HeadgearDokument9 SeitenActivator HeadgearThendral DevanathanNoch keine Bewertungen
- Role of Bone Screw (Izc & BSS) in Skeletal Anchorage System - A Review ArticleDokument5 SeitenRole of Bone Screw (Izc & BSS) in Skeletal Anchorage System - A Review ArticleAlvaro ChacónNoch keine Bewertungen
- Risk and Limitations of Orthodontic TreatmentDokument41 SeitenRisk and Limitations of Orthodontic TreatmentAjay ChhetriNoch keine Bewertungen
- Biomechanics of TorqueDokument8 SeitenBiomechanics of TorquehemaadriNoch keine Bewertungen
- Vertical Skeletal DysplasiaDokument119 SeitenVertical Skeletal DysplasiaAshish Mathew0% (1)
- Finishing Orthodontic Treatment for Optimal Esthetics, Function and StabilityDokument13 SeitenFinishing Orthodontic Treatment for Optimal Esthetics, Function and StabilityMargarita Lopez Martinez100% (1)
- Understanding the History and Mechanisms of the Activator ApplianceDokument91 SeitenUnderstanding the History and Mechanisms of the Activator ApplianceCarlosAndresPabonCortesNoch keine Bewertungen
- Journal Club1 / Orthodontic Courses by Indian Dental AcademyDokument19 SeitenJournal Club1 / Orthodontic Courses by Indian Dental Academyindian dental academyNoch keine Bewertungen
- Fundamentals of Occlusion and RestorativeDokument9 SeitenFundamentals of Occlusion and RestorativePhạm Văn KhoaNoch keine Bewertungen
- TADSDokument8 SeitenTADSDIANA PAOLA FONTECHA GONZÁLEZNoch keine Bewertungen
- Bond FailureDokument3 SeitenBond Failuredentist97Noch keine Bewertungen
- Molares InclinadosDokument13 SeitenMolares Inclinadosmaria jose peña rojas100% (1)
- Skeletally-Anchored Maxillary Expansion: Promising Effects and LimitationsDokument23 SeitenSkeletally-Anchored Maxillary Expansion: Promising Effects and LimitationsAya ElsayedNoch keine Bewertungen
- Myth in OrthoDokument7 SeitenMyth in Orthosurendra334Noch keine Bewertungen
- Torque in Orthodontics ReviewDokument3 SeitenTorque in Orthodontics ReviewchaitreeNoch keine Bewertungen
- Clear Aligners: An Insight To BiomechanicsDokument12 SeitenClear Aligners: An Insight To BiomechanicsIJAR JOURNALNoch keine Bewertungen
- Development of Dental OcclusionDokument89 SeitenDevelopment of Dental OcclusionMothi KrishnaNoch keine Bewertungen
- Smile Analysis: A Review Part IIDokument4 SeitenSmile Analysis: A Review Part IIGustavoAndresGarciaNoch keine Bewertungen
- Orthodontic Indices OverviewDokument10 SeitenOrthodontic Indices OverviewBhavikPatelNoch keine Bewertungen
- AMERICAN BOARD OF ORTHODONTICS OBJECTIVE GRADING SYSTEMDokument11 SeitenAMERICAN BOARD OF ORTHODONTICS OBJECTIVE GRADING SYSTEMNasira Adnan100% (1)
- White Spot Lesion Formation Prevention TreatmentDokument9 SeitenWhite Spot Lesion Formation Prevention TreatmentRubén Godoy CisternasNoch keine Bewertungen
- Comparison Between Surgically-Assisted Rapid Palatal Expansion (Sarpe) and Miniscrew-Assisted Rapid Palatal Expansion (Marpe) A Systematic ReviewDokument28 SeitenComparison Between Surgically-Assisted Rapid Palatal Expansion (Sarpe) and Miniscrew-Assisted Rapid Palatal Expansion (Marpe) A Systematic Reviewaa bbNoch keine Bewertungen
- ARCH EXPANSIONDokument33 SeitenARCH EXPANSIONGareth BaleNoch keine Bewertungen
- Intrusion MechanicsDokument31 SeitenIntrusion Mechanicsaa bbNoch keine Bewertungen
- American Journal QF Orthodontics: Facial Types Associated With Class II MalocclusionsDokument18 SeitenAmerican Journal QF Orthodontics: Facial Types Associated With Class II MalocclusionsKhyati Gupta100% (1)
- Surgical OrthodonticsDokument5 SeitenSurgical OrthodonticsInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Space AnalysisDokument43 SeitenSpace AnalysismarieNoch keine Bewertungen
- Journal Club List Second Year Postgraduates: Department of Orthodontics and Dentofacial OrthopedicsDokument6 SeitenJournal Club List Second Year Postgraduates: Department of Orthodontics and Dentofacial OrthopedicsMariyam0% (1)
- 3-Molar Distalization With Modified Palatal DistalizerDokument8 Seiten3-Molar Distalization With Modified Palatal DistalizerJunaid Israr - OrthodonticsNoch keine Bewertungen
- Management of Vertical Maxillary ExcessDokument24 SeitenManagement of Vertical Maxillary ExcesssweetieNoch keine Bewertungen
- Sterilization in OrthodonticsDokument121 SeitenSterilization in OrthodonticsSwati PawarNoch keine Bewertungen
- Behavioural Factors in Orthodontic TreatmentDokument96 SeitenBehavioural Factors in Orthodontic TreatmentarshabharataNoch keine Bewertungen
- Non XNDokument9 SeitenNon XNNaveenNoch keine Bewertungen
- Orthodontic Management of A Maxillary Midline Diastema Using Beggs Mechanics Case ReportDokument3 SeitenOrthodontic Management of A Maxillary Midline Diastema Using Beggs Mechanics Case ReportEditor IJTSRDNoch keine Bewertungen
- Bonding and Debonding From Metal To Ceramic: Research and Its Clinical ApplicationDokument13 SeitenBonding and Debonding From Metal To Ceramic: Research and Its Clinical Applicationgriffone1Noch keine Bewertungen
- Diagnostic Imaginf of TMJ - A ReviewDokument4 SeitenDiagnostic Imaginf of TMJ - A ReviewRhea RejiNoch keine Bewertungen
- Kinzer Kokich-Managing Congenitally Missing Lateral Incisors Part I Canine Substitution PDFDokument5 SeitenKinzer Kokich-Managing Congenitally Missing Lateral Incisors Part I Canine Substitution PDFAdrian Silva SantosNoch keine Bewertungen
- Tads 1Dokument6 SeitenTads 1travolta0Noch keine Bewertungen
- Bolton Analysis According To ABODokument54 SeitenBolton Analysis According To ABOkerminkNoch keine Bewertungen
- American Journal of Orthodontics and Oral Surgery study on Frankfort-mandibular plane angleDokument56 SeitenAmerican Journal of Orthodontics and Oral Surgery study on Frankfort-mandibular plane angleAnonymous 1uVifBp6100% (1)
- Retention Management Decisions A Review of Current Evidence and Emerging Trends 2017 Seminars in OrthodonticsDokument8 SeitenRetention Management Decisions A Review of Current Evidence and Emerging Trends 2017 Seminars in Orthodonticsdruzair007Noch keine Bewertungen
- A New Spring For Torque CorrectionDokument1 SeiteA New Spring For Torque CorrectionDorian RiosNoch keine Bewertungen
- Creekmore1993 1 PDFDokument13 SeitenCreekmore1993 1 PDFsmritiNoch keine Bewertungen
- Combined Surgical and Orthodontic TreatmentDokument7 SeitenCombined Surgical and Orthodontic TreatmentAnonymous GyqTkXMwMNoch keine Bewertungen
- Evolution, Epidemiology and Etiology of Temporomandibular Joint DisordersDokument6 SeitenEvolution, Epidemiology and Etiology of Temporomandibular Joint DisordersakNoch keine Bewertungen
- ISSN 2347-5579: 0.018" Versus 0.022" Bracket Slot Systems in Orthodontics: A ReviewDokument4 SeitenISSN 2347-5579: 0.018" Versus 0.022" Bracket Slot Systems in Orthodontics: A ReviewRahulLife's100% (1)
- 242418KUDokument17 Seiten242418KURahulLife'sNoch keine Bewertungen
- LEUKAEMIA AND ORTHDONTICS by AlmuzianDokument3 SeitenLEUKAEMIA AND ORTHDONTICS by AlmuzianRahulLife'sNoch keine Bewertungen
- Madhya Pradesh Medical Science University Jabalpur: Statement of MarksDokument1 SeiteMadhya Pradesh Medical Science University Jabalpur: Statement of MarksRahulLife'sNoch keine Bewertungen
- Skeletal and Soft Tissue Point A and B Changes Following Orthodontic Treatment of Nepalese Class I Bimaxillary Protrusive PatientsDokument6 SeitenSkeletal and Soft Tissue Point A and B Changes Following Orthodontic Treatment of Nepalese Class I Bimaxillary Protrusive PatientsRahulLife'sNoch keine Bewertungen
- Failure Rates For Stainless Steel Versus Titanium Alloy Infrazygomatic Crest Bone Screws: A Single-Center, Randomized Double-Blind Clinical TrialDokument7 SeitenFailure Rates For Stainless Steel Versus Titanium Alloy Infrazygomatic Crest Bone Screws: A Single-Center, Randomized Double-Blind Clinical TrialRahulLife'sNoch keine Bewertungen
- PROBLEMS LIST, AIMS & TREATMENT PLAN by AlmuzianDokument3 SeitenPROBLEMS LIST, AIMS & TREATMENT PLAN by AlmuzianRahulLife'sNoch keine Bewertungen
- Surgically Assisted Rapid Palatal Expansion: A Literature ReviewDokument13 SeitenSurgically Assisted Rapid Palatal Expansion: A Literature ReviewRahulLife'sNoch keine Bewertungen
- Applications of Nanotechnology in Orthodontics and Its Future Implications: A ReviewDokument6 SeitenApplications of Nanotechnology in Orthodontics and Its Future Implications: A ReviewRahulLife'sNoch keine Bewertungen
- The K Test and Condylar Test: Measuring Orthodontic ProgressDokument5 SeitenThe K Test and Condylar Test: Measuring Orthodontic ProgressRahulLife'sNoch keine Bewertungen
- 16 Anjali Gheware PDFDokument4 Seiten16 Anjali Gheware PDFRahulLife'sNoch keine Bewertungen
- 16 Anjali GhewareDokument4 Seiten16 Anjali GhewareRahulLife'sNoch keine Bewertungen
- Prolonged Retention, Ankylosis and Infraocclusion of Deciduous Teeth Ok OkDokument5 SeitenProlonged Retention, Ankylosis and Infraocclusion of Deciduous Teeth Ok OkRahulLife'sNoch keine Bewertungen
- Comparison of-WPS OfficeDokument1 SeiteComparison of-WPS OfficeRahulLife'sNoch keine Bewertungen
- Article-Pdf-N. RAGHUNATH NITIN V. MURLIDHAR KANHU CHARAN SAHOO-204 PDFDokument7 SeitenArticle-Pdf-N. RAGHUNATH NITIN V. MURLIDHAR KANHU CHARAN SAHOO-204 PDFRahulLife'sNoch keine Bewertungen
- Houston 1989Dokument5 SeitenHouston 1989RahulLife'sNoch keine Bewertungen
- 9 EJBPSorthoandrootresorptionDokument8 Seiten9 EJBPSorthoandrootresorptionRahulLife'sNoch keine Bewertungen
- Cephalometrics For Orthognathic SurgeryDokument11 SeitenCephalometrics For Orthognathic SurgeryGowri ShankarNoch keine Bewertungen
- Biological Aspects of Orthodontic Tooth MovementDokument6 SeitenBiological Aspects of Orthodontic Tooth MovementRahulLife'sNoch keine Bewertungen
- Ijodr 4 3 146 150Dokument5 SeitenIjodr 4 3 146 150RahulLife's100% (1)
- Davidovitch1995 PDFDokument6 SeitenDavidovitch1995 PDFRahulLife'sNoch keine Bewertungen
- Davidovitch1995 PDFDokument6 SeitenDavidovitch1995 PDFRahulLife'sNoch keine Bewertungen
- PIIS0889540607007536Dokument13 SeitenPIIS0889540607007536Amina NehaNoch keine Bewertungen
- 24040Dokument4 Seiten24040RahulLife'sNoch keine Bewertungen
- AS5686375790387201512585171069 Content 1Dokument6 SeitenAS5686375790387201512585171069 Content 1RahulLife'sNoch keine Bewertungen
- Resorption in OrthodonticsDokument6 SeitenResorption in OrthodonticsRahulLife'sNoch keine Bewertungen
- Template Analysis PDFDokument49 SeitenTemplate Analysis PDFRahulLife'sNoch keine Bewertungen
- Overlays JCODokument5 SeitenOverlays JCORahulLife'sNoch keine Bewertungen
- Blueprint of LifeDokument42 SeitenBlueprint of Lifesophiehee1234Noch keine Bewertungen
- Yellow Belt Level 01 - Solution - 0Dokument2 SeitenYellow Belt Level 01 - Solution - 0Jo Marie LeeNoch keine Bewertungen
- Introduction To Fitness TrainingDokument25 SeitenIntroduction To Fitness TrainingShailendra Singh ChouhanNoch keine Bewertungen
- Peri Implant Health: Mauricio G. Araujo - Jan LindheDokument7 SeitenPeri Implant Health: Mauricio G. Araujo - Jan LindheCristian CulcitchiNoch keine Bewertungen
- Chapter 31 - Assessment and Management of Patients With Vascular DisordersDokument7 SeitenChapter 31 - Assessment and Management of Patients With Vascular DisordersMichael Boado100% (1)
- Arab Board Orthopedic Exam June 2013Dokument35 SeitenArab Board Orthopedic Exam June 2013Nasser AlbaddaiNoch keine Bewertungen
- StomachDokument16 SeitenStomachnevelle4667Noch keine Bewertungen
- Hoa Silver Edition Manual V1 5-0-120308 enDokument23 SeitenHoa Silver Edition Manual V1 5-0-120308 enAlex KrobbachNoch keine Bewertungen
- Learning Theories of PersonalityDokument13 SeitenLearning Theories of Personalitypavitra_madhusudanNoch keine Bewertungen
- Biochemistry Notes-Study GuideDokument3 SeitenBiochemistry Notes-Study Guidegmanb5100% (2)
- 11.transportation in Plants & AnimalsDokument51 Seiten11.transportation in Plants & AnimalsReshma ModhiaNoch keine Bewertungen
- Neuropathic Painn PDFDokument20 SeitenNeuropathic Painn PDFkaktusNoch keine Bewertungen
- Organic Molecules: Chapter 2-3Dokument33 SeitenOrganic Molecules: Chapter 2-3Gissele AbolucionNoch keine Bewertungen
- Neurological Complications in Lumbar Spine SurgeryDokument9 SeitenNeurological Complications in Lumbar Spine SurgeryMimi SyakilaNoch keine Bewertungen
- Cell Biology Test - 70 Possible Points: Prokaryotic and Eukaryotic Cells (2 Points Per Question)Dokument3 SeitenCell Biology Test - 70 Possible Points: Prokaryotic and Eukaryotic Cells (2 Points Per Question)Vienne MonroidNoch keine Bewertungen
- Language and BrainDokument23 SeitenLanguage and Brainalbino100% (1)
- Qualitative Tests for Bile ComponentsDokument8 SeitenQualitative Tests for Bile ComponentsSoh Rodriguez100% (1)
- Pathology of Neurodegenerative DiseasesDokument22 SeitenPathology of Neurodegenerative DiseasesKarel GuevaraNoch keine Bewertungen
- Shaun's 4 Day Muscle Building Split Routine - Muscle & StrengthDokument85 SeitenShaun's 4 Day Muscle Building Split Routine - Muscle & StrengthYoucefNoch keine Bewertungen
- DecongestantsDokument3 SeitenDecongestantskNoch keine Bewertungen
- Cerebral EdemaDokument5 SeitenCerebral EdemaAdilah AdeebNoch keine Bewertungen
- Pediatric DehydrationDokument27 SeitenPediatric DehydrationAbraham ChiuNoch keine Bewertungen
- Understanding 1st, 2nd and 3rd Degree Heart BlocksDokument3 SeitenUnderstanding 1st, 2nd and 3rd Degree Heart BlockslhenNoch keine Bewertungen
- FCA (SA) - Part - II - Past - Papers 10Dokument30 SeitenFCA (SA) - Part - II - Past - Papers 10matentenNoch keine Bewertungen
- GIT - Dr. Allam 2021 PDFDokument47 SeitenGIT - Dr. Allam 2021 PDFMohammedNoch keine Bewertungen
- Individual Behaviour: Biographical CharacteristicsDokument15 SeitenIndividual Behaviour: Biographical Characteristicsapi-3792827Noch keine Bewertungen
- A Presentation On Pantothenic Acid or b5Dokument28 SeitenA Presentation On Pantothenic Acid or b5jainsaketNoch keine Bewertungen
- Role Play KomkepDokument7 SeitenRole Play KomkepSyubban AfifNoch keine Bewertungen
- CH 7 The Nervous SystemDokument4 SeitenCH 7 The Nervous Systemapi-267543553Noch keine Bewertungen
- Haemodialysis CatheterDokument10 SeitenHaemodialysis CatheterRizqi AhmadNoch keine Bewertungen