Beruflich Dokumente
Kultur Dokumente
MCN Partial
Hochgeladen von
Abbeygale Galan0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
52 Ansichten9 SeitenOriginaltitel
mcn.partial (1).docx
Copyright
© © All Rights Reserved
Verfügbare Formate
DOCX, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
52 Ansichten9 SeitenMCN Partial
Hochgeladen von
Abbeygale GalanCopyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 9
BSN 12-D which allows smallest diameters
to move down the birth canal and
HIGH RISK FACTORS pass through the maternal pelvis.
1.Passenger or Fetus Its ability to change its shape is also
2.Passageway or pelvic bones and other important
pelvic structure - eases its passage during
3.Power or uterine contractions labor & delivery
4. Placenta - in response to the pressure exerted
5. Psyche - client’s psychological state by the maternal pelvis & birth canal
HIGH-RISK LABOR AND during labor & delivery
DELIVERYProblems of the Passenger
1. Fetal malposition Fetal Malposition
2. Fetal malpresentation Position- is the relationship of the
Vertex presenting part to a specific quadrant of
presentation a woman’s pelvis.
Brow presentation Fetal Malpositions - are abnormal
Face presentation position of the vertex in relation to the
Occiput posterior maternal pelvis.
3. Fetal Distress Occipito-posterior position
4. Prolapse of the Cord - The most common
TYPES OF PELVIS malposition
1. GYNECOID – normal female Occipito-transverse position
pelvis - Head initially engages
2. ANDROID – male pelvis; narrow correctly but fails
pelvic inlet and outlet to rotate and remains in
3. ANTHROPOID – narrow transverse position.
transverse diameter and larger Positions in Vertex
antero-posterior diameter Presentation (occiput)
4. PLATYPELLOID – inlet is oval Right occipito anterior
and AP diameter is shallow Right occipito posterior
5. PASSENGER Right occipito transverse
Description Left occipito anterior
Refers to the fetus & its ability to Left occipito posterior
move through the passage Left occipito transverse
Affected by several fetal features Positions in Breech Presentation
Fetal Skull (sacrum)
Its size is important as the fetus Right sacroanterior
travels the birth canal Right sacroposterior
The head can flex or extend 45 Right sacrotransverse
degrees and rotate 180 degrees, Left sacroanterior
Left sacroposterior 11. Longer labor due to ineffective
Left sacrotransverse contractions and slow or
Positions in Face Presentation arrested fetal descent
(mentum) 12. Cesarean birth if brow
Right mentoanterior presentation persists
Right mentoposterior 13. Fetus – increased mortality
Right mentotransverse because of cerebral and neck
Left mentoanterior compression and damage to
Left mentoposterior trachea & larynx
Left mentotransverse - facial edema, bruising
Shoulder Presentation (acromion Risks of Face Presentation
process) Increased risk of CPD &
Right scapuloanterior prolonged labor
Right scapuloposterior Increase risk of infection
Right scapulotransverse Cesarean birth
Left scapuloanterior Cephalhematoma
Left scapuloposterior Edema of the face & throat
Left scapulotransverse Fetal Malpresentation
Fetal Malpresentation Types of breech Presentation:
Presentation – describes the body part 1. Complete- thighs of the fetus
that will be first to pass through the are tightly flexed on the
cervix and be delivered abdomen; buttocks and flexed
Fetal Malpresentation is where the legs present first
baby is in difficult position for delivery 2. Frank – hips are flexed but
Types of fetal presentation: legs are extended; buttocks
1. Cephalic- head presents first present first
2. Breech – buttocks or feet 3.Incomplete – one or both hips
presents first partially of fully extended
3. Shoulder – shoulder, iliac crest, Nursing Management (Breech)
hand, or elbow presents first Assess maternal & fetal status- to
4. Fetal Malpresentation promote maternal-fetal physical
5. Types of Cephalic: well being
6. 1. Vertex – head sharply flexed Continuous fetal monitoring-
(Normal) increased risk for cord prolapse
7. 2. Brow- head moderately flexed CBR without BRP
8. 3. Face- head poorly flexed Teaching & information about the
9. 4. Mentum- hyperextension of breech presentation
head; chin presents first Evaluation (Breech)
10. Risks of Brow Presentation
The woman & partner understand Fetal Heart Rate PatternsA. Early
the implications of breech Decelerations
presentation = caused by fetal head compression
Major complications are • Periodic DECREASE in FHR
recognized early & corrective resulting from pressure on the
measures are instituted fetal head during contractions.
The mother and baby have safe B. Late Decelerations
labor & birth = caused by uteroplacental
insufficiency
Fetal Malpresentation • Are smooth, uniform waveforms
Shoulder Presentation – the fetus is that inversely mirror the
lying horizontally in the pelvis contractions, they may drop to
Compound Presentation- prolapse of a below 100 beats/minute.
limb of the fetus alongside the head in a C. Variable Decelerations
cephalic presentation or of one or both = caused by umbilical cord
arms in a breech presentation compression
Fetal Distress • In severe cases the FHR may
HYPOXIA - decelerate below 70beats/minute
Late deceleration appear for more than 30 seconds, with a
Fetal breathing stops slow return to baseline.
Fetal movement ceases • Management:
Fetal tone absent 1. place pt in left-lateral position
• Causes of Fetal DistressCord 2. increased IV flow rate
Prolapse/cord compression 3. administer O2 as per doctors order
• PROM 4. discontinue oxytocin infusion (induce
• Oligohydramnios labor)
• Meconium Staining Nursing Intervention:
• Maternal complication – DM, 1. continue monitoring contractions and
anemia, infection record FHR.
• Preterm/IUGR fetus 2. anticipate amnioinfusion for repetitive
• How it is detected? Special test variable decelerations
and monitoring procedures 3. If rate falls below 70beats/minute
> X-ray pelvimetry reveals persists for more than 60 seconds, the
malpositioning doctor may choose to intervene.
> Ultrasonography shows pelvic masses 4. Prepare double set-up delivery
that interfere with vaginal birth Prolapse of the Umbilical Cord
> Auscultation of FHR (by fetoscope, A loop of the umbilical cord slips
Doppler unit, or electronic fetal monitor) down in front of the presenting
determines fetal intolerance of labor. fetal part
Prolapse may occur anytime after presenting part in the woman's vagina
the membranes rupture if the (to keep pressure off the cord) until
presenting part is not fitted firmly delivered by CS.
into the cervix. 5. If prolapsed cord is exposed to room
Causes: Premature rupture of air (drying will begin- leading to atrophy
membranes of the umbilical vessels).
Fetal presentation other than • Don't push the cord back to
cephalic vagina (may add to compression
Tends to occur most often with by knotting/kinking), instead
the ff conditions: cover exposed portion with sterile
Placenta previa sponge soaked in sterile saline to
Intrauterine tumors preventing the prevent drying.
presenting part from engaging Nursing Interventions:
A small fetus Inform client and watchers about
CPD preventing firm engagement the additional procedures &
Hydramnios techniques that may be
ASSESSMENT: necessary during the delivery
= cord may be felt as the process.
presenting part initially during IE Prepare additional equipment &
= identified on UTZ, CS is personnel for delivery
necessary before rupture of Assisting with amniotomy,
membranes. ultrasonography, forceps or
= if rupture occurs, the cord will vacuum extraction application as
slide down into the vagina needed
(pressure exerted by amniotic Assisting with neonatal
fluid) resuscitation, if necessary
= cord may be visible at the vulva Explaining any newborn
Management: 1. Position patient on characteristics related to the high
Trendelenburg or knee chest (for fetal risk birth, such as forcep marks,
head to fall back thus relieving pressure bruising
on cord preventing compression and Encouraging parental interaction
fetal anoxia) with neonates immediately after
2. Administer O2 at 10L/min to mother delivery
(helpful to improve oxygenation of the • PASSAGERefers to the route
fetus). that the fetus must travel when
3. A tocolytic agent is used (to reduce leaving the uterus arriving at the
uterine activity and pressure on fetus) external perineal area of birth.
4. If fully dilated, the physician may PROBLEMS with the PASSAGEWAY:
deliver infant quickly, if incomplete A. Abnormal Size or Shape of the
dilatation, upward pressure on the Pelvis
B. Cephalo-pelvic Disproportion passage
C. Shoulder Dystocia except when
• Refers to the route that the fetus fetus is in
must travel when leaving the occiput
uterus arriving at the external posterior
perineal area of birth. position
PROBLEMS with the PASSAGEWAY: c. Android- shaped pelvis occurs in
A. Abnormal Size or Shape of the about 20% of females
Pelvis It’s heart-
B. Cephalo-pelvic Disproportion shaped, like
C. Shoulder Dystocia the normal
• Refers to the route that the fetus male pelvis
must travel when leaving the Diameter is
uterus arriving at the external somewhat
perineal area of birth. narrowed,
Shape of pelvis making fetal
-also can determine the ability and ease passage
with which the fetus can pass difficult
a. Gynecoid- shaped pelvis is the most d. Platypelloid- shaped pelvis occurs in
common type of pelvis about 5% of females
Occurs in It’s oval or
about 50% of flat
females The fetus
Round shape may have
with difficulty
adequate rotating
diameters to sufficiently to
allow easy match the
passage of shape of the
fetal skull pelvis at the
b. Anthropoid- shaped pelvis occurs in appropriate
about 25% of females diameters
It’s oval with CEPHALOPELVIC DISPROPORTION
longer • Refers to the narrowing of the
anteroposteri birth canal which can occur at the
or diameter inlet, midpelvis, or outlet.
This type of • Involves a disproportion between
pelvis may the size of the normal fetal head
pose and the pelvic diameters.
difficulty in
• Results in failure to progress in may also be frightened and feel
labor helpless
Causes :
• The physical size of the maternal
pelvis is a major contributor –
small pelvis is a factor.
• Outlet contraction can also be a
contributing factor
- There's a narrowing of the transverse
diameter
Treatment :
• If the pelvic measurements are
borderline or just adequate,
especially the inlet measurement
, and the fetal lie and position are
good, the physician may allow a
trial labor (to determine whether
labor can progress normally).
• If labor doesn't progress or
complications develop, cesarean
birth is the method of choice.
• Nursing Intervention:
• 1. Instruct the primi patient to
maintain her prenatal visit
schedule so that pelvic
measurements are taken and
recorded before week 24 of
pregnancy.
• 2. Monitor progress of the trial
labor – if, after 6-12 hours, no
progress of labor and if fetal
distress occurs, prepare for CS.
• 3. If the trial labor fails and
cesarean birth is scheduled,
provide an explanation about why
it's necessary and is best for the
neonate.
• 4. Provide support for the
patient's significant person; he
Shoulder Dystocia Hypotonic uterine
• The problem occurs at the contractions
second stage of labor when the Uncoordinated uterine
fetal head is born but the contractions
shoulders are too broad to enter 2. Premature labor
and be delivered through the 3. Precipitate labor & birth
pelvic outlet. 4. Uterine prolapse/inversion
Causes : 5. Uterine rupture
- Occur in women with diabetes, and DYSFUNCTIONAL LABOR
in post-date pregnancies, poor fetal • Also known as “inertia” ; refers to
position, multiple pregnancy, and large a sluggishness in the force of
fetus. contractions.
• Hazardous to the Mother = • Dysfunctional labor can occur at
because it can result in vaginal or any point in labor but is generally
cervical tearing. classified as primary (occurring at
• Hazardous to the Fetus = the onset of labor) or secondary
compressed between the fetal (late in labor).
body and the bony pelvis, Causes:
possibly resulting in a fractured • It may be related to problems
clavicle or a brachial plexus with the passenger, passage or
injury. power.
Assessment Findings > malposition or malpresentation or an
• Suspected if the 2nd stage of unusually large fetus.
labor is prolonged, there is arrest > pelvic contractures, cervical rigidity
of descent or when head appears > uterine contractions that are
in perineum but retracts instead hypotonic, hypertonic, or uncoordinated.
of protruding with each • Presence of full rectum or urinary
contraction. (turtle sign) bladder (impedes fetal descent)
• Treatment : • Mother becoming exhausted from
• Initially = Applying suprapubic labor
pressure may help the shoulder Hypotonic Contractions
escape from beneath the • Termed when the number or
symphysis pubis. frequency of contractions is low,
• CS is necessary if maternal and not increasing beyond two or
fetal condition is in complication. three in a 10-minute period, and
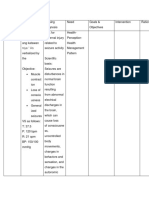
Problems with the POWERS the strength of contractions does
Problems with the Powers not rise above 25mmHg. The
1. Dystocia or difficult labor resting tone of the uterus remains
Hypertonic uterine below 10mmHg during active
contractions phase.
• Irregular and not painful (lack of - If contractions are too weak or
intensity) infrequent to be effective, labor may
causes: need to be induced or augmented to
• Occur when analgesia has been make uterine contractions stronger.
administered too early (before - Cervical ripening via stripping of
cervical dilatation of 3-4cm) membranes or application of
• Overstretched uterus by a prostaglandin gel or laminaria may be
multiple gestation done to prepare for the induction of
• Larger fetuses labor.
• Lax uterus from grand multiparity • Hypertonic contractions
• Bowel or bladder distention = involves promoting rest, providing
* due to cervix dilated for a long period analgesia with a drug such as morphine
both uterus and fetus are at risk of sulfate, possibly inducing sedation(for
INFECTION woman to rest).
HYPERTONIC UTERINE - promote comfort (changing the linen
CONTRACTION and the mother's gown, darkening room
• Are marked by an increased in lights, and decreasing noise/stimuli).
resting tone to more than - if decelerating FHT or lack of progress
15mmHg, with pushing, CS delivery may be
• The uterus don't rest between necessary.
contractions, high resting • Uncoordinated Contractions =
pressure of 40-50mmHg. - Oxytocin administration to stimulate a
• complains of pain more effective and consistent pattern of
• *lack of relaxation between contractions
contractions does not allow - if HPN occurs, stop oxy drip and
optimal uterine artery filling, notify physician.
which may lead to FETAL Nursing Interventions :
ANOXIA. 1. Explain the events to the patient and
Uncoordinated Uterine Contractions her support person; explain that the
• Occur erratically, such as one on contractions are ineffective
top of another followed by a long 2. Provide comfort measures, including
period without any. nonpharmacologic pain relief measures.
• The lack of a regular pattern to 3. Continuously monitor uterine
contractions makes it difficult for contractions and FHR patterns.
the woman to use breathing 4. Offer fluids as appropriate; institute IV
exercises bet contractions. therapy to supply glucose to replace
Management depleted stores from prolonged labor.
• Hypotonic contractions involves 5. Assist with measures to induce or
improving the strength of augment labor; monitor oxytocin infusion
contractions if used.
6. Encourage frequent voiding to • Magnesium sulfate is typically the
prevent bladder distention from first drug used to stop
interfering with labor contractions. contractions.
PREMATURE LABOR - It's a central nervous system
• Also known as “preterm labor”; depressant that prevents reflux of
the onset of rhythmic uterine calcium into the myometrial cells,
contractions that produce cervical thereby keeping the uterus relaxed.
changes after fetal viability but - Antidote is Calcium gluconate.
before fetal maturity. • Nifedipine (Procardia) is a
• Usually occurs between 20 and calcium channel blocker, it
below 37 weeks gestation. decreases the production of
• Premature labor increases the calcium, a substance associated
risk of neonate morbidity or with the initiation of labor.
mortality from excessive - There's no antidote, DC the drug.
maturational deficiencies. Nursing Intervention :
• Maternal causes : 1. Closely observe the patient in preterm
- Cardiovascular and renal disease labor for signs of fetal or maternal
- DM distress.
- Infection 2. Provide guidance about the hospital
- Abdominal surgery or trauma stay, potential for delivery of a
- Incompetent cervix premature infant, and the possible need
• Fetal causes : for neonatal intensive care.
- Infection 3. Maintain bed rest; provide appropriate
- Hydramnios diversionary activities.
- Multiple pregnancy 4. Administer medications as ordered.
Assessment Findings: 5. Monitor VS, FHR and uterine
• Onset of rhythmic uterine contractions.
contractions 6. Keep the patient in left side-lying
• Possible rupture of membranes , position to ensure adequate placental
passage of cervical mucus plug, perfusion.
and a bloody discharge 7. Administer fluids as ordered to ensure
• Cervical effacement and dilation adequate hydration.
on vaginal exam 8. If necessary during active premature
Treatment: labor, administer O2 to the patient.
drug therapy with tocolytic agent 9. If labor is suppressed, begin
• Terbutaline, a beta-adrenergic discharge teaching with the woman and
blocker, is the most commonly family about tocolytic therapy, and
used tocolytic (smooth muscle anticipate referral and follow up.
relaxation).
- Antidote is propranolol (Inderal)
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Maternal Care Package - Full.1-76Dokument76 SeitenMaternal Care Package - Full.1-76goobee93% (14)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- 3rd Stage of Labour PDFDokument15 Seiten3rd Stage of Labour PDFvarshasharma05Noch keine Bewertungen
- HEJE. Family Health Assessment Form.Dokument9 SeitenHEJE. Family Health Assessment Form.Abbeygale GalanNoch keine Bewertungen
- Care of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManDokument26 SeitenCare of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManLaurence Docog100% (1)
- Seminar On Obstructed LabourDokument98 SeitenSeminar On Obstructed Labourtesfahuntekletilahun80% (5)
- The Stages of Labor AreDokument2 SeitenThe Stages of Labor AreSheryll Almira HilarioNoch keine Bewertungen
- Terbutaline SulfateDokument1 SeiteTerbutaline SulfateIvanne Hisoler100% (2)
- Cesarean Section: History, Indications, Types and ProcedureDokument62 SeitenCesarean Section: History, Indications, Types and Proceduresanthiyasandy75% (4)
- Management of Third Stage of LaborDokument6 SeitenManagement of Third Stage of LaborYogesh BharankarNoch keine Bewertungen
- Nursing Care Management of a Client with Eclampsia: A Case StudyDokument72 SeitenNursing Care Management of a Client with Eclampsia: A Case StudyMauren Daza100% (4)
- Theoretical FrameworkDokument2 SeitenTheoretical FrameworkAbbeygale GalanNoch keine Bewertungen
- Pedia Final NCPDokument10 SeitenPedia Final NCPAbbeygale GalanNoch keine Bewertungen
- Journal #1 The Role of Nurses in Community Awareness and Preventive HealthDokument3 SeitenJournal #1 The Role of Nurses in Community Awareness and Preventive HealthAbbeygale GalanNoch keine Bewertungen
- Precipitate Labor, Uterine Inversion, Uterine RuptureDokument3 SeitenPrecipitate Labor, Uterine Inversion, Uterine RuptureAbbeygale Galan100% (2)
- Scientific BasisDokument2 SeitenScientific BasisAbbeygale GalanNoch keine Bewertungen
- Certificate for online class webinar participationDokument1 SeiteCertificate for online class webinar participationAbbeygale GalanNoch keine Bewertungen
- Gender and Society Week 1 - HWDokument2 SeitenGender and Society Week 1 - HWAbbeygale GalanNoch keine Bewertungen
- Ra1425 Rizal FamilyDokument7 SeitenRa1425 Rizal FamilyRoselle JoyceNoch keine Bewertungen
- Risk For InfectionDokument1 SeiteRisk For InfectionAbbeygale GalanNoch keine Bewertungen
- Maternal InjuryDokument2 SeitenMaternal InjuryAbbeygale GalanNoch keine Bewertungen
- NCP CP2Dokument4 SeitenNCP CP2Abbeygale GalanNoch keine Bewertungen
- Ra1425 Rizal FamilyDokument7 SeitenRa1425 Rizal FamilyRoselle JoyceNoch keine Bewertungen
- Scientific BasisDokument2 SeitenScientific BasisAbbeygale GalanNoch keine Bewertungen
- Risk For InfectionDokument1 SeiteRisk For InfectionAbbeygale GalanNoch keine Bewertungen
- GALANDokument2 SeitenGALANAbbeygale GalanNoch keine Bewertungen
- NCP CP2Dokument4 SeitenNCP CP2Abbeygale GalanNoch keine Bewertungen
- GALANDokument2 SeitenGALANAbbeygale GalanNoch keine Bewertungen
- MCN PartialDokument9 SeitenMCN PartialAbbeygale GalanNoch keine Bewertungen
- GALANDokument2 SeitenGALANAbbeygale GalanNoch keine Bewertungen
- MCN PartialDokument9 SeitenMCN PartialAbbeygale GalanNoch keine Bewertungen
- MCN PartialDokument9 SeitenMCN PartialAbbeygale GalanNoch keine Bewertungen
- Pedia Final NCPDokument10 SeitenPedia Final NCPAbbeygale GalanNoch keine Bewertungen
- GALANDokument2 SeitenGALANAbbeygale GalanNoch keine Bewertungen
- NewncpformDokument4 SeitenNewncpformAbbeygale GalanNoch keine Bewertungen
- NCP CP2Dokument4 SeitenNCP CP2Abbeygale GalanNoch keine Bewertungen
- MCN PartialDokument9 SeitenMCN PartialAbbeygale GalanNoch keine Bewertungen
- WW.05.21 Forceps Assisted Vaginal DeliveryDokument3 SeitenWW.05.21 Forceps Assisted Vaginal DeliveryLani Munawir Holis HolisNoch keine Bewertungen
- Komplikasi Persalinan Kala IIIDokument27 SeitenKomplikasi Persalinan Kala IIIfebryana wulandariNoch keine Bewertungen
- Essay Ge Sintiya B19022Dokument3 SeitenEssay Ge Sintiya B19022sintiaNoch keine Bewertungen
- Chapter 23 ContinuationDokument7 SeitenChapter 23 ContinuationArabelle GO100% (1)
- Diagnostic Tests of Placenta Accreta Index Score PDokument6 SeitenDiagnostic Tests of Placenta Accreta Index Score PBogdan CăpățînăNoch keine Bewertungen
- Caesarean DeliveryDokument207 SeitenCaesarean Deliverynsaid007Noch keine Bewertungen
- Bicol University Polangui CampusDokument3 SeitenBicol University Polangui CampusYOLANDA P. DELCASTILLONoch keine Bewertungen
- Antepartum BleedingDokument7 SeitenAntepartum Bleedingbluecrush1Noch keine Bewertungen
- Intrauterine Fetal DemiseDokument17 SeitenIntrauterine Fetal DemiseDewey NguyenNoch keine Bewertungen
- Abnormal Uterine ActionDokument33 SeitenAbnormal Uterine ActionRadwa Ebed100% (1)
- Malpresentations: Liji Raichel Kurian Dept of OBGDokument41 SeitenMalpresentations: Liji Raichel Kurian Dept of OBGliji raichel kurian100% (1)
- Nursing Care of The Newborn With Special Needs Nursing Care of The Newborn With Special NeedsDokument35 SeitenNursing Care of The Newborn With Special Needs Nursing Care of The Newborn With Special NeedsMichelle DislaNoch keine Bewertungen
- Supervisor: Dr. Agus Thoriq, Spog DM: AkbarDokument31 SeitenSupervisor: Dr. Agus Thoriq, Spog DM: AkbarAkbar GazaliNoch keine Bewertungen
- Intranatal CareDokument32 SeitenIntranatal CareMnm Ikljh100% (1)
- Postpartum ChecklistDokument2 SeitenPostpartum ChecklistSara roseNoch keine Bewertungen
- Torch Infection and Its Management With Ayurveda, An Indigenous MedicineDokument2 SeitenTorch Infection and Its Management With Ayurveda, An Indigenous MedicineDhiraj BaksheNoch keine Bewertungen
- Benefits of Rooming-In for Mothers and BabiesDokument3 SeitenBenefits of Rooming-In for Mothers and BabiesAlisha Buyungan MundocNoch keine Bewertungen
- OB Return DemoDokument7 SeitenOB Return DemoSophia RubiaNoch keine Bewertungen
- Fetal MacrosomiaDokument4 SeitenFetal MacrosomiaCristhian CruzNoch keine Bewertungen
- BreechDokument2 SeitenBreechBrel KirbyNoch keine Bewertungen
- Antepartum Hemorrhage: Causes, Diagnosis and ManagementDokument45 SeitenAntepartum Hemorrhage: Causes, Diagnosis and ManagementGeorge C. KasondaNoch keine Bewertungen
- Anesthetic Implications of Molar PregnancyDokument2 SeitenAnesthetic Implications of Molar PregnancyNovi KartikadewiNoch keine Bewertungen
- APH & PPH: Causes, Diagnosis and ManagementDokument81 SeitenAPH & PPH: Causes, Diagnosis and ManagementSheilla ElfiraNoch keine Bewertungen