Beruflich Dokumente
Kultur Dokumente
Arkansas Works Opinion
Hochgeladen von
Law&CrimeOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Arkansas Works Opinion
Hochgeladen von
Law&CrimeCopyright:
Verfügbare Formate
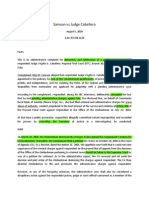
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 1 of 19
United States Court of Appeals
FOR THE DISTRICT OF COLUMBIA CIRCUIT
Argued October 11, 2019 Decided February 14, 2020
No. 19-5094
CHARLES GRESHAM, ET AL.,
APPELLEES
v.
ALEX MICHAEL AZAR, II, SECRETARY, UNITED STATES
DEPARTMENT OF HEALTH AND HUMAN SERVICES IN HIS
OFFICIAL CAPACITY, ET AL.,
APPELLANTS
STATE OF ARKANSAS,
APPELLEE
Consolidated with 19-5096
Appeals from the United States District Court
for the District of Columbia
(No. 1:18-cv-01900)
Alisa B. Klein, Attorney, U.S. Department of Justice,
argued the cause for federal appellants. With her on the briefs
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 2 of 19
2
were Mark B. Stern, Attorney, Robert P. Charrow, General
Counsel, U.S. Department of Health and Human Services, and
Brenna E. Jenny, Deputy General Counsel.
Leslie Rutledge, Attorney General, Office of the Attorney
General for the State of Arkansas, Nicholas J. Bronni, Solicitor
General, Vincent M. Wagner, Deputy Solicitor General, and
Dylan L. Jacobs, Assistant Solicitor General, were on the brief
for appellant State of Arkansas.
Ian Heath Gershengorn argued the cause for plaintiff-
appellees. With him on the brief were Jane Perkins, Thomas
J. Perrelli, Devi M. Rao, Natacha Y. Lam, Zachary S. Blau, and
Samuel Brooke.
Kyle Druding was on the brief for amici curiae American
College of Physicians, et al. in support of plaintiffs-appellees.
Edward T. Waters, Phillip A. Escoriaza, and Charles J.
Frisina were on the brief for amici curiae Deans, Chairs, and
Scholars in support of plaintiffs-appellees.
Judith R. Nemsick, Jon M. Greenbaum, and Sunu Chandy
were on the brief for amici curiae Lawyers Committee for Civil
Rights Under Law, et al. in support of appellees and
affirmance.
Before: PILLARD, Circuit Judge, and EDWARDS and
SENTELLE, Senior Circuit Judges.
Opinion for the Court filed by Senior Circuit Judge
SENTELLE.
SENTELLE, Senior Circuit Judge: Residents of Kentucky
and Arkansas brought this action against the Secretary of
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 3 of 19
3
Health and Human Services. They contend that the Secretary
acted in an arbitrary and capricious manner when he approved
Medicaid demonstration requests for Kentucky and Arkansas.
The District Court for the District of Columbia held that the
Secretary did act in an arbitrary and capricious manner because
he failed to analyze whether the demonstrations would promote
the primary objective of Medicaid—to furnish medical
assistance. After oral argument, Kentucky terminated the
challenged demonstration project and moved for voluntary
dismissal. We granted the unopposed motion. The only
question remaining before us is whether the Secretary’s
authorization of Arkansas’s demonstration is lawful. Because
the Secretary’s approval of the plan was arbitrary and
capricious, we affirm the judgment of the district court.
I. Background
Originally, Medicaid provided health care coverage for
four categories of people: the disabled, the blind, the elderly,
and needy families with dependent children. 42 U.S.C.
§ 1396-1. Congress amended the statute in 2010 to expand
medical coverage to low-income adults who did not previously
qualify. Id. at § 1396a(a)(10)(A)(i)(VIII); NFIB v. Sebelius,
567 U.S. 519, 583 (2012). States have a choice whether to
expand Medicaid to cover this new population of individuals.
NFIB, 567 U.S. at 587. Arkansas expanded Medicaid coverage
to the new population effective January 1, 2014, through their
participation in private health plans, known as qualified health
plans, with the state paying premiums on behalf of enrollees.
Appellees’ Br. 14; Gresham v. Azar, 363 F. Supp. 3d 165, 171
(D.D.C. 2019).
Medicaid establishes certain minimum coverage
requirements that states must include in their plans. 42 U.S.C.
§ 1396a. States can deviate from those requirements if the
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 4 of 19
4
Secretary waives them so that the state can engage in
“experimental, pilot, or demonstration project[s].” 42 U.S.C.
§ 1315(a). The section authorizes the Secretary to approve
“any experimental, pilot, or demonstration project which, in the
judgment of the Secretary, is likely to assist in promoting the
objectives” of Medicaid. Id.
Arkansas applied to amend its existing waiver under
§ 1315 on June 30, 2017. Arkansas Administrative Record
2057 (“Ark. AR”). Arkansas gained approval for its initial
Medicaid demonstration waiver in September 2013. In 2016,
the state introduced its first version of the Arkansas Works
program, encouraging enrollees to seek employment by
offering voluntary referrals to the Arkansas Department of
Workforce Services. Dissatisfied with the level of
participation in that program, Arkansas’s new version of
Arkansas Works introduced several new requirements and
limitations. The one that received the most attention required
beneficiaries aged 19 to 49 to “work or engage in specified
educational, job training, or job search activities for at least 80
hours per month” and to document such activities. Id. at 2063.
Certain categories of beneficiaries were exempted from
completing the hours, including beneficiaries who show they
are medically frail or pregnant, caring for a dependent child
under age six, participating in a substance treatment program,
or are full-time students. Id. at 2080–81. Nonexempt
“beneficiaries who fail to meet the work requirements for any
three months during a plan year will be disenrolled . . . and will
not be permitted to re-enroll until the following plan year.” Id.
at 2063.
Arkansas Works included some other new requirements in
addition to the much-discussed work requirements. Typically,
when someone enrolls in Medicaid, the “medical assistance
under the plan . . . will be made available to him for care and
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 5 of 19
5
services included under the plan and furnished in or after the
third month before the month in which he made application.”
42 U.S.C. § 1396a(a)(34). Arkansas Works proposed to
eliminate retroactive coverage entirely. Ark. AR 2057, 2061.
It also proposed to lower the income eligibility threshold from
133% to 100% of the federal poverty line, meaning that
beneficiaries with incomes from 101% to 133% of the federal
poverty line would lose health coverage. Id. at 2057, 2060–61,
2063. Finally, Arkansas Works eliminated a program in which
it used Medicaid funds to assist beneficiaries in paying the
premiums for employer-provided health care coverage. Id. at
2057, 2063, 2073. Arkansas instead used Medicaid premium
assistance funds only to help beneficiaries purchase a qualified
health plan available on the state Health Insurance
Marketplace, requiring all previous recipients of employer-
sponsored coverage premiums to transition to coverage offered
through the state’s Marketplace. Id. at 2057, 2063, 2073.
On March 5, 2018, the Secretary approved most of the new
Arkansas Works program via a waiver effective until
December 31, 2021, but with a few changes. He approved the
work requirements but under the label of “community
engagement.” Id. at 2. The Secretary authorized Arkansas to
limit retroactive coverage to thirty days before enrollment
rather than a complete elimination of retroactive coverage. Id.
at 3, 12. He also approved Arkansas’s decision to terminate the
employer-sponsored coverage premium assistance program.
Id. at 3. The Secretary did not, however, permit Arkansas to
limit eligibility to persons making less than or equal to 100%
of the federal poverty line. Id. at 3 n.1, 11. Instead, the
Secretary kept the income eligibility threshold at 133% of the
federal poverty line. Id. at 3 n.1, 11.
In the approval letter, the Secretary analyzed whether
Arkansas Works would “assist in promoting the objectives of
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 6 of 19
6
Medicaid.” Id. at 3. The Secretary identified three objectives
that he asserted Arkansas Works would promote: “improving
health outcomes; . . . address[ing] behavioral and social factors
that influence health outcomes; and . . . incentiviz[ing]
beneficiaries to engage in their own health care and achieve
better health outcomes.” Id. at 4. In particular, the Secretary
stated that Arkansas Works’s community engagement
requirements would “encourage beneficiaries to obtain and
maintain employment or undertake other community
engagement activities that research has shown to be correlated
with improved health and wellness.” Id. Further, the Secretary
thought the shorter timeframe for retroactive eligibility would
“encourage beneficiaries to obtain and maintain health
coverage, even when they are healthy,” which, in turn,
promotes “the ultimate objective of improving beneficiary
health.” Id. at 5. The letter also summarized concerns raised
by commenters that the community engagement requirement
would “caus[e] disruptions in care” or “create barriers to
coverage” for beneficiaries who are not exempt. Id. at 6–7.
In response, the Secretary noted that Arkansas had several
exemptions and would “implement an outreach strategy to
inform beneficiaries about how to report compliance.” Id.
The new work requirements took effect for those aged 30
to 49 on June 1, 2018, and for those aged 20 to 29 on January
1, 2019. Gresham, 363 F. Supp. 3d at 172. Charles Gresham
along with nine other Arkansans filed an action for declaratory
and injunctive relief against the Secretary on August 14, 2018.
The district court on March 27, 2019, entered judgment
vacating the Secretary’s approval, effectively halting the
program. Gresham, 363 F. Supp. 3d at 176–85. In its opinion
supporting the judgment, the district court relied on Stewart v.
Azar, 313 F. Supp. 3d 237 (D.D.C. 2018) (Stewart I), which is
the district court’s first opinion considering Kentucky’s similar
demonstration, Gresham, 363 F. Supp. 3d at 176. In Stewart I,
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 7 of 19
7
the district court turned to the provision authorizing the
appropriations of funds for Medicaid, 42 U.S.C. § 1396-1, and
held that, based on the text of that appropriations provision, the
objective of Medicaid was to “furnish . . . medical assistance”
to people who cannot afford it. Stewart I, 313 F. Supp. 3d at
260–61.
With its previously articulated objective of Medicaid in
mind, the district court then turned to the Secretary’s approval
of Arkansas Works. First, the district court noted that the
Secretary identified three objectives that Arkansas Works
would promote: “(1) ‘whether the demonstration as amended
was likely to assist in improving health outcomes’;
(2) ‘whether it would address behavioral and social factors that
influence health outcomes’; and (3) ‘whether it would
incentivize beneficiaries to engage in their own health care and
achieve better health outcomes.’” Gresham, 363 F. Supp. 3d
at 176 (quoting Ark. AR 4). But “[t]he Secretary’s approval
letter did not consider whether [Arkansas Works] would reduce
Medicaid coverage. Despite acknowledging at several points
that commenters had predicted coverage loss, the agency did
not engage with that possibility.” Id. at 177. The district court
also explained that the Secretary failed to consider whether
Arkansas Works would promote coverage. Id. at 179. Instead,
the Secretary considered his alternative objectives, primarily
healthy outcomes, but the district court observed that “‘focus
on health is no substitute for considering Medicaid’s central
concern: covering health costs’ through the provision of free or
low-cost health coverage.” Id. (quoting Stewart I, 313 F. Supp.
3d at 266). “In sum,” the district court held:
the Secretary’s approval of the Arkansas Works
Amendments is arbitrary and capricious because it
did not address—despite receiving substantial
comments on the matter—whether and how the
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 8 of 19
8
project would implicate the “core” objective of
Medicaid: the provision of medical coverage to the
needy.
Id. at 181. The district court entered final judgment on April
4, 2019, and the Secretary filed a notice of appeal on April 10,
2019.
This case was originally a consolidated appeal from the
district court’s judgment in both the Arkansas and Kentucky
cases. The district court twice vacated the Secretary’s approval
of Kentucky’s demonstration for the same failure to address
whether Kentucky’s program would promote the key objective
of Medicaid. Stewart v. Azar, 366 F. Supp. 3d 125, 156
(D.D.C. 2019) (Stewart II); Stewart I, 313 F. Supp. 3d at 274.
On December 16, 2019, Kentucky moved to dismiss its appeal
as moot because it “terminated the section [1315]
demonstration project.” Intervenor-Def.-Appellant’s Mot. to
Voluntarily Dismiss Appeal 1–2 (Dec. 16, 2019), ECF No.
1820334. Neither the government nor the appellees opposed
the motion. Gov’t’s Resp. (Dec. 18, 2019), ECF No. 1820655;
Appellees’ Resp. (Dec. 20, 2019), ECF No. 1821219.
Although the Secretary has considerable discretion to
grant a waiver, we reject the government’s contention that such
discretion renders his waiver decisions unreviewable. The
Administrative Procedure Act’s (APA) exception from judicial
review for an action committed to agency discretion is “very
narrow,” Citizens to Preserve Overton Park, Inc. v. Volpe, 401
U.S. 402, 410 (1971); see also Dep’t of Commerce v. New York,
139 S. Ct. 2551, 2568 (2019), barring judicial review only in
those “rare instances” where “there is no law to apply,”
Overton Park, 401 U.S. at 410 (internal quotation marks and
citation omitted). The Medicaid statute provides the legal
standard we apply here: The Secretary may only approve
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 9 of 19
9
“experimental, pilot, or demonstration project[s],” and only
insofar as they are “likely to assist in promoting the objectives”
of Medicaid, 42 U.S.C. § 1315(a). Section 1315 approvals are
not among the rare “categories of administrative decisions that
courts traditionally have regarded as committed to agency
discretion.” Dep’t of Commerce, 139 S. Ct. at 2568.
Additionally, the government asked that we address “the
reasoning of the district court’s opinion in Stewart and the
underlying November 2018 HHS approval of the Kentucky
demonstration,” and second that we vacate the district court’s
judgment against the federal defendants in the Kentucky case
Stewart II, 66 F. Supp. 3d 125. Gov’t’s Resp. 1–2. The
appellees opposed both of those additional requests.
Appellees’ Resp. 1–4. We granted the motion to voluntarily
dismiss but declined to vacate the district court’s judgment
against the federal defendants in Stewart II. As to the
government’s first request, we do not rely on the Secretary’s
reasoning in the November 2018 approval of Kentucky’s
demonstration when considering the Secretary’s approval of
Arkansas’s demonstration.
“We review de novo the District Court’s grant of summary
judgment, which means that we review the agency’s decision
on our own.” Castlewood Prods., L.L.C. v. Norton, 365 F.3d
1076, 1082 (D.C. Cir. 2004). Therefore, we will review the
Secretary’s approval of Arkansas Works in accordance with the
Administrative Procedure Act and will set it aside if it is
“arbitrary, capricious, an abuse of discretion, or otherwise not
in accordance with law.” 5 U.S.C. § 706(2)(A); see also C.K.
v. New Jersey Dep’t of Health & Human Servs., 92 F.3d 171,
181–82 (3d Cir. 1996) (applying the arbitrary and capricious
standard of review to a waiver under § 1315); Beno v. Shalala,
30 F.3d 1057, 1066–67 (9th Cir. 1994) (same); Aguayo v.
Richardson, 473 F.2d 1090, 1103–08 (2d Cir. 1973) (same).
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 10 of 19
10
An agency action that “entirely failed to consider an important
aspect of the problem, offered an explanation for its decision
that runs counter to the evidence before the agency, or is so
implausible that it could not be ascribed to a difference in view
or the product of agency expertise” is arbitrary and capricious.
Motor Vehicle Mfrs. Ass’n of U.S., Inc. v. State Farm Mut.
Auto. Ins. Co., 463 U.S. 29, 43 (1983).
II. DISCUSSION
A. Objective of Medicaid
The district court is indisputably correct that the principal
objective of Medicaid is providing health care coverage. The
Secretary’s discretion in approving or denying demonstrations
is guided by the statutory directive that the demonstration must
be “likely to assist in promoting the objectives” of Medicaid.
42 U.S.C. § 1315. While the Medicaid statute does not have a
standalone purpose section like some social welfare statutes,
see, e.g., 42 U.S.C. § 601(a) (articulating the purposes of the
Temporary Assistance for Needy Families program); 42 U.S.C.
§ 629 (announcing the “objectives” of the Promoting Safe and
Stable Families program), it does have a provision that
articulates the reasons underlying the appropriations of funds,
42 U.S.C. § 1396-1. The provision describes the purpose of
Medicaid as
to furnish (1) medical assistance on behalf of
families with dependent children and of aged, blind,
or disabled individuals, whose income and
resources are insufficient to meet the costs of
necessary medical services, and (2) rehabilitation
and other services to help such families and
individuals attain or retain capability for
independence or self-care.
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 11 of 19
11
Id. In addition to the appropriations provision, the statute
defines “medical assistance” as “payment of part or all of the
cost of the following care and services or the care and services
themselves.” 42 U.S.C. § 1396d(a). Further, as the district
court explained, the Affordable Care Act’s expansion of health
care coverage to a larger group of Americans is consistent with
Medicaid’s general purpose of furnishing health care
coverage. See Stewart I, 313 F. Supp. 3d at 260 (citing Pub.
L. No. 111-148, 124 Stat. 119, 130, 271 (2010)). The text
consistently focuses on providing access to health care
coverage.
Both the First and Sixth Circuits relied on Medicaid’s
appropriations provision quoted above in concluding that
“[t]he primary purpose of Medicaid is to enable states to
provide medical services to those whose ‘income and
resources are insufficient to meet the costs of necessary
medical services.’” Pharm. Research & Mfrs. of Am. v.
Concannon, 249 F.3d 66, 75 (1st Cir. 2001) (quoting 42 U.S.C.
§ 1396 (2000)), aff’d, 538 U.S. 644 (2003); Price v. Medicaid
Dir., 838 F.3d 739, 742 (6th Cir. 2016). Similarly, the Ninth
Circuit relied on both the appropriations provision and the
definition of “medical assistance” when describing Medicaid
as “a federal grant program that encourages states to provide
certain medical services” and identifying a key element of
“medical assistance” as the spending of federally provided
funds for medical coverage. Univ. of Wash. Med. Ctr. v.
Sebelius, 634 F.3d 1029, 1031, 1034–35 (9th Cir. 2011).
Beyond relying on the text of the statute, other courts have
consistently described Medicaid’s objective as primarily
providing health care coverage. For example, the Third
Circuit succinctly stated, “We recognize, of course, that the
primary purpose of medicaid is to achieve the praiseworthy
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 12 of 19
12
social objective of granting health care coverage to those who
cannot afford it.” W. Va. Univ. Hosps., Inc. v. Casey, 885 F.2d
11, 20 (3d Cir. 1989), aff’d, 499 U.S. 83 (1991). Likewise, the
Supreme Court characterized Medicaid as a “program . . .
[that] provides joint federal and state funding of medical care
for individuals who cannot afford to pay their own medical
costs.” Ark. Dep’t of Health & Human Servs. v. Ahlborn, 547
U.S. 268, 275 (2006); see also Virginia ex rel. Hunter Labs.,
L.L.C. v. Virginia, 828 F.3d 281, 283 (4th Cir. 2016) (quoting
Ahlborn in the section of the decision explaining the important
aspects of Medicaid).
The statute and the case law demonstrate that the primary
objective of Medicaid is to provide access to medical care.
There might be secondary benefits that the government was
hoping to incentivize, such as healthier outcomes for
beneficiaries or more engagement in their health care, but the
“means [Congress] has deemed appropriate” is providing
health care coverage. MCI Telecomms. Corp. v. Am. Tel. &
Tel. Co., 512 U.S. 218, 231 n.4 (1994). In sum, “the intent of
Congress is clear” that Medicaid’s objective is to provide
health care coverage, and, as a result, the Secretary “must give
effect to [that] unambiguously expressed intent of Congress.”
Chevron, U.S.A., Inc. v. Nat. Res. Def. Council, Inc., 467 U.S.
837, 842–43 (1984).
Instead of analyzing whether the demonstration would
promote the objective of providing coverage, the Secretary
identified three alternative objectives: “whether the
demonstration as amended was likely to assist in improving
health outcomes; whether it would address behavioral and
social factors that influence health outcomes; and whether it
would incentivize beneficiaries to engage in their own health
care and achieve better health outcomes.” Ark. AR 4. These
three alternative objectives all point to better health outcomes
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 13 of 19
13
as the objective of Medicaid, but that alternative objective
lacks textual support. Indeed, the statute makes no mention of
that objective.
While furnishing health care coverage and better health
outcomes may be connected goals, the text specifically
addresses only coverage. 42 U.S.C. § 1396-1. The Supreme
Court and this court have consistently reminded agencies that
they are “bound, not only by the ultimate purposes Congress
has selected, but by the means it has deemed appropriate, and
prescribed, for the pursuit of those purposes.” MCI
Telecomms., 512 U.S. at 231 n. 4; see also Waterkeeper All. v.
EPA, 853 F.3d 527, 535 (D.C. Cir. 2017); Colo. River Indian
Tribes v. Nat’l Indian Gaming Comm’n, 466 F.3d 134, 139–
40 (D.C. Cir. 2006). The means that Congress selected to
achieve the objectives of Medicaid was to provide health care
coverage to populations that otherwise could not afford it.
To an extent, Arkansas and the government characterize
the Secretary’s approval letter as also identifying transitioning
beneficiaries away from governmental benefits through
financial independence or commercial coverage as an
objective promoted by Arkansas Works. Ark. Br. 14, 37–42;
Gov’t Br. 24–25, 32. This argument misrepresents the
Secretary’s letter. The approval letter has a specific section
for the Secretary’s determination that the project will assist in
promoting the objectives of Medicaid. Ark. AR 3–5. The
objectives articulated in that section are the health-outcome
goals quoted above. That section does not mention
transitioning beneficiaries away from benefits. The district
court’s discussion of the Secretary’s objectives confirms our
interpretation of this letter. It identifies the Secretary’s
alternative objective as “improv[ing] health outcomes.”
Gresham, 363 F. Supp. 3d at 179. There is no reference to
commercial coverage in the Secretary’s approval letter, and
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 14 of 19
14
the only reference to beneficiary financial independence is in
the section summarizing public comments. In response to
concerns about the community engagement requirements
creating barriers to coverage, the Secretary stated, “Given that
employment is positively correlated with health outcomes, it
furthers the purposes of the Medicaid statute to test and
evaluate these requirements as a means to improve
beneficiaries’ health and to promote beneficiary
independence.” Ark. AR 6. But “[n]owhere in the Secretary’s
approval letter does he justify his decision based . . . on a belief
that the project will help Medicaid-eligible persons to gain
sufficient financial resources to be able to purchase private
insurance.” Gresham, 363 F. Supp. 3d at 180–81. We will not
accept post hoc rationalizations for the Secretary’s decision.
See State Farm, 463 U.S. at 50.
Nor could the Secretary have rested his decision on the
objective of transitioning beneficiaries away from government
benefits through either financial independence or commercial
coverage. When Congress wants to pursue additional
objectives within a social welfare program, it says so in the
text. For example, the purpose section of TANF explicitly
includes “end[ing] the dependence of needy parents on
government benefits by promoting job preparation, work, and
marriage” among the objectives of the statute. 42 U.S.C.
§ 601(a)(2). Also, both TANF and the Supplemental Nutrition
Assistance Program (SNAP) condition eligibility for benefits
upon completing a certain number of hours of work per week
to support the objective of “end[ing] dependence of needy
parents on government benefits.” 42 U.S.C. §§ 601(a)(2),
607(c) (TANF); 7 U.S.C. § 2015(d)(1) (SNAP). In contrast,
Congress has not conditioned the receipt of Medicaid benefits
on fulfilling work requirements or taking steps to end receipt
of governmental benefits.
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 15 of 19
15
The reference to independence in the appropriations
provision and the cross reference to TANF cannot support the
Secretary’s alternative objective either. The reference to
“independence” in the appropriations provision is in the
context of assisting beneficiaries in achieving functional
independence through rehabilitative and other services, not
financial independence from government welfare programs.
42 U.S.C. § 1396-1. Medicaid also grants states the “[o]ption”
to terminate Medicaid benefits when a beneficiary who
receives both Medicaid and TANF fails to comply with
TANF’s work requirements. See 42 U.S.C.
§ 1396u-1(b)(3)(A). The provision gives states, therefore, the
ability to coordinate benefits for recipients receiving both
TANF and Medicaid. It does not go so far as to incorporate
TANF work requirements and additional objectives into
Medicaid.
Further, the history of Congress’s amendments to social
welfare programs supports the conclusion that Congress did
not intend 42 U.S.C. § 1396u-1(b)(3)(A) to incorporate
TANF’s objectives and work requirements into Medicaid. In
1996, SNAP already included work requirements to maintain
eligibility. 7 U.S.C. § 2015(d)(1) (1994). Also in 1996,
Congress passed the Personal Responsibility and Work
Opportunity Reconciliation Act, which replaced Aid to
Families with Dependent Children with TANF and added
work requirements. Personal Responsibility and Work
Opportunity Reconciliation Act of 1996, Pub. L. No. 104-193,
sec. 103, § 407, 110 Stat. 2105, 2129–34. At the same time, it
added 42 U.S.C. § 1396u-1(b)(3)(A) to Medicaid. Id. at sec.
114, § 1931, 110 Stat. at 2177–80. The fact that Congress did
not similarly amend Medicaid to add a work requirement for
all recipients—at a time when the other two major welfare
programs had those requirements and Congress was in the
process of amending welfare statutes—demonstrates that
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 16 of 19
16
Congress did not intend to incorporate work requirements into
Medicaid through § 1396u-1(b)(3)(A).
In short, we agree with the district court that the
alternative objectives of better health outcomes and
beneficiary independence are not consistent with Medicaid.
The text of the statute includes one primary purpose, which is
providing health care coverage without any restriction geared
to healthy outcomes, financial independence or transition to
commercial coverage.
B. The Approvals Were Arbitrary and Capricious
With the objective of Medicaid defined, we turn to the
Secretary’s analysis and approval of Arkansas’s
demonstration, and we find it wanting. In order to survive
arbitrary and capricious review, agencies need to address
“important aspect[s] of the problem.” State Farm, 463 U.S. at
43. In this situation, the loss of coverage for beneficiaries is an
important aspect of the demonstration approval because
coverage is a principal objective of Medicaid and because
commenters raised concerns about the loss of coverage. See,
e.g., Ark. AR 1269–70, 1277–78, 1285, 1294–95.
A critical issue in this case is the Secretary’s failure to
account for loss of coverage, which is a matter of importance
under the statute. The record shows that the Arkansas Works
amendments resulted in significant coverage loss. In Arkansas,
more than 18,000 people (about 25% of those subject to the
work requirement) lost coverage as a result of the project in just
five months. Ark. Dep’t of Human Servs., Arkansas Works
Program 8 (Dec. 2018),
https://humanservices.arkansas.gov/images/uploads/011519_
AWReport.pdf. Additionally, commenters on the Arkansas
Works amendments detailed the potential for substantial
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 17 of 19
17
coverage loss supported by research evidence. Ark. AR 1269–
70, 1277–78, 1285, 1294–95, 1297, 1307–08, 1320, 1326,
1337–38, 1341, 1364–65, 1402, 1421. The Secretary’s
analysis considered only whether the demonstrations would
increase healthy outcomes and promote engagement with the
beneficiary’s health care. Id. at 3–5. The Secretary noted that
some commenters were concerned that “these requirements
would be burdensome on families or create barriers to
coverage.” Id. at 6. But he explained that Arkansas would have
“outreach and education on how to comply with the new
community engagement requirements” and that Centers for
Medicare and Medicaid Services could discontinue the
program if data showed that it was no longer in the public
interest. Id. The Secretary also concluded that the “overall
health benefits to the [a]ffected population . . . outweigh the
health-risks with respect to those who fail to” comply with the
new requirements. Id. at 7. While Arkansas did not have its
own estimate of potential coverage loss, the estimates and
concerns raised in the comments were enough to alert the
Secretary that coverage loss was an important aspect of the
problem. Failure to consider whether the project will result in
coverage loss is arbitrary and capricious.
In total, the Secretary’s analysis of the substantial and
important problem is to note the concerns of others and dismiss
those concerns in a handful of conclusory sentences. Nodding
to concerns raised by commenters only to dismiss them in a
conclusory manner is not a hallmark of reasoned
decisionmaking. See, e.g., Am. Wild Horse Pres. Campaign v.
Perdue, 873 F.3d 914, 932 (D.C. Cir. 2017) (critiquing an
agency for “brush[ing] aside critical facts” and not “adequately
analyz[ing]” the consequences of a decision); Getty v. Fed.
Savs. & Loan Ins. Corp., 805 F.2d 1050, 1055 (D.C. Cir. 1986)
(analyzing whether an agency actually considered a concern
rather than merely stating that it considered the concern).
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 18 of 19
18
True, the Secretary’s approval letter is not devoid of
analysis. It does contain the Secretary’s articulation of how he
thought the demonstrations would assist in promoting an
entirely different set of objectives than the one we hold is the
principal objective of Medicaid. In some circumstances it may
be enough for the agency to assess at least one of several
possible objectives. See Fresno Mobile Radio, Inc. v. FCC,
165 F.3d 965, 971 (D.C. Cir. 1999). But in such cases, the
statute lists several objectives, some of which might lead to
conflicting decisions. Id.; see also Melcher v. FCC, 134 F.3d
1143, 1154 (D.C. Cir. 1998). For example, in both Fresno
Mobile Radio and Melcher, the statute at issue included five
separate objectives for FCC to consider when creating auctions
for licenses, including “the development and rapid deployment
of new technologies,” “promoting economic opportunity and
competition,” and the “efficient and intensive use of the
electromagnetic spectrum.” 47 U.S.C. § 309(j)(3). In Fresno
Mobile Radio, we recognized that these objectives could point
to conflicting courses of action, so the agency could give
precedence to one or several objectives over others without
acting in an arbitrary or capricious manner. Fresno Mobile
Radio, 165 F.3d at 971; see also Melcher, 134 F.3d at 1154;
Rural Cellular Ass’n v. FCC, 588 F.3d 1095, 1101–03 (D.C.
Cir. 2009) (explaining that an agency may not “depart from”
statutory principles “altogether to achieve some other goal”).
The crucial difference in this case is that the Medicaid statute
identifies its primary purpose rather than a laundry list. The
primary purpose is
to furnish (1) medical assistance on behalf of
families with dependent children and of aged, blind,
or disabled individuals, whose income and
resources are insufficient to meet the costs of
necessary medical services, and (2) rehabilitation
USCA Case #19-5094 Document #1828589 Filed: 02/14/2020 Page 19 of 19
19
and other services to help such families and
individuals attain or retain capability for
independence or self-care.
42 U.S.C. § 1396-1. Importantly, the Secretary disregarded
this statutory purpose in his analysis. While we have held that
it is not arbitrary or capricious to prioritize one statutorily
identified objective over another, it is an entirely different
matter to prioritize non-statutory objectives to the exclusion of
the statutory purpose.
III. CONCLUSION
Because the Secretary’s approval of Arkansas Works was
arbitrary and capricious, we affirm the district court’s judgment
vacating the Secretary’s approval.
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- United States v. Dighera, 10th Cir. (2007)Dokument4 SeitenUnited States v. Dighera, 10th Cir. (2007)Scribd Government DocsNoch keine Bewertungen
- St. Mary's Academy Vs CarpitañosDokument2 SeitenSt. Mary's Academy Vs CarpitañosKeneth Wilson VirayNoch keine Bewertungen
- Human Trafficking Smugling ProcDokument36 SeitenHuman Trafficking Smugling ProcHasenNoch keine Bewertungen
- D.2.1 Samson Vs Judge Caballero Case DigestDokument2 SeitenD.2.1 Samson Vs Judge Caballero Case DigestAlejandro de LeonNoch keine Bewertungen
- PalemidtermsDokument19 SeitenPalemidtermszarah08Noch keine Bewertungen
- United States v. McCabe, 4th Cir. (2005)Dokument3 SeitenUnited States v. McCabe, 4th Cir. (2005)Scribd Government DocsNoch keine Bewertungen
- Ricarze Vs Court of AppealsDokument5 SeitenRicarze Vs Court of AppealsQueenie BoadoNoch keine Bewertungen
- Reviewer in Administrative Law by Atty SandovalDokument23 SeitenReviewer in Administrative Law by Atty SandovalRhei BarbaNoch keine Bewertungen
- Law of Evidence Admissibility: Introduction To Forensic ScienceDokument40 SeitenLaw of Evidence Admissibility: Introduction To Forensic ScienceRoxanne Torres San PedroNoch keine Bewertungen
- En ConsultaDokument3 SeitenEn ConsultaMJ PerryNoch keine Bewertungen
- ABAKADA Guro v. PurisimaDokument95 SeitenABAKADA Guro v. PurisimaKRIZEANAE PLURADNoch keine Bewertungen
- 245 Legal Office Procedures R 2014Dokument6 Seiten245 Legal Office Procedures R 2014api-250674550Noch keine Bewertungen
- Sachin and ANR V. Jhabbu Lal and ANR Case AnalysisDokument7 SeitenSachin and ANR V. Jhabbu Lal and ANR Case AnalysisParbatNoch keine Bewertungen
- The Role of The Criminal Defence LawyerDokument5 SeitenThe Role of The Criminal Defence LawyerSebastián MooreNoch keine Bewertungen
- CRIM LAW 1 Midterm ExamDokument16 SeitenCRIM LAW 1 Midterm ExamMichyLG100% (4)
- Mercado - Assignment 2Dokument8 SeitenMercado - Assignment 2Sophia Ysabelle Mercado (sophie)Noch keine Bewertungen
- Sample ManifestationDokument2 SeitenSample ManifestationChevrolie Maglasang-IsotoNoch keine Bewertungen
- Atizado vs. PeopleDokument1 SeiteAtizado vs. PeopleRieland CuevasNoch keine Bewertungen
- CALAUS vs. BUYA, ARIZALA-Falsification of Public Document, Theft, Estafa - RESOLUTIONDokument8 SeitenCALAUS vs. BUYA, ARIZALA-Falsification of Public Document, Theft, Estafa - RESOLUTIONNafiesa ImlaniNoch keine Bewertungen
- Victim Impact StatementDokument108 SeitenVictim Impact StatementJanet Tal-udanNoch keine Bewertungen
- Julito Sagales V. Rustans Commercial G.R. No. 166554 FactsDokument2 SeitenJulito Sagales V. Rustans Commercial G.R. No. 166554 FactsKing Monteclaro MonterealNoch keine Bewertungen
- 4.digested Manliclic v. CalaunanDokument3 Seiten4.digested Manliclic v. CalaunanArrianne ObiasNoch keine Bewertungen
- GR No 99026Dokument5 SeitenGR No 99026Cherry UrsuaNoch keine Bewertungen
- WHO Vs Aquino Case DigestDokument2 SeitenWHO Vs Aquino Case DigestMaria Cherrylen Castor Quijada100% (3)
- 3) 342 Scra 20Dokument25 Seiten3) 342 Scra 20LoveAnneNoch keine Bewertungen
- Gomez v. CA GR No. 127692 March 10 2004Dokument6 SeitenGomez v. CA GR No. 127692 March 10 2004Joseph John Santos RonquilloNoch keine Bewertungen
- Alfonso V PasayDokument3 SeitenAlfonso V PasayNikki Estores GonzalesNoch keine Bewertungen
- Plaintiff-Appellee Vs Vs Defendants-Appellants Pedro C. Quinto Alejo Mabanag Tomas B. TadeoDokument5 SeitenPlaintiff-Appellee Vs Vs Defendants-Appellants Pedro C. Quinto Alejo Mabanag Tomas B. TadeomenggayubeNoch keine Bewertungen
- Reciprocal ObligationsDokument6 SeitenReciprocal ObligationsSolarEclipp CandelansaNoch keine Bewertungen
- Republic vs. Yu - Res JudicataDokument9 SeitenRepublic vs. Yu - Res JudicataJennyNoch keine Bewertungen