Beruflich Dokumente
Kultur Dokumente
NCP Oedia
Hochgeladen von
Kimberly Gonzaga Vasquez0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
10 Ansichten5 Seitenjjj
Originaltitel
ncp-oedia
Copyright
© © All Rights Reserved
Verfügbare Formate
DOCX, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenjjj
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
10 Ansichten5 SeitenNCP Oedia
Hochgeladen von
Kimberly Gonzaga Vasquezjjj
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 5
Name of Patient: C.V Age: 1 year old Male Room/Bed No.
: 213-1
Chief Complaint: Bronchial asthma Physician: Dr. T
Diagnosis:
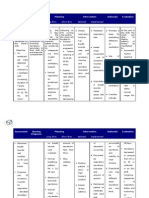
DATE CUES NEED NURSING DIAGNOSIS PATIENT OUTCOME NURSING INTERVENTIONS IMPLEMENTATION EVALUATION
TIME
M Subjective: A Ineffective breathing After 4 hours of 1.) Monitor Oxygen Saturation
A “Naglisod man C pattern related to nursing intervention using Pulse Oximeter.
R gud na sya ug T bronchial asthma as the patient will be able R: Oxygen Saturation of less
C ginahawa I evidence by dyspnea, to established than 90% indicates problems
H maong gidala V fast breathing, respiratory rate within with oxygenation.
namo sya diri I expiratory wheezes normal limits. 2.) Elevate head of the bed,
0 ospital, naa pud T and tachypnea. encourage early ambulation or
5 na sya asthma” Y change the client’s position
as verbalized every 2 hours.
2 by the mother. & R: It will allow to take
0 advantage of the gravity
2 Objective: E decreasing pressure on the
0 -dyspnea X diaphragm and enhancing
@ -fast breathing E drainage of/ventilation to
RR: 51 bpm R different lung segments.
CR: 155 bpm C 3.) Encourage parents to
-expiratory I prepare warm water for
wheezing S bathing and use humidifier.
-irritable E R: to help open the airways
-tachypnea and ease the breathing.
-presence of 3.) Position the child sitting or
O2 inhalation upright when giving sips of
via facemask water.
-oxygen R: Sitting up straight will
saturated help to open the airways,
machine making it easier for air to move
through the lungs.
-Prescription of 4.) Administer medications
salbutamol given and prescribed assuring
nebulization, its right dose, right time and
Ipratropium right patient.
Bromide R: It is an important tool for
nebulization. ensuring the health of these
individuals as well as
managing their health care
costs
5.) Observe for breathing
patterns.
R: Unusual breathing patterns
may imply an underlying
disease process or
dysfunction.
6.) Monitor the respiratory rate
as well as its corresponding
rate and rhythm.
R: Changes in the respiratory
rate and rhythm may indicate
an early sign of impending
respiratory distress.
7.) Encourage watcher to pray
with the child.
R: to strengthen spiritual
relationship
8.) Monitor for diaphragmatic
muscle fatigue or weakness
(paradoxical motion).
R: Paradoxical movement of
the abdomen (an inward
versus outward movement
during inspiration) is indicative
of respiratory muscle fatigue
and weakness
9.) Stay with the patient during
acute episodes of respiratory
distress.
R: This will reduce the patient’s
anxiety, thereby reducing
oxygen demand.
10.) Refer patient for
evaluation of exercise potential
and development of
individualized exercise
program.
R: Exercise promotes
conditioning of respiratory
muscles and patient’s sense
of well-being.
11.) Place patient with proper
body alignment for maximum
breathing pattern.
R: A sitting position permits
maximum lung excursion and
chest expansion.
12.) Encourage small frequent
meals.
R: This prevents crowding of
the diaphragm.
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- MedSurg Medications & TablesDokument71 SeitenMedSurg Medications & TablesSarah PlunkettNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- (MT 6322 - MYCO VIRO LAB) Unit 7 Laboratory Diagnosis For Negative-Sense (-) ssRNA VirusesDokument15 Seiten(MT 6322 - MYCO VIRO LAB) Unit 7 Laboratory Diagnosis For Negative-Sense (-) ssRNA VirusesAbbas MaghazehiNoch keine Bewertungen
- Radiographic Signs of Pulmonar DiseaseDokument10 SeitenRadiographic Signs of Pulmonar DiseaseMarleeng CáceresNoch keine Bewertungen
- Nursing Care Plan For Ineffective Airway ClearanceDokument7 SeitenNursing Care Plan For Ineffective Airway Clearancearlee marquez96% (118)
- Nursing Care Plan Problem: Difficulty of BreathingDokument5 SeitenNursing Care Plan Problem: Difficulty of BreathingIvan Louise Fajardo ManiquizNoch keine Bewertungen
- TRANS - Pediatric Patient ProblemsDokument4 SeitenTRANS - Pediatric Patient ProblemsRencel Hope Bañez100% (1)
- Respiratory SystemDokument41 SeitenRespiratory Systemshendie cadiatanNoch keine Bewertungen
- Srotas Final 2Dokument112 SeitenSrotas Final 2Sanjana SajjanarNoch keine Bewertungen
- Bronchial AsthmaDokument8 SeitenBronchial AsthmaBrylle CapiliNoch keine Bewertungen
- Case Study Pneumonia)Dokument20 SeitenCase Study Pneumonia)Jai - Ho83% (6)
- Medical Surgical TransesDokument144 SeitenMedical Surgical Transesmarlou agananNoch keine Bewertungen
- Functional Anatomy and Control of BreathingDokument34 SeitenFunctional Anatomy and Control of BreathingIvan Yudha PradityaNoch keine Bewertungen
- AtelektasisDokument10 SeitenAtelektasisSaputri AnggiNoch keine Bewertungen
- CH 15 Respiratory Practice Exam: StudentDokument10 SeitenCH 15 Respiratory Practice Exam: StudentSevilla ErnestdonNoch keine Bewertungen
- How Physiotherapy Helps - Patient StoriesDokument2 SeitenHow Physiotherapy Helps - Patient StoriesDobreanu Bianca100% (1)
- Aerosol DeliveryDokument63 SeitenAerosol DeliveryviaereaNoch keine Bewertungen
- NCP 1 Ineffective Airway ClearanceDokument6 SeitenNCP 1 Ineffective Airway ClearanceJezebhel ArestaNoch keine Bewertungen
- Obstructive Versus Restrictive Pulmonary DiseaseDokument47 SeitenObstructive Versus Restrictive Pulmonary DiseaseAntony WaithakaNoch keine Bewertungen
- Circulatory and Respiratory Systems - Module 3Dokument47 SeitenCirculatory and Respiratory Systems - Module 3CaityNoch keine Bewertungen
- PhysioEx Exercise 7 Activity 2Dokument7 SeitenPhysioEx Exercise 7 Activity 2ian tapiaNoch keine Bewertungen
- 5 Bronchiolitis Nursing Care Plans - NurseslabsDokument14 Seiten5 Bronchiolitis Nursing Care Plans - NurseslabsAnnapoorna SHNoch keine Bewertungen
- MsdsDokument6 SeitenMsdsRUFUSNoch keine Bewertungen
- Respiratory System - TransesDokument4 SeitenRespiratory System - TransesMLS1C - PLARISAN, VALENT DAVENoch keine Bewertungen
- pg1-33 of Pneumothorax Case StudyDokument36 Seitenpg1-33 of Pneumothorax Case StudyikemasNoch keine Bewertungen
- NCPDokument3 SeitenNCPDyanne BautistaNoch keine Bewertungen
- Nursing Care Plan Cues Nursing Diagnosis Rationale Planning Intervention Rationale Evaluation General Objectives: IndependentDokument2 SeitenNursing Care Plan Cues Nursing Diagnosis Rationale Planning Intervention Rationale Evaluation General Objectives: IndependentEden Marie FranciscoNoch keine Bewertungen
- Unit 3 Anatomy of Respiratory System: External Respiration. The Exchange of Gases Between The Blood in The Capillaries ofDokument35 SeitenUnit 3 Anatomy of Respiratory System: External Respiration. The Exchange of Gases Between The Blood in The Capillaries ofAnne RonquilloNoch keine Bewertungen
- BronchosDokument3 SeitenBronchosNAENAENoch keine Bewertungen
- Nursing Care Plan For Ineffective Airway ClearanceDokument6 SeitenNursing Care Plan For Ineffective Airway ClearanceCaroline ChaNoch keine Bewertungen
- Third Hand Smoke FeatureDokument5 SeitenThird Hand Smoke Featureapi-278601052Noch keine Bewertungen