Beruflich Dokumente
Kultur Dokumente
Bone Reviewer
Hochgeladen von
AALIYAH REIGN MAPUSAOOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Bone Reviewer
Hochgeladen von
AALIYAH REIGN MAPUSAOCopyright:
Verfügbare Formate
BONE Bone cells
• Specialized connective tissue composed Osteoblasts
of bone matrix (calcified ECM) • Originates from mesenchymal stem cells
• Produce organic components of bone
Bone tissue
matrix (type I collagen fibers,
• Provides support proteoglycans, and matricellular
• Protect vital organs (cranial and thoracic glycoproteins such as osteonectin)
cavities) • are polarized cells with ultrastructural
• Encloses internal (medullary) cavities features denoting active protein
containing bone marrow synthesis and secretion during process
• Reservoir for calcium, phosphate, and of matrix synthesis and calcification
other ions that can be stored and • release membrane-enclosed matrix
release to maintain concentrations in vesicles rich in alkaline phosphate and
body fluids other enzymes
• Three (3) major cell types: o matrix vesicles raise local
o Osteocytes (Gr. osteon, bone; concentration of PO43- ions
kytos, cell) • Active osteoblasts
§ found in the cavities o Located exclusively at the
(lacunae) between bone surfaces of bone matrix, which
matrix layers (lamellae), are bound by integrins, and
with cytoplasmic forming single layer of cuboidal
processes in small cells joined by adherent and gap
canaliculi (L. canalis, junctions
canal) that extend to • Bone lining cells
the matrix o Flattened osteoblasts that cover
o Osteoblasts (osteon; Gr. blastos, the matrix surface
germ) • Majority of osteoblasts undergo
§ Growing cells which apoptosis when synthetic activity is
synthesize and secrete
completed
organic components of
• Osteoid
matrix
o Layer of unique collagen-rich
o Osteoclasts (osteon; Gr. klastos,
material between the osteoblast
broken)
layer and preexisting bone
§ giant, multinucleated
surface
cells involved in
o Produced when matrix
removing calcified bone
components are secreted in the
matrix and remodeling
cell surface and come in contact
bone tissue
with the bone matrix
• Endosteum o Calcium salts
o internal surface surrounding the § Responsible of bone
marrow cavity appositional growth
o layers of connective tissue
• Osteocalcin
containing osteogenic cells
o a Vitamin K-dependent
• Periosteum
polypeptide, noncollagen
o External surface protein secreted by osteoblasts
o Layers of CT containing o binds and concentrates Ca2+
osteogenic cells
Osteocytes Bone Matrix
• differentiated from osteoblasts that • About 50% of the dry weight of bone
became trapped with the material they matrix is inorganic materials;
secrete o Calcium hydroxyapatite; most
• significantly less rER; smaller Golgi abundant
complexes; and more condensed nuclear o Bicarbonate, citrate,
chromatin than osteoblasts magnesium, potassium, sodium
• some included proteins: paracrine and ions
endocrine (both help regulate bone o Significant quantities of
remodeling noncrystalline calcium
• the cells extend many long dendritic phosphate
processes during the transition of o Surface of hydroxyapatite
osteoblasts to osteoclasts; also become crystals are hydrated; facilitating
surrounded by calcifying matrix exchange of ions between
• also communicate with nearby minerals and fluids
osteoblasts and bone lining cells via gap • Organic matter embedded in the
junctions at the ends of their processes calcified ECM is 90% type I collagen; also
• maintain the calcified matrix includes small proteoglycans and
• death if followed by rapid matrix osteonectin (multiadhesive
resorption glycoproteins)
• Osteocalcin
Osteoclasts o calcium binding proteins
• very large, motile cells, multinucleated • osteocalcin and phosphatases released
(essential for matrix resorption during from cells in matrix vesicles promote
bone growth and remodeling) calcification of the matrix
• originates from the fusion of bone • association of minerals with collagen
marrow-derived monocytes, causing its fibers during calcification provides
characteristics hardness and resistance required for
• osteoclasts development (formation and bone function
activity) requires two polypeptides • decalcified bone matrix is usually
produced by osteoblasts acidophilic due to high collagen content;
o macrophage-colony-stimulating decalcified bone becomes soft and
factor (M-CSF) pliable like connective tissues but can
o receptor activator of nuclear still hold its shape
factor-kB ligand (RANKL)
• Resorption lacunae (or Howship lacunae) Periosteum and Endosteum
o Enzymatically etched • connective tissue covering the external
depressions or cavities in the and internal surfaces of all bones
matrix Periosteum
o Where osteoclasts on the bone • with an outer fiber layer of dense
surface lie during bone connective tissue containing mostly
resorption bundled type I collagen and also
• Osteoclast activity is controlled by local fibroblasts and blood vessels
signaling factors from other bone cells • Perforating (or Sharpey) fibers
o bundles of periosteal collagen
o penetrate the bone matrix;
o bind the periosteum to the
bone In flat bones:
• periosteum’s inner layer is cellular; o Flat bones that form calvaria (skullcap)
osteoblasts, bone lining cells, and have two (2) layers of compact bone
osteoprogenitor cells (mesenchymal (plates) and separated by a thick layer of
stem cells) cancellous bone (diploë)
Endosteum Lamellar bone
• very thin internal layer • Common organization of compact and
• covers small trabeculae of bony matrix cancellous bone in adults
that project into the marrow cavities • Characterized of multiple layers of
• also contains osteoprogenitor cells, lamellae (3-7 um thick)
osteoblasts, bone lining cells, but within • Lamellae
a sparse, delicate matrix of collagen o Parallel sheets or concentrically
fibers around a central canal
o In each lamella, type I collagen
are aligned
Types of Bone • Osteon (or Haversian system)
• Compact (cortical) bone o Refers to the complex of
o dense area near the surface concentric lamellae
o 80% of the total bone mass o Surrounding a central canal that
• Cancellous (trabecular) bone contains small blood vessels,
o 20% of the bone mass nerves, and endosteum
• Microscopic level of compact and o All cells of an osteon receive
cancellous bone shows two (2) types of nutrients and oxygen from
organization: vessels in the central canal
o Lamellar bone o Cement line
o Woven bone § Outer boundary of each
osteon that includes
In long bones: many more noncollagen
Epiphyses (Gr. epiphysis, an excrescence) proteins in addition to
o Bulbous ends of long bones mineral and collagen
o Composed of cancellous bone covered • Lacunae
by a thin layer of compact cortical bone o Found between successive
lamella; Each one with osteocyte
Diaphysis (Gr. diaphysis, a growing between) • Perforating canals (or Volkmann canals)
o Cylindrical part of long bones o have few concentric lamella
o Almost totally dense compact bone with o all central osteonic and
a thin region of cancellous bone on the perforating canals form when
inner surface around the central marrow matrix is laid down around areas
cavity with preexisting blood vessels
• Interstitial lamellae
In short bones: o Numerous, irregularly shaped
o wrist, ankles groups of parallel lamellae
o Have cores of cancellous bone scattered among the intact
surrounded completely by compact osteons
bone
o Lamellae remaining from • In both processes, woven bone is
osteons partially destroyed by produced first and then replaced by
osteoclasts during growth and stronger lamellar bone
remodeling of bone
• External circumferential lamella Intramembranous ossification
o Immediately beneath the • Which most flat bones begin to form
periosteum o Takes place within condensed
• Inner circumferential lamellae sheets of embryonic
o Around the marrow cavity mesenchymal tissue
• Most bones of the skull, jaws, scapula,
Bone remodeling clavicle are formed embryonically by
• Occurs continuously throughout life intramembranous ossification
• In compact bone, remodeling resorbs • Ossification centers
parts of old osteons and produces new o Where bone formation begins
ones o Areas in which osteoprogenitor
• 5%-10% of bones in healthy adults turns cells arise, proliferate, and form
over annually incomplete layers of osteoblasts
around a network of developing
Woven bone capillaries
• Nonlamellar and characterized by • Fontanelles (or soft spots) on the head
random disposition of type I collagen of newborns are areas of the skull in
fibers which the membranous tissue is not yet
• First bone tissue to appear in embryonic ossified
development and in fracture repair
• Usually temporary and replaced by Endochondral ossification (Gr. endon, within;
lamellar bone in adults chondros, cartilage)
• Typically has a lower mineral content • Takes place within hyaline cartilage
and higher proportion of osteocytes shaped as a small version of the bone to
than mature lamellar bone be formed
o Reflects that immature woven • Forms most bones of the body and
bone forms more quickly but studied in long bones
has less strength than lamellar • Bone collar
bone o Produced by osteoblasts that
differentiate within the
Osteogenesis (or bone development) perichondrium (trans. To
Occurs by one of two processes periosteum) around the
• Intramembranous ossification cartilage model diaphysis
o Osteoblasts differentiate • Primary ossification center
directly from mesenchyme and o forms in the diaphysis
begin secreting osteoid o beginning in many embryonic
• Endochondral ossification bones as early as the first
o Preexisting matril of hyaline trimester
cartilage is eroded and invaded • Secondary ossification center
by osteoblasts, then begin o Appear later at the epiphyses of
osteoid production the cartilage and develop in a
similar manner
• After the primary and secondary matrix calcification by
ossification centers, two (2) regions of the formation of
cartilage remain: hydroxyapatite crystals
o Articular cartilage o Zone of ossification
§ within the joints § Where bone tissue first
between long bones appears
during adult life § Osteoblasts settle in a
o Epiphyseal cartilage (or layer over the spicules
epiphyseal plate/ growth plate) of calcified cartilage
§ Connects each epiphysis matrix and secrete
to the diaphysis and osteoid which becomes
allows longitudinal bone woven bone; this woven
growth bone is remodeled as
§ Responsible for the lamellar bone
growth in length of • Appositional growth
bone and disappears o Growth in the circumference of
upon development at long bones through the activity
adulthood (age 20) of osteoblasts developing from
• Starting with the cartilage and farthest osteoprogenitor cells in the
from the ossification center in the periosteum
diaphysis: o Begins with the formation of the
o Zone of reserve (or resting) bone collar on the cartilaginous
cartilage diaphysis
§ Composed of typical
hyaline cartilage Bone remodeling and repair
o Proliferative zone • Bone turnover
§ Cartilage cells divide o Very active in young children
repeatedly (200x faster than adults)
§ Enlarge and secrete • Bone remodeling
more type II collagen o Continuous renewal of skeleton
and proteoglycans in adults
§ Become organized into o Involves coordinated, localized
columns parallel to the cellular activities for bone
long axis of bone resorption and bone formation
o Zone of hypertrophy • Bone repair
§ Contains swollen, o Bone has excellent capacity for
terminally differentiated repair because it’s well
chondrocytes which vascularized and it contains
compress the matrix osteoprogenitor stem cells in the
into aligned spicules periosteum, endosteum, and
and stiffen it by marrow
secretion of type X o Signaling molecules and
collagen processes active in bone
o Zone of calcified cartilage remodeling after a fracture or
§ Chondrocytes about to other damage uses cells
undergo apoptosis
release matrix vesicles
and osteocalcin to begin
• Callus
o Soft callus of fibrocartilage-like Major subtypes of synarthroses:
tissue produced by the • sutures
activation of periosteal o thin layers of dense
fibroblasts connective tissue with
o Hard callus of woven bone osteogenic cells; unites
replaces the soft callus and soon skull bones in children
remodeled into lamellar bone • syndesmoses
o join bones by dense
Metabolic role of bone connective tissue
• Skeleton serves as calcium reservoir • symphyses
containing 99% of body’s total calcium o have a thick pad of
• Concentration of calcium in blood and fibrocartilage between
tissues is generally stable due to the the thin articular
continuous interchange between blood cartilage covering the
calcium and bone calcium ends of the bones
• Ca2+ mobilization is regulated mainly by o all symphyses
paracrine interactions among bone cells (intervertebral discs,
• Polypeptide hormones influencing pubic symphysis) occur
calcium homeostasis: in the midline of the
o Parathyroid hormone (PTH) body
§ Raises low blood Intervertebral discs
calcium levels by • large symphyses between the
stimulating osteoclasts articular surfaces of successive
and osteoblasts to bony vertebral bodies
resorb bone matric and • annulus fibrosus
release calcium ions o outer portion of each
o Calcitonin discs
§ Produced within the o consists of concentric
thyroid gland fibrocartilage laminae;
§ Reduce elevated blood collagen fibers are
calcium levels by arranged orthogonally
opposing the effects of (intersecting or lying at
PTH in bone right angles) in adjacent
layers
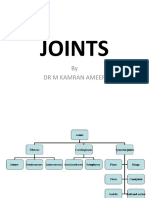
Joints • nucleus pulposus
• Regions where adjacent bones are o gel-like body situated in
capped and held together by other the center of the
connective tissues annulus fibrosus
• Synarthoses (Gr. syn, together; arthrosis, o allows each disc to
articulation) function as shock
o determines degree of absorber
movement between bones
o allow limited or no movement
o subdivided into fibrous and
cartilaginous joints
o unites skull bones in adults
Joints are classified as diarthroses
Diarthroses
• permit bone movement
• elbows and knees unite long bones and
allow great mobility
• ligaments and dense connective tissue
maintain alignment of bones
• joint cavity
o enclosed by the capsule
o contains synovial fluid (clear,
viscous liquid)
o lined by synovial membrane
• synovial membrane
o (specialized connective tissue)
o extends folds and villi into the
joint cavity
o produces synovial fluid
characterized by two specialized cells:
o macrophage-like synovial cells
(or type A cells)
§ derived from blood
monocytes
§ remove wear-and-tear
debris from the synovial
fluid
§ represents 25% cell
lining of the synovium
§ important in regulating
inflammatory events
within diarthrotic joints
o fibroblastic synovial cell (or type
B cells)
§ produce abundant
hyaluronan and smaller
amounts of
proteoglycans
§ transported by water
from the capillaries into
the joint cavity to form
synovial fluid
• synovial fluid
o lubricates the joint
o reduce friction on all internal
surfaces
o supplies nutrients and oxygen to
articular cartilage
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Chapter 5: Connective TissueDokument5 SeitenChapter 5: Connective TissueAALIYAH REIGN MAPUSAONoch keine Bewertungen
- CHAPTER 4: Epithelial TissueDokument3 SeitenCHAPTER 4: Epithelial TissueAALIYAH REIGN MAPUSAONoch keine Bewertungen
- Chapter 6: Adipose Tissue: Two Major Types of AdiposeDokument3 SeitenChapter 6: Adipose Tissue: Two Major Types of AdiposeAALIYAH REIGN MAPUSAONoch keine Bewertungen
- Experiment 8 Nucleic Acids PDFDokument19 SeitenExperiment 8 Nucleic Acids PDFAALIYAH REIGN MAPUSAONoch keine Bewertungen
- Experiment 10 - Digestion PDFDokument17 SeitenExperiment 10 - Digestion PDFAALIYAH REIGN MAPUSAONoch keine Bewertungen
- Experiment 9 - Vitamin Analysis PDFDokument14 SeitenExperiment 9 - Vitamin Analysis PDFAALIYAH REIGN MAPUSAONoch keine Bewertungen
- Experiment 11 - Non Protein Nitrogen PDFDokument26 SeitenExperiment 11 - Non Protein Nitrogen PDFAALIYAH REIGN MAPUSAONoch keine Bewertungen
- Rumple LeedeDokument3 SeitenRumple LeedeIrene Dewi Isjwara40% (5)
- Blood Gases: Arterial VenousDokument11 SeitenBlood Gases: Arterial VenousDerper WatsonNoch keine Bewertungen
- Anemia With PregnancyDokument22 SeitenAnemia With PregnancyRadwa EbedNoch keine Bewertungen
- Solution Manual For Laboratory Manual For Anatomy Physiology Featuring Martini Art Main Version Plus Masteringap With Etext Package 5 e Michael G WoodDokument4 SeitenSolution Manual For Laboratory Manual For Anatomy Physiology Featuring Martini Art Main Version Plus Masteringap With Etext Package 5 e Michael G WoodKarenAcevedotkoi100% (40)
- Coagulation Disorders in PregnancyDokument20 SeitenCoagulation Disorders in PregnancyHannaTashiaClaudiaNoch keine Bewertungen
- Approach To Bleeding NeonateDokument20 SeitenApproach To Bleeding NeonateIndranil DuttaNoch keine Bewertungen
- Zulekha Hospital LLC - (DUBAI) : Print DT: 20/05/2023 10:02Dokument2 SeitenZulekha Hospital LLC - (DUBAI) : Print DT: 20/05/2023 10:02Abc AbcNoch keine Bewertungen
- RBCDokument3 SeitenRBCSupreeth RulesNoch keine Bewertungen
- Functional Matrix HypothesisDokument3 SeitenFunctional Matrix HypothesisMuhammad Najib bin JamailNoch keine Bewertungen
- Electrical Impedance: Hematology AnalyzerDokument2 SeitenElectrical Impedance: Hematology AnalyzerAzura JKNoch keine Bewertungen
- Pathology Outlines - Abnormal PT and PTT - CausesDokument1 SeitePathology Outlines - Abnormal PT and PTT - CausesShane AranetaNoch keine Bewertungen
- HDB - Tropical Haematology and Blood Transfusion Laboratory NotesDokument78 SeitenHDB - Tropical Haematology and Blood Transfusion Laboratory NotesAbdul AleemNoch keine Bewertungen
- Autologous Blood Products and Their Roles Within DentistryDokument6 SeitenAutologous Blood Products and Their Roles Within DentistryMax FaxNoch keine Bewertungen
- Indonesian Journal of Nursing Research (IJNR)Dokument7 SeitenIndonesian Journal of Nursing Research (IJNR)mulyono yonoNoch keine Bewertungen
- Lupus AnticoagulantDokument27 SeitenLupus AnticoagulantAndrew Arnold David Villanueva100% (1)
- Skeletal Muscle and The Molecular Basis of Contraction-TextDokument23 SeitenSkeletal Muscle and The Molecular Basis of Contraction-TextSuraj BisoiNoch keine Bewertungen
- Humaclot JuniorDokument40 SeitenHumaclot JuniorJonatan Rolong Ibáñez100% (3)
- Primary and Secondary Thrombocytosis in ChildhoodDokument13 SeitenPrimary and Secondary Thrombocytosis in ChildhoodSofia RuanoNoch keine Bewertungen
- 0259147-HLH CCO-0122-7259: Lab No: Patient NoDokument2 Seiten0259147-HLH CCO-0122-7259: Lab No: Patient NoSami UllahNoch keine Bewertungen
- Diagon Blood Controls PRESENTACION 2017Dokument47 SeitenDiagon Blood Controls PRESENTACION 2017Leidy Tatiana RiveraNoch keine Bewertungen
- Sarthak Mechanism of Blood ClottingDokument42 SeitenSarthak Mechanism of Blood ClottingVishal MishraNoch keine Bewertungen
- Group 5 PhysioEx Experiment 2Dokument27 SeitenGroup 5 PhysioEx Experiment 2Liane LomioNoch keine Bewertungen
- Worksheet - RLE 1 Significance of Laboratory ResultsDokument9 SeitenWorksheet - RLE 1 Significance of Laboratory Results1H - Althea VestilNoch keine Bewertungen
- EL TENDON Valoracion y Tratamiento en Fi-121-180Dokument60 SeitenEL TENDON Valoracion y Tratamiento en Fi-121-180doradoNoch keine Bewertungen
- Joints: by DR M Kamran AmeerDokument22 SeitenJoints: by DR M Kamran AmeerKamran AmeerNoch keine Bewertungen
- ABO Blood Group SystemDokument26 SeitenABO Blood Group SystemFahimNoch keine Bewertungen
- 8a. Skeletal Lab-HPWDokument10 Seiten8a. Skeletal Lab-HPWTrinh Tat-TranNoch keine Bewertungen
- Platelet-Rich Plasma: Clinical Applications in DentistryDokument4 SeitenPlatelet-Rich Plasma: Clinical Applications in DentistryVijithNoch keine Bewertungen
- Dissecting A Chicken Wing: Lab SafetyDokument21 SeitenDissecting A Chicken Wing: Lab SafetyWynona Louiz TangcoNoch keine Bewertungen
- DR - Suneetha 3 Year Post Graduate: Haemostasis in EndodonticsDokument91 SeitenDR - Suneetha 3 Year Post Graduate: Haemostasis in EndodonticsElika VaishnaviNoch keine Bewertungen