Beruflich Dokumente
Kultur Dokumente
Review: Tamara G Fong, Daniel Davis, Matthew E Growdon, Asha Albuquerque, Sharon K Inouye
Hochgeladen von
Andi Mahifa 93Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Review: Tamara G Fong, Daniel Davis, Matthew E Growdon, Asha Albuquerque, Sharon K Inouye
Hochgeladen von
Andi Mahifa 93Copyright:
Verfügbare Formate
Review
The interface between delirium and dementia in elderly adults
Tamara G Fong*, Daniel Davis*, Matthew E Growdon, Asha Albuquerque, Sharon K Inouye
Delirium and dementia are two of the most common causes of cognitive impairment in older populations, yet their Lancet Neurol 2015
interrelation remains poorly understood. Previous studies have shown that dementia is the leading risk factor for Published Online
delirium and that delirium is an independent risk factor for subsequent development of dementia. However, a major June 30, 2015
http://dx.doi.org/10.1016/
area of controversy is whether delirium is simply a marker of vulnerability to dementia, whether the effect of delirium S1474-4422(15)00101-5
is solely related to its precipitating factors, or whether delirium itself can cause permanent neuronal damage and lead
*Both authors contributed
to dementia. Ultimately, all of these hypotheses are likely to be true. Emerging evidence from epidemiological, equally to this work
clinicopathological, neuroimaging, biomarker, and experimental studies lends support to a strong relation between Department of Neurology
delirium and dementia, and to both shared and distinct pathological mechanisms. New preventive and therapeutic (T G Fong PhD) and Department
approaches that target delirium might offer a sought-after opportunity for early intervention, preservation of cognitive of Medicine
(Prof S K Inouye MD), Beth Israel
reserve, and prevention of irreversible cognitive decline in ageing.
Deaconess Medical Center,
Harvard Medical School,
Introduction epidemiological, clinicopathological, neuroimaging, Boston, MA, USA; Aging Brain
With the unprecedented increases in the proportion of biomarker, and experimental evidence linking delirium Center, Institute for Aging
Research, Hebrew SeniorLife,
individuals older than 75 years in most industrialised and dementia, with the aim of understanding the nature
Boston, MA, USA (T G Fong,
countries, cognitive impairment is an increasingly of the relation between the two disorders. In each of A Albuquerque BA,
frequent problem, calling for a thoughtful and effective these areas, we highlight important gaps in knowledge Prof S K Inouye); MRC Unit for
approach to its recognition and management. Delirium and future directions for research. Furthermore, we Lifelong Health and Ageing,
UCL, London, UK (D Davis PhD);
and dementia are among the most common causes of discuss potential mechanisms underlying the links
Department of Medicine,
cognitive impairment in clinical settings, yet they are between delirium and dementia, and their implications Brigham and Women’s Hospital
often either unrecognised or mistaken for each other. for treatment. and Harvard Medical School,
Dementia, an insidious neurodegenerative condition, is Boston, MA, USA
(M E Growdon MD)
characterised by chronic and progressive cognitive Distinguishing delirium from dementia
Correspondence to:
decline from a previous level of performance in one or Until now, dementia and delirium have been conceptualised
Prof Sharon K Inouye, Aging
more cognitive domains that interferes with as distinct and mutually exclusive conditions. Indeed, the Brain Center, Institute for Aging
independence in everyday activities.1 By contrast, fifth edition of the Diagnostic and Statistical Manual of Research, Hebrew SeniorLife,
delirium is a syndrome manifesting as an acute change Mental Disorders (DSM-5) states that dementia should not Boston, MA 02131, USA
agingbraincenter@hsl.harvard.
in mental status that is characterised by inattention and be diagnosed in the face of delirium and that delirium
edu
disturbance in cognition that develops over a short period should not be diagnosed when symptoms can be “better
of time with a fluctuating course of symptoms. Delirium accounted for by a pre-existing, established, or evolving
is a common, serious, and often fatal disorder that affects dementia”.1 Distinguishing between the two diagnoses in
as many as 50% of people older than 65 years who are the clinical setting can be difficult, even for experienced
admitted to hospital.2 It is consistently associated with clinicians. Delirium symptoms can persist for months or
increased cognitive impairment and functional decline,2 even years,4–9 and the recognised conditions of persistent
and is preventable in about 30–40% of cases. Typically, delirium and reversible dementia blur the boundaries
evidence exists for a medical or multifactorial cause for between these previously demarcated syndromes of
delirium;1 predisposing and precipitating factors for cognitive impairment.1 The differentiation between
delirium have been derived from previously validated delirium and dementia is of crucial importance, since their
predictive models (panel).2 assessment and clinical management are distinct. Many
Delirium and dementia commonly coexist, with pre- signs and symptoms can be used to distinguish delirium
existing dementia being a leading risk factor for delirium. from dementia (table 1).10–12 Most prominently, the onset of
Although the substantial overlap between these delirium is typically abrupt, over hours to days, whereas the
conditions is recognised, the nature of their interrelation onset of dementia is insidious and progressive, over
remains unclear. Moreover, shared pathophysiological months to years. With delirium, attention and level of
mechanisms—including cholinergic deficiency, consciousness are reduced and fluctuating; with dementia,
inflammation, and reduced cerebral oxidative these cognitive domains typically remain intact until the
metabolism2,3—have been postulated for these advanced stages. Ultimately, the differentiation might
syndromes. A fundamental understanding of the depend on the presence of an acute change in mental
interface between delirium and dementia could provide status or behaviour from baseline noted by an informed
an important opportunity to advance our caregiver, or could be established only in retrospect by
conceptualisation of and treatment approaches to both resolution of symptoms after precipitating factors have
conditions. been removed or the acute illness has been treated. If
In this Review, we briefly describe how delirium can be uncertain, mental status changes should be treated as
distinguished from dementia, and examine the delirium, until proven otherwise.
www.thelancet.com/neurology Published online June 30, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00101-5 1
Review
itself might cause permanent neuronal damage and
Panel: Predisposing and precipitating factors for delirium from validated predictive lead to dementia. With regard to the question of whether
models2 delirium itself leads to dementia, clinically, the
Predisposing factors development of delirium might have direct toxic effects
• Dementia or pre-existing cognitive impairment related to periods of lethargy, psychomotor retardation,
• History of delirium psychomotor agitation, or unsafe behaviours. The
• Functional impairment lethargy and psychomotor retardation could result in
• Sensory impairment—eg, vision impairment and hearing impairment immobility and related complications, including but not
• Comorbidity or severity of illness limited to aspiration pneumonia, respiratory com-
• Depression promise, decreased oral intake with dehydration or
• History of transient ischaemia or stroke malnutrition, pressure ulcers, urinary tract infection,
• Alcohol abuse deep-vein thrombosis, and pulmonary emboli.13
• Older age Complications from psychomotor agitation and unsafe
behaviour might include falls and use of antipsychotics
Precipitating factors and other sedative drugs or physical restraints. Thus,
• Polypharmacy, use of psychoactive or sedative-hypnotic drugs the occurrence of delirium itself might set off a cascade
• Use of physical restraints of noxious stimuli that could adversely affect the brain.
• Use of bladder catheter Several mechanisms have so far been hypothesised to
• Physiological and metabolic abnormalities—eg, high blood-urea-nitrogen:creatinine explain how delirium might contribute to permanent
ratio, abnormal sodium, glucose, or potassium concentrations in serum, hypoxaemia, neuronal damage and dementia. These include
or metabolic acidosis neurotoxicity (eg, drugs, anaesthesia, endotoxins),
• Infection inflammation, chronic stress, neuronal damage (eg,
• Any iatrogenic event prolonged ischaemia, hypoglycaemia, shock, sepsis),
• Major surgery acceleration of dementia pathology (eg, amyloid β [Aβ]
• Trauma or urgent admission to hospital and tau pathology), and diminished cognitive reserve
• Coma (figure).10,14–16 Certain insults, such as metabolic derange-
ments or particular drugs (eg, anticholinergics), might
directly cause neuronal dysfunction via alterations in
Delirium Dementia neurotransmitter concentrations (eg, acetylcholine
Onset Abrupt, although initial loss of mental Insidious and progressive deficiency17 or dopamine excess18). Hypoxia or cerebral
clarity can be subtle ischaemia might lead directly to cerebral dysfunction via
Duration Hours to days (although it can be Months to years impaired cerebral blood flow and metabolism. Some
prolonged in some cases)
anaesthetics might directly facilitate acceleration of Aβ
Attention Reduced ability to focus, sustain, or shift Normal except in severe dementia
attention is a hallmark feature that occurs
accumulation, leading to apoptosis and cholinergic
early in presentation dysfunction, which in turn could further accelerate or
Consciousness (ie, Fluctuating (thus assessment at multiple Generally intact initiate Aβ pathology.19 Infections or response to a
awareness of the timepoints is necessary); reduced level of stressor (eg, surgery or acute illness) can cause neuronal
environment) consciousness and impaired orientation dysfunction through activation of inflammatory
Speech Incoherent and disorganised; distractible in Ordered, but development of mechanisms.20 Neuronal injury in these cases can occur
conversation anomia or aphasia is possible
indirectly through a range of mechanisms, including
Cause Underlying medical condition, substance Underlying neurological process (eg,
intoxication, or side-effect of drugs amyloid β plaque accumulation in altered neurotransmission, apoptosis, activation of
Alzheimer’s disease) microglia and astrocytes, or a combination of these
Other features Hyperactive, hypoactive, and mixed forms, Symptoms vary depending on mechanisms, in turn leading to the production of free
as determined by the type of psychomotor underlying pathology (eg, radicals, complement factors, glutamate, and nitric
disturbance, are possible; disruption in fluctuations in cognition are a
oxide.21 Findings from various types of study, reviewed
sleep duration and architecture; perceptual feature of Lewy body dementia)
disturbances here, suggest the existence of important relations
between delirium and dementia, and yield new insights
These two syndromes have substantial overlapping features and can coexist in an individual patient.
into these syndromes, and their shared and distinct
Table 1: Comparative features of delirium and dementia pathological mechanisms.
Epidemiological evidence
Evidence linking delirium and dementia Large cohort studies suggest that cognitive impairment
The way in which delirium and dementia are linked is and dementia are important risk factors for delirium. In
the subject of debate. Delirium could be a marker of most of these studies, delirium has been assessed in
vulnerability to dementia, delirium might unmask populations that include patients with dementia. Studies
unrecognised dementia, the effect of delirium might be from a comprehensive review have examined pre-existing
solely related to its precipitating factors, or delirium cognitive impairment or dementia as risk factors for
2 www.thelancet.com/neurology Published online June 30, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00101-5
Review
delirium in validated predictive models that include Direct mechanisms
adjustment for important confounding variables
Stroke
(table 2).22–32 The studies included 5166 participants with Metabolic abnormalities Drugs
mean ages ranging from 68 to 85 years, recruited from
diverse settings, including hospital medical or geriatric Hypoxia Anaesthetics
medicine wards, emergency departments, and surgical
services. Cognitive baseline status was determined using • Accelerated
Aβ pathology
various approaches, including brief cognitive screening • Apoptosis
Delirium
tests (eg, Short Portable Mental Status Questionnaire33
and Mini-Mental State Examination34), proxy-based
• Alterations in
measures (eg, Informant Questionnaire on Cognitive neurotransmitter
Decline in the Elderly [IQCODE]35 and Blessed Dementia concentrations
• Neuronal dysfunction
Rating Scale36), clinician diagnosis, or chart documentation • Neuronal death
of dementia. Delirium was also measured using a range No dementia Dementia
of approaches, including the Confusion Assessment
Method,37 DSM editions III, III revised (IIIR), and IV,38–40 Indirect mechanisms
and the Delirium Observation Screening Scale.41 The
Systemic infection
proportion of individuals with delirium ranged from 9%
to 44% across these studies. Baseline cognitive impairment
or dementia is therefore an important independent risk Inflammation
factor for delirium, consistently increasing delirium risk Delirium
by two to five times (table 2).
Conversely, delirium is an independent risk factor for
long-term cognitive decline and dementia, according to
a comprehensive review of studies representing Exaggerated stress response Preclinical or
• Sympathetic nervous system pre-existing
4745 individuals (table 3).42–49 The studies vary in design, • Hypothalamic–pituitary–adrenal axis dementia
including population-based approaches, retrospective
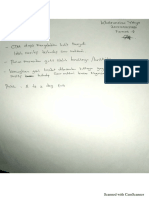
analyses of outpatients such as those attending memory Figure: A hypothetical model for the pathophysiological relation between
clinics, and assessment of intensive-care unit inpatients delirium and dementia
and patients undergoing elective surgery. Nonetheless, Aβ=amyloid β. Delirium is a known risk factor for new-onset dementia and
could arise as a direct result of factors such as hypoxia, metabolic abnormalities,
these studies consistently suggest that an episode of stroke, or drugs. In turn, delirium is associated with alterations in
delirium carries substantial dementia risk and an neurotransmitter concentrations, neuronal dysfunction, and neuronal death,
altered trajectory of cognitive recovery following surgical and could lead directly to dementia. Growing evidence shows that some
procedures. Cognitive outcomes were determined using anaesthetics associated with postoperative delirium might accelerate Aβ
pathology and cause apoptosis, which in turn might suggest a role for these
various measures, including neuropsychological anaesthetics in new-onset dementia. Delirium is also likely to be a marker of
assessments (eg, Automated Geriatric Examination for vulnerability in patients with preclinical or pre-existing dementia and might
Computer Assisted Taxonomy,50 Repeatable Battery for accelerate existing dementia. This might occur indirectly—eg, via inflammation
the Assessment of Neuropsychological Status,51 Blessed triggered by systemic infection or an exaggerated response to a stressor.
Information-Memory-Concentration test,36 and Mini-
Mental State Examination34), clinician diagnosis, or particularly those patients with prolonged delirium,
consensus panel diagnosis. Despite the many methods never returned to baseline. In a study of 821 intensive-
for operationalising delirium and dementia, the care unit patients,43 a longer duration of delirium was
findings are consistent and robust across the studies. independently associated with significantly worse global
For example, delirium was consistently associated with cognition and worse executive function scores on the
a significantly increased risk of both long-term cognitive basis of a neuropsychological battery at 3-month and
decline (ie, substantial declines on cognitive testing) 12-month follow-up. Moreover, clinical trial evidence
and dementia (odds ratios 6–41), with follow-up periods has suggested that treatment of delirium was associated
ranging from 1 year to 5 years after baseline assessment. with better cognition during follow-up.53 Although
A meta-analysis52 involving two studies with a total of postoperative cognitive dysfunction is not directly
241 patients showed that delirium was associated with linked to delirium, the scientific literature also suggests
an increased rate of incident dementia, even after persistent long-term cognitive impairment following
controlling for relevant confounders (adjusted relative surgery.54–56
risk 5·7, 95% CI 1·3–24·0). In another study of Careful follow-up studies have shown that people with
225 patients who had undergone cardiac surgery,45 dementia who develop delirium have worse outcomes
delirium resulted in a punctuated decline in cognitive than individuals with dementia alone,57 including
function, followed by recovery over 6–12 months in increased rates of readmission to hospital,
most patients; however, a substantial proportion, institutionalisation, mortality, and subsequent cognitive
www.thelancet.com/neurology Published online June 30, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00101-5 3
Review
Sample Sample size Cognitive baseline Delirium measure Mean age at Patients Adjusted effect
baseline with size (95% CI)
(years) delirium
Kennedy et al22 (2014) Patients aged ≥65 years admitted to 700 Documented dementia Prevalent delirium by 77 9% OR 4·3 (2·2–8·5)
emergency department by chart CAM
Koster et al23 (2013) Patients aged ≥70 years undergoing 300 MMSE <23 DOSS 74 17% OR 4·5 (1·9–13·0)
elective cardiac surgery
Moerman et al24 (2012) Patients aged ≥65 years with acute 378 Clinical diagnosis of Prevalent delirium by 84 27% OR 2·8 (1·7–4·6)
hip fracture dementia DSM-IV
Bo et al25 (2009) Patients aged ≥70 years admitted to 252 SPMSQ to establish Incident delirium by 82 11% RR 2·1 (1·6–2·6)
medical or geriatric wards presence and severity CAM
of cognitive
impairment
Rudolph et al26 (2009) Patients aged ≥60 years undergoing 122 in development Preoperative MMSE Incident delirium by 75 44% RR 1·3 (1·0–1·7)
elective cardiac surgery sample; 109 in ≤23 CAM
validation sample
Kalisvaart et al27 (2006) Patients aged ≥70 years undergoing 603 Preoperative MMSE Postoperative 78 12% RR 5·5 (3·6–8·6)
elective hip surgery <24 delirium by DSM-IV
and CAM
Wilson et al28 (2005) Patients aged ≥75 years admitted to 100 IQCODE to establish Incident delirium by 85 12% OR 3·2 (1·2–9·0)
acute medical wards presence of cognitive DSM-III
change over time
O’Keeffe et al29 (1996) Patients with acute medical 225 Clinical diagnosis of Incident delirium by 82 28% OR 4·8 (2·0–11·6)
admissions to geriatric units dementia or BDRS ≥4 DSM-III
Marcantonio et al30 (1994) Patients aged ≥50 years admitted to 1341 TICS <30 Postoperative 68 9% OR 4·2 (2·4–7·3)
elective surgical units delirium by CAM
Pompei et al31 (1994) Patients aged ≥65 years with no 432 in development MMSE <24 (adjusted Incident delirium by 74 15% OR 3·6 (2·1–6·2)
delirium admitted to acute hospital sample; 323 in for education level) DSM-IIIR
medical and surgical wards validation sample
Inouye et al32 (1993) Patients aged ≥70 years with no 107 in development MMSE <24 on Incident delirium by 79 25% RR 2·8 (1·2–6·7)
dementia or delirium admitted to sample; 174 in admission CAM
acute hospital medical wards validation sample
CAM=Confusion Assessment Method. OR=odds ratio. MMSE=Mini-Mental State Examination. DOSS=Delirium Observation Screening Scale. DSM=Diagnostic and Statistical Manual of Mental Disorders.
SPMSQ=Short Portable Mental Status Questionnaire. RR=relative risk. IQCODE=Informant Questionnaire on Cognitive Decline in the Elderly. BDRS=Blessed Dementia Rating Scale. TICS=Telephone Interview for
Cognitive Status.
Table 2: Baseline cognitive impairment and dementia as an independent risk factor for delirium from predictive models
decline.58–62 In one study of 771 outpatients with the effects of this condition. For example, long-term
Alzheimer’s disease living in their own homes,60 after follow-up of a well characterised cohort who are free of
adjustment for confounders, delirium was associated dementia at baseline could help to clarify whether
with a greatly increased adjusted risk of death (relative incident delirium can lead to new-onset dementia. The
risk 5·4, 95% CI 2·3–12·5) or of institutionalisation patient’s individual experience with delirium, including
(9·3, 5·5–15·7). At 1 year, 21% of cases of cognitive distress and development of post-traumatic stress
decline, 15% of institutionalisations, and 6% of deaths disorder, have not been fully examined as outcome
were attributable to delirium. In another study of measures. Finally, genetic and other important
263 patients with Alzheimer’s disease,44 despite their determinants of delirium risk and risk stratification to
trajectories (ie, rates of decline in cognitive function) identify particularly high-risk individuals should be
being similar before an index admission to hospital, explored. Ultimately, these data will support early
delirium resulted in a fundamental alteration in the identification, prevention, and treatment of delirium.
trajectory of cognitive decline, with a doubled rate of
decline over the year following admission to hospital and Clinicopathological evidence
accelerated decline persisting over the entire 5-year The interaction between delirium and dementia has
follow-up period. This study was important because it been shown in a population-based study, Vantaa 85+,46
showed that, in patients with Alzheimer’s disease, examining the effect of delirium (determined
delirium resulted in a marked increase in the rate of retrospectively) on cognitive and functional outcomes. In
cognitive decline and that this change seemed to be this cohort of 553 individuals aged 85 years or older,
irreversible. delirium increased the risk of incident dementia (odds
Additional long-term follow-up studies looking at ratio 8·7, 95% CI 2·1–35·0). Moreover, consistent with
outcomes of delirium are still needed to fully understand findings of cognitive trajectories reported in the scientific
4 www.thelancet.com/neurology Published online June 30, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00101-5
Review
Sample Sample Delirium measure Cognitive outcome Mean age at Patients Adjusted effect size
size baseline with (95% CI)
(years) delirium
Cognitive function and Population-based sample; 2197 Algorithmic AGECAT-defined dementia 77 6% OR 8·8 (2·8–28·0)
ageing study42 (2014) multicentre sampling from operationalisation of at 2 years
health authority lists DSM-IV based on Geriatric
Mental State examination
BRAIN-ICU43 (2013) Multicentre ICU admissions 821 CAM-ICU RBANS score at 1 year 61 74% –5·6 (–9·5 to –1·8) points per
day of delirium
Gross et al44 (2012)* Memory clinic patients with 263 Retrospective diagnosis of Worsening of Blessed IMC 78 56% Additional 1·2 (0·5–1·8) points
clinically diagnosed delirium from case notes test score over 5 or more per year
Alzheimer’s dementia (validated algorithm) years
Saczynski et al45 (2012) Patients aged ≥60 years 225 CAM Trajectory of MMSE change 73 46% Prolonged impairment in
undergoing elective CABG or over 1 year recovery
valve surgery
Vantaa 85+46 (2012) Population-based sample of 553 Participant and informant Dementia (DSM-IIIR; 89 13% OR 8·7 (2·1–35·0)
all residents aged ≥85 years interview, along with individual clinician) at
medical record review 2·5 years
Fong et al47 (2009)* Memory clinic patients with 408 Retrospective diagnosis of Worsening of Blessed IMC 74 18% Additional 2·4 (1·0–3·8) points
clinically diagnosed delirium from case notes test score over 0·7 years
Alzheimer’s disease (validated algorithm)
Bickel et al48 (2008) Patients aged ≥60 years 200 CAM Cognitive impairment or 74 21% OR 41·0 (4·3–396·0)
undergoing elective hip dementia, or both
surgery
LundstrÖm et al49 (2003) Dementia-free patients aged 78 DSM-IV Consensus diagnosis of 79 38% OR 5·7 (1·3–24·0)
≥65 years with acute hip dementia at 5 years
fracture
DSM=Diagnostic and Statistical Manual of Mental Disorders. AGECAT=Automated Geriatric Examination for Computer Assisted Taxonomy. OR=odds ratio. BRAIN-ICU=Bringing to Light the Risk Factors and
Incidence of Neuropsychological Dysfunction in Intensive Care Unit Survivors. ICU=intensive care unit. CAM=Confusion Assessment Method. RBANS=Repeatable Battery for the Assessment of
Neuropsychological Status. IMC=Information-Memory-Concentration. CABG=coronary artery bypass grafting. MMSE=Mini-Mental State Examination. *Related analyses with some overlap of data.
Table 3: Delirium as an independent risk factor for long-term cognitive decline and dementia
literature, delirium was associated with increased Neuroimaging evidence
dementia severity, new functional deficits, and Despite the routine use of neuroimaging in clinical
accelerated decline in cognitive scores. This study also practice and an increasing number of studies using this
examined the neuropathological correlates of dementia technique to investigate the pathophysiology and effects of
in the presence or absence of a history of delirium. The delirium, there are few studies that provide long-term
relations between dementia and measures of follow-up or convincing evidence of permanent
neurofibrillary tau, amyloid burden, apolipoprotein E neurological changes attributable to delirium. Most studies
(APOE) ε4 variant, vascular lesions, and Lewy body so far have been limited by small sample sizes, inadequate
pathology were strongest in the absence of a delirium control groups, and absence of baseline scans before the
history. When these pathological markers were assessed onset of delirium.63,64 Two studies65,66 on the same sample of
in relation to cases of dementia in which delirium was 47 intensive-care unit survivors used volumetric analysis
also part of the history, no associations were detectable. and diffusion tensor imaging at hospital discharge and
Although the results were not powered to be conclusive, 3-month follow-up. In the volumetric analysis, longer
they show that when delirium is part of the trajectory of duration of delirium was significantly associated with
dementia development, the pathological substrates can greater brain atrophy at hospital discharge and at 3-month
be different from conventional pathological changes of follow-up. Additionally, duration of delirium was
dementia, such as Alzheimer’s, vascular, or Lewy body significantly associated with white matter disruption both
pathology. These findings raise the intriguing possibility at hospital discharge and at 3-month follow-up.
that the acceleration of cognitive decline following The absence of baseline scans in previous studies
delirium might result from an alternative mechanism precludes any strong conclusions about whether the
leading to neuronal damage. development of delirium itself contributed to subsequent
Studies that include markers of Alzheimer’s pathology, neuroimaging findings. Future studies, with larger
such as CSF biomarkers, or tau and amyloid β imaging, cohorts, baseline characterisation, careful selection of
and additional post-mortem studies will yield substantial controls, and advanced neuroanatomical and functional
insights into the fundamental pathophysiology of neuroimaging measures, should lead to a greater under-
delirium and might ultimately help with development of standing of the anatomical and functional links between
effective treatments. delirium and dementia.
www.thelancet.com/neurology Published online June 30, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00101-5 5
Review
Biomarker evidence By contrast, other studies that did not specifically
A range of serum and CSF biomarkers have been exclude people with dementia have shown a possible
considered in efforts to understand delirium association between postoperative delirium and
pathogenesis. Previous studies in intensive-care unit biomarkers of Alzheimer’s disease. In a study of
patients showed that high concentrations of baseline 153 older adults aged 64–80 years (mean 71 years [SD 5])
inflammatory markers were associated with subsequent undergoing elective total hip or knee replacement,19 CSF
development of delirium.65,67 In a pilot study of patients was obtained during initiation of spinal anaesthesia,
who were critically ill owing to infection, the pro- and patients were monitored postoperatively for the
inflammatory cytokine interleukin 8 was associated with development and severity of delirium. A significantly
delirium,68 whereas in non-infected patients, the anti- higher incidence of delirium was seen in participants
inflammatory cytokine interleukin 10 was associated with preoperative CSF Aβ1–40:tau and Aβ1–42:tau ratios in
with delirium. These findings suggest that the underlying the lowest quartile versus all other quartiles (32% vs
mechanisms governing the development of delirium in 17%, p=0·05 for both comparisons), suggesting a
patients with inflammation might differ from the possible threshold effect in the relation between
mechanisms in individuals without inflammation.69 preoperative biomarkers of Alzheimer’s disease and
Other studies have shown cytokines such as insulin-like postoperative delirium. After adjusting for age and sex,
growth factor (IGF)-1, interleukin 1β, and interleukin 1 lower preoperative CSF Aβ1–40:tau and Aβ1–42:tau ratios
receptor antagonist to be associated with delirium,70–72 were associated with significantly higher scores on a
and the combination of high concentrations of delirium severity scale (β=–0·12 ± 0·05 [p=0·018] and
interferon γ and low concentrations of IGF-1 was β=–0·62 ± 0·27 [p=0·022], respectively), suggesting that
associated with delirium severity.73 S100B, a marker of lower CSF Aβ:tau ratios, similar to ratios seen in
astrocyte damage, has been shown to be present at high Alzheimer’s disease, are associated with greater
concentrations in both the plasma and the CSF of delirium severity.9 Another study69 has shown that high
patients with delirium.69,74,75 Further study is needed to serum Aβ1–42 and Aβ1–40 concentrations are associated
determine whether these changes in biomarkers are a with delirium occurrence and subjective complaints of
direct result of delirium, whether they are caused by cognitive impairment 18 months after the delirium
indirect associations with delirium, or whether they are episode. Taken together, these findings suggest a role
due to dementia via progressive neurodegeneration, or a for Aβ and tau in the neuropathogenesis of postoperative
combination of these factors. delirium and that delirium could represent the first sign
Several studies have looked for a direct association of a (subclinical) dementia process in some cases.
between delirium and biomarkers of Alzheimer’s Although these studies are generally small and need
disease. In a cohort of 76 individuals admitted to hospital cautious interpretation, the accumulating evidence lends
for emergency hip fractures, concentrations of Aβ1–42, tau, support to the hypothesis that delirium itself contributes
and phosphorylated tau in CSF were not associated with to or mediates permanent cognitive impairment. Future
delirium status, nor did they correlate significantly with studies in patients with careful baseline assessment of
IQCODE score, despite a strong association of cognitive function, control for confounding factors such
postoperative delirium with premorbid cognitive decline as age and pre-existing dementia, and long-term follow-
(as measured with the IQCODE).76 In view of the limited up with characterisation by neuropsychological testing
sample size, however, the results should be interpreted and neuroimaging are needed to better address this
with caution. important area.
In a more recent study of 557 non-demented patients
aged 70 years or older undergoing major non-cardiac Animal models and neuronal tissue culture
surgery, after adjusting for age, sex, surgical procedure, Studies involving animal models relevant for delirium
and preoperative cognitive function, APOE ε4 and have shown that systemic inflammatory insults can cause
APOE ε2 carrier status were not associated with punctuated cognitive decline typical of delirium, followed
postoperative delirium. Furthermore, no associations by persistent acceleration in disease progression typical of
between APOE genotype and delirium severity or the dementia.78 In many studies, researchers have tried to use
number of delirium episodes were reported. Thus, in a a clinically relevant experimental approach to delirium by
sample with careful exclusion of people with underlying including both predisposing and precipitating factors. In
dementia, APOE genotype does not seem to confer these models, underlying pathology or brain vulnerability
either risk or protection for postoperative delirium has been induced either by neurodegeneration associated
incidence, severity, or duration.77 The results of both with prion infection,79 or through selective and partial
studies are consistent with the Vantaa 85+ lesioning of the cholinergic projections of the basal
epidemiological study of cerebral pathology,46 suggesting forebrain.80 Subsequent to this induction, the animals
that postoperative delirium might arise through have been exposed to an inflammatory challenge to
pathophysiological pathways that are distinct from simulate bacterial infection (eg, using lipopolysaccharide
those in Alzheimer’s disease. [LPS]) or viral infection (eg, using polyinosinic:polycytidylic
6 www.thelancet.com/neurology Published online June 30, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00101-5
Review
acid [poly(I:C)]).81,82 In these models, acute peripheral inflammation have suggested that the effect of delirium
inflammation induced by LPS or poly(I:C) leads to acute itself might be a contributor to or a mediator of permanent
deficits in cognition and motor function, analogous to cognitive impairment, or both. Taken together, these
delirium, and similar deficits are noted with inflammation experimental studies lend strong support to the
superimposed on either of these underlying neuro- pathophysiological links between delirium mechanisms
degenerative models. Thus, such animal models provide and long-term cognitive impairment or dementia, and
an opportunity to probe specific pathophysiological further studies are necessary to substantiate and extend
pathways in delirium and dementia.83 Other studies84–86 these findings.
using a single dose of LPS to induce an inflammatory
insult that is comparable to sepsis in human beings, a Conclusions and future directions
frequent contributing factor to delirium, have reported Ultimately, delirium is likely to interface with dementia
that inflammation via inducible nitric oxide synthase on many levels: it is a marker of vulnerability of the brain,
contributes to neuronal death, microglial activation, it unmasks unrecognised dementia, mediates the effects
decreased regional blood flow, and loss of cholinergic of noxious insults, and itself leads to permanent neuronal
activation, with persistent cognitive deficits in attention, damage and dementia. There is little doubt that occurrence
executive function, and working memory. of an episode of delirium can signal underlying
Microglial priming has been shown in chronic vulnerability of the brain, with decreased cognitive reserve
neurodegeneration79 and ageing,87 whereby microglia and increased risk for development of dementia in the
cause a more aggressive inflammatory response to future.92 Delirium reflects a decompensated cognitive
peripheral inflammation than in either younger or non- state under stress conditions, and its presence implies
diseased animals. The acute insult triggered acute, diminished cognitive reserve. In some cases, delirium
transient,82 and fluctuating88 cognitive deficits during could bring previously unrecognised cognitive impairment
T-maze testing, and further neurodegeneration79 and to medical attention. Moreover, severe precipitating
acceleration of disease trajectory were reported.78 Other factors for delirium, such as prolonged hypoglycaemia or
studies using this model have shown that microglia hypoxaemia, can lead to neuronal death and permanent
express cyclooxygenase (COX) 1 and synthesise cognitive impairment.93 Delirium might also mediate the
prostaglandins. Selective inhibition of COX1 is effect of many factors, such as general surgery,
protective against systemic LPS-induced cognitive anaesthesia, critical illness, acute respiratory distress
defects, and non-selective inhibition of microglia with syndrome, prolonged intubation, or sepsis, on long-term
ibuprofen protects against cognitive defects induced by cognitive outcomes.
interleukin 1β.89 In cholinergic-deficient mice, Study of the relation between delirium and dementia
inflammation was sufficient, but microglial priming poses myriad challenges, highlighting the barriers to
was not essential, to cause similar cognitive deficits.81 investigation of this important area. In view of the lengthy
Furthermore, the cognitive deficits could be blocked by prodromal stage of dementia along with its unpredictable
the acetylcholinesterase inhibitor donepezil.81 This progression, knowledge of the baseline state and trajectory
finding suggests an important interplay between of any cognitive changes is essential. The target population
acetylcholine deficiency and systematic inflammation, is often frail, with many medical comorbidities, and
but the finding that worsening neurodegeneration delirium might remain undetected; thus, active
makes animals progressively more susceptible to the surveillance is essential. Refinement of distinct diagnostic
cognitively disrupting effects of LPS88 implicates several criteria and demarcation of the overlap syndrome will be
neuronal networks. crucial to differentiate between the two conditions.
Previous studies in human neuronal cell culture have Identification of the contribution of the presence of
shown that exposure to some inhalational anaesthetics delirium is a paramount first step; however, evidence for a
(eg, isoflurane, sevoflurane) can induce neurotoxicity, dose–response relation of dementia with delirium severity
including apoptosis, caspase activation, Aβ oligomerisation and duration will help to strengthen causal inference.
and accumulation, neuroinflammation, and mitochondrial Appropriate control for confounding factors, without
dysfunction,6,90 whereas this effect is not seen with use of overcontrolling, will be necessary to assess the
other agents (eg, desflurane, nitrous oxide, propofol).91 contribution to dementia of delirium itself and the effects
Studies using animal models and neuronal tissue of other precipitating insults mediated by delirium.
culture have already begun to explore pathophysiological Moreover, the presence of delirium poses many logistical
pathways that might enable identification of future targets challenges, including informed consent, ethical dilemmas,
for intervention. Other areas will need to be explored, and challenges to conducting procedures and
including neurotransmitter dysregulation, oxidative neuroimaging in the study of older adults with agitation,
stress, and aberrant stress response. Progress in these behavioural disturbances, severe illness, multimorbidity,
mechanistic studies will be crucial and will ultimately be and frailty.
the primary means to advance understanding of the Acknowledgment of delirium as a determinant of
pathophysiology of delirium. Initial studies focusing on chronic cognitive impairment compels a broadening of
www.thelancet.com/neurology Published online June 30, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00101-5 7
Review
our understanding of dementia. Recognition that slowly 8 McCusker J, Cole M, Dendukuri N, Han L, Belzile E. The course of
evolving neurodegenerative processes might be delirium in older medical inpatients: a prospective study.
J Gen Intern Med 2003; 18: 696–704.
accelerated by delirium necessitates consideration of 9 Rockwood K. The occurrence and duration of symptoms in elderly
the long-term effects of acute illness and other patients with delirium. J Gerontol 1993; 48: M162–66.
precipitating factors on the vulnerable brain. Thus, 10 Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults:
diagnosis, prevention and treatment. Nat Rev Neurol 2009; 5: 210–20.
delirium might serve as an important model system for
11 Downing LJ, Caprio TV, Lyness JM. Geriatric psychiatry review:
research, offering a unique approach to advance our differential diagnosis and treatment of the 3 D’s—delirium,
understanding of cognitive disorders and dementia dementia, and depression. Curr Psychiatry Rep 2013; 15: 365.
more generally. The frequency and acuity of delirium 12 Gower LE, Gatewood MO, Kang CS. Emergency department
management of delirium in the elderly. West J Emerg Med 2012;
and its associated serious adverse outcomes make it a 13: 194–201.
highly promising area for investigation. The presence of 13 Inouye S, Marcantonio E. Delirium. In: Growdon J, Rossor M, eds.
delirium could help to identify people who are The Dementias. Philadelphia, PA: Butterworth-Heinemann Elsevier,
2007: 285–312.
vulnerable to cognitive decline through genetic
14 Maclullich AM, Anand A, Davis DH, et al. New horizons in the
predisposition, diminished cognitive reserve, or the pathogenesis, assessment and management of delirium.
presence of unrecognised dementia. Investigation of Age Ageing 2013; 42: 667–74.
delirium also provides an opportunity to study the link 15 Marcantonio ER. Postoperative delirium: a 76-year-old woman with
delirium following surgery. JAMA 2012; 308: 73–81.
between brain pathophysiology and behavioural 16 Xie Z, Dong Y, Maeda U, et al. Isoflurane-induced apoptosis:
manifestations, which might hold broader implications a potential pathogenic link between delirium and dementia.
for other neurological and psychiatric disorders. J Gerontol A Biol Sci Med Sci 2006; 61: 1300–06.
17 Hshieh TT, Fong TG, Marcantonio ER, Inouye SK. Cholinergic
Moreover, progress in understanding of the patho- deficiency hypothesis in delirium: a synthesis of current evidence.
genesis of delirium will be crucial to identify modifiable J Gerontol A Biol Sci Med Sci 2008; 63: 764–72.
or preventable factors that lead directly to neuronal 18 Ramirez-Bermudez J, Ruiz-Chow A, Perez-Neri I, et al.
Cerebrospinal fluid homovanillic acid is correlated to psychotic
injury and thus permanent cognitive sequelae. features in neurological patients with delirium.
Implementation of therapies for prevention of delirium Gen Hosp Psychiatry 2008; 30: 337–43.
holds particular relevance in terms of their potential to 19 Xie Z, Swain CA, Ward SA, et al. Preoperative cerebrospinal fluid
delay or alter both the typical cognitive ageing process beta-amyloid/tau ratio and postoperative delirium.
Ann Clin Transl Neurol 2014; 1: 319–28.
and the progression of cognitive decline in people with 20 Maclullich AM, Ferguson KJ, Miller T, de Rooij SE,
dementia. Cunningham C. Unravelling the pathophysiology of delirium: a
focus on the role of aberrant stress responses. J Psychosom Res
Contributors 2008; 65: 229–38.
All authors contributed to the search strategy, selection of articles,
21 Simone MJ, Tan ZS. The role of inflammation in the pathogenesis
synthesis of information identified in the search, and drafting and editing of delirium and dementia in older adults: a review.
of this Review. All authors have seen and approved the final version. SKI CNS Neurosci Ther 2011; 17: 506–13.
had full access to all the material reported in this Review and had final 22 Kennedy M, Enander RA, Tadiri SP, Wolfe RE, Shapiro NI,
responsibility for the decision to submit for publication. Marcantonio ER. Delirium risk prediction, healthcare use and
Declaration of interests mortality of elderly adults in the emergency department.
J Am Geriatr Soc 2014; 62: 462–69.
We declare no competing interests.
23 Koster S, Hensens AG, Schuurmans MJ, van der Palen J. Prediction
Acknowledgments of delirium after cardiac surgery and the use of a risk checklist.
We acknowledge Eva Schmitt and Dulce Pina for assistance with Eur J Cardiovasc Nurs 2013; 12: 284–92.
coordinating the writing of this paper. This Review is dedicated to the 24 Moerman S, Tuinebreijer WE, de Boo M, Pilot P, Nelissen RG,
memory of Joshua Bryan Inouye Helfand. This Review was supported in Vochteloo AJ. Validation of the risk model for delirium in hip
part by grants P01AG031720 (SKI), R01AG044518 (SKI), and fracture patients. Gen Hosp Psychiatry 2012; 34: 153–59.
K07AG041835 (SKI) from the US National Institute on Aging and by the 25 Bo M, Martini B, Ruatta C, et al. Geriatric ward hospitalization
Milton and Shirley F Levy Family Chair. reduced incidence delirium among older medical inpatients.
Am J Geriatr Psychiatry 2009; 17: 760–68.
References
26 Rudolph JL, Jones RN, Levkoff SE, et al. Derivation and validation
1 American Psychiatric Association. Diagnostic and statistical manual
of a preoperative prediction rule for delirium after cardiac surgery.
of mental disorders, 5th edn (DSM-5). Arlington, VA: American
Circulation 2009; 119: 229–36.
Psychiatric Association, 2013.
27 Kalisvaart KJ, Vreeswijk R, de Jonghe JF, van der Ploeg T,
2 Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly
van Gool WA, Eikelenboom P. Risk factors and prediction of
people. Lancet 2014; 383: 911–22.
postoperative delirium in elderly hip-surgery patients:
3 Inouye SK. Delirium in older persons. N Engl J Med 2006; implementation and validation of a medical risk factor model.
354: 1157–65. J Am Geriatr Soc 2006; 54: 817–22.
4 Cole M, McCusker J, Dendukuri N, Han L. The prognostic 28 Wilson K, Broadhurst C, Diver M, Jackson M, Mottram P. Plasma
significance of subsyndromal delirium in elderly medical insulin growth factor-1 and incident delirium in older people.
inpatients. J Am Geriatr Soc 2003; 51: 754–60. Int J Geriatr Psychiatry 2005; 20: 154–59.
5 Levkoff SE, Evans DA, Liptzin B, et al. Delirium. The occurrence 29 O’Keeffe ST, Lavan JN. Predicting delirium in elderly patients:
and persistence of symptoms among elderly hospitalized patients. development and validation of a risk-stratification model.
Arch Intern Med 1992; 152: 334–40. Age Ageing 1996; 25: 317–21.
6 Levkoff SE, Liptzin B, Evans DA, et al. Progression and resolution 30 Marcantonio ER, Goldman L, Mangione CM, et al. A clinical
of delirium in elderly patients hospitalized for acute care. prediction rule for delirium after elective noncardiac surgery.
Am J Geriatr Psychiatry 1994; 2: 230–38. JAMA 1994; 271: 134–39.
7 Marcantonio ER, Flacker JM, Michaels M, Resnick NM. Delirium is 31 Pompei P, Foreman M, Rudberg MA, Inouye SK, Braund V,
independently associated with poor functional recovery after hip Cassel CK. Delirium in hospitalized older persons: outcomes and
fracture. J Am Geriatr Soc 2000; 48: 618–24. predictors. J Am Geriatr Soc 1994; 42: 809–15.
8 www.thelancet.com/neurology Published online June 30, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00101-5
Review
32 Inouye SK, Viscoli CM, Horwitz RI, Hurst LD, Tinetti ME. 56 Newman S, Stygall J, Hirani S, Shaefi S, Maze M. Postoperative
A predictive model for delirium in hospitalized elderly medical cognitive dysfunction after noncardiac surgery: a systematic review.
patients based on admission characteristics. Ann Intern Med 1993; Anesthesiology 2007; 106: 572–90.
119: 474–81. 57 Watt D, Koziol K, Budding D. Delirium and confusional states.
33 Pfeiffer E. A short portable mental status questionnaire for the In: Noggle C, Dean R, eds. Disorders in neuropsychiatry. New York:
assessment of organic brain deficit in elderly patients. Springer Publishing Company, 2012.
J Am Geriatr Soc 1975; 23: 433–41. 58 Baker FM, Wiley C, Kokmen E, Chandra V, Schoenberg BS.
34 Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. Delirium episodes during the course of clinically diagnosed
A practical method for grading the cognitive state of patients for the Alzheimer’s disease. J Natl Med Assoc 1999; 91: 625–30.
clinician. J Psychiatr Res 1975; 12: 189–98. 59 Fick D, Foreman M. Consequences of not recognizing delirium
35 Jorm AF. A short form of the informant questionnaire on cognitive superimposed on dementia in hospitalized elderly individuals.
decline in the elderly (IQCODE): development and cross-validation. J Gerontol Nurs 2000; 26: 30–40.
Psychol Med 1994; 24: 145–53. 60 Fong TG, Jones RN, Marcantonio ER, et al. Adverse outcomes after
36 Blessed G, Tomlinson BE, Roth M. The association between hospitalization and delirium in persons with Alzheimer disease.
quantitative measures of dementia and of senile change in the Ann Intern Med 2012; 156: 848–56, W296.
cerebral grey matter of elderly subjects. Br J Psychiatry 1968; 61 McCusker J, Cole M, Dendukuri N, Belzile E, Primeau F. Delirium
114: 797–811. in older medical inpatients and subsequent cognitive and functional
37 Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. status: a prospective study. CMAJ 2001; 165: 575–83.
Clarifying confusion: the confusion assessment method. A new 62 Rockwood K, Cosway S, Carver D, Jarrett P, Stadnyk K, Fisk J.
method for detection of delirium. Ann Intern Med 1990; 113: 941–48. The risk of dementia and death after delirium. Age Ageing 1999;
38 American Psychiatric Association. Diagnostic and statistical manual 28: 551–56.
of mental disorders, 3rd edn (DSM-III). Washington, DC: American 63 Alsop DC, Fearing MA, Johnson K, Sperling R, Fong TG,
Psychiatric Association, 1980. Inouye SK. The role of neuroimaging in elucidating delirium
39 American Psychiatric Association. Diagnostic and statistical manual pathophysiology. J Gerontol A Biol Sci Med Sci 2006; 61: 1287–93.
of mental disorders, 3rd edn, revised (DSM-IIIR). Washington, DC: 64 Soiza RL, Sharma V, Ferguson K, Shenkin SD, Seymour DG,
American Psychiatric Association, 1987. Maclullich AM. Neuroimaging studies of delirium: a systematic
40 American Psychiatric Association. Diagnostic and statistical manual review. J Psychosom Res 2008; 65: 239–48.
of mental disorders, 4th edn (DSM-IV). Washington, DC: American 65 Gunther ML, Morandi A, Krauskopf E, et al. The association
Psychiatric Association, 2000. between brain volumes, delirium duration, and cognitive outcomes
41 Schuurmans MJ, Shortridge-Baggett LM, Duursma SA. The in intensive care unit survivors: the VISIONS cohort magnetic
delirium observation screening scale: a screening instrument for resonance imaging study*. Crit Care Med 2012; 40: 2022–32.
delirium. Res Theory Nurs Pract 2003; 17: 31–50. 66 Morandi A, Rogers BP, Gunther ML, et al. The relationship between
42 Davis DH, Barnes LE, Stephan BC, et al. The descriptive delirium duration, white matter integrity, and cognitive impairment
epidemiology of delirium symptoms in a large population-based in intensive care unit survivors as determined by diffusion tensor
cohort study: results from the Medical Research Council cognitive imaging: The VISIONS prospective cohort magnetic resonance
function and ageing study (MRC CFAS). BMC Geriatr 2014; 14: 87. imaging study. Crit Care Med 2012; 40: 2182–89.
43 Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive 67 McGrane S, Girard TD, Thompson JL, et al. Procalcitonin and
impairment after critical illness. N Engl J Med 2013; 369: 1306–16. C-reactive protein levels at admission as predictors of duration of
44 Gross AL, Jones RN, Habtemariam DA, et al. Delirium and acute brain dysfunction in critically ill patients. Crit Care 2011;
long-term cognitive trajectory among persons with dementia. 15: R78.
Arch Intern Med 2012; 172: 1324–31. 68 MacLullich AM, Edelshain BT, Hall RJ, et al. Cerebrospinal fluid
45 Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories interleukin-8 levels are higher in people with hip fracture with
after postoperative delirium. N Engl J Med 2012; 367: 30–39. perioperative delirium than in controls. J Am Geriatr Soc 2011;
46 Davis DH, Muniz Terrera G, Keage H, et al. Delirium is a strong 59: 1151–53.
risk factor for dementia in the oldest-old: a population-based cohort 69 van den Boogaard M, Kox M, Quinn KL, et al. Biomarkers
study. Brain 2012; 135: 2809–16. associated with delirium in critically ill patients and their relation
47 Fong TG, Jones RN, Shi P, et al. Delirium accelerates cognitive with long-term subjective cognitive dysfunction; indications for
decline in Alzheimer disease. Neurology 2009; 72: 1570–75. different pathways governing delirium in inflamed and
noninflamed patients. Crit Care 2011; 15: R297.
48 Bickel H, Gradinger R, Kochs E, Forstl H. High risk of cognitive
and functional decline after postoperative delirium. A three-year 70 Cape E, Hall RJ, van Munster BC, et al. Cerebrospinal fluid markers
prospective study. Dement Geriatr Cogn Disord 2008; 26: 26–31. of neuroinflammation in delirium: a role for interleukin-1beta in
delirium after hip fracture. J Psychosom Res 2014; 77: 219–25.
49 Lundström M, Edlund A, Bucht G, Karlsson S, Gustafson Y.
Dementia after delirium in patients with femoral neck fractures. 71 Pearson A, de Vries A, Middleton SD, et al. Cerebrospinal fluid
J Am Geriatr Soc 2003; 51: 1002–06. cortisol levels are higher in patients with delirium versus controls.
BMC Res Notes 2010; 3:33.
50 Copeland JR, Dewey ME, Griffiths-Jones HM. A computerized
psychiatric diagnostic system and case nomenclature for elderly 72 Westhoff D, Witlox J, Koenderman L, et al. Preoperative cerebrospinal
subjects: GMS and AGECAT. Psychol Med 1986; 16: 89–99. fluid cytokine levels and the risk of postoperative delirium in elderly
hip fracture patients. J Neuroinflammation 2013; 10: 122.
51 Randolph C, Tierney MC, Mohr E, Chase TN. The repeatable battery
for the assessment of neuropsychological status (RBANS): 73 Adamis D, Lunn M, Martin FC, et al. Cytokines and IGF-I in
preliminary clinical validity. J Clin Exp Neuropsychol 1998; 20: 310–19. delirious and non-delirious acutely ill older medical inpatients.
Age Ageing 2009; 38: 326–32.
52 Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P,
van Gool WA. Delirium in elderly patients and the risk of 74 Hall RJ, Ferguson KJ, Andrews M, et al. Delirium and cerebrospinal
postdischarge mortality, institutionalization, and dementia: fluid S100B in hip fracture patients: a preliminary study.
a meta-analysis. JAMA 2010; 304: 443–51. Am J Geriatr Psychiatry 2013; 21: 1239–43.
53 Pitkala KH, Laurila JV, Strandberg TE, Tilvis RS. Multicomponent 75 van Munster BC, Korevaar JC, Korse CM, Bonfrer JM,
geriatric intervention for elderly inpatients with delirium: Zwinderman AH, de Rooij SE. Serum S100B in elderly patients
a randomized, controlled trial. J Gerontol A Biol Sci Med Sci 2006; with and without delirium. Int J Geriatr Psychiatry 2010; 25: 234–39.
61: 176–81. 76 Witlox J, Kalisvaart KJ, de Jonghe JF, et al. Cerebrospinal fluid
54 Selnes OA, Gottesman RF, Grega MA, Baumgartner WA, Zeger SL, beta-amyloid and tau are not associated with risk of delirium:
McKhann GM. Cognitive and neurologic outcomes after coronary- a prospective cohort study in older adults with hip fracture.
artery bypass surgery. N Engl J Med 2012; 366: 250–57. J Am Geriatr Soc 2011; 59: 1260–67.
55 Avidan MS, Evers AS. Review of clinical evidence for persistent 77 Vasunilashorn SNL, Kosar CM, Fong TG, Jones RN, Inouye SK,
cognitive decline or incident dementia attributable to surgery or Marcantonio ER. Does apolipoprotein E genotype increase risk of
general anesthesia. J Alzheimers Dis 2011; 24: 201–16. postoperative delirium? Am J Geriatr Psychiatry (in press).
www.thelancet.com/neurology Published online June 30, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00101-5 9
Review
78 Cunningham C, Campion S, Lunnon K, et al. Systemic inflammation 86 Weberpals M, Hermes M, Hermann S, et al. NOS2 gene deficiency
induces acute behavioral and cognitive changes and accelerates protects from sepsis-induced long-term cognitive deficits. J Neurosci
neurodegenerative disease. Biol Psychiatry 2009; 65: 304–12. 2009; 29: 14177–84.
79 Cunningham C, Wilcockson DC, Campion S, Lunnon K, Perry VH. 87 Godbout JP, Chen J, Abraham J, et al. Exaggerated
Central and systemic endotoxin challenges exacerbate the local neuroinflammation and sickness behavior in aged mice following
inflammatory response and increase neuronal death during chronic activation of the peripheral innate immune system. FASEB J 2005;
neurodegeneration. J Neurosci 2005; 25: 9275–84. 19: 1329–31.
80 Field RH, Gossen A, Cunningham C. Prior pathology in the basal 88 Davis DH, Skelly DT, Murray C, et al. Worsening cognitive
forebrain cholinergic system predisposes to inflammation-induced impairment and neurodegenerative pathology progressively
working memory deficits: reconciling inflammatory and cholinergic increase risk for delirium. Am J Geriatr Psychiatry 2014; 23: 403–15.
hypotheses of delirium. J Neurosci 2012; 32: 6288–94. 89 Griffin EW, Skelly DT, Murray CL, Cunningham C.
81 Field R, Campion S, Warren C, Murray C, Cunningham C. Cyclooxygenase-1-dependent prostaglandins mediate susceptibility
Systemic challenge with the TLR3 agonist poly I:C induces to systemic inflammation-induced acute cognitive dysfunction.
amplified IFNalpha/beta and IL-1beta responses in the diseased J Neurosci 2013; 33: 15248–58.
brain and exacerbates chronic neurodegeneration. 90 Zhang Y, Xu Z, Wang H, et al. Anesthetics isoflurane and
Brain Behav Immun 2010; 24: 996–1007. desflurane differently affect mitochondrial function, learning, and
82 Murray C, Sanderson DJ, Barkus C, et al. Systemic inflammation memory. Ann Neurol 2012; 71: 687–98.
induces acute working memory deficits in the primed brain: 91 Xie Z, Xu Z. General anesthetics and beta-amyloid protein.
relevance for delirium. Neurobiol Aging 2012; 33: 603–16.e3. Prog Neuropsychopharmacol Biol Psychiatry 2013; 47: 140–46.
83 Cunningham C, Maclullich AM. At the extreme end of the 92 Jones RN, Manly J, Glymour MM, Rentz DM, Jefferson AL, Stern Y.
psychoneuroimmunological spectrum: delirium as a maladaptive Conceptual and measurement challenges in research on cognitive
sickness behaviour response. Brain Behav Immun 2013; 28: 1–13. reserve. J Int Neuropsychol Soc 2011; 17: 593–601.
84 Cunningham C. Systemic inflammation and delirium: important 93 Inouye SK. Delirium and cognitive decline: does delirium lead to
co-factors in the progression of dementia. Biochem Soc Trans 2011; dementia? In: Fillit HM, Butler RN, eds. Cognitive decline:
39: 945–53. strategies for prevention: proceedings of a White House Conference
85 Semmler A, Okulla T, Sastre M, Dumitrescu-Ozimek L, on Aging. London: Greenwich Medical Media, 1997: 85–107.
Heneka MT. Systemic inflammation induces apoptosis with
variable vulnerability of different brain regions.
J Chem Neuroanat 2005; 30: 144–57.
10 www.thelancet.com/neurology Published online June 30, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00101-5
Das könnte Ihnen auch gefallen
- Delirium: A Guide For The General Physician: Authors: Oliver M ToddDokument6 SeitenDelirium: A Guide For The General Physician: Authors: Oliver M ToddAnonymous tgLZ9uvXsNoch keine Bewertungen
- Dissociative Identity Disorder Out of The Shadows at LastDokument2 SeitenDissociative Identity Disorder Out of The Shadows at LastSusana Pérez ReyesNoch keine Bewertungen
- Latecia 2023 ResumeDokument6 SeitenLatecia 2023 Resumeapi-643213493Noch keine Bewertungen
- The Usui System of ReikiDokument35 SeitenThe Usui System of Reikimmorrison_2000Noch keine Bewertungen
- BLS Test PDFDokument76 SeitenBLS Test PDFalex rodman50% (2)
- What Is Head and Neck CancerDokument42 SeitenWhat Is Head and Neck CancerrositaNoch keine Bewertungen
- Dengue Hemorrhagic FeverDokument86 SeitenDengue Hemorrhagic FeverBryan EspanolNoch keine Bewertungen
- Dementia A Neurodegenerative DisorderDokument16 SeitenDementia A Neurodegenerative DisorderRishabh SinghNoch keine Bewertungen
- Borderline Personality DisorderDokument8 SeitenBorderline Personality DisorderVarsha Ganapathi100% (1)
- Genes Associated With Alzheimer's Disease: An Overview and Current StatusDokument17 SeitenGenes Associated With Alzheimer's Disease: An Overview and Current StatusHaseeba KhanNoch keine Bewertungen
- Ofra Ayalon Healing Trauma With Metaphoric Cards PDFDokument3 SeitenOfra Ayalon Healing Trauma With Metaphoric Cards PDFKrisztina MkNoch keine Bewertungen
- Induction of Labour: Maternity and Neonatal Clinical GuidelineDokument30 SeitenInduction of Labour: Maternity and Neonatal Clinical GuidelineFino GunnersNoch keine Bewertungen
- The Interface Between Delirium and Dementia in Elderly AdultsDokument10 SeitenThe Interface Between Delirium and Dementia in Elderly AdultsRestuti HandayaniNoch keine Bewertungen
- Tuokko DCL To DemenciaDokument23 SeitenTuokko DCL To DemenciaRAYMUNDO ARELLANONoch keine Bewertungen
- Attention-Deficit/hyperactivity Disorder As A Risk Factor For Dementia and Mild Cognitive Impairment: A Population-Based Register StudyDokument8 SeitenAttention-Deficit/hyperactivity Disorder As A Risk Factor For Dementia and Mild Cognitive Impairment: A Population-Based Register Studymonica izvanariuNoch keine Bewertungen
- Neurocognition in Individuals at High Familial Risk of Mood Disorders With or Without Subsequent Onset of DepressionDokument11 SeitenNeurocognition in Individuals at High Familial Risk of Mood Disorders With or Without Subsequent Onset of DepressionNerea Montero GarcíaNoch keine Bewertungen
- The Inter Relationship Between Delirium and Dementia. The Importance of Delirium PreventionDokument18 SeitenThe Inter Relationship Between Delirium and Dementia. The Importance of Delirium PreventionJorge LusagaNoch keine Bewertungen
- NIH Public Access: Delirium in Elderly PeopleDokument32 SeitenNIH Public Access: Delirium in Elderly PeopleMonika Diaz KristyanindaNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument22 SeitenNIH Public Access: Author ManuscriptMohanBabuNoch keine Bewertungen
- Rosso Intervención 2020Dokument9 SeitenRosso Intervención 2020Par DoNoch keine Bewertungen
- 2021 Naasan Psychosis BrainDokument14 Seiten2021 Naasan Psychosis BrainPriscila SelingardiNoch keine Bewertungen
- Artigo AlzheimerDokument21 SeitenArtigo Alzheimerbeatriz assunesNoch keine Bewertungen
- Hallucinations in Dementia Psychosis in Neurodegenerative Disease Differential Patterns of Hallucination and Delusion SymptomsDokument14 SeitenHallucinations in Dementia Psychosis in Neurodegenerative Disease Differential Patterns of Hallucination and Delusion SymptomsSultan TarlacıNoch keine Bewertungen
- 10.1038@s41380 019 0634 7Dokument16 Seiten10.1038@s41380 019 0634 7Steven MenaNoch keine Bewertungen
- Geriatric Depression and Its Relation With Cognitive Impairment and DementiaDokument7 SeitenGeriatric Depression and Its Relation With Cognitive Impairment and DementiajcurazanNoch keine Bewertungen
- Beelen 2009Dokument7 SeitenBeelen 2009isabela echeverriNoch keine Bewertungen
- 1 s2.0 S0191886922004573 MainDokument12 Seiten1 s2.0 S0191886922004573 Mainreza.scienceloverNoch keine Bewertungen
- Bipolar Lancet 2015Dokument12 SeitenBipolar Lancet 2015Javier Alonso Jara CánovasNoch keine Bewertungen
- Jamainternal Reuben 2024 RV 230006 1708983217.17671Dokument10 SeitenJamainternal Reuben 2024 RV 230006 1708983217.17671Juan Carlos Perez ParadaNoch keine Bewertungen
- Depression, Cognitive Impairment and Dementia Why.7Dokument6 SeitenDepression, Cognitive Impairment and Dementia Why.725paramveerNoch keine Bewertungen
- Revision D Lewys LancetDokument13 SeitenRevision D Lewys LancetJohana Zamudio RojasNoch keine Bewertungen
- DFT2019Dokument25 SeitenDFT2019Consulta externa Clinica montserratNoch keine Bewertungen
- DialoguesClinNeurosci 11 7 PDFDokument14 SeitenDialoguesClinNeurosci 11 7 PDFTry Wahyudi Jeremi LoLyNoch keine Bewertungen
- Dementia Preventia, Intervention and Care - LANCETDokument34 SeitenDementia Preventia, Intervention and Care - LANCETFernando lazzarettiNoch keine Bewertungen
- Revisiting The Etiological Aspects of Dissociative Identity Disorder: A Biopsychosocial PerspectiveDokument10 SeitenRevisiting The Etiological Aspects of Dissociative Identity Disorder: A Biopsychosocial Perspectivetitinmaulina06Noch keine Bewertungen
- Review 2021Dokument21 SeitenReview 2021Par DoNoch keine Bewertungen
- Primer: Autism Spectrum DisorderDokument23 SeitenPrimer: Autism Spectrum DisorderMakanudo.Noch keine Bewertungen
- Frontiers Autism Spectrum Disorders: Clinical and Research: Arch. Dis. ChildDokument7 SeitenFrontiers Autism Spectrum Disorders: Clinical and Research: Arch. Dis. ChildBernardita LoredoNoch keine Bewertungen
- Diabetes and Brain Health 2: Type 2 Diabetes and Cognitive Dysfunction-Towards Effective Management of Both ComorbiditiesDokument11 SeitenDiabetes and Brain Health 2: Type 2 Diabetes and Cognitive Dysfunction-Towards Effective Management of Both ComorbiditiesAndreaPacsiNoch keine Bewertungen
- Major Depressive Disorder and Difference Between Genders: Dzevad Sabic, Adela Sabic, Amila Bacic-BecirovicDokument4 SeitenMajor Depressive Disorder and Difference Between Genders: Dzevad Sabic, Adela Sabic, Amila Bacic-BecirovicDzevad SabicNoch keine Bewertungen
- Lancet 2020Dokument34 SeitenLancet 2020Javier ValeroNoch keine Bewertungen
- DEMENCIADokument7 SeitenDEMENCIANATALIA CRISTINA ARANGO SOLORZANONoch keine Bewertungen
- Obsessive Compulsive Personality Traits: Understanding The Chain of Pathogenesis From Health To DiseaseDokument11 SeitenObsessive Compulsive Personality Traits: Understanding The Chain of Pathogenesis From Health To DiseaseJuan Alberto GonzálezNoch keine Bewertungen
- Tab VS DFTDokument15 SeitenTab VS DFTAntu NandaNoch keine Bewertungen
- Ni Hms 613426Dokument13 SeitenNi Hms 613426ArdianNoch keine Bewertungen
- Dementia - Prevention - Intervention - and - Care - 2020 - Lancet - Commision 2Dokument34 SeitenDementia - Prevention - Intervention - and - Care - 2020 - Lancet - Commision 2Jorge Sánchez DomínguezNoch keine Bewertungen
- Jamapsychiatry Straub 2022 Oi 210078 1646173266.58264Dokument11 SeitenJamapsychiatry Straub 2022 Oi 210078 1646173266.58264Liércio Pinheiro de AraujoNoch keine Bewertungen
- Allott Et Al-2016-Brain and BehaviorDokument13 SeitenAllott Et Al-2016-Brain and BehaviorbssNoch keine Bewertungen
- Profile of and Risk Factors For Poststroke CognitiveDokument16 SeitenProfile of and Risk Factors For Poststroke CognitiveFera EyFeraNoch keine Bewertungen
- Alternatives To Psychiatric DiagnosisDokument3 SeitenAlternatives To Psychiatric Diagnosisfabiola.ilardo.15Noch keine Bewertungen
- Arvanitakis, Shah, Bennett - 2019 - Diagnosis and Management of Dementia ReviewDokument11 SeitenArvanitakis, Shah, Bennett - 2019 - Diagnosis and Management of Dementia ReviewJuan Carlos AlfaroNoch keine Bewertungen
- Disrupted in Schizophrenia 1: Building Brains and Memories: David J Porteous and J Kirsty MillarDokument7 SeitenDisrupted in Schizophrenia 1: Building Brains and Memories: David J Porteous and J Kirsty Millarrocambolescas perthNoch keine Bewertungen
- Alz Dem Diag Ass Dis Mo - 2020 - Pulsifer - Language Skills As A Predictor of Cognitive Decline in Adults With DownDokument11 SeitenAlz Dem Diag Ass Dis Mo - 2020 - Pulsifer - Language Skills As A Predictor of Cognitive Decline in Adults With DownLivea Sant'AnaNoch keine Bewertungen
- Differentiation of Delirium, Dementia and Delirium Superimposed On Dementia in The Older Person-2018Dokument5 SeitenDifferentiation of Delirium, Dementia and Delirium Superimposed On Dementia in The Older Person-2018Juan Paredes100% (1)
- Research Paper: Alzheimer's DiseaseDokument13 SeitenResearch Paper: Alzheimer's DiseaseABC Four CornersNoch keine Bewertungen
- Delusional Infestation: Clinical Presentations, Diagnosis, and ManagementDokument6 SeitenDelusional Infestation: Clinical Presentations, Diagnosis, and ManagementnardiniyanNoch keine Bewertungen
- HHS Public Access: Cognitive Decline and Dementia in Diabetes: Mechanisms and Clinical ImplicationsDokument27 SeitenHHS Public Access: Cognitive Decline and Dementia in Diabetes: Mechanisms and Clinical ImplicationsSaddam FuadNoch keine Bewertungen
- 10.1016@B978 0 444 64012 3.00003 4Dokument13 Seiten10.1016@B978 0 444 64012 3.00003 4loloasbNoch keine Bewertungen
- Mild Cognitive Impairment Continuum 2016Dokument15 SeitenMild Cognitive Impairment Continuum 2016Habib G. Moutran BarrosoNoch keine Bewertungen
- 2017 Harripaul ColdSpringHarbPerspectMedDokument14 Seiten2017 Harripaul ColdSpringHarbPerspectMedEAPNoch keine Bewertungen
- Early-Onset Dementia: Frequency and Causes Compared To Late-Onset DementiaDokument7 SeitenEarly-Onset Dementia: Frequency and Causes Compared To Late-Onset DementiaLuis Alfredo Soares FalcãoNoch keine Bewertungen
- Jama 2017 DeliriumDokument30 SeitenJama 2017 DeliriumLina MariaNoch keine Bewertungen
- Delirium in Older Adults in Associated With Development of New DementiaDokument11 SeitenDelirium in Older Adults in Associated With Development of New DementiaIrvin MarcelNoch keine Bewertungen
- Bipolaridad 1Dokument12 SeitenBipolaridad 1JambisNoch keine Bewertungen
- Nöthen Et Al (2010)Dokument9 SeitenNöthen Et Al (2010)Micaela TaverniniNoch keine Bewertungen
- Captura de Pantalla 2022-10-28 A La(s) 10.55.14Dokument9 SeitenCaptura de Pantalla 2022-10-28 A La(s) 10.55.14Juan Carlos Carbajal SilvaNoch keine Bewertungen
- Understanding the Many: Navigating Dissociative Identity DisorderVon EverandUnderstanding the Many: Navigating Dissociative Identity DisorderNoch keine Bewertungen
- SHDHDJDJDDokument1 SeiteSHDHDJDJDAndi Mahifa 93Noch keine Bewertungen
- Formulasi Dan Uji Stabilitas Fisik Sediaan Emulsi Minyak IKAN LEMURU (Sardinella Lemuru) Patihul Husni, Yasarah Hisprastin, Melinda JanuartiDokument10 SeitenFormulasi Dan Uji Stabilitas Fisik Sediaan Emulsi Minyak IKAN LEMURU (Sardinella Lemuru) Patihul Husni, Yasarah Hisprastin, Melinda JanuartiAndi Mahifa 93Noch keine Bewertungen
- Development and Optimization of Novel Diclofenac Emulgel For Topical Drug DeliveryDokument5 SeitenDevelopment and Optimization of Novel Diclofenac Emulgel For Topical Drug DeliveryAndi Mahifa 93Noch keine Bewertungen
- Aquaculture: Bo Liu, Xianping Ge, Yanhui He, Jun Xie, Pao Xu, Yijin He, Qunlan Zhou, Liangkun Pan, Ruli ChenDokument7 SeitenAquaculture: Bo Liu, Xianping Ge, Yanhui He, Jun Xie, Pao Xu, Yijin He, Qunlan Zhou, Liangkun Pan, Ruli ChenAndi Mahifa 93Noch keine Bewertungen
- Obat Tradisional China: Kelompok 1Dokument13 SeitenObat Tradisional China: Kelompok 1Andi Mahifa 93Noch keine Bewertungen
- Analysis Journal ContentsDokument10 SeitenAnalysis Journal ContentsSLNoch keine Bewertungen
- How To Use Chia Seeds To Lose WeightDokument2 SeitenHow To Use Chia Seeds To Lose WeightMax OratioNoch keine Bewertungen
- JONES Criteria: Rheumatic FeverDokument5 SeitenJONES Criteria: Rheumatic FeverChristopher GarrettNoch keine Bewertungen
- Bird FluDokument3 SeitenBird FludocspaNoch keine Bewertungen
- Article in Press: Neuroscience and Biobehavioral ReviewsDokument10 SeitenArticle in Press: Neuroscience and Biobehavioral ReviewsSahrul FajarNoch keine Bewertungen
- WWDP Requirements PDFDokument2 SeitenWWDP Requirements PDFPure GreenNoch keine Bewertungen
- Introduction To Environmental EngineeringDokument41 SeitenIntroduction To Environmental EngineeringPaul Santos NonatNoch keine Bewertungen
- Preventing Deep Vein ThrombosisDokument8 SeitenPreventing Deep Vein ThrombosisOncology NurseNoch keine Bewertungen
- 011-Vito Armando Laudicina 2013Dokument8 Seiten011-Vito Armando Laudicina 2013Leni Widiarti LenwidNoch keine Bewertungen
- ASD Interventions Theories, Age Range and SettingsDokument4 SeitenASD Interventions Theories, Age Range and SettingstracycwNoch keine Bewertungen
- Operation Maintenance of EtpDokument1 SeiteOperation Maintenance of Etpaminur rahamanNoch keine Bewertungen
- Healthy LifestyleDokument2 SeitenHealthy LifestyleEmmalyn Cabillan SereñoNoch keine Bewertungen
- Lactose Intolerance: Diano, Gabriella Hilde Fanged, Paula Mandy Marrero, Xandra 9-KryptonDokument15 SeitenLactose Intolerance: Diano, Gabriella Hilde Fanged, Paula Mandy Marrero, Xandra 9-KryptonArrianne AcopNoch keine Bewertungen
- Bio-Medical Waste Management Rules: DR NaveenDokument26 SeitenBio-Medical Waste Management Rules: DR Naveenmani kandanNoch keine Bewertungen
- Thyriodectomy BrochureDokument2 SeitenThyriodectomy BrochureHeedahNoch keine Bewertungen
- Carmin WentworthDokument4 SeitenCarmin Wentworthapi-356549360Noch keine Bewertungen
- MastitisDokument27 SeitenMastitisLaprida RecoletaNoch keine Bewertungen
- Kleihauer TestDokument3 SeitenKleihauer Testteo2211Noch keine Bewertungen
- Chlinical Pharmacokinetics On Renal Failure PatientsDokument29 SeitenChlinical Pharmacokinetics On Renal Failure PatientsDenadaPutriNoch keine Bewertungen
- Veris TOHDokument35 SeitenVeris TOHtofssbiNoch keine Bewertungen
- 2011 Colposcopic Terminology of The International Federation For Cervical Pathology and Colposcopy - 2012Dokument7 Seiten2011 Colposcopic Terminology of The International Federation For Cervical Pathology and Colposcopy - 2012Alejandro BritoNoch keine Bewertungen
- Cayman Islands National Youth Policy September 2000Dokument111 SeitenCayman Islands National Youth Policy September 2000Kyler GreenwayNoch keine Bewertungen
- Iqoro Making Strides Into New International MarketsDokument2 SeitenIqoro Making Strides Into New International MarketsGeorge BustonNoch keine Bewertungen