Beruflich Dokumente
Kultur Dokumente
Helping New Mothers Find Their Voices
Hochgeladen von
Lecery Sophia WongOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Helping New Mothers Find Their Voices
Hochgeladen von
Lecery Sophia WongCopyright:
Verfügbare Formate
Postpartum Depression: How Childbirth
Educators Can Help Break the Silence
Cheryl Zauderer, MS, RN, CNM, NPP
ABSTRACT
The voices of women suffering from postpartum depression are often silent. Women are reluctant to
reveal to others that they are unhappy after the birth of their babies. Much has been written on pos-
sible causes, risk factors, and treatments for postpartum depression, but little has been done to in-
vestigate why women take so long to seek help. Early detection and treatment are key to a full
recovery. Childbirth educators are in the position to offer anticipatory guidance on possible compli-
cations of the postpartum period, including postpartum depression. This article explores why women
with postpartum depression choose to suffer in silence and suggests how childbirth educators can help
new mothers find their voices.
The Journal of Perinatal Education, 18(2), 23–31, doi: 10.1624/105812409X426305
Keywords: postpartum depression, childbirth education, anticipatory guidance
Pregnancy, the postpartum period, and parenting may be a time of high vulnerability for women, cou-
present a multitude of challenges for many women pled with feelings of loss of control. Tremendous
and their partners. Findings from the Listening to changes occur in the mother’s interpersonal and fa-
Mothers II survey demonstrate that many new moth- milial world. The birth of a new baby is expected to
ers experience a variety of physical and emotional be a joyful milestone in a woman’s life, but that is
symptoms after birth (Declercq, Sakala, Corry, & not always the case. Some women experience minor
Applebaum, 2006). Survey results found that ‘‘im- adjustment issues, and others experience a grave
proving the knowledge and skills of childbearing and debilitating mood disorder, known as postpar-
women’’ (p. 14) must be a priority, in addition to tum depression. More than half of the women with
providing reliable and trustworthy maternity care. PPD go undetected and undiagnosed because the
new mother may be unwilling to reveal how she
POSTPARTUM DEPRESSION is feeling to her provider or close family members,
Pregnancy, labor, and birth are perhaps the most including her spouse (Beck, 2006). She may be
significant life experiences that a woman and her embarrassed by her symptoms, or afraid that, if
partner will encounter. It is a time of extreme phys- revealed, she will be institutionalized and separated
ical and emotional transition with intense hor- from her baby (Kennedy, Beck, & Driscoll, 2002).
monal, psychological, and biological changes, all Postpartum depression occurs in approximately
of which can have an effect on the central nervous 13% of new mothers (Gaynes et al., 2005; O’Hara &
system (Studd & Panay, 2004). The puerperium Swain, 1996). It is usually detected between 2 and 6
Postpartum Depression | Zauderer 23
The new mother who is depressed is deprived of the pleasures and which causes her to suffer in silence. The new mother
who is depressed is deprived of the pleasures and
joy of giving birth and caring for her newborn baby.
joy of giving birth and caring for her newborn baby
weeks postpartum and can last up to 2 years. Beck (Kennedy et al., 2002).
(2006) describes PPD as a ‘‘crippling mood disor- Childbirth educators can play a significant role in
der’’ (p. 40) often overlooked by health-care providers, helping to break this silence, first by providing the
which can cause the woman anxiety and confusion. necessary education to help women and their part-
ners recognize the early signs and symptoms of
CHILDBIRTH EDUCATION AND postpartum depression (PPD). Second, educators
POSTPARTUM DEPRESSION can help increase a woman’s understanding of
Morton and Hsu (2007) investigated ways for child- how to meet her own needs. This approach can im-
birth educators to enhance the curricula in their prove a woman’s overall state of mental wellness,
classes in order to remain current and accommo- thereby possibly preventing or lessening the experi-
date a new generation of consumers. Childbearing ence of PPD. Although prevention of PPD may not
couples are attending childbirth education classes be completely possible, health professionals can
with a new set of eyes. Young couples today are help recognize and reduce key risk factors. Dennis
more technologically savvy and have many alterna- (2004) found that several interventions—including
tives to education, including the Internet (Declercq providing antenatal classes, information during the
et al., 2006). Many of those who do attend child- antenatal period, intrapartum support, early post-
birth education classes have broader interests than partum checkups, and continuity of care—may
simply learning the Lamaze way of breathing have significant nonpharmacological preventative
(Morton & Hsu, 2007). Childbirth educators are results. Ogrodniczuk and Piper (2003) conducted
modifying their curricula to support the social a literature review to analyze results from studies
and cultural changes of the childbearing community that examined the relationship between prevention
and including topics such as postpartum care, new- of PPD and selective interventions. Interventions
born care, and the prevention and identification of assessed included postpartum debriefing, continuity
early signs of postpartum depression. of care in the postpartum period, education in the
Childbirth education classes provide an oppor- prenatal period, early postpartum checkups, sup-
tunity to teach a new mother to anticipate the help port at home following childbirth, and social sup-
and support she might need for the birth of her port in the postpartum period. An overview of such
child. According to Day (2007), depression and studies provides support for introducing and dis-
abuse are not adequately attended to prior to child- cussing these topics and preventative methods dur-
birth, and weaknesses exist in identifying and sup- ing childbirth education classes. The childbirth
porting women at risk. Day (2007) suggests ways education class is an ideal environment because the
to improve communication and support among educator usually has the attention of both parents
childbirth education class members, including or a mother and her significant other.
maintaining contact via e-mail, sending photos to The overall subject matter of childbirth educa-
each other, and even getting together for a reunion. tion should include the postpartum period as
All of these techniques may help to keep the lines of well as newborn and infant care and expectations
communication open. It is known that social isola- (Kattwinkel et al., 2004). Through childbirth educa-
tion as well as the strong desire for social support tion, health-care professionals can also reach out to
during the postpartum period are related to the de- new fathers. Men often complain about not being an
velopment of postpartum depression (Martinez- integral part of the childbirth experience. In a study
Schallmoser, Telleen, & MacMullen, 2003). conducted by Premberg and Lundgren (2006),
Lothian (2007) notes that childbearing women fathers felt that the information obtained through
want information regarding complications and risks childbirth classes was inadequate for their particular
of childbirth, including caesarean section, epidural needs. However, they also reported that the classes
analgesia, and induction. Although often a hidden not only helped prepare them for the labor and birth
occurrence of illness, postpartum depression is be- experience, but also gave them anticipatory guid-
lieved to be the leading complication of childbirth ance for what to expect when bringing the newborn
today (Gaynes et al., 2005). It is an illness that is often infant home. A new mother may be overwhelmed
undetected and usually obscured by the woman, and sleep deprived while caring for her newborn;
24 The Journal of Perinatal Education | Spring 2009, Volume 18, Number 2
thus, it is often the father (or partner) who may rec- in appetite (weight loss or gain) (Bennett & Indman,
ognize the early signs and symptoms of PPD. The 2003).
new mother may not want to admit to having these
symptoms, but the father/partner can encourage or Postpartum Obsessive-Compulsive Disorder
urge her to seek help when needed. If the father or Postpartum obsessive-compulsive disorder presents
partner learns about the early warning signs of PPD in 3% to 5% of new mothers (Bennett & Indman,
during classes, he or she will be in a better position 2003). The primary symptom consists of repetitive
to assess and notice these changes and to encourage and unrelenting thoughts, fears, or images. The
the new mother to seek help. thoughts appear spontaneously and may or may
not involve harming the baby either intentionally
POSTPARTUM MOOD DISORDERS AND or accidentally.
SYMPTOMS
Bennett and Indman (2003) classify postpartum Postpartum Panic Disorder
mood disorders into five categories: (1) postpartum Postpartum panic disorder occurs in about 10% of
depression and/or anxiety; (2) postpartum ob- postpartum women (Bennett & Indman, 2003).
sessive-compulsive disorder; (3) postpartum panic Feelings come on suddenly, and the woman experi-
disorder; (4) postpartum psychosis; and (5) post- ences extreme anxiety. An episode includes physical
partum posttraumatic stress disorder. Each disorder symptoms such as shortness of breath, chest pain,
presents a range of mood changes and physical com- and sensations of choking, dizziness, derealization,
plaints. Bennett and Indman (2003) also note that hot or cold flashes, trembling, restlessness, palpita-
postpartum ‘‘blues’’ is not considered a disorder; tions, numbness, or tingling (Beck & Driscoll,
it is regarded as part of the normal postpartum ad- 2006).
justment.
Postpartum Psychosis
Postpartum ‘‘Blues’’ According to Bennett & Indman (2003), postpar-
According to Bennett and Indman (2003), normal tum psychosis is the most extreme of all the post-
postpartum adjustment and the ‘‘blues’’ represent partum mood disorders. It is rare, occurring in 1 to
normal biological and psychosocial adjustments 3 mothers per 1,000 births. Onset is within the first
to giving birth and do not impair the daily function- 24 to 72 hours after giving birth. Postpartum psy-
ing of the mother or impinge on the maternal-new- chosis has a 5% suicide and a 4% infanticide rate.
born bonding experience. Approximately 80% of Afflicted women have an abnormal thought process
postpartum women experience the ‘‘blues,’’ which and lose touch with reality. Considerable confusion,
are mild hormonal changes that take place within poor judgment, delusions, and hallucinations are
the first 48 hours after giving birth. These symptoms noted, usually with a religious quality. Postpartum
may last up to 6 weeks (Bennett & Indman, 2003). psychosis can be life-threatening to both the mother
Symptoms of the ‘‘blues’’ include mood instability, and the baby (Bennett & Indman, 2003).
weepiness, sadness, anxiety, lack of concentration,
and feelings of dependency (Beck, 2006). If symp- Postpartum Posttraumatic Stress Disorder
toms last longer than 6 weeks or worsen during According to Bennett and Indman (2003), postpar-
the 6-week interval, a woman meets the criteria tum posttraumatic stress disorder is usually con-
for being diagnosed with PPD. nected to a specific trauma relating to the birth
of the baby or an event from the woman’s past.
Postpartum Depression and/or Anxiety A new mother who is reminded of this past trauma
Symptoms of PPD and anxiety are presented in can often suffer from panic attacks. Symptoms may
a number of ways. They may include excessive include recurrent nightmares, extreme anxiety, or
worry or anxiety; irritability or short temper; feel- reliving past traumatic events, including sexual
ings of being overwhelmed; feeling very sad, guilty trauma, physical or emotional trauma, and child-
or phobic; hopelessness; sleep disturbances (either birth (Bennett & Indman, 2003).
too much or too little sleep); excessive physical
complaints; loss of focus or concentration (fre- A COMPLEX HEALTH PROBLEM
quently missing appointments); loss of interest or The occurrence of PPD is rapidly being recognized
pleasure in anything; lack of libido; and changes as a major public health problem (Gaynes et al.,
Postpartum Depression | Zauderer 25
2005). Furthermore, the occurrence of PPD is an untreated, a new mother can begin to experience re-
apparent paradox. It is an unusual disparity for peated thoughts of death or suicide, which can oc-
a woman to become clinically depressed just weeks cur in any major depressive illness (Beck, 2002).
after giving birth, a time when one would assume Postpartum depression has become a type of psy-
the new mother is happy and joyous. Although chological block for women who suffer. According
PPD mimics a traditional clinical depression, there to Gilligan (1982), when a girl grows into woman-
are major symptomatic differences between the two hood, she is expected to become a selfless individ-
disorders. Women who suffer from PPD usually ual. Attachment or bonding is fundamental in the
manifest symptoms that are much more severe than development of a loving and trusting relationship
women who suffer from a major depressive disorder between a mother and her newborn baby. What
that is unrelated to the postpartum period (Jacobsen, new mothers do not realize is that bonding with
1999). their infant can take some time and effort. A new
Mauthner (2002) conducted interviews and mother’s expectation of an immediate bonding
found that women with PPD perceive themselves can cause her to feel incompetent. A combination
and those around them with trepidation. These of physical, psychological, and biopsychosocial fac-
women assume a passive attitude, and they will of- tors can cause this bonding experience to go awry.
ten isolate themselves from others due to fear and The social stigma of a lack of bonding or the pos-
a lack of understanding of their illness. Women with sibility of a new mother not feeling complete bliss
PPD would rather separate themselves from friends over the birth of her child causes the woman to re-
and loved ones than reveal what they are experienc- main silent. ‘‘This loss of relationship leads to a mut-
ing, especially when it goes against social and cul- ing of voice, leaving inner feelings of sadness and
tural standards and expectations. Their fear of isolation. In effect, the young woman becomes shut
being labeled as a nonperfect mother creates the si- up within herself’’ (Gilligan, 1995, p. 125). The
lence that makes their illness difficult to endure and woman with PPD may feel a loss of relationship
their recovery complex. with her newborn, spouse, friends, and even her
own mother. Women have described feeling totally
SIGNS, SYMPTOMS, AND BEHAVIORAL alone, unaware that they may be causing their own
CHANGES IN WOMEN WITH POSTPARTUM isolation.
DEPRESSION
A variety of symptoms of PPD contribute to the si- WHY THE SILENCE?
lence in sufferers. The experience from one woman Women with PPD tend to suffer with their symp-
to the next varies tremendously, which results in toms for quite some time before admitting to their
confusion for the woman who tries to distinguish symptoms or seeking help. Some women never get
and understand what she is experiencing (Venis & help and just wait until the symptoms dissipate with
McClosky, 2007). Some women may feel that they time. Many choose to suffer alone, unable to tell
do not have PPD because they do not feel ‘‘de- their friends, spouse or health-care provider what
pressed.’’ Instead, they may be experiencing severe is happening. They often struggle with this decision,
anxiety, disrupted sleep, loss of appetite, and obses- knowing that by not seeking help they are being ir-
sive thoughts about their newborn. Some women responsible, placing themselves and their new baby
actually feel as if they are ‘‘going crazy’’ because in possible danger, yet they still choose to remain
their symptoms do not match what they read or silent.
hear about, and they are afraid to reveal the things Mauthner (2002) found that many new mothers
that are really going on inside their heads. These are afraid to admit to their symptoms of PPD and
symptoms can lead to feelings of worthlessness are disinclined to seek any form of medical or psy-
and of being a bad mother, no interest in previous chotherapeutic help because they are fearful of the
enjoyable activities, little interest in her newborn, consequences. These women know that, if they ad-
and obsessive worry over the baby’s health. If left mit to having thoughts of harming their newborn or
themselves, they will be hospitalized. They are also
Women with postpartum depression tend to suffer with their terrified of having their baby taken away from them.
These women are concerned about the public hu-
symptoms for quite some time before admitting to their symptoms
miliation. They do not want to feel different from
or seeking help. other mothers, and they are apprehensive about
26 The Journal of Perinatal Education | Spring 2009, Volume 18, Number 2
the stigma related to depression and being under the newborn, tending to their physical appearance, their
care of a mental health provider. Some women, es- homes, breastfeeding around the clock, and so on.
pecially those who grew up in a cultural community Their silence may stem from that fastidiousness, vy-
that has high expectations of motherhood and par- ing for perfection, and not being able to admit that
enting, may be afraid of disapproval by others in they might be less than a perfect mother.
their society. They are gravely concerned about Edhborg, Friberg, Lundh, and Widstrom (2005)
their future relationship with their child and found that the new mothers in their study tried so
how their depression will affect the child’s devel- hard to manage their newborn and their feelings that
opment. they were afraid to show any kind of weakness. The
Childbirth education classes provide information women were not willing to discuss their feelings with
about the process of pregnancy, childbirth, and the anyone, even close friends and family. Mauthner
early stages of becoming a parent. The purpose is to (1999, 2002) found that women with PPD are often
help expectant couples gain awareness and prepare thankful when they discover they have a diagnosable
for their birthing experience and to provide them illness as opposed to being ‘‘crazy’’ or ‘‘bad mothers.’’
with comfort and pain-management skills (Nichols Lamberg (2005) notes that health-care providers may
& Humenick, 2000). Although the general philoso- not be able to pick up on symptoms of depression
phy of Lamaze International (2007) is to promote because the symptoms often mimic other perinatal
normal birth, according to Lothian (2007), child- disorders, such as anemia, thyroid disease, and ges-
birth educators have a captive audience and can tational diabetes. Women with PPD may not report
broaden their curricula. Childbirth classes are an their symptoms to their health-care provider due to
ideal time to introduce the possibility that things stigmatization, and they may refuse psychotropic
may not go as planned and to provide content about medications, thinking the medication will harm their
signs and symptoms of PPD. newborn if they are breastfeeding. Most of the studies
Mauthner (1999) argues that women, in general, on PPD have included women who presented with
are deeply concerned with relationships and become symptoms in their health-care provider’s office or
somewhat vulnerable and dependent on others. clinic. Study results reveal that not many women seek
Their vulnerability intensifies when they have a treatment on their own. Women who do seek treat-
new baby and realize that the workload, sleep dep- ment are probably more symptomatic than those
rivation, responsibilities, and social isolation are not who do not, and they may also have had a prior
what they anticipated. This creates a sense of loss history of depression (Battle, Zlotnick, Miller,
of control, causing depression to set in. Mauthner Pearlstein, & Howard, 2006).
(1999) believes that mothers are constantly belittled, Edwards and Timmons (2005) found that five
and motherhood is viewed in a negative light. out of six women in their study were reluctant to
Women who are career-oriented are looked upon come forward about their illness and, therefore,
more favorably in the public eye and are viewed did not receive treatment for PPD in a timely man-
as independent. Mauthner (1999) states, ‘‘Postpartum ner. The women all felt that their symptoms were
depression occurs when women are unable to expe- a reflection of them as mothers, and if they were
rience, express and validate their feelings and needs perceived as unable to cope with motherhood, their
within supportive, accepting and non-judgmental babies would be taken from their care. They felt that
interpersonal relationships and cultural context’’ they did not have the natural maternal instincts that
(p. 160). other mothers reported, and even though they were
In Lauer-Williams’ (2001) phenomenological re- caring for their infants in a mechanical way, they
search study on women with PPD, a general theme feared that even those tasks might become difficult
that emerged was guilt, humiliation, and a feeling of as their illness progressed. Once the women were
not being an average mother. These women wanted told that they actually had a treatable illness, they
to fit in with everyone else and felt somewhat dis- were quite relieved.
graced by the fact that they did not. Lauer-Williams Childbirth educators can offer anticipatory guid-
(2001) concludes that women with PPD who choose ance and instruction by increasing awareness of
to remain silent are more concerned about their ex- possible mental health changes in the postpartum
posure to the public than they are about what is go- period. According to results in a study by Roux,
ing on inside of themselves. They seem to have high Anderson, and Roan (2002), postpartum women
expectations of themselves around caring for their are unprepared for the feelings of stress, loneliness,
Postpartum Depression | Zauderer 27
and seclusion that they experience. Ho and Holroyd ples may face in the postpartum period may prevent
(2002) found that the women in their study who serious consequences that can happen from delayed
attended childbirth education classes did not feel pre- diagnosis and treatment.
pared for motherhood. Although they felt confident
in their knowledge regarding self and newborn care, Stress Importance of Advance Planning Prior
they were unprepared for the demands of the first to Birth
postpartum month. However, couples who attended The topic of PPD can be added to the last class in the
a subsequent class on emotional issues felt prepared series when the discussion mostly focuses on prep-
for the demands of bringing home a newborn, as well aration for labor, the hospital, bringing the newborn
as the possibility of mood disorders, and were told home, and what to expect in the postpartum period.
to alert their spouses for help if symptoms of mood Couples can be encouraged to do some after-birth
disorders became apparent. According to Roux et al. planning such as interviewing pediatricians, prepar-
(2002), childbirth and Lamaze educators need to be ing their hospital bag, and stocking up on all the
upfront with couples and provide information on necessities and paraphernalia that they will need
postpartum changes and possible mood disorders, for their arrival home from the hospital with their
offering them appropriate resources on where to newborn. This is also a good time to discuss breast-
get help if the need arises. feeding.
The last class may also be reserved for discussions
PRACTICE IMPLICATIONS on how couples can prepare their home in order to
Nurses and childbirth educators in all clinical areas make life as easy as possible. Most new couples are
need to be aware of the signs and symptoms of PPD unaware of the magnitude of bringing a newborn
and increase awareness that PPD is a treatable disor- home. Educators can suggest that the couples pre-
der. By teaching women and their partners about pare meals in advance or obtain takeout menus
symptoms of PPD, educators can increase the chance from local restaurants. Most of all, they can be en-
that an afflicted woman will receive proper screening, couraged to arrange in advance for domestic help
diagnosis, and treatment. Couples who have been during the postpartum period. Many new mothers
educated about the signs and symptoms of PPD will are unaware of how tired, sore, and overwhelmed
be aware and alert if and when the disorder occurs. they will be during the postpartum period. There
Knowing that PPD is an illness that does happen on is also always the possibility of having an unplanned
occasion, and the odd feelings they may experience caesarean section, which can further immobilize the
are all part of the syndrome, will help new mothers mother in the first few days after birth. By making
come forward and not feel stigmatized. This knowl- advance arrangements—with her mother, mother-
edge will enable them to ask for help and to seek out in-law, or even hired help such as a doula—the new
the necessary resources for their care. mother can anticipate the ability to get the rest
that she needs. According to Simkin (2001), a new
INCORPORATING POSTPARTUM mother’s most important tasks in the early postpar-
DEPRESSION CONTENT INTO THE LAMAZE tum period are to initiate a good feeding relation-
CURRICULUM ship with her newborn, to get enough rest, and to
According to Humenick (2002), it is during the pre- eat properly in order to give both partners an op-
natal period that couples are most receptive to the portunity to get to know their newborn.
changes that are happening in their lives, and they Stressing the importance of planning in advance
are willing to take in and absorb a great deal of in- for help during the postpartum period may prevent
formation on their pregnancy and beyond. Even the fatigue, sleep deprivation, and/or social isolation
though educators try to maintain a sense of ‘‘nor- that can sometimes create vulnerability in postpar-
malcy’’ in childbirth and do not want to instill fear tum women and, in turn, may make them more likely
in couples, approaching the possible challenges cou- to develop PPD. According to Sichel and Driscoll
(1999), women may have various psychological
or psychosocial issues or stressful life events that
Childbirth educators can offer anticipatory guidance and instruction occur over time. The weight of these life events
can disrupt the balance of the brain biochemistry,
by increasing awareness of possible mental health changes in the
resulting in a sort of ‘‘emotional earthquake’’
postpartum period. (Sichel & Driscoll, p. 99).
28 The Journal of Perinatal Education | Spring 2009, Volume 18, Number 2
Introduce Possibility of Developing Postpartum TABLE 1
Depression Warning Signs of Postpartum Mood Disorders (Onset May
Occur at 4 Weeks up to 1 Year)
Studies have shown that many physiological, bio-
logical, and psychosocial factors may contribute d Increasing insomnia, even when the baby is sleeping
to the etiology of PPD. Some of the physiological d Extreme emotional lability, crying excessively
factors include fatigue, pain, thyroid abnormalities, d Overeating or undereating
weakened immune system, and elevated cholesterol d Increasing depression or irritability
(Kendall-Tackett, 2005). Some of the psychosocial
d Thoughts of hurting themselves or their newborn
d Becoming increasingly socially withdrawn
factors include alterations in self-esteem, expecta- d Not interacting with the baby, feeling discomfort in the role of
tions of motherhood, a sense of loss, prior psychi- motherhood
atric diagnosis, family history of psychiatric illness, d Anxiety or panic attacks
history of abuse or violence, parenting difficulties, d Hypomania or mania symptoms—no need for sleep, speaking
stressful life events, socioeconomic status, social very fast, hyperactive
d Psychotic break—hallucinations/delusion (extremely rare)
support, and cultural rituals (Kendall-Tackett,
2005).
Again, the final childbirth education or Lamaze a prior history of depression, postpartum blues, sin-
class, which typically focuses on the postpartum gle parenting, and low self-esteem) can alert parents
period, is an appropriate time to introduce the to their risks of developing PPD and increase their
possibility of developing PPD. A brief discussion of awareness of these factors (Beck, 2006).
normal postpartum adjustment issues and postpar- Many different resources are available to post-
tum blues can be presented, followed by a discussion partum women. The two largest national organiza-
of more severe emotional reactions such as PPD. tions are Depression After Delivery and Postpartum
Because the spectrum of symptoms can vary, it is Support International. These organizations focus
important to review the five categories of postpar- on helping women through education, information,
tum mood disorders, as described by Bennett and support, and referrals in the event of difficulties af-
Indman, (2003). Sometimes, a postpartum woman ter birth. They also offer support-group informa-
will feel a variety of symptoms and not be aware that tion, conferences, recommended reading lists, and
she is experiencing PPD because she is having more lists of mental health providers in every state. Post-
anxiety than depression. Providing a list of warning partum Support International has a Web site that
signs (Table 1) will help couples understand what to includes information about PPD and offers self-help
look for and when to know to seek help. It is im- suggestions. Web sites are a good source of informa-
portant to emphasize that early detection and treat- tion for childbirth educators to keep up on current
ment is the fastest way to recovery. It is also information regarding postpartum mood disorders.
important to explain to the couples how to differ- They are also helpful for couples to access informa-
entiate between normal postpartum adjustment, tion on their own, so they can recognize their symp-
postpartum blues (Table 2), or a postpartum mood toms and not feel as if they are completely alone. A
disorder. list of Internet resources is presented in Table 3.
It is probably wise to approach the subject of
PPD gently and to ease it into an already established CONCLUSION
curriculum. Some childbirth educators and Lamaze The veil of the stigma associated with PPD will
instructors address postpartum emotions during slowly lift as more women struggle to find their
the class scheduled for discussion of possible com- voice. Childbirth educators and Lamaze instructors
plications in labor and caesarean sections. Potential
complications in the postpartum period and warn-
ing signs such as increased bleeding and fever are TABLE 2
typically discussed; this would be a good opportunity Postpartum Blues (Lasts from a Few Days to 3 Weeks)
to mention the possibility of developing postpartum d Mood swings
blues, which is very normal, and, if the depression d Weepiness
worsens, that a small percentage of women can d Mild anxiety
develop PPD. A discussion of risk factors (e.g., pre- d Fatigue/Low energy
natal depression, childcare stress, life stress, a lack of d Worry
d Mild sleep disturbances
social support, prenatal anxiety, marital conflicts,
Postpartum Depression | Zauderer 29
TABLE 3 tional U.S. survey of women’s childbearing experiences.
Internet Resources for Postpartum Depression New York: Childbirth Connection.
Dennis, C. E. (2004). Preventing postpartum depression
Postpartum Depression – Information from the Mayo Clinic Part II: A critical review of nonbiological interven-
d http://www.mayoclinic.com/health/postpartum-depression/ tions. Canadian Journal of Psychiatry, 49(8), 526–538.
DS00546 Edhborg, M., Friberg, M., Lundh, W., & Widstrom, A. M.
Postpartum Depression – Information from MedlinePlus, (2005). ‘‘Struggling with life’’: Narratives from women
a service of the U.S. National Library of Medicine and the with signs of postpartum depression. Scandinavian
National Institutes of Health (available in English and Spanish) Journal of Public Health, 33(4), 261–267.
d http://www.nlm.nih.gov/medlineplus/postpartumdepression. Edwards, E., & Timmons, S. (2005). A qualitative study of
html stigma among women suffering from postnatal illness.
Postpartum Support International (PSI) Journal of Mental Health, 14(5), 471–481.
d http://postpartum.net/ Gaynes, B. N., Gavin, N., Meltzer-Brody, S., Lohr, K. N.,
d Includes the PSI Postpartum Depression Helpline: 1-800-944- Swinson, T., Gartlehner, G. , et al. (2005, February).
4PPD Perinatal depression: Prevalence, screening accuracy, and
Postpartum Depression and the Baby Blues – Information screening outcomes. Evidence Report/Technology Assess-
from the American Academy of Family Physicians ment No. 119. AHRQ Publication No. 05-E006-2. Rock-
d http://familydoctor.org/online/famdocen/home/women/preg- ville, MD: Agency for Healthcare Research and Quality,
nancy/ppd/general/379.html U.S. Department of Health and Human Services.
Depression after Delivery, Inc. (DAD) Gilligan, C. (1982). In a different voice: Psychological theory
d http://depressionafterdelivery.com and women’s development. Cambridge, MA: Harvard
University Press.
Gilligan, C. (1995). Symposium on care and justice: Hear-
ing the difference: Theorizing connection. Hypatia,
are in the front line to alert expectant couples to the
10(2), 120–127.
possibility of a postpartum mood disorder. Many Ho, I., & Holroyd, E. (2002). Chinese women’s percep-
obstetrics and pediatric offices now provide screen- tions of the effectiveness of antenatal education in
ing tests for women who exhibit signs and symp- the preparation for motherhood. Journal of Advanced
toms of PPD. However, many of these women Nursing, 38(1), 74–85.
will still be reluctant to admit to or come forward Humenick, S. S. (2002). Dancing with the one who ‘‘brung’’
you into perinatal education. The Journal of Perinatal
with their symptoms. By educating them in their
Education, 11(4), v–viii.
prenatal classes, it is hoped that these women will Jacobsen, T. (1999). Effects of postpartum disorders on
be empowered to admit that they are having a prob- parenting and on offspring. In L. J. Miller (Ed.), Post-
lem. Likewise, their spouse or significant other will partum mood disorders (pp. 119–139). Washington,
also be more aware of the signs and symptoms and DC: American Psychiatric Publishing, Inc.
Kattwinkel, J., Cook, L. J., Nowacek, G., Bailey, C., Crosby,
encourage the new mother to seek help.
W. M., Hurt, H., et al. (2004). Regionalized perinatal
education. Seminars in Neonatology, 9(2), 155–165.
REFERENCES Kendall-Tackett, K. D. (2005). Depression in new mothers:
Battle, C. L., Zlotnick, C., Miller, I. W., Pearlstein, T., & Causes, consequences, and treatment alternatives Bing-
Howard, M. (2006). Clinical characteristics of perina- hamton, NY: Haworth Press, Inc.
tal psychiatric patients: A chart review study. The Jour- Kennedy, H. P., Beck, C. T., & Driscoll, J. W. (2002). A
nal of Nervous and Mental Disease, 194(5), 369–377. light in the fog: Caring for women with postpartum
Beck, C. T. (2002). Theoretical perspectives of postpartum depression. Journal of Midwifery & Women’s Health,
depression and their treatment implications. MCN. 47(5), 318–330.
The American Journal of Maternal Child Nursing, Lamaze International. (2007). Position paper: Promoting,
27(5), 282–287. supporting, and protecting normal birth. The Journal
Beck, C. T. (2006). Postpartum depression: It isn’t just the of Perinatal Education, 16(3), 11–15.
blues. The American Journal of Nursing, 106(5), 40–50. Lamberg, L. (2005). Risks and benefits key to psychotropic
Beck, C. T., & Driscoll, J. W. (2006). Postpartum mood and use during pregnancy and postpartum period. Journal
anxiety disorders: A clinician’s guide. Sudbury, MA: of the American Medical Association, 294(13), 1604–
Jones and Bartlett Publishers. 1608.
Bennett, S. S., & Indman, P. (2003). Beyond the blues. Pre- Lauer-Williams, J. (2001). Postpartum depression: A phe-
natal and postpartum depression. San Jose, CA: Mood- nomenological exploration of the woman’s experience.
swings Press. Dissertation Abstracts International, 62(4-B), 2064.
Day, E. H. (2007). Applying the Listening to Mothers II Lothian, J. A. (2007). The Lamaze Certified Childbirth Edu-
results in Lamaze class. The Journal of Perinatal Educa- cator. The Journal of Perinatal Education, 16(1), 29–31.
tion, 16(4), 52–54. Martinez-Schallmoser, L., Telleen, S., & MacMullen, N. J.
Declercq, E. R., Sakala, C., Corry, M. P., & Applebaum, S. (2003). The effect of social support and acculturation
(2006). Listening to mothers II: Report of the second na- on postpartum depression in Mexican-American
30 The Journal of Perinatal Education | Spring 2009, Volume 18, Number 2
women. Journal of Transcultural Nursing, 14(4), 329– Roux, G., Anderson, C., & Roan, C. (2002). Postpartum
338. depression, marital dysfunction, and infant outcome:
Mauthner, N. S. (1999). ‘‘Feeling low and feeling really A longitudinal study. The Journal of Perinatal Education,
bad about feeling low’’: Women’s experiences of 11(4), 25–36.
motherhood and postpartum depression. Canadian Sichel, D., & Driscoll, J. W. (1999). Women’s moods: What
Psychology, 40(2), 143–161. every woman must know about hormones, the brain, and
Mauthner, N. S. (2002). The darkest days of my life: Stories emotional health. New York: HarperCollins.
of postpartum depression. Cambridge, MA: Harvard Simkin, P. (2001). The birth partner: Everything you need
University Press. to know to help a woman through childbrith (2nd ed.).
Morton, C. H., & Hsu, C. (2007). Contemporary dilem- Boston Harvard Common Press.
mas in American childbirth education: Findings from Studd, J., & Panay, N. (2004). Hormones and depression
a comparative ethnographic study. The Journal of Peri- in women. Climacteric, 7(4), 338–346.
Venis, J. A., & McClosky, S. (2007). Postpartum depression
natal Education, 16(4), 25–37.
Nichols, F. H., & Humenick, S. S. (2000). Childbirth ed- demystified: An essential guide for understanding and
overcoming the most common complication after child-
ucation: Practice, research and theory (2nd ed.). Phila-
birth. New York: Marlowe and Company.
delphia: W.B. Saunders.
O’Hara, M. W., & Swain, A. M. (1996). Rates and risk
of postpartum depression – A meta-analysis. Interna-
tional Review of Psychiatry (Abingdon, England, 8, 37– CHERYL ZAUDERER is a certified nurse-midwife and a psychi-
54. atric nurse practitioner with 23 years of nursing experience in the
Ogrodniczuk, J., & Piper, W. E. (2003). Preventing post- maternal-newborn field and 5 years of experience in the psychi-
natal depression: A review of research findings. Har- atric field. Currently, she is a full-time instructor in the Depart-
vard Review of Psychiatry, 11(6), 291–307. ment of Nursing, School of Health Professions, Behavioral, and
Premberg, A., & Lundgren, I. (2006). Fathers’ experiences Life Sciences, at the New York Institute of Technology and has
of childbirth education. The Journal of Perinatal Edu- a private psychotherapy practice specializing in postpartum de-
cation, 15(2), 21–28. pression.
Doulas...
Caring and Sharing
at the Heart of Birth
Science & Sensibility
A Research Blog About Healthy
Pregnancy, Birth & Beyond
We have updated the published
version of Research Summaries to
a new online blog format to
provide an easy way for busy
n li
childbirth professionals to stay up-
to-date on the latest evidence that
postpa
supports normal birth.
•
www.scienceandsensibility.org
Contact us at
(800) 368-4404 or
info@lamaze.org.
PO Box 626 • Jasper, IN 47547
www.DONA.org • info@DONA.org
888-788-DONA (3662)
Postpartum Depression | Zauderer 31
Das könnte Ihnen auch gefallen
- Written Case Report - Group 5.1Dokument15 SeitenWritten Case Report - Group 5.1YSABELLA MARI CUNANNoch keine Bewertungen
- 379-891-1-PBDokument16 Seiten379-891-1-PBDeva FaradinaNoch keine Bewertungen
- Teenage Pregnancy: A Psychopathological Risk For Mothers and Babies?Dokument5 SeitenTeenage Pregnancy: A Psychopathological Risk For Mothers and Babies?Ronald Pacquiao MacaseroNoch keine Bewertungen
- Prenatal mental health vulnerabilitiesDokument7 SeitenPrenatal mental health vulnerabilitiesFernando PenaNoch keine Bewertungen
- Impact of Doulas Delivery and BFDokument10 SeitenImpact of Doulas Delivery and BFFabiola AndreaNoch keine Bewertungen
- Research The Experiences of Mothers Who Lost A Baby During Pregnancy DR L ModibaDokument11 SeitenResearch The Experiences of Mothers Who Lost A Baby During Pregnancy DR L ModibaNichola GouveiaNoch keine Bewertungen
- Improving The Postnatal Outcomes of New Mothers: Carol MorseDokument23 SeitenImproving The Postnatal Outcomes of New Mothers: Carol Morseani galihNoch keine Bewertungen
- admin,+27649+-+INPRESS PagenumberDokument8 Seitenadmin,+27649+-+INPRESS PagenumberJesica MulyadiNoch keine Bewertungen
- Jognn: Mood and Anxiety Disorders in Pregnant and Postpartum WomenDokument3 SeitenJognn: Mood and Anxiety Disorders in Pregnant and Postpartum Womenyosevangelika hutabaratNoch keine Bewertungen
- Maternal Mental Wellbeing During PregnancyDokument6 SeitenMaternal Mental Wellbeing During PregnancyJuanda RaynaldiNoch keine Bewertungen
- Teenage Pregnancy's Impact on Academic PerformanceDokument13 SeitenTeenage Pregnancy's Impact on Academic PerformanceChristson Ceniza100% (1)
- 10 Sreeja GangadharanDokument12 Seiten10 Sreeja GangadharanSreeja GangaNoch keine Bewertungen
- Jjam ResearchDokument13 SeitenJjam ResearchsamyangjjimiclatNoch keine Bewertungen
- Factors Predicting Postpartum Depression in NigeriaDokument12 SeitenFactors Predicting Postpartum Depression in NigeriaWasiu AfoloabiNoch keine Bewertungen
- Nifas Depressi Post PartumDokument20 SeitenNifas Depressi Post PartumaprimayonaNoch keine Bewertungen
- Free Research Papers On Postpartum DepressionDokument4 SeitenFree Research Papers On Postpartum Depressiongw1gnz6b100% (1)
- annotated__5BREVISED_MANUSCRIPT_5D_FIRST_TIME_MOTHERS_WITH_POSTPARTUM_DEPRESSION.pdfDokument26 Seitenannotated__5BREVISED_MANUSCRIPT_5D_FIRST_TIME_MOTHERS_WITH_POSTPARTUM_DEPRESSION.pdflexfred55Noch keine Bewertungen
- What Can Cause Postpartum Depression - EditedDokument7 SeitenWhat Can Cause Postpartum Depression - EditedkimsmakicheNoch keine Bewertungen
- Mood and Anxiety Disorders in Pregnant and Postpartum Women: PositionDokument7 SeitenMood and Anxiety Disorders in Pregnant and Postpartum Women: PositionMuhammad rizalNoch keine Bewertungen
- Postpartum Depression DissertationDokument7 SeitenPostpartum Depression DissertationPaperWritingServiceCheapAnnArbor100% (1)
- Literature Review Postpartum Depression FinalDokument14 SeitenLiterature Review Postpartum Depression Finalapi-730811728Noch keine Bewertungen
- Postpartum DepressionDokument6 SeitenPostpartum Depressionapi-522555065Noch keine Bewertungen
- Chapter 1-3 (Ineedit)Dokument73 SeitenChapter 1-3 (Ineedit)Majoysa MagpileNoch keine Bewertungen
- Maternal and Child Health Nursing Care of The Childbearing and Childrearing Family Joanne Flagg and Adele PilitteriDokument46 SeitenMaternal and Child Health Nursing Care of The Childbearing and Childrearing Family Joanne Flagg and Adele PilitteriMarianne Angela CortezNoch keine Bewertungen
- Cousineau2007 PDFDokument16 SeitenCousineau2007 PDFtutor 4bNoch keine Bewertungen
- Common Fears Related To Pregnancy, Labor, and Delivery and Coping Mechanisms Among Primigravida MothersDokument70 SeitenCommon Fears Related To Pregnancy, Labor, and Delivery and Coping Mechanisms Among Primigravida MothersSmile Tambanillo0% (1)
- Breastfeeding discomforts and management by primigravida mothersDokument19 SeitenBreastfeeding discomforts and management by primigravida mothersNazria Gilman Kapusan75% (4)
- Postpartum Depression ThesisDokument4 SeitenPostpartum Depression Thesisangelalovettsavannah100% (1)
- Effects Prenatal Stress ChildDokument5 SeitenEffects Prenatal Stress ChildmiguelNoch keine Bewertungen
- Bounding AttachmentDokument20 SeitenBounding AttachmentNerz Clish100% (1)
- Journal of Advanced Nursing - 2015 - Brown - Understanding The Relationship Between Breastfeeding and Postnatal DepressionDokument10 SeitenJournal of Advanced Nursing - 2015 - Brown - Understanding The Relationship Between Breastfeeding and Postnatal DepressionErika WulandariNoch keine Bewertungen
- TSWJ2021 9512854Dokument7 SeitenTSWJ2021 9512854Raden Ayu Miftah CahyaniNoch keine Bewertungen
- New Born ScreeningDokument22 SeitenNew Born ScreeninglendiibanezNoch keine Bewertungen
- Fear of Childbirth: Mothers' Experiences of Team-Midwifery Care - A Follow-Up StudyDokument8 SeitenFear of Childbirth: Mothers' Experiences of Team-Midwifery Care - A Follow-Up Studyyayusuk desamtaNoch keine Bewertungen
- Exclusive Breastfeeding Duration and Perceptions of Infant Sleep: The Mediating Role of Postpartum AnxietyDokument11 SeitenExclusive Breastfeeding Duration and Perceptions of Infant Sleep: The Mediating Role of Postpartum AnxietyJAN CAMILLE LENONNoch keine Bewertungen
- Postnatal Depression: How Can Midwives Help?: Midwifery December 1997Dokument10 SeitenPostnatal Depression: How Can Midwives Help?: Midwifery December 1997caipillanNoch keine Bewertungen
- Jurnal Kesehatan Masyarakat: Benefit of Childbirth Care Counseling For Mood of Postpartum PeriodDokument10 SeitenJurnal Kesehatan Masyarakat: Benefit of Childbirth Care Counseling For Mood of Postpartum PeriodseptiaNoch keine Bewertungen
- Article 38 Martinez Shaw 2021Dokument19 SeitenArticle 38 Martinez Shaw 2021Naoual EL ANNASNoch keine Bewertungen
- Term Paper On Postpartum DepressionDokument8 SeitenTerm Paper On Postpartum Depressionc5mr3mxf100% (1)
- GHDokument9 SeitenGHReginald JuliaNoch keine Bewertungen
- Literature Review On Postpartum DepressionDokument5 SeitenLiterature Review On Postpartum Depressionea6bmkmc100% (1)
- Learn: Communication With Women During The Postpartum Period 1Dokument6 SeitenLearn: Communication With Women During The Postpartum Period 1api-301056711Noch keine Bewertungen
- Social Science & Medicine: Qiong Wu, Tatjana Farley, Ming CuiDokument9 SeitenSocial Science & Medicine: Qiong Wu, Tatjana Farley, Ming CuiLaura Valentina Huertas SaavedraNoch keine Bewertungen
- Leche Materna, Lágrimas MaternasDokument7 SeitenLeche Materna, Lágrimas MaternasMaria Del GuercioNoch keine Bewertungen
- Artigo CapacitaçãoDokument14 SeitenArtigo CapacitaçãoKaren AraujoNoch keine Bewertungen
- First-time Mothers' Social Support, Self-Efficacy and Postnatal DepressionDokument10 SeitenFirst-time Mothers' Social Support, Self-Efficacy and Postnatal Depressionmotanul2Noch keine Bewertungen
- E Table of Contents. Postpartum Psychosis: The Role of Women's Health Care Providers and The Health Care SystemDokument15 SeitenE Table of Contents. Postpartum Psychosis: The Role of Women's Health Care Providers and The Health Care System4mdw25zqghNoch keine Bewertungen
- Web-Based Versus Home-Based Postnatal Psychoeducational Interventions For First-Time Mothers: A Randomised Controlled TrialDokument13 SeitenWeb-Based Versus Home-Based Postnatal Psychoeducational Interventions For First-Time Mothers: A Randomised Controlled Trialnur fadhilahNoch keine Bewertungen
- Postpartum Depression, Anxiety, and Stress PredictorsDokument8 SeitenPostpartum Depression, Anxiety, and Stress PredictorsKyze LQNoch keine Bewertungen
- Midwifery Dissertation Postnatal DepressionDokument8 SeitenMidwifery Dissertation Postnatal DepressionCollegePaperHelpCanada100% (1)
- 05 N091 30875Dokument25 Seiten05 N091 30875MayaciucuOfsixthesistersNoch keine Bewertungen
- 932-955 CH28 Lowdermilk - QXDDokument24 Seiten932-955 CH28 Lowdermilk - QXDnicoletagr2744Noch keine Bewertungen
- IndianJContNsgEdn17169-1808062 050120Dokument6 SeitenIndianJContNsgEdn17169-1808062 050120rmconvidhya sri2015Noch keine Bewertungen
- Family-Centered Maternity Care ApproachDokument4 SeitenFamily-Centered Maternity Care ApproachEga suryaniNoch keine Bewertungen
- RRL Adolescent MothersDokument3 SeitenRRL Adolescent MothersJoseph TamelinNoch keine Bewertungen
- Melly Nirma SyahrianiDokument9 SeitenMelly Nirma SyahrianimellyNoch keine Bewertungen
- Anxiety, Depression PregnancyDokument15 SeitenAnxiety, Depression PregnancyZakkiyatus ZainiyahNoch keine Bewertungen
- Postnatal DepressionDokument6 SeitenPostnatal DepressionWasemBhatNoch keine Bewertungen
- Perinatal Palliative Care: A Clinical GuideVon EverandPerinatal Palliative Care: A Clinical GuideErin M. Denney-KoelschNoch keine Bewertungen
- Psychopharmacology and Pregnancy: Treatment Efficacy, Risks, and GuidelinesVon EverandPsychopharmacology and Pregnancy: Treatment Efficacy, Risks, and GuidelinesNoch keine Bewertungen
- Wong Worksheet PediaDokument3 SeitenWong Worksheet PediaLecery Sophia WongNoch keine Bewertungen
- Wong - NCP Pneumonia RedoDokument5 SeitenWong - NCP Pneumonia RedoLecery Sophia WongNoch keine Bewertungen
- Pediatric CAP Diagnostic and Treatment ChallengesDokument2 SeitenPediatric CAP Diagnostic and Treatment ChallengesLecery Sophia WongNoch keine Bewertungen
- Wong - NCP Pneumonia RedoDokument5 SeitenWong - NCP Pneumonia RedoLecery Sophia WongNoch keine Bewertungen
- WONG, LECERY C. Significance of Studying LiDokument1 SeiteWONG, LECERY C. Significance of Studying LiLecery Sophia WongNoch keine Bewertungen
- Isbar Galanza PediaDokument1 SeiteIsbar Galanza PediaLecery Sophia WongNoch keine Bewertungen
- Post Partum Journal (Drnur)Dokument4 SeitenPost Partum Journal (Drnur)Lecery Sophia WongNoch keine Bewertungen
- Case Study ONLINEDokument2 SeitenCase Study ONLINELecery Sophia WongNoch keine Bewertungen
- Wong - NCP Pneumonia RedoDokument5 SeitenWong - NCP Pneumonia RedoLecery Sophia WongNoch keine Bewertungen
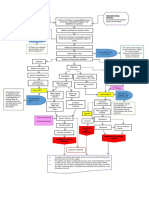
- WONG Concept MapDokument1 SeiteWONG Concept MapLecery Sophia WongNoch keine Bewertungen
- LSCW - Hand Out - Postpartum ComplicationsDokument2 SeitenLSCW - Hand Out - Postpartum ComplicationsLecery Sophia WongNoch keine Bewertungen
- WONG, LECERY C. Significance of Studying LiDokument1 SeiteWONG, LECERY C. Significance of Studying LiLecery Sophia WongNoch keine Bewertungen
- Wong CusDokument1 SeiteWong CusLecery Sophia WongNoch keine Bewertungen
- The Ten Commandments and Other Biblical PassagesDokument2 SeitenThe Ten Commandments and Other Biblical PassagesLecery Sophia WongNoch keine Bewertungen
- Wong - Activity Checklist Pediatric WardDokument2 SeitenWong - Activity Checklist Pediatric WardLecery Sophia WongNoch keine Bewertungen
- That May Used in Neurological Ward: Miguelito M. GultianoDokument32 SeitenThat May Used in Neurological Ward: Miguelito M. GultianoLecery Sophia WongNoch keine Bewertungen
- Etiologic Agent: Tuberculosis Is A Disease Caused by Mycobacterium Tuberculosis. Although TB IsDokument3 SeitenEtiologic Agent: Tuberculosis Is A Disease Caused by Mycobacterium Tuberculosis. Although TB IsLecery Sophia WongNoch keine Bewertungen
- 10 Reasons To Read The BibleDokument3 Seiten10 Reasons To Read The BibleLauren CarlosIINoch keine Bewertungen
- Wongl C - Act2-Respiratory-DisordersDokument2 SeitenWongl C - Act2-Respiratory-DisordersLecery Sophia WongNoch keine Bewertungen
- Promissory NoteDokument1 SeitePromissory NoteLecery Sophia WongNoch keine Bewertungen
- Wong, L.C. - Philippine Health SituationDokument1 SeiteWong, L.C. - Philippine Health SituationLecery Sophia WongNoch keine Bewertungen
- College Nursing Learning Contract GuideDokument2 SeitenCollege Nursing Learning Contract GuideLecery Sophia WongNoch keine Bewertungen
- Wong, Lecery Sophia C. Obward BSN 2-I1 Iii. Drug Study 1. Naproxen SodiumDokument3 SeitenWong, Lecery Sophia C. Obward BSN 2-I1 Iii. Drug Study 1. Naproxen SodiumLecery Sophia WongNoch keine Bewertungen
- Wong, L.C - Perioperative NursingDokument5 SeitenWong, L.C - Perioperative NursingLecery Sophia WongNoch keine Bewertungen
- Wong, Lecery Sophia C. Obward BSN 2-I1 Iii. Drug Study 1. Naproxen SodiumDokument3 SeitenWong, Lecery Sophia C. Obward BSN 2-I1 Iii. Drug Study 1. Naproxen SodiumLecery Sophia WongNoch keine Bewertungen
- Pediatric CAP Diagnostic and Treatment ChallengesDokument2 SeitenPediatric CAP Diagnostic and Treatment ChallengesLecery Sophia WongNoch keine Bewertungen
- WONG BrochureCovid 19Dokument2 SeitenWONG BrochureCovid 19Lecery Sophia WongNoch keine Bewertungen
- WONG TeachingCarePlanCOVID 19Dokument3 SeitenWONG TeachingCarePlanCOVID 19Lecery Sophia WongNoch keine Bewertungen
- WONG BrochureCovid 19Dokument2 SeitenWONG BrochureCovid 19Lecery Sophia WongNoch keine Bewertungen
- Pediatric CAP Diagnostic and Treatment ChallengesDokument2 SeitenPediatric CAP Diagnostic and Treatment ChallengesLecery Sophia WongNoch keine Bewertungen
- No Health Without Mental Health PDFDokument19 SeitenNo Health Without Mental Health PDFAmany IbrahimNoch keine Bewertungen
- Case StudyDokument2 SeitenCase StudydamecutebabeNoch keine Bewertungen
- Reference Note: Mental Health CareDokument17 SeitenReference Note: Mental Health CareRajeshwari IshuNoch keine Bewertungen
- Everest English School SQC TeamDokument13 SeitenEverest English School SQC TeamUmeshNoch keine Bewertungen
- Students List PG PH.D UG Nov 2021Dokument7 SeitenStudents List PG PH.D UG Nov 2021Ashwat ANoch keine Bewertungen
- Sacks, Oliver - 'The Lost Virtues of The Asylum'Dokument3 SeitenSacks, Oliver - 'The Lost Virtues of The Asylum'DylanOSullivan100% (1)
- Bereavement and GriefDokument28 SeitenBereavement and GriefGeorgiana PrisoschiNoch keine Bewertungen
- Attack of Nerves ReadworksDokument6 SeitenAttack of Nerves Readworkssalsa amiraNoch keine Bewertungen
- MR - Pheh Kai ShuenDokument3 SeitenMR - Pheh Kai Shuenகிரிஷா ShaliniNoch keine Bewertungen
- 04 - ADHD Diagnosis and Testing Guide - ADD Symptom EvaluationsDokument7 Seiten04 - ADHD Diagnosis and Testing Guide - ADD Symptom EvaluationstenahernanNoch keine Bewertungen
- Peace Corps Mental Health Treatment Summary Form TG-510-3 (Initial Approval 08/2012)Dokument5 SeitenPeace Corps Mental Health Treatment Summary Form TG-510-3 (Initial Approval 08/2012)Accessible Journal Media: Peace Corps DocumentsNoch keine Bewertungen
- Bipolar 2Dokument5 SeitenBipolar 2Kenny KenNoch keine Bewertungen
- Critical Reflection 1Dokument2 SeitenCritical Reflection 1MTCNoch keine Bewertungen
- Why Is Mental Health Important? Mental Health Is Important Because It AffectsDokument1 SeiteWhy Is Mental Health Important? Mental Health Is Important Because It AffectsJellina Joya RosgaNoch keine Bewertungen
- Antisocial Personality DisorderDokument11 SeitenAntisocial Personality Disorderapi-376421588% (8)
- Treatment For Eating DisordersDokument13 SeitenTreatment For Eating DisordersPsihoterapeut Alina VranăuNoch keine Bewertungen
- Psychosocial Rehabilitation Techniques for Mental HealthDokument11 SeitenPsychosocial Rehabilitation Techniques for Mental Healthrajasamuel100% (1)
- Qualities of A Clinical PsychologistDokument8 SeitenQualities of A Clinical Psychologistpsy22Noch keine Bewertungen
- Basic Counseling Skills For Addiction Professionals: Module 1-Training IntroductionDokument36 SeitenBasic Counseling Skills For Addiction Professionals: Module 1-Training IntroductionlissarlissaaNoch keine Bewertungen
- Sluggish Cognitive Tempo in Abnormal Child PsychologyDokument6 SeitenSluggish Cognitive Tempo in Abnormal Child PsychologyRasa ChomicieneNoch keine Bewertungen
- Martin Dahlen 2005Dokument12 SeitenMartin Dahlen 2005iulia_filNoch keine Bewertungen
- MRC-NADA Handout Ear Acupoints For Trauma Recovery-Finalv2Dokument2 SeitenMRC-NADA Handout Ear Acupoints For Trauma Recovery-Finalv2Omar MesbahiNoch keine Bewertungen
- NCPDokument3 SeitenNCPeun kyung shinNoch keine Bewertungen
- HHS Public AccessDokument16 SeitenHHS Public AccessLuis CsrNoch keine Bewertungen
- CamDokument2 SeitenCamkhadijah100% (2)
- AlcoholismDokument28 SeitenAlcoholismMonika JosephNoch keine Bewertungen
- New Bulletproof Confidence ReadyDokument28 SeitenNew Bulletproof Confidence ReadyRafael100% (2)
- Hub Hospitalisasi DG Tgkat Kecemasan OtDokument15 SeitenHub Hospitalisasi DG Tgkat Kecemasan OtyuniatiNoch keine Bewertungen
- NCP Inffective Individual CopingDokument1 SeiteNCP Inffective Individual CopingNatalie DulawanNoch keine Bewertungen
- Psychosocial ActivitiesDokument18 SeitenPsychosocial ActivitiesRyan Q. Blanco50% (2)