Beruflich Dokumente
Kultur Dokumente
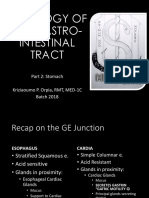
3.0 Grand Physiology Finals Compilation - Batch 2017
Hochgeladen von
Sheryl Layne Lao-SebrioOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
3.0 Grand Physiology Finals Compilation - Batch 2017
Hochgeladen von
Sheryl Layne Lao-SebrioCopyright:
Verfügbare Formate
GRAND PHYSIOLOGY B FINALS REVIEWER
Page 1 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
CARDIOVASCULAR PHYSIOLOGY 1 Remember this: MA SISI DSSD
MITRAL VALVE STENOSIS DIASTOLE
*Blood flow from the Heart* INCOMPETENCE SYSTOLE
AORTIC VALVE STENOSIS SYSTOLE
INCOMPETENCE DIASTOLE
Question: When is Mitral Stenosis murmur best heard?
Answer: Diastole
th
Question: You heard a murmur in the 5 ICS Mid Clavicular
Line during Systole, what kind of lesion is this? What valve is
affected? Incompetence @ Mitral valve
*Myocardial cells*
o Automatic
A. SA Node/ Node of Keith and Flack
Atria: Primer pumps
-found in junction of SVC and RA
Ventricle: Major pumps
-Primary pacemaker
Left ventricle is thicker
- highest frequency of AP generation
*Cardiac Valves*
B. AV Node/ Node of Kent and Tawara
Atrioventricular valve: -found in posterior R side of interatrial septum;
o Mitral- 2 cusps; (+) chordae tendinae for better Ventricular filling
o Tricuspid- 3 cusps; (+) chordae tendinae -small fiber diameter and few gap junctions
- most common site for heart block= Nodal zone
Semilunar Valves: of AV node
o Pulmonary- 3 cusps C. Purkinje system
o Aortic- 3 cusps -Fastest AP conduction
-large fiber diameter kase
#Chordae tendinae + Papillary muscle = prevent
overbulging of AV valves into atria
#Valve closure is due to pressure difference *SA NODE*
*Heart Sounds*
Phase 4/RMP
Less K channels are open
More Na leak channels open
Kaya RMP is less negative
Appointment from 2pm – 5pm Phase 0 (depo)
APTM Voltage gated Ca channels open
Aortic 2nd ics Right sternal border slowly (L type > T type)
nd
Pulmonic 2 ics left sternal border Ca and some Na Influx
Tricuspid 5th ics left sternal border Phase 1 2 3
th
Mitral= 5 ics MCL Ca influx K efflux= slow repo
st
AV valve closure= 1 heart sound; simultaneous Midway- Ca channel closes
K channels open continuously
nd
SL valve closure: 2 heart sound; simultaneous or not #Action potential= Ca Influx
; due to physiologic splitting s/t Inspiration - ,mauuna
mag close si Aortic valve
rd
3 heart sound= normal in children; Ventricular
gallop; due to rapid inflow of blood from Atria to
ventricle upon opening of the AV valve
4th heart sound=atrial gallop; due to atrial contraction
or systole
*Cardiac Valve Lesion*
Stenosis- narrowing = dec blow flow
Incompetence/Insufficiency= regurgitation or
backflow of blood
Murmurs- heart sound due to lesions
Page 2 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
*VENTRICULAR MUSCLE*
*Ion channels in Cardiac muscle membrane:
Ca enter T tubule Some binds with troponin C forming Ca-
Troponin complex= contraction;
Some binds with ryanodine receptors- activate Ca gated
channels, Ca moves out , some binds with troponin C forming
Phase 4(RMP) Ca-Troponin complex= contraction
High permeability to K
Slight permeability to Na O diba dami nyang source for calcium!
Phase 0 (depo)
Na influx Calcium pump para mag relax un muscle babalik na sa
Ca influx pinanggalin nya si calcium
Na channels close
Phase 1 #Cardiac Glycosides- Digitalis for HF
K channels open Inhibit Na-K pump para walang calcium pump para si
Phase 2 Calcium dun lang sa loob para stronger contraction
Plateu (Pla-2, phase 2 )
K efflux and Ca influx effect:
Membrane potential ain’t moving Positive Inotropy= Inc force of contraction
Phase 3 Negative Chronotropy- Dec HR
Ca channels close Negative Dromotropy- Dec Conduction
K channels remain open
#Ca influx is most important during plateu or Phase 2, ito un
responsible sa ST segment sa ECG
#Action Potential is d/t Na Influx mainly, secondary lang Ca
influx
#Absolute RP= Phase 0-2
#Relative RP= End of phase 2- Phase 4(RMP)
*Heart Block*
-Common sa AV Node, particularly sa Nodal Zone
1st degree
Incomplete heart block
PR interval > 0.20 sec
2nd degree
Incomplete heart block
Not all impulses are transmitted
P> QRS = P wave P wave QRS T P wave
3rd degree
Complete heart block
After 20 sec purkinje fibers take over
#Extra systole occurs only during: mid diastole and late
diastole
*Contractility properties of the heart:
#Involuntary; smaller muscle fiber
#intercalated disc- connects muscle fiber thru gap junctions
#exhibits functional syncitium
#fair amount of connective and elastic tissue
#more mitochondria and active capillaries
#Sarcoplasmic reticulum is less developed
#well developed Transverse tubular system
Page 3 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
CARDIOVASCULAR PHYSIOLOGY 2
Tips: Pakinggan ng paulit ulit yung Narration ng Cardiac Cycle.
Pag nagets nyo nayun, madali na lang
Atrial Systole
#Onset of Isovolumic Contraction= 1st heart sound= AV valve
-preceded by P wave
closure
-4th heart sound
#end of Isovolumic Contraction= Open Semilunar valve
-A wave (JVP curve) d/t inc atrial
#marks the beginning of Isovolumic Relaxation= Closure of
pressure d/t atrial systole
semilunar valves=2nd heart sound
#Onset of Ventricular filling= AV valves open
Isovolumic contraction
-C wave
AV valve Open= Atrial Pressure> Vent Pressure
- Av valve close; SL valve still close
AV valve Close= Vent Pressure> Atrial Pressure
-After onset of QRS SL valve Open= R Vent Pressure>10 mmHg
L Vent Pressure> 80mmHg
Rapid Ejection SL valve close= Aortic Pressure> Vent Pressure
*-Ventricular pressure > than Aortic
pressure * *Structure Innervated by Sympathetic Nerve
-atrial filling begins
1. SA node
Reduced Ejection 2. AV node
-T wave 3. Purkinje Conduction System
-atrial filling continuous 4. Atria
-Protodiastole 5. Ventricle
6.
Isovolumic Relaxation *Structure Innervated by Paraympathetic Nerve/Vagus
-Incisura/dicrotic notch
Av valve close; SL valve still close 1. SA node
-V wave (JVP curve) d/t inc atrial 2. AV node
pressure d/t inc atrial filling 3. Proximal bundle of his
4. Atrial muscle
5. Ventricular muscle- INDIRECT LANG!
Rapid Inflow #Why? Kasi diba parasympa, prolonged ang AV nodal
rd
-3 heart sound- open na kasi AV delay, so more filling sa ventricle, mas stretched ang
valve Ventricular wall, so increased ang Force of Ventricular
Diastasis contraction
-SL valve is close In short pag direct innervations ang tinatanong sa
-AV valve is open Parasympathetic NS, di kasama ang Ventricular
-75% Ventricular filling muscle!
Page 4 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
CARDIOVASCULAR PHYSIOLOGY 3 #dapat hindi Overstretched or Overdistended ang cardiac
muscle, prevented yan ng connective tissue sa heart.
Cardiodynamics
A. Heart Rate= Number of heart beats or
contraction per minute, N=60-100 (adult) Factors affecting cardiac muscle length=
o Stronger Atrial Contraction=
B. Cardiac Output=
- Diba may 25% pa sa atria, o di pag mas
-Vol/Amt/Quantity ejected by each ventricle
per MINUTE; SVxHR malakas yan mas madami pupunta sa
ventricle, mas distended ang heart, Inc EDV
mas malakas contraction, Dec ang ESV
C. Stroke volume=
-Vol/Amt/Quantity ejected by each ventricle o Inc Total Blood Volume
per CONTRACTION/CARDIAC CYCLE/ HEART BEAT - Strength in number! In this case,
amount/volume.
D. End Diastolic Volume(EDV)/Preload= o Inc Venous Tone
-Vol of blood in Ventricle after relaxation - Sustained contraction, hindi constriction!
- Sa peripheral BV to ah, so ibig sabihin ang
before contraction; vol of blood that will exert force
veins, partially contracted sila, veins are your
on ventricular wall. Ave= 110-130ml; ESV+SV
capacitance vessel diba, so kapag inc ang
venous tone decrease ang venous capacity,
# ito yung baon mo sa school, ito un motivation mo
sa pagpasok, mas malaki ang baon mas may force so Inc ang venous return and so on
o Inc Pumping of skeletal muscle
pumasok!
- You move= compress vein= open venous
valves= inc venous return and so on
#Intrinsic Factors= Force of ventricular contraction
o Inc negative intrathoracic Pressure
#Peripheral Factors= blood vol, venous return, arterial system
- Suction effect sa heart= heart dilate= more
blood= Inc EDV so on
EDV/Preload Factors:
F. Afterload
Venous return- Most important
- Pressure sa Aorta
-yung babalik sa heart mo; In short mas
madaming babalik na blood, mas malakas - This is different from ESV
yung contraction ng heart, inc CO - Pag ito increased di makakaflow yung blood
mula Left ventricle papuntang AORTA, so
Effective filling time- mas mahaba ang diastole, mas bababa ang CO
madaming filling, mas madaming blood sa Ventricles
mas malakas yung contraction ng heart, inc CO; 20-
CONCLUSION: ANG EDV/PRELOAD mo, maganda yan, pag
180 bpm ok pa ang filling pero pag >180 bpm na OA
na, din a kaya magcompensate, panget na. mataas yan, mataas din ang Cardiac output (CO) mo; ANG ESV
naman masama yan, kasi yan yung natitira sa heart, pag
Bpm= beats per minute/ (HR)
mataas yan ibig sabihin hindi maganda yung pag pump ng
heart mo, so mag dedecrease ang CO mo.
Effective Filling Pressure
-Difference of Central Venous Pressure (CVP)
Autonomics
& Intrathoracic Pressure (IP)
Sympathetic: Excitatory
CVP= Pressure sa RIGHT ATRIUM
Parasympathetic: Inhibitory, pero may indirect “excitatory”
IP= pressure outside heart.
If CVP>IP= Inc EDV effect sya sa Ventricle diba? Naalala mo pa un? Hindi na? sige
basahin mo ulit from the top.
Myocardial Compliance
-ability to distend d/t elastic tissue; change Sympathetic:
in volume should be greater than change in pressure Epi and Norepi binds with B1 receptor sa heart, ang
daming mangyayare daming sinasabe grrrr. Pero eto
E. End Systolic Volume (ESV) lang yan:
-Volume of blood remaining in ventricles
Phosphorylated and Ca channel= more Ca enters=
after contraction
INC FORCE OF CONTRACTION
N=45-50ml; SV-EDV
#tira ng baon mo, naks di naubos! Balik mo sa nanay
mo yan! Phosphorylate ang Trop I= Troponin tropomyosin will
cover active site of actin= RELAXATION
ESV Factors:
Myocardial Contraction= MOST IMPORTANT Phosphorylated or Inhibited ang phospholamban,
- Malamang, mas malakas contraction, mas yang phospholamban nayan, masama yan, kasi
konti matitira sa ventricle, so dec ang ESV iniinhibit nya ang Ca pump, so pag inhibited ang
phospholamban, magkakaron ng calcium pump, so
Frank Starling Law: Inc blood sa Ventricle, mas stretched ang babalik ang Ca sa Sarcoplasmic reticulum=
ventricle, Inc ang Contraction force RELAXATION
Factors
*End of autonomics
-EDV
Autonomics
Page 5 of 89 Frank starling’s law By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Heart Rate Point A
= Inc heart rate, Inc ang Ca influx, Inc force of - Opening of AV Valves
contraction
Point A to B
Factors that will regulate HR -Ventricular filling
1. Autonomic or neural- MOST IMPORTANT -P wave in ECG
-Sympa/ Para! - Inc Vol of blood in the ventricles
-Diastasis
rd
2. Hormones -3 heart sound
- Thyroid & Cortisol (inc)
3. Neuroreflexes Point B
a. Baroreceptor Chemoreceptor -Closure of AV Valves 1st heart sound
b. Bainbridge reflex-Inc blood return sa Atria= - ito na un amt ng EDV mo
stretched ang atria mo= stimulated ang
stretch receptors= SA node stimulation=Inc * para makuha ang SV/ Stroke volume, I minus mo un EDV sa
AP = Inc HR ESV mo.
4. Moderate to heavy exercise
5. Emotions Point B to C
6. Temperature, Inc= Inc HR -Period of isovolumic contraction
Yang HR ok lang na mataas yan, wag lang lalagpas ng 180 bpm - QRS complex
kase OA na un.
Point C
Yung mga nakalagay sa taas will either Increase or decrease o SL valve opens
your CO, depende sa anong state nila.
Point C to D
Other factors that will influence CO: o Period of Ejection and Dec volume of blood
in the ventricles
A. Ejection fraction- percentage ng EDV na naeject ng
Point D
ventricle or in short, Stroke volume; N=65-70% of
o Closure of Semilunar Valves dito na un sa
EDV ( measured via 2d echo)
ESV mo
B. Body surface are- more developed skeletal muscle
o 2nd heart sound
(athlete)= Inc CO
- physiologic splitting of 2nd heart sound
-Aortic pressure exceeds Ventricular pressure
With athletes pala, its okay to have Low HR, normal un.
Point D to A
C. Cardiac Reserve
Isovolumic relaxation
-Max amount ng CO na kayang I increase ng Heart
atrial filling is increasing
o Hypereffective- Increased eg. during Exercise
o Hypoeffective- weak heart eg. (+) Heart
Test of knowledge:
Failure
San imeameasure ang CVP?
EJECTION LOOP
Kelan maririnig ang murmur pag Insufficient ang Aortic valve?
Anong phase ng Cardiac cycle mas mataas ang Ventricular
pressure as compared to Aortic Pressure? E yung 3rd heart
sound? Yung 4th?
Paki Auscultate nga ang Pulmonic valve? E ang Apex? Sige
ngaaa saan?
San pinakamabilis ang conduction ng AP? Ano sagot mo? SA
node? WRONGGG!
HALFWAY THEREEEEE! SA CARDIO KA PALANG ANG HABA PA
GIRL. PUSH MO YAN!
Page 6 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
CARDIOVASCULAR PHYSIOLOGY 4 *BLOOD FLOW*
Vascular System Ohms Law- Change in Pressure/Resistance; so pag
A. Aorta mas mataas ang pressure gradient, mas maganda
-Largest ARTERYYY blood flow
-Highest presssureeeeee,
-Highest velocity of blood flow Poiseuilles- Resistance= Length x Viscocity x 8 / nr4;
-Inc Transmural pressure in short mas mahaba, mas malapot mas mataas
-More Elastin than Smooth muscle fiber, resistance, pero pag inc ang radius ng BV dec ang
-pag nag branch out= Arteries resistance
- Blood contained= Stress blood volume
#kaya ang arteriole, pag nagconstrict sya, sobrang liit
B. Venous system ng lumen nya diba, tapos nagconstrict pa, di wala ng
-Collecting blood vessel, CAPACITANCE VESSEL Blood nadaan na blood.
reservoir
-thinner wall Reynolds Number- tendency of blood to become
-Vena Cava= biggest radius turbulent
= lowest transmural pressure = Diameter x Velocity x density / viscosity
; Inc diameter density and velocity= turbulence inc;
C. Microcirculation pero pag Viscous and blood less turbulence, kasi
malapot masyado, so magiging mabagal ang blood
o Arterioles flow, like sa case ng polycythemia vera, kaya dec ang
-formed when arteries branch out Reynolds number.
- pinaka madaming smooth muscle, so sya
ang thickest ang muscular layer= #Types of blood flow
RESISTANCE VESSELS Laminar- Silent
Turbulent- Loud
o Capillaries Heart-Murmur
- No sympathetic innervations but responds to Blood vessel- Bruit
circulating vasoconstrictor <2000= laminar
- Smallest BV; largest Cross sectional area 2000-3000= transitional
- Thinnest >3000= turbulent
- No smooth muscle
- EXCHANGE VESSEL Venous return
- Amount of blood that will return to
o Venules heart ( okay. buti pa yung dugo
- BV that is in direct contact to tissues bumabalik sa puso, ikaw, anyare
sayo?)
Left side of Heart Aorta Arteries Arterioles
Metarterioles Venules Veins Right side of
Heart
La Place Equation:
Wall tension= Distending pressure x radius Inc total BV= Inc MCSFP= Inc Venous Return=Inc
of blood vessel CO
Inc Resistance and Vascular Capacity= Dec CO
#Prone to aneurysm ang ARTERIES kasi they have
high pressure and they must have high wall tension. Once wall Central Venous Pressure
tension is low and pressure is high = RUPTURE -Pressure in R atrium
- diba ang lahat ay dahil sa Pressure difference? Ibig
#tunica intima= site ng atherosclerotic plaque sabihin dapat ang CVP mo mababa (N=0 mmHG) para from
#Sympa adrenergic(norepinephrine)= venous circulation pupunta sya sa Right atrium.
Bind A1= Vasoconstriction (peripheral BV)
Bind Beta 2= Coronary Vasodilation ABP/ Arterial blood pressure
#Sympa Cholinergic(acetylcholine)= -force exerted by volume of blood on arterial wall.
Bind M3 M4= Vasodilation (peripheral BV) a. Systolic Pressure(SP)- highest during ventricular
#Smooth muscle (BV)= Ca binds to calmodulin, walang systole
troponin C dun! b. Diastolic Pressure (DP)- lowest during ventricular
#myosin dephosphorylation= Relaxation diastole
# LATCH BRIDGE MECHANISM- c. Pulse pressure= SP-DP
Inc tone ng Vascular wall -> Dec ang Vascular
capacity -> Dec capacity of BV to hold blood -> Inc venous #Kelan wide ang pulse pressure? Meaning malayo ang pagitan
returnnn ng Systolic at Diastolic pressure mo
#Biggest pressure drop= From Artery to arteriole Exercise- Sympathetic sa lahat (inc SP), pero dahil
#Lowest pressure= Vena Cava may heat production at inc metabolism= dec ang
peripheral resistance (dec DP)
Hyperthyroidism- same with exercise
Page 7 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Atherosclerosis- SP increase, pero walang Dec sa DP #kaya kapag may hypoproteinemia ka may edema ka
kasi walang nagpupull ng fluid mula interstitium mo pabalik ng
MAP or Mean Arterial Pressure Intravascular compartment
=DP x 2 + SP/3 or DP + 1/3 of Pulse Pressure
4. Interstitial Fluid Pressure or Interstitial Fluid Hydrostatic
ABP= CO x TPR (total periph resistance) Pressure (Pif)
Increased pag Inc ang blood volume, tapos ano - Force exerted by the volume of fluid in the
mangyayare pag increase ang Blood volume? Dapat interstitial space ; water pushing from Interstitium pabalik ng
alamonayan! So mag inc ang EDV/preload tapos alam mo na Intravascular compartment
talaga yan!!!
Which Favors movement of fluid from Intravascular to
TPR (total periph resistance)- main factor is Interstitial?
VASOCONSTRICTION -Interstitial Fluid Colloid Osmotic Pressure or
Interstitial Fluid Osmotic Pressure (Пif) and
Test of knowledge: Dahil tapos ka na sa CVS 4, pag may mali -Capillary Hydrostatic Pressure (Pc)
back to start hah!
Interstitial to Intravascular?
Ano pinaka importanteng factor sa EDV? E sa ESV? -Interstitial Fluid Pressure or Interstitial Fluid
Anong nga uli yung iniinhibit ng Cardiac Glycoside? Hydrostatic Pressure (Pif)
Anong pagkakaiba ni Latch bridge at Bainbridge bukod sa -Plasma Colloid Osmotic Pressure (Пp)
spelling at pronunciation?
Anong phase sa Ventricula Muscle AP may equal conductance
ng K at Ca?
Sino responsible sa AP ng SA node? E ng Ventricular muscle?
Ang pulse pressure ba ay ang pressure ng pulse?
CARDIOVASCULAR PHYSIOLOGY 5
Microcirculation
Left side of Heart Aorta Arteries Arterioles
Metarterioles Venules Veins Right side of *If the value is POSITIVE = Favors FILTRATION
Heart (occurring at the arterial end) fluid will move out
* If the value is NEGATIVE =Favors ABSORPTION (at
4 Forces Responsible for Filtration and Absorption to take the venous end) = fluid will move in
place =STARLING’S FORCES #Autoregulation
1. Capillary Hydrostatic Pressure (Pc) A.Active hyperemia- pag inc ang tissue
- force exerted by blood on capillary wall; in short metabolism-> inc oxygen consumption->
fluid pushing papuntang interstitium! Hypoxia-> vasodilation-> inc blood flow so ma wawash out
din un metabolites
Factors: B. Reactive Hyperemia- reaction pag may
A. Arteriolar Dilation- pag dilated ang arteriole inc occlusion sa BV; occlusion->Hypoxia->
ang CHP vasodilation-> inc blood flow so ma wawash out
B. Venoconstriction- Pooling of blood sa Capillary din un metabolites
so Inc ang CHP
C. Inc Venous pressure- diba ang flow dahil sa Myogenic Theory
pressure difference? O edi pag ganyan, din a When BP inc, blood flow should also inc, only applicable
maka flow un blood, so pooling uli sa Capillary so between BP of 75-175 mmHg
Inc uli CHP If BP decrease below 75 mmHg ↓ Blood Flow
D. Inc Arterial BP- pag ganyan Inc ang blood flow, If BP rises above 175 mmHg ↑ Blood flow
so madami din dugong pupunta sa Capillary, edi
inc ang CHP Vasoconstrictors: Vasodilators:
E. Increased Total blood volume (TBV)- paulit ulit na Norepi/ Epi Prostacyclin
to kung bakit hah! Alamonayan Endothelin Nitric Oxide
Angiotensin 2 Bradykinin
2. Interstitial Fluid Colloid Osmotic Pressure or Interstitial Vasopressin Histamine
Fluid Osmotic Pressure (Пif) Serotonin Inc K, Mg, CO2 & H+
- fluid pulling pabalik ng Interstitium Inc Calcium Acetylcholine
- not much of a problem unless sira capillary
membrane mo Mechanisms to Regulate BP
3. Plasma Colloid Osmotic Pressure (Пp) Neural Mechanisms
-force exerted by the presence of osmotically active 1. Provides Immediate BP regulation
substances in the plasma that will attract fluids a. Baroreceptor reflex- mechanical stimulus,
- fluid pulling pabalik ng Intravascular compartment i.e inc or dec in BP
Page 8 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
2 types of receptor
a.1 Carotid Sinus
- more sensitive, stimulated by either increase or 2. Mechanisms that provide intermediate BP
decrease in BP regulation
-Impulse Gen by CN IX or Glossopharyngel nerve, a. Stress relaxation mechanism
more accurately the Herring’s nerve
a.2 Aortic Sinus
- stimulated only by increase in BP
- Impulse Gen= CN X or Vagus
b. Capillary Fluid Shift
b. CNS System Ischemic Response
c. Renal Fluid Shift
Cushings Reaction, nangyayare to pag may
Brain tumor or pag inc ang CSF e yung fluid sa CNS.
c. Chemoreceptor reflex
- Stimulated by chemical stimulus, i.e dec O2
inc CO2, Dec pH or Inc H 3. Long term BP regulation (within several hours)
- Carotid and Aortic Receptors din
a. RAAS
Angiotensin 2:
Potent Vasoconstrictor = Inc Tpr-> Inc ABP
Stimulate adrenal gland to secrete Aldosterone-
so Na Reabsorption sa DCT-> Inc ang Blood Vol->
alamonayan
Stimulate Hypothalamus to secrete ADH -> so Na
Reabsorption sa DCT-> Inc ang Blood Vol->
alamonayan
Page 9 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
RAAS mechanism: ST segment elevation= Myocardial Ischemia
ST segment depression=Myocardial Infarction
#Bundle branch block= QRS> 0.10 secs; longer wider QRS
#Peak T waves= Hyperpataasemia (Inc K)
#Prolonged ST and QT interval= Hypocalcemia
#Cardiac Enlargement= Very tall R waves, Deep S waves
and QRS interval > 0.10 secs
#In cases of Orthostatic hypotension, ang mechanism na
nagwowork is yung BARORECEPTOR REFLEX
#
#Coronary Blood flow of the heart is BEST during
DIASTOLE, kasi hindi sya nacocompress unlike in systole
Neural Mechanisms in Regulating BP
Immediate Intermediate Long term
Baroreceptor Stress Relaxation RAAS
(angiotensin+
aldosterone)
CNS Ischemic Capillary fluid Aldosterone
Response shift
Chemoreceptor Renal Fluid Shift
Angiotensin
CARDIOVASCULAR PHYSIOLOGY 6
ECG
ECG WAVESSSSS
P wave- Atrial Depolarization; depolarization of
whole atrial muscle
Q wave= Interventricular Septum depo
R wave= Apical depolarization
S wave= Base depolarization
PR segment- AV nodal delay
PR interval- duration of atrial depo + AV nodal
delay
T wave- only represent part of Vent Repo; tells
duration of phase 3
QRS complex- Ventricular Depolarization-Phase 0
QT interval- Ventricular muscle Action potential
or Vent muscle Depo and Repo; electrical systole
of the heart
ST segment-after depo of ventricle; Phase 2
(remember Plateu?)
ST interval- Ventricular Repolarization; Phase 1-3
U wave- Uncommon; HypUUUUkalemia (dec K)
#J point- end of depo, start of repo, in isoeltric line #Most common Cardiac Vector= 59 degrees
#Left side- most common problem
Page 10 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
TEST OF KNOWLEDGE Bago sa last topic para either ma
stress ka or maging confident ka >:)
>Represents Ventricular Repo? T wave? ANONGGG T
WAVE?????
>paki explain ang frank starlings law!
> ano mas sensitive? Carotid o Aortic Bodies?
> San nag bibind ang Ca sa Smooth muscle?
> Saan galling si Renin?
>san makikita ang C wave? Ang V wave?
>Lead I + Lead III= ?? 4?? Anong 4???
> Formula ng MAP?
> Capacitance vessel?
> Differentiate SV vs CO
>other name for EDV?
> Pareho ba ang ESV sa Afterload?
>anong pinagsasasabe ni Ohm’s law? E ni Poiseuille? Pano
ito ipronounce?
> other term for Asystole? Nice to know lang to, dali
macurious ka I google mo!
#Einthoven’s Eq= Lead II= Lead I + Lead III
PAPASA KA! Power of Words, Power of Faith! PRAYERS
PRAYERS!!!!! GODBLESS SATING LAHAT!
Tatabihan kita pag natulog ka.
Page 11 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
BLOOD PHYSIOLOGY 1 2. Recipient is Rh Rhogam-
Functions of blood: Composition of negative and donor given within
Homeostasis blood is Rh positive 72 hours after
Respiratory 1. Plasma giving birth to
Nutritive 2. Formed Rh positive
Excretory elements baby
Endocrine a.RBC
Immunity b.WBC
c.Platelets
Red Cell production:
Embryo- Yolk sac Maturation
2nd trimester -Liver of RBC- need
spleen lymph nodes ang Vit B12
3rd trimester to 5 y/o- at Folic Acid,
Bone marrow pag wala
>20 y/o-Bone magkaka
marrow (flat bones) MEGALOBLA
STIC
ANEMIA
RBC Hypertonic -
-transport hgb which Crenate/shrink
carries O2
-120 days life span; 1% Isotonic- NR
replacement everyday;
destroyed in spleen Hypotonic-
Swell/burst
Sickle cell anemia- sickle
shaped RBC; abnormal beta
chain; causes hemolysis
and sickle cell crisis!
ANEMIA POLYCYTHEMIA VERA
Causes: Hemorrhage, IDA, Causes: Genetics, High
Aplastic anemia, Hemolysis, altitude
SCA etc
Normal Cardiac
Greater Cardiac Workload Workload
Rh Blood Group (1) magdedevelop si
mother ng Antibody,
Reactions Happen when: magdedevelop pa lang Major Reaction in cross matching:
1. Mother is Rh kaya yung first baby a. donor’s cell and recipient’s serum
Negative & Baby is safe pa , unless b. donor’s agglutinogen and recipient’s
Rh Positive nakagawa na sya ng agglutinin
(hemolytic disease antibody if kunwari
of the nasalinan sya ng Rh
newborn/Erythrobl Positive na blood(2).
astosis Fetalis)
Page 12 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
BLOOD PHYSIOLOGY 2 For Acquired or Adaptive Antigen Presenting cells
Complement System Immunity: AKA
Para ma activate si C1 Interleukin 2- tagasumbong/tagatawag
Innate Immunity = C3 need mo ng antigen Stimulate ng backer kay CD8 & CD4:
Acquired or Adaptive= C1 antibody complex diba? So Cytotoxic T cell Dendritic Cells
meaning dun nag sstart and Suppressor T Macrophage
C3b- Opsonization ang acquired immunity cell and T helper B-Lymphocyte
&phagocytosis cells
C3 naman, sa innate
C5B6789- Lysis immunity kasi diba, sa C3, Interleukin 4,5,6 -
papatayin nya agad, for stimulates B cell
C5a- chemotaxis opsonization agad, so stimulating factors
excited sya, kaya sa Innate
C3a C4a C5a- immunity sya, hindi nya IgG= Gadami (most IgA= Secretions eg
Activation of mast need ng Ag-Ab complex, abundant) ; Gamommy Colostrum from Breastmilk
cells and basophils carry nya na agad. (crosses placenta) ; Gronic
(chronic) infection, first to IgE= Ellergies (allergies)
Antibody appear sa 2nd or
subsequent infestation IgD= Dimaunawaan;
Constant portion= vAriable Portion= attaches to B lymphocytes
Activates the where Antigen IgM= Mauuna; Malaki;
Complement Attaches first to appear sa 1st or Most abundant to least
system initial infestation (order) : G A M D E
Cytokines
For Innate Immunity: Cell Mediated Immunity Humoral Immunity ( B)
Interleukin 12 – T helper cells= inactivated (T)
calls Natural Killer in AIDS Chimumea
cells Transplant
Suppressor T cells and T Rejection Chicken pox
Interferon y- helper Cells= REGULATORY TB Mumps
secreted by NK CELLS Tancer cells Measles
cells to activate (cancer)
macrophage CD4= helper T cells Tungi (fungi)
*yung 4 mukang H Tiruses (virus)
Interleukin 1 &
TNF- chemo CD8= Cytotoxic T cells
attractants, calls Active Natural= own Ab Passive Natural (maternal
neutrophils; Allergy Primary infections Ab)
secreted by Acute= IgE eg primary chicken Anti Rh antibodies
activated Chronic= CD8 pox IgG, IgA
macrophage Anti Rh antibodies Passive Artificial (Ab
Active Artificial= Injected Injectables)
Immunizations Anti Rh Ab
Rabies vaccine Ig Injectables
Tetanus toxoid Hep B
Antitetanus Serum
Active= Takes time pero Rabies Ab
pangmatagalan (true love) Antivenin
Passive= Mabilis, pero
pang madaliaan (fling)
Page 13 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
BLOOD PHYSIOLOGY 3
Blood Coagulation Rate Limiting Factor=
FORMATION OF PROTHORMBIN
ACTIVATING FACTOR= Activated
Factor 10 / 10a
Intravascular anticoagulants
Glycocalyx= smoothness property
Thrombomodulin=binds to thrombin
Thrombomodulin-Thrombin complex=
activates Protein C
Protein C= Inactivates Factor 5 and 8
Fibrin Fibers=Adsorbs thrombin
Antithrombin 3= block and inactivate
thrombin
Fibrin fibers and Antithrombin 3= strong
anticoagulants
Heparin= low concentration in blood.
Of little use alone
Antithrombin 3+ Heparin= POWERFUL
ANTICOAGULANT; inactivates factor
9a, 10a, 11a, 12a and thrombin
Needs Ca= Factor 2, 7, 9 & 10; guyton: all in intrinsic
pathway except factor 12 and 11
Needs K= Factor 2, 7, 9 & 10; protein C
Others key points:
Needs Phospholipids= Factor 10 and 2
Thrombostenin= clot retraction
Thrombin stimulates activation of Factors 5, 8 & 13
Intrinsic Pathway= Collagen contact, blood trauma ;Partial
Plasmin= Lysis of fibrin fibers, Factors 1,2, 5, 8
thromboplastin time(PTT); Heparin therapy
and 12 (antidote=Protamine Sulfate) (HPITT)
Extrinsic Pathway= trauma to vascular wall and tissue
Coagulation factor present in Intrinsic and Prothrombin time (PT); Coumadin (warfarin) therapy
Extrinsic= 4 / Calcium (samplex) (antidote= Vit K) (PWET)
Warfarin= opposes VCOR c1 (vit k epoxide reductase
Fibrinogen= naturally occurring anti coagulant complex 1)
VCOR c1= reduces back Vit K to functional form
t-PA meds like Streptokinase converts So Warfarin= No VCOR c1= No Vit K= No Coagulation
plasminogen to plasmin, it does not dissolve
clots. The PLASMIN dissolve clots.
Abruptio placenta= tissue factor source=
follows the extrinsic pathway
Page 14 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
RENAL PHYSIOLOGY I Constrict - Dec GCHP; kasi papunta pa lang yan ng
glomerulus, so kapag nagsara yan di di na nag flow
For Homeostasis un blood
State of equilibrium! Balance! Dilate - Inc GCHP, better blood flow
Maintenance of internal environment 8. Glomerulus
What is more important is what you excrete! Lesser in
High pressure capillary bed facilitating Filtration. High
what you take in.
pressure kasi un supply nya galing mismo sa
abdominal aorta (60-100 mmHg)
Lungs – H20, CO2
9. Efferent Arteriole
GIT – Undigested food, H20, meds, heavy metals,
Controls pressure in peritubular capillaries or Vasa
electrolytes, etc.
recta bec it can constrict or dilate. Can also affect
Skin – H20, electrolytes
GCHP
Constricts - Increase GCHP kasi onti magfflow un
KIDNEYS
blood palabas ng glomerulus, pero pag nagsuper
Main Role: Excretion of metabolic wastes and foreign
constrict na sya wala na talaga blood flow, ediba ang
chemical
blood may proteins, proteins imparts onctic pressure
Regulates H20, electrolytes, plasma osmolarity, arterial so magkakaron ng water pulling, so maooppose ang
pressure (RAAS), acid base balance, volume and
filtration, reabsorption ang mangyayare
composition of ECF
Dilates - Edi mas maganda blood flow so mas mag
For excretion, secretion and metabolism of hormones fflow un blood out of the glomerulus, edi dec GCHP
For gluconeogenesis 10. Peritubular Capillaries/Vasa recta
Endo functions: Give rise to venous drainage; give O2 and nutrients to
Erythropoietin - stimulates bone marrow to produce renal tubules; low pressure capillary- 13-15 mmHg
RBC 11. Interlobular Vein
Renin - secreted by granular cells or JG cells, targets 12. Arcuate Vein
Angiotensinogen from liver to be converted to 13. Interlobar Vein
Angiotensin 1 14. Segmental Vein
Vit D is activated in kidneys, for calcium absorption 15. Renal Vein
16. Vena Cava
HORMONES THAT TARGET KIDNEYS:
ADH/Vasopressin - produced in hypothalamus, released
by posterior pit or neurohophysis
Aldosterone - from the adrenal cortex, most potent
mineralocorticoid in the Zona Glomerulosa
ANP - from the atria
Calcitonin, PTH, Vit D - Calcium and phosphate metab
RENAL TUBULES:
RENAL CORTEX RENAL MEDULLA 1. Bowman's Capsule
ISOTONIC HYPERTONIC Mula glomerulus kung san ka nag filter ng blood,
yung ultrafiltrate mo mapupunta sa bowman's space
Composed of: Composed of:
2. PCT
Glomerulus Loop of Henle
Bowman's capsule Medullary Collecting Where majority of substances is reabsorbed and
secreted.
PCT Duct
Hula Exam Tip: Basta, kung di mo na alam kung san
DCT
Cortical Collecting duct na sesecrete or reabsorb, PCT na agad.
3. Loop of Henle
Renal Hilum - where renal artery enters and renal
Thin Descending Limb, Thick and Thin Ascending
vein exits
Limb
Nephron - Basic functional units of kidney;
4. DCT
Approximately 1 M per kidney
Where macula densa is, for Na tonicity sensor for
filtrate, hindi plasma! Filtrate!
CHARACTERISTICS OF KIDNEY: 5. Cortical Collecting Duct
Retroperitoneal, located around costovertebral angle; 6. Medullary Collecting Duct
weighs 150g, bean shaped
Cilia
BLOOD SUPPLY: - Encoded by cholecyteine 1 and 2
1. Abdominal Aorta
- Important for flow dependent K secretion
2. Renal artery
- Mechanoreceptors that detect tubular flow rate
3. Segmental arteries
- Chemosensors for calcium dependent pathways
4. Interlobar arteries
5. Arcuate arteries
JG APPARATUS
6. Interlobular arteries
7. Afferent Arteriole JG cells/Granular cells- elaborates renin & erythropoietin;
Contains JG or granular cells (renin and erythropoietin lines the afferent arteriole
production); part of JG apparatus Macula densa- Na Tonicity sensor
Can modify Glomerular capillary hydrostatic pressure Lacis /extraglomerular mesangial cells
Page 15 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
For elaboration of diff subs that will control renal RENAL BLOOD FLOW THROUGH VASA RECTA:
blood flow Receives <2% of total RBF, so hypoxemic incidents is
For supporting structure higher
A=J M=D || afferent=jg cells macula densa = DCT Flow is sluggish - majority of h2O filtered na sa
glomerulus so concentrated na un mapupunta sa efferent
2 TYPES OF NEPHRON: arteriole and so on so sluggish na kasi mas viscous na
Cortical Nephron Juxtamedullary
Nephron RBF = Parterial – Pvenous
BLOOD Peritubular Vasa Recta F = (Parterial – Pvenous) / Renal Vascular Resistance
SUPPLY capillary; better BP = SV x HR x TPR
perfused
TONICITY Isotonic - So filtrate Hypertonic - filtrate Increased P arterial = Inc flow
stays in the tubule, flows from tubules to Increased P venous = Dec flow syempre mas madami un
di pupunta sa medullary interstitium; babalik sa heart edi bababa un magfflow sa kidneys
interstitium so greater concentrating Increases resistance = Negative yan malamang, so bababa
capability kasi mas ang flow
mataas ang osmotic
potential AUTOREGULATION
7 CN is to 1 JN 1 JN is to 7 CN Controls amount of plasma being filtered!
BP of 80-160 mmHg arterial pressure is CONSTANT!
RENAL BLOOD FLOW: If <80mmHg= dec RBF and GFR syempre mahina un flow
Receives 20-25% or 1.1 L of cardiac output kasi diba may e
direct supply sya from Abdominal aorta If > 160mmHg= inc RBF and GFR, edi malakas, edi better
Normal Urine Output flow
Adult: 0.5-1 ml/kg/hr
Pedia: 1-2 ml/kg/hr E pag 130???? sige ngaaa!!!
Ave UO: 1,000 - 1,500 ml/day Better RBF 90 mmHg o 150 mmHg????
So mas prone sa dehydration ang pedia, pati din Constant within 80-160 mmHg padin kasi ang nagaadjust
oldies is si resistance, sina efferent at afferent, interlobar arteries,
so constrict dilate constrict dilate kaya within that range,
same pa din ang flow! AMAAAAZINGGG
Ohm's Law Pouseuilles Law
F = Δ P/R; Flow= Pressure R = 8lη/Πr4 TUBULOGLOMERULAR FEEDBACK MECHANISM:
gradient / Resistance GFR and RBF control when BP dec
Diba lahat naglalaro sa pressure Measure of resistance!!! So BP dec Mag dec din GFR kasi syempre mababa
gradient, tigan mo yan in a pressure dibaaa so less filtrate is produced, so dec filtrate
positive way, si resistance flow sa tubules, pag dec ang filtrate flow ibig sabihin mas
naman in a negative syempre mabagal un flow so mas mahaba un time for the filtrate na
resistance nga e. kakaunti to be reabsorbed sa tubules papuntang
Inc flow pag ⬆Pressure Inc resistance pag circulation, mag fflow flow tapos pupunta ng DCT Dec
gradient and/or ⬇ang mas mahaba ang Na conc sa DCT kasi nga nareabsorb mo na, madedetect
resistance vessel, mas viscous un ni Macula Densa, sstimulate nya si JG cells to produce
Dec flow pag ⬇Pressure ang blood at mas Renin RAAS activation Angiotensin 2 activated
gradient and/or ⬆ang maliit ang radius ng Inc BP and Efferent arteriole constricts Inc GFR
resistance vessel (constricted) Afferent arteriole dilates Inc GFR
RBF MEASUREMENT: MYOGENIC MECHANISM:
Direct Method Regulates pressure and RBF when BP inc
Tedious, invasive and impractical Inc BP Inc RBF and GFR initially Arterioles stretches
Indirect Method kasi Inc un circulating blood vol sa kidney Vasodilation
Utilizes Clearance principle- volume of plasma cleared Mech gated Ca channels activated Contraction
of a substance per unit time Reflex Afferent arteriole constriction Dec GCHP Dec
GFR
A. Get PAH clearance (infuse PAH to patient)
B. Get Urine sample and determine PAH conc OTHER MECHANISM:
C. Get Blood sample determine plasma conc of PAH High CHO or CHON diet
Inc glucose conc in blood – So need mo sya i filter
Clearance of plasma PAH actuates Renal plasma flow; it When CHO is reabsorbed , co transport mechanism
doesn’t enter the cell, it stays in the plasma happens, So Na is also reabsorbed So sa DCT,
PAH is filtered and secreted madedetect nanaman ni macula densa na dec un Na
RBF = RPF / (1 – Hct) conc ng filtrate nya - Activates tubuloglomerular
C = UV / P (Clearance= Urince conc x Urine vol / Plasma feedback, so afferent arteriole dilates and efferent
conc) arteriole constricts Inc GFR
High CHON intake All should be filtered so it again
Activates tubuloglomerular feedback - if efferent
Page 16 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
arteriole is severely constricted, blood flow to vasa FILTRATION BARRIER:
recta or peritubular capillaries will severely dec Bowman’s Epithelium
Ischemia Acute tubular necrosis (+) slit pores and podocytes
(+) Sialoglycoproteins
Sympathetic or Neural Innervation is not important in Basement Membrane
URINE FORMATION (+) proteins type 4 collagen, laminin, polyanionic
Blood vessels constricts -> dec RBF -> Dec Filtration -> proteoglycan entactin, heparan sulphate and
dec urine volume (inc urine osmolality) mas konti mas fibronectin
concentrated Lamina rara externa
Lamina densa
Severe sympa: Lamina rara interna
Oliguria= 300-500 ml/day of urine Capillary endothelium
Anuria- less than 50 ml/day of urine (+) fenestrated , Sialoglycoproteins
VASOCONSTRICTORS VASODILATORS
Angiotensin I & II Nitric Oxide 100x more permeable ang glomerulus dahil sa mga slit
pores, fenestrations, podocytes , yung mga plasma
Epinephrine Histamine
proteins or negative particles di makapenetrate kasi may
Norepinephrine Prostaglandin (PGE2, PGI2) mga proteins din un mismong filtration apparatus, so
Endothelin Bradykinins (Produce Nitric narerepel nya un mga plasma proteins, plus big size sila
Oxide) like un mga formed elements. Plus high GCHP pa sya kasi
Anesthetics Dopamine diba direct blood supply sa Abd Aorta.
Angiotensin Receptor Pyrogens: Interleukin, Bacterial
Blockers endo and exotoxin MESANGIAL CELLS:
ACE inhibitors antagonist Support structure within glomerulus
ANP BNP β antagonist Properties: contractility, phagocytosis
Produces matrix for support of basement membrane
No parasympathetic innervations Prostaglandin, and other important proteins
NSAID causes Renal Failure because it decreases the
production of prostaglandins necessary for vasodilation, Nakakapag regulate din sila ng RBF kasi may
so puro vasoconstriction Ischemia Renal failure! prostaglandin which has a vasodilating effect
RENAL PHYSIOLOGY II FILTERABILITY:
Glomerular Filtration Eg Na Glucose: F= 1.0 , meaning 100% is filtered, lahat
Tubular Reabsorption pumunta sa renal tubule for possible excretion, but still
subject for reabsorption
Tubular Secretion
Eg. Myoglobin: F=0.75, meaning only 75% is filtered
Highest to lowest filterability
1. Positively charged
2. Neutrally charged
3. Negatively charged
Mas maliit mas madali i filter
GIBBS DONNAN EFFECT:
Behavior of charged particles near a semi-permeable
membrane that sometimes fail to distribute evenly across
the two sides of the membrane. The usual cause is the
presence of a different charged substance that is unable to
pass through the membrane and thus creates an
uneven electrical charge.
Eg. Nagfilter ka, matitira sa plasma mo e si Albumin,
albumin is negatively charged, so kung may mga to be
filtered pa sa plasma dina sya makakadaan papuntang
tubules kasi un mga positively charged particles na ififilter
sana e kay albumin na naattract.
EFFECTIVE FILTERING PRESSURE:
Substance A- Filtered Only
Substance B- Filtered, Partly reabsorbed
Substance C - Filtered and Completely Reabsorbed
Substance D -Filtered, None Reabsorbed + Secretions
GLOMERULAR FILTRATION
Nonselective, as long as it is small and positively charged,
it is filtered indiscriminately
Page 17 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Glomerular Hydrostatic Pressure generated by the
pumping action of the heart, hydrostatic pressure so yung
blood ipupush nya palabas papuntang renal tubules
filtrate
Bowman’s Oncotic Pressure normally 0 in value because
proteins are not filtered. Oncotic, meaning water pulling
effect, so yung asa tubule na , hihigop sya ng water edi
dagdag filtrate
Bowman’s Hydrostatic Pressure due to the presence of
filtrate inside the Bowman’s space, so yung fluid sa filtrate
ipupush nya pabalik ng systemic circulation MECHANISM FOR REABSORPTION:
Glomerular Oncotic Pressure plasma proteins present in A. ACTIVE TRANSPORT - uses energy; uphill
the glomerulus, again ang proteins nagiimpart ng oncotic 1. Transport Maxima
pressure, so nag pupull yan ng water, so mula tubule Energy and carrier dependent
hihigopin ng plasma proteins yung water pabalik sakanya, How Glucose, amino acids, PO4, SO4, Vitamin C,
sa systemic circulation malate, lactate, aceto-acetate, βhydroxybutyrate
are handled.
FILTRATION COEFFICIENT: In DM patients, sobrang daming nafilter na
Permeability: glucose but since may certain amount lang na
Inc kayang i handle ang carriers mo, di nya
Permeability marereabsorb lahat kasi saturated na lahat, wala
Inc Kf Inc ng magbabalik sa ibang glucose kaya merong
GFR; so eh nag glucosuria.
thicken ang 2. Gradient Time Limitation
membrane, edi How Sodium and Bicarbonate are handled
mas mahirap Inc Gradient Inc Reabsorption
ipenetrate, dec ang Kf Dec GFR Oliguria Inc time of contact within epithelium Inc
Surface Area: Inc SA Inc Kf Inc GFR; so for example Reabsorption
partial nephrectomy, o edi mas konti un nephrons mo na Syempre pag mas matagal un filtrate mo sa
makakafilter Dec Kf Dec GFR epithelium mas may time mag reabsorb ng Na or
Mesangial Cell Activity: Vasodilating property via HCO3 yung tubular cells mo. Think of
prostaglandin Inc Kf Inc GFR tubuloglomerular feedback!
3. Pinocytosis
QUANTIFICATION OF GLOMERULAR FILTRATION: Cell drinking
Inulin – Gold How PROTEINS Amino Acids are handled
standard in
measuring GFR, B. PASSIVE TRANSPORT - no energy needed; downhill
it is only filtered How WATER, UREA and CHLORIDE are handled
plus almost
same sya with Quantification of Reabsorption:
normal GFR, but expensive and not readily available R= filtered – excreted
BUN (Blood Urea Nitrogen) – Filtered and reabsorbed so RX = (GFR x PX) – (UX x V)
it underestimates GFR If the filtered load > excretion rate, net reabsorption has
Creatinine – Filtered and Secreted so it is overestimated occurred
FILTRATION FRACTION: FACTORS AFFECTING TUBULAR REABSORPTION:
Flow rate – Inc Flow rate Dec Reabsorption
Osmotic pressure of the filtrate If Inc Osmotic P Dec
Reabsorption
Hormone influence
ADH (Inc Water absorption)
Aldosterone ( Inc Na reapbsorption)
Inc FF= Inc Plasma proteins. ANP( Dec Na reabsorption)
So yung plasma mo nafifilter sya, natitira un mga plasma Angiotensin II (Inc Na Reabsorption)
proteins, naiipon. PTH, (Inc Calcium Reabsorption; Dec PO4 reabsorption
Vit D (Inc Calcium and PO4 rebsorption)
Higher Inc FF sa Efferent arteriole kasi mas increased na Calcitonin (Dec Ca and PO4 Reabsorption)
yung oncotic pressure dun kasi nakadaan na ng
glomerulus
TUBULAR REABSORPTION
Selective, purpose is to bring back essential substances
into the body.
Page 18 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
2. LOH
Exposed in Hypertonic Medium
a. Thin Descending Limb
Water Reabsorption ONLY
PI – Fluid Pressure na magpupush pabalik sa systemic circ b. Thin Ascending Limb
ΠC – Oncotic or water pulling effect pabalik ulit ng systemic Passive reabsorption of Solutes ONLY; DILUTING
circ SEGMENT Diluted filtrate
PC – Fluid Pressure na magpupush mula capillary papuntang c. Thick Ascending Limb
interstitium Active reabsorption of Solutes ONLY; DILUTING
ΠI – Oncotic or water pulling effect pabalik ng interstitium SEGMENT Diluted filtrate
Since only water is reabsorbed in Thin Desc Limb
REABSORPTION: Inc filtrate conc= concentration gradient In thin
Powered by Pumps Asc Limb, NaCL is passively reabsorbed
Na-K Pump concentration gradient between your Claudin 16- tight junction; permits Mg or Ca passage
filtrate and your tubular cell Power for Secondary When Filtrate exits LOH: Hypotonic na yung Filtrate
pump Na from your filtrate goes into cell via kasi puro solute un nireabsorb mo sa ascending limb,
secondary pump transport substance X = every Na so halos puro water un matitira
that is pumped out, a Substance X is reabsorbed
For anion eg Chloride, it causes electrochemical Barters’ Syndrome & Na-K-Cl Symport Defect:
gradient powering passive transpo, so didikit lang sya K is not reabsorbed= Hypokalemia
kay Na since opposite attracts, sabay na silang Na is not reabsorbed= Hyponatremia Dec Circ volume
marereabsorb RAAS activation
Back Leak Aldosterone reabsorbs Na in exchange for H, HCO3 is left=
Commonly happens with Potassium Metabolic Alkalosis
Pabalik ng filtrate
Via paracellular route or in bet cells 3. DCT & CD
SEGMENTS OF NEPHRON:
1. PCT
a. Early DCT
Reabsorption of Solutes ONLY; DILUTING
SITE OF OBLIGATORY REABSORPTION SEGMENT
Reabsorbs 67% of filtered H2O, Na, Cl, K Fluid leaving this segment is then HYPOSMOTIC
Requires tons of Mitochondria b. Late DCT & CD
Commensurate Water reabsorption- amt of solute = FACULTATIVE REABSORPTION OF WATER
amt of water reabsorbed Influenced by ADH- aquaporin formation
Filtrate tonicity= ISOTONIC & ISOSMOTIC Without ADH= 8% H2O reabsorption
Solvent drag via paracellurar route- flowing water With ADH= 17% H2O reabsorption
drags along solutes, and since changes in Na Aldosterone- Inc Na-K pump, So Na is
reabsorption influences H2O and solute reabsorption , reabsorbed, K is excreted ;targets Principal and
pag dec ang Na conc sa filtrate dec reabsorption Intercalated cells
din yung ibang solutes K-H pump, K goes inside Intercallated cells, H is
excreted = alkalosis (hyperaldosteronism)
Renal Tubular Acidosis - Na-HCO3 transport defect,
no HCO3 reabsorption= acidosis Distal Renal Tubular Acidosis = Metab Acidosis,
Cystinuria - Amino acid transport defect= Hypokalemia, Hypercalciuria, nephrolithiasis
aminoaciduria Liddles Syndrome- Amiloride-Sensitive Na
Channels= Dec Na excretion Hypernatremia
Hypertension
Page 19 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
TUBULAR SECRETION GLOMERULOTUBULAR BALANCE:
Same with reabsorption but direction is different If there is Inc in Tubular load Inc GFR Inc filtrate
Any substance ↑ concentration to a greater extent than Counteracted by Inc in Reabsorption rate
does inulin is secreted Purpose:
Prevents overloading of distal segments with an ↑ GFR
MECHANISMS FOR TUBULAR SECRETION: Prevents large changes in fluid flow in the distal
Na-K pump concentration gradient Power for tubules brought about by:
Secondary pump (more often ANTIPORTS) So for every - Changes in arterial pressure
Na reabsorbed, substance X goes out into filtrate = every - Disturbances that would create problems in the
Na that is pumped out, a Substance X is secreted into the maintenance of Na and vol homeostasis
filtrate
TEST OF KNOWLEDGE
Active Secretion: Reabsorption of Amino Acid? PCT
Transport maxima Needs most Mitochondria? PCT
Carboxylic, sulfonic acids, hippurate, creatinine, Obligatory Reabsorption? PCT
penicillin, thiazide, glucoronides, urological contrast Facultative Reabsorption? PCT??? Nanaman! Mali!
Organic bases, guanidine, thiamine, choline, histamine Diluting Segments? 3 yan!
Gradient-time limited Specific Mechanism of Secretion ng H? K?
How H & K are handled Diff Glomerulotubular balance vs Myogenic Mech vs
Tubuloglomerular feedback
Passive Secretion: Reabsorption mechanism ng Urea? Creatinine? Glucose?
Diffusion trapping Inc BP GFR will??
Weak bases, quinine, quinacrine, procaine, Afferent arteriole Dilates GCHP will?
chloroquine, NH3 Efferent arteriole moderately constricts GCHP will?
Weak acids, salicylic acid, phenobarbital Asan si Macula densa? Si JG cells?
- Weak bases and acids are unionized, meaning no
charge, once filtered returns to ionized form RENAL PHYSIOLOGY III
(positive and negatively charged) if this
happens, they can no longer cross back into the REGULATION OF PLASMA AND WATER VOLUME
cell membrame, dun na sila forever, then KIDNEYS:
excreted Maintain plasma osmolality of 282 mOsm/L
Antidote for Aspirin poisoning = Sodium Bicarbonate Conserve fluid and excrete solute
(it follows the diffusion trapping mech) Normal urine osmolality= 50-1400 mOsm/L
50- diluted || 1400- concentrated
SEGMENTS OF NEPHRON: Normal Urine Specific gravity (measure of the
concentration of solutes in the urine)
1.002-1.400
1.002- diluted ||1.400- concentrated
Plasma specific gravity= 1
BLOOD:
5 Liters 3L plasma & 2L of formed elements
ADH
Synthesized within hypothalamus in the supraoptic nuclei
(mainly) and paraventricular nuclei
Posterior pituitary only functions as for storage and
release
For water reabsorption in Late DCT and CD (aquaporin
There is no secretion
synthesis)
in THIN DESCENDING LIMB;
Inc in urea transporters: UT-A1, UT-A3 || NKCC2
wala din nabanggit sa Thin
transporter || NaCl symporter|| ENaC Promotes solute
Ascending limb diba?? Di ko
reabsorption Water goes along
alam!
2 Stimuli
Sa late DCT at CD,
1% inc in plasma osmolality (more sensitive, day to
Aldosterone ulit gagalaw
day basis)
Inc Na-K pump
10% dec in BP and/or BV ( state of shock or
Principal cells =
haemorrhage)
Handles K (secretes K)
Intercalated cells =
Handles H (secretes H) Antero-Ventral portion of 3rd ventricle- (+) osmoreceptors
Indirectly detects plasma tonicity If Plasma tonicity
QUANTIFICATION OF SECRETION: inc Inc CFS (cerebrospinal fluid) tonicity
Osmoreceptors will shrink stimulates supraoptic and
If the filtered load <
paraventricular nuclei Posterior pituitary releases ADH
excretion rate, net secretion
Targets late DCT and CD H2O reabsorption
has occurred
Page 20 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Baroreceptor and cardiopulmonary receptors- BV and BP ADH MECHANISM:
detectors ADH attaches to V2 receptor activated coupled
Subfornical region and Organum vasculosum of lamina with G protein activating adenylyl cyclise Inc cAMP
terminals - Thirst regulator Protein kinase A activated Aquaporin 2
(Regulated by ADH) exocytosis into luminal side ng
membrane Water from luminal membrane will be
transferred to Circulatory system via AQP3&4 which
are always in the basolateral membrane = water is
then reabsorbed
So kapag walang ADH, wala si AQP2, so walang
channel mula luminal side pabalik ng circulatory
system= no H2O reabsorption
Syndrome of Nephrogenic Syndrome of
Inappropriate Antidiuretic Inappropriate Antidiuresis
Hormone (SIADH)
ADH Water V2 receptors
ADH H2O reabsorption Regulates plasma Retention= continuous AQP2
osmolality/tonicity Hypoosmotic body production even in the
Aldosterone Reabsorbs solute Commensurate water fluids (diluted) Absence of ADH, (+) water
reabsorption = Isotonic fluid is reabsorbed Regulates Hyperosmotic urine Retention=
volume (concentrated) Hypoosmotic body
fluids (diluted)
Hyperosmotic urine
(concentrated)
DI/DIABETES INSIPIDUS/DAMI IHI
CENTRAL DI NEPHROGENIC DI
⬇Neurophysin (shuttle of (+) ADH but no
ADH going to Posterior RECEEPTORS water is
Pituitary) =⬇ADH water then excreted instead =
is then excreted instead = Polyuria {Hypoosmotic
Polyuria {Hypoosmotic urine (diluted)}
urine (diluted)} Hyperosmotic body fluids
Hyperosmotic body fluids (concentrated)
(concentrated) Polydipsia
Polydipsia
Plasma Osmolality THIRST/UHAWWW
<280/282 mOsm/L ZERO ADH release Stimulated with a:
>280/282 mOsm/L INC ADH release 2-3% Inc in Plasma Osmolality
Blood Pressure/Volume 10-15% Dec in BP/BV
Zero change or Inc in BP/BV ZERO ADH Thirst threshold > Threshold for ADH secretion
release Thirst: 295 mOsm/kg H2O
Dec BP/BV INC ADH release ADH: 285 mOsm/kg H2O
Chronic Hypotension >270 mOsm/L INC Mas nauuna magsecrete ng ADH kesa sa feeling ng
ADH release UHAWW
Chronic Hypertension <290 mOsm/L ZERO
ADH release Angiotensin II Inc Thirst
>290 mOsm/L --> INC ADH release Pag uminom ka Stimulated ang Oropharyngeal &
Chronic meaning matagal na, normally UGIT receptors mo, kaya maski hindi pa sya naaabsorb
mag rerelease ka lang ng ADH pag ng GIT Dec Thirst agad
>280/282 mOsm/L ang plasma osmolality
mo, what happens in chronic Coke Story: Coke contains solute Solutes Inc plasma
hypo/hypertensive condition is osmolality Thirst threshold is reached again
“nasasanay”yung body mo na mataas or INOM PA!
mababa yung BP, so nag aadjust sya, kaya Alcohol Story: Alcohol contains happiness
sa chronic HYPOTENSION >270 mOsm/L Happiness Inc plasma osmolality Thirst threshold is
pa lang nagrerelease na sya ng ADH para reached again INOM PA! (After hell week?
makaconserve na agad sya ng water. In GAMEE!!!)
chronic Hypertension naman
magrerelease lang ng ADH pag >290 WATER REABSORPTION
mOsm/L pa, so matagal kasi in HPN PCT
patients sanay yung body nila na conc 67% of H2O is reabsorbed (OBLIGATORY REABSORPTION)
yung plasma.
Page 21 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
LOH: Descending Limb Counter current exchanger (U shape kasi)- this also
20% of H2O is reabsorbed minimizes solute wash out from medullary interstitium
LOH: Ascending Limb PS: Actually dami nanamang sinasabi ni Guyton pero
Solutes are reabsorbed NO H2O REABSORPTION basta, Si Vasa Recta Maintenance lang ng tonicity ng Renal
DCT Medulla, di sya nagcocontribute ng maski pisong mOsm.
H2O permeability is ADH-dependent (late dct) Inc Arterial Pressure Inc Renal Medullary blood flow
(FACULTATIVE REABSORPTION) Inc wash out of solutes sa Intersitium Dec ability of
CD urine to be concentrated
H2O permeability is ADH-dependent (FACULTATIVE
REABSORPTION) Absent ADH = Diluted Urine, syempre walang
Without ADH = 8% H2O reabsorption magrereabsorb ng water edi ilalabas mo na lang yung
With ADH = 17% H2O reabsorption water
Present ADH = Concentrated urine, narereabsorb kasi
OBLIGATORY URINE VOLUME: water pabalik ng systemic circ, edi konti lang ieexcrete
Minimal vol of urine that must be excreted mong water
Serves as a dissolving and suspension medium
Excretion: 600 mOsm/day INCREASE DECREASE INCREASE DECREASE:
Concentrating ability : 1200 mOsm/L (renal medulla Ganito, pag sa interstitium, pending for reabsorption yan
tonicity) ,yung vasa recta, ang role nya, ibalik yung ibang solute
600 mOsm/day is to be excreted divide it with 1200 mula interstitium pabalik ng systemic circ para i conserve;
mOsm/L pag asa tubules, yan un pending urine
0.5 L/day ( amount of fluid needed to remove 600 Renal medulla - hypertonic for concentration of urine
mOsm/day Dec solute loss in interstitium mas macoconcentrate ang
urine, dadami yung pending for reabsorption
HYPERTONIC RENAL MEDULLA:
Tonicity is 1,200-1,400 mOsm Inc length of LOH more solute is pumped into
NaCl- 600 (active transpo) interstitium Inc Osmotic Gradient Dec Solute loss in
Urea-600 (Recycling of Urea) medullary interstitium
Vasa Recta- only maintains tonicity Inc # of Juxtamedullary nephrons more solutes will
Absorbs water via Osmosis with action of ADH enter medullary interstitium Inc Osmotic Gradient
For Urine Concentration (DCT, CD) Dec Solute loss in medullary interstitium
With ADH Water is reabsorbed into the Interstitium Inc flow rate in LOH (vasodilation) Dec Osmotic
Vasa Recta (contains plasma proteins, imparts gradient Inc solute loss or solute wash off
oncotic pressure or water pulling effect) returns water Inc flow rate in vasa recta Dec Osmotic gradient Inc
back into circulation thereby concentrating urine solute loss or solute wash off in Medullary interstitium
Corticopapillary osmotic gradient- secondary to CC Remember, sa vasa recta 1-2% lang ng RBF meron sya
mechanism, urea recycling and vasa recta; this will at dahil dyan decrease ang solute loss sa interstitium
minimize solute loss in medullary interstitium Inc ADH vasoconstriction Dec RBF Dec GFR
filtrate is low filtrate flow slows down more time for
COUNTERCURRENT MECHANISM: NaCl reabsorption (gradient time limitation to) Inc
ANG DAMING SINASABI NI GUYTON. Pero ito lang yan: Osmotic gradient Decrease solute loss in Medullary
Maglalagay ka ng madaming solute sa medulla in excess interstitium
of water, in time, ma ttrap na lang dun yung mga solutes, Inc Urea more hypertonic ang medulla Inc osmotic
so mauulit ulit lang yung reabsorption ng NaCl by the gradient Dec Solute loss in Medullary interstitium
thick ascending limb, tapos meron pang continuous inflow
ulit ng new NaCl galing ng PCT So paikot ikot lang FREE WATER CLEARANCE:
hanggang sa ma reach nya ang 1,200-1400
UREA RECYCLING:
Mediated by ADH, diba nga ADH Inc urea transporters:
UT-A1, UT-A3.
Urea is permeable only in Medullary collecting duct and
due to conc gradient babalik sya ng Ascending limb basta
paikot ikot lang din yan.
Patients with protein malnutrition Dec urea production
Dec renal medullary tonicity Dec urine concentration
= Diluted urine
Estimates the ability to concentrate or dilute the urine
VASA RECTA:
Rate at which solute-free water is excreted= water lang
Medullary blood flow is low and sluggish= 1-2% lang ng
Free H2O
RBF ang meron sya, pero sufficient na yon, plus dahil dun,
Produced in the diluting segments of the kidney
minimized ang solute loss sa medullary interstitium para
- Thin and Thick Asc Limb & Early DCT
sakto lang yung ibabalik mo sa circulation since ang main
function nga ng kidney mo is to EXCRETE “wastes”
Page 22 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
+CH2O: -ADH Positive water clearance, nilabas mo will promote secretion of K or H
daw un water so ibig sabihin since nilabas mo ang water, Epinephrine, Stimulated by dec in ECF volume
wala kang ADH urine is diluted norepinephrine Inc NaCl and water reabsorption
-CH2O: +ADH Negative water clearance, wala kang RAAS will potentiate sympathetic
inilabas na tubig, ibigsabihn may ADH ka urine is effects
concentrated Cortisol Glucocorticoid produced by
0 CH2O: +loop diuretic use (furosemide) inhibited ang adrenal gland
NKCC2 in thick asc limb dec medullary tonicity Will have mineralocorticoid effect
medulla becomes isotonic water and solute stays in Inc Na Reabsorption
tubules urine is neither conc or diluted BUT When filtered load >
ADH - water conservation reabsorption rate Inc GFR
Diuretic - meds that promotes urination Dec Na Reabsorption
Redistribution to More solutes will be pumped into
WATER REABSORPTION: deeper renal tissue the interstitium Na
Reabsorption
Efferent Arteriole Dec Hydrostatic Pressure in
Constriction Peritubular capillaries Dec
NaCl and H2O backleak ( back
into tubular fluid) Inc Na and
H2O reabsorption
Increase Inc GFR Inc Filtered load
Glomerular plasma proteins accumulate and
Capillary imparts onctic pressure) water
Hydrostatic reabsorption
Pressure
ANTI-REABSORPTION:
ANP, BNP Produced in Atrium (ANP) and
Ventricles (BNP)
Will decrease NaCl and water
reabsorption in the collecting
REGULATION OF OSMOTIC EQULIBRIUM AND PLASMA ducts
IONIC BALANCE:
Decrease the total peripheral
PRO-REABSORPTION:
resistance
If ECF vol Dec RAAS decrease ADH secretion and ADH
Angiotensin II activation A II increases mediated water reabsorption
targets:
UROGUANYLIN, produced in GIT and kidneys
PCT: Inc NaCl reabsorption
GUANYLIN stimulated by high salt diet
Na-H antiport
Targets PCT to decrease NaK pump
Starling forces adjustment
and Na-H antiport Dec NaCl and
LOH, DCT, CD:Inc Na reabsorption
H2O reabsorption
Weak vasoconstrictor of afferent
Target your DCT and CD
arteriole and strong
decreasing now your ROMK which
vasoconstrictor of efferent
is a K channel dec K
arteriole Dec GFR
reabsorption
Mesangial cell contraction dec
surface area dec Kf Dec GFR DOPAMINE Stimulated by Inc in ECF volume
Aldosterone release Dec NaCl and water reabsorption
ADRENOMEDULLIN Produced by kidneys
ECF volume regulation via
Stimulated by CHF & long
Aldosterone commensurate water
standing HPN
reabsorption
Inc RBF Inc GFRDec NaCl &
Na reabsorption
H2O reabsorption
Na-Cl symport , Na-K pump,
ENaC, Sgk1, CAP1, prostatin URODILANTIN Produced by kidneys
LOH, DCT, CD: Inc NaCl Stimulated by Inc ECF vol & long
reabsorption standing HPN
DCT, CD: Inc K secretion decreases salt and water
Paracellular Cl reabsorption reabsorption
(sumama si Cl nung nireabsorb si
Na) ELECTROLYTES
Inc aldosterone release if (+) SODIUM Most abundant extracellular cation
hyperkalemia & RAAS Determines the ECF vol- along with
Dec aldosterone release if (+) anions (HCO3, Cl)
hypokalemia, ANP DCT and CT reabsorption is concerned
Will have glucocorticoid effect with acid-base balance
Page 23 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
high salt dietECF volume is Aldosterone also promotes water
increased Inc BP BV counteracted reabsorption flow rate dec by
by inc in excretion of NaCl virtue of gradient time limitation K
secretion goes down; so Net effect,
NA REABSORPTION constant or no change in K secretion
or excretion
Dec aldosterone release if (+)
hypokalemia, ANP
ADH Targets Principal cells Inc
Na uptake (hyponatremic effect) K
secretion
Pag pumasok kasi ang positive
ion (Na), dapat may lalabas din
na positive ion (K)
BUT, ADH also reabsorbs water
flow rate dec by virtue of gradient
time limitation K secretion goes
down; so Net effect, constant or no
change in K secretion or excretion
Inc flow rate K secretion Inc &
Depends on Na Availability; for every
PKD1&2 Ca conducting channel is
POTASSIUM K excreted, Na is reabsorbed
also activated Ca goes inside cell
Renal handling: filtered ; Reabsorbed
K channels activated K goes out
PCT: 67% LOH: 20% DCT,
CD:aldosterone dependent ||
Inc Na in filtrate Inc Na uptake
Secreted in DCT CD
pag may pumasok dapat may lalabas
Regulation of K excretion:
K goes out
Aldosterone targets Principal cells
Eg Dec Na in renal tubules K
secretion Dec Glucocorticoids Inc K secretion
and also Inc GFR and other traspo
Eg Inc H in renal tubultes
mech
Intercalated cells are targeted K
secretion Dec
Acidosis Intercalated cells rather Acidosis Dec K secretion;
loses H than K Intercalated cells rather loses H than
Excretion and secretion is Primary K; Plus there is Dec NaK pump so Na
regulated by Plasma K goes outside cellInc Na Excretion
aldosterone release H secretion
HYPOKALEMIC HYPERKALEMIC
EFFECT EFFECT Acute Chronic
Metabolic Metabolic
Epinephrine: β2 Epinephrine: Acidosis Acidosis
Stimulation = α stimulation
K uptake of cells = K release Na-K pump is Mag wowork na
Inhibited + Dec si aldosterone
Insulin- K uptake from cells, liver
of cells K mechanism
permeability Inc Na-K pump
Aldosterone- K
Dec K excretion and Inc K
uptake of cells &
permeability
K excretion
Inc K excretion
Metabolic Metabolic Aldosterone mechanism, matagal yan,
alkalosis Acidosis
remember? Kaya sa chronic pa sya
Respiratory Inc Plasma magkakaron ng Inc K excretion
alkalosis Osm Then again, in acute cases, Aldosterone
Cell lysis has no change in K excretion
Inc Exercise
Respiratory Acidosis: NO EFFECT
REGULATION OF K REABSORPTION
AND SECRETION:
(+) Hyperkalemia Inc K secretion
and this will also Inc Aldosterone and
will stimulates Principal cells to
Secrete K in DCT and CD || But
Page 24 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
CALCIUM If protein bound, not filtered pressure) IncH2O reabsorption, then via solvent drag,
Only Ionized is filtered solutes come along
Low excretion rate Balance nga e, so nangyayare to para my state ng balance,
PTH & Vit D Inc Ca reabsorption para maski Inc GFR mag Iinc din agad reabsorption rate
Calcitonin Dec Ca reabsorption para naman hindi lahat e iihi mo na
are reabsorbed through Claudin 16 in
ascending limb TUBULOGLOMERULAR FEEDBACK
PHOSPHATE Acts as buffers (Owmygad bakit may Renal blood flow and GFR are kept constant for as long
buffers nanaman, BIOCHEM???) arterial pressure range is within autoregulatory range.
PTH and Calcitonin Dec PO4
reabsorption What Specific/Immediate Segments are Impermeable to
Vit D Inc PO4 reabsorption water or has no ADH pakebells? O bakit 2 lang? 3 yan!
CHLORIDE Associated with Na and H2O Inc Osmotic gradient Solute loss is? Urine conc is?
handling, diba nga passively Claudin 16 transports?
reabsorbed lang sya along with Na Aldosterone effect in K secretion is?
and H2O
MAGNESIUM If protein bound, not filtered
All filtered are reabsorbed through RENAL PHYSIOLOGY IV
Claudin 16 in ascending limb
SULFATES BODY FLUIDS AND ACID-BASE BALANCE:
Actively transported
PS wala kasing list ng kung ano un
passively and actively
transported/reabsorbed, pero basta 3
lang yung Passively reabsorbed: Urea
Chloride at water.
AMMONIA Acid base balance
HYDROGEN ALL OF FILTERED HCO3 is
BICARBONATE REABSORBED
(+) Alkalosis counteracted by Dec
in HCO3 reabsorption Whatever goes In, must go out
(+) Acidosis counteracted by Inc in
Normally Intake=Output
HCO3 reabsorption
The lining epithelium of the skin prevents rapid
GLUCOSE evaporation of water, kaya in cases of burns Inc Fluid
loss Tx= Fluid administration
Glucose conc> renal threshold=
Sweat loss varies in temperature and physical activity
Glucosuria
Glucose conc< Tm = Glucosuria Fecal water loss Inc in cases of diarrhea
Di naman kasi parepareho ng # of
carriers ang nephron Body = 60% Water (42L)
AMINO ACIDS 2 Main compartments:
ICF 40% (28L) (K, PO4, CHON)
VITAMIN C Filtered, Reabsorbed and Excreted ECF 20% (14L) (Na, Cl, HCO3)
Inc Adrenal steroids and/or Inc Interstitialfluid 15% (11L)
Filtered load of Na Inc Vit C Plasma 5% (3L)
secretion Transcellular fluid CSF, peritoneal fluid etc
Tm=2 around 2L
UREA Filtered and reabsorbed (remember Body = 7% Blood (5L)
narerecycle lang yan) Plasma 60%
ADH dependent Formed Elements 40%
URIC ACID Actively Secreted
Tm=15 INDICATOR DILUTION PRINCIPLE
CREATINE Filtered and reabsorbed
No Tm
Essential source of energy of muscle
CREATININE Byproduct of creatine
Secreted actively
Tm 16
Allows one to measure the compartments in the body
3 criteria forindicator:
GLOMERULOTUBULAR BALANCE Disperses evenly
Filtered load = GFR x Na in filtrate Stays in the compartment
Inc GFR Inc filtered load Inc reabsorption of Na Not metabolized
and H2O .Why? Eg of Indicators
Inc GFR Inc filtered load Inc Filtration Fraction Tritium/Deuterium – heavy water will go to all
(plasma protein concentration that imparts oncotic compartments for total body water measurement
Page 25 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Inulin & Na Isotope ECF measurement MASKI AKO DI KO GETS TO. AT AYOKO ALAMIN.
Radiolabeled albumin Plasma measurement NAKAKAINIS BAKIT MAY MATH! GRRR
OSMOTIC PRESSURE
ICF- 5423; Interstitum-5423; Plasma-5443
Plasma has higher osmotic Pressure as compared to
ICF and Interstitium
OSMOTIC EQUILIBRIA BETWEEN ECF & ICF
Plasma and interstitial fluid volume; Determined by: Isosmotic - Same osmotic pressure or same osmotic
Hydrostatic pressure potential with plasma, not about concentration. Same
Colloid osmotic pressure ability to attract water
Extracellular and intracellular fluid volume; Determined by: Isotonic - Same solute concentration
Osmotic effect of solutes
Intracellular fluid is isotonic with the extracellular fluid HYPOTONIC ISOTONIC HYPERTONIC
0.3 NaCl NSS/ 0.9 NaCl D5NSS,D5LR
OSMOLES:
0.45 NaCL PLR D10W,D50-50
Total number of osmotically active particles in a D5 in 0.45 NaCl
solution
D5W - Isoosmotic. take into consideration that Glucose
1 osm = 1 mol = 6.02x1023 particles
enters the cell, therefore, when it does, it behaves as a
1 mOsm = 0.001 osm hypotonic solution. So Isoosmotic talaga sya, hindi isotonic.
OSMOLALITY:
High Osmotic Potential = Hypertonic Solution
Osm/kg of H2O
Low Osmotic Potential = Hypotonic Solution
More accurate
ADDING SOLUTIONS IN ECF
OSMOLARITY:
Hypotonic= Tonicity decreases Water enters the cell
Osm/L of H2O
Affected by temp ICF increases and ECF Increases too
Hypertonic= Tonicity Increases Cell shrinks ICF
OSMOTIC PRESSURE: decreases and ECF Increases
The pressure required to oppose osmosis Isotonic=Tonicity is the same ECF Increases, ICF the
Indirectly measures H2O and solute concentrations same
parang ability to make the water stay ganun
Inc osmotic Pressure Inc solute conc GLUCOSE AND AMINO ACIDS:
Inc osmotically active molecules Inc Osmotic Ineffective osmoles because they enter the cell
pressure Adjusted to isotonicity; admin slowly
Size doesn’t matter. Number of ion does!!!
In case of shock Give Isotonic solutions Inc ECF
compartment Inc circulating blood volume
VAN’T HOFF’S LAW Pag D5W Imemetabolize lang ng cell yung glucose
Ineffective for shock
HYPONATREMIA HYPERNATREMIA
Dec NaCl due to Inc NaCl
hypoosmotic dehyreation Dec H2O
caused by
Electrolyte, H2O loss Hyperosmotic dehydration
Used in measuring osmotic pressure Diarrhea, vomiting caused by:
But, take into account the Osmotic coefficient or the Diuretics DI
correction factor, remember Na is a cation Cl is an anion, Addison’s Disease Excessive sweating
they are attracted to each other (aww sweet), therefore,
not all may dissociate. (di daw lahat maghihiwalay, kaya Inc H2O due to hypoosmotic Hyperosmotic
asa ka pa) overhydration caused by overhydration caused by:
For NaCl, there is a 0.93 Correction factor only 93% Conn’s syndrome
dissociated (93% chance daw para maghiwalay! Mygad!) SIADH (Dilutional Hyperaldosteronism
Hyponatremia)
EDEMA
Swelling caused by fluid retention
A. INTRACELLULAR EDEMA
Dec metabolism
Dec nutrition Dec ion pump activity
- Na-K pump is inhibited Na stays inside
water follows
Inc osmosis- Increase ability to attract water
Page 26 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Inflammation- Increase membrane permeability
II. INCREASED LYMPH FLOW 10-50x
CVA/Stroke Dec blood supply going to brain Increased Filtered fluid Inc interstitial hydrostatic
NaK pump is inhibited Na stays inside water pressure (edi mapupush yung fluid papalabas ng
follows Brain swells Inc ICP interstitium) + Increase lymph flow ( inc yung
drainage ng fluids papuntang plasma) No edema
B. EXTRACELLULAR EDEMA
Inc fluid in the interstitial space due to III. WASHDOWN OF INTERSTITIAL FLUID CHON
Plasma leakage- tagas, punta un fluid sa Lymphatics are permeable to CHON sasama yung
interstitium interstititium CHON sa lymph flow babalik ng
Failure of the lymphatic drainage- di nya plasma = no edema
mababalik un excess fluid pabalik ng systemic
circ Low compliance of the interstitium 3mmHg
Increased lymph flow 10-50x 7mmHg
Washdown of interstitial fluid CHON 7mmHg
Total 17mmHg
For Edema to occur Capillary Hydrostatic Pressure should
exceed 17mmHg
TRANSCELLULAR COMPARTMENT
Specialized compartments in the body
STARLING FORCES:
Capillary Hydrostatic Pressure - Fluid na napupush
paputang Interstitium
Capillary Oncotic Pressure - Andyan kasi un plasma
proteins diba, kaya pag meron kang hypoalbuminemia,
walang magi impart ng water pulling effect pabalik ng
plasma
Hindi kasama si interstitial oncotic pressure kasi normally
walang protein sa interstitium
SAFETY FACTORS THAT PREVENT EDEMA
I. LOW COMPLIANCE OF THE INTERSTITIUM: Fluids to prevent friction during movement
A. Negative Pressure Fluid exchange bet capillaries and potential spaces
-3mmHg, so may vacuum effect or sucking effect Eg synovial, pericardial, peritoneal, pleural fluid and etc
12L of fluid, pag nag exceed pa dyan, mag sspill
Drained by lymphatics
out lang pabalik ng plasma kasi nga may vacuum
effect
C = V/P ACID BASE BALANCE
Pag sinabi kasing Increase compliance, kahit
madami kang ilagay na fluid, yung pressure mo
konti lang yung change para mas maccomodate
nya un fluid. Pero, sa Interstitium mo, pag
dinagdagan mo pa ng fluid yan, mag increase
agad ng mataas yung Pressure mo. Pag tumaas
yung pressure mo ilalabas nya din lang agad
yung excess fluid. Kaya maganda pa gang
compliance mo is low.
B. Interstitial Gel HYDROGEN ION:
Para syang barrier so prevented ang flow ng Determines body pH ( Normal pH= 7.35-7.45)
water; plus nagiimpart sya ng elasticity and
compact brush pile. Urine pH is affected by diet or intake, it can be alkaline in
C. Proteoglycan and Collagen Filaments pH but is usually acidic.
Spacers; parang tulay, pero modulated ang flow
ng water, more on metabolites at nutrients yung CONTROLLING H
pinapadaan nya. Buffers - Substances that can reversibly bind to H; pang
maintain ng pH parang ganun!
Pag ang pressure mo nag 0 or higher No more vacuum
effect magi increase ang compliance mo, so maski Chemical Respiratory Renal
madaming malagay na water, maliit lang yung change sa Buffer system System
pressure, so hindi maibabalik un water sa plasma Onset Instantaneous 3-15mins Hours-days
Edema Handles Acids and Volatile Non Volatile
Brush piles pulled apart, dec ang gel formation increase bases acids (CO2; acids and
spacers Edema H2CO3) ECF bases
Page 27 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Power 1 1-2x greater Most To reabsorb bicarbonate, H+ is needed. To generate a new
important bicarbonate, H+ will combine to non-bicarbonate buffers.
A. Chemical Buffers P.S. Ayoko ng buffers. Ayoko ng kahit anong bahid ng
Intracellular CHON biochem. Physio na nga may biochem pa, dibaaa! Pero wag
Hgb- remember the hgb dissociation curve. Pag nayan! Last shifting naman din naman tinanong ni doc kung
Inc H/Dec pH release oxygen anong blab la bla ang mangyayari sa blab la bla diba? CHOOSE
Pag dec ang H/Inc pH mas rigid ang Hgb so mas YOUR BATTLES ika nga.
maghohold sya ng oxygen
Extracellular Buffers QUANTIFYING ACID-BASE EXCRETION
HCO3 buffer system- MOST important ECF buffer; Bicarbonate Excretion
Urine flow rate X concentration of bicarbonate in the
Henderson-Hasselbach equation- computes for blood urine
pH given a conc of HCO3 and CO2 Measures the removal of bicarbonate from the blood
PO4 buffer system – not that important ECF or the addition of H+ in the blood
buffer but, it plays a major role in Buffering renal Ammonium Excretion
tubular fluid (DCT, CT Intercalated cell) and ICF Urine flow rate X concentration of ammonia in the
(yes ICF din sabi ni Guyton); Bicarbonate buffer urine
system is reabsorbed while the phosphate buffer Measures the amount of new bicarbonate added into
is not reabsorbed so it bears the burden of the blood
controlling pH within the tubules. Titratable Acids
Non-bicarbonate and non-ammonium buffer excreted
Isohydric principle- Any condition that changes the like the phosphate, citrate, urate buffers
balance of one system also changes the balance of Measured via titration via NaOH. (amount of H+
the others, meaning pa gang H mo nag iba ng present)
concentration, lahat ng system mo mag aadjust
B. Respiratory Buffers
Control CO2 and carbonic acid
Hypoventillate- more CO2 stays, respi acidosis
REGULATORY MECHANISM
Hyperventillate- more CO2 goes out, respi alkalosis
PRO ACID: HCO4 (Othocarbonic acid) , H, NH4, Titratable
acid
C. Renal Buffers
PRO ALKA: HCO3
Excretes acidic or basic urine
Acid-base balance
ALKALOSIS ACIDOSIS
Secretion of H ions
HCO3>H / Excess HCO3 H>HCO3 / Excess H
Reabsorption of HCO3
WHAT TO DO? WHAT TO DO?
Generation of new HCO3
Excrete HCO3– Sobra pala Excrete H – Sobra pala e!
Secretion of H Ions: e! Edi ilabas mo! Edi ilabas mo! Acidic
Via Na-H counter transport Alkaline Urine Urine
In DCT, CT Intercalated cell Dec H Secretion- Need mo Reabsorb HCO3- Dali para
To reabsorb HCO3, H is secreted yan e! bumalik sa systemic circ!
NH4 & Titratable acid is Generate new HCO3 –
If walang H, Na HCO3 goes out in urine
not excreted – Wag mong Bicarbonate paaa!
DCT, CT Intercalated cell: Aldosterone Effect
tanggalin, need mo nga Excrete Ammonia (NH4) –
Hyperaldosteronism alkalosis; kasi H is
yan eee! Ilabas ang alak! Ay
spilled out
No Generation of New ammonia pala!
Stimuli for secretion of H ions :
HCO3 – sumosobra ka na Mag Hyperventillate-
Inc PCO2-respi acidosis hah! Ilabas ang feelings, uh I
Dec extracellular pH
Hypoventillate-kimkimin mean acid (CO2)!
Excess aldosterone ang sama ng loob (CO2)
Inc loss of H, NH4, titratable acids
Inc HCO3 ABG INTERPRETATION
BABALA: GANITO KO SYA NAALALA HAH, PWEDENG MALI
Reabsorption of HCO3: AKO, PWEDE DING TAMA.
85% PCT; 10% Thick Asc Limb; 4.9% DCT&CD
Normal Value Alka Acid
Generation of New HCO3:
Blood pH 7.35-7.45 >7.45 <7.35
Hydrogen Ion Secretion (e makakagawa ka daw
e!) PCO2 (RESPI) 35-45 mmHg <35 >45
Phosphate buffer HCO3 (METAB) 22-26 >26 <22
Ammonia, Urate, citrate buffer
Glutamine metabolism Step 1: Blood pH Check if Acidic o Alkaline
Page 28 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Step 2: Pick a partner bet PCO2 or HCO3; dapat pareho sila
hah! Kung Sino ang partner or kung sino mas malala, sya ang
MAIN problem, yung mga kabit, pang compensate lang.
Step 3: Idamay ang kabit!
Eg#1
Step 1: Blood pH is Acidic
Step 2: HCO3 is Acidic; PCO2 is Acidic, Sino mas malala? HCO3!
So Metabolic Acidosis Tx: Treat the cause or the primary problem
Step 3: Anyare kay PCO2? Ganito, since nagaway si Blood pH at For Alkalosis Ammonium chloride, lysine
HCO3, affected si PCO2, e CO2 is acid diba. monohydrochloride (more common)
Ans= Metabolic Acidosis with Respi component For Acidosis Safest are Sodium lactate and Sodium
gluconate, pero pwede din Sodium Bicarbonate
Eg#2
MICTURITION
Conscious and unconscious action
Micturition reflex autonomic spinal cord reflex, can be
inhibited or facilitated by centers in the cerebral cortex or
brain stem
Pelvic nerves via Sacral Plexus (S2 S3 as Center)
Yung sa compensatory ek ek, nung nursing days kasi
Principal nerve supply of bladder Both sensory nerve fiber
namin, ganito
and motor nerve fiber;
Compensation pH HCO3 PCO2
Sensory fibers- detect stretch in bladder wall; Stretch
Fully NORMAL Abn Abn signals in the posterior urethra initiates reflexes that
Compensated causes bladder emptying
Partially Abn Abn Abn Motor fibers- Parasympathetic fibers that innervates
Compensated the detrusor muscle
Uncompensated Abn Abn Normal Skeletal muscle fibers transmitted through Pudendal
Uncompensated Abn Normal Abn nerves to the external bladder sphincter – Somatic nerve
fibers that can voluntary control the ext sphincter
How I Understand It: Hypogastric nerves (L2) – For fullness sensation and pain
Pag fully compensated ata, yung parang example sa taas, Urinary bladder (+) Stretch receptors when stimulated
yung may Chronic Respi acidosis; Chronic na kasi e, so si and stretched Sends impulse to Afferent nerve: Pelvic
blood pH mo, nagnormalize na, din a sya nag adjust nerves S2 S3 ( Sensory) Motor fibers S2 S3
Pag Partial naman yung sa Metabolic Acidosis with Respi contraction of detrusor muscle and relaxation of internal
component; component meaning, dumagdag lang, urethral sphincter signals pass through pudendal nerves
nagcomplicate lang. to the external sphincter to inhibit it; Impulse will be sent
Pag Uncompensated naman, sa Acute cases, kunwari, to pons and cerebral cortex to see if voiding is convenient,
Acute Metabolic Acidosis. Acute kasi diba, bago lang, wala if it is (+) voluntary contraction of abdominal muscle
pang complication plus nagaadjust pa yung blood pH. Inc Pressure in bladder extra urine enters bladder neck
Inuulit ko. Pwedeng mali ako. Pwede ding tama. Wag nyo and posterior urethra Stimulates sretch receptors
ko awayin micturition reflex is excited and external urethral sphincter
is inhibited urination
ANION GAP
Cation # = Anion # Samplex: If you transect L3 Diba si L2 mo ang
responsible for sympathetic innervations mo, for fullness
(+) Metabolic Acidosis HCO3 Decreases, Na & Cl stays
and pain sensation, o edi di na magfflow yung impulse
the same Anion gap increases; In cases when anion gap
is normal, check for other unmeasured anions (PO4, SO4 dyan, Puno na yung bladder mo di mo pa alam
etc) INCONTINENCE (involuntary urination)
-oh, wag ka na magrerenal failure ulit ha
Kaya mo yan! Ikaw pa
Page 29 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Sex Tests
SEX DETERMINATION AND DIFFERENTIATION 1. Sex Chromatin Test
Test that detects the presence of Barr bodies
First discovered by Barr and Bertram the presence of sex
chromosome body AKA Barr Body in female somatic
cells
Individual has 1 X in excess of 1, so 2 X meron sya (+)
Barr Body Positive Sex Chromatin Genetic Female
3 Specimens used
Buccal Blood Vaginal
Scrape from the inner
cheek
Barr Body Appears as Barr Body Appears
darkly-staining like a drumstick in
bodies attached to human female
Oogenesis and Spermatogenesis nuclear membrane Leukocyte, in its
nucleus
Oogenesis Spermatogenesis (+) Barr Body in 20 (+) Barr Body in 1-5
Autosomal 44 44 out of 100 cells out of 300
Chromosomes Positive Female Neutrophils
Sex XX XY Positive=Female
Chromosomes (+) Barr Body in 0-4
After Several Mitotic divisions and 2 Meiotic divisions... cells out of 100
Negative= Male
Autosomal 22 22 Possible to have false Frequency of HIGHEST POSITIVITY
Chromosomes positive results bec Distribution of PMN bec of the direct
Sex X X or Y there are many Drumstick: effects of estrogen in
Chromosomes chromatin materials > 1-5/300 the epithelium
in nucleus > 2-3/1000
>3. 6/500
Establishment of Genetic Sex at Fertilization
Summary of Chromosomal Abnormalities in Man
Genetic Sex/Gender/Sex
Established at fertilization
YOU CAN ONLY HAVE ONE OF TWO SEXES, NOTHING
IN BETWEEN (Yes, wala daw mga Bi )
Genetic Female = XX
Fertilization= Sperm cell carrying X chromosome fertilizes
ovum (carries X, ALWAYS) 22 pairs of autosomal
chromosome and XX sex chromosome
Non-fused labia with small clitoris
Urogenital Sinus is open
Genetic Male = XY
Fertilization= Sperm cell carrying Y chromosome fertilizes Remember mag aappear lang ang Barr bodies pag 2 ang X sex
ovum (carries X, ALWAYS) 22 pairs of autosomal chromosome nya eg. Normal Genetic female, Klinefelter’s ,
chromosome and XY sex chromosome Female Mongoloid and Superfemale
Fused scrotal sac with penis or phallus
Super Female
Urogenital sinus is closed
44 autosomal chromosome and 3 Sex chromosomes:
External Genetalia XXX= 47 in total
Basis for determining sex at birth Klinefelter’s
Problem arises when Genitalia is Ambiguous (hard to 44 autosomal chromosomes and 3 Sex chromosomes:
determine) XXY=47 in total
It’s a male, since there is Y but then again, Sex
Chromatin is positive or (+) Barr bodies bec of 2 X sex
chromosome
Turner’s syndrome
44 autosomal chromosome and 1 Sex chromosome: X0=
Phallus is too big to be considered as clitoris 45 in total
Labioscrotal swelling looks like labia majora Negative Sex Chromatin test since 1 lang X
There is incomplete fusion of urogenital sinus
In cases of Ambiguity Defer signing of Birth cert Mongoloids/ (+) Down Syndrome/ Trisomy 21
Determine genetic sex, do Sex Test NO PROBLEM IN SEX CHROMOSOME, problem is in
Autosomal chromosomes
Page 30 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
CalvinKlein Kleinfelters Develops in male Karyotypes:
Tina Turner Turner’s syndrome Develops in female
Remember: when a sperm or ovum matures, meaning they have
nd
undergone 2 meiotic division only 1 sex chromosome shall
remain, either X or Y in male and only X in female.
Normally
Sperm cell carries 1 X sex chromosome and it fertilizes
an ovum with of course, as always, carrying 1 X sex SEX DIFFERENTIATION
chromosome Normal Genetic Female 1. Differentiate Primary Gonads
Sperm cell carries 1 Y sex chromosome and it fertilizes 2. Differentiate Genital ducts that will differentiate into
an ovum with of course, as always, carrying 1 X sex internal genitalia
chromosome Normal Genetic Male 3. Differentiate External genitalia structures
Nondisjunction Primary Gonads
Failure of paired chromosomes or sister chromatids to Primary organ of reproduction
separate after 2nd meiotic division; di naghiwalay! Differentiation is Genetically determined
results to 2 sex chromosomes in 1 mature cell and none Males: Testes ; Female: Ovaries
on the other Common anlage in M&F Bilateral Genital Ridge:
Male: 1 sperm cell has 2 Sex chromosome, other th
indifferent from fertilization up to 7 week AOG
sperm cell has 0 2 parts: Inner medulla & outer cortex
Female: 1 ovum has 2 Sex chromosome, other Testes dev’t
ovum has 0 (+) Y (+) HY antigen, a membrane protein= Testes
Eg: (How to create a) determining product medulla develops, cortex
1. Superfemale regresses
Sperm cell with X sex chromosome fertilizes an ovum with XX
7th-8th week || Tesdulla (testes medulla)
sex chromosome =XXX
2. Turner’s Syndrome Ovary dev’t
Sperm cell with X sex chromosome fertilizes an ovum with 0 (-) Y (-) HY antigen cortex develops, medulla
sex chromosome =X0 regresses ; XX sex chromosome are required
Spermcell with 0 sex chromosome + ovum with X chromosome
(as always) =X0 8th-10th week || Corvary (Ovary Cortex)
3. Klinefelter’s Syndrome
Sperm cell with 1 Y sex chromosome fertilizes an ovum with XX Turner’s XO= No Y , only 1 X neither testes or ovaries
sex chromosome =XXY develops Gonads are long pale streak of connective
Sperm cell with XY sex chromosome+ ovum with X sex
chromosome=XXY tissue
4. Sperm cell with 0 sex chromosome + Ovum with XX sex Hormonal treatment of mother during pregnancy has no
chromosome Normal Genetic Female effect on gonadal differentiation
5. Sperm cell with XY chromosome + Ovum with XX
chromosome=XXXY considered as male bec of Y
6. Sperm cell with XY sex chromosome + Ovum with 0 sex Genital Ducts
chromosome Normal Genetic Male Indifferent during early stage of embryonic life
Sperm cell carrying Y sex chromosome fertilizes ovum with 0 sex Male: Wolffian duct ; Female: Mullerian duct
chromosome or Sperm cell and ovum with no sex chromosome
Not viable Male differentiation
2. Hair Root Test Mullerian duct regresses, wolffian duct develops, giving
Pluck 3-4 strands of normal scalp hair tease hairroots rise to:
then stain with fluorescent dye (Quinachrine diHCl)
Internal Genitalia:
microscope: see that Y body? That is the part of the Y Epididymis Seminal Vesicles
sex chromosome look for the F or Fluorescent body Vas Deferens Ejaculatory duct
within it, if (+) Genetic male Female differentiation
3. Karyotyping or Chromosomal Analysis Wolffian ducts disappears, mullerian duct develops
Most accurate and Most expensive giving rise to:
Tissue cultures are made and autosomal & sex Internal Genitalia: Fallopian tubes
chromosomes are paired; usually done by scientists who Uterus
specializes in genetics
Page 31 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Presence and Absence of functional testes Components of Sexual Identity
Present Absent Component Female Male
Males: XY (+) Y sex Females or in males with Chromosomal Sex/ XX XY
chromosome (+) HY antigen nonfunctional testes mullerian Genetic Sex
testes develops if testes duct develops, wolffian duct Nuclear Sex/Test Positive Negative
functions normally wolffian regresses (+) Barr Bodies
duct develops into male internal Gonadal Sex Ovary Testes
Hormonal Sex Mainly Estrogen Mainly Androgen
genitalia
Internal Genitalia Mullerian Duct Wolffian Duct
mere presence of testes does not guarantee that it will
External Genitalia Lack of Androgen DOS Penis & Scrotum
develop to be the wolffian ducts, TESTES SHOULD BE Labia Majora & Minora,
FUNCTIONING NORMALLY. Clitoris, Vesibule
Development of Genital ducts
MALE Sex Chromosomes Conditions in Ambiguous Ext genitalia
Function of embryonic testes: (+)Ambiguous External genitalia, Possible chromosomal make up:
Spermatogenesis o Normal Female:44XX=46 in total
Secretes: o Normal Male: 44XY=46 in total
o Mullerian Regression factor (MRF)- inhibits
o Abnormal sex Chromosome
mullerian duct dev't no female internal genitalia
(Unilateral action) ; for dev't of vas deferens and
related structures
o Duct Organizing Substance (DOS) & Testosterone
- stimulate dev't of wolffian duct ; for dev't of vas
deferens and related structures
No testes or non-functional testes there will be no
secretory products, therefore:
nothing will inhibit the dev't of mullerian ducts
genital ducts have the tendency to feminize
wolffian ducts will not be developed no male
internal genitalia
FEMALE
XX NO Y NO HY antigenno testes no MRF, DOS & TRUE HERMAPHRODITE
testosterone genital ducts feminizes Causes: Nondisjunction and Mutations
Gonads: (+) Ovarian and Testicular tissues: Ovotestis
Ovaries are not needed for the dev't of female internal (+) Male facial hair, 2/3 of patients have normal breast dev’t,
genitalia i.e fallopian tube and uterus abundant pubic hair
So if there is no Gonad or Gonad is only rudimentary , (+) Uterus may or may not menstruate; not possible to get
irregardless of chromosomal sex only uterus and fallopian preggy on their own
tube develops 70% Chromatin Positive will menstruate
Turner's syndrome X0 No testes, No ovaries uterus Negative will not menstruate
and fallopian tubes develops nonetheless bec without testes External Genitalia- either male or female; often ambiguous
again, internal genitalia tends to feminize. Reared as males more often (3 out of 4) bec of big phallus
Male Pseudohermaphrodite Female Pseudohermaphrodite
Development of External Genitalia Sex Chromosomes: XY Sex Chromosome:XX
Gonads: Testes ONLY Gonads: Ovaries ONLY
Cause: Non-functional Testes Int Genitalia: uterus and
or No receptors in target fallopian tubes
cells Tendency of Int&Ext Ambiguity only in Ext
Genitalia to feminize genitalia: Big phallus, labia
Ambiguous Int&Ext Genitalia majora looks like scrotum,
No facial and body hair, incomplete Urogenital sinus
sparse pubic hair, small closure
phallus, ample breast dev’t, Short stature, with body and
body is of female shape facial hair, male like pubic
MALE
hair distribution, small
If testes is functional secretes also dihydrotestosterone along
breast, prominent muscles
with testosterone for masculinization of male external genitalia
Without testosterone and dihydrotestosterone external Cause: CAH and exogenous
genitalia tends to feminize too intake of androgens by
st
Testosterone- also responsible for male secondary sexual pregnant Mom during 1
characteristics i.e facial, body and pubic hair growth, low pitch trimester
voice, more developed muscles (anabolic hormone function) CAH/ Congenital Adrenal Hyperplasia
FEMALE Hyperplastic adrenal glands Inc androgen secretion
XX NO Y No MRF, DOS, testosterone and Masculinization of external genitalia. Determined during Newborn
dihydrotestosterone feminine external genitalia (also internal) screening test.
Estrogen - main secretory product of ovary for dev't of Turner’s Syndrome Characteristics:
secondary female characteristics i.e high pitch voice, more fat Short stature, neck webbing, small breast, sparse pubic hair, small
deposition in breast buttocks and thighs phallus; No gonads, but with Infantile uterus, fallopian tube and
SAD TRUTH: You can change the appearance of your female Ext Genitalia, bec there is no ovaries therefore no
external genitalia through surgery but you won't be able to estrogen so no maturation.
change your genetic make up No estrogen and androgen No negative feedback Increased
FSH&LH
Page 32 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Male Reproductive System Formed from Testosterone by Sertoli cells when stimulated
by FSH
Essential for spermiogenesis
3 Major Subdivisions
Growth Hormone (GH) and most of other body hormones
1. Spermatogenesis For controlling background metabolic functions of testes
2. Performance of male sexual act Promotes early division of spermatogonia
3. Hormonal Regulation of Reproductive functions If absent (pituitary dwarfs) Spermatogenesis is deficient or
Spermatogenesis absent Infertility
Occurs due to stimulation of Ant Pituitary
Gonadotropic homones beginning at Puberty (13 y/o) Maturation and Storage of sperm
Occurs in all Seminiferous tubule Maturation Happens in EPIDIDYMIS after 18-24 hours
they develop capability of motility
Sperm removed from S.tubule and early portions of epididymis
are NONMOTILE and CAN’T FERTILIZE ovum
Several inhibitory proteins in epididymal fluid prevents final
motility until after ejaculation
Storage can be in epididymis but mainly in VAS
DEFERENS, its fertility is maintained for at least 1
month, they are deeply suppressed and therefore
become nonmotile there.
Excessive sexual activity and ejaculation storage is shortened
Testes produces about 120M sperm/day
Maturation/Actual Maturation of Sperm
Happens after ejaculation sperms become motile and
capable of fertilizing ovum
This is different from the “maturation” happening in
epididymis, dun kasi di pa kaya mag fertilize ng ovum
Before onset of puberty, sperm is absent. Up until puberty, Physiology of mature sperm
Spermatogonia only. Normal Motile sperm capable of flagellated
movement @ 1-4 mm/min velocity
Steps of Spermatogenesis: Activity of sperm is greatly enhanced in a neutral or
slightly alkaline pH (eg. Ejaculated semen)
Inc temp Inc Metabolism Inc sperm activity but
dec sperm life span
Strong acid medium (eg. Female genitalia) sperm
dies
Lifespan in female genital tract when ejaculated is 1-2 days only
Not the actual sperm that can fertilize egg
Genetic sex depends on the sperm that fertilizes the egg
Mitochondria synthesizes ATP for sperm motility
Hormones that stimulates Spermatogenesis
Luteinizing Hormone (LH) SEMEN
Secreted by APG ejaculated by male during sex
Stimulates Leydig cell to secrete testosterone composed of fluid from (and sperm )Vas deferens, Prostate gland
Testosterone and Seminal Vesicles and few from mucous glands i.e
Secreted by Leydig cells located in interstitium of testis bulbourethral gland
st
Essential for 1 stage of forming sperm (growth and division pH of 7.5
of testicular germinal cells) Seminal Vesicles
Follicle Stimulating Hormone (FSH) 60% BULK of the semen
Secreted by APG Mucoid semen (same with mucous glands)
Stimulates Sertoli cell Composed of products Last to be ejaculated
Without FSH, Process of spermiogenesis does not occur i.e Serves to wash sperm through ejaculatory duct and urethra
spermatidssperm. Contains Cholesterol, Fructose, Citric acid, Fibrinogens and
Estrogen Prostaglandins
Page 33 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Fibrinogens and also causes falling off of any sperm that had already begun
for semen to be a coagulum binding
Prostaglandins
Makes female cervical mucus more receptive to Abnormal Spermatogenesis and Male Fertility
sperm movement
For reverse peristaltic contraction in oviducts Destruction of Seminiferous tubule
and uterus to move sperm toward ovaries o Bilateral orchitis resulting from mumps or STD’s
Prostate Gland may result to Sterility
30% o Inborn degenerated tubular epithelia may result
Milky semen, slightly alkaline enhances sperm motility and
fertility to Sterility
Contains Calcium, Citrate Ion (for alkalinity), Phosphate Ion (for o Excessive temp of testes seminiferous tubular
alkalinity), Clotting enzyme, profribrinolysis cells degenerate spermatogenesis is prevented
(+) clotting enzyme catalyzes reaction forming Coagulum from
may cause temporary sterility
fibrinogens to hold sperm in uterine cervix dissolves because of
fibrinolysin liquefies sperm sperm becomes highly motile Scrotum acts as a controlled cooling mechanism (maintains 2 C
again below internal temp)
Vas deferens o Warm-down
10% o Cold-up
Secretes Acidic fluid Cryptorchidism
Sperm motility optimum at pH 6-6.5 o Undescended testes at or near the time of birth
Seminal vesicle Fibrinogen Coagulum o Testes are derived from genital ridges in abdomen 3
Prostate gland (+) clotting enzyme for Fibrinogen to weeks or 1 month before birth, testes normally descends
form coagulum through inguinal canal into scrotum mediated by
Testosterone under HCG stimulation of testes.
Capacitation of Spermatozoa o Testes remains on abdomen abdomen has higher
Enables sperm to penetrate ovum temperature than scrotum tubular epithelium
Requires 1-10 hours degenerates may cause sterility
Changes that Occurs in capacitation After 1 year and still no descent may cause tumor growth
Uterine and fallopian tubes wash away inhibitory factors do surgery
that suppressed sperm activity in male genital ducts
Sperm Count, Morphology and Motility on fertility
After Ejaculation sperm swim upward toward uterus
Count
gradual loss of cholesterol in sperms membrane
Semen per ejaculation = 3.5ml
acrosome becomes weaker enzymes from acrosome Average sperm is 120M per ml of semen
will be released Zona Pellucida penetration In “normal” males, it varies from 35M to 200M
Cholesterol Sperm per ejaculation = 400M
o Contained in seminal vesicle Infertile if sperm is 20M and below
o Toughens acrosome and prevents enzyme release Morphology
Abnormal: 2 heads, abnormal tails etc motility is affected
Membrane becomes more permeable to Ca Ions may cause sterility
flagellum becomes more powerful for whiplash motion Motility
For reasons not known they are entirely or relatively not
Acrosome Reaction motile likely to be infertile
Movement of sperm should be 1 direction only
Release of enzyme and digestion of membrane of ovum
Acrosome have abundant:
MALE SEXUAL ACT
o Hyaluronidase depolymerises hyaluronic acid
Results from inherent reflex mechanisms integrated in
polymers in intercellular cement that hold ovarian
the sacral and lumbar spinal cord initiated by either
granulose cells together
psychic stimulation from the brain or actual sexual
o Proteolytic enzymes digest proteins in
stimulation from the sex organs or both.
structional elements of tissue cells that adheres to
Glans Penis
ovum
most important source of sensory nerve signals for
FERTILIZATION initiating the male sexual act
Ovum is expelled sperm dissolutes the ovum’s granulose cell very sensitive, have lots of nerve endings causes one to
layers acrosomes release enzyme to penetrate zona experience sexual sensation
pellucida anterior membrane of sperm binds with receptor
proteins in zona pellucida entire acrosome dissolves all Stimulation of the anal epithelium, the scrotum, and
acrosomal enzymes are further released passageway is perinealstructures in general can send signals into the cord
formed for sperm head to go through zona pellucidacell that add to the sexual sensation, which also includes urethra,
membrane of sperm head and oocyte fuses= single cell with bladder,prostate, seminal vesicles, testes, and vas deferens.
equal number of chromosomes from motherfather.
STD improperly treated organism still infects the male
st genitalia causing tingling sensation increases libido
Only 1 sperm enters the oocyte bec when the 1 sperm
penetrates zona pellucida calcium ions diffuse inward through
oocyte membrane multiple cortical granules will be released
by exocytosis thereby preventing binding of additional sperm
Page 34 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
High testosterone
Psychic element o Negative feedback Hypothalamus and APG inhibits
Sexy thoughts, wet dreams during some stages of sexual life further release of GnRH and FSH LH respectively
(teenager) o FSH stimulate sertoli cells to secrete Inhibin inhibit
hypothalamus and APG
STAGES OF MALE SEXUAL ACT
1. Penile Erection
By Parasympathetic Nerves (sacral nerves pelvic nerves penis Effect of Testosterone on Development of Adult Primary
first effect of male sexual stimulation, degree of erection is and Secondary Sexual Characteristics
proportional to the degree of stimulation, whether psychic or Penis, scrotum, and testes enlarge about eightfold before
physical the age of 20 years
2. Lubrication More prolific hair distribution
By the Parasympathetic Baldness Testosterone decreases the growth of hair on
cause the urethral glands and the bulbourethral glands to secrete the top of the head
mucus
Voice hypertrophy of the laryngeal mucosa and
most of the lubrication is provided by the female sexual organs
Without lubrication painfulmale sexual act is seldom
enlargement of the larynx masculine voice
successful Thickening of skin and development of acne
3. Emission & Ejaculation Protein Formation and Muscle Development
By the Sympathetic nerves Increases Bone Matrix and Causes Calcium Retention
culmination of the male sexual act Male Orgasm growth spurts
Emission forerunner of ejaculation (up to formation of semen) Inc BMR Inc RBC production
Increases the reabsorption of Na in the distal tubules of
CONTROL OF MALE SEXUAL FUNCTIONS BY HORMONES the kidneys
Controlled by Anterior Pituitary Gonadotropins
GnRH from Hypothalamus APG releases LH & FSH MALE CLIMACTERIC
o LH= stimulate Leydig cells Testosterone release Decrease in male sexual function due to dec testosterone
o FSH= stimulate Sertoli cells Spermatogenesis production
Symptoms:
TESTOSTERONE o Hot Flashes
o Suffocation
Mainly Secreted by Leydig cells (numerous in the newborn
o Psychic disorders Male Menopause
male infant for the first few months of life and in the adult
male after puberty)
Abnormalities of Male Sexual Function
Not present during childhood years
Old Age (above 50y/o) decrease in testosterone
production Prostate Gland
For development of Male secondary characteristics from Normally, small throughout childhood and begins to grow
puberty to maturity at puberty under the stimulus of testosterone. Stationary
The Primary testicular hormone (along with size at age of 20-50
dihydrotestosterone, and androstenedione) Benign Prostatic Fibroadenoma Cancer of the Prostate
Dihydrotestosterone more active hormone Older men 2-3% of male deaths
Small amount secreted by Adrenals, that’s why women Causes urinary obstruction Testosterone increases CA
Hypertrophy caused by cell growth
with adrenal tumor manifests with male secondary sex overgrowth of prostate Treatment:
characteristics tissue itself, not by Remove Testes no
For Masculinisation testosterone testosterone production
CA cell growth is
o Fetal life: HCG from placenta stimulates testes inhibited.
For Testicular descent Estrogen decreases
o Puberty-Remainder of life: Testosterone under size of Prostate
stimulus of LH
HYPOGONADISM VS HYPERGONADISM
HYPOGONADISM HYPERGONADISM
Causes: Interstitial Leydig cell
Nonfunctional testes tumors 100x increase in
Castration testosterone production
genetic inability of the S/Sx:
hypothalamus to secrete rapid growth of the
normal amounts of GnRH musculature and bones
S/Sx: but also cause early
Childlike voice uniting of the
No Hairloss; Sparse epiphyses Small
hair distribution stature
Infantile penis Excessive dev’t of male
Less muscular body sexual organs and male
Decrease Libido secondary characteristics
Page 35 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Female Physiology GnRH
PART I Produced in Arcuate nucleus in the medial basal
ANATOMY Hypothalamus
External Genitalia/Vulva Stimulates synthesis and release of LH & FSH if secreted in
Anything seen from Mons Pubis down to Perineal Body a pulsatile manner (every 1-2 hours)
Vagina is a part of external Genitalia If released in continuous manner No release of
Internal Genitalia FSH LH Amenorrhea
3 Major Structures: FSH & LH
o Uterus, Ovaries and Fallopian tubes/Oviducts Produced by Basophilic cells of APG
Same alpha units with TSH and HCG
GENETICS Hyperthyroidism
Genetic Sex established upon FERTILIZATION, Elevated T3 T4 APG decreases release of TSH, since they
determined by the Sperm (either X or Y sex chromosome) have similar alpha units and came from the same cell
BUT BUT BUT, it is still indifferent, meaning you will not be (basophilic cells) FSH & LH release is also inhibited
able to identify if it’s Male/Female just yet. amenorrhea
6 Weeks of Gestation the sex can be distinguished as Pregnancy test check for Beta HCG also as this may
female or male, first evidence is the Primordial germ cell cause a false positive result in PT
FSH
OVARIAN DEVELOPMENT Acts on Granulosa cell facilitating their proliferation and
1. 3-6mos AOG Primordial germ cells undergo mitosis production of estrogen and FSH&LH receptors
producing now 7Million oogonia which contains the Stimulate follicle growth
ovum called PRIMARY OOCYTE LH
st
2. After 6 mos AOG Oogonium enters 1 Meiotic division After ovulation, LH acts on the granulosa cells for the
BUT STOPS AT DIPLOTENE STAGE OF PROPHASE production of progesterone and,
3. Upon Birth DIPLOTENE STAGE OF PROPHASE of Meiosis Theca cells for the production of androgens Later
1 ; 2 Million Primordial follicles converted to estradiol through the 2 cell 2 gonadotropin
4. Puberty First Meiotic Division will resume and is system.
completed upon OVULATION becoming now a Secondary FSH granulosa cells Estrogen
Oocyte ( 22X) ; 400,000 Primary follicles LH granulosa cells Progesterone
5. Second Meiotic Division is completed upon Fertilization, Festrogen || Logesterone
That is, after Meiosis 1 ovum will go directly into Synergistic for FSH Follicular Maturation
Metaphase, bypassing now the prophase stage producing Without LH No ovulation No fertilization
now a haploid chromosome INFERTILITY
WHOLE REPRODUCTIVE SPAN OF FEMALE (13-46 y/o)
only 400 oocytes will be ovulated, the rest of the 7Million
undergoes Atresia MENSTRUAL CYCLE
MATURE GRAAFIAN FOLLICLE Ave Duration: 28 days (+/- 7 days)
Among thousands of follicle only 1 will mature to ovulate, o Polymenorrhea= <21 days
after which what remains is the Corpus luteum o Oligomenorrhea= >35 days
After meiosis I (upon ovulation) a Secondary Oocyte is o Menorrhagia = abnormally heavy or long
formed menstrual flow
Group of Granulosa cells surrounding the oocyte is the o Metrorrhagia= irregular bleeding in between
Cumulus Oophorus, this Granulosa cells produce menstrual period
ESTROGEN (and Progesterone) o Dysmenorrhoea= painful menstruation
Theca cells outside produces ANDROGENS 2 cycles: (occurs at the same time)
o Ovarian Ovum is fertilized
FEMALE HORMONAL SYSTEM o Endometrial Endometrium is prepared for
possible implantation of fertilized ovum
Regulation
Depends on FSH LH Pag wala Atrophic Ovary
o GnRH from Hypothalamus:
Occurs in ovary and endometrium from day 21-28 of cycle
Stimulatory and inhibitory
Menstruation happens every 28 days
feedback effects of ovarian
Children (source of estrogen is the adrenal cortex)
steroids: estradiol &
APG is very sensitive to Estrogen, so iinhibit agad
progesterone via Long
nya si FSH LH No menstruation || Puberty
feedback loop
estrogen sensitivity of APG is lost no more FSH LH
o GnRH inhibition via GnRH itself
inhibition Menstruation
via ultrashort feedback
mechanism and via neural PUBERTY
input pathway 9-12 y/o Inc FSH & LH
o Gonadotropins from APG: 4 Stages:
inhibitory effect via Short o Thelarche Breast Budding
Feedback loop o Adrenarche pubic and axillary hair growth
o Accelerated growth spurt
o Menarche @ 11-15 y/o
Page 36 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
2. LUTEAL PHASE – FIXED AT 14 DAYS
Remaining 14 days
Corpus Luteum
Formed after ovulation by LH; it’s granulose cells produce
more Progesterone than that of estrogen || Theca cells
produces androgen (androstenedione) & Testosterone
After Ovulation LH converts granulose and theca cells
into Lutein Cells produces more progesterone, So
in the cycle after 14 days (during Luteal phase) Level of
progesterone is much higher than estrogen.
LH decreases corpus luteum regresses becomes
corpus albicans Estrogen and Progesterone are now
only moderately secreted on 26th day or 12 days after
ovulation Onset of Menstruation is signaled
Inhibin
From ovary, inhibits FSH secretion
REVIEW
Midluteal phase High level of Progesterone and Estrogen
OVARIAN CYCLE Negative Inhibition Dec FSH LH
TWO PHASES (28 days): Mid Follicular phase Dec FSH, Inc Estrogen
1. FOLLICULAR PHASE – NOT PREDICTABLE Corpus Luteum produced by LH
st Cause of LH surge Estradiol peak
1 14 days
FSH Growth || LH Maturation
Birth= 2 Million primordial follicles
Ovum is with 1 layer of granulose cells for P.S
nourishment and oocyte maturation inhibiting factor Day 1 is the first day of your Menstruation. So yung
to keep it on diplotene stage of prophase @ meiosis “cycles” mo nagsstart upon menstruation.
1 ENDOMETRIAL CYCLE
Puberty= FSH LH Increases TWO PHASES (28 days):
Meiosis I is resumed and completed upon ovulation PROLIFERATIVE/ESTROGEN PHASE
giving rise to secondary oocyte || 400,000 primary >Corresponds with Follicular phase
follicles Begins at Day 1:
From Primary to pre Antral FSH is not needed / Non Estrogen for progressive growth of endometrial glands
Gonadotropin dependent
(which secrete thin mucus into the cervical canal)
Rapid proliferation of granulose cells and theca cell
formation follicles become Pre Antral
thickening of endometrium, continues up to day 14
Pregnancy (ovulation) even upon entering secretory phase
Placenta releases high Estrogen and Progesterone Day 5:
APG is not releasing FSH and LH bec of Negative feedback Due to the thickening of endometrium Covering up of
Mechanism blood vessels that are exposed Menstruation ceases
Day 1 of Menstrual cycle SECRETORY PHASE
Estrogen and Progesterone is low ; FSH is TOO HIGH Day 14-28
recruitment for accelerated growth of 6-12 pre antral Estrogen still promotes endometrial proliferation
follicle only 1 dominates 1 follicle becomes Antral Progesterone Prepares endometrium for possible
follicle rich in estrogen implantation by causing swelling and secretory dev’t in
Vesicular follicle- a follicle that exhibits excessive growth endometrium and increasing its blood supply
due to FSH too much estrogen FSH receptors also No fertilization or implantation
increases Increase FSH responsiveness produce more On 26th day( 2 days before menstruation) corpus
ESTROGEN AND ESTROGEN ONLY follicle becomes luteum regresses becomes corpus albican
larger ( Positive Feedback Mechanism) Progesterone Estrogen decreases no more support to
FSH and Estrogen increased in theca cells receptor endometrium causing vasospasm of blood vessels due to
allows LH to act for FINAL MATURATION of follicle.
prostaglandins endometrium is sloughed off
Vesicular follicle becomes the Dominant follicle the other
11 follicle undergoes atresia because the Increase in blood vessels are exposed again Menstruation on day
estrogen secreted by the dominant follicle inhibits APG to 1
release FSH REVIEW
ESTROGEN In Proliferative phase Endometrial Proliferation
Dominant Follicle Ovulation proceeds PROGESTERONE for Secretory development and support
for possible implantation of fertilized ovum
LH Progesterone decline signals onset of menstruation
For Final follicular growth and ovulation
LH Surge LH at its peak for 2 days before ovulation MENSTRUAL PERIOD
10-12 hours after LH surge Ovulation happens 40 ml of blood loss (whole duration)
Causes of LH surge Estradiol peak, When estrogen is Contains fibrinolysin so it doesn’t clot, if (+) clot Heavy
secreted on highest level APG is stimulated even more to menstruation bec fibrinolysn is not enough, too much blood.
release LH at highest peak. Ceases 4-7 days due to re epithilialization
Too little estrogen is secreted No Estradiol peak
No LH surge No ovulation Infertility
Page 37 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
OVARIAN STEROIDS magiging infantile sila, I think breast growth
Cholesterol wrong choice of word lang. for breast feeding
Parent compound of all sex hormones Turner’s syndrome
Rate limiting step= Cholesterol Pregnenolone no ovaries no Promotes secretory
2 pathway of Pregnenolone estrogen changes in
DHEA pathway Androgen converted to infantile int & ext endometrium
Estrogen genitalia
Progesterone pathway Progesterone Precocious
th
During Follicular Phase DHEA (5 ) pathway is puberty Dec freq and
favoured oversecretion of intensity of uterine
During Luteal Phase when Corpus luteum is produced estrogen contractions
th
due to LH Progesterone(4 ) pathway is favoured children with prevents
mature ext genitalia miscarriage
ESTROGEN Dev’t and maturation
Sources: of female secondary for nutrition of
o Ovary characteristics travelling fertilized
o Adrenal cortex Androgen estrogen Maintains normal ovum
o If pregnant major source PLACENTA structure of skin and Cervical mucus:
Types: blood vessels Scanty, viscous
o Beta-estradiol – Major form from ovary Accelerates growth and acidic “white
o Estrone –majority from peripheral coversion of and early closure of mens”
androgen; some from ovaries epiphysis of long Signals entering
o Estriole – oxidative product of estradiol and bones ( nauuna in next cycle of
estrone tumangkad ang babae) menstruation
PROGESTERONE Growth of ovarian (+) itch and foul
Most important among progestins follicle smell
Sources: Cervical mucus Infection
o 2nd half of ovarian cycle ( Luteal Phase) production clear,
o Placenta if preggy of course watery and slightly Increases basal
o Adrenal Cortex alkaline (after mens) body temperature
Greater Osteoblastic
activity for bone
HORMONE PRODUCTION IN GRAAFIAN FOLLICLE
deposition
Menopause no
THECA CELLS Androgens: Androstenedione estrogen dec
Testosterone
osteoblastic act
GRANULOSA CELLS Estrone osteoporosis prone
Estradiole Protein synthesis in
During Follicular phase: liver
Estrogen Blood coagulation,
CORPUS LUTEUM (Lutein Mainly Progesterone water retention
cells) Estrogen Preggy High
estrogen Edema
TWO-CELL TWO-GONADOTROPIN HYPOTHESIS
Two cells Granulosa and Theca cells
Two Gonadotropin FSH LH PART II
THE FASTEST SPERM
Principle: Millions of sperm is introduced into vagina upon
Cholesterol to Androgen conversion occurs only in THECA ejaculation BUT ONLY 1 SPERM CAN FERTILIZE IT
cells because the LH dependent enzyme is only present in Once sperm fertilizes ovum Zona pellucida solidifies
THECA cells. preventing other sperm from entering
TRANSPORT AND IMPLANTATION
Androgens (Androstenedione & Testosterone) Brought Ovum travels along fallopian tube for 3-4 days
inside granulosa cells converted to estrogen via FSH Blastocyst
dependent enzyme aromatase. (Only in Granulose cells) Mature zygote
2 types of cell:
o Inner cell fetus
ESTROGEN & PROGESTERONE o Outer cell trophoblast placenta
Metabolized in liver; mainly secreted via Urine Cilia will propel the zygote toward uterus
ESTROGEN PROGESTERONE DAY 7 trophoblast secrete proteolytic enzyme
Dev’t of Female Glandular and endometrium is digested and liquefied
reproductive organs. secretory dev’t of IMPLANTATION (with bleeding)
P.s reproductive organs Implantation in endometrium of uterus need to
ang alam ko magdedevelop pa
maintain corpus luteum for sustained progesterone
din ang female repro even
without estrogen pero secretion preventing sloughing off of endometrium
Lobuloalveolar
Page 38 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
(will cause abortion if corpus luteum regresses <7 weeks HUMAN CHORIONIC SOMMATOMAMMOTROPIN (hCS)
AOG) secreted by placenta
PLACENTA an anti insulin diabetogenic hormone
1.) Diffusion of oxygen from the mother to the baby increases level of maternal glucose to be given to fetus
Fetus Does not have functional respiratory sytem if not tolerated by mothergestational diabetes
depends on mother for Oxygen For maternal lipolysis Inc free Fatty acids energy
Factors that enable the fetus to deliver enough oxygen to source for maternal metabolism
the tissue: May play a role in fetal vasculature formation
Fetal hgb carries 20-50% more oxygen than an adult hgb
Hgb concentration of the fetal blood is 50% greater than OTHER HORMONES OF PREGNANCY
the mother
Bohr effect : CORTICISTEROIDS
o Curve is shifted to the right = Oxygen Inc Inc glucocorticoids inc mobilization of amino acids
o Maternal and fetal blood meets baby donates for fetal growth
CO2 to mom fetal CO2 level is dec shifts Inc aldosterone causes edema to mother
curve to left oxygen affinity decreases baby
gets oxygen. Double Bohr effect THYROID GLAND
4 parameters that will shift the Inc cellular and vascularity of gland inc in size
curve to the right: Inc in thyroxine production for fetal brain
increase H+ or decrease pH increase 2-3DPG development
increase CO2 increase temperature
PARATHYROID GLAND
2.) Diffusion of carbon dioxide from the baby to the Enlarged Maternal calcium mobilization Ca is
mother given to fetus fetal bone and teeth development
o Baby has higher CO2 levels, tendency is you give Ca supplements to mom to prevent early
transfer CO2 to mother osteoporosis
3.) Diffusion of foodstuff from the mother to the baby
o mainly glucose MATERNAL ADAPTATION TO PREGNANCY
4.) Excretion of fetal waste product to the mother
WEIGHT GAIN Normally around 24lbs:
Placenta is Connected to baby via Umbilical cord: 7lbs from fetus
o 3 vessels of Umbilical cord 6lbs from intravascular vol
2 umbilicar artery – carries deoxygenated 4lbs from amniotic fluid, placenta and
blood fetal membranes
1 umbilical vein – carries oxygenated blood 3lbs from fats
Fetal blood does not mix with maternal blood, if it does
METABOLISM Inc maternal thyroid hormone
may lead to Erythroblastosis fetalis
production Inc BMR by 15%
HORMONES OF PREGNANCY NUTRITION balanced diet
Iron supplements (1000 mg), calcium,
HCG
vitamins etc
FIRST hormone secreted during pregnancy
Pregnant add 300 kcal to diet
Secreted by the trophoblast cells of zygote
Lactating add 500 kcal to diet
Maintains corpus luteum (+) progesterone and
BLOOD VOLUME Estrogen and aldosterone fluid
estrogen pregnancy maintenance
Peaks at 8th week declines after 8th week Plateau retention Inc BV
starts at 18-20 weeks CARDIAC OUTPUT Increased blood volume Inc CO
After 8 weeks HCG declines corpus luteum RENAL Inc blood volume Inc GFR
regresses (13-17th week) Doesn’t matter because RESPIRATION Progesterone inc tidal volume
th
PLACENTA takes over during the 7 week (+) Inc RR
progesterone and estrogen pregnancy maintenance
PARTURITION/LABOR
ESTROGEN process of giving birth
Pregnant for enlargement of uterus, palpated just 2 causes:
below xiphoid process A. Progressive hormonal changes
for enlargement of stromal and ductal structures of the Estrogen Progesterone ratio Oxytocin on uterus
breast AOG <7 mo: More Synthesized in hypothalamus,
for enlargement of female ext (and int) genitalia Progesterone stored and released by
for relaxation of pelvic joints and ligaments AOG >7mo: More estrogen Posterior pituitary gland for
Uterine Contractions titigas yung tyan strong uterine contraction
(also for milk letdown)
PROGESTERONE Fetal hormones
Causes decidual cells to develop Fetal Pituitary gland Inc oxytocin uterine contraction
decreases contractility of pregnant uterus Fetal adrenal gland Inc cortisol
nourishes morula and blastocyst as it travels in fallopian Fetal Membranes Inc Prostaglandinuterine contraction
tube for 3-4 days
for preparation for lactation
Page 39 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
B. Progressive mechanical changes Mitosis starts when? (developing female 3-6mo AOG
Stretch of uterine musculature eagers contraction baby)
Cervical stretch and irritation prostaglandin release When is genetic sex established? Upon fertilization
uterine contraction Stage of oocyte during menstruation Metaphase 2 of
Meiosis 2
upon reaching full term and post dated na advice
When is Meiosis 2 completed? Upon fertilization
mom to have sex sperm contains prostaglandin and
When is Meiosis 1 completed? Upon Ovulation
penis will irritate cervix which causes further
Stage of oocyte upon birth? Prophase:
prostaglandin release uterine contraction
Diplotene stage
STAGES OF LABOR What confers or determines sex of baby? The sperm
To be stimulatory, how do you release GnRH? Pulsatile, every 1-2
1st Onset of REGULAR uterine hours
contraction up to Full cervical Hormone of Ovulation? LH LH surge
dilation (10cm) st
1 sign of puberty? Thelarche
2nd Full cervical dilation up to Last sign of puberty? Menarche
delivery of baby Ovulation happens when? 14 days before (or
3rd Delivery of baby up to after) onset of
**Very important, if not done delivery of placenta menstruation ||
10-12 hours after
massive bleeding
LH surge
Uterine Involution 4-6 weeks after delivery, it goes What causes LH surge? Estradiol peak
back to non pregnant state Culprit of Infertility? LH
LACTATION What hormone signals onset of Mainly a decline in
Estrogen stromal and ductal structures of the breast menstruation? progesterone (LH
and stimulus for prolactin release minor only)
Progesterone lobuloalveolar growth What phase does LH surge happen? (late) follicular
breastfeeding When does Estradiol peak happen? (late) follicular
Effect of Estrogen in APG and Hypothalamus: Stimulatory
Very High
PROLACTIN
Effect of Estrogen in APG and Hypothalamus: Inhibitory
released in APG stimulated by estrogen
Moderate-low
for milk production, starts at 5th week of Pregnancy
Main hormone of corpus luteum Progesterone
until delivery of baby
Day 1 of cycle, FSH level is HIGH ( low
Estrogen and
ESTROGEN & PROGESTERONE Progesterone)
inhibitory to effect of prolactin in the BREAST so if not Transport of ovum along fallopian tube? 3-4 days
pregnant you will not lactate Who fertilizes ovum?
st
1 sperm to arrive
Pregnant after delivery dec estrogen and Hormone maintaing pregnancy Progesterone
progesterone dec suppression of prolactin effects in Who can make the uterus contract? Estrogen
breast lactation after several Progesterone or Estrogen?
days Nipple stimulation causes release of: Oxytocin and
after delivery dec estrogen no more stimulus for Prolactin
prolactin release in APG dec prolactin WHAT TO Hormone responsible for non ovulation when PIF/Dopamine
DOOO? stimulate nipples: breastfeeding?
o Release Oxytocin (milk letdown or milk Hormone for milk production Prolactin
expression and uterine contraction to For milk letdown? Oxytocin
prevent post partum bleeding) What hormone produces corpus luteum LH
o Release Prolactin for milk production Corpus luteum secretes Progesterone >
Estrogen
What phase varies? Luteal or Follicular? Follicular
Family planning factor: Prolactin release PIF or
Produced by corpus luteum, inhibits APG Inhibin
dopamine is also released GnRH is inhibited no FSH
causing a dec in FSH & LH during luteal phase
and LH no menstruation and ovulation pregnancy
# of oocytes ovulated during entire repro 400
prevented for max of 6mos period
# of oocytes At birth? 2M
FAQ’s/MLAQ’s Puberty? 400,000
3-6 mos AOG? 7M
th th
Blastocyst implants in endometrium 5 -7 day post What causes proliferation of granulose cells? FSH
ovulation Stage of follicular growth wherein you don’t Primary stage
th
HCG peaks at? 8 week AOG need gonadotropins
Layer of uterus involved in menstruation? Endometrium
For contraction? Myometrium
Most common site of Ectopic pregnancy? Ampulla of
fallopian tube
Usual Site of Fertilization Ampulla of
fallopian tube
Who guides ovum towards Fallopian tube? Fimbriae
What are the stages of Mitosis? PMAT, Interphase
is not included
Page 40 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Anti stress hormones: Cortisol, Epinephrine,
General Principles in Endocrinology Norepinephrine
Classification of Endocrine Glands
Purely Endocrine Partly Endocrine
Endocrine System Nervous System -only secretes hormones -secretes hormones and serve
Regulate body functions and processes other functions
Enable signals from one cell to be transmitted to Anterior Pituitary Gland Nerve Endings
another cell to respond (Adenohypophysis) Trophic Ach, EP
Hormones:
Releases Releases GH, PrL, TSH, ACTH,
Hormones Neurotransmitters FSH, LH
Slower but more Fast but localized Master Gland
diffused Posterior Pituitary Gland Kidneys
(Neurohypophysis) Erythropoietin, Vit. D
Stores and releases
Types of Chemical Messenger System (Mediators) ADH & Oxytocin
Thyroid Gland GIT
T3, T4, Calcitonin Gastrin, CCK, Secretin
1. Neurotransmitter
Parathyroid Gland Placenta
Synthesized in axon terminal, released due to action PTH HCG
potential, NTA released via exocytosis into synaptic Islets of Langerhans Heart
cleft facilitated by calcium Ions. Eg: Ach, Nep Insulin, Glucagon ANP
Adrenal Cortex
MC, GC, Androgen Skin
2. Endocrine Hormones Melanin
Synthesized by Endocrine glands released into body
fluids i.e. circulating blood because target cell is Adrenal Medulla Liver
EP, NEP IGF, VIt. D
located away from secretory cell
Testes Pineal Gland
Testosterone Melatonin
Both a NTA and Hormone: Norepinephrine. Ovaries Hypothalamus
Synthesized in post ganglionic nerve ending and Estrogen, Progesterone Releasing and
Inhibiting hormones
Synthesized by the adrenal medulla.
3. Neuroendocrine Hormones
Synthesized by neuroendocrine cells, released in
circulating blood Eg. Oxytocin & ADH
4. Paracrine
Target cell is located just near the secretory cell Eg.
Insulin & Glucagon
Synthesized by Endocrine gland released in
interstitial fluid
Hormones Secreted by the Hypothalamus
5. Autocrine GHRH (Somatotropin Releasing Factor) (+) GH
Also released in Interstitial fluid, acts on the same GHIH (Somatostatin) (-) GH
cell that synthesized them Eg. Tumor Growth factor PIH (Dopamine) (-) PrL
PRH (+) PrL
6. Cytokines TRH (+) TSH, PrL
CRH (+) ACTH, MSH
Peptides synthesized and released by the cells of
GnRH (+) FSH, LH
immune system
Releasing/Inhibiting Hormone- Hypothalamus
Trophic Hormones- Ant Pituitary
Functions of the Endocrine system
Chemical Homeostasis General Characteristic of Hormones
Fat, CHON, CHO metabolism Secreted by secretory cells called Endocrine Glands
Water and electrolyte metabolism Thrown directly to body fluids, mostly in circulating
Reproduction blood
Estrogen, Progesterone, Testosterone Regulate existing body function or process
Growth Long Latent period and duration of response
GH, TH, Insulin, Progesterone estrogen testosterone Low plasma concentration
Behavior Transport BLOOD
Free= ACTIVE
Page 41 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Protein-bound
Mechanism of Action of a Hormone
INACTIVE
Prolongs plasma half life 1. Hormone Receptor Interaction
Facilitate transport of hormone to a. Receptor
target cell Chemical subunits
Reservoir Most are proteins- can be degraded
Binding proteins are produced by liver, and estrogen or resynthesized
can stimulate the production of such Stereospecific
Main site of Inactivation is in the LIVER, Cleared by
kidneys Up Regulation
o If there is an increase in 1 hormone, this can
Classification According to Chemical Composition increase the number of receptors for itself or
POLYPEPTIDES another hormone
o Eg. Increased Estrogen Increased
production of Oxytocin receptors in
Myometrium
Down Regulation
o (+) Excess hormones , this can decrease
Can be stored, secretion is not continuous, only upon
the number of receptors for itself or another
stimulation
Secretion is via exocytosis facilitated by Ca ions hormone
Soluble, transported in unbound form, shorter plasma half o Increased Progesterone Decreased
life Estrogen Receptor
Cannot cross cell membrane, cannot be given orally
ALL Hypothamalic hormones: GHRH, GHIH, PRH, TRH,
CRH, GnRH, well, EXCEPT PIF/Dopamine Location of Rceptors
Anterior and Posterior Pituitary hormones: ADH, CELL MEMBRANE
Oxytocin, GH etc
Protein
TSH FSH LH Glycoproteins
Peptide
PTH, Calcitonin
Catecholamines
Insulin Glucagon
cAMP Other than
BIOGENIC AMINES cAMP/Phospholipase C/
Synthesized from the Amino Acid Tyrosine whatever
Thyroid Hormones: T3, T4 CRH, GHIH GnRH, GHRH, TRH
Bound to thyroglobulin ACTH, FSH, LH, TSH Oxytocin
Stored, secreted upon stimulation, not HCG, PTH, Calcitonin ADH (V1 receptor in the
continuous. ADH (V2 receptors in the vascular smooth muscle)
Released via exocytosis DCT) Catecholamines (α
99% bounded; 1% free Catecholamines (β receptor)
Can cross cell membrane receptors) A II (vascular smooth
Long halflife Angiotensin II (epithelial muscle)
cells in renal tubules) Insulin
Ep, Nep, PIF (dopamine) Glucagon
80% Ep, 20% Nep, Very small PIF (adrenal
medulla)
PIF produced in hypothalamus and adrenal Cytoplasm Nucleus
medulla Steroid Hormones: Thyroid Hormones
Either bound or loosely bound to albumin Estrogen, Progesterone, T3 , T4
Cannot cross cell membrane Testosterone
Steroid Cortisol, Aldosterone,
Synthesized from Cholesterol Androgens
Lipid soluble, insoluble to circulating blood Vit D
Bound to plasma proteins, long half life
Not stored, whatever is synthesized is also released Regulation of Endocrine Secretion
Can cross cell membrane
Estrogen, Progesterone, Testosterone
Cortisol, Aldosterone, Androgens
1. Indirect Nervous Control
Vit D
Classification According to the Site of Target Cell
Local Hormones General Hormones
Target cell is located Target cell is located far
near the secretory cell from secretory cell
Released in the blood
H-H target gland axis
GI Hormones Thyroid Hormones
Glucagon,Insulin Growth Hormones Ant Pituitary Gland, thyroid, adrenal cortex, ovaries,
(released in Interstitium) Trophic Hormones: Eg. testes
NTA- Ach, Nep TSH
Page 42 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
B. Positive Feedback Mechanism
Excess free hormone from a target gland further
stimulates the hypothalamus and anterior pituitary
gland
Only true for Estrogen
3 Levels of Endocrine Disorders
Primary Target Gland i.e., Thyroid etc
Secondary Anterior Pituitary Gland
ACTH dependent Zona Fasciculata and Reticularis Tertiary Hypothalamus
Aldosterone from Zona Glomerulosa is not ACTH
dependent. It is regulated by RAAS and K.
2. Direct Nervous Control
ADH Oxytocin
Nep, Ep
C. Modified Negative Feedback Mechanism
AKA Physiologic Response Driven Feedback
Independent of the hypothalamus and anterior
pituitary gland
Regulated secondary to a blood metabolite
PTH Calcium Levels
REGULATION OF HORMONE SECRETION
A. Negative Feedback Mechanism
aka Endocrine Driven Axis Feedback
Excess free hormone from a target gland will inhibit Insulin, Glucagon Blood Glucose
the hypothalamus and anterior pituitary gland. Aldosterone mainly Hyperkalemia
Hypothalamus-Long loop; Anterior Pituitary gland-
Short Loop D. Permissive action of a Hormone
Eg.
Hormone A does not act directly on the target cell.
Instead, hormone A increases the production of
hormone B and hormone B will act on the target cell.
ANTERIOR & POSTERIOR PITUITARY GLAND
Bet Cortisol and Androgen, It is mainly excess in Cortisol
In females, Progesterone NFM mainly affects LH
In Females, Estrogen NFM mainly affects FSH (beginning
of monthly cycle)
In Males, Testosterone NFM mainly affects LH ; If
Increased Inhibin FSH is affected
Page 43 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
I. ANTERIOR PITUITARY GLAND
GH REGULATION
Types of Adenohypophyseal Cells
Staining Characteristics
Granular Agranular Chromophobes
Acidophils (40%)
– GH, Prl –ACTH
Basophils (10%)
– FSH, LH,TSH, ACTH
Secretory Activity
Somatotropes GH/STH 50%
Lactotropes Prl, GH 10-25%
(Mammosomatotropes)
Corticotropes (POMC) ACTH, β-LPH 15-20%
Gonadotropes FSH, LH 10-15%
Thyrotropes TSH <10% Controlled via Negative Feedback Mechanism: Inc IGF
1 Ant PG is Inhibited NO GH; and the
A. GROWTH HORMONE Hypothalamus is also stimulated INC GHIH/
Somatostatin Ant PG is Inhibited NO GH (Dual
GH Stimulates Liver to Secrete IGF 1/ Somatomedin
Inhibition);
Maximizes effect in promoting growth
Excess plasma GH Hypothalamus is Inhibited NO
GROWTH HORMONE IGF-1
GHRH Ant PG is Inhibited NO GH
Polypeptide; Specie Major Intermediary of
specific the physiologic action Growth Hormone Release
Uses cytokine receptors of GH Presents diurnal rhythm
(JAK2 and STATs) Regulates cellular Peak secretions before midnight and in the early morning
o STAT = Signal proliferation, Secretion is pulsatile
Transducer and differentiation, and
Activator of metabolism Factors Promoting Growth Factors Inhibiting Growth
Transcription Has autocrine, Hormone Release Hormone Release
Plasma level higher in paracrine, and
Hypoglycemia ;Fasting Hyperglycemia
infants and children than endocrine effects
Exercise Lack of exercise
adults
Increase in plasma level of amino Increase in plasma free fatty acids
Released in a Pulsatile
acids – Protein meal –
manner ARGININE (most effective in
Stimulates the liver to stimulating GH
produce IGF-1 NREM Sleep - (SWS) Deep REM Sleep – (FWS) Light Sleep
Sodium retention Sleep
aka Somatotropin (STH) aka Somatomedin Norepinephrine and α-adrenergic α-adrenergic blockers
agonists
Half life 6-20mins Half-life is about 12 Β-adrenergic antagonists β-adrenergic agonists
hours
Apomorphine and L-Dopa Serotonin Agonist
Hyperglycemic Hormone, Insulin-like Activity
Hormones of puberty (Androgens Chronic intake of steroids
Inc Insulin resistance,
and Estrogens)
Antagonizes insulin effect
on muscle and adipose Stressful stimuli - Fever Somatostatin
Increases lipolysis Anti-Lipolytic Activity Ghrelin – coordinates food intake Increase level of Somatomedin
with growth and Growth Hormone
Directly affects the liver, Secreted by many
muscles, and adipose tissues of the body
tissue but the predominant Important Hormones in Human growth:
Stimulates growth of source is the liver T3 & T4 High during Childhood
human cells, most Mitogenic and have Androgen, Estrogen Puberty only
especially bones and marked effects on STH/GH
cartilages Linear Growth bone and cartilage
Insulin
Promotes protein anabolism, prevents protein catabolism
(+) Nitrogen and phosphorus balance
Epiphyseal growth Growth Abnormalities
Excessive GH
IGF-I is the major form in adults Early Onset (Before Puberty) GIGANTISM
IGF-II is the major form in the fetus Late Onset (After Puberty) ACROMEGALY
GH and IGF Maximized effect if epiphyseal plate is open During Puberty ACROMEGALIC-GIGANTISM
I. Gigantism
Excessive GH before puberty when epiphyseal plate is
still open
Page 44 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
II. Acromegaly B. Melanocyte Stimulating Hormone
Excessive GH after puberty when epiphyseal plate is
already closed Stimulates the melanocytes to produce melanin Even
Complications: distribution
o Diabetes- most common cause of death Adrenocorticotropic Hormone (ACTH)
o Visual deffect Tunnel Vision o Hormone with melanocyte stimulating effect
o Altered Protein anabolism o When present in excessive amount in the
o Hypertrophy of sweat & sebaceous glands blood, skin pigmentation occurs, but it not
o Galactorrhea evenly distributed
o Cardiomegaly, HPN o Affects not only the skin, also the mucosa
o Sexual dysfunction Degree of pigmentation depends on the number of
o Peripheral Neuropathy melanocytes present in your skin, they serves as
o Prominent supraorbital ridge protection for UV rays
o Arthrosis o Lighter Skin: Dec melanocytes Prone to
o Enlarged distal body parts skin CA
Prognathism, Frontal Bossing, Big jaw, o Darker Skin: Inc melanocytes
normal number of teeth, teeth separated,
Large nose, spade shaped hands and feet Recently, it was found out that MSH does not exist,
ACTH is actually the one stimulating the melanocytes
Other Growth Abnormalities to produce melanin, giving it a melanocyte
Tall Stature Endocrine Disorder Tall Stature Non Endocrine stimulating effect
Disorder
Sexual Precocity Cerebral Gigantism Abnormal Skin Pigmentation/Lack of Pigmentation
Thyroxicosis height (Soto’s Syndrome) Albinism – congenital absence of melanin
dec when left untreated Marfan’s Syndrome Piebaldism – congenital defect characterized by patches
Homocystinuria
of skin that lacks melanin
Beckwith-Wiedemann
Syndrome
XYY Syndrome Degree of severity of injury in the Pituitary Gland
Klinefelter’s Syndrome depends on the activity of the Anterior Pituitary
Gland, particularly to the amount of secretions
Dwarfism (Endocrine Disorders) Dwarfism (Non-Endocrine Pituitary Failure (Hypopituitarism)
Disorders) Decrease in the secretion:
Laron Dwarfism Kaspar-Hauser Syndrome Gn (FSH/LH Mild cases
GH insensitivity due to a pyschosocial dwarfism; TSH Mild to moderate
defect in GH receptors seen in neglected and ACTH Moderate to severe
and a marked decrease in chronically abused
GH (STH Severe cases
IGF-1 children
Malnutrition *GTAG
African Pygmies Syndromes of short stature
IGF-1 fails to increase at (Turner’s) II. POSTERIOR PITUITARY GLAND (NEUROHYPOPHYSIS)
the time of puberty; Autosomal Chromosomal
partial defect in GH Disorders (Down’s) Neurohypophyseal Hormones
receptors Produced as prehormones
Glucocorticoid excess Chronic Cardiac/Pulmonary Cosecreted with a peptide – Neurophysin
Disorders Neurophysin I = for ADH
GI/Hepatic/Renal Disorders
Neurophysin II = for Oxytocin
Cretinism Achondroplasia
Thyroid Hormone Autosomal dominant
Deficiency condition wherein there is
A. Anti-Diuretic Hormone (ADH
alteration in fibroblas Aka Arginine Vasopressin (AVP)
growth factor receptor receptors:
o V1a and V1b = Vasoconstrictive Effects (PI
Ca++)
o V2 = Anti-Diuretic Effects (G-Protein
cAMP)
Half-life = 15-20 minutes
For water balance; Facultative reabsorption of water in
late DCT and CD
Location of Receptors
Plasma Osmolality R Organum Vasculosum of the
Lamina Terminalis
Volume sensitive R Subfornical Organs
Thirst Center R Superolateral Part of the
Hypothalamus median
preoptic nucleus
Page 45 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
During labor or parturition for uterine contraction
ADH Regulation Estrogen reduces the membrane potential of
Excitatory Stimuli for ADH Inhibitory Stimuli for ADH uterine smooth muscles, lowering the threshold for
Release stimulation (increase the number of Oxytocin receptor
Increase Effective PCOP (OPPP) Decrease effective PCOP mRNA in the uterus)
1% increase in (OPPP) Uterine effects – inhibited by progesterone
plasma osmolarity
Dehydration Overhydration Effects of Oxytocin
Nausea, Vomiting, Major Effects: Minor Effects:
Diarrhea
Hypovolemia Hypervolemia
Milk ejection in lactation Control of Estrous Cycle
5-10% decrease in BV
Ovarian Steroidogenesis
Warm/Hot Environment Cool/Cold Environment Testicular Steroidogenesis
Nicotine,, Clofibrate, Alcohol Intake Male Ejaculation
Carbamazepine , Angiotensin Induction of parturition Body osmolarity
Pain, Emotion , Stress , (Effective Natriuretic Agent)
Standing , Exercise Lipogenesis
ADH Abnormalities
Thyroid Gland
Butterfly-shaped, located anterior part of the neck on
either side of the trachea
Divided into right and left lobes joined by the isthmus at
appx at the level of the cricoids cartilage
Non-palpable, weighs 15-25g (adult)
Moves up during swallowing due to the thyroglossal duct
Recurrent Laryngeal nerve – located behind TG, commonly
compressed when TG enlarges. Vital in Thyroidectomy, if cut
loss of voice
SIADH Can be seen in patients with cerebral and Funtional unit Thyroid follicles or acini contains
pulmonary diseases
Thyroglobulin, a large glycoprotein molecule and colloid
which stores newly synthesized thyroid hormones
Well vascularised (5ml/g/min) via superior and inferior
thyroid arteries.
Receives sympathetic innervations only regulates
blood flow
Hyperthyroidism blood supply inc (+) Bruit upon
auscultation
BIOSYNTHESIS AND RELEASE OF THYROID
HORMONES
Hypersecretion of ADH
Long surgical procedures secrete excessive ADH
low plasma osm and dilutional hyponatremia water
intoxication so monitor I&O (input & output)
B.
Oxytocin
Synthesized mostly by the paraventricular nucleus
(hypothalamus)
Supra-ADH; Para-Ox
Uses G-protein coupled serpetine receptors which can
increase intracellular calcium levels
Excitatory Stimuli:
Major: Nipple Stimulation Milk letdown
Prolactin Milk production BIOSYNTHESIS: ECF CYTOPLASM LUMEN
Stimulation of reproductive body parts 1. Iodide uptake/trapping
During Coitus acts as vacuum to facilitate sperm to Thyroid Gland can take up and also release Iodides in the
move up, thus fertilization occurs, free ride baby circulating blood
Psychogenic stimuli – baby cries
Page 46 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Thyroid Gland needs 150 ug Iodide; Balance Diet 500 ug Iodide; Albumin Little of T3 & T4
80% excreted via kidneys, 20% taken up by TG Highest plasma conc;
Active Transport: Sodium-Iodide symporter lowest affinity
T3 is more potent and active than T4 i.e. It is mainly in excess of
Iodide (ECF)
T3 causes Negative Feedback Mechanism
REGULATION OF THYROID HORMONE SECRETION
Salivary glands, gastric mucosa, mammary glands, placenta,
choroid plexus, ciliary body capable of transporting of iodides
but do not synthesize TH Hypothalamic-Hypophyseal Thyroid Gland Axis
Competitive Inhibitors = Perchlorate, Nitrate, Thiocyanate & o Major mechanism
Pertechnitate (anti-thyroid drugs)
Passive Transport: Cl-I
o (+) TRH (+) TSH (+) T3, T4
2. Oxidation TRH Uses Phospholipase C as 2nd messenger
nd
TSH Uses cAMP as 2 messenger
3. Organification Wolff-Chaikoff effect
o Autoregulatory mechanism of TG depending on
Iodide availability
o Deficiency/Excess in Iodides Dec Thyroid
4. Coupling/Condensation hormone synthesis
o Eg. (+) Excess iodides Na-I symporter and
Organification is inhibited Dec Thyroid
Thyroid Hormones hormone synthesis Hyperthyroidism is
T4 DIT T3 MIT prevented
Wolf-Chaikoff escape: happens when wolf-chaikoff effect
STORAGE: Colloid, bound to throglobulin persists for several days loss of inhibition Thyroid
Can be able to supply body for 2-3 months hormone synthesis
RELEASE: LUMEN CYTOPLASM ECF TSH + Membrane receptor
1. Endocytosis of Colloid (Pinocytosis) @ apical border
Cytoplasm
2. Proteolysis of thyroglobulin = Free MIT, DIT, T3, T4
(Cytoplasm) TSH stimulates Iodide uptake, oxidation, organification,
3. Deiodination of MIT & DIT coupling, endocytosis, T3 T4 release
MOST IMMEDIATE ACTION: Inc Proteolysis of
thyroglobulin
Iodine product here can either be released or recycled
4. T3 T4 excretion T3 & T4
Synthesized from Tyrosine;
Biogenic Amine, receptors are in the nucleus
Crosses the cell membrane via OAT-P, a carrier protein
o OAT-P 1 Thyroxine/T4
o MCT 8 T3
Acts on all type of cells except Spleen, lens of the eyes
HORMONE TRANSPORT
and Gonads
TBG ( Thyroid Binding T4> T3
PHYSIOLOGIC ACTION OF THYROID HORMONES
Globulin)
Lowest Plasma Conc; Growth Children: Physical and Mental Growth
Highest affinity Growth Hormone Skeletal growth = Soft
tissue growth
Thyroxine Binding Prealbumin T4
Thyroid Hormone Skeletal growth > Soft
(TBPA) /Transerythin
tissue growth
Page 47 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Physical Retardation – can be corrected as Carbohydrate Increased glucose absorption; increased cellular
long as proper diagnosis and treatment is Metabolism utilization of glucose
applied and epiphyseal plates are still open Hyperthyroidism (+) epinephrine induced
Congenital Pituitary Dwarfism glycogenolysis in liver Inc CBG
Hypothyroidism Fat Metabolism Increased lipolysis > increased lipogenesis
> Cretinism Ugly (-) GH Both bones Hypothyroidism Hypercholesterolemia
dwarf, a non and Soft tissue Protein Normal dose anabolic
proportional dwarfism growth is loss Metabolism Hyperthyroidism Hypothyroidism
Bones fails to proportional dwarf Inc Protein Dec Protein
grow, but soft tissue beautiful dwarf Catabolism Dec Anabolism Dec
growth persists (-) Mental muscle strength muscle strength
short stature and Retardation Vitamins Thyroid hormone Conversion of carotene to
limbs, pot belly, small vitamin A
skull, macroglossa
Hypothyroidism Carotenemia
(+) Mental
Adrenal Medulla Increased secretion of EP and NEP Sympathetic
Retardation
adrenergic effects
Mental Retardation- treatable as long as it
is diagnosed and treated before 6 months of THYROID DISORDERS
devt, beyond that, condition becomes Goiter – Enlargement of the thyroid gland
permanent
2 Types:
CNS Increased cerebration, increased synaptic
transmission, increased nerve myelinization o Diffuse Goiter- generalized enlargement
Hyperthyroidism Hypothyroidism o Multi-nodular Goiter- lumpy enlargement
Hyperkinesia, Hypokinesia,
Insomnia, anxious, Sluggish movements GOITER Hyperthyroidism Toxic Goiter
fine tremors and speech, Euthyroidism Non-Toxic Goiter
drowsiness, poor
Hypothyroidism Non-Toxic Goiter
memory, poor
mental ability, low IQ
CVS Increased HR, SV, Increased CO Inc Systolic WHO: CLASSIFICATION OF GOITER
Pressure Stage Goiter Palpable Visible
Increased Heat production Vasodilation Dec 0
TPR Dec Diastolic pressure
1a
Hyperthyroidism Hypothyroidism Even if neck is fully
Palpitaions, Bradycardia, extended
tachycardia, Systolic Hypotension 1b
HPN, wide pulse Includes Only if neck is fully
pressure glands with extended
GIT Increased motility, secretion, absorption nodules
Hyperthyroidism Hypothyroidism 2
Diarrhea Constipation No need Even in normal
position and when
Blood Inc cellular metabolism Inc O2 consumption
near the examiner
hypoxia (+) Erythropoiesis
3
Respi Increased IC activity decreased PO2, increased
Very large No need Even at
pCO2 (+) respiratory center increased RR
gland considerable
Endo Increased metabolism and clearance of various distance
hormones
Bones Increased bone formation and resorption
Hyperthyroidism Hypothyroidism HYPOTHYROIDISM
Resorption>Formation Formation and Dry coarse hair Easy fatigability
resorption dec Goiter Irregular
Bradycardia menstrual cycle
Muscle Normal or physiologic dose of thyroid hormones
Arthritis Weight gain
increase protein synthesis increasing muscle
Cold intolerance Constipation
strength
Dry skin, brittle Myxedema-
Hyperthyroidism Hypothyroidism nails Generalized
Inc Protein Dec Protein Puffy face
Catabolism Dec Anabolism Dec Dull expression
muscle strength muscle strength
Skin CAUSES OF GOITER
Hyperthyroidism Hypothyroidism
Heat Intolerance Cold Intolerance
Diaphoresis Dry skin Primary – Problem in Thyroid Iodine deficiency (endemic
gland goiter)
Body Weight
Goitrogen Intake (cabbage,
Hyperthyroidism Hypothyroidism turnips)
Increased appetite Dec appetite and dec Late stage Thyroiditis /
and also Inc in in metabolism Inc Hashimoto’s Thyroiditis
metabolism Body weight Thyroid Cancer
Decreased body Post Total thyroidectomy
weight Radiation therapy,
Page 48 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
excessive intake of Anti Causes of Hyperthyroidism
thyroid drugs Primary Grave’s Disease (exopthalmic goiter)
Secondary - Problem in TSH deficiency Autoimmune Plasma cells produce TSI
Anterior Pituitary Gland Brain tumor (thyroid stimulating Immunoglobulin)
Tertiary Problem in Hypothalamus Goiter, Inc Thyroid Hormone secretion like
so all is Decreased (T3,T4, TSH
TSH, TRH
Thyroiditis / Hashimoto’s Thyroiditis – Autoimmune disease Solitary Toxic Adenoma- Benign Hormone
causing the plasma cells to produce antibodies that destroy Na-I secreting tumor of thyroid gland
symporter and inhibit peroxidise activity Secondary/ Pituitary Adenoma Inc TSH, T3& T4, dec
In a previously hyperthyroid patient, when treatment is excessive Extrathyroidal TRH, Goiter
Fastidious or Iatrogenic Intake of Exogenous
Hypothyroidism
T3 & T4 – (NOT RELATED TO PITUITARY
MYXEDEMA CRETINISM GLAND) Can cause rare cases of ectopic
Occurs after birth Occurs At birth or before thyroid tissue
Most common in the face Caused by Iodine Tertiary All are Increased
especially around the eyes deficiency on the part of TSI, unlike TSH, is not subject to negative feedback mechanism
Low husky voice the mother; rare cases despite of an increase in T3 and T4 levels, so there is continuous
Carotenemia unknowingly pregnant
production of TSI
Low IQ mom takes antithyroid
Myxedema madness drugs crosses placenta
Hypercholesterolemia depresses fetal thyroid Hyerthyroidism
due to: development T3 T4 TSH TRH Goiter
o low BMR= -40; and Nonproportional dwarf / Primary
st
Inc (1 ) Dec Dec YES
decreased cholesterol ugly dwarf Secondary Inc
st
Inc (1 ) Dec YES
degradation Mental Retardation Tertiary Inc Inc
st
Inc (1 ) YES
Pot Belly
Large Tongue /
Macroglossia Differential Diagnosis of Hyperthyroidism
Deaf & Mute
Short Limbs
Hypothyroidism
T3 T4 TSH TRH Goiter
st
Primary Dec (1 ) Inc Inc YES
st
Secondary Dec Dec (1 ) Inc UNLIKELY
st
Tertiary Dec Dec Dec (1 ) NO
DIFFERENTIAL DIAGNOSIS OF HYPOTHYROIDISM
Normally, Thyroid gland should’ve taken up
TRH CHALLENGE TEST- IV admin of TRH 6hours=15%
Before TRH After TRH 24hours=25%
Hormone T4 TSH T4 TSH
Thyroidal Low High Same Inc TREATMENT
Pituitary Low Low Same Same
Patient is Young, gland is small, and mild disease
Hypothalamic Low Low Inc Inc
Anti-thyroidal drugsBlocks Peroxidase Catalyzed step
HYPERTHYROIDISM/THYROTOXICOSIS in TH synthesis (ano nga ulit yung 3 yun?) Eg:
Hyperfunctioning Thyroid gland Inc Thyroid hormone o Propylthiouracil(PTU)- inhibit peripheral
secretion. conversion of T4 to T3
Clinical Manifestations o Methimazole
Diaphoresis Heat Intolerance Anions Compete with Iodide and blocks first step in
Tachycardia** Insomnia biosynthesis of TH
Goiter Infertility
Radioactive Iodine If drugs are not effective and
Irritability Muscle weakness
Anxious Weight loss gland continues to grow, this will destroy all
Diarrhea Fine tremors of fingers** hyperfunctioning cells; not for pregnant and those with
Inc SBP; Dec DBP Increased Pulse Pressure heart problems
Inc BMR High Output Failure
Pre-tibial myxedema (localized) Exopthalmos If malignant Total Thyroidectomy
Hairloss If Benign Subtotal Thyroidectomy leave 5g
**= Conclusive of
Hyperthyroidism
Surgery even when thyroid is hyperfunctioning Stress
Hypothyroidism Generalized Myxedema common in face
Stimulate further release of TH Thyroid crisis or Thyroid
Hyperthyroidism Localized Pretibial storm Pre op, give Anti thyroid drugs and Iodides and
Beta blocker (minimize sympathetic effect especially on
the heart
Page 49 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Snow Whites’ Favorite >17 mg/dL Ca
(pero i don’t think lalabas to sa finals, pero malay mo!) precipitation may
occur
Tetany CNS depression
o Earliest Sign Dec QT interval
Carpopedal spasm / Tachycardia
Trosseaus sign Lack of Appetite
o Chvostek’s sign Constipation
Diarrhea
ABSORPTION AND SECRETION OF CALCIUM
A After TRH admin in Pituitary Hypothyroidism
Admin of high doses of exogenousT3
Effect of TRH admin to Patient with Pituitary
Hypothyroidism
B Prolonged Iodine deficiency
Admin of high doses of Iodides
After TRH admin in Primary Hypothyroidism
Inc intake of Goitrogens
Admin of high doses of Thiocyanate and Nitrate
Hashimoto’s Thyroiditis (late stage)
Effect of TRH admin to Patient with TPO deficiency With the help of Vit D, Ca absorption in the intestine
C TROLOLOL occurs
D Inc TSI production
Plummer’s Disease Renal Excretion
Hashimoto’s Thyroiditis (early stage) Controlled by PTH
E Pituitary Adenoma 10% or 100mg/day excreted thru urine
Tertiary Hyperthyroidism
o 90% reabsorbed in the PCT, LOH, Early DCT
o 10% late DCT, early CD
Parathyroid Gland PHOSPHATE
Normal value:
CALCIUM o Adults: 3-4 mg/dL
Normal values: o Children: 4-5 mg/dL
o 9.4 mg/dL or 2.4mmol calcium/L Bones 85%
o 8.9-10.1 mg/dL Intracellular 14-15%
Contraction of muscles Extracellular <1%
Blood clotting (Factor IV) 2 forms:
Transmission of nerve impulses HPO4= 1.05mmol/L
Extracellular fluid Intracellular fluid H2PO4= 0.26mmol/L
0.1% of total body calcium 1% of total body calcium Acidic Plasma ↑H2PO4, ↓ HPO4
Most important, if altered, Cells and organelles Alkaline Plasma ↑ HPO4, ↓H2PO4
immediate s/sx manifests
Bones – where the rest of the total body Calcium are Renal PO4 Overflow Mechanism
located 1mmol/L = critical value
Calcium in the Plasma <1mmol/L
Combined with Combined with Ionized o PO4 will be reabsorbed and will not go into the
plasma CHON anionic substances urine.
(citrate, PO4) o All PO4 in the glomerular filtrate will be absorbed
41% (1mmol/L) 9% (0.2mmol/L) 50% (1.2mmol/L or >1mmol/L
2.4mEq/L o excretion is directly proportional to additional
non-diffusible; Most important form PO4
cannot pass through Functional calcium BONE
the capillary Composed of 2 major components:
membrane
Organic matrix Bone salts
Hypocalvemia Vs Hypercalemia 90-95% collagen fibers Compressional strength
Powerful tensile
Hypocalcemia Hypercalemia
strength
↓ Ca ↑ Na entry to the ↑ Ca Ca blocks Na entry 5-10% ground substance 2 major bone salts in the
cell Hyper-excitable cell to the cell No action Chondroitin sulphate body
potential Ca & PO4
Hyaluronic acid
Below 50%: tetanic muscle 12 mg/dL effects Hydroxyapatite form
contraction, seizures begin to appear (crystalline salts)
6mg/dL: Tetany 15 mg/dL marked Others:
4mg/dL: Lethal effects Mg, Na, K, Carbonate
Page 50 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
do not form crystals Osteoblasts for bone deposition; starts to act if (+)
Strontium, uranium, osteoclastic activity; Secretes Osteoprotegerin
plutonium, lead, gold (OPG) competitive antagonist to OPGL no bone
foreign substances that lysis
can form crystal salts and
may cause osteogenic
sarcoma
DEPOSITION AND ABSORPTION OF BONE
Occurs even with normal calcium levels to maintain
PRECIPITATION AND ABSORPTION OF CALCIUM &
equilibrium
PHOSPHATE
For Rearrangement of shape of the bone
For Proper distribution of support of mechanical forces
Ca is found in almost all parts of the body but it is only in
For Renewal of “old degenerated organic matrix”
the BONES that it precipitates.
Bone strength proportion to bone stress
Hydroxyapatite in ECF does not precipitate
o ↑bone usage ↑osteoblastic activity
Pyrophosphate – present in all other tissues; inhibits the ↑thickening of bone
precipitation of Ca and PO4 o ↓bone usage atrophy
o Diminished Pyrophosphate atherosclerosis o ↓bone stress ↓bone deposition ↓bone
strength
MECHANISM OF BONE CALCIFICATION
VITAMIN D
Increase absorption of Ca and PO4 in the gut, bones
(deposition) and kidneys (reabsorption)
Decreases renal calcium and PO4 excretion
For Bone deposition
Forms complex with Retinoid-X receptors
In some cases, the osteoblast doesn’t form
hydroxyapatite become osteocytes or quiescent
osteoids source of osteocytes during emergency
Without hydroxyapatite Bone remains amorphous
will be the source of Ca during rapid dec in Ca levels
BONE RESORPTION
Breakdown and assimilation of components of bone
Happens in cases of chronic hypocalcemia wherein all
amorphous bones are used up to inc Ca
Osteoclasts For Bone resorption
Low Ca PTH stimulate kidneys kidneys will activate
25-Hydroxycholecalciferol to become 1,25-
Dihydroxycholecalciferol binds to Calbindin binds
to calcium for intestinal absorption
↑Calcium levels conversion of Vit D via PTH to active
form is prevented
PARATHYROID GLAND
Situated near thyroid Gland
In cases of thyroidectomy:
o If 1 or 2 parathyroid glands are removed OKAY
o If 3-4 parathyroid glands are removed
hypoparathyroidism
Page 51 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
PARATHYROID HORMONE (PTH) Dec PTH Normal PTH Normal PTH
Controls extracellular Ca and PO4 Dec Ca Dec Ca Normal Ca
Regulates intestinal absorption, renal excretion of PO4, Dec PO4 Inc PO4 Normal PO4
reabsorption of Ca, exchange between ECF and bones
Excess PTH Hypercalcemia RICKETS Affects children
Decrease PTH Hypocalcemia Highly dec PO4; slight dec
Ca
Due to lack of Vit D
EFFECTS OF PTH ON CA AND PO4 Causes Tetany and Weak
Increase calcium and phosphate resorption from bone bones
and Inc reabsorption of Ca in Late DCT, CT, Early CD and
Asc LOH Inc Serum Ca levels OSTEOMALACIA Fat Malabsorption No
↑PTH ↑osteoclastic activity Bone resorption Inc Vit D absorption Low
Serum Ca Serum Ca and PO4 Inc
↑PTH ↑ renal excretion of PO4 in PCT Dec Serum Osteoclastic activity (bone
PO4 resorption) Osteoblast
Others: compensates: forms new
bone and new cells for
↑ reabsorption of Mg and H ions bone growth BUT,
↓ Na, K and amino acid ions remember, Ca and PO4
* Bones levels are decreased No
1. RAPID PHASE 2. SLOW PHASE hydroxyapatite Weak
bones
PTH causes rapid removal of salts Activated osteoblasts and
from amorphous bone crystals osteocytes send signals to
osteoclasts Osteoporosis Sedentary lifestyle No
bone stress Inc
Acts more on the amorphous Osteoprotegerin Ligand (OPGL) is
osteoclastic activity
bones secreted stimulates osteoclast
bone atrophy
to mature bone resorption
Congetinal Hypophosphatemia Vitamin D resistant rickets
Failure to reabsorb PO4 by
Control of PTH by Calcium the renal
Dec Ca Inc PTH prolonged Parathyroid gland tubules
hypertrophies Eg. Rickets and pregnancy May present as
Inc Ca (Diet high in Ca, prolonged sun exposure etc) hypoparathyroidism
Dec Parathyroid gland activity atrophy May lead to osteomalacia
CALCITONIN Calcium, For the
PREGNANCY & LACTATION developing baby and as a
Peptide hormone from thyroid gland
component of breast milk
Opposite effects of PTH Dec Ca and PO4 Management: Inc Ca
↓ absorptive activities of osteoclasts and↓ formation of intake prevents
osteoclasts secondary
Effect is weak in humans hyperparathyroidism
HYPERPARATHYROIDISM
PRIMARY SECONDARY
HYPERPARATHYROIDISM HYPERPARATHYROIDISM
Hypersecretion of PTH Extreme Chronic Hypocalcemia
osteoclastic activity Osteoblast Hypersecretion of PTH
compensates Inc alkaline
VIt D and Calcitonin works, in contrast with the other. PTH, phosphatase
on the other hand Increases INTESTINAL absorption of both Causes: Causes
Ca and PO4 but, in the bones it only resorps Ca and in the Adenoma/carcinoma Chronic renal disease
kidneys, it only reabsorbs Ca. So, overall effect of PTH Inc Von Reckling Hausen’s Rickets / Osteomalacia
Serum Ca, Dec Serum PO4 disease Pregnancy and lactation
PTG Hypertrophy
CLINICAL CONSIDERATIONS: S/Sx S/Sx
High Serum Ca , Low Low Serum Ca , High
HYPOPARATHYROIDISM
Serum PO4 Serum PO4
TRUE PSEUDOHYPOPARAT PSEUDO- Brittle bones
HYPOPARATHYRO HYROIDISM PSEUDOHYPOPARA Osteitis fibrosa cystic
IDISM THYROIDISM Calciuria, Phosphaturia
Causes Resistance to Genetic Renal lesion
Hypoplasia/ PTH; Biologically defects Nephrolithiasis &
Congenital inert PTH o Short stature Nephrocalcinosis
absence of Circulating PTH o Round face PARATHYROID POISONING
PTG inhibitors o Short metacarpals
Accidental Auto-antibodies Extreme elevation of PTH rapid Inc of Ca & PO4
o Ectopic bone
removal of to PTH receptor -knuckle knuckle hydroxyapatite develops outside bone Metastatic
PTG Kidneys do not dimple dimple sign calcification in alveoli, Kidney tubules, stomach, arteries
respond to PTH
Page 52 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
ADRENAL PHYSIOLOGY EXCRETION
Degraded in Liver and Kidneys
ADRENAL GLANDS Mainly in liver by conjugation with glucoronic acid and
4gms; lies at superior pole of both kidneys sulphate
2 Parts: 25% feces || 75% urine
Adrenal Medulla
Secretes Catecholamines Epi & NorEpi GLUCOCORTICOIDS
Functionally related to Sympathetic NS 1. Cortisol (95%)
Adrenal Cortex Aka Hydrocortisone
Secretes Corticosteroids: Primarily affects glucose metabolism
Mineralocorticoid– Aldosterone
MOST IMPORTANT GLUCOCORTICOID
Glucocorticoid- Cortisol
Sex Androgens 2. Corticosterone
3 layers: 3. Deoxycorticosterone
Zona Glomerulosa – Aldosterone 4. Aldosterone mainly mineralocorticoid
Zona Fasciculata – Mainly Cortisol
Zona Reticularis – Mainly Androgens REGULATION
Whatever happens to Glomerulosa, happens only in STRESS Major Stimulus for secretion of CRF
Glomerulosa, Fasciculata and Reticularis is not
(Corticotropin Releasing Factor) in Hypothalamus
affected.
APG is stimulated releases ACTH adrenal cortex is
stimulated Cortisol is released
ADRENAL STEROIDOGENESIS
Negative feedback Mechanism: Inc Cortisol APG
Parent Compound of all human steroids and Hypothalamus is Inhibited
CHOLESTEROL
Major contributor for cholesterol Plasma LDL EFFECT OF ACTH TO ADRENAL CORTEX
Rate Limiting Step: Cholesterol Pregnenolone by the Main stimuli of Adenylyl cyclase ACTH
enzyme cholesterol desmolase or cytochrome P450 cAMP acts as second messenger (receptors are in Cell
sidechain cleavage enzyme membrane) and it stimulates cholesterol desmolase for
the conversion of cholesterol to pregnenolone
ADRENAL STEROID HORMONES
CIRCADIAN RHYTHM Supraoptic nucleus
NATURAL STEROIDS Guides release of CRF, ACTH and Cortisol
CORTISOL o Highest in early AM
Highest Plasma concentration o Lowest in late evening
Major glucocorticoid activity (but same Interpret cortisol levels base on sleep cycle, if you
Mineralocorticoid activity)
change sleep pattern cycle changes too.
Effect is best achieved when dose is high
ALDOSTERONE
Highest mineralocorticoid activity GLUCOCORTICOID FUNCTION
Lowest Plasma concentration 1. Gluconeogenesis (synthesis of Amino acid to
CORTICOSTERONE glucose)
Little mineralocorticoid and glucocorticoid activity Main effect
Increase in enzymes of gluconeogenesis
SYNTHETIC STEROIDS Mobilizes amino acids from extrahepatic tissue
Dexamethasone Highest glucocorticoid activity; no
Mineralocorticoid activity 2. Dereases Glucose utilization
Prednisolone little glucocorticoid activity; little Dec oxidation of NADH to NAD+; (-) NAD+ No
Mineralocorticoid activity
glycolysis
Methyl Prednisone little glucocorticoid activity; no
Mineralocorticoid activity
3. Diabetogenic
Gluconeogenesis + dec Glucose uptake = Inc Blood
sugar
Excess cortisol Insulin is also inhibited Adrenal
Diabetes
Binding Proteins To prevent rapid fluctuations and as
reservoir CORTISOL ON PROTEIN METABOLISM
Reduces Cellular protein in all body cells EXCEPT
LIVER
Inc Protein Catabolism
Dec Protein Anabolism
Page 53 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Dec Amino acid transport to Extrahepatic Bone Resorption Osteoporosis
tissues Excess cortisol Mineralocoid activity water
To Liver and Plasma Proteins retention water toxicity
Inc Amino Acid transport to liver Deficient Cortisol ADH effect is potentiated water
Inc Mobilization of Amino Acid from retention water toxicity
extrahepatic tissues
MINERALOCORTICOID
Aldosterone
Secreted by Zona Glomerulosa
HIGHEST Mineralocorticoid activity
Cortisol has the same Mineralcorticoid and
glucocorticoid activity
CORTISOL ON FAT METABOLISM
For Na Reabsorption and K secretion
For Fatty acid Mobilization from adipose tissues
Cells cannot utilize glucose Glycerophosphate REGULATION OF ALDOSTERONE SECRETION
is not produced Inc Free FA in plasma Inc 1. MAINLY STIMULATED BY: HYPERKALEMIA
glucose for energy 2. Angiotensin 2 (next of importance)
Oxidation of Fatty Acids in cells 3. Very Slightly inhibited by Hypernatremia
Stimulates appetite, more generation of fats than ACTH is necessary for aldosterone secretion but has
mobilization Central obesity, Moon Facie, Buffalo
little or no effect in its regulation
hump, Thin extremities
(+) STRESSOR = (+) CORTISOL RELEASE
FUNCTIONS OF ALDOSTERONE
ANTI INFLAMMATORY EFFECTS OF CORTISOL
Inc Renal tubular reabsorption of Na and secretion of
Sometimes, Inflammation is more damaging than the
K in principal cells of DCT and CD
trauma itself
Inc Tubular cells secretion of H in Intercalated cells
Infection/Trauma Causes Tissue Inflammation may
Principal K (Principal cells K )
cause tissue and even organ destruction Give
Inter-H (Intercalated cells H)
Corticosteroid Suppress Immune system prevents
Excess aldosterone Inc ECF (5-15%) and arterial
and suppresses Inflammation Rapid healing
pressure (20-25 mmHg), Slight only because of
Aldosterone Escape
FIVE MAIN STAGES OF INFLAMMATION
Stage 1-4 is blocked by Cortisol ECF and Arterial Pressure Inc atrium senses
increase in Venous return ANP is released
causes Pressure diuresis or Pressure Natriuresis
(Aldosterone Escape)
Only Slightly increases Na levels bec if you can
remember, where Na goes water follows, there is
concomitant water reabsorption, so Na is diluted
immediately
ANTI INFLAMMATORY ACTION OF CORTISOL Excess Aldosterone Inc K secretion Hypokalemia &
Muscle weakness
Depolarization – all K will exit causes very negative RMP
(hyperpolarization) Harder to reach critical firing level
manifest as Muscle weakness
Excess Aldosterone Inc H secretion Inc Blood pH
Metabolic Alkalosis
Phospholipase A2 – Parent compound of Leukotrienes and
prostaglandin productions.
Too Little Aldosterone K is not secreted
Hyperkalemia and Cardiac toxicity
Cortisol Inhibits Phospholipase A2 No Leukotrienes
and PG’s No inflammation
Depolarization – K will not go out RMP negativity is
decreased (hypopolarization) Easier to reach critical
firing level cell is more excitable Cardiac
OTHER EFFECTS OF CORTISOL toxicity
Blocks Inflammatory response to allergic rxns Too little Aldosterone H is not secreted Dec pH
Dec # of Eosinophil and lymphocyte Metabolic Acidosis
Stimulates Erythropoiesis Inc RBC Aldosterone causes Na retention during period of
Dec Cortisol Anemia sweating and/or salivation (sweat and salivary glands)
Excessive Cortisol Polycythemia Aldosterone for Intestinal reabsorption of Na
Enhances production of Surfactant by stimulating Type 2 (colon) prevents Diarrhea
pneumocytes necessary for lung maturation
When administering steroid injections to mother,
WOF inc blood sugar level, give insulin if Increased
CBG
Page 54 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
CELLULAR MECHANISM OF ALDOSTERONE ACTION Susceptibility to stress Hyponatremia
Aldosterone is a steroid Receptors are in Cytoplasm and Infection Dec K secretion
Hyperkalemia
o ACTH receptor is in Cell membrane utilizing H retention Metabolic
cAMP acidosis
POMC (proopiomelanocortin) Parent compound of Primary Hypoadrenalism / Addison’s disease Dec Cortisol
ACTH , MSH, B-Lipotropin and Endorphin Secretion APG compensates Inc POMC Inc ACTH Increased
If ACTH is released so are its siblings (haha) Melanin Pigmentation “bronze skin appearance”
ABNORMALITIES OF ADRENOCORTICAL SECRETION
TREATMENT FOR Hypoadrenalism/Addison’s disease:
Most Important Give aldosterone to prevent
HYPERADRENALISM AKA CUSHING’S SYNDROME hypovolemic shock
Hyper secretion of cortisol Hypercortisolism Cortisol administration
CAUSES
Primary : (Inc Cortisol, Dec ACTH)
PRIMARY ALDOSTERONISM AKA CONN’S SYNDROME
Adenoma of Adrenal Cortex
No secondary cause bec APG doesn’t care about Zona
Secondary (Inc ACTH , inc Cortisol dec CRF)
APG Adenoma most common cause glomerulosa
Tertiary (Inc CRF, Inc ACTH, Inc Cortisol) Primary cause Tumor in Zona Glomerulosa
Abnormal hypothalamic function Effects of too much Aldosterone
Others: (di ko kasi macategorize kung primary or what) Hypokalemia weakness and paralysis
Ectopic ACTH secretion from tumour (lung Slight Hypernatremia
tumor) Slight Inc in ECF
Prolonged steroid therapy exposure Constantly Elevated BP
S/Sx: Diagnosis
Central Obesity Inc Aldosterone, Dec Renin:
Moon Facie Tumor in Zona Glomerulosa Inc Aldosterone
Buffalo hump Negative feedback mechanism Renin
Inc Androgen Hirsutism and Acne, oily face should decrease
Cortisol has mineralocorticoid activity Water Treatment:
retention Hypertension Surgical Resection of tumor
Inc Gluconeogenesis dec Glucose cell Medical:
utilization Inc Blood sugar Epleronone
Dec extrahepatic tissue proteins Muscle Spinorolactone
weakness, striae, Susceptibilty to infection Aldosterone Receptor blocker
Inc Bone resorption Osteoporosis
Treatment: FAQ’s/MLAQ’s
Surgery If pituitary adenoma pituitary resection ACTH receptor Cell membrane
Transphenoidal hypophysectomy Steroid receptors (cortisol, estrogen, Cytoplasm
Adrenal Adenoma resection of Adrenal cortex aldosterone etc)
Layer that secretes Aldosterone Zona Glomerulosa
Rate limiting step of Corticosteroid Cholesterol to
production Pregnenolone
Highest Natural Glucocorticoid Activity Cortisol
Highest Synthetic Glucocorticoid Dexamethasone
Activity
Highest Glucocorticoid Activity Dexamethasone
Highes Plasma Glucocorticoid conc Cortisol
HYPOADRENALISM AKA ADDISON’S DISEASE Cause of obesity in Hypercortisolism Inc Appetite
More dangerous than Cushings Most potent stimulus in Aldosterone Hyperkalemia
Dec secretion of Adrenocortical hormones secretion
Glucocorticoids and Mineralocorticoids Amino acid of Epi and NorEpi Tyrosine
What adrenal condition causes Addison’s / Primary
Hyperpigmentation Hypoadrenalism
What causes this Hyperpigmentation Inc ACTH
Target organ of aldosterone Kidney DCT and CD
Cortisol is highest at Early morning
Most common cause of Cushing’s Pituitary Adenoma
Glucocorticoid deficiency S/Sx: Mineralocorticoid
S/Sx
deficiency Pancreas
Composed of: Head, Body and Tail
Hypoglycemia Inability to reabsorb Na 2 Major types of tissue
Dec amino acid and fat and water dec CO and o Acini cells- secretes directly @ duodenum
mobilization Dec BP hypovolemic
o Islets of Langerhans
metabolic functions shock death
Weakness and Inc Reduced Na reabsorption
Page 55 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Secretes hormones directly into glucose uptake muscles, adipose and
bloodstream, it has capillary network other tissues
GLUT 5 *Fructose transport Jejunum, Sperm
Cell types: GLUT 6 LALALA LALALA
Cell Secretion Function Overall effect GLUT 7 *Glucose 6 Phosphate Liver and other
type % transporter in ER tissues
Alpha 20 Glucagon Stimulate Inc Hepatic glucose
Proglucagon Beta and production,
Delta cells Opposes Glycolysis = Inc INSULIN ON CHO METAB
Blood Glucose Muscle glucose uptake and metabolism
Beta 75% Insulin Inhibits Inhibits peripheral o Remember:
C peptide Alpha cells glucose uptake, oppose
during much of the day, muscles
Proinsulin glycogenolysis and
gluconeogenesis = Dec depends on fatty acids for energy
Blood Glucose source
Delta 3-5% Somatostati Inhibits Inhibits Intestinal glucose Normal resting muscle is only slightly
n Alpha and absorption = Dec Blood permeable to glucose except when
Beta cells glucose stimulated by insulin
F <2% Pancreatic Inhibits Direct Pancreatic effect In bet meals, amount of glucose is too
polypeptide Beta and small to promote significant glucose
Delta cells entry into the cell
o Muscles use large amount of glucose during:
INSULIN Moderate or heavy exercise
Secretion: Proinsulin is cleaved C peptide dissociates Few hours after meal: Inc Blood
leaving behind 2 Amino Acid Chains: Alpha and Beta glucose Inc Insulin secretion
subunits Connected via Disulfide linkages o If muscle is not exercising after meal:
Insulin Receptors: Abundance of glucose transported in
muscle cell Glucose is stored as
2 Alpha Subunit 2 Beta Subunit Muscle glycogen
External portion Cytosolic Portion Insulin increases the rate of transport of glucose into resting
(+) Hormone binding (+) Tyrokinase activity muscle cell for at least 15 folds. Without insulin, no matter
domain When occupied, how high your extracellular glucose is, glucose cannot enter
receptor phoporylates the cell. Insulin facilitates this Uptake.
itself and other
proteins Peripheral Glucose uptake via Facilitated diffusion
o Insulin receptors causes insertion of glucose
Mechanism transporters in the membrane, eg:
Insulin Binds to Alpha subunits Because of the disulfide linkages Adipose tissues
(bet Alpha and Beta), The beta subunit becomes autophosphorylated Resting skeletal muscle
activation of local tyrosine kinase Phosphorylation of multiple Insulin acts by enhancing glucose metabolism
intracellular enzymes including IRS or Insulin-receptor substrates Glucose can enter working muscles without aid of
Translocation of multiple intracellular vesicles to the cell membrane insulin
the vesicles carry glucose transport proteins, which binds with cell Other tissues not affected by Insulin:
membrane glucose uptake into cells Nervous tissues- eg. Brain
Kidney tubules
Glucose Transporters Intestinal mucosa
a. Secondary Active Transport RBC
-Na-Glucose Co transport B cells of pancreas
-Energy dependent Liver – but it accelerates the uptake
SGLT1 SGLT2 EFFECT OF INSULIN TO LIVER
For absorption in Small For Absorption if Renal Anabolic effects:
Intestine and Renal Tubule Tubule o Glycolysis Glycogen storage
Anti-catabolic effects:
b. Facilitated diffusion o Inhibits Glycogenolysis No glucose release
-No need energy o Inhibits Gluconeogenesis no glucose
generation
Transporter Function Present in For liver glucose uptake, storage and use. Mechanism:
GLUT 1 *Basal glucose uptake Placenta, BBB , RBC, o Insulin Inhibits Phosporylase prevents
Kidneys, Colon, etc glycogen breakdown glycogen remains
GLUT 2 *B cell Sensor B cells of islets of stored in liver cells
*Insulin independent langerhans, Liver, o Insulin Enhances glucokinase for
*Transport out of Epithelial cells of phosphorylation of glucose to glucose 6
intestinal and renal small intestines, phosphate and for stimulating glycogen
epithelial cells Kidneys synthase for glycogen synthesis
GLUT 3 *Basal glucose uptake Brain, Placenta, NET EFFECT: Increase Glycogen upto 5-6% of liver
Kidneys, Etc mass or 100g of stored glycogen in the liver
GLUT 4 *Insulin stimulated Skeletal and cardiac
Page 56 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
WHEN GLUCOSE IS RELEASED FROM THE LIVER Promotes storage of CHO, CHON and fats
Decreased blood glucose Pancreas decreases Insulin release Inhibits catabolism of proteins ; decreases amino acid
Reverse effects: Stops Glycogen synthesis in liver, prevents release from cells especially muscle cells
further glucose uptake. In the liver, depresses gluconeogenesis plasma
amino acids are conserved or stored
Inc Glucagon + Dec Insulin Phosphorylase is activated Without Insulin
Glycogen is broken down into Glucose 6 phosphate Inc o Protein depletion &Increased Plasma Amino
Blood Glucose acids Increase protein catabolism, decrease
protein anabolism
Dec Insulin Glucose 6 phospatase is stimulated phosphate o S/sx: Protein wasting, Extreme weakness and
radical splits away from glucose free glucose in blood Deranged organ functions
INSULIN ON FAT METABOLISM INSULIN AND GH
Promotes Fat Synthesis and storage Interacts synergistically for growth when given
Fat sparer simultaneously Dramatic Growth
Factors that lead to Increase Fatty acid synthesis: Both promotes cellular uptake of different selection of
o Inc glucose transport into liver cells when amino acids which is required for growth
the 5-6% limit is reached Glycogen synthesis
is inhibited; Glucose splits into pyruvate INSULIN AND POTASSIUM
Converted to Acetyl Coa ( precursor to lipid Insulin Increases NaK ATPase pump in most tissues
synthesis FAT FORMATION pumps K into the cell
Excess Citrate and Isocitrate o For acute life threatening hyperkalemia
Direct effect of activating Acetyl Coa Carboxylase
For carboxylation of Acetyl Coa Forms Malonyl PRINCIPAL ACTIONS OF INSULIN
CoA (1st stage of FA synthesis) FA synthesis RAPID (secs) INTERMEDIATE (mins) DELAYED (hrs)
Liver produces Lipoproteins Inc Triglyceride levels
Inc transport of: (+)Protein Inc mRNA for
in blood Lipoprotein lipase is activated Glucose Anabolism lipogenesis
Triglyceride is broken down into Fatty acids and Alpha Amino acids (-) Protein
Glycerol Phosphate Hormone Sensitive lipase is K Catabolism
Activated Triglyceride is formed, the storage form (+) Glycolysis
of fats in adipose tissues (-)Gluconeogenesis
Insulin is Lacking : MECHANISM OF INSULIN SECRETION
Hormone sensitive lipase is inhibited (+) release of Primary Insulin Controller: Increased Blood glucose
fatty acids from adipose into circulating blood Concentration Glucose influx thru GLUT2 receptors of
Storage of FA is almost blocked Beta cells once inside, glucose is phosphorylated to G6P
by Glucokinase (rate limiting step) G6P is oxidized to form
Promotes Lipolysis Release of Free FA this ATP ATP-sensitive K channels of the cell is inhibited K
becomes main energy substrate used by all tissues channel closes and depolarizes cell membrane Voltage
EXCEPT THE BRAIN gated Ca channel opens Ca influx (+) fusion of docked
Increases Plasma Cholesterol and Phospholipid insulin containing vesicles with cell membrane Insulin is
Concentrations worsens Atherosclerosis especially excreted in ECF via exocytosis
in people with uncontrolled DM
(+) use of fat as energy substrate Ketosis and REGULATION OF INSULIN SECRETION
Acidosis may lead to coma and DEATH INCREASE DECREASE
Inc Blood glucose Dec Blood
Insulin promotes glucose transport through cell Inc Plasma FA glucose
membrane into the fat cells|| Some glucose is used to Inc Plasma Amino acids Fasting
form large Quantities of Glycerol Phosphate B adrenergic Act Somatostatin
o Glycerol Phosphate Supplies Glycerol Glucagon, Ach A adrenergic Act
Combines with FA forms TRIGLYCERIDES, GI hormones: Secretin, Norepinephrine
stored in Adipose tissues Gastrin CCK, GIP Epinephrine
GH, cortisol (alpha
With Insulin Without Insulin Parasympathetic receptors)
Hormone Present Absent stimulation
Senstitive lipase Insulin resistance, obesity
Phospholipids Decrease Increased Sulfonylurea drugs:
Ketone Bodies Negative Positive Glyburide, Tolbutamide
INSULIN ON PROTEIN METABOLISM & GROWTH Amino Acids strongly potentiates glucose stimulus for
For transport of amino acids into the cells insulin secretion
Increases translation of mRNA forming new proteins GI hormones only moderately increases insulin
Turns on Ribosomal machinery secretion, Anticipatory release
Increases rate of transcription of selected DNA Glucagon, GH, cortisol, Progesterone estrogen may
genetic sequences in the cell nuclei increases RNA increase risk of DM development when secretion is
quantiyties and protein synthesis large in quantity and prolonged
Page 57 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
CCK and Gastrin) * FFA,
INCREASED BLOOD GLUCOSE *=same with Insulin Ketones
When blood glucose increases 2-3x normal:
Plasma Insulin Increases 10-fold within 3- SOMATOSTATIN
5mins Secreted by delta cells
Then decreases about halfway back toward Remember: delta cells inhibits Alpha & Beta cells
norm n another 5-10 mins Hypoglycemic
At about 15mins, insulin rises (even higher Inhibits Intestinal glucose absorption
nd
than the initial) the 2 time and reaches Inc secretion when:
plateau in 2-3hours Inc Blood glucose
Inc Blood glucose Inc Insulin Secretion Inc Increase amino acids and Fatty acids
glucose transport into liver, muscle and other cells Inc GI hormones concentration
Dec blood glucose concentration to normal Inhibitory effects
Acts locally by suppressing within the Islets
ROLE OF INSULIN IN SWITCHING BETWEEN CHO and LIPID of langerhans dec secretion of insulin and
METABOLISM glucagon dec utilization of absorbed
Insulin promotes CHO utilization for energy and nutrients by the tissues prevent rapid food
depresses fat usage exhaustion makes food available for
Low blood glucose Insulin is inhibited Fat is longer time
used (except the brain) Decreased pancreatic polypeptide secretion
High blood glucose Insulin is stimulated CHO is Inhibits secretion of GIT hormones and dec
used instead of fats blood flow to GIT Decreases GI motility
GH and cortisol Extend period of time over which food
secreted during periods of hypoglycaemia nutrients are assimilated into the blood, dec
both hormones inhibits cellular utilization of CHO absorption and Inc water and
glucose (no glucose uptake) Slow effect: electrolyte absorption
Fat utilization APG Inhibits GH and Thyrotropin Secretion
Epinephrine
Enhances fat utilization during periods of
stress: exercise, anxiety, circulatory shock etc IMPORTANT
Stress Epi release Inc plasma glucose Normal Person
conc and a greater Inc in Plasma FA Fasting Blood Glucose = 80-90 mg/100 ml of blood
st
concentration 1 hour conc increases to 120=140mg.100 ml of blood
Within 2 hours goes bact to controlled levels
GLUCAGON
Starvation
Large polypeptide hormone; Molecular weight: 3485 Gluconeogenesis provides glucose to maintain blood
with 29 chains of amino acids glucose levels
Secreted by Alpha cells
Primary target LIVER DISORDERS OF GLUCOSE METABOLISM
Skeletal muscle is not a target tissue of this hormone DIABETES MELLITUS
Hyperglycemic hormone Syndrome of disordered metabolism (+)
Half life: 5-10 mins inappropriate hyperglycemia, secondary to
Degraded mainly by liver Defects in insulin production
Autoimmune beta cell destruction
Mechanism: Insulin insensitivity or resistance
Glucagon Activates Adenylyl cyclise Activates cAMP Impaired action of insulin on target tissues
Phosphorylase B is converted to phosphorylase (+) Due to either an absolute deficiency of insulin
Glycogenolysis Glycogen is broken down into glucose Inc secretion or reduction in biologic effectiveness of
Blood Glucose insulin or BOTH
Diagnostics:
Actions: Fasting Blood Sugar (FBS)
Inc Glycogenolysis No caloric intake for atleast 8 hours, no water
Inc Gluconeogenesis intake
Inc Ketogenesis OGTT
Inc Ureagenesis (+) fasting
Inc Insulin secretion 3 blood extractions
Inc Lipolysis a.Get fasting blood levels
Decrease Lipogenesis st
b.1 hour after drinking 100 or 75g
glucose drink blood glucose is as
Regulation: expected, high
Increase secretion Decrease c.2
nd
hour after goes back to
Inc Blood Amino Acid (alanine, arginine) * Inc Blood glucose controlled level
same with Insulin* (+) insulin and
Exhaustive exercise somatostatin
Beta adrenergic stimulation (via cAMP) secretion
Vagal Stimulation Secretin
Page 58 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
RBS or Random Blood Glucose Always protect foot and check for any wounds as
Should not be more than 200mg/dL patients may not feel pain and since there is delay in
wound healing prone to infection + ischemia
Hb1ac or Glycosylated Hgb gangrene
shows the average level of blood glucose over the
previous 3 months
It shows how well you are controlling your diabetes
HYPOGLYCEMIA
Insulinoma
(+) DM if Adenoma of islets Excessive insulin production
Hb1ac = Greater than or equal to 6.5%
10-15% malignant administer 1,000g of glucose
FBS= Greater than or equal to 126 mg/dL (7 mmol/L)
OGTT= Greater than or equal to 200 mg/dL (11 mmol/L) every 24 hours to prevent hypoglycaemia
RBS= Greater than or equal to 200 mg/dL (11 mmol/L) Insulin Shock and Hypoglycemia
Do repeat testing to confirm Blood glucose falls to
50-70 mg/dL CNS becomes excitable
TYPE 1 VS. TYPE 2 DM Hallucinations, extreme nervousness,
TYPE 1 TYPE 2 trembling, cold sweat, Tachycardia,
AKA Juvenile onset DM, Non Insulin Weakness, Apprehension, Hunger
Insulin dependent dependent DM 20-50 mg/dL Clonic seizures, loss of
DM consciousness, confusion, drowsiness,
Age Of onset Usually <20 y/o Usually >30 y/o diplopia, headache
Body Mass Low to normal Obese <20 mg/dL Seizure stops Comatose
Plasma Insulin Low or absent Normal to High death
initially
Treatment:
Plasma Glucagon High, can be High, resistant to
suppressed suppression
Immediate IV large quantities of glucose
Insulin sensitivity Normal Insensitive or
(D50-50)
reduced Glucagon
Therapy Insulin, Lipid Diet, exercise, oral Epinephrine
Lowering drugs hypoglycaemic Hard candies, Juice
agent, Lipid lowering
drugs
Insulin (latter part of
disease progression)
Ketosis prone Positive Negative
Ketosis is due to glycogen and protein breakdown
Other factors that can cause Insulin resistance in type 2 DM
o PCOS/ Polycystic Ovarian syndrome
o Cushing’s syndrome
o Excess GH Acromegaly
Metabolic Syndrome
(+) if 3 out of 5 of the ff:
Insulin resistant
Fasting Hyperglycemia
Lipid Abnormalities Inc Triglycerides, Dec
HDL
Hypertension
Inc Abdominal circumference
Gestational Diabetes
High blood glucose occurring during pregnancy
s/sx: Polyuria, Polyphagia, Polydipsia
Rapid weight loss and asthenia, always feels
sleepy, dehydrated etc
Complications of DM
Tissue Injury
Inc risk for heart attack, retinopathy and
blindness, ischemia of limbs Gangrene
Peripheral neuropathy and ANS dysfunction
Impaired CVS reflexes, bladder control,
dec peripheral sensation, and other
symptoms of nerve damage
Hypertension due to renal injury Antok ka na?
Atherosclerosis die to abnormal lipid
metabolism
Page 59 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
VISION 1 Posterior Pole, the area of Retina with most acute vision,
within it is a depression called
Fovea Centralis, the more specific area of most acute
LAYERS OF THE EYE vision because of 1:1:1 photoreceptor interneuron Ratio,
Fibrous Layer/Coat that is 1 Photoreceptor (rods and cones) synapses with 1
Outermost layer Bipolar cell which will also synapse with 1 Ganglion cell,
Made up of: there is direct impulse to brain plus there is no Rods, no
1/5 anteriorly Cornea blood vessels, Contains Densely packed Cones
4/5 Posteriorly Sclera GREATEST VISUAL ACUITY
Vascular or Muscular Layer/Coat
Middle layer 3-4mm away from Fovea centralis Optic nerve exits,
Contains Stored Vit A which goes 15 degrees Medialwards or toward nasal
Made up of: side of eyeball forming now your Optic Disc or
On the posterior side, Choroid, which is extended papilla
anteriorly. (+) Blood vessels, and melanin pigments o Contains axons of ganglion cells
from dark brown, light brown, gray, blue , as is seen in o No Photoreceptors Action Potential
the Iris. cannot be generated BLIND SPOT
Expansion of the Choroid Ciliary Body Retina terminates anteriorly as Ora Serrata
o Ciliary muscles – intrinsic muscle, Origin o No photoreceptors
is on Medial side or inner portion, Inserts
on Lateral side or outer portion Using Opthalmoscope Find the orange or yellowish portion
o Ciliary Process – outside part, secretes Red Reflex At its most center portion is your Fovea
Aqueous Humor Centralis
Ciliary Process contains Zonules or Ligaments that An absent or reduced red reflex indicates an opacity of the
helps hold the lens. cornea (infection or scar), lens (cataract), or vitreous
REMEMBER: hemorrhage.
Ciliary muscles Contract it is pulled toward Medial Side Suspensory Ligaments and Ciliary muscles determines shape
loosens Suspensory Ligament Lens Thickens or becomes of the lens
rounder stronger lens (+) or increased Light bending
COMPARTMENTS OF THE EYEBALL
Ciliary Muscles Relax pulled toward Lateral side Iris
Stretches or tightens Suspensory Ligaments Lens thins or o Like in the Choroid, it Contains Deposited
flatten, dec curvature weaker lens (-) or dec Light
melanin pigments
Bending
o Opaque, Colored portion of the eye
o (+) Radial and Circular muscles (discussed
Ciliary Body narrows anteriorly Iris, gives color to
earlier)
the eyes. Contains:
o Regulates Light entering in the pupil
o (+) RADIAL or dilator pupillae muscles
Color of the Iris is never black, it is actually Dark
- Innervated By the Sympathetic NS, C8 &
brown, Other color includes light brown, gray, blue
T1
(associated with Osteogenesis Imperfecta), Violet to
- (Destruction causes Horner’s Syndrome)
Transparent if melanin pigments are absent, lastly,
-For Mydriasis or Pupillodilation
Green associated with presence of other pigments
(Pheomelanin)
o (+) Sphincter or Constrictor pupillae
muscles or Circular Iris is Transparent Difficulty in concentrating light
- Innervated by the Parasympathetic NS,
Cranial Nerve 3 or Occulomotor Nerve. Pupil
Preganglionic Neuron Edinger o Space in between Iris
westphal Nucleus, Postganglionic o Colorless, appears black depending on light
Neuron Ciliary ganglion refraction
- For Miosis or Pupilloconstriction o Normal Size: 1.5mm ( Most constricted) –
10mm (most dilated)
Space in between Iris Pupils o Size is regulated by the circular and radial
Anterior to Iris Anterior Chamber muscles of the Iris
Posterior to Iris Posterior Chamber
Circular Pupilloconstrict See
o Both Contains Aqueous Humor synthesized
lesser details
by Ciliary Process
More posteriorly, at the back of Lens Vitreous Radial Pupillodilate Bird’s eye
Space: view
o (+) Vitreous Body – has semisolid fluids so Lens
fluid flows slowly o Anterior to vitreous body
o Held in place by Zonular or Suspensory
Nervous or Neural Layer/Coat
Ligaments which are attached to the cilliary
Innermost layer, The Retina has 10 layers with different
process
cells in each
o Normally Biconvexed so light entering is
Ganglion cells of Retina converges forms Optic
converged to fall in the focal point (Retina)
Nerve
Macula lutea, yellowish pigmented spot near the
Page 60 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Anterior cilliary vein empties into sclera area
Venous Circulation
Choroid
o Vascular portion IOP/ Intraoccular Pressure
Normal: 10-20 cmH2O
o Supplies oxygen and nutrients to eye Ave: 15cmH2O
structures
Retina Glaucoma
o Neural Tissue with photoreceptors, Posterior degenerative disease involving loss of retinal ganglia cells due
2/3 lining of the choroid to but not limited to inc in IOP as a result of poor drainage of
Posterior Chamber the aqueous humor through the Anterior Chamber
o space between the Iris, zonule, and the lens Beta blockers may help by decreasing AH production
that contains aqueous humor Open Angle: Increase secretion of aqueous humor
o Lateral to suspensory ligaments, Posterior to Closed Angle: Obstruction in the drainage
Iris
Anterior Chamber MUSCLES OF THE EYE
o space between the cornea and iris that Extraoccular Muscles
contains aqueous humor Muscle Action, Moves Nerve Innervation
o anterior to Iris and pupil eyeball
Vitreous Chamber or Body Superior Oblique Downward & CN 4
o space between the Lens and the Retina that Laterally
is filled with Vitreous Humor (clear and Inferior Oblique Upward & Laterally CN 3
gelatinous material) Superior Rectus Superiorly & Medially CN 3
o maintains or gives shape to the eyeball Inferior Rectus Inferiorly & Medially CN 3
Lateral Rectus Laterally CN 6
ACCESSORY STRUCTURES OF THE EYE Medial Rectus Medially CN 3
Eyelids
o Secretions hydrates the conjunctiva Intraocular Muscles
o Tear films keeps the eye moist, for nourishment
Radial Muscles or Dilator Pupillae
and protection from injury and infection
Glands: Circular Muscles or Constrictor Pupillae
Zeis Moll Kraus Meibomian Cilliary Muscles: Thickens lens when Contracted
Modified Modified Exocrine and Modified sebaceous gland. Thins Lens when Relaxed
Sebaceous Apocrine aqueous (+) lipid secretion, prevents
gland sweat secreting water from evaporating
Gland accessory maintains eye moisture FORMATION OF IMAGE
lacrimal Image is in retina, Retinal field is the one inside the
glands retina
Object is in Visual Field, The one that you see is the
SYNTHESIS OF AQUEOUS HUMOR visual field
1. Ultrafiltration of Plasma There is inversion of Image in retina Bec of
o Ciliary body has fenestrated capillaries lamination in Retina, as it goes up in the cerebrum
filters both solutes and solvents along with You see an upright position of the Image
electrolytes and small proteins Adequate Stimulus for Photoreceptor is Electromagnetic
2. Transport of Ions & Electrolytes toward the Posterior Light
Chamber Can also be stimulated by Mechanical and electrical
o This will produce a concentration gradient stimuli if the intensity of the stimulus is greater than the
causing now stimulus to see light rays. To see a phosphene ring
3. Osmosis apply heavy pressure
o Fluid is now attracted towards posterior
chamber
Stimulate Temporal side by pressing See
light/Phosphene ring in nasal side
Aqueous Humor Vs Plasma Stimulate Nasal side See light/ Phosphene ring in
Aqueous Humor Plasma Temporal side
(+) Prostaglandin (-) Prostaglandin Rods are stimulated when adequate pressure is
(+) cAMP (-) cAMP applied
20x more Ascorbic acid and lactic
acid ACCOMODATION / NEAR RESPONSE
Near Response is actually accommodation
OUTFLOW OF AQUEOUS HUMOR
o Thickening Of the lens
o Converging of the Eyeball
Conventional Pathway Unconventional
Pathway o Pupilloconstriction
Aka Anterior Circulation, Uveo-scleral circulation,
THICKENING OF THE LENS
Trabecular Pathway Posterior Pathway Principle:
% of drainage 80-95% 5-20% Light Rays should enter and leave perpendicular to the
Drains into Canal of Schlemn Posterior Chamber surface
Route Collateral vessels Cilliary Body Ascends to Your eyes has the capability to bend light
suprachoroidal area
Aqueous vein
Page 61 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
This depends on the activity of your Ciliary muscles, Near point closest distance at which you can focus on an object
whether it contracts or relaxes. ( alam mo na yan!) Remember:
Increased thickness Better Light bending Inc The Human lens is normally Biconvex
Refractive capability Biconvex lens will converge light focuses light in one
focal point
Biconcave lens will diverge light light scatters
CONVERGENCE
Bring the visual axis toward each other as attention is
focused on nearer objects
this is to focus towards the area of fovea centralis ERRORS OF REFRACTION
PUPILLOCONSTRICTION Emmetropic Eye Normal Eye
Ammetropic Abnormal Eye
You focus the light in Fovea centralis Focus on the 2 Factors:
lesser details
o Axial Length
REFRACTION o Refractive power of lens
Capability to bend and absorb light
Refractive Media of the Eyeball (CLAV) Myopia Hyperopia
o Cornea Aka Near Sightedness Far Sightedness
Angulated surface Bends light Causes Long Eyeball Small or short eyeball
most (2/3) Short Lens, Spherical etc Lens is too weak
o Lens Too Strong Lens
Bends 1/3 of light Image Loc In front of Retina Behind Retina
o Aqueous Humor Mgt Biconcave lens Biconvex lens to
Diverge light first before converge light
Bends small % of light it converges immediately
o Vitreous Humor Remarks Usually happens to
Bends small % of light children who watch TV
Focal Point/Principal focus at very near distance
o where all the refracted light meet behind the
lens
o where all light rays converge after the lens
Nodal Points
o The 2 centers of the lens, i.e, Anterior and
Posterior centers
o Assures that light rays will enter parallel, at
right angles perpendicular to the surface,
does not bend light
Focal Distance
o Distance between the LENS (nodal points)
and the FOCAL POINT/PRINCIPAL FOCUS,
considering also the light source
Presbyopia
Old sightedness
Lens becomes Inelastic by age 14, becomes evident at
age of 40
Lens is weak cannot thicken or thin out immediately
Correction Bifocal lenses, progressive lenses both for
near and far sightedness
Astigmatism
Cornea is uneven or is oblong shaped, no lens problem
Image falls behind or in front of Retina
Correction Cylindrical lenses- forms focal line
Contact lens will refract light
Test For Visual Acuity
Snellen’s Chart ( Normal=20/20)
Chart should be at eye level, 20 ft or 6m away
Make sure room is well lighted and convenient
Test one eye at a time, cover the other
Mistakes are allowed, 2 at most
Use E chart if patient cannot read (ask point of direction)
How to Interpret:
o Numerator - distance at which the tested eye
can see
@ 20ft= Far point Lens is relaxed, no accommodation is needed;
furthest point an eye can focus on
o Denominator - distance at which a normal
healthy eye can see.
Page 62 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Eg. 20/40 o Bipolar cells are stimulated releases NTA’s
you correctly read at 20 feet away what can be read by a Stimulates Amacrine cells releases
person with normal vision from 40 feet away. inhibitory NTA’s Inhibits ganglion cells
To check for
astigmatism
Normal : No
distortions seen
Minimum Separable Acuity/ Gap resolution
Detects smallest space
between parts of a target
Make sure that subject is
parallel and same level
Are they kissing or what???
Normal (accdg to Doc Valerio
and Guyton) = 25 seconds of an Arc
Minimum Perceptible Acuity/Spot detection
detect smallest
possible target
Horizontal Pathway
Pathway of vision mediated both by Amacrine and
Horizontal cells
Amacrine and Horizontal cells sends impulse and
Vernier Acuity
influences activity of adjacent bipolar and ganglion cells
These cells are not only directly connected to
photoreceptors
Detects smallest lateral
o Axon of horizontal cell is connected to
displacement
dendrite of bipolar cell
o Amacrine cells is connected to the ganglion,
it also communicates with the bipolar cells
which will send impulse directly to the brain
If lateral side is stimulated it will not push through
VISION 2 to the visual centers image is blurred
NEUROPHYSIOLOGY OF VISION Samplex: The horizontal cells inhibits the
Photoreceptors
RETINA The Amacrine cells inhibits adjacent bipolar and
ganglion cells
Most posterior aspect or the innermost portion of
eyeball
Light strikes perpendicular to axis light falls in macula PHOTORECEPTORS: RODS AND CONES
lutea Most specifically in Fovea Centralis, the area of Both a Receptor and Sensory Neuron for vision
most acute vision bec of the 1:1:1 ratio discussed earlier Rods and cones are actually modified dendrites of a
Parafoveal or extrafoveal area 1 photoreceptor neuron, this dendrites have:
synapses with plenty of bipolar cells which will also o Outer segment – contains photopigments;
synapse with plenty of ganglion cells image wouldn’t phototransduction
be as clear as compared in the fovea centralis o Inner Segment – contains organelles, i.e
The photoreceptors, bipolar cells and ganglion cells are mitochondria ((+) ATP) which supplies
bridged by Horizontal and amacrine cells energy to process photopigments, also
contains pumps
Horizontal and Amacrine cells o Nerve cell body or Perikaryon – contains the
o Inhibitory in nature nucleus
o Commonly releases GABA & glycine o Synaptic body – axon in the photoreceptor,
inhibitory to retina forms synapses with other assoc neurons.
o May also release Ach and other NTA’s also Releases NTA’s that will commonly stimulate
inhibitory to retina assoc neuron most specifically the bipolar
o Depolarization of Photoreceptors cells
Stimulates Horizontal cells releases
inhibitory NTA’s Bipolar cells are inhibited
Page 63 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Rods Cones Rhodopsin is further converted into all-trans retinal
Shape (Outer Rod shape Cone or Pyramid because barthorhordopsin, lumirhodopsin etc are all
Segment) shape unstable chemicals so they must be converted to all-
Inner Segment Thin Thick trans retinal
All-trans retinal may be converted into 11 cis-retinal by
Location Parafoveal or Mainly in foveal or
using isomerase
Extrafoveal central region
Synthesis of Rhodopsin= 11 Cis-retinal + scotopsin(from
dispersed retinal highly convergent
metarhodopsin II) Rhodopsin
pathway retinal pathway.
All-trans retinal or cis retinol is from RETINOL
Can also be seen in
Trans-Retinol is from Vit A
parafoveal region
All-trans retinal will activate G proteins specifically
Number 120 million 6 million Transducin
Sensitivity High Low
When light strikes Rods Rhodopsin is converted
Threshold Low High into all trans-retinal (same with cones)
Function Night or scotopic Day or Photopic or
vision greater color vision VITAMIN A
Acuity Lesser Higher Stored in liver ito cells
Photosensitive Rhodopsin Iodopsin First sign of Hypovitaminosis A or Vit A deficiency is
pigment Nyctalopia or Night Blindness
High sensitivity to Lower sensitivity to Vit A shots:
light light o Every month 6,000 units
More Less Photopigments o Every 6 months 200,000 units
photopigments
captures more light Leak Channels
High Amplification, Low amplification Non gated, always activated
single photon So ions can go in and out
detection This is true for K leak channel
Low temporal High Temporal
Resolution: slow resolution: fast Na Channel
response + long response + short Not considered as a leak channel, but a gated channel, it
integration time integration time closes when cGMP levels are low
Most sensitive to Most sensitive to Always open because of cGMP
scattered light direct axial rays cGMP mediated
Rod System Cone system
Achromatic, 1 type Chromatic, 3 types of When GDP is acted upon by guanylyl cyclise it becomes
of rod pigment cones cGMP Plenty of cGMP Na channels opens
Photopigments and Vit A (retinol) are stored in pigment
epithelium. When needed goes to apices of Na is abundant extracellularly so tendency is that there is Na
photoreceptor and converted to iodopsin and influx Na goes inside so membrane potential of outer
rhodopsin. segment of rods becomes less negative
BUT BUT BUT,
RODS - RHODOPSIN Remember, there is mitochondrion in inner segment for Na-K-
Only detects black and white, which are not colors ATPase pump. So Na that enters the outer segment will go to
btw inner segment and again will be pumped outside + there is a
Active Rhodopsin Metarhodopsin 1 Active drive for K to go out via K leak channels Maintained Rods
Rhodopsin Metarhodopsin 1 ( Metarhodopsin 2 membrane potential
sabi ni Doc Valerio, Sabi din ni Guyton)
Howerever, When light strikes most apical portion of the outer
segment of rods Bleaching of Rods all-trans retinal is
formed and will activate G-protein which always holds GDP
let goes GDP because of GTP GTP will now also activate
phosphodiesterase but all-trans retinal may also activate your
phosphodiesterase Phosphodiesterase will cleave cGMP to
5’-GMP.
If you do not have any cGMP, Na channels will not
open and when Na channels are closed, the activity of
Na-K pump and K leak channels are both continuous
and the whole photoreceptor becomes
hyperpolarized. That’s why you would see that when
light strikes your photoreceptors, your photoreceptors
are not actually depolarized – they are hyperpolarized
Light strikes Rods Rhodopsin is converted to its
metabolic products: Light will bleach rhodopsin until it All-trans retinal and activated G-proteins can activate
becomes All-trans Retinal your phosphodiesterase because when you have your
active G-protein, your guanylyl cyclase is active and
Page 64 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
your GTP is cleaved to GDP and cGMP Each contains diff photopigments and are maximally
G-proteins have an inherent GTPase activity that will sensitive to one of 3 primary colors (RYB)
cleave GTP to GDP for G-proteins to be inactive again. Cones responds to all colors but is maximally sensitive
GTPase wants to be inactive but G-proteins want to only to 1 color
be active Sensation of any color is determined by the frequency
of impulse from each of cone system, the frequency of
SO IN SHORT, WHEN LIGHT STRIKES THE PHOTORECEPTORS, light waves that will strike the color cones
THEY ARE HYPERPOLARIZED you do not release glutamate
and when glutamate is not released, horizontal cells are not Opponent Process Theory
stimulated and it will not be able to inhibit the bipolar cells so Colored lights activates opposing neural process
it will be able to generate local potential until it summates for Green as to Red
it to stimulate ganglion cells. When you Stimulate green, you don’t Stimulate Red and vice versa
Yellow as to Blue
So pano Pag DARK? When you stimulate blue you don’t stimulate yellow and vice versa
Black as to white
But they are not really colors, so yeah whatever
Dark Somehow depolarized but does not reach AP, local
potential only unless they summate reaches Action
Potential releases NTA’s: Glutamate (present in bipolar cells Retinex Theory
as well as in horizontal cells) Horizontal cells are stimulated Attributes color vision to combined action of neural
activity at several neural levels of visual system which
to release inhibitory neurotransmitters and it goes to the
photoreceptor and inhibits the bipolar cells includes retina and visual cortex
Cones will just be receptors will send impulse to
In Ganglion cells, upon NTA release you produce visual cortex Color is created and processed in Visual
cortex you see colors
immediate Action Potential
We have layers in the cerebral cortex – V1, V2, V3, V4, V5,
Bipolar cells local potential but it can summate V1V4a and V1V4B wherein the colors would fall.
Glutamate
COLORS
Common NTA used
Both Inhibitory and Stimulatory
Primary Secondary Complementary Color Cones
Synapses in Center Stimulatory
Colors Colors Colors
Synapses in Round Inhibitory
Red R+Y = Orange Red-Green Red
Yellow R+B= Violet Blue-Yellow Green
CONES: COLOR VISION Blue B+Y= Green Blue
Wavelength range of visible light = 397nm-723nm, in
this wavelength you will be able to discriminate colors,
and Cones are responsible for this detection
Photochemicals in cones almost have same chemical
composition with that of rhodopsin
Difference is in Protein Portion The opsin or
Photopsin
Sees Black No color cones are stimulated
Sees White All color cones are stimulated
Damaged cones Black and white vision Interpretation:
Orange You stimulate more of Red cones than Green
THEORIES OF COLOR VISION Blue You only stimulate blue cones
Yellow Equal red and green cones
Trichromasy Theory Red Only red cones
The difference in absorption of light accounts for color White All color cones, equally
vision Black None
Tricolor mechanism of color detection and this depends
upon absorption of lightwaves to recognize a certain Attributes of Color
color, and they are your: Hue – Name of color. Eg: Red
Intensity – Quality . Bright or dull? Eg: Bright Red
Primary colors (RYB) Saturation – relative purity of color Eg: Fuchsia Pink
Red Longest wavelength
Yellow Intermediate
GANGLION CELLS
Blue Shortest
Primary Retinal or Color Cones (RGB) W X Y
Red Longest wavelength 570nm 40% 55% , most numerous 5%, least
Green Intermediate 535 nm numerous,
Blue Shortest 445 nm LARGEST
In short, this theory states that there are cones sensitive to Directional Dendrites don’t For Light changes
certain lightwaves to be able to recognize the color movement: Left right spread widely For
front back small fields of vision,
Young Helmholts Theory Specific
Postulates theory of 3 kinds of Cones ( Red, Green, Blue)
Page 65 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Crude rod or Gen Fine details of visual For rapid changes Green blindness problem in green-red and green-
vision under dark image. in visual Image blue combinations
conditions
Receives most Eg: nose, mouth etc Fires without
Tritanope blue blindness, almost the gray color is
excitation from accuracy
seen, may have few spots of blue
Rods Black and
white only Matching of Spectral Colors
Eg. Shapes Eg. Shadow, for patients who can’t read or write
“Malikmata” patient will find and match the colors.
COLOR BLINDNESS American Optical Instruments
X linked recessive uses shapes
o Due to abnormality in 1 or 3 cones Holgren’s Test
o Males are commonly affected Stilling’s Test
o Females are most likely carriers, but they can Rayleigh Match test
be affected too, provided that the dominant
X gene did not neutralize the recessive other LIGHT ADAPTATION
X gene Moment from dark going into bright light
Prefixes Prot Red Stimulates mainly Cones, little of Rods
Deuter Green
Tri Blue Person is exposed to bright light for hours now
Suffixes Anomalous/Anomaly Color large portions of photochemicals in rods and cones is
reduced to retinal and opsins
weakness
Retinal of both rods and cones is converted to Vit A
Anopia or anope Color
blindness
Concentrations of photosensitive chemicals of rods
Eg: Protonomalous Weakness in seeing shades of Red and cones remaining are significantly reduced
Protananopia Cannot see red so you it is hard to Sensitivity of eyes to light is reduced
distinguish violet from blue, orange tinted red appears as dim
yellows etc Other changes:
Pupilloconstriction – to regulate light rays entering
DISORDERS OF THE COLOR VISION OF THE EYE pupil that will strike retina for better vision
Trichromats Utilization of central portion of retina ( fovea)
All cones system are functioning, Normal RGB cones Bleaching of rhodopsin
Normal Colour Vision Greater activation of cones
Dichromats
2 cones system are functioning, but 1 is missing DARK ADAPTATION
You only stimulate your Rods bec of low light
Monochromats intensity
Only 1 cone system is functioning, 2 are missing Remember: cones are only stimulated when there is
high intensity of light
Achromatopsia Person is exposed to darkness for so long
Total color blindness only, patient can still see Black and Retinal and opsins in the rods and cones are
white converted back into the light sensitive
pigments
TEST FOR COLOR BLINDNESS Vit A is converted back to retinal give more
light sensitive pigments
Ishihara Color Blind Test
most common test for color blindness The limit is determined by amount of opsins in the
uses numbers and lines, plates contg. figures made up rods and cones to combine with retinal
of colored spots on a background of similarly shaped Other changes:
colored spots Pupillodilation – so all lights may enter
Utilization of peripheral portion of retina (parafovea)
Synthesis of Rhodopsin
Greater rods activation
Visual Field
Visual area seen by one of your eyes at a given instant
(monocular vision)
The right eye sees something that the left eye cannot,
and vice versa
Nasal field of Vision area seen at nasal side
Temporal field of vision area seen at lateral side
Barriers:
o Nose, medially
o High cheekbones, lower portion
Page 66 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
o Thick eyebrows and Scaphocephaly (long Size Perspective
narrow head), upper portion
This is why when you check for visual field, you tell
patient to stare at straight level Smaller one is
farther, the bigger one
PERIMETRY is closer
Systematic measurement of differential light sensitivity
in visual field by detection of presence of test targets in
a defined background
Maps and quantifies visual field especially at extreme
periphery of visual field Distribution of Shadows and Illumination
Tests all angles and measures peripheral vision
Known as
Usage: Chiaroscuro
Placed on cheek Illumination
One eye is covered, other eye looks and intensity is bright
in the mirror
near
Patient should not move If it is lighter
Far
Motion Parallax
DEPTH PERCEPTION
Assess Distance and movement of a particular object If object
3 cues: is near and
o Distance by sizes formed in retina moving almost
o Distance by stereopsis ( binocular vision) all parts are
o Distance by moving parallax moving
Parallax- if you look at some nearby object and move your
Object
head a little from side to side, the object looks like it is
moving back and forth. is far you only
see few parts of
them moving
MONOCULAR CUES – FARFIELD DEPTH PERCEPTION
Familiar Size STEREOSCOPIC CUES- NEARFIELD DEPTH PERCEPTION
You know the size of an object
Pupils are normally 6cm or 2 in apart
In a considerable distance, one may appear thin and
Fixation point (Merriam-Webster) - the point in the
small but as you move closer it becomes bigger, that is
visual field that is fixated by the two eyes in normal
your familiar size
vision and for each eye is the point that directly
stimulates the fovea of the retina
Occlusion
When you move
The one seen wholly is the
the object closer
nearer object
distance between images
If only some parts are seen
formed in both retinas
farther
will become farther
When you move
it farther distance
between images formed
in both retinas will
become closer
Linear perspective
If near Appears
Parallel
As it goes farther It
VISUAL PATHWAY
converges until only 1 line is
seen All info coming from left visual field of both eye is
conveyed to the right side of brain and vice versa
The Retina has Temporal and nasal side on both eyes
Temporal side and nasal side forms part of optic
nerve
The Ipsilateral temporal side forms the optic tract, the
nasal side will cross over and joins the optic tract
Page 67 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Damage/Lesion: Images are formed in Retina
Temporal side of retina conducts impulse on ipsilateral
primary visual area
Nasal Side of retina conducts impulse going to
contralateral side of primary visual cortex ( BA # 17)
Cuneus Vs Lingual Gyrus
Cuneus Lingual Gyrus
Location Superior Calcarine Inferior Calcarine
Area Area
Projection in Projected inferiorly Projected
visual field Superiorly
(remember the
principle of
inversion)
Lesion Inferior Superior
Quadrantanopsia Quadrantanopsia
If you damage the right side of Cuneus left inferior
quadrantanopsia
Damage of most of the portion of calcarine area
except the most posterior aspect (occipital lobe)
Macular Sparing sees small pinpoint
Both Cuneus and Lingual is affected Homonymous
Quadrantanopsia
Pathways
Magnocelluar Parvocellular
Conduction speed Rapid Slow
Receives input Large Type Y Type X Retinal
from retinal ganglion ganglion cells
cells
Transmits Black and white Color and conveys
info accurate point to
point or detailed
infos
DIE VISION. DIEEEE!
From Retina Optic Nerve Optic chiasm optic tract
superior colliculus lateral geniculate body optic
radiation or geniculo calcarine tract primary visual center or
commonly known as the calcarine area.
Page 68 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
long-chain organic substances that
TASTE AND SMELL PHYSIOLOGY contain nitrogen
allow us to separate undesirable or even lethal foods from alkaloids. such as quinine, caffeine,
those that are pleasant to eat and nutritious.
strychnine, and nicotine.
elicit physiological responses that are involved in digestion
and utilization of foods. o In high intensity, usually causes the person
strongly tied to primitive emotional and behavioral functions or animal to reject the food. Important for
of our nervous systems. poisonous substance rejection
The sense of smell also allows animals to recognize the Saccharine sweet taste + Bitter aftertaste
proximity of other animals or even individuals among
animals. Umami
Reference: Guyton and Hall 12th Edition + Handouts o Japanese word meaning delicious
TASTE PHYSIOLOGY o the dominant taste of food
o containing l-glutamate,
TASTE o the precise molecular mechanisms
responsible for umami taste are still unclear.
mainly a function
of the taste buds in the
A person can perceive hundreds of different tastes.
mouth,
Slight changes in the chemical structure, such as addition of
one's sense of a simple radical, can often change the substance from sweet
smell also contributes to bitter
strongly to taste
perception. THRESHOLD FOR TASTE
it allows a person
to select food in accord
with desires and often in
accord with the body
tissues' metabolic need for
specific substances.
Threshold minimum at 20-30 degrees Celcius
the texture of food, as detected by tactual senses of Varies with temp of solution
the mouth, and the presence of substances in the LOWEST THRESHOLD IS BITTER protective function
food that stimulate pain endings, such as pepper,
greatly alter the taste experience TASTE BLINDNESS
Occurs especially for different types of thiourea
PRIMARY SENSATIONS OF TASTE compounds.
Phenylthiocarbamide
o substance used frequently by psychologists
for demonstrating taste blindness
o 15 to 30 percent of all people exhibit taste
blindness
TASTE BUDS
diameter = 1/30 millimeter
length =1/16 millimeter.
sour composed of about 50 modified epithelial cells,
o caused by acids, hydrogen ion o sustentacular cells
concentration, o taste cells
o more acidic the food, the stronger the sour Taste pores – has taste hairs as receptor
sensation becomes. surface for taste.
Salty continually being replaced by mitotic division of
o elicited by ionized salts, mainly by the surrounding epithelial cells,
sodium ion concentration. o young cells
o sodium cations, are mainly o mature cells lie toward the center of the bud
o anions also contribute to a lesser extent soon break up and dissolve.
sweet o The life span of each taste cell is about 10
o not caused by any single class of chemicals. days in lower mammals but is unknown for
o Some of the types of chemicals that cause humans.
this taste include sugars, glycols, alcohols, The outer tips of the taste cells are arranged around a
aldehydes, ketones, amides, esters, some minute taste pore
amino acids, some small proteins, sulfonic Microvilli
acids, halogenated acids, and inorganic salts o From the tip of each taste cell
of lead and beryllium. o Aka taste hairs that protrude outward into
Bitter the taste pore to approach the cavity of the
o Also not caused by any single type of mouth.
chemical agent. o provide the receptor surface for taste.
o almost entirely organic substances.
o Two particular classes of substances
Page 69 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Vesicles Sweet and bitter taste sensations the portions of the
o contain a neurotransmitter substance that is receptor protein molecules that protrude through the apical
released through the cell membrane to membranes activate second-messenger transmitter
excite the nerve fiber endings in response to substances inside the taste cells, and these second messengers
taste stimulation. cause intracellular chemical changes that elicit the taste
Stimulation of Taste Buds Substances must be in signals.
solution or dissolved in saliva
Generation of Nerve Impulses by the Taste Bud
Location of Taste Buds First application of the taste stimulus the rate of
Circumvalate papillae discharge of the nerve fibers from taste buds rises to
o Forms a V-line posterior of the tongue a peak in a small fraction of a second then adapts
o Large number of taste buds within the next few seconds back to a lower, steady
Fungiform papillae level as long as the taste stimulus remains.
o Distributed all over, Moderate numbers of Strong immediate signal is transmitted by the taste
taste buds nerve, and a weaker continuous signal is transmitted
o over the flat anterior surface of the tongue as long as the taste bud is exposed to the taste
Foliate papillae stimulus.
o Postero-lateral surface of the tongue TRANSMISSION OF TASTE SIGNALS INTO CNS
o Moderate Numbers Taste impulses from the anterior 2/3 of the tongue
pass first into the lingual nerve chorda tympani
Additional taste buds are located on the palate, and a
few are found on the tonsillar pillars, on the epiglottis, facial nerve tractus solitarius in the brain stem.
and even in the proximal esophagus. Taste sensations from the Posterior 1/3 of tongue,
circumvallate papillae on the back of the tongue and
Adults have 3000 to 10,000 taste buds, and children
from other posterior regions of the mouth and throat
have a few more.
are transmitted through the glossopharyngeal nerve
Beyond the age of 45 years many taste buds
degenerate causing taste sensitivity to decrease in tractus solitarius, but at a slightly more posterior
old age. level.
Base of the tongue and other parts of the pharyngeal
Specifity region by way of the vagus nerve tractus solitarius f
taste substance is in low concentration single taste .
responds mostly to one of the five primary taste All taste fibers synapse in the posterior brain stem in
stimuli the nuclei of the tractus solitaries send second-
high concentration most buds can be excited by order neurons to a small area of the ventral posterior
two or more of the primary taste stimuli, as well as by medial nucleus of the thalamus third-order
a few other taste stimuli that do not fit into the neurons are transmitted to the lower tip of the
"primary" categories postcentral gyrus in the parietal cerebral cortex it
curls deep into the sylvian fissure adjacent
MECHANISM OF STIMULATION OF TASTE BUDS opercular insular area
Receptor Potential
change in electrical potential in the taste cell The taste pathways closely parallel the somatosensory
membrane of the taste cell,is negatively charged on pathways from the tongue.
the inside with respect to the outside
Application of a taste substance to the hairs causes Taste Reflexes Are Integrated in the Brain Stem
them to be depolarized it is proportional to the o From the tractus solitarius, superior and
logarithm of concentration of the stimulating
inferior salivatory submandibular,
substance.
sublingual, and parotid glands help
Mechanism = binding of the taste chemical to a protein control the secretion of saliva during the
receptor molecule that lies on the outer surface of the taste ingestion and digestion of food.
receptor cell near to or protruding through a villus membrane
opens ion channels allows positively charged sodium ions ADAPTATION AND TASTE PREFERENCE
or hydrogen ions to enter and depolarize the normal negativity Taste sensations adapt rapidly, often almost
of the cell taste chemical itself is gradually washed away completely within a minute or so of continuous
from the taste villus by the saliva, which removes the stimulus. stimulation.
Final extreme degree of adaptation that occurs in
Type of receptor protein central nervous system itself, although the mechanism
Sodium ions elicit salty sensations and site of this are not known.
Hydrogen ions sour taste sensations adapt almost entirely at the receptors.
For Salty and Sour the receptor proteins open specific ion Taste preference
channels in the apical membranes of the taste cells, thereby simply means that an animal will choose certain types
activating the receptors. of food in preference to others, and the animal
automatically uses this to help control the diet it eats
often change in accord with the body's need for
certain specific substances.
Page 70 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
results from some mechanism located in the central activating olfactory nerves greatly multiplies the
nervous system previous experience with excitatory effect of even the weakest odorant.
unpleasant or pleasant tastes plays a major role in even the most minute concentration of a specific
determining one's taste preferences or taste aversions odorant initiates a cascading effect that opens
extremely large numbers of sodium channels. This
Taste receptors often become sensitized in favor of a accounts for the exquisite sensitivity of the olfactory
needed nutrient. neurons to even the slightest amount of odorant.
SMELL PHYSIOLOGY
PHYSICAL FACTORS THAT AFFECT THE DEGREE OF
least understood among senses.
STIMULATION
Sense of smell is a subjective phenomenon that
only volatile substances that can be sniffed into the
cannot be studied with ease in lower animals
nostrils can be smelled.
poorly developed in human beings
stimulating substance must be at least slightly water
soluble so that it can pass through the mucus to reach
the olfactory cilia
it is helpful for the substance to be at least slightly
lipid soluble, presumably because lipid constituents of
the cilium itself are a weak barrier to non-lipid-
soluble odorants.
MEMBRANE POTENTIALS AND ACTION POTENTIALS IN
OLFACTORY MEMBRANE OLFACTORY CELLS
lies in the superior part of each nostril.
Medially folds downward along the surface of the Membrane potential inside unstimulated olfactory
superior septum cells = -55 millivolts. At this potential, most of the
laterally, it folds over the superior turbinate and even cells generate
over a small portion of the upper surface of the o once every 20 seconds up to two or three
middle turbinate per second of continuous action potential
In each nostril, has a surface area of about 2.4 square
centimeters. depolarization of the olfactory cell membrane = -30
millivolts or less
OLFACTORY CELLS o action potentials increases to 20 to 30 per
receptor cells for the smell sensation second, which is a high rate for the minute
are bipolar nerve cells derived originally from the olfactory nerve fibers.
central nervous system itself. the rate of olfactory nerve impulses changes
about 100 million of these cells in the olfactory approximately in proportion to the logarithm of the
epithelium interspersed among sustentacular cells, stimulus strength
The mucosal end of the olfactory cell forms a knob RAPID ADAPTATION OF OLFACTORY SENSATIONS
from which 4 to 25 olfactory hairs (also called Olfactory receptors
olfactory cilia), adapt about 50 percent in the
o react to odors in the air and stimulate the first second or so after
olfactory cells stimulation they adapt very
o 0.3 micrometerin diameter little and very slowly
o 200 micrometers in length Most of the additional
o project into the mucus that coats the inner adaptation occurs within the
surface of the nasal cavity form a dense central nervous system. Same
mat in the mucus with taste.
Bowman's glands
Secrete mucus onto the surface of the olfactory
membrane. Postulated neuronal mechanism for the adaptation is the
Spaced among the olfactory cells in the olfactory following:
membrane Large numbers of centrifugal nerve fibers pass from
the olfactory regions of the brain backward along the
STIMULATION OF OLFACTORY CELLS olfactory tract and terminate on special inhibitory
Olfactory Signal Transduction= Binding of the odorant to a cells in the olfactory bulb, the granule cells.
G-coupled protein receptor activation of adenylate cyclise after the onset of an olfactory stimulus, CNS quickly
converts ATP to cAMP cAMP activates a gated sodium develops strong feedback inhibition to suppress relay
channel that increases sodium influx and depolarizes the cell of the smell signals through the olfactory bulb.
exciting the olfactory neuron transmitting action potentials
to the central nervous system Granule Cells
Olfactory cilia o special inhibitory cells in the olfactory bulb
o portion of each olfactory cell that responds o Means of sharpening specific ability to
to the olfactory chemical stimuli distinguish odor
Psychological adaptation > receptor adaptation
Page 71 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
AFFECTIVE NATURE OF SMELL to the hypothalamus.
Smell, even more so than taste, has the affective
quality of either pleasantness or unpleasantness Septal nuclei
smell is probably even more important than taste for are midline nuclei that feed into the hypothalamus
the selection of food. and other primitive portions of the brain's limbic
In addition, in some lower animals, odors are the system.
primary excitant of sexual drive.
This is the brain area most concerned with basic
THRESHOLD FOR SMELL behaviour, basic olfactory reflex
Very Low The Less Old Olfactory System
methylmercaptan can be smelled when only one 25 The Lateral Olfactory Area
trillionth of a gram is present in each milliliter of air composed mainly of the prepyriform and pyriform
mixed with natural gas to give the gas an odor that cortex plus the cortical portion of the amygdaloid
can be detected when even small amounts of gas leak nuclei
from a pipeline. Learned Control
Concentrations only 10 to 50 times above the
threshold evoke maximum intensity of smell. Hippocampus
smell is concerned more with detecting the presence most important for learning to like or dislike certain
or absence of odors rather than with quantitative foods depending on one's experiences with them.
detection of their intensities
many signal pathways from this area also feed directly
TRANSMISSION OF SMELL SIGNALS INTO CNS into an older part of the cerebral cortex called the
Limbic System part of the brain that originally subserved paleocortex in the anteromedial portion of the
olfaction later evolved into the basal brain structures that temporal lobe
control emotions and other aspects of human behavior only area of the entire cerebral cortex where sensory
signals pass directly to the cortex without passing first
Olfactory bulb through the thalamus
Olfactory signals are transmiited into automatic but partially learned control of food intake
lies over the cribriform plate, separating the brain and aversion to toxic and unhealthy foods
cavity from the upper reaches of the nasal cavity. The Newer Pathway
The cribriform plate has multiple small perforations passes through the thalamus dorsomedial
through which an equal number of small nerves pass thalamic nucleus lateroposterior quadrant of the
upward from the olfactory membrane in the nasal orbitofrontale cortex
cavity to enter the olfactory bulb in the cranial cavity
There is close relation between the olfactory cells in the conscious perception and analysis of olfaction
olfactory membrane and the olfactory bulb:
o short axons from the olfactory cells terminating in
multiple globular structures within the olfactory bulb
called glomeruli.
Each bulb has several thousand such glomeruli, each of which is
the terminus for about 25,000 axons from olfactory cells.
Each glomerulus also is the terminus for dendrites from about 25
large mitral cells and about 60 smaller tufted cells, the cell
bodies of which lie in the olfactory bulb superior to the
glomeruli.
These dendrites receive synapses from the olfactory cell neurons,
and the mitral and tufted cells send axons through the olfactory
tract to transmit olfactory signals to higher levels in the CNS
Different glomeruli respond to different odors. It is possible
that specific glomeruli are the real clue to the analysis of
different odor signals transmitted into the central nervous
system.
The Very Old, Less Old, and Newer Olfactory Pathways
The olfactory tract enters the brain at the anterior
junction between the mesencephalon and cerebrum;
there, the tract divides into two pathways,
one passing medially into the medial olfactory area of
the brain stem very old olfactory system
the other passing laterally into the lateral olfactory
area input to
(1) a less old olfactory system
(2) a newer system
Very Old Olfactory System
The Medial Olfactory Area
area consists of a group of nuclei located in the
midbasal portions of the brain immediately anterior
Page 72 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
EQUILIBRIUM o Predictive function : Signal beginning or end of
Source: Dr Barbon’s Lecture, Lecture guide, Icelimpin notes head rotation, and predicts incoming
Ability to maintain posture or balance malequilibrium
Depends on receptors of inner ear Vestibular apparatus
Receptor organ in the Semicircular canal is the Crista Ampullaris,
Involves activity of: which is Located in the Ampulla
1. Proprieceptors Activation of the Canal
2. Visual receptors - weak Hair cells is embedded at the base of cupula
3. Exteroreceptors 1. Head rotates Movement of the canal displacement
of endolymph inside the canal Cupula activation
Normal Body Position 2. Movement of the cupula activation of the hair cells
Concerned more with head (receptors)
Upright head, thorax and extremities 3. Receptor or hair cells activity is transferred to afferent
Attributed to stimulation of extensor muscles of extremities, nerve or the vestibular nerve aka utriculosaccular nerve
back and neck antagonizes gravity, these are your impulse transmitted to center
postural or antigravity muscles
Displacement of endolymph Movement of cupula hair
Functional unit of nervous system reflex arc cells activity is change transmitted to vestibular nerve
VESTIBULAR APPARATUS center
The receptors of the canal, utricle and saccule & cochlea is
Receptors of the inner ear
the same = hair cells
Present in temporal bone, 2 sets Left and Right
Mediated by CN 8 or Vestibulocochlear nerve specifically
UTRICLE AND SACCULE
Vestibular portion
Connected to Semicircular canal, also for maintenance of
1. (+) branches for both vestibular apparatus and cochlear
balance
structures
Also have endolymph, hair cells and gelatinous mass , No
Neuronal Acitivity associated with Audition
cupula (walang name yung gelatinous mass nya)
Made up of:
Contains the Otoconia / Otoliths / Statoconia / Ear dust
1. Semicircular canal
o Considered as gravity receptors
2. Utricle and Saccule
o Mass of calcium carbonate crystals embedded in
SEMICIRCULAR CANAL gelatinous substance or layer
Hair cells are also embedded in the gelatinous
substance
Receptor organ in Utricle and Saccule = MACULA
Macula
For Static Equilibrium: determination of head or body
position when body is not moving or with respect to
direction of gravitational pull
For linear movement or acceleration
o Suddent thrust forward of the body otoconia is
Arranged at right angles to each other, representing 3 planes thrown backward d/t inertia
in space when the head is bent forward around 30 degrees o Backward Otoconia is thrown forward d/t inertia
Composed of 3 paired ducts/canal = total of 6 For detection of Centrifugal forces(a form of inertia)
1. Right and Left Anterior or Superior Vertical tendency of an object following a curved path to fly way
Located in vertical plane, projects from center of curvature so we correct this by leaning
forward and 45 degrees outward towards the center
2. Right and Left Posterior Vertical Macula is never concerned with linear velocity
Located in vertical plane, projects
backward and 45 degrees outward
Orientation of Utricle and Saccule
3. Right and Left Horizontal Approximately Horizontal,
o Horizontal: Macula of utricle
located in same plane, so it will meet the horizontal Upright position Utricle dependent (upo)
plane when you bend the neck 30 degrees || if neck is
o Vertical: Macula of Saccule
straight canal is Semi horizontal Lying position Saccule dependent (sahig)
Identical or Parallel or on same plane:
o Righ Anterior and Left Posterior Upright Lying
o Left Anterior and Right Posterior
Maccula of utricle is Horizontal in Maccula of saccule is Horizontal
o Right and Left Horizontal
position in position
PURPOSE: DETERMINE DIRECTION OF MOVEMENT
Maccula of saccule is vertical Maccula of utricle is vertical
These canals contain Endolymph Utricle is Stimulated Saccule is Stimulated
Receptor organ in Semicircular canal Crista Ampullaris Saccule is Inhibited Utricle is Inhibited
Crista Ampullaris Motion Sickness Problem is in Utricle
WHOLE SENSORY ORGAN OF SEMICIRCULAR CANAL Management: Lie down, so Saccule is the one stimulated
Located in the ampulla, the dilated or swollen end of the dizziness disappears or lessens
canal
Made up of hair cells (located at the base of the cupula, Activation of Utricle and saccule
attached to vestibular nerve) with Stereocilia and a large Activity of hair cells is dependent on otoconia displacement
Kinocillium covered by a gelatinous mass called Cupula caused by gravity
Cupula is where the hair tufts from hair cells project Otoconia is made up of crystal Heavier and denser than
Cupula is considered as the whole structure in the gelatinous mass, and is mostly affected by gravity
ampulla that represents the side of the canal
separating the other side Static:
For Dynamic or Kinetic Equilibrium for body in motion: 1. Otoconia is pulled down by gravity gelatinous mass is
spinning or rotator movement compressed haircells embedded on it are displaced
Page 73 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
2. Displaced hair cells impulse goes to Center (CNS) Movement is dependent on hair cells activity
Additional movement in macula if there is linear motion This is where the Kinocilium of different hair cells are directed
inorder to determine forward, backward or sideward
movement LINEAR ACCELERATION
Forward, Backward or sideward movement
Receptor organ in Semicircular canal = Crista Ampullaris For Activation of Utricle is due to effect of inertia, which would
dynamic or kinetic equilibrium cause movement of the hair cells
Receptor organ in Utricle and Saccule = MACULA for static
equilibrium, linear movement and centrifugal forces Statoconia or Otoconia
HAIR CELLS o Gelatinous mass, which is heavier than hair cells
2 types: Kinocilium and Stereocilia because of the calcium carbonate crystals
Kinocilium Stereocilia o Due to Inertia:
Tall and large diameter Thin and shorter Movement forward statoconia or
Movement of both hair cells are important for determination their activity otoconia moves backward, opposite
Movement Backward Statoconia or
otoconia moves forward
Activation of Hair Cells Isipin nyo na lang masyadong mabigat yung
RMP = -16mv otoconia kaya naiiwan sya sa opposite direction
Ion channels activated = K and Ca channels
NTA= Glutamate Striolar Groups or Division
Depolarized/Activated Hyperpolarized/Inactivated o Forward movement
Movement of stereocilia is toward Movement is away from Anterior group of hair cells are activated
the Kinocilium kinocilium or toward stereocilia Posterior group of hair cells are inactivated
Stereocilia is pushed toward Stereocilia is pushed away from
Kinocilium Kinocilium o Lateral movement (eg. Towards left)
lateral group of the left utricle and medial
Kinocilium moves away from Stereocilia moves away from
group of right utricle is activated
stereocilia kinocilium
o Lateral movement (eg. Towards right)
Lateral group of right utricle and medial
Impulse Generation of Hair cells in Vestibular Apparatus: Saccule, group of left utricle is activated
Utricle and Semicircular canal
Resting Activity ofHair cells or tonic activity (not moving) Utricle is mainly responsible for detection of movement when
o generates 100-200 impulses/sec negotiating a curve (In centrifugal forces), when head is upright.
o this tonic activity is helpful to determine position
of head SEMICIRCULAR CANAL PART 2
No impulses generating Patient is asleep and doesn’t Again, this is where the Crista Ampullaris is so it is for
know head position Dynamic or Kinetic equilibrium
(+) sideward, forward, backward movement of head or body o Detection of angular or rotator
changes in positioning of macula Increased activity of acceleration
hair cells, stereocilia moves toward kinocilium Predictive function associated with cerebellar
depolarization of hair cells activity which is for coordination and muscle tone
in preparation for movement
UTRICLE & SACCULE PART 2 o This predictive functions is associated
This is where the macula is so it is for most particularly with Archicerebellum
Static equilibrium or vestibulocerebellum mostly of the
Head position determination posterior part
Space orientation Again receptors are present in the Crista ampullaris, its
Linear movement or acceleration determination activation is due to rotation of the body: the displacement of
Detection of centrifugal forces endolymph causes movement of cupula and this
Saccule Activation Utricle Activation displacement will cause hair cells to move
Vertical Acceleration Up and down Horizontal acceleration Forward,
backward, movement toward a circle Movement of Endolymph
either clockwise, counterclockwise Movement is Clockwise rotation Endolymph moves
(Centrifugal force)
opposite side or counterclockwise initially d/t inertia
Eg. Going up and down in elevator etc Eg. Walking towards a circle, walking
forward etc
Movement of the body Endolymph inside also moves, in
Lying Position, also for upright Upright Position opposite direction
position only in determining up or To determine the spinning movement of the head / body speed
down movements rotation should be equal or greater than 1°/sec2
If < 1°/sec2 you will not determine any movement
Gravitational forces exerted by Otoliths/Otoconia/Statoconia Kinocilium is oriented towards the center
Otoliths are your gravitational receptors in Utricle and There is tonic activity when resting 100-200 impulses/sec
saccule
Head at rest : 100-200 impulses/sec ROTATION
Tilts toward Kinocilium Depolarization Head Rotation to the Right
Tilts toward stereocilia Hyperpolarization Semicircular Canal moves toward the right
o because it is fixed in the inner ear
STRIOLA o canal follows movement of the head
Central, depressed portion
Endolymph moves toward opposite side
in the otoconia or otoliths
o d/t inertia
Serves as a reference point
to determine divisions of group of hair Increased activity in the right Crista stereocilia moves
cells in macula, which includes: toward kinocilium Depolarization Increase Action
Anterior, Posterior, Lateral potential
and medial group Decreased activity or inbited activity in Left Crista
Page 74 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
o On the left side: Kinocilium moves toward o Rotation to the left in horizontal plane Past
stereocilia pointing to the right
We know the direction of the rotation because there is
variation in the activity of left and right Crista Tendency to fall
o A false sensation, you fall because you try to
Head Rotation Continues correct the balance
Like for Ballet dancers o Tendency to fall and vertiginous sensation are
If you can talk to rotating person rotating person will not opposite in direction, like in past pointing
be able to determine the direction of the rotation
Comtinuous rotation eventually, endolymph will follow Autonomic sensations
the rotation of the canal hair cells in the crista will assume o Nausea and vomiting
again a normal resting position so Direction of rotation is o Pallor
only determined at the start of rotation o Sweating
Right and left crista is equally activated o Vasoconstriction pale
o Changes in BP, HR, RR
Head Rotation Ends o Miosis during rotation
When you stop d/t inertia Endolymph continues to flow o Mydriasis after rotation
towards the right there is continuous sensation of rotation o Dizziness- like vertigo but environment doesn’t
and this will cause Post rotatory sensation spin
Sensation of the direction of rotation is towards the left this TEST MADE TO DETERMINE INTEGRITY OF CANAL
time, d/t movement of endolymph Remember: Opposite Opposite, same same
o Left Crista is activated *Sa lecture guide kasi Opposite din yung sa Tendency to fall at PP, pero siguro
o Right Crista is inactivated initially lang yun, e yung case naman dito Post rotation na, yun siguro yun? Haha
After a while, Crista ampullaris or the canals will assume its ewan.
normal resting position
POST ROTATORY SENSATION/REACTIONS
Effects produced by rotation
Vertigo
o Sensation that environment is rotating, feeling of
unsteadiness and of actual disturbance of
equilibrium If you rotate in Horizontal plane stimulate Horizontal canals
o d/t excitation of semicircular canals or their central
connections
o Horizontal plane: Post rotator vertiginous
sensation is in opposite direction of rotation
o Sagittal plane: Post rotator vertiginous sensation
is falling backward or forward
o Frontal plane: Post rotator vertiginous sensation is If you rotate in Sagittal plane You stimulate all canals
falling to right or left side
Nystagmus/Eye movements
o Rhythmical slow eye deviation to one side and a
quick return to normal, forward looking position
o 3 types:
Horizontal- due to stimulation of
horizontal canals so when turning in If you rotate in Frontal or coronal plane You stimulate all vertical canals
an upright position of the head in
horizontal plane PARTS OF NERVOUS SYSTEM ESSENTIAL FOR EQUILIBRIUM
Vertical- eyes move up and down; d/t Spinal cord
stimulation of all canals, rotation on o Neck reflexes
sagittal plane tumbling o Motor neurons at anterior horn regulates activity
Rotatory- round about movement of the of the muscles
eyes in antero-posterior axis. d/t Brainstem
rotation of frontal plane and stimulation o Subconscious maintenance of posture
of vertical canals body attached to o Midbrain for righting reflex/correcting reflex
wheel (with involvement of photoreceptors) allows
At the beginning of rotation nystagmus would be on same body to have correct position
direction as rotation
o Pons and medulla maintain balance
After rotation nystagmus would be on opposite direction as
rotation
o Reticular system of pons keeps us awake
Whatever the direction of the fast or quick or phase/ component is, o Dec activity of pons muscles that maintain
that is the direction of nystagmus postures weaken (observerd when asleep)
o Controlled by the Higher center brainstem Righting reflex is the only reflex not located
Used for reading in cerebral cortex
Maintain visual fication on stationary point Problems in the eye imbalance
while body rotates
Slow phase/component All righting reflex is dependent on Midbrain
o Dictated by the vestibular apparatus Labyrinth except for optical righting reflex (uses
occipital cortex)
Past Pointing (PP) Cerebral cortex
o An involuntary act, a subconscious correction for o Conscious maintenance of posture
the impression that there is continuous rotation
immediately after stopping the rotation Cerebellum- Unconscious maintenance of psoture
o Vestibulocerebellum/Archicerebellum
Page 75 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Flocculonodular lobe, mostly posterior
Posture, gait and equilibrium
maintenance, when not moving (static
equilibrium)
Prediction of movements, to prepare
body for rapid movements
o Paleocerebellum/Spinocerebellum
Greater connection with Spinal cord
Control of muscle activity
Maintain equilibrium while in motion
(Dynamic Equilibrium)
Motor coordination
Located in anterior lobe, mostly in
medial portion
o Neocerebellum/Cerebrocerebellum
Posterior lobe, mostly lateral
Control and coordination of voluntary
and learned movements
For motor learning
o Athletes have well
coordinated muscle
Problems in inner ear, cerebellum, spinal cord, brainstem and cerebral
cortex will lead to Malequilibrium
For Fine adjustment of posture Brainstem, Cerebral cortex and
Cerebellum
Anti Gravity muscles
Muscles (mostly extensors) required to maintain posture,
includes leg muscles when standing
Arm extensors pro gravity
Flexors are anti gravity but is not used for posture
maintenance well unless you’re a bird
Damage on structures inability to maintain posture
Posture regulating mechanisms
Maintains upright and balanced position and provides
constant adjustments needed to maintain a stable postural
background for voluntary activity
In whatever we do we maintain upright position
of the head, except when sleeping
VESTIBULO-OCULAR REFLEX or DOLL’s EYE REFLEX
(+) movement of head (+) movement of endolymph (+)
Attitudinal Reflex = Inborn
action of vestibular apparatus Crista sends impulses to
Tonic Labyrinthine reflex
Vestibular nuclei activates abducens, trochlear and
No selection, pag extend extension lahat etc
occulomotor nerve Effect: Extraocular muscles
Mostly involved in animals, little in humans
At start of rotation Abducens activates opposite side of
eyeball || Occulomotor activates ipsilateral side
Rotation towards right, tendency is you move eyeball to the
left
Corticobulbar tract
Sets of neuroncontrolling muscles in cephalic area including the neck
includes all CN except (also 1 and 2) CN 3, 4, 6 Tonic neck reflex
PRINCIPAL POSTURAL REFLEXES
To maintain equilibrium
OTHER SENSORY RECEPTORS FOR EQUILIBRIUM
Proprioceptive Receptors
o Golgi tendon Organs
o Pacinian corpuscles
o Muscle spindles
o Joint receptors
Page 76 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
o Eletrical stimulation on mastoid (painful)
Eyes/Vision activates labyrinth in temporal region
o Essential for balance maintenance if there is o OBSOLETE
abnormality in labyrinth or brainstem and
proprieceptors, if none, one will be able to Posturography
maintain balance even in the absence of vision o Platform moves on all sides vestibular and
o For us to see the relation in the environment, but retinal nystagmus is observed
this is slow, and will not help in performing rapid o Movement of extraocular muscles ((+) sensors) to
movements determine movement
o So damage in vision pero intact yung ibang o Computer records change of muscle tone
receptors slow movements
EQUILIBRIUM DISORDERS
Exteroreceptors Kinetosis/Motion Sickness
o Detects wind on the body o Most common problem
o Usually utricle problem
Vestibular nucleus o Management: lie down / tilt or bend head forward
o Has superior, lateral, medial and inferior regions when in a car
o Lateral receives impulses from utriclefor static
equilibrium Meniere’s diseas/Endolympatic Hydrops
o Superior and medial receives impulses from o Excessive production of endolymph
semicircular canal for dynamic equilibrium o Whole vestibular app is the problem including the
o Inferior receives impulses from all structures in cochlea
Vestibular App Lesion will lead to static and o Problems include Malequilibrium Vertigo
dynamic equilibrium problems
o Hearing tinnitus and Sensory neural hearing
o Lateral and Medial utricle and semicircular so
for dynamic and static for trunk and neck loss, most specifically low frequency deafness
muscle maintain normal posture of head and (problem in Apex)
body (vestibulocollic refelex) o (+) Nystagmus
o All connected to vestibular apparatus and to
different parts of the nervous system
Tinnitus Nystagmus
Ampulla is bulged Even without doing caloric
TEST FOR EQUILIBRIUM
You hear sounds even when test
Positional testing it is absent ringing Slow component always
o Tests integrity of Proprieceptors sensation moves toward the direction
o Hand (proprieceptors of dorsal cuneatus) d/t Excessive endolymph of the abnormality
that can activate organ of Fast component moves away
Romberg’s Test corti from abnormality
o Test for proprioceptors and vestibular apparatus
o Stand upright, feet together close eyes Sa samplex, included ang Past pointing for meniere’s
o Observe for swaying movements disease, so is it safe to assume that they can also experience
other post rotatory sensations such as Tendency to fall and
Barany’s Test etc? Makes sense naman diba?
o Test for Vestibular apparatus
o Utilize a swivelling or rotating chair to detect
Guys,till now, yung nakahighlight ng ganito di pa din clear,
responses from the labyrinth (vestibular apparatus)
sabe sa recordings sa isa, Neo, sabe dun sa isa Paleo, sabe sa
o Look at post rotator sensation
previous trans archi. Huhu I don’t knowww.
o Usually upright position
Caloric Stimulation
o Cheapest
o Test for the semicircular canals
o Instill warm or cold water in external ear
changes in activity of labyrinth
o Effect of convection current
o Change in temp will affect movement of
endolymph with consequent motion of cupula
Normal:
Warm water= 40-41 C
Nystagmus towards stimulated ear (fast component)
Cold water= 18-19 C
Nystagmus towards unstimulated ear(fast component)
Abnormal if no movement is elicited or no nystagmus is
seen
Remember this when irrigating an infected ear to avoid
development of nystagmus or vertigo use water with
same temp as body
o Patient is only malingering if he states that he is
experiencing vertigo
o Before doing this test, check ear first for any
problems like serumen blockage, perforations etc.
Bec nothing will be stimulated if there is any
Galvanic stimulation
o Test for semicircular canals
Page 77 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
MOTOR PHYSIOLOGY 1 o Loc: Precentral Gyrus of Frontal lobe
o Commands skeletal muscles to contract
Sources: Dr. Vila’s Lecture, Ganong’s Lecture guide, Icelimpin and Bernabe Trans
o Somatotopic map or Body Part Representation in
pre central gyrusMOTOR HOMUNCULUS
SOMATIC MOTOR SYTEM
Under Peripheral Nervous system Motor Homunculus
Cortical association area found in parietal Lobe No Specificity, Entire face and hand is mainly represented
Connection with frontal lobe (Motor function) Effect in Muscles of the face: Brachiomeric in origin, meaning they
Skeletal muscle (Voluntary motor system) are small muscles that do fine movements
Eg. Palakihan ng butas ng ilong
Law of Plasticity / Neural Plasticity The more you use it, the greater
Descending Fiber tracts
the representation in Motor homunculus
Will cause contraction of skeletal muscle, for VOLUNTARY Feet at the top of the gyrus and the face at the bottom
MOTOR SYSTEM The facial area represented bilaterally; the rest generally
From cerebrum specifically, the FRONTAL LOBE, with Inputs unilateral
from Parietal lobe Cortical motor area controls the musculature on the opposite side of
They will descend utilizing your Spinal cord and Brainstem the body.
o Corticospinal Tract The cortical representation of each body part is proportional in size
to the skill with which the part is used in fine, voluntary movement.
o Vestibulospinal
Areas for speech and hand movements are especially large in the
o Reticulospinal cortex
o Rubrospinal
Lamarck’s theory
Supplies the cranial motor nucleus o Theory of use and disuse
Commander o Frequent use Hypertrophy || Disuse Atrophy
40% Arises from Parietal assoc area
60% arises from Frontal Lobe PREMOTOR AREA
Remember: Involuntary Motor System ANS o Brodmann area #6
o Effectors: Smooth and Cardiac muscles + Glands o Loc: Lies anterior to precentral gyrus on lateral and
Pyramidal and Extrapyramidal system This terms are not used medial cortical surface of BA#4
anymore o Sets posture of complex movement get
individual prepared to move
CEREBELLUM AND BASAL GANGLIA How to write, jump, shoot etc
Command Modifiers o Also has a somatotopic map Greater
Where Action Potential are noted first representation of Contralateral eye movements,
Head rotation, hands, ear (ear daw ba?)
o Receives input from sensory regions of parietal
Cerebellum Basal Ganglia cortex and projects to primary motor area, spinal
Feedforward Mechanism Feedback Mechanism cord and brainstem reticular formation
Exact Anticipation Are you sure?
o Mostly involved in control of proximal limb
Planning of movement before Corrects and
they are initiated evaluates muscles needed to orient the body for movement
Prevents extra movements or movements as they
Contractions happen SUPPLEMENTARY MOTOR AREA
to adjust and smooth movement o Counterpart of BA # 6 & BA # 8, extension in
Where motor memory is medial side
st
“In 2018, MD naako” “After 1 shifting, Gusto ko pa o Loc: on and above the superiorbank of the
ba to? Gusto ko pa ba to? cingulate sulcus on the medial side of the
Huhuhu
hemisphere.
Lesion Intentional tremors Lesion Resting tremors
o It projects to the primary motor cortex and also
Bell Magendie Law
contains a map of the body
o Posterior Horn Sensory Function
o Antereior Horn Motor Function o For mental rehearsal of complex movement
Most Proximal/Lateral portion of anterior horn organizes and plans motor sequences
represents the most proximal/Lateral portion o Less precise than primary motor area Needs
of body respectively greater amount of stimulus to command primary
motor area to do things
5 NEURAL AREAS o Cause complex bilateral contraction
1. Cerebral Cortex 4. Spinal Cord
2. Basal Ganglia 5. Brainstem Both Primary motor and Supplementary motor area are involved in
3. Cerebellum performing voluntary movements that are complex and involves
planning
Primary Motor Executes movement
Supplementary Motor Organizes and plans motor sequences
CEREBRAL CORTEX Premotor setting of posture for complex movement
4 Anatomical Lobes
Parietal Lobe Sensory POSTERIOR PARIETAL AREA
Occipital Lobe Vision o Projects to premotor area
Temporal Lobe Hearing o Lesions of thes omatic sensory area cause defects
Frontal Lobe Motor in motor performance that are characterized by
Main Concern in Motor Sytem FRONTAL LOBE inability to execute learned sequences of
Groups of Gyri=4 1 Vertical, 3 Horizontal movements such as eating with a knife and fork.
Vertical Gyrus aka Pre central Gyrus o Concerned with aiming the hands toward an
object and manipulating it, and hand–eye
Motor Cortex and Voluntary Movement coordination
o Anterior to Central Sulcus Lesion inability to execute learned
sequences of movements. Eg, using knife and
o Occupies appx posterior 1/3 of frontal lobe fork while eating
o Contribute to the descending pathways involved in
PRIMARY MOTOR AREA motor control.
o Brodmann area #4
Page 78 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Other areas: Pars Compacta Pars Reticulata
Frontal lobeInferior frontal gyrusBROCA’S AREA Location Superior Inferior
o BA#45 Pars Triangularis NTA Domapine GABA
o BA#44 Pars Opercularis (O-four-cularis) Function Motor Vision
o Motor speech area
o also well represented since you speak everyday, Ventro Anterior(VA) and Ventro Lateral(VL) Nucleus
well unless you’re mute or whatever Functionally related to basal ganglia via Ventral group of
FRONTAL EYEFIELD AREA lateral area of thalamus
o Brodmann Area #8 Portion of thalamus used by the descending (motor) tracts
o Loc: Ant to BA #6 VA= BA # 6; Substantia Nigra, Globus Pallidus and Reticular
o Eyeball coordination, Vertical or horizontal, Formation
depending on vestibular nuclei (medulla VL= BA # 4 ;Substantia Nigra, Globus Pallidus and
oblongata) involved Cerebellum
o Lesion @ right side Nystagmus towards left side Structure NTA
STRIATUM (Caudate Nucleus and GABA(inhibitory)
Primary somatosensory cortex in the postcentral gyrus of Putamen)
the parietal lobeSensory Homunculus GPi&GPe GABA (inhibitory)
Sensory Homunculus VA & VL Nucleus Glutamate (stimulatory)
Parts of the body are represented in order along the postcentralgyrus Cortex Glutamate(stimulatory)
Legs on top and the head at the foot of the gyrus
Thalamus Glutamate(stimulatory)
The size of the cortical receiving area for impulses from a particular
part of the body is proportionate to the use of the part Subthalamic Nucleus Glutamate(stimulatory)
(+) Specificity Face particularly the Lips; Hands particularly the SubstantiaNigra: Pars Compacta Dopamine (stimulatory &Inhibitory)
thumb SubstantiaNigra: Pars Reticulata GABA (inhibitory)
Law of plasticity :Greater representation in cerebrum Greater sensitivity *For Vision*
Ideas Cortex
Planning Basal Gangli and Lateral Cerebellum
Execution Intermediate cerebellum /Spinocerebellum *Principal Connections of Basal Ganglia*
BASAL GANGLIA Dashed lines = Inhibitory || Solid lines = Excitatory
A misnomer, should be BASAL NUCLEUS since it is found in DIRECT PATHWAY INDIRECT PATHWAY
Cerebrum (CNS) Function For facilitation of Inhibition of movement Slow
Involved in the planning and programming of movement; in movement Fast motor motor activity
the processes by which an abstract thought is converted into activity Reduce Motor Activity
voluntary action Enhance Motor Activity
Feedback Mechanim Corrects and evaluates movements as Lesion Indirect pathway Direct pathway predominates
they happen leads to predominates Hyperkinesia
Influence the motor cortex via the thalamus (corticospinal Hypokinesia
pathways provide the final common pathway to motor Pathway Cerebral Cortex Cerebral Cortex releases
flow releases Glutamate Glutamate Striatum is
neurons)
Command Striatum is stimulated stimulated Striatum releases
: I will
Contract
Striatum releases GABA GPe is inhibited GPe
my Biceps GABA GPi is cannot release GABA (2 things
inhibited GPi happen)
cannot release GABA 1. GPe Will not Inhibit
No one will inhibit GPiGPi can release GABA
Thalamus Thalamus Thalamus is Inhibited
Caudate Nucleus releases Glutamate to Stop contraction
Have interconnections with frontal portion of neocortex cerebral cortex 2. GPe Will not Inhibit
Plays a role in some cognitive process Biceps Contract Subthalamic Nucleus
Putamen Subthalamic Nucleus
Part of Lentiform Nucleus releases Glutamate GPi is
Globus Pallidus stimulated GPi releases
Part of Lentiform Nucleus GABA Thalamus is
2 Portion Inhibited Stop
o Medial Globus Pallidus Interna (GPi) contraction
Projects to nuclei in brainstem to motor Dopamine STIMULATORY INHIBITORY
neurons and Drain in Spinal cord
o Lateral Globus Pallidus Externa (GPe)
Both portion contains inhibitory GABAergic neurons they
release GABA
Subthalamic Nucleus (Diencephalon)
Functionally related to basal ganglia
Substantia Nigra (Midbrain)
Functionally related to basal ganglia
2 divisions
Balance is the key for optimum functioning
Page 79 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
PARKINSON’S DISEASE Where cerebrocerebellum projects
Aka Paralysis Agitans Emboliform Nucleus & Globose Nucleus
Damage in Midbrain (BEST ANSWER) / SubstantiaNigra / Adjacent hemispheric portion of
Nigrostriatal tract / Striatum spinocerebellum
Most severely affected = Putamen *Ganong Fastigeal Nucleus
Result from the degeneration of dopaminergic neurons in Most medial
the substantianigra pars compacta No Dopamine Medial portion of spinocerebellum
Direct Pathway Affectation: DIVISIONS
No DopamineStriatum will not be able ANATOMICAL DIVISION
to release GABA No Inhibition of Anterior Spinocerebellum/ Paleocerebellum / Intermediate
GPiGPi releases GABA Thalamus is cerebellum
inhibited No Glutamate release Posterior Neocerebellum / Corticocerebellum / Cerebrocerebellum
Hypokinetic symptoms Flocculonodular Archicerebellum/ Vestibulocerebellum
Indirect Pathway Affectation: Vermis
No Dopamine Striatum will not release connects 2 cerebellar hemisphere
GABA to GPe No Inhibition of GPe Control of axial and proximal limb muscles
Regulates antigravity muscles
A. GPe releases GABA o Muscles of the neck, back, trunk and proximal
Inhibits GPiGPi will not release GABA to muscles of extremity
ThalamusThalamus releases Glutamate
Hyperkinetic Symptoms Paravermal portion/ Intermediate cerebellum
B. GPe releases GABA Regulates distal portion of extremities
Inhibitory to Subthalamic Nucleus GPi
will not be stimulated, will not release FUNCTIONAL/PHYSIOLOGICAL DIVISION (via longitudinal)
GABA Thalamus releases Glutamate
Hyperkinetic Symptoms Neocerebellum/ Corticocerebellum / Cerebrocerebellum
Newest
No Dopamine No Stimulatory for Direct Pathway + No Lateral hemisphere, with Anterior and Posterior portion
Inhibitory to Indirect Pathway INDIRECT PATHWAY For motor planning (along with premotor area) learning,
PREDOMINATES somehow motor coordination
(+)hypokinetic and hyperkinetic features Works with premotor and supplementary motor area (mental
Hypokinetic Hyperkinetic rehearsal)
Akinesia (difficulty initiating Cogwheel Rigidity
movt) Paleocerebellum / Spinocerebellum
Bradykinesia Resting tremors (pill rolling Also with anterior and posterior portion
tremors) For distal portion of extremities
Smooths and coordinates movement while being executed
prevents extra movements
HUNTINGTON’S CHOREA Formed by of the most vermis and adjacent medial portions
Initially, damage in Striatum of hemisphere
Facilitated activity of STN: Striatum is Degenerated No Receives proprioceptive input
GABA from striatum GPe will not be inhibited Receives a “copy” of motor plan from motor cortex
continuous release of GABA from GPe to GPiGPi is further Control of distal portion of the limb especially hands and
inhibited GPi will not release GABA to Thalamus fingers (lateral brainstem pathway)
Thalamus can release Glutamate Hyperkinesia
Problem in subthalamic nucleus Inc inhibition to Archicerebellum/ Vestibulocerebellum
Subthalamic Nucleus(STN) STN will not release Glutamate Oldest part
GPi will not be stimulated, no release of GABA from Flocculonodular lobe (same with anatomical)
GPiGPi will not be able to Inhibit the Thalamus Thalamus Concerned with Gait or Equillibrium in general Vestibular
releases Glutamate Hyperkinesia Input
Refer to Principal Connections of Basal Ganglia Diagram
Learning induce changesin vestibulo ocular reflex
S/Sx: Choreiform movement/ dance like movement, Slurred
Eye movement regulation (along with Frontal eyefield Area)
and incomprehensible speech, incapacitation, dementia,
Athetosis, Ballismus
Guys, inemphasize ni doc dito na ang problem talaga e dahil kay Lesion/Damage in cerebellum:
Subthalamic nucleus Incoordination
Ataxia
Dysmetria
CEREBELLUM Dysdiadochokinesia
Feedforward mechanism, Motor learning, store knowledge Intention tremors- leads to Decomposition of movement
about motor activity (motor memory) Malequilibrium
Inputs from Spinal cord, vestibular nuclei, Pons Asthenia – loss of muscle strength
Output is from deep cerebellar nuclei (specially Dentate Astasia- loss of muscle endurance
Nucleus) To ventrolateral Nucleus of Thalamus Hypotonia, Atonia
Regulate rate, range and force of contraction of muscle and Dyskinesia
even the direction of the contraction to prevent any
o Intention tremors, Dysdiadochokinesia, dysmetria BRAINSTEM
Deep Cerebellar Nuclei Midbrain, Pons and Medulla
o provide the only output for the spinocerebellum Control of axial and proximal musculature, postural muscles
and the cerebrocerebellum Regulates activity of most of your antigravity muscles
o Counterpart of basal ganglia in cerebrum muscles of proximal extremities, back, trunk and neck
Dentate Nucleus Pathways:
Most lateral, Biggest, and most active
Page 80 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Medial Descending Pathways LESIONS
o Reticulospinal Remember:
reticular formation to spinal cord o Facilitation of Lateral Corticospinal and
facilitates extensors Rubrospinal tract flexed extremities
Medial Reticulospinal tract – for ANS o Reticulospinal, Tectospinal and Vestibulospinal
regulation Extended Extremities
o Vestibulospinal
vestibular nuclei to spinal cord STROKE Bilateral Lesion in cerebrum (+) damage in
facilitates extensors lateral and medial corticospinal tract, Rubrospinal tract is
lesion loss of balance intact Flexed upper extremities, Extended Lower
o Tectospinal extremities = DECORTICATE
tectum to spinal cord
facilitates extensors
STROKEBilateral Lesion in Midbrain (+) damage
Lateral Descending Pathways
corticospinal tract, rubrospinal tract yung mga asa Medulla
o Rubrospinal
nalangang intact (sabe ni doc yan, pero sa samplex, sa pons
(midbrain)Red nucleus to spinal cord
daw) extended upper and lower extremities
Facilitates flexors of upper extremities
=DECEREBRATE
SPINAL CORD Para mag decerebrate or decorticate dapat bilateral ang
Gray matter and white matter lesion
Anterior Motor || Posterior Sensory
Damage in Medulla rarely lives because this is the location
Anterior horn cells of respiratory and cardiac centers
where the spinal cord fibers synapses
Motor neurons can be: Lesion in Tectospinal and Rubrospinal difficulty in leg
o alpha motor neurons – innervate entire turning, unresponsive pupillary light reflex, will still contrict
extrafussalfibers when asked to read, so positive saaccommodation
o gamma motor neurons – innervates Damage in level of pons Ipsilateral affectation
intrafussalfibers Damage in midbrain Contralateral affectation
o Beta motor neurons – interneurons or association
neurons; most abundant, inhibitory or excitatory
Arrangement:
PATHOLOGIC REFLEXES
o Flexor muscles, Proximal muscles medial side
o Extensor muscles, distal muscles Lateral side Manifests due to damage in descending tracts UMNL
Chaddock’s reflex
o From sheen going downward
CORTICODESCENDING PATHWAYS o Stimulation over lateral malleolus to external edge
Corticobulbar and Corticospinal both originates from cortex
of foot
o Corticobulbar – descend into brainstem bilaterally
o Corticospinal – most important output pathway from the
o Abnormal Big toe points upward, extension of
cerebral cortex great toe/dorsiflexion of great toe
60% from frontal lobe Babinski reflex
o 30% Primary motor area o Normal in infants
o 30% Premotor area o Strike from lateral side going to medial side of the
40% from Posterior Parietal lobe sole of the foot, draw an imaginary inverted J
2 Pyramidal tract o Test plantar flexion = Normal
1. Corticobulbar o Abnormal dorsiflexion of the big toe on
2. Corticospinal
stimulation of the sole, fanning of smaller toes
A. Lateral Corticospinal
descends lateral side of spinal cord, decusates at Oppenheims
level of lower medulla, o Strike from Lateral side, towards big toe *sabi ni
Considered Pyramidal (80-90%) doc
Descends with rubrospinal tract o Sabi sa Medical free dictionary (+) if dorsiflexion
regulates flexors of upper and lower extremities, of the big toe upon stroking downward along the
fine movements, distal limbs medial side of tibia
B. Medial/Anterior/Ventral Corticospinal tract
Does not decussate at the level of medulla
o Test plantar flexion = Normal
oblongata, it decussates in spinal cord
Considered as Extrapyramidal (10-20%)
Descends with tectospinal, vestibulospinal and
reticulospinal
Postural changes, adjustments
For control of axial and proximal musculature,
antigravity musles
Most of projections come from premotor cortex
Corticobulbar and Corticospinal
Primary pathway for the initiation of skilled voluntary
movement. But it does not mean that movement, even skilled
movement is impossible without it, this applies for dogs and
cats, for us humans, we need this of course.
Lateral Descending Pathway Lateral Corticospinal and
Rubrospinal tract For Flexion of upper and lower extremities
rubrospinal Upper extremity flexor only
Lateral corticospinal Upper and lower extremity flexor
Medial descending Pathway Reticulospinal (lateral part lang
yung Extensor), Vestibulospinal and Tectospinal For Extension of
upper and lower extremities
Page 81 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
P.S Nag Recordings at Lecture Guide sya, dagdagan ko lang ng Ganong notes,
plust tatanggalin ko yung ibang takaw sa space na picture maski ayaw nya.
Haha
LATERAL AND MEDIAL CORTICOSPINAL TRACT
Lateral Corticospinal Tract
“PYRAMIDAL TRACT” The reason why it is called your Pyramidal
Tract is because it decussates at the Pyramidal Decussation in your
Lower Medulla.
80-90% of Corticospinal Go down to the lateral side
Medial/Anterior/Ventral Corticospinal Tract
Included in the “EXTRAPYRAMIDAL TRACT” It does not decussate on
the pyramids. It goes straight down and decussates at the level of the
spinal cord.
10-20% Go down to the medial side Terminate in the anterior
Decussate in the Anterior White Commissure Stimulate
Anterior Horn Cells on the CONTRALATERAL SIDE
Whether it is lateral or medial/anterior corticospinal, they will
stimulate the anterior horn cells on the contralateral side. The
only difference is where they decussate.
Lateral Spinothalamic Tract Decussates at the level of the spinal cord
Decussate at the Anterior White Commissure
Page 82 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
MUSCLE SPINDLE AND GOLGI TENDON
Skeletal muscle Inside it you will find MUSCLE SPINDLE
Tendon You will find GOLGI TENDON
When you strike the tendon, you stretched the muscle Muscle
Spindle is stretched
When muscles contract, you stretch Golgi Tendon
Both are stretch receptors, but it depends how you stretch it.
MUSCLE SPINDLE GOLGI TENDON
Sensory Neuron/
IA and II IB
Sensory Innervation
The side that experienced weakness does not have full supply that is why Gamma Motor
Motor Innervation -
it only experienced weakness. Neurons
For example we are at the level of T1 At this level, you have Stretch Contraction
hemisection Anterior, Lateral and Posterior Funniculus is destroyed Stimulus (Stimulated when the (Stimulated when the
Anterior Horn Cell is destroyed So it will manifest as LOWER MOTOR muscle is stretched) muscle contracted)
NEURON LESION because you destroyed the Anterior Horn Cell itself Contraction/Tension
Stretching of the built by the muscle
What about Below the level of T1? anterior horn cells are not Monitors
muscle during muscle
destroyed There would still be supply to their descending tract (10%) contraction
UPPER MOTOR NEURON LESION
If it is a sensory receptor, it is innervated by sensory neurons. Muscle
Spindles are an exemption. They are also innervated by motor
neurons. It is also innervated by Gamma Motor Neurons.
What is the reaction of your muscle when you stimulated it? CONTRACT
What happened when it contracted? STRETCH/RELAX
How I understand it : When you stretch your muscle Muscle spindle
works after some time It will contract After contractions Golgi
tendon works muscle relaxes
MUSCLE SPINDLE
Stretch sensitive receptor
Feedback circuit for muscle length
Consists of thin intrafusal muscle
fibers attached to the associated
muscle fibers which surrounds the
muscle spindle.
Inside the muscle spindle
Intrafusal Fiber
Whole muscle Extrafusal
Fiber
Intrafusal Muscle Fibers are devoid
of actin-myosin contractile
elements. They form a capsule
containing several nuclei.
─ When nuclei are arranged in a
linear fashion NUCLEAR CHAIN
─ When nuclei are clustered or
KNEE JERK REFLEX (PATELLAR-TENDON REFLEX)
clumped in the central region
When you elicit a knee jerk reflex, what stretch receptors are you
NUCLEAR BAG
stimulating? MUSCLE SPINDLE
How do you elicit patellar tendon reflex?
As mentioned earlier, muscle spindle is quite unique It has
1. Ask the patient to sit on a high chair Make sure that the legs are
both sensory and motor innervation Motor Innervation:
hanging
Gamma Motor Neuron Gamma Motor Neuron Supply
If there is no high chair, ask the patient to cross his/her legs
Intrafusal Fibers Both Nuclear Chain and Bag Why? In its
2. Using the reflex hammer, tap the patella
end, it has actin and myosin filaments That is why it is
Not totally at the patella Tendon will only pass through it (Tendon
stretched and return to its normal
is near the patella)
Golgi Tendon When it is stretched, it does not return No
When you strike the reflex hammer You stimulate the MUSCLE
actin and myosin filaments, what they have is connective tissue
SPINDLE first
That is why muscle spindle has an efferent innervation and golgi
tendon doesn’t.
Page 83 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Structures of muscle spindle and group II neurons neurons
Remember: Innervated by static gamma Innervated by Dynamic gamma
2 types of intrafusal fibers: motor neuron motor neuron
o Nuclear bag fibers, also with 2 subtypes --- Oppose sudden changes in
Static nuclear bag muscle length
Dynamic nuclear bag steady-state length of the speed of movements
o Nuclear chain fibers
muscle and allow for quick corrective
2 kinds of sensory endings
movements.
o Primary (group Ia)
Wraps around the center of the dynamic
DYNAMIC RESPONSE
and static nuclear bag fibers and nuclear
Primary Endings Responsible for DYNAMIC RESPONSE
chain fibers. In short, sa lahat mag wrap sya
o Rate of the change or velocity of the change in the
o Secondary (group II)
length
Located adjacent to the centers of the static
Dynamic Reflexes = Rate in the change of muscle length
nuclear bag and nuclear chain fibers; these
fibers do not innervate the dynamic nuclear
STATIC RESPONSE
bag fibers.
Secondary Endings and also Primary Endings Responsible for
Dynamic nuclear bag is only innervated by Group 1a or primary
STATIC RESPONSE
sensory endings
o Maintain length of muscle fiber
Nuclear chain is supplied by both Ia and II
For maintenance of the length of the muscle which is contracting
2 types of gamma motor neuron
Which is the one that gives the signal that the muscle is
shortening and lengthening / Isotonic contractions Primary
Dynamic gamma motor neuron Static gamma motor neurons
Endings (Ia)
Supply dynamic nuclear Supply static nuclear bag
When you maintain a certain length / Isometric contractions ( you
bag fibers fibers and the nuclear chain
don’t change muscle length) Secondary Endings (II)
Activation of this fibers
increases the dynamic Activation of this increases the
sensitivity of the group tonic level of activity in both
Ia endings group Ia and II endings
decreases the dynamic
sensitivity of group Ia
afferents, and can prevent
silencing of Ia afferents during
muscle stretch
Two types of sensory fibers are associated with muscle spindle
intrafusal muscle fibers:
PRIMARY ENDINGS (Ia) SECONDARY ENDINGS (II)
Annulo Spiral Flower Spray
Type Ia myelinated sensory fiber Type II myelinated sensory fiber
Innervates both the Dynamic & Innervates only the nuclear
Static nuclear bag and nuclear chain fibers and the Static
chain nuclear bag
Detects amount of muscle Not sensitive to rate of change
stretch but more sensitive to of muscle length but provides
the rate of change of muscle information about the static
length length of the muscle
Velocity sensitive fibers --
STRETCH REFLEX
─ Type Ia sensory fibers conduct impulses to the spinal cord entering
the dorsal root and synapse directly (monosynaptic) with alpha
motor neurons in the ventral horn that conduct impulses to the
extrafusal muscle fibers in the same muscle where the type Ia fibers
originated.
─ Also known as MYOTATIC REFLEX which results to contraction of the
Size Principle The firs one to be recruited is your slow twitch
stretched muscle
type I muscle since the size is small
─ Stretch Reflex has two components: DYNAMIC PHASE AND STATIC
Slow twitch muscle – for Marathoners
PHASE
Fast twitch muscle Sprinters
STATIC PHASE (RESPONSE) DYNAMIC PHASE (RESPONSE)
GOLGI TENDON
Weak, slow, continuous Strong, sudden stretch of the Tension sensitive encapsulated receptors which consist of a net like
stretch of the muscle spindle muscle spindle For carrying collection of knobby nerve endings among the fascicles of a tendon
For posture and balance load, when doing work arranged in series with the extrafusal muscle fibers
Involves almost equal activity Involves activity mostly of the Intermingle with the tendon fibers
of the static nuclear bag and dynamic nuclear bag; same Stimulated when the tension imposed by muscle contraction is
nuclear chain activity of the nuclear chain increased
Involves activation of group Ia Greater activity of the group Ia
Page 84 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Like the muscle spindle, the golgi tendon organ reacts vigorously when
the tendon is undergoing stretch (dynamic response) and then settles
down to a steady state level that is proportional to the degree of
tension (static response)
Stimulated by pressure stretch and active contraction
Low threshold
Functions as transducers in feedback circuit that regulates muscle force
RENSHAW CELL
TYPES OF MOVEMENT GENERATED BY MOTOR SYSTEM ─ Interneuron Release inhibitory neurotransmitter Inhibit
both stimulatory and inhibitory
VOLUNTARY MOVEMENT
Voluntary ─ It doesn’t mean that when it is inhibitory, it is really inhibited
When you inhibit the inhibitor = stimulation
Movement is purposeful
Learned ─ this circuitry prevents refl ex stimulation of the extensors when
flexors are active
REFLEXES
─ Prevents clonus
Rapid
Stereotype
Involuntary DYNAMIC REFLEX
Sensory Neuron: Ia Primary Afferent Supplying both static and
RYTHMIC MOTOR PATTERNS
dynamic Nuclear Bag and Nuclear Chain (Intrafusal Fiber)
Stereotype
Repetitive
Static Reflex Secondary Afferent Supply on the Nuclear
Confer initially as fast repetitive Eventually stops
Chain and static nuclear bag
Can be seen in pathologic conditions, especially in an upper motor
neuron lesion
INVERSE MYOTATIC
Disynaptic
Upper Motor Neuron Lesion Comatose patient (CVA,
hemorrhage) Try to dorsiflexthe foot for some time
Release Knee-Jerk Reflex Stretch muscle (MYOTATIC) Reaction:
Normally: It would return Contraction Stimulate INVERSE MYOTATIC
Reflex-like
In comatose patient, when you release it It would return,
but it would have repetitive movements until it stops Receptor: Golgi Tendon
REFLEX Sensory Neuron: Ib
Receptor Sensory Neuron Motor Neuron Effector (Skeletal Center: Spinal Cord
Muscle)
RECEPTOR:Muscle Spindle, Golgi Tendon, and Free Nerve Endings (PAIN)
or sometimes touch We know that there is no motor neuron that innervates golgi
tendon, however, there is a motor neuron in inverse myotatic
reflex. It is a reflex, so it just doesn’t end at the center (it should
have a receptor, sensory neuron, center, motor neuron and an
effector).
Motor Neuron: Alpha Motor Neuron
Effector: Skeletal Muscle
SENSORY / RECEPTOR ORGAN:Muscle Spindle, Golgi Tendon, Free Nerve
Endings WITHDRAWAL REFLEX
AFFERENT NEURON: I, II III, IV Reflex when you are trying to avoid noxious stimulus
CENTER: Spinal Cord (if it is a spinal cord reflex) Withdraw Usually a flexor reflex
EFFERENT NEURON:Alpha or Gamma Motor Neuron Polysynaptic Involves the contralateral and ipsilateral leg
EFFECTOR: Skeletal Muscle Receptor: Pain Receptor (Free Nerve Endings)
Sensory Neuron: Spinal Nerve
Center: Spinal Cord
TYPES OF REFLEX Motor Neuron: Alpha Motor Neuron
MYOTATIC REFLEX Monosynaptic Effector: Skeletal Muscle
INVERSE MYOTATICDisynaptic
WITHDRAWAL REFLEX Polysynaptic
MYOTATIC REFLEX
Monosynaptic Example: KNEE JERK REFLEX
Receptor: Muscle Spindle
Sensory Neuron: Dorsal Root Ganglion Ia and II
Center: Spinal Cord
Motor Neuron: Alpha Motor Neuron
Effector: Skeletal Muscle
Muscle spindle is innervated by Gamma motor neurons
So if ang tanong is direct innervation of muscle spindle Gamma
RECIPROCAL INHIBITION motor neurons
─ When you stimulate the flexor, you inhibit the extensor Golgi Tendon has no motor neurons
─ You cannot stimulate both flexor and extensor at the same time Extrafussal fibers or whole muscle are innervated by Alpha
motor neuron
If mga reflex, eg: Myotatic, reverse myotatic and withdrawal
reflex Alpha motor neuron
Muscle spindle: 1a and II
Golgi Tendon: 1b
Page 85 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
THERMOREGULATION TEMPERATURE READINGS
Source: recordings + Limpin notes Average body temperature
BODY TEMPERATURE o calculates total amount of heat stored in the body
o difference between heat produced & heat lost by = 1/3 surface T + 2/3 core T
the body
o Normal range = 36.7 – 37.1 C Core Temperature Vs. Skin/Surface Temperature
o Most common temp taken
Importance of maintenance of Body Temp:
o Metabolic process Core Temp Skin/Surface Temp
Inc temp Inc metabolism Core temp of deep tissues = constant depends on the temperature of the
varying less than 1 F under normal environment Varies widely
The body is the one that maintains
condition Almost constant, no wide
metabolic process it cannot be variations Eg: Dec environment temp body
controlled by temperature of the temp also decreases
environment This is the Internal environment of the
o Enzyme system body : organs with blood flowing Inc environment temp body temp
Body depends on the enzymes system thorough it also increases
present in the body
CNS maintained
Extreme temp Enzymes are very
fragile and can be broken down easily Big Variation between Skin temp and Core Temp In a matter of
The Body temp is also able tomaintain time Core temperature will compensate
the function of the enzymess system
HEAT PRODUCTION: Factors that Inc Temp
TEMPERATURE VARIATIONS BMR- MAIN FACTOR
Various parts of the body or different sites: Extra metabolic production of heat Muscular exercise
Oral, axillary and Rectal Specific dynamic action of food
o Oral temperature o with corresponding caloric equivalent
Influenced a by breathing, drinks o Inc caloric equivalent in fat then protein and
always from the internal environment of lastly Carbohydrates
the body Cooler Sympathetic stimulation
Considered as superficial o Epinephrine and Norepinephrine elaboration
o Axillary Temp Inc heat production
Considered as superficial Hormonal stimulation
o Rectal Temperature o endocrine cause like thyroxine etc Inc heat
Highest, represents core temperature production
Not very accurate reading because of Infections, Drugs & anesthetics
bacteria unusually high temp
o Tympanic membrane HEAT TRANSFER
Facilitated by physical loss of heat
Temperature from oral to axillary – difference of 0.5 centigrade 1. Radiation (60%)
Temperature from axillary to rectal difference of 0.5 centigrade o Heat loss thru heat waves, no direct contact of
Temperature from oral to rectal – a difference of 1 centigrade body & the wall
Temperature from outside towards inside of the body 2. Conduction (air 15%,objects 3%)
increases o With direct contact between 2 surfaces
There is consistency in these Variations of temperature o Eg: when you seat down on a cold chair direct
movement of heat towards the chair since the
Time of Day body has higher temperature than the chair
o circadian rhythm= 0.5-0.7 C fluctuations
o Early Morning 3. Convection
Still in bed, not doing anything Basal o utilizes air movement
Temperature o Eg: When a person is on cool environment air
Lowest temperature movement from the body towards the
o Early evening (6-7pm) environment
done all physical activities throughout
the day Inc temp and BMR 4. Insensible water loss and Sweating or Evaporation (27%)
Highest temp o even if seating on the chair only there is
perspiration
Hormonal influence
o Ovulation period 5. Respiration (2%)
Morning: Lowest basal Temp then o observed in animals
temperature spurts o not very useful in human unless aso ka
Inc temp= increase possibility to get
pregnant (female is probably ovulating) 6. Via Urine and Feces (1%)
So Temperature here can serve as a Rhythm for family
planning Transfer of heat is from a higher temperature to lower
temperature, it depends on which has a higher gradient or
Age in Children whic is warmer
o Children usually have higher BMR (Basal o If Environment Temp higher than body Transfer
Metabolic Rate) Higher temperature of heat is from environment to the body
o If the environment temp is lower than the body
Constitutional Hyperthermia
transfer of heat is from the body to the
o Seen in some normal adults
o Normally high body temperature even without a environment
cause
Page 86 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
ADAPTABILITY TO TEMP CHANGES o came from the inner surface of the body warm
Poikilothermic Vs. Homeothermic
Poikilothermic Homeothermic As blood goes along artery has close contact with venous
Eg. Cold blooded animals Eg. Human beings, except plexuses : if the temp is cold
newborn/infants o Venous plexuses will prevent the warm blood
Body temp depends on the temp of
the environment going to the artery to go to the skin
No means of maintaining body
With means of maintaining body o There is transfer of heat from the artery to venous
temperature and no compensation temperature
plexus & carried back to the interior part of the
body
Newborns or infants are considered as poikilothermic
o Coping up mechanism is immature o There is a conservation of heat from a mixture of
o no adequate means of maintaining body direction from the artery to the vein
temperature + body temperature is maintained
rudimentarily When BV constrict it prevents the blood going to the skin &
o So when exposed to cold temperature lead to the warm blood goes towards the artery so less blood is
hyperthermia and eventually dies
going to the skin
Adaptive Mechanism
Specific physiological mechanism 2 Mechanisms:
Employed by the body towards the vessels A. Counterheat Mechanism
o Cold place VASOCONTRICTION heat is o direct transfer of heat from the artery to venous
conserved plexus, to conserve heat
o Hot place VASODILATION Increases heat loss B. Constriction of Blood Vessel
Cold temp (+) Shivering Inc contraction of muscle o prevents the arterial blood to go to the skin
(uncoordinated) Increases BMR Inc Body heat
o Conserves a lot of heat
Brown fat For Non-shivering thermogenesis (NST)
o found in body especially used for newborn
Sweating When Temp is warm
o Compensation for hyperthermia o (+) Vasodilation more warm blood goes to
skin heat loss
Types of Fat
TEMPERATURE REGULATING MECHANISM PART 1
Structural Neutral
Cold related mechanisms to increase heat production:
Found in different parts of the body Found in waistline = Bilbil
Shivering
Eg: cells, cell memembrane nerves, all Contains many mitochondria, o Increases BMR 300-400x
that has lipid component sympathetic innervations & Blood o Problem: Inc BMR There is Inc in
vessels oxygen demand, so people with chronic
Brown Fat White Fat heart disease can’t tolerate the decrease
Specialized fat for baby Appears during adult life in oxygen may lead to Ischemia
o Only seen in adults,
Very rich tissue with a lot of Also contains Lipid droplets Hunger
mitochondria, nuclei & lipid droplets
with a lot of sympathetic innervations, Also have sympathetic stimulation
o food caloric equivalent is a natural
blood vessels all around response mechanism
Found in inner structure like thorax, o Inc caloric equivalent Inc heat
Means of the body to maintain heat abdomen & shoulder production
especially in newborn(baby) o Mas malamig mas masarap kumain
Voluntary activity
no sufficient heat limited only In adults, brown fats Inc catecholamine secretion (Epi & NEpi)
disappears o Remember: Cold is a form of physical
upon sympathetic stimulation (cold)
catecholamine released most stress Inc release of catecholamine
specifically norepinephrine Inc sympathetic stimulation Inc BMR
breakdown of energy substrates inc Inc heat production
heat production
ENERGY EXPENDITURE CHANGES WITH ENVIRONMENTAL TEMP
SKIN RADIATOR SYSTEM 1. Zone of thermoneutrality
Skin together with subcutaneous fat (especially the fats)
o temperature of the body where energy
o Very important for conservation of heat
expenditure is almost zero
o Fat is a very good insulator
o Important for children
they are not a good medium for heat
transfer Eg: Baby in a very cold operating room + cold IV fluids
Baby will try to compensate to Inc heat production by any means
8 fold difference in heat conduction between maximum o This adaptive mechanism can lead to failure on the
dilation & maximum constriction system of the baby because the baby cannot response
o Inc temp vasodilatation high heat adequately to that condition
conduction o Baby needs a higher the temperature, so we try to find
temperature where energy expenditure is almost zero.
o Dec temp vasoconstriction low heat
conduction
2. Sweating in Hot; Shivering in Cold
o Uses energy
ROLE OF SKIN BLOOD FLOW IN TEMPERATURE REGULATION
Blood going to the arteries
TEMPERATURE REGULATING MECHANISM PART 2
Page 87 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Cold related mechanisms to decrease heat loss: Efficient receptors/ effector organ
Cutaneous vasoconstriction o Cold environment detected by cold
o less blood is exposed to the skin receptors send impulse brain adapt to
low temperature regulate organs
Curling up
adaptive mechanisms takes place correct
o maintain fetal position dec body surface
area dec heat loss the low temperature Inc temp
Horripilation (goose bumps/goose flesh) TYPES OF BODY RESPONSE
o Normally: the hair in skin is slant position 1. Behavioral response
o When exposed to cold arrector pili contract o occurs mostly as a response to skin temperature
hair moves up (upright) skin thickens changes
dec heat loss
Eg: cold wear a jacket or rub hands together
COUNTER CURRENT HEAT EXCHANGE
Direct transfer of warm blood 1. Autonomic response
o Heat Transfer=artery to vein without blood going o occurs as a response to core temperature changes
to skin o Responsible in 80% of cases
Direct constriction o Includes vasoconstriction, vasodilatation,
o preserves heat of the body sympathetic & thyroid stimulation as well as
increasing catecholamine, sweating, shivering
Mechanism Regulated by Heat Mechanism Activated by heat Interthreshold change
To Inc Heat Loss To dec Heat production o Narrow range of core temperature maintained by
Cutaneous Vasodilation Anorexia hypothalamus
Sweating Apathy o not triggered by autonomic response
Increase Respiration (common in Inertia
animals) PHASES OF TEMP INFORMATION PROCESSING
1. Cold receptor – C & A delta fibers;
Heat receptor – C fiber
Heat loss from body when environmental Temp is greater
2. Afferent thermal sensing
than body temperature
o Heat Transfer is from high temp to low temp 3. Via Spinothalamic tract
o You tend to sweat to lower the body temp 4. Center: Preoptic area/ anterior hypothalamus
Heat center
SWEATING Post hypothalamus
A form of evaporative heat loss Received impulses from anterio
(+) Stimulation of PREOPTIC AREA of hypothalamus via hypothalamus and periphery
sympathetic preganglionic cholinergic fibers sweating is Cold center
stimulated Heat producing and heat conserving
Circulating NEpi & Epi
2 components of sweat gland Extremes of temperature will lead to pain sensation
1. Deep subdermal coiled portion There is more cold receptors than heat receptors more
o secretes sweat dangerous kasi ang hypothermia
2. Duct portion Most of the deep body receptors are cold receptors
o passes outward thru the dermis & epidermis of
skin BODY TEMP DETECTION
Primary Secretion is similar to plasma but modified (no HYPOTHALAMUS TEMPERATURE CONTROL CENTER
proteins) as it passes up towards the skin where there is o Via Preoptic area of anterior hypothalamus
absorption of NaCl o Heat sensitive & cold sensitive neurons
Light sweating Dec Na secretion, narereabsorb kasi
Increased or excessive sweating Inc Na Secretion SKIN & DEEP BODY TEMPERATURE
o Mainly detects cold & cool temperatures
As sweat comes out: Na along with water is reabsorbed o Function to prevent hypothermia
dec secretion of Na along with water in sweat
During strenuous exercise sweat comes out fast so POSTERIOR HYPOTHALAMUS
reabsorption does not take place (mabilis kasi) Inc NaCl as o Receives input from anterior hypothalamus &
well as water secretion peripheral temperature receptors to elicit mainly
In case of excessive sweating there is a possibility of having heat producing & heat conserving reactions
dehydration
PATHOLOGIC CONDITIONS
TEMPERATURE CENTERS Fever
Posterior Hypothalamus o Oldest, universally known Hallmark of disease
Preoptic area of hypothalamus ( Anterior Hypothalamus) o Temp above 100° F/ 38° C
o Thermostat is set at higher level activating
Temp Regulation thru feedback mechanism temperature raising mechanism
Always via a negative feedback to counteract temperature o (+) Chills & shivers
Working center/area i.e brain FEVER – Resetting Set Point Temperature
Page 88 of 89 By: Ayesha Bea Federizo Batch 2017
GRAND PHYSIOLOGY B FINALS REVIEWER
Pyrogens Can Directly Reset Point Pyrogens Can Indirectly Reset Point HYPOTHERMIA
Temp Temp Heat regulation is lost at 85°F/29°C
Bacteria Liposaccharides are Interleukin 1 released from phagocytes In a man exposed to ice water for 20-30 minutes Cause of
pyrogens following phagocytosis of blood borne death is cardiac standstill
Pyrogens from degenerating tissue pyrogens Causes Frost bites,
o Due to formation of microcrystal in cells
Interleukin 1 reset set point of temp by o usually affects ear lobes
increasing production of Prostaglandin
E2 (PG E2)
o Gangrene may follow after thawing
Phatogenesis of Fever
Tissue becomes infected with bacteria, viruses, etc
WBC/leukocyte responds to infection & releases a protein
called IL-1 or Interleukin 1 IL-1 stimulates the production
of PROSTAGLANDIN E1 and PROSTAGLANDIN E2
Prostaglandins cross the blood brain barriers and signals the
Preoptic Area or Ant Hypothalamus Inc Set point brain
perceives that body is cold (+) chills and shivering Fever
Time Course of Fever
If baby has cold
feet (+) vasoconstriction as
a means of compensation
prone to fever
Aspirin prevents or
inhibits prostaglanding
production
Benefits of Fever
Acts as warning signal for the presence of disease processes
High Temp Inc in Antibody production
Slows growth of some tumor
Limits of Survival
Extreme Temp: Very High/Low FATAL
Hyperthermia may lead to heat sroke
HEAT STROKE
Above critical temperature of 106-108° F / 41-42 C
S/Sx:
o dizziness, abnormal distress, delirium & coma
Death is usually due to circulatory collapse
Remember: the Limit of temperature one can withstand
depends on the humidity of air
Water – good medium for heat, it absorbs heat from
environment
HUMIDITY – amount of water in air
MALIGNANT HYPERTHERMIA
Usually happens to young and newborn, but also happens to
adults
o Associated with congenital anomalies
A rare case, Fatal if not recognized early
Triggered by traumatic events, most commonly triggered by
drugs
Familial
o include 2 or more members of the family
(+) Disorder in Ca metabolism
o Ca from Sarcoplasmic Reticulum release Ca
actin/myosin causes contraction Ca does not
go back to Sarcoplasmic Reticulum persistent
muscle contraction Inc muscle metabolism Inc
heat production
Problem in ryanodine receptors
S/Sx: Severe fever, tachycardia, arrhythmia, rigidity, Inc muscle
metabolism
ManagementDantrolene Sodium (muscle relaxant) very
expensive, has short life and short expiration
o Effective when given early
Page 89 of 89 By: Ayesha Bea Federizo Batch 2017
Das könnte Ihnen auch gefallen
- Reflex Facilitation: Vol Control of Micturition (Corticol Areas) Control EUS & Abd MDokument1 SeiteReflex Facilitation: Vol Control of Micturition (Corticol Areas) Control EUS & Abd MTharani KumaraNoch keine Bewertungen
- MicturitionDokument7 SeitenMicturitionOsama MohamedNoch keine Bewertungen
- Patterns of RespirationDokument67 SeitenPatterns of Respirationsteven hkNoch keine Bewertungen
- Cardiac Action PotentialDokument41 SeitenCardiac Action PotentialRadijska Postaja KoprivnicaNoch keine Bewertungen
- Anatomy Dec 2019 - One LinersDokument19 SeitenAnatomy Dec 2019 - One LinersJijoNoch keine Bewertungen
- Focal Atrial Tachycardia I: Clinical Features, DiagnosisDokument10 SeitenFocal Atrial Tachycardia I: Clinical Features, Diagnosisapi-26166949Noch keine Bewertungen
- 4.03 Anti-Arrhythmic Drugs PDFDokument8 Seiten4.03 Anti-Arrhythmic Drugs PDFKarl ChavezNoch keine Bewertungen
- Spinal and Epidural Anesthesia: Jedarlyn G. Erardo, RPH, MDDokument101 SeitenSpinal and Epidural Anesthesia: Jedarlyn G. Erardo, RPH, MDjedarlynNoch keine Bewertungen
- Cerebral Spinal Fluid & The MeningesDokument25 SeitenCerebral Spinal Fluid & The MeningeschintyamontangNoch keine Bewertungen
- Anatomy of AirwaysDokument6 SeitenAnatomy of Airwaysgdubs215Noch keine Bewertungen
- 2 ThoraxDokument7 Seiten2 Thoraxapi-3757921Noch keine Bewertungen
- 24 Cerebral Blood FlowDokument31 Seiten24 Cerebral Blood FlowZuhaib Ahmed100% (1)
- Anatomy of Cerebral Blood Supply & Cerebral PhysiologyDokument32 SeitenAnatomy of Cerebral Blood Supply & Cerebral Physiologykiran kizhakkiniNoch keine Bewertungen
- Describe The Factors Affecting Cardiac OutputDokument6 SeitenDescribe The Factors Affecting Cardiac OutputSis SukarnoNoch keine Bewertungen
- Physio Coursepack 2016Dokument282 SeitenPhysio Coursepack 2016Amanda KimNoch keine Bewertungen
- Physio-DES-6 (Cardiac)Dokument56 SeitenPhysio-DES-6 (Cardiac)Joseph Kim100% (1)
- Neurology Work BookDokument73 SeitenNeurology Work BookCastleKGNoch keine Bewertungen
- Symptom Flow Chart (Difficulty Breathing)Dokument2 SeitenSymptom Flow Chart (Difficulty Breathing)Jeff ZhouNoch keine Bewertungen
- PRES (Posterior Reversible Encephalopathy Syndrome) and Eclampsia-ReviewDokument5 SeitenPRES (Posterior Reversible Encephalopathy Syndrome) and Eclampsia-ReviewAvicena M IqbalNoch keine Bewertungen
- Cardiovascular Physiology Review QuestionsDokument44 SeitenCardiovascular Physiology Review QuestionsTim100% (1)
- Pericardial EffusionDokument3 SeitenPericardial EffusionNita Hurek100% (1)
- Pediatric Anesthesia For StudentsDokument4 SeitenPediatric Anesthesia For StudentsMarco TolentinoNoch keine Bewertungen
- Lung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesVon EverandLung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesAlain JunodNoch keine Bewertungen
- Heart MuscleDokument10 SeitenHeart Muscle22194Noch keine Bewertungen
- Pons MedullaDokument32 SeitenPons MedullaEnaWahahaNoch keine Bewertungen
- 337 Pdfsam NMS PhysiologyDokument166 Seiten337 Pdfsam NMS PhysiologydrpnnreddyNoch keine Bewertungen
- Using The ACLS Primary Survey For A Patient in Respiratory ArrestDokument34 SeitenUsing The ACLS Primary Survey For A Patient in Respiratory Arrest강기연100% (1)
- Jugular Venous PressureDokument9 SeitenJugular Venous Pressuremoh86-Noch keine Bewertungen
- PONS: NeuroanatomyDokument20 SeitenPONS: NeuroanatomyHassan IlyasNoch keine Bewertungen
- Short and Long Term Regulation and Determinants of BPDokument90 SeitenShort and Long Term Regulation and Determinants of BPDan Tristam MicabaloNoch keine Bewertungen
- Endocrine Notes - All in One FileDokument182 SeitenEndocrine Notes - All in One FilekjNoch keine Bewertungen
- Algorithms of Care (Myocardial Infarction)Dokument3 SeitenAlgorithms of Care (Myocardial Infarction)Julius Delos SantosNoch keine Bewertungen
- Difficult Weaning From Cardiopulmonary Bypass Final Edit LiaDokument41 SeitenDifficult Weaning From Cardiopulmonary Bypass Final Edit LiaYuri SadewoNoch keine Bewertungen
- Anes Preoperative-AssessmentDokument6 SeitenAnes Preoperative-AssessmentChristine Mendoza100% (1)
- Md2024 Physio SamplexDokument11 SeitenMd2024 Physio SamplexSHAN-SHAN CHANGNoch keine Bewertungen
- Paediatric Notes - Moodle/Text: Paediatric Emergencies (Textbook Ch.5)Dokument6 SeitenPaediatric Notes - Moodle/Text: Paediatric Emergencies (Textbook Ch.5)Jana AldourNoch keine Bewertungen
- Cholinergic Agonists/ Cholinomimetic Agents: Dr. Kyi Kyi Tha Basic Medical Sciences Kulliyyah of Pharmacy IiumDokument21 SeitenCholinergic Agonists/ Cholinomimetic Agents: Dr. Kyi Kyi Tha Basic Medical Sciences Kulliyyah of Pharmacy IiumZhuan AhmadNoch keine Bewertungen
- Bates Outline of Chapter 8Dokument15 SeitenBates Outline of Chapter 8KatherynSotoNoch keine Bewertungen
- FBC Interpretation and Function of Blood ComponentsDokument7 SeitenFBC Interpretation and Function of Blood ComponentsFrancesca LiNoch keine Bewertungen
- HEENT Cheat SheetDokument22 SeitenHEENT Cheat SheetKatrina FeriNoch keine Bewertungen
- Physical ExaminationDokument55 SeitenPhysical Examinationdakshpanchal26369Noch keine Bewertungen
- Esap 2010Dokument107 SeitenEsap 2010Χρήστος ΣαββίδηςNoch keine Bewertungen
- 2 - Renal PhysiologyDokument8 Seiten2 - Renal PhysiologyKunware TropaNoch keine Bewertungen
- B4 DyspneaDokument100 SeitenB4 DyspneaAnonymous HH3c17osNoch keine Bewertungen
- Table of 12 Cranials and TractusDokument5 SeitenTable of 12 Cranials and TractusjuwitavalenNoch keine Bewertungen
- Classification of Nerve FiberDokument21 SeitenClassification of Nerve FiberNayab IftikharNoch keine Bewertungen
- NMB MyDokument91 SeitenNMB MyGirish Bk B KNoch keine Bewertungen
- 1 - Anatomy of The KidneyDokument15 Seiten1 - Anatomy of The Kidneysara khanNoch keine Bewertungen
- Basics of Chest X-RayDokument44 SeitenBasics of Chest X-RayvmamikonNoch keine Bewertungen
- Head Injury 1Dokument33 SeitenHead Injury 1drvishal bhattNoch keine Bewertungen
- Acid Base PhysiologyDokument1 SeiteAcid Base PhysiologyPrabjot SehmiNoch keine Bewertungen
- Assessment of The Chest and LungsDokument46 SeitenAssessment of The Chest and LungsSumathi GopinathNoch keine Bewertungen
- Guyton and Hall Textbook of Medical Physiology 13th Ed (2015) - 974-1006Dokument33 SeitenGuyton and Hall Textbook of Medical Physiology 13th Ed (2015) - 974-1006siñthiNoch keine Bewertungen
- Ransport Of: Dr. Roopa Kotha Dr. Shaji MathewDokument36 SeitenRansport Of: Dr. Roopa Kotha Dr. Shaji MathewRenganathan SockalingamNoch keine Bewertungen
- Histology of GIT Part 2 Stomach PDFDokument27 SeitenHistology of GIT Part 2 Stomach PDFJeffrey RamosNoch keine Bewertungen
- 20 - Toronto Notes 2011 - Ophthamology PDFDokument46 Seiten20 - Toronto Notes 2011 - Ophthamology PDFSisterzzShopDua0% (1)
- AnisocoriaDokument11 SeitenAnisocoriaChaturangaNSenerathNoch keine Bewertungen
- Aldwin A. Yaneza, MD Course Director. Gross AnatomyDokument40 SeitenAldwin A. Yaneza, MD Course Director. Gross AnatomyfilchibuffNoch keine Bewertungen
- Patho OB - Breech DeliveryDokument7 SeitenPatho OB - Breech DeliverySheryl Layne Lao-SebrioNoch keine Bewertungen
- Cardio - ECGDokument13 SeitenCardio - ECGSheryl Layne Lao-SebrioNoch keine Bewertungen
- 1.acute Respiratory Disease: DDX: Kawasaki, Strep. InfectionDokument5 Seiten1.acute Respiratory Disease: DDX: Kawasaki, Strep. InfectionSheryl Layne Lao-SebrioNoch keine Bewertungen
- Most Common Complication: Sabay SilaDokument6 SeitenMost Common Complication: Sabay SilaSheryl Layne Lao-SebrioNoch keine Bewertungen
- Finals PHARMACOTHERAPHY OF DIABETES MELLITUS 2017Dokument8 SeitenFinals PHARMACOTHERAPHY OF DIABETES MELLITUS 2017Sheryl Layne Lao-SebrioNoch keine Bewertungen
- EndoDokument8 SeitenEndoSheryl Layne Lao-SebrioNoch keine Bewertungen
- 9 Topnotch Internal Medicine Superexampdf PDFDokument95 Seiten9 Topnotch Internal Medicine Superexampdf PDFSheryl Layne Lao-Sebrio100% (1)
- IGCSE-Revision-Booklet-Part-1-2018-2019 - (New-Spec)Dokument69 SeitenIGCSE-Revision-Booklet-Part-1-2018-2019 - (New-Spec)MaryamNoch keine Bewertungen
- 1040 A Day in The Life of A Veterinary Technician PDFDokument7 Seiten1040 A Day in The Life of A Veterinary Technician PDFSedat KorkmazNoch keine Bewertungen
- Article WritingDokument10 SeitenArticle WritingmutabargaybullayevnaNoch keine Bewertungen
- Grammar Summary Unit 8Dokument2 SeitenGrammar Summary Unit 8Luana Suarez AcostaNoch keine Bewertungen
- Carr v. NH State Prison, Warden - Document No. 2Dokument5 SeitenCarr v. NH State Prison, Warden - Document No. 2Justia.comNoch keine Bewertungen
- DAA R19 - All UnitsDokument219 SeitenDAA R19 - All Unitspujitha akumallaNoch keine Bewertungen
- The Spartacus Workout 2Dokument13 SeitenThe Spartacus Workout 2PaulFM2100% (1)
- Contoh DVDokument5 SeitenContoh DVHiruma YoishiNoch keine Bewertungen
- Technical Activities: Ken Goldberg, VP Technical Activities Spring 2007, ICRA, RomeDokument52 SeitenTechnical Activities: Ken Goldberg, VP Technical Activities Spring 2007, ICRA, RomeWasim Ahmad KhanNoch keine Bewertungen
- Latihan Soal CausativeDokument1 SeiteLatihan Soal Causativeanakosagista anakosagistaNoch keine Bewertungen
- Paras Vs ComelecDokument2 SeitenParas Vs ComelecAngel VirayNoch keine Bewertungen
- Sales Manager Job DescriptionDokument8 SeitenSales Manager Job Descriptionsalesmanagement264Noch keine Bewertungen
- Archive Purge Programs in Oracle EBS R12Dokument7 SeitenArchive Purge Programs in Oracle EBS R12Pritesh MoganeNoch keine Bewertungen
- Direct Method (Education) : Navigation SearchDokument5 SeitenDirect Method (Education) : Navigation Searcheisha_91Noch keine Bewertungen
- Rubrics On Video Analysis - 2022Dokument2 SeitenRubrics On Video Analysis - 2022jovenil BacatanNoch keine Bewertungen
- Stock Control Management SyestemDokument12 SeitenStock Control Management SyestemJohn YohansNoch keine Bewertungen
- Week 4Dokument5 SeitenWeek 4عبدالرحمن الحربيNoch keine Bewertungen
- 2003catalog PDFDokument25 Seiten2003catalog PDFPH "Pete" PetersNoch keine Bewertungen
- The Daily Jinx 0 - ENG-3 (1) - 1Dokument3 SeitenThe Daily Jinx 0 - ENG-3 (1) - 1NoxNoch keine Bewertungen
- Grade12 Rigel Group4 Assesing The Solid Waste Management Off Small Foos Store in Gingoog CityDokument31 SeitenGrade12 Rigel Group4 Assesing The Solid Waste Management Off Small Foos Store in Gingoog CityMa. Joan ApolinarNoch keine Bewertungen
- Intensive Care Fundamentals: František Duška Mo Al-Haddad Maurizio Cecconi EditorsDokument278 SeitenIntensive Care Fundamentals: František Duška Mo Al-Haddad Maurizio Cecconi EditorsthegridfanNoch keine Bewertungen
- Syntax 1Dokument35 SeitenSyntax 1galcarolina722202100% (1)
- Handbook For Inspection of Ships and Issuance of Ship Sanitation CertificatesDokument150 SeitenHandbook For Inspection of Ships and Issuance of Ship Sanitation CertificatesManoj KumarNoch keine Bewertungen
- Trading SecretsDokument99 SeitenTrading SecretsGary100% (3)
- BY DR Muhammad Akram M.C.H.JeddahDokument32 SeitenBY DR Muhammad Akram M.C.H.JeddahMuhammad Akram Qaim KhaniNoch keine Bewertungen
- Lecture Note 10 - Mortgage and Mortgage-Backed SecuritiesDokument58 SeitenLecture Note 10 - Mortgage and Mortgage-Backed Securitiesben tenNoch keine Bewertungen
- Chapter 2: Related Theoretical Design Inputs 2.1 Sihwa Lake Tidal Power StationDokument9 SeitenChapter 2: Related Theoretical Design Inputs 2.1 Sihwa Lake Tidal Power Stationaldrin leeNoch keine Bewertungen
- Nursing Philosophy Apa PaperDokument7 SeitenNursing Philosophy Apa Paperapi-449016836Noch keine Bewertungen
- Tesla, Inc.: Jump To Navigation Jump To Search Tesla Induction Motor AC MotorDokument90 SeitenTesla, Inc.: Jump To Navigation Jump To Search Tesla Induction Motor AC MotorEdi RaduNoch keine Bewertungen
- Student Skeletal System Exam QuestionsDokument3 SeitenStudent Skeletal System Exam Questionsawiniemmanuel247Noch keine Bewertungen