Beruflich Dokumente
Kultur Dokumente
Oral Candidosis: G T. M I
Hochgeladen von
Yerly Ramirez MuñozOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Oral Candidosis: G T. M I
Hochgeladen von
Yerly Ramirez MuñozCopyright:
Verfügbare Formate
O R A L M E D I C IO
N R
E A L M E D I C I N E
Oral Candidosis
GRANT T. MCINTYRE
isolated from oral candidoses in the
Abstract: Oral candidoses are frequently encountered in the practice of dentistry.
Although most oral candidoses are symptomless, they can indicate the presence of an
immunocompromised patient, and in
underlying systemic disease, and the persistence of oral candidosis following such individuals the course of oral
appropriate conventional management may be one of the first signs of undiagnosed candidosis can be protracted and
immunosuppression. The opportunistic pathogen Candida albicans is the most resistant to normal management
commonly isolated species from oral candidal lesions; however, the non-albicans protocols.
Candida spp. are also implicated in the aetiology of oral candidoses. The effective
management of oral candidosis is dependent on an accurate diagnosis, identification
and elimination of any predisposing factors (where possible), and the prescription of Organisms Involved in Oral
either topical or systemic antifungal agents. Oral candidosis may have significant Candidosis
implications for the general health of immunosuppressed patients, particularly when Although C. albicans is frequently
caused by the non-albicans spp. and, in cases of severe immunosuppression, systemic
identified in the aetiopathogenesis of
candidosis can be life-threatening. This article outlines the clinical presentation and
appropriate management for the commonly presenting oral candidal conditions.
candidosis, other candidal species can be
isolated from oral candidal lesions:
Dent Update 2001; 28: 132-139
! C. tropicalis;
Clinical Relevance: Dental professionals should be aware of the clinical signs of ! C. pseudotropicalis;
intraoral candidosis, the appropriate special investigations that may be required in
! C. glabrata;
order to derive a definitive diagnosis, the significance of immunosuppression in oral
candidosis and the appropriate methods of management of the condition.
! C. krusei;
! C. parapsilosis.
PREDISPOSING FACTORS
ral candidosis is a collective term symptomless and can be a marker of A number of predisposing factors have
O for the group of diseases that
result from infection with Candida spp.,
underlying immunosuppression, and are
therefore referred to as the ‘diseases of the
been identified, all with the common
feature of producing a change in the host–
affecting both immunocompetent and diseased’. Immunosuppression is an commensal balance (altered oral
immunocompromised individuals. (The important consideration for any homeostasis), allowing the proliferation of
terms ‘candidosis’ and ‘candidiasis’ are candidosis that either does not resolve the candidal organisms that results in
synonymous: candidosis will be used rapidly with appropriate conventional candidosis. C. albicans normally co-
throughout this article.) Non-candidal oral management, or recurs frequently. exists with Lactobacillus acidophilus in
mycoses (cryptococcosis, histoplasmosis Oral candidal species can be identified the vegetative (yeast or blastospore) state;
and geotrichosis) are extremely rare and as part of the oral commensal flora in 41% however, it can readily change to the
generally diagnosed only in HIV-infected of the ‘normal’ population,2 and it is elongated cellular form (pseudohyphae) or
individuals.1 The effects of oral impossible to eradicate Candida from the chlamydospore forms. C. albicans has
candidosis may range from localized oral cavity completely. Candida spp. are weak pathogenicity and when an
infections to acute, systemic disseminated opportunistic pathogens, resulting in imbalance occurs in the host–commensal
disease. Oral candidoses are often disease when the host–commensal relationship this commensal organism has
relationship is disturbed. Candida the opportunity to become pathogenic.
albicans is the species most often The production of an endotoxin – an
Grant T. McIntyre, BDS, FDS RCPS (Glasg.), cultured from candidoses in extracellular proteolytic enzyme – is
Specialist Registrar, Dundee Dental Hospital and
School, Dundee, Scotland.
immunocompetent individuals; however, responsible for most of the adverse
the non-albicans spp. are more frequently effects of the intraoral mucous membrane
132 Dental Update – April 2001
Downloaded from magonlinelibrary.com by 144.082.238.225 on June 24, 2018.
O R A L M E D I C I N E
Factor Examples
rectification should form an integral
component of the overall patient
Physiological Age (old and young), pregnancy management: the failure either to identify
Trauma Ill-fitting dentures and orthodontic appliances or manage predisposing factors will
Dietary factors High carbohydrate intake, deficiency states (iron, vit. B 12, folate) prevent the expedient resolution of oral
candidosis, and will most likely result in
Endocrine Diabetes mellitus, Addison’s disease, Hypothyroidism
recurrence. Where it is not possible to
Malignancy Agranulocytosis, leukaemias eliminate predisposing factors, such as in
Immune defects AIDS the long-term use of inhaled steroids or
Xerostomia Drug-induced, Sjögren’s syndrome, radiation-induced where malignancy is present, the
Disturbed oral flora Antibiotics (especially broad spectrum), steroids
prophylactic prescription of an antifungal
agent may prevent recurrence.
‘Other’ factors Smoking, hospitalization
Immunocompromization is the single
Table 1. Predisposing factors in oral candidosis. most important predisposing factor that
should be considered in patients with
oral candidosis, owing to the potential for
in oral candidosis. carcinomata predispose to oral significant general health sequelae and,
Predisposing localized and systemic candidosis. The therapeutic use of in severe cases of immunosuppression,
factors can be classified as natural chemotherapy and radiotherapy in the patient’s immune response may
factors, dietary factors, mechanical malignancy are associated with an become overwhelmed by systemic
factors and iatrogenic factors or grouped increased risk of oral candidosis: the candidosis, leading to a life-threatening
according to physiological factors, mechanisms are complex, but involve situation. The prophylactic prescription
trauma, dietary factors, endocrine factors, these therapies having a direct effect on of an antifungal may not only improve life
malignancy, immune defects, xerostomia, the rate of cellular turnover in the oral quality, but also life expectancy for the
disturbed oral flora and ‘other’ factors. mucous membrane and reducing the severely immunocompromised patient.
Table 1 summarizes the predisposing salivary flow, respectively. Oral
factors in oral candidosis. candidosis may be one of the earliest
The physiological factors – the signs of AIDS, and in HIV-infected CLASSIFICATION OF ORAL
extremes of age – predispose to oral patients candidoses can affect multiple CANDIDAL CONDITIONS
candidosis, as they are associated with intraoral sites.1 The first classification of oral candidosis
an impaired host response. Xerostomia results in reduced flow and was proposed by Lehner in 1966.5 Lehner
Mechanical irritation (from acrylic quality of saliva and predisposes to oral recognized two major subdivisions:
dentures and orthodontic appliances) candidosis. The reduced effectiveness of
may result in the breakdown of the the antimicrobial properties of saliva ! acute, including pseudomembranous
integrity of the mucous membrane, (lysozyme, lactoferrin, the and atrophic candidosis; and
destroying its intrinsic antimicrobial lactoperoxidase system, and salivary ! chronic, including atrophic and
resistance,3 while the close contact of the glycoprotein4) favours the proliferation hyperplastic candidiasis.
acrylic and mucous membrane prevents of Candida spp.
salivary antimicrobial substances Broad-spectrum antibiotics, steroid The currently accepted classification6
(lysozyme, lactoferrin, the aerosols and smoking interfere with the
lactoperoxidase system and salivary normal balance of the oral microbial flora
glycoproteins) coming into contact with by removing the competition between the
Primary oral candidoses (group 1)
the invading microorganisms. various microorganisms for adherence ! Acute: Pseudomembranous,
Some dietary factors such as a high and nutrition which, in health, limits the erythematous
carbohydrate intake provide Candida growth and dissemination of fungi. ! Chronic: Pseudomembranous,
spp. with ideal metabolites, whereas the Hospitalization may predispose erythematous, hyperplastic (plaque-like and
deficiency states (iron, vitamin B12 and individuals to oral candidosis; patients in nodular)
folate) may reflect the poor resistance of hospital may encounter microorganisms ! Candida-associated lesions: Candida-
the intraoral and perioral tissues to to which they cannot mount an effective associated denture-induced stomatitis,
angular cheilitis, median rhomboid glossitis
infection by Candida spp. immune response, either because of
Endocrine disturbances, the presence reduced immunocompetence as a result Secondary oral candidoses (group 2)
of malignancy and immune defects (e.g. of ill-health or due to the exposure to ! Oral manifestations of systemic
mucocutaneous candidosis (due to diseases
AIDS) are associated with an inferior previously unmet potential pathogens. such as thymic aplasia and candidosis
host response, particularly cell-mediated Following the discovery of a endocrinopathy syndrome)
immunity. Furthermore, areas of ulcerated predisposing factor in a patient Table 2. Classification of oral candidosis (after
mucous membrane associated with oral diagnosed with oral candidosis, its Holmstrup and Axéll6).
Dental Update – April 2001 133
Downloaded from magonlinelibrary.com by 144.082.238.225 on June 24, 2018.
O R A L M E D I C I N E
Management
a b
Pseudomembranous candidosis in the
immunocompetent patient is usually
managed using topical agents alone,
although use of systemic agents may be
associated with increased compliance
because nystatin pastilles and
amphotericin B lozenges have an
unpleasant taste (Table 4). In patients
with AIDS, systemic antifungals are more
Figure 1 (a and b). Widespread intraoral pseudomembranous candidosis.
effective than topical agents.
Patients who do not experience
resolution of pseudomembranous
is based upon clinically relevant bacteria. Although pseudomembranous candidosis within two weeks of the
terminology and accounts for the candidosis is usually termed ‘acute’ in institution of antifungal therapy should
limitations of Lehner’s original view of the short duration of the be referred for investigation of possible
classification (see Table 2). As condition, in immunocompromised underlying disease. Pseudomembranous
pseudomembranous candidosis can be individuals the condition is often of a candidosis in the immunosuppressed
present for an extended period of time, chronic, protracted nature, and can last (e.g. AIDS) should be managed in
particularly in immunocompromised for months (and even years). specialist centres.
patients or in those using inhaled
steroids, ‘pseudomembranous’ should be
prefixed with ‘acute’ or ‘chronic’ as Diagnosis ERYTHEMATOUS
appropriate.6 The diagnosis of pseudomembranous CANDIDOSIS
The term ‘erythematous’ represents a candidosis can usually be based on the Erythematous candidosis may be termed
more valid term than ‘atrophic’ for lesions clinical findings, although a swab of the ‘acute’ or ‘chronic’, depending on the
that appear more ‘red’ than the lesion should be sent for culture and time factor in the course of the condition.
surrounding mucous membrane, as sensitivity, and a phosphate-buffered The acute form was formerly known as
redness of the mucous membrane may be saline rinse may indicate the fungal load ‘acute atrophic candidosis’, ‘antibiotic
due to either atrophy or increased present within the patient’s mouth (Table sore tongue’ or ‘glossodynia’ and is now
vascularity. 3). A smear may also be helpful in the known as erythematous candidosis. It
As angular cheilitis and denture diagnosis of pseudomembranous often results from treatment with broad-
stomatitis and median rhomboid glossitis candidosis; however, biopsy is not spectrum antibiotics, steroid preparations
may have a combined bacterial and usually necessary. The identification of (e.g. asthma inhalers), and short-course
fungal aetiology, they are more the causative candidal species and any topical antibiotics. The tongue is most
appropriately classified as Candida- resistance to proposed antifungal agents often affected, although any area of the
associated lesions. will allow the clinician to provide oral mucous membrane is susceptible.
effective patient management. Erythematous candidosis resulting from
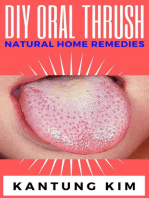
PSEUDOMEMBRANOUS
CANDIDOSIS
This condition (see Figure 1) is also Condition Swab Smear Oral rinse Biopsy Blood
known colloquially as ‘thrush’. The tests*
clinical lesions of pseudomembranous Pseudomembranous + + + – –
candidosis are very characteristic. Non-
adherent creamy white patches or flecks Erythematous + +(–) + – –
are easily wiped from an underlying Hyperplastic + +(–) + +(–) +
erythematous and bleeding mucous
membrane. Commonly affected areas are Candida-associated denture-
induced stomatitis + + + – +
the soft palate, oropharynx, tongue,
cheek and gingivae. Surprisingly, pain is Angular cheilitis + + + – +
rarely reported.
Median rhomboid glossitis + + + +(–) +(–)
The pseudomembrane consists of a
mesh of fungal hyphae containing *Blood tests include iron, vitamin B 12, folate, glucose
entangled desquamated epithelial cells, +: Useful; – not useful; +(–) may be useful
fibrin, keratin, necrotic tissue and Table 3. Appropriate laboratory investigations for oral candidosis.
134 Dental Update – April 2001
Downloaded from magonlinelibrary.com by 144.082.238.225 on June 24, 2018.
O R A L M E D I C I N E
Condition Topical treatment Systemic treatment candidal leukoplakia and is
characterized by irregular whitish
Pseudomembranous Nystatin pastilles or amphotericin Fluconazole 50 mg tablet daily for raised plaque-like lesions on the
B lozenges sucked four times daily 14 days or itraconazole 150 mg
for 7–10 days capsule daily for 15 days buccal mucous membrane near to the
commissures (see Figures 2 and 3).
Erythematous Nystatin pastilles or amphotericin B Fluconazole 50 mg tablet daily for The tongue is rarely involved. The
lozenges sucked four times daily for 14 days or itraconazole 150 mg
7–10 days. Stop offending antibiotic capsule daily for 15 days patient and referring dentist are often
(where present). Oral rinsing after concerned about potential malignancy
inhaling steroids (Figure 3). Lesions are usually
Hyperplastic Miconazole gel applied to lesions Fluconazole 50 mg tablet daily for bilateral, do not have a surface that is
four times daily until resolution. 14 days or itraconazole 150 mg easily removed, and can be extensive.
Low-carbohydrate diet capsule daily for 15 days Most patients are smokers. Other
Candida-associated Miconazole gel applied to fitting Fluconazole 50 mg tablet daily for candidal lesions may also be present,
denture-induced surface of appliance and palate four 14 days or itraconazole 150 mg possibly angular cheilitis.
stomatitis times daily for 7 days. Soak capsule daily for 15 days
prostheses in 1% hypochlorite
(acrylic) or 2% chlorhexidine (metal-
based). 2% chlorhexidine mouthwash Diagnosis
four times daily. Low-carbohydrate Biopsy may be considered appropriate
diet
in certain cases to exclude neoplasia
Angular cheilitis Miconazole gel applied to lesions Fluconazole 50 mg tablet daily for (Table 3) and to diagnose hyperplastic
four times daily until resolution. Soak 14 days or itraconazole 150 mg candidosis definitively.
prostheses in 1% hypochlorite capsule daily for 15 days
(acrylic) or 2% chlorhexidine Microbiological investigation in the
(metal-based). 2% chlorhexidine form of swabs can help in clarifying
mouthwash four times daily the presence of Candida in the
Median rhomboid Nystatin pastilles or amphotericin Fluconazole 50 mg tablet daily for lesions, and a phosphate-buffered
glossitis B lozenges sucked four times daily 14 days or itraconazole 150 mg saline rinse may be confirmatory of the
for 7-10 days. Anti-smoking advice capsule daily for 15 days intraoral presence of the organism and
Table 4. Management of the oral candidoses in immunocompetent patients. indicate the fungal load.
Haematological investigations are also
important to assess any underlying
predisposing factors such as
the prescription of broad-spectrum prescriptions should be advised to rinse deficiency of iron, vitamin B12 or folate
antibiotics is the only oral candidosis their mouth after inhalation to ensure (Table 3).
where pain is a common symptom. speedy resolution of erythematous
candidosis. Moreover, routine oral
rinsing after inhalation should be Management
Diagnosis suggested as a preventive measure to all The condition is managed by
The clinical diagnosis of erythematous people using inhaled steroid rectification of any predisposing
candidosis may be confirmed by prescriptions. factors (e.g. smoking), provision of an
microbiological analysis of the appropriate antifungal (either topically
organisms cultured from a swab of the or systemically) and by institution of a
lesion, and a phosphate-buffered saline HYPERPLASTIC low-carbohydrate diet (see Table 4).
rinse may indicate the intraoral fungal CANDIDOSIS Sometimes the protracted nature of
load (see Table 3). A biopsy provides no This chronic condition is also known as hyperplastic candidosis necessitates
additional diagnostic value.
a b
Management
Cessation of treatment with the
offending antibiotic medication usually
leads to spontaneous resolution:
however, this may not be possible and
topical antifungals may be necessary
prophylactically if the causative therapy
is to be continued (Table 4).
Figure 2 (a and b). Hyperplastic candidosis in an edentulous heavy smoker.
Patients using inhaled steroid
Dental Update – April 2001 135
Downloaded from magonlinelibrary.com by 144.082.238.225 on June 24, 2018.
O R A L M E D I C I N E
appliances should be sent for culture
and sensitivity, while a phosphate-
buffered saline oral rinse will indicate
the intraoral fungal load.
Blood tests form an essential part of
the management of this condition, in
order to identify any predisposing
factors, which include the deficiency
states (iron, vitamin B12, folate) and
Figure 3. Same patient as in Figure 2. Lesions possible undiagnosed diabetes Figure 5. Angular cheilitis.
extend onto perioral skin. A biopsy was mellitus. A biopsy specimen provides
performed to eliminate neoplasia. no additional diagnostic information.
mouthwash can also be of benefit
due to its antifungal action.
combined and lengthy treatment. Management 5. Systemic antifungal agents (see
Follow up is imperative to ensure The management of the condition Table 4) may be considered for
complete resolution, and for persistent should follow the following lines: patients whose compliance may be
lesions cryosurgery or surgical expected to be poor (such as
excision should be considered unless 1. Correction of any predisposing elderly people in care),
precluded by the size of the lesion. factors. immunocompromised patients and
2. Improved appliance hygiene: for patients with Newton’s Type 3
immersion of the appliance in a 1% Candida-associated denture-
CANDIDA-ASSOCIATED hypochlorite solution for acrylic induced stomatitis (in addition to
DENTURE-INDUCED appliances, or 2% chlorhexidine the application of miconazole oral
STOMATITIS solution for metal-based dentures, gel to the palate and the fitting
This condition is classified as a whilst sleeping. surface of the denture).
Candida-associated lesion, as it may 3. Advice regarding a low-
result from a combined bacterial/fungal carbohydrate diet.
aetiology. Patients affected by 4. Prescription of antifungals. ANGULAR CHEILITIS
Candida-associated, denture-induced Miconazole oral gel should be Angular cheilitis presents as erythema
stomatitis are not usually aware of its applied to the fitting surface of the and crusting of the skin at the
presence. Curiously, in full-denture appliance and the denture-bearing commissures of the lips (Figure 5). As
wearers, the maxillary denture-bearing area four times daily (the antifungal a mixed bacterial/fungal aetiology may
area is more often affected than the is most effective while the patient be present, it should be classified as a
mandibular denture-bearing area. is sleeping due to the reduced Candida-associated lesion. Edentulous
Newton7 classified this condition into salivary flow). Miconazole is elderly people are most commonly
three distinct clinical categories: available over the counter as well affected by angular cheilitis. In most
as on prescription, but should be cases of angular cheilitis, simultaneous
! Type 1: pinpoint erythema. avoided by patients concurrently intraoral candidosis is evident. A
! Type 2: diffuse areas of erythema being prescribed oral multifactorial aetiology has been
and oedema of palatal mucosa. The anticoagulants. A 2% chlorhexidine proposed for this disease and includes:
affected area is sharply demarcated
from surrounding normal mucosa. ! infection by either Candida spp. or
Angular cheilitis can accompany Staphylococcus spp. (sometimes
this condition (Figure 4). both);
! Type 3: nodular, hyperplastic areas ! deficiency states: notably iron,
of mucosa with interspersed normal vitamin B12 and folate deficiency
areas of mucosa. (these may also be identified in the
anaemias and latent anaemias);
! undiagnosed or poorly controlled
Diagnosis diabetes mellitus;
The appropriate investigations for ! skin creasing due to advancing
Candida-associated, denture-induced age;
Figure 4. Newton’s Type 2 denture stomatitis
stomatitis are outlined in Table 3. A affecting an edentulous patient. Note the food ! poor dentures with inadequate
swab of the lesions, the fitting particles on the erythematous denture-bearing vertical component, allowing the
surface(s) of dentures and orthodontic area. skin at the commissures to crease
136 Dental Update – April 2001
Downloaded from magonlinelibrary.com by 144.082.238.225 on June 24, 2018.
O R A L M E D I C I N E
and retain saliva; The concomitant prescription of
! systemic disorders, e.g. diabetes topical and systemic antifungals for
mellitus, HIV infection. angular cheilitis (where intraoral and/or
intranasal reservoirs have been
identified) may be regarded as a ‘belt
Diagnosis and braces’ approach but should
Haematological investigations are ensure speedy resolution. Systemic
important to exclude deficiency disease antifungals are the treatment of choice
(ferritin, vitamin B12, folate); for angular cheilitis in
importantly, a blood glucose assay may immunocompromised individuals, for Figure 6. Median rhomboid glossitis.
highlight possible undiagnosed lesions resistant to topical measures
diabetes mellitus, which may be a alone, and where compliance is likely to
significant predisposing factor. be poor.
Swabs of the commissures and the The failure to identify or treat a of smoking is an integral part of the
anterior nares, and any potential reservoir of organisms will result in the management of patients with median
intraoral reservoir for organisms angular cheilitis recurring. Sufferers rhomboid glossitis, in order to prevent
(commonly the fitting surface of should be discouraged from any habits successive recurrences.
dentures, the palate and areas of that involve contact of nose and mouth
hyperplastic candidosis) should also be in close succession. Fabrication of new
sampled. These samples are important full dentures should be delayed until OTHER CONDITIONS
to identify the causative organism as angular cheilitis has resolved. These include cheilocandidosis,
well as the nucleus of organisms, which mucocutaneous candidosis and chronic
may be ‘feeding’ the angular cheilitis. oral multifocal candidosis. The reader is
A phosphate-buffered saline oral MEDIAN RHOMBOID referred to a specialist text for further
rinse should also be undertaken. This GLOSSITIS information.
may detect the presence of Candida at The usual clinical manifestation of
intraoral sites not otherwise sampled. median rhomboid glossitis is of a
diamond-shaped depapillated LABORATORY
erythematous patch on the midline of INVESTIGATIONS FOR
Management the tongue dorsum (Figure 6). It is ORAL CANDIDOSIS
The management of angular cheilitis classified as a Candida-associated The most appropriate laboratory
(see Table 4) will depend on the lesion as a mixed microbiological flora investigations are outlined in Table 3.
elimination of organisms from the may be implicated in the aetiology. Swabs, first moistened with sterile
reservoir of infection and the treatment saline and then rubbed along the
of any systemic sources of surface of the lesions, should be
microorganisms. The empirical Diagnosis promptly submitted to the
application of miconazole gel four The diagnosis is usually clinically microbiological laboratory with a
times daily to the lesions is helpful, as based; however, a swab and a request for culture and sensitivity.
it is active against both Candida spp. phosphate-buffered saline oral rinse These allow the identification of the
and Staphylococcus spp., as well as should be carried out, as a mixed causative candidal species, which in
other Gram-positive organisms; and aetiological flora may be identified. most cases is C. albicans. However,
therefore will eliminate many cases of Biopsy is unnecessary, unless the identification of non-albicans
infection. An alternative is fusidic acid diagnostic uncertainty still exists Candida spp. is of considerable
(Fucidin), again applied four times daily following the microbiological relevance in the management of oral
to the lesions, but this is generally only investigations and the lesion fails to candidosis – especially in the
prescribed on the basis of a respond to antifungal agents. immunocompromised patient – as non-
confirmatory microbiological report albicans organisms may not respond to
exclusively identifying Staphyloccus common topical and systemic
spp. as the causative organism. Management antifungals.
If microbiology reveals an intraoral Treatment requires the prescription of A smear of the lesion may duplicate
source of infection (commonly the topical or systemic antifungals. the information provided by a swab but
fitting surface of a denture and palate) However, Nystatin and amphotericin B in cases of diagnostic uncertainty, may
this must also be treated appropriately. are not palatable, and compliance may be indicated.
Similarly, if organisms are identified in be poor, in which case systemic A phosphate-buffered saline oral
the anterior nares, they must also be antifungals may be more effective rinse will determine the presence of
treated. (Table 4). Advice regarding cessation Candida within the oral cavity; and
138 Dental Update – April 2001
Downloaded from magonlinelibrary.com by 144.082.238.225 on June 24, 2018.
O R A L M E D I C I N E
high candidal counts correspond with and the departments of Dental Illustration at
high fungal loads in the diseased areas Glasgow Dental Hospital and School and Media
R EFERENCES
Services at the University of Dundee for their
of mucous membrane. help in the preparation of the images.
1. Samaranayake LP. Oral mycoses in HIV
Biopsy is generally unnecessary for infection. Oral Surg Oral Med Oral Pathol 1992;
73: 171–180.
the diagnosis of oral candidosis, except 2. Lynch DP. Oral candidiasis: History, classification
where potential malignancy is one of the and clinical presentation. Oral Surg Oral Med
provisional diagnoses. F URTHER R EADING Oral Pathol 1994; 78: 189–193.
Blood investigations should be Samaranayake LP, Lamey P-J. Oral candidosis: 1. 3. Budtz-Jörgensen E. Etiology, pathogenesis,
therapy, and prophylaxis of oral yeast infections.
instigated where appropriate, in order to Clinicopathological aspects. Dent Update 1988;
Acta Odontol Scand 1990; 48: 61–69.
15: 227–231.
identify any deficiency states and Lamey P-J, Samaranayake LP. Oral candidosis: 2. 4. Oksala E. Factors predisposing to oral yeast
undiagnosed or poorly controlled Diagnosis and management. Dent Update 1988; infections. Acta Odontol Scand 1990; 48: 71–74.
diabetes mellitus, which may indicate 15: 328–331. 5. Lehner T. Classification and clinicopathological
features of Candida infections in the mouth. In:
poor tissue resistance to candidal Lewis MA, Samaranayake LP, Lamey P-J. Diagnosis
Winner HI, Hurley R, eds. Symposium on
and treatment of Oral Candidosis. J Oral
infection. Maxillofac Surg 1991; 49: 996–1002. Candidal Infections. Edinburgh: E & S Livingstone,
US Department of Health and Human Services. Oral 1966; pp.119-136.
Health in America: A Report of the Surgeon 6. Holmstrup P,Axéll T. Classification and clinical
General. Rockville, MD: U.S. Department of manifestation of oral yeast infections. Acta
A CKNOWLEDGEMENTS Health and Human Services, National Institute Odontol Scand 1990; 48: 57–59.
I thank Dr D. Felix of Glasgow Dental Hospital and of Dental and Craniofacial Research, National 7. Newton AV. Denture sore mouth: A possible
School for providing the clinical photographs Institutes of Health, 2000. aetiology. Br Dent J 1962; 112: 357–360.
The book concludes with a
BOOK REVIEW
discussion of novel diagnostic
Contemporary Issues in Oral Cancer. techniques and finally summarizes
D. Saranath (editor). Oxford University certain of the more recent
Press, 2000 (405pp., £25.00). ISBN 0 19 observations in the field of oral
565023 9. malignancy, considering their possible
future applications in the management
This multi-author text aims to provide of this disease.
an up-to-date account of the The work is extensively referenced,
pathogenesis and management of oral but a number of the illustrations lack
cancer. It embraces the basic science, clarity and are difficult to interpret.
pathology and clinical aspects of this There is a widespread and
disease. unnecessary use of abbreviations
No fewer than 29 authors have throughout the text. A number of
contributed to this book, which these abbreviations are not in common
comprises 17 chapters and runs to usage and this may be a source of
some 405 pages in length. Ten of the irritation to the reader.
contributors work at the Tata Memorial In summary, this book is very broad
Centre and thus it is not surprising in its scope and perhaps, as a result,
that the text is biased somewhat represents somewhat of a compromise,
towards the issue of oral cancer in lacking a particularly authoritative
South Asia. approach. However, it should appeal
The first chapter addresses the to both clinicians and basic scientists
epidemiology and possible prevention The text continues with chapters on who either have an interest in, or are
of oral cancer, introducing the subject serological markers in head and neck involved with, the management of
matter effectively, whilst chapter two malignancy, the possible aetiological patients with oral cancer. The
provides an overview of the molecular role of viruses and a chapter devoted publication contains a very
biology of the disease. This is an to chemoprevention. considerable amount of information
intrinsically complex topic and, in Six chapters address therapeutic and at a cost of £25, notwithstanding
parts, the grammatical style of the text modalities of oral cancer and, as well as some of the above criticisms, it
does not encourage the reader’s grasp summarizing the more traditional represents good value for money.
of the subject matter. approaches, the potential use of
The following three chapters outline photodynamic therapy, immunotherapy John Hamburger
immunological aspects of oral cancer. and gene therapy are also discussed. Birmingham Dental School
Dental Update – April 2001 139
Downloaded from magonlinelibrary.com by 144.082.238.225 on June 24, 2018.
Das könnte Ihnen auch gefallen
- Diagnosis and Treatment of Oral CandidosisDokument7 SeitenDiagnosis and Treatment of Oral CandidosisYerly Ramirez MuñozNoch keine Bewertungen
- Oral Candidiasis An Overview and Case ReportDokument7 SeitenOral Candidiasis An Overview and Case ReportPutri NingrumNoch keine Bewertungen
- Fmicb 06 01391 PDFDokument10 SeitenFmicb 06 01391 PDFChellaPremitaNoch keine Bewertungen
- Oral Candidiasis: ReviewDokument5 SeitenOral Candidiasis: ReviewRiris RetnoNoch keine Bewertungen
- Candidiasis 1Dokument5 SeitenCandidiasis 1jodericoNoch keine Bewertungen
- Oral CandidiasisDokument5 SeitenOral CandidiasisJNoch keine Bewertungen
- Pseudomembranous Candidiasis Induced byDokument5 SeitenPseudomembranous Candidiasis Induced byGenevieve Florencia Natasya SaraswatiNoch keine Bewertungen
- Oral Candidiasis An Opportunistic Infection A ReviewDokument5 SeitenOral Candidiasis An Opportunistic Infection A ReviewDino JalerNoch keine Bewertungen
- Candidiasis - Red and White Manifestations in The Oral CavityDokument8 SeitenCandidiasis - Red and White Manifestations in The Oral CavityFajarRahmantiyoNoch keine Bewertungen
- Oral Candidosis in The Paediatric PatientDokument6 SeitenOral Candidosis in The Paediatric Patientrahastuti drgNoch keine Bewertungen
- Candidiasis Red and White Manifestations in The Oral CavityDokument8 SeitenCandidiasis Red and White Manifestations in The Oral CavityDaniela Juárez CastellanosNoch keine Bewertungen
- Oral Candidiasis: Dr. Ahmad Yusran, SPPDDokument87 SeitenOral Candidiasis: Dr. Ahmad Yusran, SPPDM Nedi Sevtia BudiNoch keine Bewertungen
- Candidiasis Red and WhiteDokument8 SeitenCandidiasis Red and WhitejnrrszrnvmNoch keine Bewertungen
- Review Article: What Makes Oral Candidiasis Recurrent Infection? A Clinical ViewDokument6 SeitenReview Article: What Makes Oral Candidiasis Recurrent Infection? A Clinical ViewAF KoasNoch keine Bewertungen
- 2 ApikDokument5 Seiten2 ApikAhmad Syauqie Al MuhdarNoch keine Bewertungen
- CandidiasisDokument6 SeitenCandidiasismirayanti astariNoch keine Bewertungen
- Candida-Associated Cheilitis: Online Images in The Medical SciencesDokument2 SeitenCandida-Associated Cheilitis: Online Images in The Medical Sciencesfelaxis fNoch keine Bewertungen
- Oral Candidiasis - ReviewDokument9 SeitenOral Candidiasis - ReviewAdhelia Galuh PrmtsrNoch keine Bewertungen
- Guide to Diagnosing and Treating Oral CandidiasisDokument5 SeitenGuide to Diagnosing and Treating Oral CandidiasisNovita Indah PratiwiNoch keine Bewertungen
- Candida-Associated Denture StomatitisDokument5 SeitenCandida-Associated Denture StomatitisAyik DarkerThan BlackNoch keine Bewertungen
- Fungal Infections of Oral Cavity: Diagnosis, Management, and Association With COVID-19Dokument12 SeitenFungal Infections of Oral Cavity: Diagnosis, Management, and Association With COVID-19Roxana Guerrero SoteloNoch keine Bewertungen
- 455.full CandidiasisDokument6 Seiten455.full CandidiasisIdris Siddiq CuakepNoch keine Bewertungen
- Oropharyngeal Candidosis in Older PatientsDokument8 SeitenOropharyngeal Candidosis in Older Patientsnugraheni.riniNoch keine Bewertungen
- Oral Health in America A Report of The Surgeon General (Prosiding)Dokument4 SeitenOral Health in America A Report of The Surgeon General (Prosiding)Zkdlin SpaceNoch keine Bewertungen
- CH 084 Oral ThrushDokument7 SeitenCH 084 Oral ThrushSavir GuptaNoch keine Bewertungen
- Chronic Hyperplastic Candidiasis of The Oral Mucosa Case Report PDFDokument3 SeitenChronic Hyperplastic Candidiasis of The Oral Mucosa Case Report PDFGita Dwi DesianiNoch keine Bewertungen
- Clinical Characteristics of Patients With Oral CandidiasisDokument8 SeitenClinical Characteristics of Patients With Oral CandidiasisHilya Aliva AufiaNoch keine Bewertungen
- Drug-Induced Oral Candidiasis - A Case ReportDokument4 SeitenDrug-Induced Oral Candidiasis - A Case ReportFajarRahmantiyoNoch keine Bewertungen
- Oral Candidiasis: An Overview: Arun Singh, Renuka Verma, Aditi Murari, Ashutosh AgrawalDokument5 SeitenOral Candidiasis: An Overview: Arun Singh, Renuka Verma, Aditi Murari, Ashutosh AgrawalazyuNoch keine Bewertungen
- Red and White Lesions of The Oral Mucosa: DR - Wisam RasoolDokument43 SeitenRed and White Lesions of The Oral Mucosa: DR - Wisam RasoolFlorida ManNoch keine Bewertungen
- Candidiasis A Fungal Infection Current Challenges and ProgressDokument11 SeitenCandidiasis A Fungal Infection Current Challenges and ProgressLau's WorldNoch keine Bewertungen
- Oral Candidiasis: A Short Review and A Case Report: December 2018Dokument5 SeitenOral Candidiasis: A Short Review and A Case Report: December 2018RAfii KerenNoch keine Bewertungen
- Guide to Oral Candidosis: Types, Causes and TreatmentsDokument39 SeitenGuide to Oral Candidosis: Types, Causes and TreatmentsArmada Eka FredianNoch keine Bewertungen
- CandidiasisDokument19 SeitenCandidiasisTeguh Adi PartamaNoch keine Bewertungen
- Dental Antifungal Drug ReviewDokument17 SeitenDental Antifungal Drug ReviewMonaNoch keine Bewertungen
- Current Treatment of Oral Candidiasis A Literature ReviewDokument8 SeitenCurrent Treatment of Oral Candidiasis A Literature ReviewRonaldo PutraNoch keine Bewertungen
- b.8 Oral CandidiasisDokument14 Seitenb.8 Oral Candidiasisbryamjbriceno100% (1)
- Kandidiasis Akut Eritematous Pada Penderita Diabetes MellitusDokument9 SeitenKandidiasis Akut Eritematous Pada Penderita Diabetes MellitusditacahyadewiiiNoch keine Bewertungen
- 588-Article+Text-1884-1-10-20220107 (1)Dokument9 Seiten588-Article+Text-1884-1-10-20220107 (1)Dave PutraNoch keine Bewertungen
- Assoc. Prof. G. Tomov, PHD: Division of Oral Pathology, Faculty of Dental Medicine Mu - PlovdivDokument106 SeitenAssoc. Prof. G. Tomov, PHD: Division of Oral Pathology, Faculty of Dental Medicine Mu - PlovdivAustine OsaweNoch keine Bewertungen
- Aparna. K Et AlDokument7 SeitenAparna. K Et AlAparna SanathNoch keine Bewertungen
- Infectious Eosophagitis 2013Dokument5 SeitenInfectious Eosophagitis 2013Adhytia PradiarthaNoch keine Bewertungen
- Apical Periodontitis - Virulence Factors of Enterococcus: Faecalis and Candida AlbicansDokument5 SeitenApical Periodontitis - Virulence Factors of Enterococcus: Faecalis and Candida AlbicansEfika ChoirunnisaNoch keine Bewertungen
- Pitts NB, Et Al. Understanding Dental Caries As A Non-Communicable Disease. British Dental Journal. 2021Dokument5 SeitenPitts NB, Et Al. Understanding Dental Caries As A Non-Communicable Disease. British Dental Journal. 2021miranda gitawNoch keine Bewertungen
- Odontogenic Cellulitis Care in ChildrenDokument6 SeitenOdontogenic Cellulitis Care in Childrenana mariaNoch keine Bewertungen
- TK Sepsis Karena Kandidiasis InvasifDokument23 SeitenTK Sepsis Karena Kandidiasis InvasifsamudraandiNoch keine Bewertungen
- Angular Chelitis in Complete Dentures: Sharmila.R, N.P MuralidharanDokument2 SeitenAngular Chelitis in Complete Dentures: Sharmila.R, N.P MuralidharanindahdwitasariNoch keine Bewertungen
- Candidiasis CryptococcosisDokument3 SeitenCandidiasis CryptococcosisJuan Carlo CacaoNoch keine Bewertungen
- Yeast Infection PDFDokument12 SeitenYeast Infection PDFAhmed GaberNoch keine Bewertungen
- Esquemas OclusalesDokument18 SeitenEsquemas OclusalesKarla AlanisNoch keine Bewertungen
- Being A Dentist in The PandemicDokument2 SeitenBeing A Dentist in The PandemicLarissa CostaNoch keine Bewertungen
- Candidiasis (Hasznalt)Dokument4 SeitenCandidiasis (Hasznalt)Ilyes FerenczNoch keine Bewertungen
- Author:Dwi Nugroho Juanda Department: Institution:: Faculty of Dentistry Trisakti UniversityDokument2 SeitenAuthor:Dwi Nugroho Juanda Department: Institution:: Faculty of Dentistry Trisakti UniversitydwinugrohojuandaNoch keine Bewertungen
- Oral Candidiasis: An OverviewDokument9 SeitenOral Candidiasis: An Overviewامجد شاكرNoch keine Bewertungen
- Journal of Periodontology - 2018 - Holmstrup - Non Plaque Induced Gingival DiseasesDokument18 SeitenJournal of Periodontology - 2018 - Holmstrup - Non Plaque Induced Gingival DiseasesMonica MartínezNoch keine Bewertungen
- Haider OralllllllllllllllllllllllDokument13 SeitenHaider OralllllllllllllllllllllllAli YehyaNoch keine Bewertungen
- Candida Infection in Oral Leukoplakia An Unperceived Public Health ProblemDokument5 SeitenCandida Infection in Oral Leukoplakia An Unperceived Public Health ProblemBrili AnenoNoch keine Bewertungen
- Oral Candidiasis: Madhu Priya.MDokument4 SeitenOral Candidiasis: Madhu Priya.MinventionjournalsNoch keine Bewertungen
- Risk Factors Related To Oral Candidiasis in Patients With Primary Sjögren's SyndromeDokument6 SeitenRisk Factors Related To Oral Candidiasis in Patients With Primary Sjögren's SyndromeEdith TrejoNoch keine Bewertungen
- Mass Retraction Movement of The Anterior Upper Teeth Using Orthodontic Mini-Implants As AnchorageDokument6 SeitenMass Retraction Movement of The Anterior Upper Teeth Using Orthodontic Mini-Implants As AnchorageYerly Ramirez MuñozNoch keine Bewertungen
- Henrikson J, Persson M, Thilander B. Long-Term Stability ofDokument12 SeitenHenrikson J, Persson M, Thilander B. Long-Term Stability ofyerly ramirezNoch keine Bewertungen
- Occlusal Vertical Dimension Treatment Planning Decisions and Management ConsiderationsDokument16 SeitenOcclusal Vertical Dimension Treatment Planning Decisions and Management ConsiderationsHector Flores Soto100% (4)
- Mass Retraction Movement of The Anterior Upper Teeth Using Orthodontic Mini-Implants As AnchorageDokument6 SeitenMass Retraction Movement of The Anterior Upper Teeth Using Orthodontic Mini-Implants As AnchorageYerly Ramirez MuñozNoch keine Bewertungen
- Trip To San AndresDokument1 SeiteTrip To San AndresYerly Ramirez MuñozNoch keine Bewertungen
- Effect of Orthodontic Treatment On Periodontal Clinical Attachment A Systematic Review and MetaanalysisDokument9 SeitenEffect of Orthodontic Treatment On Periodontal Clinical Attachment A Systematic Review and MetaanalysisYerly Ramirez MuñozNoch keine Bewertungen
- Efectos Del Tto OrtodonticoDokument18 SeitenEfectos Del Tto OrtodonticoFelipe Andres Morales IbañezNoch keine Bewertungen
- Intrusion of Incisors in Adult Patients With Marginal Bone LossDokument10 SeitenIntrusion of Incisors in Adult Patients With Marginal Bone LossYerly Ramirez MuñozNoch keine Bewertungen
- Reduction of Gingival Recession Following Orthodontic Intrusion in Periodontally Compromised PatientsDokument5 SeitenReduction of Gingival Recession Following Orthodontic Intrusion in Periodontally Compromised PatientsYerly Ramirez MuñozNoch keine Bewertungen
- Orthodontic Treatment in Periodontitis Susceptible Subjects A Systematic Literature ReviewDokument12 SeitenOrthodontic Treatment in Periodontitis Susceptible Subjects A Systematic Literature ReviewYerly Ramirez MuñozNoch keine Bewertungen
- Melsen, B., 2001. Tissue Reaction To Orthodontic Tooth MovementDokument12 SeitenMelsen, B., 2001. Tissue Reaction To Orthodontic Tooth MovementYerly Ramirez MuñozNoch keine Bewertungen
- Efficacy of Diode Laser Therapy in Acceleration ofDokument7 SeitenEfficacy of Diode Laser Therapy in Acceleration ofYerly Ramirez MuñozNoch keine Bewertungen
- Noticias 1368018543 PDFDokument14 SeitenNoticias 1368018543 PDFdrzana78Noch keine Bewertungen
- Intrusion of Migrated Incisors With Infrabony Defects in Adult Periodontal PatientsDokument5 SeitenIntrusion of Migrated Incisors With Infrabony Defects in Adult Periodontal PatientsYerly Ramirez MuñozNoch keine Bewertungen
- Method To Classify Dental Arch Forms: Original ArticleDokument10 SeitenMethod To Classify Dental Arch Forms: Original ArticleYerly Ramirez MuñozNoch keine Bewertungen
- 36 PDFDokument10 Seiten36 PDFPae Anusorn AmtanonNoch keine Bewertungen
- Guide to Oral Candidosis: Types, Causes and TreatmentsDokument39 SeitenGuide to Oral Candidosis: Types, Causes and TreatmentsArmada Eka FredianNoch keine Bewertungen
- Diagnosis and Management of Oral Candidosis: PracticeDokument7 SeitenDiagnosis and Management of Oral Candidosis: PracticeYerly Ramirez MuñozNoch keine Bewertungen
- Ot Dis Tribut E: Spectroscopic Sensing of Cancer and Cancer TherapyDokument9 SeitenOt Dis Tribut E: Spectroscopic Sensing of Cancer and Cancer TherapyYerly Ramirez MuñozNoch keine Bewertungen
- 25 CalciumandOralHealthAReviewDokument3 Seiten25 CalciumandOralHealthAReviewAndrea Fernanda SánchezNoch keine Bewertungen
- Matthews 1998Dokument8 SeitenMatthews 1998Yerly Ramirez MuñozNoch keine Bewertungen
- The Following Resources Related To This Article Are Available Online atDokument11 SeitenThe Following Resources Related To This Article Are Available Online atYerly Ramirez MuñozNoch keine Bewertungen
- Case ReportDokument6 SeitenCase ReportYerly Ramirez MuñozNoch keine Bewertungen
- Articulo 8Dokument8 SeitenArticulo 8Yerly Ramirez MuñozNoch keine Bewertungen
- Articulo6 PDFDokument17 SeitenArticulo6 PDFYerly Ramirez MuñozNoch keine Bewertungen
- Detection and Diagnosis of Oral Cancer by Light-Induced FluorescenceDokument8 SeitenDetection and Diagnosis of Oral Cancer by Light-Induced FluorescenceYerly Ramirez MuñozNoch keine Bewertungen
- Photodynamic Diagnosis of Oral Neoplasms Using Topical PhotofrinDokument10 SeitenPhotodynamic Diagnosis of Oral Neoplasms Using Topical PhotofrinYerly Ramirez MuñozNoch keine Bewertungen
- Assessment of Oral Premalignancy Using Elastic Scattering SpectrosDokument7 SeitenAssessment of Oral Premalignancy Using Elastic Scattering SpectrosYerly Ramirez MuñozNoch keine Bewertungen
- NAS Drive User ManualDokument59 SeitenNAS Drive User ManualCristian ScarlatNoch keine Bewertungen
- Work, Energy and Power: Checkpoint 1 (p.194)Dokument12 SeitenWork, Energy and Power: Checkpoint 1 (p.194)U KILLED MY DOGNoch keine Bewertungen
- ISO 9001 internal audit criteria and examples guideDokument22 SeitenISO 9001 internal audit criteria and examples guideMukesh Yadav100% (2)
- Entrepreneurship - Quarter 2 - Week 1-3 - 4 M's of Production and - Business ModelDokument6 SeitenEntrepreneurship - Quarter 2 - Week 1-3 - 4 M's of Production and - Business ModelJude Del RosarioNoch keine Bewertungen
- Aspartame Literature ReviewDokument10 SeitenAspartame Literature Reviewapi-272556824Noch keine Bewertungen
- Summary Essay Items..EditedDokument8 SeitenSummary Essay Items..EditedJoboy FritzNoch keine Bewertungen
- Compiled May 5, 2017 Case DigestDokument16 SeitenCompiled May 5, 2017 Case DigestGrace CastilloNoch keine Bewertungen
- CRUSADE of PRAYERS 1-170 Litany 1-6 For The Key To Paradise For DistributionDokument264 SeitenCRUSADE of PRAYERS 1-170 Litany 1-6 For The Key To Paradise For DistributionJESUS IS RETURNING DURING OUR GENERATION100% (10)
- Evirtualguru Computerscience 43 PDFDokument8 SeitenEvirtualguru Computerscience 43 PDFJAGANNATH THAWAITNoch keine Bewertungen
- Segmenting, Targeting, and Positioning (STP)Dokument16 SeitenSegmenting, Targeting, and Positioning (STP)Rachmat PutraNoch keine Bewertungen
- Compilation of Activities UBCVDokument13 SeitenCompilation of Activities UBCVRenell Vincent RamosNoch keine Bewertungen
- RITL 2007 (Full Text)Dokument366 SeitenRITL 2007 (Full Text)Institutul de Istorie și Teorie LiterarăNoch keine Bewertungen
- Superstitious Beliefs of MaranaoDokument13 SeitenSuperstitious Beliefs of MaranaoKhent Ives Acuno SudariaNoch keine Bewertungen
- January 2008 Ecobon Newsletter Hilton Head Island Audubon SocietyDokument6 SeitenJanuary 2008 Ecobon Newsletter Hilton Head Island Audubon SocietyHilton Head Island Audubon SocietyNoch keine Bewertungen
- BiblicalDokument413 SeitenBiblicalMichael DiazNoch keine Bewertungen
- 2005 Australian Secondary Schools Rugby League ChampionshipsDokument14 Seiten2005 Australian Secondary Schools Rugby League ChampionshipsDaisy HuntlyNoch keine Bewertungen
- 5E Lesson PlanDokument3 Seiten5E Lesson PlanSangteablacky 09100% (8)
- Class 7 Summer Vacation PDFDokument4 SeitenClass 7 Summer Vacation PDFPrince RajNoch keine Bewertungen
- Present Tense Exercises. Polish A1Dokument6 SeitenPresent Tense Exercises. Polish A1Pilar Moreno DíezNoch keine Bewertungen
- TOTAL Income: POSSTORE JERTEH - Account For 2021 Start Date 8/1/2021 End Date 8/31/2021Dokument9 SeitenTOTAL Income: POSSTORE JERTEH - Account For 2021 Start Date 8/1/2021 End Date 8/31/2021Alice NguNoch keine Bewertungen
- Eng10 LPQ3_4 Coherence and CohesionDokument2 SeitenEng10 LPQ3_4 Coherence and CohesionNiña RasonableNoch keine Bewertungen
- Study of Storm and Sewer Drains For Rajarhat (Ward No 4) in West Bengal Using Sewergems SoftwareDokument47 SeitenStudy of Storm and Sewer Drains For Rajarhat (Ward No 4) in West Bengal Using Sewergems SoftwareRuben Dario Posada BNoch keine Bewertungen
- Script - TEST 5 (1st Mid-Term)Dokument2 SeitenScript - TEST 5 (1st Mid-Term)Thu PhạmNoch keine Bewertungen
- Final Project On Employee EngagementDokument48 SeitenFinal Project On Employee Engagementanuja_solanki8903100% (1)
- SuccessDokument146 SeitenSuccessscribdNoch keine Bewertungen
- Instafin LogbookDokument4 SeitenInstafin LogbookAnonymous gV9BmXXHNoch keine Bewertungen
- Dukic WarehouselayoutsDokument14 SeitenDukic Warehouselayoutsrohitkamath7Noch keine Bewertungen
- 1995 - Legacy SystemsDokument5 Seiten1995 - Legacy SystemsJosé MªNoch keine Bewertungen
- Traditional Knowledge - The Changing Scenario in India PDFDokument9 SeitenTraditional Knowledge - The Changing Scenario in India PDFashutosh srivastavaNoch keine Bewertungen
- Size, Scale and Overall Proportion of Form, Basic Understanding of Various Shapes, Inter-Relationship of Visual FormsDokument17 SeitenSize, Scale and Overall Proportion of Form, Basic Understanding of Various Shapes, Inter-Relationship of Visual FormsJabbar AljanabyNoch keine Bewertungen