Beruflich Dokumente
Kultur Dokumente
DX Postop PT PDF
Hochgeladen von
Sherree HayesOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
DX Postop PT PDF
Hochgeladen von
Sherree HayesCopyright:
Verfügbare Formate
eNursing Care Plan 19-1
Postoperative Patient
This is a general nursing care plan for the postoperative patient. It should be
individualized and used in conjunction with a nursing care plan specific to the type of
surgery performed.
Nursing Diagnosis*
Impaired Breathing
Etiology: Use of opioid analgesia, respiratory irritation, increased secretions, and/or
airway obstruction
Supporting data: Dyspnea, crowing, shallow chest excursion, low O2 saturation level
Patient Goal
Maintains a breathing pattern that meets oxygen needs of the body
Outcomes (NOC) Interventions (NIC) and Rationales
Respiratory Status: Airway Respiratory Monitoring
Patency • Monitor rate, rhythm, depth, and effort of
• Respiratory rate ___ respirations to determine need for additional
• Respiratory rhythm ___ respiratory support.
• Depth of inspiration ___ • Monitor for noisy respirations, such as crowing or
• Ability to clear secretions ___ snoring that indicate airway obstruction.
• Monitor O2 saturation level continuously to detect
Measurement Scale inadequate respiratory ventilation and gas
1 = Severe deviation from normal exchange.
range • Auscultate breath sounds noting whether there are
2 = Substantial deviation from areas of decreased/absent ventilation and presence
normal range of adventitious sounds to detect signs of atelectasis,
3 = Moderate deviation from
secretions, or fluids.
normal range
4 = Mild deviation from normal • Determine the need for suctioning by auscultating
range for crackles and rhonchi over major airways.
5 = No deviation from normal range • Monitor patient’s ability to cough effectively to
remove secretions.
• Adventitious breath sounds • Position the patient in a lateral recovery position to
___ prevent aspiration.
• Dyspnea at rest ___
• Accumulation of sputum ___
Measurement Scale
1 = Severe
2 = Substantial
3 = Moderate
*Nursing diagnoses listed in order of priority.
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan 19-2
Outcomes (NOC) Interventions (NIC) and Rationales
4 = Mild
5 = None
Nursing Diagnosis
Acute Pain
Etiology: Surgical incision and reflex muscle spasm
Supporting data: Reports of pain, tense and guarded body posture, facial grimacing,
restlessness, irritability, moaning, diaphoresis, tachycardia
Patient Goals
1. Reports satisfaction with pain relief
2. Uses pain relief techniques effectively
Outcomes (NOC) Interventions (NIC) and Rationales
Pain Control Pain Management
• Uses analgesics as • Perform a comprehensive assessment of pain to
recommended ___ include location, characteristics, quality,
• Uses nonanalgesic relief onset/duration, frequency, intensity or severity of
measures _____ pain, and precipitating factors to plan appropriate
• Reports changes in pain interventions.
symptoms to health care • Provide the patient optimal pain relief with
professional ___ prescribed analgesics to relieve acute pain.
• Reports pain is controlled ___ • Implement the use of patient-controlled analgesia
(PCA) to permit patient control of analgesic dosing
Measurement Scale (if appropriate).
1 = Never demonstrated • Teach the use of nonpharmacologic adjunctive
2 = Rarely demonstrated techniques (e.g., relaxation, guided imagery, music
3 = Sometimes demonstrated therapy, distraction, massage) before, after, and—if
4 = Often demonstrated possible—during painful activities; before pain
5 = Consistently demonstrated
occurs or increases; and along with other pain relief
measures for patient to augment analgesics for pain
relief.
• Encourage patient to use adequate analgesics and
other pain control measures because if pain is
controlled, postoperative activities are more readily
performed, which helps prevent complications.
• Use pain control measures before pain becomes
severe to prevent pain that is difficult to control.
• Institute and modify pain control measures on the
basis of the patient’s response to individualize care.
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan 19-3
Nursing Diagnosis
Nausea
Etiology: Effects of anesthetic agents and gastrointestinal distention
Supporting data: Reports of nausea, refusal to consume fluids or solids, observed and/or
reported vomiting
Patient Goal
Has reduced or no episodes of nausea and vomiting
Outcomes (NOC) Interventions (NIC) and Rationales
Nausea and Vomiting Control Nausea Management
• Uses antiemetic medications as • Provide information about postoperative nausea,
recommended ___ such as causes of nausea and how long it will last, to
• Reports nausea, retching, and prevent negative anticipation of the nausea.
vomiting controlled ___ • Ensure that effective antiemetic drugs are given to
• Reports uncontrolled prevent nausea.
symptoms to health • Identify factors (e.g., medications, procedures) that
professional ___ may cause or contribute to nausea.
• Reduce or eliminate factors that precipitate or
Measurement Scale increase nausea (anxiety, pain, fear, and lack of
1 = Never demonstrated knowledge).
2 = Rarely demonstrated • Provide frequent oral hygiene to promote comfort
3 = Sometimes demonstrated
unless it stimulates nausea.
4 = Often demonstrated
5 = Consistently demonstrated
Vomiting Management
• Assess emesis for color, consistency, presence of
blood, timing, and extent to which it is forceful to
monitor for complications such as GI bleeding,
paralytic ileus, small bowel obstruction, etc.
• Measure or estimate emesis volume to evaluate fluid
status.
• Position to prevent aspiration. May position patient
in the lateral recovery position.
• Control environmental factors that may evoke
vomiting (e.g., aversive smells, sound, and
unpleasant visual stimulation)
• Provide comfort (such as cool cloths to forehead,
sponging face, or clean, dry clothes) during/after the
vomiting episode.
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan 19-4
Nursing Diagnosis
Fluid Imbalance
Etiology: stress response to surgery and abnormal fluid losses and gains throughout the
perioperative period
Supporting factors: Changes in blood pressure and weight, orthostatic hypotension,
tachycardia, decreased urine output, electrolyte imbalance
Patient Goals
1. Maintains fluid and electrolyte balance required for metabolic needs
2. Has no signs of hypovolemia or hypervolemia
Outcomes (NOC) Interventions (NIC) and Rationales
Fluid Balance Fluid/Electrolyte Management
• Blood pressure ___ • Obtain laboratory specimens to monitor for altered
• Radial pulse rate ___ fluid or electrolyte levels (e.g., hematocrit; blood
• Peripheral pulses ___ urea nitrogen; protein, sodium, and potassium
• Serum electrolytes ___ levels) to determine presence of fluid/electrolyte
• 24-hour intake and output imbalance.
balance ___ • Monitor for abnormal serum electrolyte levels to
• Stable body weight ___ determine need for replacements.
• Monitor vital signs to detect fluid imbalances and
Measurement Scale plan appropriate interventions.
1 = Severely compromised • Maintain IV solution containing electrolyte(s) at
2 = Substantially compromised ordered flow rate to prevent fluid and electrolyte
3 = Moderately compromised overload.
4 = Mildly compromised • Keep an accurate record of intake and output and
5 = Not compromised
weigh patient daily to document fluid losses or
gains.
• Administer prescribed supplemental electrolytes to
maintain electrolyte balance.
• Consult health care provider if signs and symptoms
of fluid and/or electrolyte imbalance persist or
worsen to intervene in a timely manner.
Nursing Diagnosis
Risk for Infection
Risk factors: altered skin integrity, inadequate nutrition and fluid intake, presence of
environmental pathogens, invasive instrumentation, and immobility
Patient Goal
Has no evidence of infection
Outcomes (NOC) Interventions (NIC) and Rationales
Infection Severity Airway Management
• Fever ___ • Position patient to maximize ventilation potential.
• White blood cell count • Remove secretions by encouraging coughing,
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan 19-5
Outcomes (NOC) Interventions (NIC) and Rationales
elevation ___ suctioning or performing oral care to prevent
• Purulent sputum ___ colonization of respiratory secretions.
• Purulent drainage • Encourage slow, deep breathing as well as turning
• Urine culture colonization ___ and coughing to remove secretions and prevent
• Wound site culture atelectasis.
colonization ___ • Assist with use of incentive spirometer to facilitate
removal of secretions and prevent atelectasis.
Measurement Scale
1 = Severe Tube or Drain Care
2 = Substantial • Administer skin care and dressing changes at the
3 = Moderate tube or drain insertion site to prevent infection.
4 = Mild • Inspect the area around the tube or drain insertion
5 = None
site for redness and skin breakdown to
identify/prevent infection.
Wound Healing: Primary
Intention • Monitor amount, color, and consistency of drainage
from tube or drain to detect infection.
• Purulent drainage ___
• Obtain cultures of any suspicious drainage to
• Serosanguineous drainage ___
identify presence of any pathogens.
• Surrounding skin erythema
___ Incision Site Care
• Periwound edema ___ • Inspect the incision site for redness, swelling, or
• Increased skin temperature ___ signs of dehiscence or evisceration to detect
• Foul odor of wound ___ complications.
• Note characteristics of drainage to detect
Measurement Scale
infection/active bleeding.
1 = Extensive
2 = Substantial • Obtain cultures of any suspicious drainage to
3 = Moderate identify presence of any pathogens.
4 = Limited • Cleanse the area around the incision with an
5 = None appropriate cleaning solution to reduce local
pathogens.
• Cleanse the area around any tube or drain site last to
prevent wound contamination.
• Change the dressing at appropriate intervals to
reduce microbial colonization.
Nutrition Management
• Determine, in collaboration with dietitian, number
of calories and type of nutrients needed to meet
nutrition requirements.
• Encourage calorie intake appropriate for body type
and lifestyle to facilitate adequate nutrition.
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan 19-6
Nursing Diagnosis
Lack of Knowledge
Etiology: Lack of information about surgery and postoperative care
Supporting data: States desire to manage postoperative care and reduce risk factors for
complications, questions about postoperative care
Patient Goals
1. Describes home management of surgical wound and pain
2. Identifies signs and symptoms that must be reported to a health care professional
Outcomes (NOC) Interventions (NIC) and Rationales
Compliance Behavior Teaching: Individual
• Discusses prescribed treatment • Appraise the patient’s current level of knowledge
regimen with health care and understanding of content to identify learning
professional ___ needs.
• Performs treatment regimen as • Tailor the content to the patient’s cognitive,
prescribed ___ psychomotor, and/or affective abilities/disabilities to
• Reports changes in symptoms promote learning.
to health care professional ___ • Provide time for the patient to ask questions and
• Monitors treatment response discuss concerns to identify any learning gaps.
___ • Document the content presented, the materials
• Performs activities of daily provided, and the patient’s understanding of the
living as prescribed ___ information or patient behaviors that indicate
learning on the permanent medical record.
Measurement Scale
1 = Never demonstrated Incision Site Care
2 = Rarely demonstrated • Teach the patient and caregiver how to care for the
3 = Sometimes demonstrated incision, including signs and symptoms of infection
4 = Often demonstrated
(e.g., redness, swelling, purulent drainage) to
5 = Consistently demonstrated
enhance the patient’s management of care.
Infection Control
• Teach the patient on how to care for the incision to
avoid infection.
• Teach patient and caregiver about signs and
symptoms of infection (e.g., increased temperature)
and when to report them to the health care provider
to enhance the patient’s management of care.
Nursing Diagnosis
Risk for Bleeding
Risk Factors: Ineffective vascular closure, changes in coagulation, treatment regimen
Patient Goal
Has no evidence of bleeding
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan 19-7
Outcomes (NOC) Interventions (NIC) and Rationales
Blood Loss Bleeding Reduction
• Decreased systolic BP ___ • Monitor for signs and symptoms of persistent
• Decreased diastolic BP ___ bleeding (i.e., check all secretions for frank or occult
• Increased heart rate ___ blood) to detect internal bleeding.
• Decreased cognition ___ • Monitor coagulation studies, including prothrombin
• Pallor ___ time (PT), partial thromboplastin time (PTT),
hemoglobin and hematocrit levels, and platelet
Blood Coagulation counts, to determine bleeding risk and detect
• Bleeding ___ hemorrhage.
• Bruising ___ • Protect patient from trauma to reduce tissue damage
• Petechiae ___ and subsequent bleeding into tissue.
• Ecchymosis ___ • Administer blood products (e.g., platelets, fresh
• Hematuria ___ frozen plasma) to replace coagulation factors.
• Hemoptysis ___ • Observe surgical site and dressings regularly,
including dependent sites (q1h for 4 hr, then q4h) to
Measurement Scale detect signs of bleeding.
1 = Severe • Monitor vital signs regularly from q15min to q2-4h
2 = Substantial as indicated to detect signs of hypovolemia.
3 = Moderate • Report abnormalities such as decreasing BP; rapid
4 = Mild pulse and respirations; cool, clammy skin; pallor;
5 = None and bright red blood on dressing, or excessive
bloody secretions from wound drains to intervene in
a timely manner.
• Monitor for changes in mental status, such as
restlessness and sense of impending doom, as
indicators of inadequate cerebral perfusion.
• Apply direct pressure or pressure dressings as
appropriate because decreases may indicate
hemorrhage.
• Maintain IV access sites for administration of fluids
and medications.
• Administer IV fluids as prescribed, keeping systolic
pressure at 90 mm Hg or more to maintain perfusion
to vital organs.
Nursing Diagnosis
Risk for Venous Thromboembolism
Risk factors: Dehydration, immobility, vascular manipulation, injury
Patient Goal
Has no evidence of venous thromboembolism
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan 19-8
Outcomes (NOC) Nursing Interventions and Rationales
Tissue Perfusion Circulatory Care: Venous Insufficiency
• Skin temperature _____ • Assess lower extremities for redness, swelling, and
• Peripheral edema _____ pain; increased warmth along path of vein; edema
• Rubor _____ or pain in extremity; chest pain; hemoptysis;
• Pain _____ tachypnea; dyspnea; and restlessness to detect
• Heart rate_____ signs/symptoms of venous thromboembolism or
• Level of consciousness _____ pulmonary embolism
• Administer anticoagulants (e.g., heparin,
Surgical Recovery enoxaparin [Lovenox]) as ordered to decrease clot
• Thrombophlebitis _____ formation.
• Pulmonary embolus ______ • Encourage early ambulation to maintain muscle
contractions and adequate vascular flow.
Measurement Scale • Avoid pressure under knees from bed or pillows to
1 = Severe deviation from normal avoid pressure on veins, constriction of circulation,
range or pooling and stasis of blood.
2 = Substantial deviation from • Apply intermittent pneumatic compression devices,
normal range if ordered, to promote venous circulation and
3 = Moderate deviation from normal remove for 1 hr q8-10h to allow for skin
range assessment.
4 = Mild deviation from normal
range
5 = No deviation from normal range
Nursing Diagnosis
Urinary Retention
Etiology: Supine positioning, pain, fear, analgesic and anesthetic medications, or surgical
procedure
Supporting data: Small voiding or absent urinary output, frequent voiding, bladder
distension, sensation of bladder fullness, overflow incontinence, residual urine
Patient Goal
Has no evidence of urinary retention
Outcomes (NOC) Nursing Interventions and Rationales
Urinary Elimination Urinary Retention Care
• Urinary retention _____ • Notify health care provider if patient does not
• Urinary incontinence _____ urinate within 6 hours after surgery to prevent
bladder distention and discomfort.
Measurement Scale • Assess for bladder pain and distention or decreased
1 = Severe or absent urinary output to detect if a problem is
2 = Substantial present.
3 = Moderate
• Percuss bladder or perform bedside bladder
4 = Mild
Copyright © 2020 by Elsevier, Inc. All rights reserved.
eNursing Care Plan 19-9
Outcomes (NOC) Nursing Interventions and Rationales
5 = None ultrasound as needed postoperatively to assess for
distention or urinary retention after voiding or
catheterization.
• Position patient in as normal a position as possible
for voiding.
• Ensure appropriate postoperative pain management
and provide privacy to reduce pain and anxiety to
optimize voiding.
Collaborative Problems
Potential Complication
Postoperative ileus
Risk factors: Bowel manipulation, immobility, pain medication, and anesthetics
Nursing Goals Nursing Interventions and Rationales
• Monitor for signs of • Assess for abdominal distention, presence of flatus
postoperative ileus or stool, bowel sounds, or nausea and vomiting to
• Report deviation from determine if postoperative ileus is present.
acceptable parameters • Maintain NPO status until peristalsis returns and
• Carry out appropriate medical ensure patency of nasogastric tube to prevent
and nursing interventions vomiting and abdominal distention.
• Encourage positioning on the right side and early
ambulation to facilitate expulsion of gas.
Copyright © 2020 by Elsevier, Inc. All rights reserved.
Das könnte Ihnen auch gefallen
- Chapter - 018 Nursing Care PlanDokument8 SeitenChapter - 018 Nursing Care PlansiewyonglimNoch keine Bewertungen
- DX Hepatitis PDFDokument14 SeitenDX Hepatitis PDFSherree HayesNoch keine Bewertungen
- DX Prostate Surgery PDFDokument4 SeitenDX Prostate Surgery PDFSherree HayesNoch keine Bewertungen
- DX Diarrhea PDFDokument11 SeitenDX Diarrhea PDFSherree HayesNoch keine Bewertungen
- Care Map UtiDokument1 SeiteCare Map UtiJonathonNoch keine Bewertungen
- DX Spine Injury PDFDokument5 SeitenDX Spine Injury PDFSherree HayesNoch keine Bewertungen
- DX Infective Endocarditis PDFDokument7 SeitenDX Infective Endocarditis PDFSherree HayesNoch keine Bewertungen
- Model Nursing CareplanDokument19 SeitenModel Nursing CareplanAnuchithra RadhakrishnanNoch keine Bewertungen
- DX Burns PDFDokument6 SeitenDX Burns PDFSherree HayesNoch keine Bewertungen
- 605 Nursing Care Plan 29-1: Patient With AsthmaDokument1 Seite605 Nursing Care Plan 29-1: Patient With AsthmaJonathonNoch keine Bewertungen
- DX Resp Failure PDFDokument5 SeitenDX Resp Failure PDFSherree HayesNoch keine Bewertungen
- Cues Nursing Diagnosis Scientific Rationale Objective Nursing Interventi ON Rationale EvaluationDokument9 SeitenCues Nursing Diagnosis Scientific Rationale Objective Nursing Interventi ON Rationale EvaluationTamil VillardoNoch keine Bewertungen
- Preoperative Care of The Patient Undergoing Orthopedic SurgeryDokument26 SeitenPreoperative Care of The Patient Undergoing Orthopedic SurgeryAbdul Gafoor CPNoch keine Bewertungen
- Patient With Acute Coronary Syndrome: N D P GDokument3 SeitenPatient With Acute Coronary Syndrome: N D P Gkazelle100% (1)
- ACSDokument21 SeitenACSchris_arc90100% (1)
- NCP Urinary Tract InfectionDokument19 SeitenNCP Urinary Tract InfectionYudistiro Adi Nugroho100% (1)
- ACS Nursing Care PlanDokument21 SeitenACS Nursing Care Planchris_arc90100% (6)
- DX Asthma PDFDokument6 SeitenDX Asthma PDFSherree HayesNoch keine Bewertungen
- 4 - Post Operative Nursing ManagementDokument38 Seiten4 - Post Operative Nursing ManagementraghadNoch keine Bewertungen
- Medical Management-Nursing Management and NCP For Acute ApendicitisDokument4 SeitenMedical Management-Nursing Management and NCP For Acute ApendicitisArki ObusanNoch keine Bewertungen
- Impaired Physical Mobility Related To Neuromuscular ImpairmentDokument17 SeitenImpaired Physical Mobility Related To Neuromuscular ImpairmentAileen Lopez83% (6)
- Penuemonia Care PalnDokument2 SeitenPenuemonia Care PalnVanessaMUellerNoch keine Bewertungen
- Understanding Medical Surgical Nursing - 0828-0828Dokument1 SeiteUnderstanding Medical Surgical Nursing - 0828-0828Anas TasyaNoch keine Bewertungen
- By: Clarissa E. Guifaya BSN301/GROUP 3Dokument17 SeitenBy: Clarissa E. Guifaya BSN301/GROUP 3Clarissa GuifayaNoch keine Bewertungen
- DiagnosisDokument12 SeitenDiagnosisHCX dghhqNoch keine Bewertungen
- Nursing Care PlansDokument5 SeitenNursing Care PlansMargaret SibugNoch keine Bewertungen
- College of Nursing Related Learning Experience Plan Course Title: NCM 109: Sample of Alternative Activities For Clinical Practice (RLE Equivalent 8 Hours)Dokument5 SeitenCollege of Nursing Related Learning Experience Plan Course Title: NCM 109: Sample of Alternative Activities For Clinical Practice (RLE Equivalent 8 Hours)Danica Yen PagalNoch keine Bewertungen
- ReportDokument60 SeitenReportNikky Rossel Flores100% (1)
- Alcohol Withdrawal Care PlanDokument1 SeiteAlcohol Withdrawal Care PlanVanessaMUeller100% (1)
- Perioperative ManagementDokument8 SeitenPerioperative ManagementJaezee RamosNoch keine Bewertungen
- © 2020 Lippincott Advisor Nursing Care Plans For Medical Diagnoses - Coronavirus Disease 2019 (COVID 19) PDFDokument7 Seiten© 2020 Lippincott Advisor Nursing Care Plans For Medical Diagnoses - Coronavirus Disease 2019 (COVID 19) PDFVette Angelikka Dela CruzNoch keine Bewertungen
- Appendicitis:: Ideal Management Nursing Interventions and Management Rationale/ResultsDokument7 SeitenAppendicitis:: Ideal Management Nursing Interventions and Management Rationale/ResultsAlmer OstreaNoch keine Bewertungen
- Nursing Care PlanDokument3 SeitenNursing Care PlanJovi BrizNoch keine Bewertungen
- Nursing Care Plan APDokument3 SeitenNursing Care Plan APMargarita PaureneNoch keine Bewertungen
- Postoperative Care PlanDokument4 SeitenPostoperative Care Plannittin006100% (1)
- Actual Nursing Care Plan GT DisorderDokument3 SeitenActual Nursing Care Plan GT DisordermandzkievonnieNoch keine Bewertungen
- Impaired Skin Integrity Related To Pruritus From Jaundice and EdemaDokument6 SeitenImpaired Skin Integrity Related To Pruritus From Jaundice and EdemaDwi Kurnia SariNoch keine Bewertungen
- Nursing Care Plan 4 Gas Exchange, ImpairedDokument9 SeitenNursing Care Plan 4 Gas Exchange, Impaireddbryant0101100% (6)
- Impaired Skin Integrity and ConstipationDokument6 SeitenImpaired Skin Integrity and Constipationdlneisha61100% (1)
- Surgical VoicedDokument38 SeitenSurgical Voicedjoyceifeoluwa04Noch keine Bewertungen
- General Anaesthesia in Acute Limb Ischemic Right R/ AmputationDokument20 SeitenGeneral Anaesthesia in Acute Limb Ischemic Right R/ AmputationBangun Cholifa nusantaraNoch keine Bewertungen
- 4 - Post Operative Phase 1Dokument39 Seiten4 - Post Operative Phase 1ننن نننن100% (4)
- Role of Anesthesia Nurse in Operation TheatreDokument37 SeitenRole of Anesthesia Nurse in Operation TheatreZainul SaifiNoch keine Bewertungen
- SCR 270 L & D Care PlanDokument5 SeitenSCR 270 L & D Care PlanRenzo MarcosNoch keine Bewertungen
- Kedarsing Care PlanDokument9 SeitenKedarsing Care PlanAmit BarveNoch keine Bewertungen
- COPD Care PLAN PDFDokument2 SeitenCOPD Care PLAN PDFVanessaMUeller100% (1)
- Pre-Operative Nursing CareDokument79 SeitenPre-Operative Nursing CarePeter FrimpongNoch keine Bewertungen
- Chapter 027Dokument7 SeitenChapter 027Diamonique95Noch keine Bewertungen
- General Nursing Care Plan PDFDokument17 SeitenGeneral Nursing Care Plan PDFTmanoj Praveen100% (1)
- DX Heart Failure PDFDokument4 SeitenDX Heart Failure PDFSherree Hayes100% (1)
- Diagno SIS Planni NG Intervention Rationale Evaluati ONDokument3 SeitenDiagno SIS Planni NG Intervention Rationale Evaluati ONAnn Nicole G. NeriNoch keine Bewertungen
- Oral Presentation 4 NeuroDokument36 SeitenOral Presentation 4 NeuroAhmad YusufNoch keine Bewertungen
- By:Mazni Binti Mirus RN1 Male Surgical Unit Security Forces Hospital Makkah 18 AUGUST 2016Dokument37 SeitenBy:Mazni Binti Mirus RN1 Male Surgical Unit Security Forces Hospital Makkah 18 AUGUST 2016Gummie Akalal Sugala100% (1)
- CASE STUDY PPT Group1 - Revised WithoutvideoDokument34 SeitenCASE STUDY PPT Group1 - Revised WithoutvideoSamantha BolanteNoch keine Bewertungen
- The Ultimate Gastric Sleeve Bariatric Diet Cookbook:The Essential Nutrition Guide For Every Phase Of Recovery After Weight Loss Surgery With Delectable And Nutritious RecipesVon EverandThe Ultimate Gastric Sleeve Bariatric Diet Cookbook:The Essential Nutrition Guide For Every Phase Of Recovery After Weight Loss Surgery With Delectable And Nutritious RecipesNoch keine Bewertungen
- Fast Facts: Perioperative Pain: Effective management has numerous benefitsVon EverandFast Facts: Perioperative Pain: Effective management has numerous benefitsNoch keine Bewertungen
- Differentiating Anesthesia Equipment: Identify and Understand Anesthesia Equipment in 1 Hour (Including the most popular manufacturers and suppliers to buy Anesthesia Equipment)Von EverandDifferentiating Anesthesia Equipment: Identify and Understand Anesthesia Equipment in 1 Hour (Including the most popular manufacturers and suppliers to buy Anesthesia Equipment)Noch keine Bewertungen
- Local Anesthesia Made Easy: Complete Guide on How to make your Local Anesthetic Procedure a Success (Including a List of Anesthetic Equipment and their Uses)Von EverandLocal Anesthesia Made Easy: Complete Guide on How to make your Local Anesthetic Procedure a Success (Including a List of Anesthetic Equipment and their Uses)Noch keine Bewertungen
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingVon EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNoch keine Bewertungen
- DX Hyperthyoidism PDFDokument10 SeitenDX Hyperthyoidism PDFSherree HayesNoch keine Bewertungen
- DX Stroke PDFDokument8 SeitenDX Stroke PDFSherree HayesNoch keine Bewertungen
- DX Spine Injury PDFDokument5 SeitenDX Spine Injury PDFSherree HayesNoch keine Bewertungen
- DX Resp Failure PDFDokument5 SeitenDX Resp Failure PDFSherree HayesNoch keine Bewertungen
- DX Osteo Issue PDFDokument9 SeitenDX Osteo Issue PDFSherree HayesNoch keine Bewertungen
- DX Heart Failure PDFDokument4 SeitenDX Heart Failure PDFSherree Hayes100% (1)
- DX Intracranial Pressure PDFDokument8 SeitenDX Intracranial Pressure PDFSherree HayesNoch keine Bewertungen
- DX Hysterectomy PDFDokument1 SeiteDX Hysterectomy PDFSherree HayesNoch keine Bewertungen
- DX Fracture PDFDokument8 SeitenDX Fracture PDFSherree HayesNoch keine Bewertungen
- COPD Concept MapDokument1 SeiteCOPD Concept MapSherree HayesNoch keine Bewertungen
- DX Burns PDFDokument6 SeitenDX Burns PDFSherree HayesNoch keine Bewertungen
- DX Alcohol Withdrawal PDFDokument3 SeitenDX Alcohol Withdrawal PDFSherree Hayes100% (1)
- DX Infective Endocarditis PDFDokument7 SeitenDX Infective Endocarditis PDFSherree HayesNoch keine Bewertungen
- DX DM PDFDokument6 SeitenDX DM PDFSherree HayesNoch keine Bewertungen
- Tuberculosis / TBDokument11 SeitenTuberculosis / TBSherree HayesNoch keine Bewertungen
- DX Asthma PDFDokument6 SeitenDX Asthma PDFSherree HayesNoch keine Bewertungen
- Chapter 27: Lower Respiratory Problems Pleural Effusion With Thoracentesis and Chest TubeDokument3 SeitenChapter 27: Lower Respiratory Problems Pleural Effusion With Thoracentesis and Chest TubeSherree HayesNoch keine Bewertungen
- Respiratory Viruses: Organisms Causing PneumoniaDokument17 SeitenRespiratory Viruses: Organisms Causing PneumoniaSherree HayesNoch keine Bewertungen
- COPDDokument11 SeitenCOPDSherree HayesNoch keine Bewertungen
- Acute Respiratory Distress SyndromeDokument17 SeitenAcute Respiratory Distress SyndromeSherree Hayes100% (2)
- EKG/ECG Study GuideDokument13 SeitenEKG/ECG Study GuideSherree HayesNoch keine Bewertungen
- Acute Coronary SyndromeDokument19 SeitenAcute Coronary SyndromeSherree HayesNoch keine Bewertungen
- ResultDokument19 SeitenResultEndri SulistyoriniNoch keine Bewertungen
- 69-Article Text-283-2-10-2022Dokument8 Seiten69-Article Text-283-2-10-2022EfanNoch keine Bewertungen
- Prime Health Med. Svcs. Co. Laila Gomaa, MD. (PD PMC)Dokument10 SeitenPrime Health Med. Svcs. Co. Laila Gomaa, MD. (PD PMC)James LindonNoch keine Bewertungen
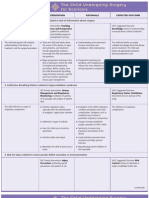
- NURSING CARE PLAN The Child Undergoing Surgery For ScoliosisDokument3 SeitenNURSING CARE PLAN The Child Undergoing Surgery For ScoliosisscrewdriverNoch keine Bewertungen
- Pain Management ProcedureDokument3 SeitenPain Management Procedurebylaw_12Noch keine Bewertungen
- Dolphin Neurostim Brochure Professional Web PDFDokument2 SeitenDolphin Neurostim Brochure Professional Web PDFNeptune ShellNoch keine Bewertungen
- Safety of Topical Ibuprofen GelDokument1 SeiteSafety of Topical Ibuprofen GelNarongchai PongpanNoch keine Bewertungen
- AnalgesikDokument2 SeitenAnalgesikNopriani InuarNoch keine Bewertungen
- Jcia QaDokument84 SeitenJcia Qahegdeshailu50% (4)
- Pain Assessment & ManagementDokument36 SeitenPain Assessment & ManagementremeroseNoch keine Bewertungen
- Chapter - 31 - Opioid - Analgesics - Antagonist - PDF Filename UTF-8''Chapter 31 Opioid Analgesics & AntagonistDokument6 SeitenChapter - 31 - Opioid - Analgesics - Antagonist - PDF Filename UTF-8''Chapter 31 Opioid Analgesics & AntagonistJoherNoch keine Bewertungen
- NUR 2115 Final Exam Fundamentals of Professional Nursing Final Exam Concept Review Fall 2020 Rasmussen College - RemovedDokument5 SeitenNUR 2115 Final Exam Fundamentals of Professional Nursing Final Exam Concept Review Fall 2020 Rasmussen College - RemovedJudy DurkinNoch keine Bewertungen
- Analysis Epidural Analgesia Intra Operative Cocktail Pain Management Knee Replacement TKRDokument7 SeitenAnalysis Epidural Analgesia Intra Operative Cocktail Pain Management Knee Replacement TKRSSR-IIJLS JournalNoch keine Bewertungen
- OsteoarthritisDokument58 SeitenOsteoarthritislina jamal100% (1)
- Essential Anesthesia From Science To Practice,.46Dokument1 SeiteEssential Anesthesia From Science To Practice,.46Jean PaulNoch keine Bewertungen
- Non-Pharmacological Pain Relief Measures During Labor and DeliveryDokument14 SeitenNon-Pharmacological Pain Relief Measures During Labor and DeliveryStudent NurseNoch keine Bewertungen
- Nursing Care PlanDokument7 SeitenNursing Care Planmcd7r883% (6)
- Brief Guide To Common PainkillersDokument1 SeiteBrief Guide To Common Painkillers11113432Noch keine Bewertungen
- Sample EssayDokument14 SeitenSample EssayNiazNoch keine Bewertungen
- Clinical Pathway For Laryngectomy Patients Rev 3-3-14Dokument6 SeitenClinical Pathway For Laryngectomy Patients Rev 3-3-14api-292187141Noch keine Bewertungen
- PainDokument230 SeitenPainAnonymous uGbcVSJTDg100% (8)
- Clin Psychology and Psychoth - 2017 - Durá Ferrandis - Confirming The Mechanisms Behind Cognitive Behavioural TherapyDokument7 SeitenClin Psychology and Psychoth - 2017 - Durá Ferrandis - Confirming The Mechanisms Behind Cognitive Behavioural TherapyNatalie JaraNoch keine Bewertungen
- Hallus Valgus and VarusDokument37 SeitenHallus Valgus and VarusAyesha ShafiqNoch keine Bewertungen
- A Randomized Controlled Trial of Exercise and Manipulative Therapy For Cervicogenic HeadacheDokument9 SeitenA Randomized Controlled Trial of Exercise and Manipulative Therapy For Cervicogenic Headachepaulina_810Noch keine Bewertungen
- Interventional Examination: Information Bulletin For Certification As Fellow of Interventional Pain Practice (FIPP)Dokument21 SeitenInterventional Examination: Information Bulletin For Certification As Fellow of Interventional Pain Practice (FIPP)DRAcula100% (1)
- "My Neck Feels Stiff and There's Pain Coming From It. Every Time I Move It, It Only Gets Worse." As Stated by TheDokument4 Seiten"My Neck Feels Stiff and There's Pain Coming From It. Every Time I Move It, It Only Gets Worse." As Stated by TheCassey CuregNoch keine Bewertungen
- Jaundice Case StudyDokument9 SeitenJaundice Case StudyAlfadz AsakilNoch keine Bewertungen
- Manajemen NyeriDokument2 SeitenManajemen Nyeriscan resepNoch keine Bewertungen
- Physical and Psychosocial Challenges in AdultDokument8 SeitenPhysical and Psychosocial Challenges in AdultYusuf ZulfikarNoch keine Bewertungen
- Daradia Pain Hospital, The Exclusive Pain Management Hospital, Not Only Treats Pain, But Also Organizes Pain Management Courses To Train PhysiciansDokument2 SeitenDaradia Pain Hospital, The Exclusive Pain Management Hospital, Not Only Treats Pain, But Also Organizes Pain Management Courses To Train PhysiciansPR.comNoch keine Bewertungen