Beruflich Dokumente
Kultur Dokumente
Pelagia Research Library: Available Online at
Hochgeladen von
Anantha LakshmiOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pelagia Research Library: Available Online at
Hochgeladen von
Anantha LakshmiCopyright:
Verfügbare Formate
Available online at www.pelagiaresearchlibrary.
com
Pelagia Research Library
Der Pharmacia Sinica, 2012, 3 (5):604-609
ISSN: 0976-8688
CODEN (USA): PSHIBD
Acute toxicity studies of metformin microspheres prepared by two
different methods
Navneet Garud* and Akanksha Garud
Institute of Professional Studies (IPS)- College of Pharmacy, Shivpuri Link Road, Gwalior
(M.P.), India
_____________________________________________________________________________________________
ABSTRACT
Previously microspheres containing metformin hydrochloride were prepared by using two different methods viz.
ionotropic gelation and solvent evaporation method. In this study, acute toxicity studies were investigated in male
albino rats following oral administration of the microspheres. The rats were carefully observed for any clinical
signs for seven days, and gross observations of the organs were performed at 14 days. The blood glucose level was
sustained to normal values till 12 h with microspheres using carbopol 934P polymer (C3, prepared by using
ionotropic gelation method) and the chitosan microspheres (CH3, prepared by using non-aqueous solvent
evaporation method). No toxic symptoms or mortality were observed for all the formulations up to dose 2 g/kg body
weight. Treatment with all formulations for fourteen days significantly attenuated (p<0.01) the elevated total
cholesterol and triglyceride levels in comparison with the vehicle treated diabetic rats.
Keywords: Microspheres, metformin hydrochloride, drug delivery, toxicity
_____________________________________________________________________________________________
INTRODUCTION
Diabetes is major causes of death and disability in the world. The latest World Health Organization (WHO) estimate
for the number of people with diabetes worldwide, in 2000, is 171 million, which is likely to be at least 366 million
by 2030. The focus of medical community is on the prevention and treatment of the disease, as is evident from the
rising number of research papers on the subject [1]. Microencapsulation is an accepted process used to achieve
controlled release and drug targeting for many years [2].
Metformin hydrochloride (MTF) is an antidiabetic drug used to treat Non-insulin dependent diabetic mellitus,
NIDDM [3] and is indicated as an adjunct to diet to lower blood glucose in cases where hyperglycemia cannot be
controlled satisfactorily on diet alone. MTF has got a short half-life of about two hours. The selected multi-unit
MTF microspheric drug delivery system in previous studies is expected to provide clinicians with a new choice of
an economical, safe and more bioavailable formulation in the management of type II diabetes mellitus. Although
much literature is available on the in-vitro studies of metformin microspheres [4-5], comparatively less work has
been done on assessing the in-vivo activity of the prepared microspheres [6]. Therefore, an attempt is made to assess
the in-vivo studies of the prepared microspheres containing metformin hydrochloride on experimental animals.
604
Pelagia Research Library
Navneet Garud et al Der Pharmacia Sinica, 2012, 3(5):604-609
______________________________________________________________________________
MATERIALS AND METHODS
MTF was a gift sample from Sun Pharmaceuticals, Baroda. Sodium alginate (CDH, New Delhi), Calcium chloride
(Qualigens, Mumbai), diSodium hydrogen phosphate (CDH, New Delhi), potassium dihydrogen phosphate (CDH,
New Delhi), NaOH (Merck Ltd, Mumbai), Hydrochloric acid (Merck Ltd, Mumbai), Sodium Chloride (Merck Ltd,
Mumbai), Acetone and Liquid paraffin (Merck Ltd, Mumbai), Ethylcellulose was commercially obtained from S.D.
Fine Chemicals, Mumbai. Hydroxypropylmethylcellulose (HPMC-E15) and Carbopol-934P was procured from
Central Drug House, Mumbai. Chitosan (medium viscosity grade) was procured from Central Institute of Fisheries
Technology, Cochin.
Glutaraldehyde from Spectrochem Pvt. Ltd (Mumbai), Streptozotocin was purchased from Sigma Chemicals
(Germany). All other reagents and solvents used in experiment were of pharmaceutical or analytical grade and
purchased from their respective commercial sources.
Test Animals
Randomly bred male albino rats of Wistar strain, weighing about 250-300 g were purchased from Animal facility
division, Defence Research and Development Establishment (DRDE) and used for the study. The animals were
maintained in the animal colony of IPS, College of Pharmacy and further used for the experiments. Rats were
allowed to acclimatize to the experimental room conditions for a period of seven days prior to pre-exposure
examination for gross motor activity and appearance. During the acclimatization period, the rats were observed for
clinical signs of disease. Prior to the experiment, a detailed physical examination was performed on the animals.
The animals were maintained in an environment-controlled room. They were housed in rooms maintained at a
temperature of 25 ± 2°C with humidity at 50-55% throughout the experimental period. The experimental room
temperature and humidity were monitored daily. A photoperiod of 12 h light and 12 h dark was maintained
throughout the duration of experiment. They were housed in polypropylene cages, four per cage, with dry and dust-
free rice husk as the bedding material. The rice husk was changed every alternate day. They were provided
commercial pellet feed (Lipton feed, Bombay, India) and water ad libitum during the experimental period.
The care and maintenance of animals were as per the approved guidelines of the “Committee for the Purpose of
Control and Supervision of Experiments on Animals (CPCSEA), India (No. 1039/AC/07/CPCSEA). All animal
procedures were approved by the Ethical Committee of the Establishment.
Preparation of microspheres
Metformin microspheres were prepared by using ionotropic gelation method and solvent evaporation method,
respectively in our previous studies [7-8] using different polymers such as ethylcellulose, HPMC, carbopol 934P and
chitosan. A comparative release profile for microspheres (at 1:3 alginate: polymer concentration) produced by using
ionotropic gelation method showed that the formulation containing alginate: carbopol 934P (1:3) gave the most
sustained effect [7]. Drug release rate at 1:3 drug: polymer for microspheres produced by solvent evaporation
method at a stirring rate of 1200 rpm was in the following order: carbopol 934P > HPMC > ethyl cellulose >
chitosan [8].
Induction of Diabetes
Experimental diabetes was induced in the rats using streptozotocin (60 mg/kg). Streptozotocin was dissolved in 0.5
ml of citrate buffer (pH 4.5) and injected intraperitoneally into rats that had been fasted overnight but with access to
water ad libitum. The extent of diabetic induction was monitored and based on blood glucose levels and weight
decrease. Blood glucose levels greater than 180 mg/dl were accepted as the basal level for diabetes. This blood
glucose level was achieved after 2-4 day of treatment with streptozotocin.
Acute toxicity evaluation in rats
The selected formulations from both the methods used for the preparation of microspheres were tested for acute
toxicity (if any) in rats. To determine the acute toxicity of a single oral administration, different doses of the
formulation (0.5, 1.0, 1.5 and 2.0 g/kg body weight) were administered to different groups of rats (six rats were used
for each group). Mortality and general behavior of the animals were observed continuously for the initial four hours
605
Pelagia Research Library
Navneet Garud et al Der Pharmacia Sinica, 2012, 3(5):604-609
______________________________________________________________________________
and intermittently for the next six hours and then again at 24 hrs and 48 hrs following dose administration. The
parameters observed were grooming, hyperactivity, sedation, loss of righting reflex, respiratory rate and
convulsions.
Antidiabetic activity evaluation
Diabetes was induced in albino rats with administration of single dose of streptozotocin (60 mg/kg body weight,
i.p.). After 72 hrs, the animals with fasting blood glucose level > 180 mg/dl were considered diabetic. The diabetic
rats were randomly divided into eleven groups containing six rats in each group. One group of six rats was kept
without streptozotocin administration as normal control. The groups were made as follows:
Group I: Normal, receive normal rat feed and water, ad libitum
Group II: Diabetic control, receive streptozotocin 60 mg/kg body weight, with normal rat feed and water, ad libitum
Group III: Diabetic standard, treated with Metformin (500 mg/kg, p.o.)
Group IV: Diabetic test, treated with the microspheric formulation A3
Group V: Diabetic test, treated with the microspheric formulation B3
Group VI: Diabetic test, treated with the microspheric formulation C3
Group VII: Diabetic test, treated with the microspheric formulation D3
Group VIII: Diabetic test, treated with the microspheric formulation E3
Group IX: Diabetic test, treated with the microspheric formulation H3
Group X: Diabetic test, treated with the microspheric formulation CA3
Group XI: Diabetic test, treated with the microspheric formulation CH3
Biochemical parameters
After the completion of 14 days, blood samples were collected from retro orbital sinus in micro-centrifuge tube
presaturated with heparin. It was centrifuged at 3000 rpm for 20 min; the serum thus obtained was separated and
used immediately for the further estimation [9]. The following biochemical parameters such as total protein, total
cholesterol and triglyceride levels were studied using diagnostic kits (Merck Limited, Mumbai).
Statistical analysis
The data obtained in present investigation was subjected to statistical analysis. All results were expressed as Mean±
S.D. The data were analyzed using Analysis of variance (ANOVA) and the group means were compared by Student-
Newman Keule’s test. Values were considered statistically significant when p<0.01. Graph Pad Instat 3 was used for
the analysis of data.
RESULTS AND DISCUSSION
In-vivo studies of microspheres
Based on the in-vitro release profile for the selected formulations namely, A3, B3, C3 and D3 (prepared by
ionotropic gelation method) and E3, H3, CA3 and CH3 (prepared by non-aqueous solvent evaporation method) were
studied for their in-vivo effect (Table 1). Intravenous injection of 60 mg/kg of Streptozotocin in male adult Wistar
rats, makes pancreas swell and at last causes degeneration in Langerhans islet beta cells and induces experimental
diabetes mellitus in 2-4 days.
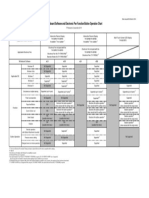
Table 1: Composition of metformin microspheres prepared using ionotropic gelation method (A3, B3, C3, D3) and solvent evaporation
method (E3, H3, CA3, CH3).
Code Drug: Polymer Method
A3 Drug:Alginate:ethylcellulose (1:1:3) Ionotropic gelation method
B3 Drug:Alginate:HPMC (1:1:3) Ionotropic gelation method
C3 Drug:Alginate:carbopol 934P (1:1:3) Ionotropic gelation method
D3 Drug:Alginate:chitosan (1:1:3) Ionotropic gelation method
E3 Drug: ethylcellulose (1:3) Solvent evaporation method
H3 Drug: HPMC (1:3) Solvent evaporation method
CA3 Drug: carbopol 934P (1:3) Solvent evaporation method
CH3 Drug: chitosan (1:3) Solvent evaporation method
Key: HPMC denotes hydroxypropyl methylcellulose, Drug used in the study is metformin hydrochloride
Induction of experimental diabetes mellitus in male adult rats weighing 250-300 g is indeed the first step in
decreasing Nicotinamide-adenine dinucleotide (NAD) in pancreas islet beta cells and causes histopathological
606
Pelagia Research Library
Navneet Garud et al Der Pharmacia Sinica, 2012, 3(5):604-609
______________________________________________________________________________
effects in beta cells which probably intermediates diabetes induction [10]. The use of Streptozotocin for diabetes
induction was done as it is claimed to have advantages of greater specificity and lower toxicity over alloxan [11].
The weight and blood glucose level changes in the rats treated with 60 mg/kg body weight of streptozotocin were
significant. This is a good way of assessing the extent of diabetes induction in the animals and this approach has
been described by other workers [12].
Acute toxicity studies
In acute toxicity study no toxic symptoms were observed for all the formulations up to dose 2 g/kg body weight. All
animals behaved normally. No neurological or behavioral effects could be noted. No mortality was found up to 14
days study. Streptozotocin (60 mg/kg) administration resulted in significant reduction in body weight.
Administration of various microspheric formulations at equivalent dose of 500 mg/kg administered were able to
correct this aberration significantly (p<0.01). The change in body weight observed is represented in Table- 2.
Effect on blood glucose
Streptozotocin (60 mg/kg) administration resulted in significant elevation of glucose level. In-vivo evaluation of the
selected formulations of metformin microspheres prepared by both the methods i.e. ionotropic gelation and non-
aqueous solvent evaporation method were carried out in healthy normal male Wistar rats by measuring the
hypoglycemic effect produced after their oral administration at a dose equivalent to 500 mg/kg of metformin in
comparison with pure metformin hydrochloride at the same dose. When pure metformin was administered, a rapid
reduction in blood glucose level was observed within 3 h which rapidly reached to the diabetic level requiring
further dosing.
In case of microspheres prepared by the ionotropic gelation method, the reduction in blood glucose levels was
slower which sustained over longer periods of time. Maximum reduction was observed with microspheres using
carbopol 934P polymer (Figure- 1) whereas the blood glucose level was sustained to normal values till 12 h in case
of the chitosan microspheres prepared by using non-aqueous solvent evaporation method (Figure- 2). The sustained
hypoglycemic effect observed over longer period of time was due to the retardant effect of the polymers used in the
microspheres.
Figure- 1
In-Vivo comparative study of blood gluose level of rats in various
formulations of metformin microspheres prepared by Ionotropic gelation
method
250
Blood gluose level (mg/dl)
200
Standard
150 A3 (EC)
B3(HPMC)
100 C3(Carbopol)
D3(Chitosan)
50
0
0 2 4 6 8 10 12 14 16
Time (hrs)
Effect on biochemical parameters
Diabetes leads to various metabolic aberrations in the animals namely increase blood glucose, decreased protein
content and increased level of cholesterol and triglyceride. There was a marked decrease in the plasma protein
content of untreated diabetic group (p<0.01) when compared with that of the control. All the selected formulations
were able to correct this metabolic disturbance significantly. Total cholesterol and triglyceride levels were found to
be significantly (p<0.01) increased in the vehicle treated diabetic group in comparison with the control group.
607
Pelagia Research Library
Navneet Garud et al Der Pharmacia Sinica, 2012, 3(5):604-609
______________________________________________________________________________
Treatment with all formulations for fourteen days significantly attenuated (p<0.01) the elevated total cholesterol and
triglyceride levels in comparison with the vehicle treated diabetic rats given in Table- 2, Figure- 3.
Figure- 2
In-Vivo comparative study of blood glulose level of rats in various
formulations of metformin microspheres prepared by solvent
evaporation method
250
Blood gluose level (mg/dl)
200
Standard
150 E3 (EC)
H3 (HPMC)
100 CA3 (Carbopol)
CH3 (Chitosan)
50
0
0 2 4 6 8 10 12 14 16
Time (hrs)
Figure- 3
Effects of various formulations on some biochemical parameters in
Streptozocin-induced diabetic rats
160
140
120
100 Cholestrol (mg/dl)
Values
80 Triglyceride (mg/dl)
60 Total protein (g/dl)
40
20
0
)
in
l
3
3
3
al
A3
tro
H
A
E
rm
D
m
on
C
+
+
+
+
or
fo
+
tic
tic
tic
tic
C
tic
tic
N
et
tic
tic
be
be
be
be
tic
(M
be
be
be
be
be
ia
ia
ia
ia
ia
ia
d
ia
ia
D
D
D
D
ar
ia
D
D
nd
ta
S
tic
be
ia
D
Groups
Table 2: Effects of various formulations biochemical parameters and change in body weight in Streptozocin-induced diabetic rats
Cholesterol Triglyceride Total protein
S No. Group (S) Change in body weight (g)
(mg/dl) (mg/dl) (g/dl)
1 Normal 111.69 ± 5.32 80.52 ± 2.78 7.79 ± 0.48 + 20.65
2 Diabetic Control 144.7 ± 5.02 105.7 ± 4.35 4.02 ± 0.24 - 33.75
3 Diabetic Standard (Metformin) 108.06 ± 3.1 84.35 ± 0.01 6.59 ± 0.13 + 28.54
4 Diabetic + A3 114.4 ± 5.85 86.7 ± 0.28 5.51 ± 0.23 + 10.12
5 Diabetic + B3 117.7 ± 4.57 88.5 ± 0.01 6.97 ± 0.12 + 11.34
6 Diabetic + C3 116.9 ± 7.27 84.06 ± 0.02 6.4 ± 0.64 + 14.85
7 Diabetic + D3 112.1 ± 8.13 92.4 ± 0.03 6.5 ± 0.44 + 11.86
8 Diabetic + E3 117.9 ± 3.87 88.4± 0.12 5.73 ± 0.32 + 14.91
9 Diabetic + H3 116.2 ± 5.87 87.5± 0.63 5.82 ± 0.52 + 11.43
10 Diabetic + CA3 118.3 ± 3.19 84.6 ± 0.03 6.27 ± 0.27 + 14.36
11 Diabetic + CH3 113.74 ± 0.6 85.6 ± 0.06 6.16 ± 0.25 + 11.24
Values are given as Mean ± S.D.
608
Pelagia Research Library
Navneet Garud et al Der Pharmacia Sinica, 2012, 3(5):604-609
______________________________________________________________________________
CONCLUSION
The microspheres of metformin hydrochloride prepared by using ionotropic gelation and solvent evaporation
method were capable to lower the blood glucose level for 12 h. The sustained hypoglycemic effect observed over
longer period of time was due to the retardant effect of the polymers used in the microspheres. Microspheres using
carbopol 934P polymer and chitosan demonstrated significant blood glucose reduction. Thus, the microspheres
produced by both methods were not only promising for the sustained oral delivery of metformin hydrochloride in-
vitro but also produced sufficient hypoglycemic effect in experimental animals.
REFERENCES
[1] Ghodake J.D., Vidhate J.S., Shinde D.A., Kadam A.N. Int. J. Pharm.Tech. Res., 2010, 2(1), 378-384
[2] Mankala S.K., Korla A.C., Gade S. J Adv Pharm Technol Res., 2011, 2(4), 245-54.
[3] Yuen K.H, Peh K.K, and Tan B.I. Drug Dev Ind Pharm, 1999, 25(5), 613-618.
[4] Choudhury PK, Kar M. J Microencapsul, 2009, 26(1), 46-53.
[5] Deb J., Venkateswarlu B.S., Ghosh A., Choudhuri T., Paul P., Faizi M. Asian Journal of Biomedical and
Pharmaceutical Sciences, 2011, 1(2), 11-19
[6] Yadav V.K., Kumar B., Prajapati S.K., Shafaat K. International Journal of Drug Delivery, 2011, 3, 357-370
[7] Garud N., Garud A., Jain N. Journal of Pharmacy Research, 2011, 4(7), 2103-2106.
[8] Garud N. and Garud A. Trop J Pharm Res, 2012, 11(4), 577-583
[9] Tenpe C.R. and Yeole P.G. Int. J. Pharm.Tech. Res, 2009, 1(1), 43-49
[10] Akbarzadeh A., Norouzian D., Mehrabi M.R., Jamshidi S., Farhangi A., Verdi A.A., Mofidian S.M.A., Rad
B.L. Indian Journal of Clinical Biochemistry, 2007, 22(2), 60-64
[11] Wimhurst J.M., Manchester K.L. Biochem. J., 1970, 120, 95-103
[12] Adikwu M.U., Yoshikawa Y., Takada K. Biological and Pharmaceutical Bulletin, 2003, 26(5), 662-666.
609
Pelagia Research Library
Das könnte Ihnen auch gefallen
- Diabetes Research PaperDokument7 SeitenDiabetes Research PaperLysol007100% (3)
- Quiz #3 - Locus of Prac, System Levels in SW, Types of Orgs.Dokument10 SeitenQuiz #3 - Locus of Prac, System Levels in SW, Types of Orgs.Hannah Christine FuertesNoch keine Bewertungen
- (Rickie Solinger) Reproductive Politics What EverDokument236 Seiten(Rickie Solinger) Reproductive Politics What EverhercuNoch keine Bewertungen
- Managing and Caring For The SelfDokument17 SeitenManaging and Caring For The SelfYen Yen100% (1)
- Advances and Challenges in Stroke RehabilitationDokument13 SeitenAdvances and Challenges in Stroke Rehabilitationarif 2006Noch keine Bewertungen
- Rat Nayak e 1995Dokument5 SeitenRat Nayak e 1995Muhammad RizkyNoch keine Bewertungen
- Antidiabetec Analysis - KumarDokument8 SeitenAntidiabetec Analysis - KumarArya NugrahaNoch keine Bewertungen
- Antidiabetic of Medicinal PlantsDokument8 SeitenAntidiabetic of Medicinal PlantsVinh Nguyen QuangNoch keine Bewertungen
- X. MDokument18 SeitenX. MDanang RaharjoNoch keine Bewertungen
- Evaluation of Anti Inflammatory Activity of Synthetic 7flavanol DerivativesDokument3 SeitenEvaluation of Anti Inflammatory Activity of Synthetic 7flavanol DerivativesgejaNoch keine Bewertungen
- 3 Ijmpsaug20183Dokument8 Seiten3 Ijmpsaug20183TJPRC PublicationsNoch keine Bewertungen
- Jurnal Fartoks KunyitDokument11 SeitenJurnal Fartoks Kunyitrambutan0408Noch keine Bewertungen
- Ijsid: International Journal of Science Innovations and DiscoveriesDokument9 SeitenIjsid: International Journal of Science Innovations and DiscoveriesijsidonlineinfoNoch keine Bewertungen
- Assessment of Antidiabetic Effect of 4-HIL in Type 2 Diabetic and Healthy Sprague Dawley RatsDokument11 SeitenAssessment of Antidiabetic Effect of 4-HIL in Type 2 Diabetic and Healthy Sprague Dawley RatsMaxin BangsalNoch keine Bewertungen
- Anti Diabetic Activity of Traditional Herbal FormulationDokument9 SeitenAnti Diabetic Activity of Traditional Herbal FormulationFina Herlinda NurNoch keine Bewertungen
- International Journal of Research in Biological Sciences: ISSN 2249 - 9687 Original ArticleDokument5 SeitenInternational Journal of Research in Biological Sciences: ISSN 2249 - 9687 Original ArticleKannadhasan DassNoch keine Bewertungen
- Study of Antidiabetic Activity of Hiptage Benghalensis (L) KurzDokument8 SeitenStudy of Antidiabetic Activity of Hiptage Benghalensis (L) KurzIOSR Journal of PharmacyNoch keine Bewertungen
- Jurnal Amlodipin UdtDokument7 SeitenJurnal Amlodipin UdtdidiisafitriNoch keine Bewertungen
- Pomegranate Juice HealingDokument23 SeitenPomegranate Juice HealingKingNoch keine Bewertungen
- Anti Diabetic Effect of BrahmiDokument8 SeitenAnti Diabetic Effect of BrahmiNilanjan RayNoch keine Bewertungen
- Hypoglycaemic Activity of The Ethanol Extract of A PDFDokument5 SeitenHypoglycaemic Activity of The Ethanol Extract of A PDFitayesung89Noch keine Bewertungen
- Determination of Erythromycin Spiramycin TilmicosiDokument7 SeitenDetermination of Erythromycin Spiramycin TilmicosiJuan Pablo EspinosaNoch keine Bewertungen
- Exercise 6 - Proposed Tables For Every ObjectivesDokument5 SeitenExercise 6 - Proposed Tables For Every ObjectivesNOREEN MITZI LOPEZNoch keine Bewertungen
- The Open Natural Products Journal, 2009, 2, 68-70Dokument3 SeitenThe Open Natural Products Journal, 2009, 2, 68-70Valentina AnutaNoch keine Bewertungen
- Evaluation of The Antidiabetic Activity of Asphodelus Tenuifolius in Normal and Alloxan-Induced Diabetic RatsDokument18 SeitenEvaluation of The Antidiabetic Activity of Asphodelus Tenuifolius in Normal and Alloxan-Induced Diabetic RatsCurrents in Pharmaceutical Research (CPR)Noch keine Bewertungen
- Drug Interaction HT and DMDokument6 SeitenDrug Interaction HT and DMAfief Izuddin MhsNoch keine Bewertungen
- 05no4 3Dokument12 Seiten05no4 3محمدأميندماجNoch keine Bewertungen
- Journal of Ayurveda and Integrative Medicine: Original Research Article (Experimental)Dokument6 SeitenJournal of Ayurveda and Integrative Medicine: Original Research Article (Experimental)Said abdul jalil GassppooeellNoch keine Bewertungen
- Academic Sciences: Asian Journal of Pharmaceutical and Clinical ResearchDokument7 SeitenAcademic Sciences: Asian Journal of Pharmaceutical and Clinical Researchrr48843Noch keine Bewertungen
- Jurnal Ekstrak MethanolicDokument6 SeitenJurnal Ekstrak MethanolicMoses FernandoNoch keine Bewertungen
- Antidiabetic Activity of Partitionates of Aegle Marmelos Linn. (Rutaceae) Leaves Ethanolic Extracts in Normal and Alloxan Induced Diabetic RatsDokument7 SeitenAntidiabetic Activity of Partitionates of Aegle Marmelos Linn. (Rutaceae) Leaves Ethanolic Extracts in Normal and Alloxan Induced Diabetic RatsIOSR Journal of PharmacyNoch keine Bewertungen
- Hypoglycemic Effect of Oral Administration of The Infusion of Leptocarpha Rivularis in Alloxan Induced Diabetic RatsDokument14 SeitenHypoglycemic Effect of Oral Administration of The Infusion of Leptocarpha Rivularis in Alloxan Induced Diabetic RatsFernando LópezNoch keine Bewertungen
- Hypoglycemic Potential of Alcoholic Root Extract of Cassia Occidentalis Linn. in Streptozotocin Induced Diabetes in Albino MiceDokument7 SeitenHypoglycemic Potential of Alcoholic Root Extract of Cassia Occidentalis Linn. in Streptozotocin Induced Diabetes in Albino MiceGeorgianaRamonaNoch keine Bewertungen
- 9873 27543 1 PBDokument5 Seiten9873 27543 1 PBManjubashini Leo SelvarajahNoch keine Bewertungen
- International Journal of Medical Research & Health SciencesDokument8 SeitenInternational Journal of Medical Research & Health ScienceseditorijmrhsNoch keine Bewertungen
- Artículo Tolbutamida RatasDokument4 SeitenArtículo Tolbutamida RatasErnesto RamírezNoch keine Bewertungen
- Comparative Hypoglycemic Effects of Different Extract of Clitoria Ternatea Leaves On RatsDokument6 SeitenComparative Hypoglycemic Effects of Different Extract of Clitoria Ternatea Leaves On RatsIOSRjournalNoch keine Bewertungen
- Hypoglycemic Activity of Erythrina Variegata Leaf in Streptozotocin Induced Diabetic RatsDokument7 SeitenHypoglycemic Activity of Erythrina Variegata Leaf in Streptozotocin Induced Diabetic RatshalimahNoch keine Bewertungen
- The Antidiabetic Effect of Low Doses of Moringa Oleifera Seeds On Streptozotocin Induced Diabetes and Diabetic Nephropathy in Male RatsDokument13 SeitenThe Antidiabetic Effect of Low Doses of Moringa Oleifera Seeds On Streptozotocin Induced Diabetes and Diabetic Nephropathy in Male RatsAnonymous 5rM5XsRjTeNoch keine Bewertungen
- Diabetes MoringaDokument14 SeitenDiabetes MoringaMichell SantamariaNoch keine Bewertungen
- A Comparative Pharmacokinetic Analysis of Oral andDokument9 SeitenA Comparative Pharmacokinetic Analysis of Oral andcandyNoch keine Bewertungen
- Sawi LangitDokument8 SeitenSawi Langitninin latwolatwoNoch keine Bewertungen
- Cns BaDokument7 SeitenCns BakumudhaveniNoch keine Bewertungen
- Antidiabetic and Antihyperlipidemic Effect of Alstonia Scholaris Linn Bark in Streptozotocin Induced Diabetic RatsDokument7 SeitenAntidiabetic and Antihyperlipidemic Effect of Alstonia Scholaris Linn Bark in Streptozotocin Induced Diabetic RatsShaik ShoaibNoch keine Bewertungen
- BMC Complementary and Alternative Medicine: Antiinflammatory Evaluation of Leaves of Plumeria AcuminataDokument6 SeitenBMC Complementary and Alternative Medicine: Antiinflammatory Evaluation of Leaves of Plumeria AcuminatadianapriyaniNoch keine Bewertungen
- Antidiarrhoeal Activity of Leaf Extract of Moringa Oleifera in Experimentally Induced Diarrhoea in RatsDokument7 SeitenAntidiarrhoeal Activity of Leaf Extract of Moringa Oleifera in Experimentally Induced Diarrhoea in Ratsjane kangNoch keine Bewertungen
- Effect of Spinosad and Imidacloprid On Serum Biochemical Alterations in PDFDokument7 SeitenEffect of Spinosad and Imidacloprid On Serum Biochemical Alterations in PDFMekala LakshmanNoch keine Bewertungen
- Ravikanth3 PDFDokument7 SeitenRavikanth3 PDFMekala LakshmanNoch keine Bewertungen
- Jurnal T 5Dokument4 SeitenJurnal T 5Komang SuartikaNoch keine Bewertungen
- Ms JPRI 62804Dokument13 SeitenMs JPRI 62804melendezjmanuelNoch keine Bewertungen
- Efficacy of Aqueous Leaf Extract of Vernonia Amygdalina On Plasma Lipoprotein and Oxidative Status in Diabetic Rat Models. H. U. NwanjoDokument4 SeitenEfficacy of Aqueous Leaf Extract of Vernonia Amygdalina On Plasma Lipoprotein and Oxidative Status in Diabetic Rat Models. H. U. NwanjoNgan HoangNoch keine Bewertungen
- Morinda Citrifolia: Research ArticleDokument5 SeitenMorinda Citrifolia: Research ArticleMayara MeloNoch keine Bewertungen
- Anti-Diabetic Activity Evaluation of The Bark of Cascabela Thevetia L. in Streptozotocin Induced Diabetic RatsDokument6 SeitenAnti-Diabetic Activity Evaluation of The Bark of Cascabela Thevetia L. in Streptozotocin Induced Diabetic RatsNeelutpal16Noch keine Bewertungen
- Original Research Article: Evaluation of The Toxicological Profile of YagariDokument30 SeitenOriginal Research Article: Evaluation of The Toxicological Profile of YagariHanif Amrulloh ZANoch keine Bewertungen
- Melinjo JournalDokument10 SeitenMelinjo JournalStephanie NangoiNoch keine Bewertungen
- 1472 6882 2 1 PDFDokument7 Seiten1472 6882 2 1 PDFThiago NunesNoch keine Bewertungen
- Anti Diabetic Activity of Ethanol Extract of Colocasia Esculenta Leaves in Alloxan Induced Diabetic RatsDokument4 SeitenAnti Diabetic Activity of Ethanol Extract of Colocasia Esculenta Leaves in Alloxan Induced Diabetic RatsyigalbyNoch keine Bewertungen
- The Effect of Aloin in Blood Glucose and Antioxidants in Male Albino Rats With Streptozotocin-Induced DiabeticDokument18 SeitenThe Effect of Aloin in Blood Glucose and Antioxidants in Male Albino Rats With Streptozotocin-Induced DiabeticJunaid MinhasNoch keine Bewertungen
- A 90-Day Subchronic Toxicity Study of Neem Oil, A Azadirachta Indica Oil, in MiceDokument11 SeitenA 90-Day Subchronic Toxicity Study of Neem Oil, A Azadirachta Indica Oil, in Micehenry72Noch keine Bewertungen
- International Journal of Pharmaceutical Sciences and Drug Research 2016 8 (5) : 275-280Dokument6 SeitenInternational Journal of Pharmaceutical Sciences and Drug Research 2016 8 (5) : 275-280Deepak ManogaranNoch keine Bewertungen
- Diabetes PDFDokument12 SeitenDiabetes PDFDANIELA MALAGÓN MONTAÑONoch keine Bewertungen
- Mahe 11Dokument8 SeitenMahe 11mahemez100% (1)
- SCREENING OF Myristica Fragrans (ARILLUS) POWDER FOR EFFECT ON LIPID LEVELS OF RABBITSDokument6 SeitenSCREENING OF Myristica Fragrans (ARILLUS) POWDER FOR EFFECT ON LIPID LEVELS OF RABBITSxiuhtlaltzinNoch keine Bewertungen
- Bioequivalence Study of Two Formulations of Bisoprolol Fumarate Tablets in Healthy SubjectsDokument7 SeitenBioequivalence Study of Two Formulations of Bisoprolol Fumarate Tablets in Healthy SubjectsSan-Clin-Eq LaboratoryNoch keine Bewertungen
- The Cleveland Clinic Manual of Dynamic Endocrine TestingVon EverandThe Cleveland Clinic Manual of Dynamic Endocrine TestingNoch keine Bewertungen
- Abdelrahman 2016Dokument12 SeitenAbdelrahman 2016Anantha LakshmiNoch keine Bewertungen
- Biocatalysis, DNA - Protein Interactions, Cytotoxicity and Molecular Docking of Cu (II), Ni (II), ZN (II) and V (IV) Schiff Base ComplexesDokument16 SeitenBiocatalysis, DNA - Protein Interactions, Cytotoxicity and Molecular Docking of Cu (II), Ni (II), ZN (II) and V (IV) Schiff Base ComplexesAnantha LakshmiNoch keine Bewertungen
- PrBlue Review CCR 2002 PDFDokument16 SeitenPrBlue Review CCR 2002 PDFAnantha LakshmiNoch keine Bewertungen
- Paper 3Dokument14 SeitenPaper 3Anantha LakshmiNoch keine Bewertungen
- DNA-binding Studies of AV-153, An Antimutagenic and DNA Repair-Stimulating Derivative of 1,4-DihydropiridineDokument9 SeitenDNA-binding Studies of AV-153, An Antimutagenic and DNA Repair-Stimulating Derivative of 1,4-DihydropiridineAnantha LakshmiNoch keine Bewertungen
- 6.ethiopia NBHQO Nov 2008Dokument6 Seiten6.ethiopia NBHQO Nov 2008Anantha LakshmiNoch keine Bewertungen
- Journal of Photochemistry & Photobiology A: Chemistry: SciencedirectDokument12 SeitenJournal of Photochemistry & Photobiology A: Chemistry: SciencedirectAnantha LakshmiNoch keine Bewertungen
- Sathish2007 TiO2 PDFDokument6 SeitenSathish2007 TiO2 PDFAnantha LakshmiNoch keine Bewertungen
- Synthesis and Spectral Studies of Transition Metal Complexes Supported Bynobidentate Schiffbase Ligand PDFDokument6 SeitenSynthesis and Spectral Studies of Transition Metal Complexes Supported Bynobidentate Schiffbase Ligand PDFAnantha LakshmiNoch keine Bewertungen
- 1 s2.0 S1319610317301072 MainDokument11 Seiten1 s2.0 S1319610317301072 MainAnantha LakshmiNoch keine Bewertungen
- Sulfur-Doped Nickel Oxide Thin Film As An Alternative To PT For Dye-Sensitized Solar Cell Counter ElectrodesDokument5 SeitenSulfur-Doped Nickel Oxide Thin Film As An Alternative To PT For Dye-Sensitized Solar Cell Counter ElectrodesAnantha LakshmiNoch keine Bewertungen
- Pelagia Research Library: Available Online atDokument6 SeitenPelagia Research Library: Available Online atAnantha LakshmiNoch keine Bewertungen
- Three-Dimensional Porous Nitrogen-Doped Nio Nanostructures As Highly Sensitive No SensorsDokument9 SeitenThree-Dimensional Porous Nitrogen-Doped Nio Nanostructures As Highly Sensitive No SensorsAnantha LakshmiNoch keine Bewertungen
- A Critical Review On Traditional Herbal Drugs: An Emerging Alternative Drug For DiabetesDokument22 SeitenA Critical Review On Traditional Herbal Drugs: An Emerging Alternative Drug For DiabetesAnantha LakshmiNoch keine Bewertungen
- DNA Drug Interaction: Saher Afshan Shaikh and B. JayaramDokument8 SeitenDNA Drug Interaction: Saher Afshan Shaikh and B. JayaramAnantha LakshmiNoch keine Bewertungen
- Inorganic Chemistry Communications: Short CommunicationDokument6 SeitenInorganic Chemistry Communications: Short CommunicationAnantha LakshmiNoch keine Bewertungen
- Whiteboard Software and Electronic Pen Function/Button Operation ChartDokument1 SeiteWhiteboard Software and Electronic Pen Function/Button Operation ChartAnantha LakshmiNoch keine Bewertungen
- DNA Complexes With Cobalt (II) Phthalocyanine Disodium DisulfonateDokument8 SeitenDNA Complexes With Cobalt (II) Phthalocyanine Disodium DisulfonateAnantha LakshmiNoch keine Bewertungen
- Vanadyl-Biguanide Complexes As Potential Synergistic Insulin MimicsDokument7 SeitenVanadyl-Biguanide Complexes As Potential Synergistic Insulin MimicsAnantha LakshmiNoch keine Bewertungen
- M.Sc. Chemistry Inorganic Chemistry Specialisation Syllabus of Iii & Iv SemestersDokument23 SeitenM.Sc. Chemistry Inorganic Chemistry Specialisation Syllabus of Iii & Iv SemestersAnantha LakshmiNoch keine Bewertungen
- Character Tables: Christopher C. CumminsDokument101 SeitenCharacter Tables: Christopher C. CumminsMohammad RameezNoch keine Bewertungen
- Novel Spectroscopic Tools To Differentiate Drug-DNA Binding InterDokument131 SeitenNovel Spectroscopic Tools To Differentiate Drug-DNA Binding InterAnantha LakshmiNoch keine Bewertungen
- Spectroscopic and Viscositic Studies On The Interaction of Solifenacin Succinate With DnaDokument5 SeitenSpectroscopic and Viscositic Studies On The Interaction of Solifenacin Succinate With DnaAnantha LakshmiNoch keine Bewertungen
- An Overview of Analytical TechniquesDokument27 SeitenAn Overview of Analytical TechniquesAnantha LakshmiNoch keine Bewertungen
- Sathish2007 TiO2 PDFDokument6 SeitenSathish2007 TiO2 PDFAnantha LakshmiNoch keine Bewertungen
- Sulfur-Doped Nickel Oxide Thin Film As An Alternative To PT For Dye-Sensitized Solar Cell Counter ElectrodesDokument5 SeitenSulfur-Doped Nickel Oxide Thin Film As An Alternative To PT For Dye-Sensitized Solar Cell Counter ElectrodesAnantha LakshmiNoch keine Bewertungen
- New Designs For Phototherapeutic Transition Metal ComplexesDokument13 SeitenNew Designs For Phototherapeutic Transition Metal ComplexesAnantha LakshmiNoch keine Bewertungen
- Saha2006 PDFDokument10 SeitenSaha2006 PDFAnantha LakshmiNoch keine Bewertungen
- Three-Dimensional Porous Nitrogen-Doped Nio Nanostructures As Highly Sensitive No SensorsDokument9 SeitenThree-Dimensional Porous Nitrogen-Doped Nio Nanostructures As Highly Sensitive No SensorsAnantha LakshmiNoch keine Bewertungen
- Risk Assessment: Workers Operating in Loading/unloading (Shipping/receiving) AreasDokument12 SeitenRisk Assessment: Workers Operating in Loading/unloading (Shipping/receiving) AreasenharNoch keine Bewertungen
- The Philosophy and Science of Caring Jean Watson: St. Luke'S College of Nursing Trinity University of AsiaDokument28 SeitenThe Philosophy and Science of Caring Jean Watson: St. Luke'S College of Nursing Trinity University of Asiaojay_88Noch keine Bewertungen
- Holistic Approach To Mental HealthDokument38 SeitenHolistic Approach To Mental HealthabhishekNoch keine Bewertungen
- Nevid CH14 TBDokument71 SeitenNevid CH14 TBAngela MarisNoch keine Bewertungen
- SDS - Whisper V - Id - enDokument10 SeitenSDS - Whisper V - Id - enAmirza PrabowoNoch keine Bewertungen
- Level of Knowledge and Attitude Among Nursing Students Toward Patient Safety and Medical ErrorsDokument125 SeitenLevel of Knowledge and Attitude Among Nursing Students Toward Patient Safety and Medical ErrorshanadiNoch keine Bewertungen
- Polymer Content of AMS (α-Methylstyrene) : Standard Test Methods forDokument3 SeitenPolymer Content of AMS (α-Methylstyrene) : Standard Test Methods forasmaNoch keine Bewertungen
- School-Based Occupational Therapy: January 2020Dokument33 SeitenSchool-Based Occupational Therapy: January 2020purplemeraldNoch keine Bewertungen
- Intervention Approaches Table 8 - 3 Edition: Create, PromoteDokument1 SeiteIntervention Approaches Table 8 - 3 Edition: Create, PromoteJM RMNoch keine Bewertungen
- General Science and AbilityDokument4 SeitenGeneral Science and AbilityUsra RasoolNoch keine Bewertungen
- Medical ReportDokument1 SeiteMedical ReportamrulNoch keine Bewertungen
- Lesson PlanDokument16 SeitenLesson PlanMELIE BAGARESNoch keine Bewertungen
- Effectively Planning For and Managing Major Disasters: John C. CavanaughDokument21 SeitenEffectively Planning For and Managing Major Disasters: John C. CavanaughMichael AquinoNoch keine Bewertungen
- Ez Mul NT MSDSDokument11 SeitenEz Mul NT MSDSyfcozNoch keine Bewertungen
- PHYSICIANS Room Assignment 03-2021Dokument13 SeitenPHYSICIANS Room Assignment 03-2021PRC BaguioNoch keine Bewertungen
- International Journal of Dental Science and Innovative Research (IJDSIR)Dokument7 SeitenInternational Journal of Dental Science and Innovative Research (IJDSIR)yusfaNoch keine Bewertungen
- Critical Essay Final Draft 1 Personal ResponseDokument5 SeitenCritical Essay Final Draft 1 Personal Responsemyron kipropNoch keine Bewertungen
- Microbiology CatalogueDokument40 SeitenMicrobiology CatalogueHari YantoNoch keine Bewertungen
- From Idea To MarketDokument6 SeitenFrom Idea To MarketvictorccNoch keine Bewertungen
- Blepharitis Lid Hygiene Advice For PatientsDokument3 SeitenBlepharitis Lid Hygiene Advice For PatientsTaniaNoch keine Bewertungen
- Clinical Epidemiology SGD 1Dokument6 SeitenClinical Epidemiology SGD 1Beatrice Del RosarioNoch keine Bewertungen
- Data Mppds Yang Menangani Pasien Covid-19 Rsup Dr. Wahidin Sudirohusodo MakassarDokument25 SeitenData Mppds Yang Menangani Pasien Covid-19 Rsup Dr. Wahidin Sudirohusodo MakassarmuhammadNoch keine Bewertungen
- Obsessive-Compulsive and Related Disorders DSM - V Ocd and Related DisordersDokument2 SeitenObsessive-Compulsive and Related Disorders DSM - V Ocd and Related DisordersJaaaaaaaaNoch keine Bewertungen
- Pages From ASME - PCC-2-2008 - Stored Energy CalDokument3 SeitenPages From ASME - PCC-2-2008 - Stored Energy CalRafeeq Ur Rahman0% (1)
- Diabetes in The Philippines, and How To Prevent It Infographic 2Dokument1 SeiteDiabetes in The Philippines, and How To Prevent It Infographic 2Orlando PalomponNoch keine Bewertungen