Beruflich Dokumente
Kultur Dokumente
CLEAR III Read
Hochgeladen von
sjulurisOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
CLEAR III Read
Hochgeladen von
sjulurisCopyright:
Verfügbare Formate
Research
A multicenter, randomized, double-blinded, placebo-controlled phase III study of
Clot Lysis Evaluation of Accelerated Resolution of Intraventricular Hemorrhage
(CLEAR III)
Wendy C. Ziai1*, Stanley Tuhrim2, Karen Lane3, Nichol McBee3, Kennedy Lees4,
Jesse Dawson4, Kenneth Butcher5, Paul Vespa6, David W. Wright7, Penelope M. Keyl3,
A. David Mendelow8, Carlos Kase9, Christine Wijman10, Marc Lapointe11, Sayona John12,
Richard Thompson13, Carol Thompson13, Steven Mayo14, Pat Reilly15, Scott Janis16,
Issam Awad17, and Daniel F. Hanley3 for the CLEAR III Investigators
Correspondence: Wendy C. Ziai*, Department of Neurology, The Johns Background In adults, intraventricular thrombolytic therapy
Hopkins Hospital, 600 Wolf Street, Baltimore, MD 21231, USA. with recombinant tissue plasminogen activator (rtPA) facili-
E-mail: weziai@jhmi.edu tates resolution of intraventricular haemorrhage (IVH),
1
Division of Neurosciences Critical Care, Department of Neurology, reduces intracranial pressure, decreases duration of cerebro-
Johns Hopkins Hospital, Johns Hopkins University School of Medicine, spinal fluid diversion, and may ameliorate direct neural injury.
Baltimore, MD, USA We hypothesize that patients with small parenchymal haema-
2
Department of Neurology, Mount Sinai School of Medicine, New York, toma volumes (<30 cc) and relatively large IVH causing acute
NY, USA obstructive hydrocephalus would have improved clinical out-
3
Division of Brain Injury Outcomes, Johns Hopkins University School of comes when given injections of low-dose rtPA to accelerate
Medicine, Baltimore, MD, USA lysis and evacuation of IVH compared with placebo.
4
Institute of Cardiovascular and Medical Sciences, University of Glasgow, Methods The Clot Lysis Evaluation of Accelerated Resolution
Glasgow, Scotland, UK of Intraventricular Hemorrhage III trial is an investigator-
5
Division of Neurology, University of Alberta, Edmonton, AB, Canada initiated, phase III, randomized, multicenter, double-blind,
6
Department of Neurosurgery, University of California, Los Angeles, CA, placebo-controlled study comparing the use of external ven-
USA tricular drainage (EVD) combined with intraventricular injec-
7
Department of Emergency Neurosciences, Grady Memorial Hospital, tion of rtPA to EVD plus intraventricular injection of normal
Emory University School of Medicine, Atlanta, GA, USA saline (placebo) for the treatment of IVH. Patients with known
8
Department of Neurosurgery, Newscastle General Hospital, Newscastle symptom onset within 24 h of the computed tomography scan
upon Tyne, UK confirmed IVH and third or fourth ventricle obstruction, with
9
Department of Neurology, Boston Medical Center, Boston, MA, USA or without supratentorial intracerebral haemorrhage volume
10
Department of Neurology and Neurological Sciences, Stanford Medi- <30 cc, who require EVD are screened with a computed tomog-
cine, Stanford, CA, USA raphy scan at least six hours after EVD placement and, if
11
College of Pharmacy, Medical University of South Carolina, Charleston, necessary, at consecutive 12-h intervals until stabilization of
SC, USA any intracranial bleeding has been established. Patients who
12
Department of Neurology, Rush University Medical Center, Chicago, IL, meet clinical and imaging criteria (no ongoing coagulopathy
USA and no suspicion of aneurysm, arteriovenous malformation, or
13
The Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, any other vascular anomaly) will be randomized to either
USA intraventricular rtPA or placebo.
14
Emissary International, LLC, Austin, TX, USA Results The primary outcome measure is dichotomized modi-
15
Genentech, Inc., San Francisco, CA, USA fied Rankin Scale 0–3 vs. 4–6 at 180 days. Clinical secondary
16
National Institute of Neurological Disorders and Stroke, National Insti- outcomes include additional modified Rankin Scale dichotomi-
tutes of Health, Bethesda, MD, USA zations at 180 days (0–4 vs. 5–6), ordinal modified Rankin Scale
17
Section of Neurosurgery and the Neurovascular Surgery Program, Uni- (0–6), mortality and safety events at 30 days, mortality at 180
versity of Chicago Pritzker School of medicine, Chicago, IL, USA days, functional status measures, type and intensity of inten-
sive care unit management, rate and extent of ventricular
Conflicts of interest: No party having a direct interest in the results of the
blood clot removal, and quality of life measures.
research supporting this article has or will confer a benefit on us or on any
Key words: intracerebral haemorrhage, protocols, randomized clinical
organization with which we are associated. We certify that all financial and
trial, stroke, thrombolysis
material support for this research has been clearly identified in the
Funding section. Pat Reilly is an employee of Genentech, Inc.
Funding: The CLEAR III trial is supported by a grant (NIH/NINDS 5U01 Introduction
NS062851 to Dr Hanley). Drs Wendy Ziai and Stanley Tuhrim, Karen
Lane, Nichol McBee, Drs Issam Awad, Kennedy Lees, Jesse Dawson, Intraventricular haemorrhage (IVH) occurs in about 40% of
Kenneth Butcher, Paul Vespa, Penelope Keyl, A. David Mendelow, Carlos
Kase, Christine Wijman, Marc Lapointe, Sayona John, Richard Thomp-
primary intracerebral haemorrhage (ICH) and 15% of aneurys-
son, Carol Thompson, and Steven Mayo receive funding from the same mal sub-arachnoid haemorrhage patients (1–3). IVH is a signifi-
grant (NIH/NINDS 5U01 NS062851 to Dr Daniel F. Hanley). Dr Hanley cant and independent contributor to morbidity, and 30-day
is also supported by grants RO1NS046309 from the NIH/NINDS, grant mortality is estimated at 40–80% (4,5). Recently, two large ran-
272–2007 from the Eleanor Naylor Dana Charitable Trust, the Jeffry and domized controlled trials (RCTs) demonstrated the importance
Harriet Legum Endowment, and materials grants from Genentech, Inc.
of IVH as a predictor of poor outcome. The Surgical Trial in
DOI: 10.1111/ijs.12097 ICH (STICH) enrolled 964 ICH patients, 42% of whom had
© 2013 The Authors. Vol ••, •• 2013, ••–•• 1
International Journal of Stroke © 2013 World Stroke Organization
Research W. C. Ziai et al.
intraventricular extension; of these, over half (55%) had obstruc- the greater the volume of blood clot injected into the ventricles
tive hydrocephalus (6). IVH with or without hydrocephalus was the greater the likelihood of animal death.
strongly associated with poor outcome; 31% without IVH and Observational clinical studies and one small randomized trial
15% with IVH experienced good outcome (P < 0·00001) (7). have demonstrated improved clot resolution, ICP, ventricular
When IVH and hydrocephalus were combined, good outcome size, and mortality with both intraventricular rtPA (off-label use)
rates fell to 11%. Similarly, IVH occurred in 49% of all patients and urokinase (not currently available in the United States) (21–
enrolled in the NovoSeven ICH trial (n = 399). Modified Rankin 33). A Cochrane review of 10 independent studies (eight case
scores at 3 months were consistently worse in this group of series or retrospective studies, one quasi-randomized study, and
patients (8). A prospective study of ICH patients indicates a one randomized study with a biased control group) using intra-
direct, continuous relationship between the volume of IVH and ventricular thrombolytic agents found anecdotal evidence sup-
mortality (9). porting safety and possible therapeutic value (34). A more recent
IVH contributes to morbidity by causing acute obstructive meta-analysis of 4 randomized and 10 observational studies
hydrocephalus, which elevates intracranial pressure (ICP) and found that intraventricular fibrinolysis was superior to EVD
decreases cerebral perfusion pressure, and, if severe enough, results alone in terms of survival and short-term functional outcome
in brain herniation. The current therapy for IVH with obstructive (35). Thus far, there are no randomized trials of sufficient size
hydrocephalus is an external ventricular drainage (EVD). EVD and quality to evaluate the safety and efficacy of this treatment
alone is often an inadequate therapy and is complicated by catheter modality.
occlusion with blood clots (10). EVD does not alter the rate of The Intraventricular Hemorrhage Thrombolysis trial was a
blood clot resolution (11) and therefore fails to decrease the degree phase II, double-blind, randomized study that evaluated rtPA for
and incidence of communicating hydrocephalus. clot lysis rate and safety. Forty-eight patients were randomized
EVD lowers ICP, but controlling ICP does not usually result in 1:1 to receive intraventricular injections of either 3·0 mg of rtPA
immediate mental status improvement (12). Thus, direct mass (n = 26) or placebo (normal saline, n = 22) every 12 h until com-
effect of IVH may be a significant pathophysiologic factor inde- plete IVH resolution, EVD removal, or a safety end-point, which-
pendent of ICP elevation. Persistent IVH is also associated with ever came first (36). Frequency of death and ventriculitis was
both mortality (12,13) and decreased level of consciousness lower than expected, and bleeding events remained below the
(14,15), which for poorly understood reasons, EVD does not con- prespecified threshold: mortality (18% rtPA; 23% placebo), ven-
sistently improve. Indeed, EVD may worsen edema and inflam- triculitis (8% rtPA; 9% placebo), and symptomatic bleeding
mation when complicated by bacterial meningitis. Other possible (23% rtPA; 5% placebo; P = 0·1). The median duration of dosing
explanations include pro-inflammatory effects of the blood com- was 7·5 days for rtPA and 12 days for placebo. There was a sig-
ponents (16) and permanent occlusion and scarring of arachnoid nificant beneficial effect of rtPA on the rate of clot resolution
granulations where CSF is absorbed (17,18). The latter results in (P < 0·001).
delayed communicating hydrocephalus, which necessitates per- Dose interval finding studies [Clot Lysis Evaluation of Acceler-
manent CSF shunt placement and is associated with impaired ated Resolution of Intraventricular Hemorrhage (CLEAR) A and
cognition, gait, balance, and urinary continence. B] randomized patients 1:1 to receive intraventricular rtPA
The natural history of IVH is for radiographically observed either at doses 0·3 or 1·0 mg q12h (n = 16) (CLEAR A) or to
blood to gradually disappear over a period of two to four weeks, receive 1·0 mg q12h or q8h (n = 36) (CLEAR B). Direct measure-
although remnants of IVH may persist for many months. Intra- ment of the initial clot lysis rate (first three days of treatment)
ventricular thrombolysis facilitates blood clot removal and, in demonstrated dose-specific rates of 21·73%/day, 25·14%/day,
experimental studies, ameliorates prolonged inflammation and 24·20%/day, and 19·98%/day for the 3·0 mg, 1·0 mg (q12h),
protects against delayed hydrocephalus (14,19). In a canine IVH 0·3 mg, and 1·0 mg (q8hr) groups, respectively. The safety profile
model 20 000 IU of urokinase, administered every 12 h through for the two lower doses was numerically superior to the 3·0 mg
an EVD until evidence of clot resolution, resulted in more rapid dose with a symptomatic haemorrhage rate of 5·8% (3/52
clearance of intraventricular blood (3–6 days vs. 38–65 days), patients).
more rapid return of consciousness (3 days vs. 7–9 days), lower Intraventricular thrombolysis is a rational therapy, with some
incidence of delayed communicating hydrocephalus, and data supporting its safety. At this point, however, there is insuffi-
improved neurological outcome without increased injury to sur- cient evidence to recommend routine use in clinical practice. We
rounding brain tissue (14,19) compared with control animals. have therefore designed a randomized controlled trial to test the
There were no intracranial or systemic haemorrhages, and no hypothesis that intraventricular thrombolysis improves clinical
chronic changes in the brain or meninges on histology at three outcomes in IVH patients.
months in the treated group. In a pig model, Mayfrank et al.
showed that the mass effect of clots distending the ventricle wall is Study objectives
the most important mechanism responsible for haemorrhagic The primary aim of this study is to test the hypothesis that IVH
ventricular dilatation and that this mass effect significantly patients requiring EVD placement, with stabilized clots, will have
diminished at the 1·5 h and seven-day time point when recombi- better clinical outcomes when treated with intraventricular rtPA
nant tissue plasminogen activator (rtPA) was used for intraven- (1 mg q8h, up to 12 doses) relative to those receiving placebo
tricular thrombolysis (20). In both canine and porcine models, within 72 h of onset.
2 Vol ••, •• 2013, ••–•• © 2013 The Authors.
International Journal of Stroke © 2013 World Stroke Organization
W. C. Ziai et al. Research
Methods • Symptom onset less than 24 h prior to diagnostic CT scan
Design • Age 18–80 years
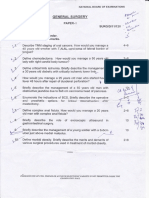
The CLEAR III study is a randomized, multicenter, double- • An EVD must be in place and stable at the time of randomiza-
tion, ideally using no more than two complete passes
blinded, placebo-controlled phase III trial (two arms with 1:1
randomization for the first 104 patients followed by adaptive • Systolic blood pressure <200 mmHg sustained for the six hours
before drug administration (closest to randomization)
randomization) in ICH/IVH patients (Fig. 1). The protocol is
registered with http://clinicaltrials.gov (NCT00784134) and • No test article may be administered until at least 12 h after
symptom onset
approved by each site’s Institutional Review Board.
• Randomization within 72 h of CT scan diagnosing IVH, and
Patient population – inclusion and exclusion criteria • Modified Rankin Score (mRS) before ICH of 0 or 1.
Inclusion criteria Imaging inclusion criteria
• Spontaneous ICH ≤30 cc and IVH obstructing third and/or • ICH/IVH clot stability: ICH must be ≤30 cc on initial presen-
fourth ventricles tation and not exceed 35 cc on subsequent prerandomization
Patient assessment
All IVH
1. Inclusion and exclusion criteria With third or fourth ventricle obstruction
2. Consent EVD placement
3. CT imaging
ICH
unstable or
> 30 cc ICH/IVH stable,
Did not meet inclusion/exclusion or CT
ICH < 30 cc
imaging criteria or consent not obtained
(n = 500)
Ineligible
Randomization
EVD + Placebo EVD + rtPA
(n = 250) (n = 250)
ASA guidelines for ICH management
Days 1 –7
CT scans (Days 1–5, 1, 3 days post last dose),
lab assessments, vital signs, documentation of
procedures
Follow-up
(Months: 1, 3, 6, 9, 12)
Documentation of neurological AE and all SAEs
Functional: NIHSS, mRS, Barthel Index, extended
GOS, Mini-Mental State Exam, Personal Health Utility
Assessment Interview
Quality of Life: Stroke Impact Scale, EQ-5D, PBSI
CT at 1 and 12 months only
Fig. 1 Clot lysis evaluation of accelerated resolution of intraventricular haemorrhage study assessment flow chart. AE, adverse event; ASA, American
Stroke Association; CT, computed tomography; EQ-5D, Euro-QuOL 5-Dimension; EVD, external ventricular drain; GOS, Glasgow outcome scale;
ICH, intracerebral haemorrhage; IVH, intraventricular haemorrhage; mRS, modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale;
PBSI, Preference-Based Stroke Index; rtPA, recombinant tissue plasminogen activator; SAE, severe adverse event.
© 2013 The Authors. Vol ••, •• 2013, ••–•• 3
International Journal of Stroke © 2013 World Stroke Organization
Research W. C. Ziai et al.
stability scans. Stability scan: A CT scan performed six hours or vided by Prelude Dynamics Inc., Austin, TX; study-specific imple-
more after EVD placement must be stable as defined by: (1) ICH mentation design developed by Emissary International LLC,
size difference is ≤5 cc compared with the most recent previous Austin, TX). The Surgical and Reading Centers centrally review
CT scan determined by the (A × B × C)/2 method; (2) the width these scans to confirm eligibility and to measure ICH, IVH, and
of the lateral ventricle most compromised by blood clot must not catheter tract clot volume/stability. All imaging data are electroni-
increase by >2 mm, allowing for movement of blood under influ- cally transferred and read at the Reading Center on a weekly basis
ence of gravity; (3) catheter tract bleeding must be ≤5 cc or mm; to assure quality of CT-based decision making at the recruiting
and (4) third and/or fourth ventricles are occluded with blood. centers. After the last enrolled subject completes the one-year
The investigator may continue to screen up to 72 h for the initial follow-up visit, data monitoring tasks will be completed to final-
bleeding to stabilize, as long as the subject can be randomized ize and lock all clinical and radiological data. The co-ordinating
within 72 h from time of the diagnostic CT scan. If clot sizes center will remain blinded to follow-up clinical information and
stabilize between two sequential CT scans at least 12 h apart, the treatment designation until after data lock occurs.
patient is eligible. Before dosing, the site investigator is required to view the most
recent CT scan, confirming that the catheter tip is within the
Exclusion criteria
ventricular system. A CT scan is required daily on days one
• Suspected (unless ruled out by conventional or CT angiogram through five, and then repeated approximately 24 and 72 h post
or magnetic resonance angiography (MRA)/magnetic resonance
last dose of test article. During dosing, all patients must receive a
imaging (MRI)) or untreated ruptured cerebral aneurysm, rup-
minimum of one scan per day, or at least after every three doses.
tured intracranial arteriovenous malformation (AVM), choroid
The CT scan will be evaluated by the site investigator for clot lysis
plexus malformation, Moyamoya disease or tumor (treatment of
and asymptomatic bleeding (including new onset or expansion of
an existing aneurysm or AVM must have occurred at least three
catheter tract haemorrhage) prior to the next administration of
months before the current onset)
test article. An unscheduled CT scan will be done if the subject
• Clotting disorders (reversing anticoagulation will be permitted improves or worsens by more than two points on the Glasgow
where long-term anticoagulation is not required)
coma scale (GCS) motor score for greater than eight hours.
• Platelet count <100 000, international normalized ratio
(INR) > 1·4 (low platelet counts on admission can normalize Randomization
within 24 h as can an INR normalize to <1·4) Patients are randomized to receive the investigational product
• Pregnancy according to a centralized procedure co-ordinated via the online
• Infratentorial haemorrhage vision-edc system. The randomization system for investigational
• ICH/IVH enlargement that cannot be stabilized in the treat- product is based on computer-generated randomization code
ment time window lists, with stratification for thalamic and nonthalamic ICH loca-
• Ongoing internal bleeding, involving retroperitoneal sites, or tion, and for IVH volume. The first 104 patients are randomized
the gastrointestinal, genitourinary, or respiratory tracts 1:1 to each treatment arm. Subsequently, the adaptive random-
• Multifocal, superficial bleeding observed at multiple vascular ization scheme gives patients a weighted chance of being random-
puncture and access sites (e.g. venous cutdowns, arterial punc- ized to each treatment arm based upon the distribution of IVH
tures) or site of recent surgical intervention size and ICH location of previously enrolled subjects at the time
• Prior enrollment in the study of the enrollment. Patients will be stratified for randomization by
• Any other condition that would pose a significant hazard to the each of the following:
subject if the investigational therapy were initiated • ICH location (thalamic or nonthalamic), and
• Subjects who are not expected to survive to the day 180 visit • IVH volume (≤20, >20–≤50, or >50 ml) measured using plani-
because of comorbidities and/or have a do not resuscitate/do not metric techniques.
intubate (DNR/DNI) status prior to randomization, and
Treatment or intervention
• Planned or simultaneous participation (between screening and A neurosurgeon and neurocritical care physicians or their trained
day 30) in another interventional medical investigation or clinical
designees perform EVD injections under standard sterile tech-
trial.
nique. Either 1·0 mg/1 ml of rtPA or one millilitre of normal
Clinical and imaging assessment saline is administered via the EVD. This is performed via isovolu-
Eligible patients are identified upon diagnosis of IVH and EVD metric injection to ensure clearance of the study drug from the
placement. The INR must remain <1·4 during dosing. Infection is catheter and delivery to the clot. At least five millilitres of CSF is
monitored through daily cultures of CSF drawn from the intra- removed prior to injection of one millilitre of test article, followed
ventricular catheter. by a four millilitres flush of sterile saline into the ventricle. Injec-
CT angiogram or digital subtraction angiogram with evalua- tion is followed by closure of the catheter for one hour and then
tion for ‘spot sign’ (37) is encouraged and considered standard of opening of the EVD for drainage of clot and CSF until the next
care to complete the evaluation for aneurysm, AVM, or other injection every eight hours. The first EVD injection occurs after
malformations. A copy of the diagnostic and stability CT elec- randomization, no sooner than 12 h after symptom onset. Treat-
tronic images is uploaded to the vision-edc (electronic data ment continues for up to 12 doses of test article unless the EVD is
capture) online database prior to randomization (software pro- discontinued, an end-point of clot lysis is reached, or an adverse
4 Vol ••, •• 2013, ••–•• © 2013 The Authors.
International Journal of Stroke © 2013 World Stroke Organization
W. C. Ziai et al. Research
treatment end-point occurs (e.g. symptomatic haemorrhage). • Absolute IVH volume and change in volume of blood at 72 h
Treatment success end-points are (1) both third and fourth ven- • Intensity of critical care management as measured by length of
tricles are open; (2) IVH-related mass effect (dilated or shifted ICU stay, duration of EVD,
ventricle) is resolved; or (3) an estimated 80% resolution of the • Intensity of ICP management, and frequency of critical care
IVH clot has occurred from the time clot stability was established. complications
After the last dose, the EVD is closed for one hour and then • Measures of functional outcome and quality of life:
reopened to drain for 24 h to allow for complete removal of test • mRS, Barthel Index, EQ-5D, and total time at home after ICH
article and free plasmin. The EVD is removed when the patient at months 1, 3, 6, 9, and 12. The mRS will be videotaped, at 1-, 6-,
tolerates 24 h of EVD closure, with no sustained elevation of ICP and 12-month clinic follow-up visits for blinded adjudication by
above 15 mmHg. the Outcomes Center located at the University of Glasgow
If the catheter does not remain patent, saline irrigation may be • Extended Glasgow Outcome Scale, the Stroke Impact Scale, the
performed. Replacement of catheters is guided by neurosurgical National Institutes of Health Stroke Scale (NIHSS), the Mini-
clinical judgment. The Surgical Center located at the University of Mental State Exam, and the Preference-Based Stroke Index at
Chicago reviews all catheter placements and monitors clot month 1, 6, and 12, and
removal assessments, catheter discontinuation protocols, and • The study principal investigator and co-ordinator are trained
evaluates the safety and efficacy of the surgical procedure. None of on all evaluations and may perform the evaluations. The study
these therapies are mandated in the protocol, but all are recorded requires annual/bi-annual certification for NIHSS and mRS,
in the case report form. respectively.
Supportive care includes ICP management with CSF drainage,
Data monitoring body
as well as osmotic therapy, hyperventilation, analgesic sedation,
Safety interim analysis is undertaken when 100, 150, 250, and 400
induced coma, surgical management, and where indicated to
patients have completed six-month assessments. These assess-
control ICP.
ments will be conducted by an independent DSMB appointed by
Investigational medicinal product the National Institute of Neurological Disorders and Stroke
The investigational product Alteplase (rtPA, Genentech, Inc., San (NINDS). Recruitment to the trial will be suspended if a thresh-
Francisco, CA) is supplied as two milligrams lyophilized powder old level is exceeded for the events of death prior to day 30
in glass vials. The dose of rtPA to be administered is 1·0 mg in following symptom onset (40%), symptomatic rebleeding within
one millilitre. Alteplase is reconstituted only with United States 72 h of last dose (25%), and bacterial infection within 72 h of last
Pharmacopoeia-grade sterile water without preservatives for dose (20%) for either treatment group. The DSMB may stop or
injection. The rtPA or normal saline (placebo) is prepared by the recommend modification of the protocol at any point. No formal
study pharmacist at each site and delivered to the intensive care interim analyses for efficacy or futility are planned.
unit (ICU) along with a four-milligram flush (nonbacteriostatic Prior to site activation and as needed, study personnel at each
saline) in a separate packet. enrolling center are trained on the protocol, ICH Good Clinical
Practices, investigator responsibilities, Food and Drug Adminis-
Blinding
tration requirements, surgical protocols, and EDC data entry
The investigational product and placebo appear identical and
screens to acquaint the center personnel with the design and
cannot be distinguished from each other. At the time of subject
methods of the trial, the study organization, treatment monitor-
randomization, the EDC system transmits the treatment assign-
ing, and integrity of data collection. Remote monitoring of source
ment via e-mail or fax to the unblinded site pharmacist and the
documentation for every randomized subject serves to verify the
central pharmacist. This is the only documentation of treatment
accuracy and completeness of data in the vision-edc system, the
assignment and is not viewable in the system by other study
existence of applicable regulatory files, and that the investigator’s
personnel. The unblinded pharmacist prepares the investigational
obligations are being fulfilled. Similar remote quality assurance
product, which is clear and colorless, in the same manner as the
methods are undertaken by the Surgical Center, the Outcomes
placebo. All others involved in the conduct of the study are
Center, the Radiology Reading Center, the medical monitors, and
blinded to treatment allocation. The Data Safety Monitoring
the Safety Endpoint Committee to assure protocol compliance
Board (DSMB) has access to pooled data and grouped by treat-
and data integrity.
ment assignment (A : B).
Sample size
Primary outcomes
From the Safety, CLEAR IVH A, and CLEAR IVH B, studies we
The primary outcome is the proportion of patients with mRS
observed an absolute difference of 15–17% in the probability of
scores of 0–3 at day 180.
better outcomes comparing EVD + rtPA with EVD + placebo
Secondary outcomes with control rates around 25%. To determine a sample size that
• Categorical shift in mRS ordinal (0–6) scale (Cochran–Mantel– adequately powers the study, we performed Monte Carlo simula-
Haenszel analysis) tions. A variety of simulation scenarios were examined to judge
• Proportion of patients with mRS 0–4 vs. 5, 6 in the two treat- the sensitivity of power toward sample size (n = 500, 600, and
ment groups at day 180 700), effect size [odds ratio(OR) = 1·8 to 2·2], control group
• Mortality at day 180 outcome rates (placebo rates of good outcome mRS ≤3 = 20%,
© 2013 The Authors. Vol ••, •• 2013, ••–•• 5
International Journal of Stroke © 2013 World Stroke Organization
Research W. C. Ziai et al.
30%), model choice (correctly specified vs. noncorrectly specified 2 Tuhrim S, Dambrosia JM, Price TR et al. Prediction of intracerebral
model), and site clustering {between site heterogeneity param- hemorrhage survival. Ann Neurol 1988; 24:258–63.
3 Steiner T, Schneider D, Mayer S et al. Dynamics of intraventricular
eterized as a latent effect with standard deviation 0·1 and 0·25 [i.e.
hemorrhage in patients with spontaneous intracerebral hemorrhage:
14%, 36% of log-odds ratio treatment effect = 0·7, (OR = 2·0), risk factors, clinical impact, and effect of hemostatic therapy with
respectively]}. The total projected sample size of 500 participants recombinant activated factor VII. Neurosurgery 2006; 59:767–73.
randomized to receive either intraventricular rtPA or placebo 4 Tuhrim S, Horowitz DR, Sacher M, Godbold JH. Validation and com-
(250 in each group) provides 80% or greater power to detect an parison of models predicting survival following intracerebral hemor-
rhage. Crit Care Med 1995; 23:950–4.
absolute difference of 13% in the proportion of patients with
5 Conway JE, Oshiro EM, Piantadosi S. Ventricular blood is an admis-
mRS 0–≤3 outcome at six months (OR = 1·92, α = 0·05, two- sion ct variable which predicts poor clinical outcome after aneurysmal
tailed comparison). subarachnoid hemorrhage. American association of neurological sur-
geons annual meeting, Philadelphia, Pennsylvania. J Neurosurg 1998;
Statistical analyses 88:398A.
All randomized subjects will be included in randomized con- 6 Mendelow AD, Gregson BA, Fernandes HM et al.; STICH investiga-
trolled trial (RCT) analyses on an intention-to-treat basis. tors. Early surgery versus initial conservative treatment in patients
Missing outcome data will be handled through multiple imputa- with spontaneous supratentorial intracerebral haematomas in the
international surgical trial in intracerebral haemorrhage (stich): a ran-
tion procedures subject to the validity of missing-at-randomness
domised trial. Lancet 2005; 365:387–97.
assumptions. For the primary outcome analysis, the proportions 7 Bhattathiri PS, Gregson B, Prasad KS, Mendelow AD; STICH Investi-
of mRS 0–3 outcomes will be compared between treatment and gators. Intraventricular hemorrhage and hydrocephalus after sponta-
placebo arms, adjusted for ICH location (thalamic and nontha- neous intracerebral hemorrhage: results from the STICH trial. Acta
lamic) and IVH volume, using a binary logistic regression model. Neurochir Suppl 2006; 96:65–8.
8 Steiner T, Diringer MN, Schneider D et al. Dynamics of intra-
Although both adjusted and unadjusted results will be reported,
ventricular hemorrhage in patients with spontaneous intracerebral
adjusted analysis is prespecified as the primary outcome analysis hemorrhage: risk factors, clinical impact, and effect of hemostatic
for this RCT. therapy with recombinant activated factor VII. Neurosurgery 2006;
A secondary analysis of the categorical shift in mRS will be 59:767–73.
undertaken on the full range (0–6) of the mRS using Cochran– 9 Tuhrim S, Horowitz DR, Sacher M, Godbold JH. Volume of ventricu-
lar blood is an important determinant of outcome in supratentorial
Mantel–Haenszel shift test and proportional odds logistic regres-
intracerebral hemorrhage. Crit Care Med 1999; 27:617–21.
sion subject to the validity of shift analysis model assumptions. 10 Carhuapoma JR. Thrombolytic therapy after intraventricular hemor-
Other secondary outcome analyses will be carried out according rhage: do we know enough? J Neurol Sci 2002; 202:1–3.
to standard statistical principles for comparison of parametric or 11 Naff NJ, Williams MA, Rigamonti DR, Keyl PM, Hanley DF. Blood clot
nonparametric distributions as appropriate. resolution in human cerebrospinal fluid: evidence of first-order kinet-
ics. Neurosurgery 2001; 49:614–9; discussion 619–621.
Study organization and funding 12 Adams RE, Diringer MN. Response to external ventricular drainage in
Both the steering committee and executive sub-committees spontaneous intracerebral hemorrhage with hydrocephalus. Neurology
1998; 50:519–23.
manage this study. The study is financially supported by the
13 Shapiro SA, Campbell RL, Scully T. Hemorrhagic dilation of the
National Institutes of Health (NIH)/Neurological and NINDS, fourth ventricle: an ominous predictor. J Neurosurg 1994; 80:805–9.
grant-in-aid number 5U01NS062851. The study drug is provided 14 Pang D, Sclabassi RJ, Horton JA. Lysis of intraventricular blood clot
by Genentech. with urokinase in a canine model: part 3: effects of intraventricular
urokinase on clot lysis and posthemorrhagic hydrocephalus. Neuro-
Conclusion surgery 1986; 19:553–72.
15 Steinke W, Sacco RL, Mohr JP. Thalamic stroke. Presentation and
prognosis of infarcts and hemorrhages. Arch Neurol 1992; 49:703–10.
CLEAR III is the first, randomized, multicenter, double-blinded, 16 Lee KR, Betz AL, Kim S, Keep RF, Hoff JT. The role of the coagulation
placebo-controlled phase III trial assessing the efficacy of intra- cascade in brain edema formation after intracerebral hemorrhage.
ventricular thrombolytic therapy in IVH patients with an EVD. Acta Neurochir (Wien) 1996; 138:396–401.
The allowance for dosing and EVD placement and removal deci- 17 Ellington E, Margolis G. Block of arachnoid villus by subarachnoid
sions by nonstudy team physicians reflects the practical nature hemorrhage. J Neurosurg 1969; 30:651–7.
18 Kibler RF, Couch RSC, Crompton MR. Hydrocephalus in the adult
and generalizability of this study. If the study outcome is positive,
following spontaneous hemorrhage. Brain 1961; 84:45–61.
it will significantly improve the therapeutic options for acute 19 Pang D, Sclabassi RJ, Horton JA. Lysis of intraventricular blood clot
haemorrhagic stroke treatment. Based on available screening with urokinase in a canine model: part 2: in vivo safety study of
data, we estimate that 10–15% of all ICH, somewhere between intraventricular urokinase. Neurosurgery 1986; 19:547–52.
10 000 and 15 000 ICH subjects in the United States yearly, and 20 Mayfrank L, Kissler J, Raoofi R. Ventricular dilatation in experimental
intraventricular hemorrhage in pigs. Characterization of cerebrospi-
150–200 000 ICH subjects worldwide would be eligible for this
nal fluid dynamics and the effects of fibrinolytic treatment. Stroke
therapy. It is an important step toward reducing the burden of 1997; 28:141–8.
ICH worldwide. 21 Coplin WM, Vinas FC, Agris JM et al. A cohort study of the safety and
feasibility of intraventricular urokinase for nonaneurysmal spontane-
References ous intraventricular hemorrhage. Stroke 1998; 29:1573–9.
1 Diringer MN, Edwards DF, Zazulia AR. Hydrocephalus: a previously 22 Naff NJ, Carhuapoma JR, Williams MA et al. Treatment of intraven-
unrecognized predictor of poor outcome from supratentorial intra- tricular hemorrhage with urokinase: effects on 30-Day survival. Stroke
cerebral hemorrhage. Stroke 1998; 29:1352–7. 2000; 31:841–7.
6 Vol ••, •• 2013, ••–•• © 2013 The Authors.
International Journal of Stroke © 2013 World Stroke Organization
W. C. Ziai et al. Research
23 Naff NJ, Hanley DF, Keyl PM et al. Intraventricular thrombolysis 32 Torres A, Plans G, Martino J et al. Fibrinolytic therapy in spontaneous
speeds blood clot resolution: results of a pilot, prospective, random- intraventricular haemorrhage: efficacy and safety of the treatment. Br
ized, doubleblind, controlled trial. Neurosurgery 2004; 54:577–83. J Neurosurg 2008; 22:269–74.
24 Rainov NG, Burkert WL. Urokinase infusion for severe intraventricu- 33 Tung MY, Ong PL, Seow WT, Tan KK. A study on the efficacy of
lar hemorrhage. Acta Neurochir (Wien) 1995; 134:55–9. intraventricular urokinase in the treatment of intraventricular haem-
25 Akdemir H, Selçuklu A, Pasaoglu A, Oktem IS, Kavuncu I. Treatment orrhage. Br J Neurosurg 1998; 12:234–9.
of severe intraventricular hemorrhage by intraventricular infusion of 34 Lapointe M, Haines S. Fibrinolytic therapy for intraventricular hem-
urokinase. Neurosurg Rev 1995; 18:95–100. orrhage in adults. Cochrane Database Syst Rev 2002; (3):CD003692.
26 Vereecken KK, Van Havenbergh T, De Beuckelaar W, Parizel PM, 35 Gaberel T, Magheru C, Emery E, Derlon JM. Antifibrinolytic therapy
Jorens PG. Treatment of intraventricular hemorrhage with intraven- in the management of aneurismal subarachnoid hemorrhage revis-
tricular administration of recombinant tissue plasminogen activator: ited. A meta-analysis. Acta Neurochir (Wien) 2012; 154:1–9.
a clinical study of 18 cases. Clin Neurol Neurosurg 2006; 108:451–5. 36 Naff N, Williams M, Keyl PM et al. Low-dose rt-PA enhances clot
27 Bartek J Jr, Hansen-Schwartz J, Bergdal O et al. Alteplase (rt-PA) treat- resolution in brain hemorrhage: the intraventricular hemorrhage
ment of intraventricular hematoma (IVH): safety of an efficient meth- thrombolysis trial. Stroke 2011; 42:3009–16.
odological approach for rapid clot removal. Acta Neurochir Suppl 37 Demchuk AM, Dowlatshahi D, Rodriguez-Luna D et al.; PREDICT/
2011; 111:409–13. Sunnybrook ICH CTA study group. Prediction of haematoma growth
28 Dunatov S, Antoncic I, Bralic M, Jurjevic A. Intraventricular throm- and outcome in patients with intracerebral haemorrhage using the
bolysis with rt-PA in patients with intraventricular hemorrhage. Acta CT-angiography spot sign (PREDICT): a prospective observational
Neurol Scand 2011; 124:343–8. study. Lancet Neurol 2012; 11:307–14.
29 Staykov D, Huttner HB, Struffert T et al. Intraventricular fibrinolysis
and lumbar drainage for ventricular hemorrhage. Stroke 2009;
40:3275–80.
30 Huttner HB, Tognoni E, Bardutzky J et al. Influence of intraventricular
fibrinolytic therapy with rt-PA on the long-term outcome of treated Supporting Information
patients with spontaneous basal ganglia hemorrhage: a case-control Additional Supporting Information may be found in the online
study. Eur J Neurol 2008; 15:342–9.
31 Todo T, Usui M, Takakura K. Treatment of severe intraventricular
version of this article at the publisher’s web-site:
hemorrhage byintraventricular infusion of urokinase. J Neurosurg
1991; 74:81–6. Appendix S1: Acknowledgements
© 2013 The Authors. Vol ••, •• 2013, ••–•• 7
International Journal of Stroke © 2013 World Stroke Organization
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Urology DNB Old QuestionsDokument8 SeitenUrology DNB Old QuestionssjulurisNoch keine Bewertungen
- Below The Knee AmputationDokument76 SeitenBelow The Knee AmputationDarell M. Book50% (2)
- Section H. Morbidity Diseases ReportDokument5 SeitenSection H. Morbidity Diseases ReportSeriel TismoNoch keine Bewertungen
- Dermatology QuizDokument10 SeitenDermatology QuizSyed Ali Haider0% (1)
- TungDokument203 SeitenTungValdemar Caumo Junior100% (5)
- Boot CampDokument190 SeitenBoot CampfekaduNoch keine Bewertungen
- 200 Points in Special PathologyDokument15 Seiten200 Points in Special Pathologyjihadeqitaal100% (1)
- Hanley 2017Dokument9 SeitenHanley 2017sjulurisNoch keine Bewertungen
- Check List For Dnb-Final Application Form: Tick The EnclosuresDokument1 SeiteCheck List For Dnb-Final Application Form: Tick The EnclosuressjulurisNoch keine Bewertungen
- MISTIEDokument10 SeitenMISTIEsjulurisNoch keine Bewertungen
- National Board of Examinations: Office Use OnlyDokument4 SeitenNational Board of Examinations: Office Use OnlysjulurisNoch keine Bewertungen
- DNB PAPERS OLD Dec 06-Jun14Dokument41 SeitenDNB PAPERS OLD Dec 06-Jun14sjulurisNoch keine Bewertungen
- Dec 2006Dokument4 SeitenDec 2006sjulurisNoch keine Bewertungen
- Indian Bank Challan For DNB FINAL Exam Fee 6008280724Dokument1 SeiteIndian Bank Challan For DNB FINAL Exam Fee 6008280724sjulurisNoch keine Bewertungen
- Limb.o,: ./T - RFLF" . Prerforation?Dokument4 SeitenLimb.o,: ./T - RFLF" . Prerforation?sjulurisNoch keine Bewertungen
- December 2010Dokument4 SeitenDecember 2010sjulurisNoch keine Bewertungen
- Dec 2007Dokument4 SeitenDec 2007sjulurisNoch keine Bewertungen
- December 2008Dokument4 SeitenDecember 2008sjulurisNoch keine Bewertungen
- June 2010Dokument4 SeitenJune 2010sjulurisNoch keine Bewertungen
- Pancreas Nad SpleenDokument2 SeitenPancreas Nad SpleensjulurisNoch keine Bewertungen
- Stomach and Duodenum-1Dokument1 SeiteStomach and Duodenum-1sjulurisNoch keine Bewertungen
- Time:: 2. A) Shock? I B) C) 3. A) B) C)Dokument5 SeitenTime:: 2. A) Shock? I B) C) 3. A) B) C)sjulurisNoch keine Bewertungen
- June 2014Dokument4 SeitenJune 2014sjulurisNoch keine Bewertungen
- Small Intestines-1Dokument3 SeitenSmall Intestines-1sjulurisNoch keine Bewertungen
- Thyroid and Parathyroid-1Dokument1 SeiteThyroid and Parathyroid-1sjulurisNoch keine Bewertungen
- Liver and Biliary TractDokument3 SeitenLiver and Biliary TractsjulurisNoch keine Bewertungen
- DKA AssignmentDokument4 SeitenDKA AssignmentHisham ShahinNoch keine Bewertungen
- Neurologic Disorders:: Anatomy & PhysiologyDokument9 SeitenNeurologic Disorders:: Anatomy & PhysiologyMaria Erlene SantosNoch keine Bewertungen
- Augmentin DdsDokument12 SeitenAugmentin DdsQureshi imtiyazNoch keine Bewertungen
- The Technique: of ThyroidectomyDokument5 SeitenThe Technique: of Thyroidectomyعمر كمالNoch keine Bewertungen
- The Content of This Leaflet Was Updated According To The Guidelines of The Ministry of Health in September 2017Dokument14 SeitenThe Content of This Leaflet Was Updated According To The Guidelines of The Ministry of Health in September 2017ddandan_2Noch keine Bewertungen
- Nursing Sensory Perception System Gustatory: Lecturer: Ns. Leni Merdawati, M.KepDokument18 SeitenNursing Sensory Perception System Gustatory: Lecturer: Ns. Leni Merdawati, M.KepfaradillaNoch keine Bewertungen
- Urinary Tract InfectionDokument3 SeitenUrinary Tract InfectionHo Yong WaiNoch keine Bewertungen
- Sexual Disorders: Ms. Kanika KumarDokument60 SeitenSexual Disorders: Ms. Kanika KumarRakesh KumarNoch keine Bewertungen
- Orofacial Infections in Children PedoDokument40 SeitenOrofacial Infections in Children PedoFourthMolar.comNoch keine Bewertungen
- DJCP/19: .2019 Clinical PharmacologyDokument40 SeitenDJCP/19: .2019 Clinical PharmacologyKeshavVashisthaNoch keine Bewertungen
- Charles Bonnet Syndrome - RNIBDokument10 SeitenCharles Bonnet Syndrome - RNIBSeplou7iNoch keine Bewertungen
- 26-11-2013 Histology 1Dokument4 Seiten26-11-2013 Histology 1hacettepe6d6nembirNoch keine Bewertungen
- Addison's Disease:-: SymptomsDokument2 SeitenAddison's Disease:-: SymptomsIjaz KhanNoch keine Bewertungen
- Urology1 UPDATEDDokument44 SeitenUrology1 UPDATEDmarwanNoch keine Bewertungen
- Acute Kidney InjuryDokument43 SeitenAcute Kidney InjuryIwan ToniroNoch keine Bewertungen
- COMMED 0503C Leptospirosis PDFDokument4 SeitenCOMMED 0503C Leptospirosis PDFGabby ElardoNoch keine Bewertungen
- Defect de Sept AtrialDokument4 SeitenDefect de Sept Atrial22194Noch keine Bewertungen
- Manejo Fungemia Guía ColombianoDokument34 SeitenManejo Fungemia Guía ColombianoLesly Peinado TorresNoch keine Bewertungen
- Ent Diseases of The Oral and Pharynx Dr. UyDokument7 SeitenEnt Diseases of The Oral and Pharynx Dr. UyAileen EmyNoch keine Bewertungen
- Pharmacotherapy Handbook - ALLERGIC RHINITISDokument8 SeitenPharmacotherapy Handbook - ALLERGIC RHINITISstella.gillesania.chenNoch keine Bewertungen
- BoneDokument5 SeitenBoneTaha IsmailNoch keine Bewertungen
- Shahan Mumraiz Khan-2017 076Dokument48 SeitenShahan Mumraiz Khan-2017 076zaminazzNoch keine Bewertungen
- Therapeutic Classification of Drugs Based On The Philippine National Drug FormularyDokument25 SeitenTherapeutic Classification of Drugs Based On The Philippine National Drug FormularyJelight Faith Salero GachoNoch keine Bewertungen
- Headnursing Final OutputDokument30 SeitenHeadnursing Final OutputCharissa Magistrado De LeonNoch keine Bewertungen