Beruflich Dokumente
Kultur Dokumente
Liver (Dr. Cham)
Hochgeladen von
yayayaniza0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
27 Ansichten4 SeitenCopyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
27 Ansichten4 SeitenLiver (Dr. Cham)
Hochgeladen von
yayayanizaCopyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 4
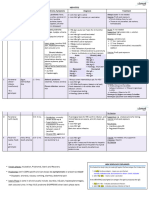
LIVER – Dra.
Cham Categories forms: Maybe acute event or asymptomatic
HBe Ag (+) chemoTx and immunosuppressive are at
Hepatitis A HBe Ag (-) risk
HBs Ag carrier state
RNA virus Diagnosis
Fecal-oral route Phases of Chronic Infection
IP: 2-6 weeks HBs Ag
(-) chronic and carrier stage Immune tolerant - General marker of infxn
st
<1% fulminant hepa Immune clearance - 1 marker to appear
5% in pedia; 70-80% in adult Residual or inactive HBc Ag
Self limitng Reactivation - Nucleocapsid that encloses the viral
Dx: anti HAV (IgM) – acute; (IgG) – DNA
Immune tolerant phase HBeAg
immunity
Rx: supportive Young, asymptomatic
- Rapid viral replication
Anti HBs
(+) HBsAg, (+) HBeAg
Hepatitis B - Protective immunity
High HBV-DNA (>2,000,000-20,000,000
- Recovered from natural infection or
Small DNA virus, Partially double stranded IU/ml)
vaccinated
Parenteral, STD’s, *perinatal ALT normal, no clinicopathological changes
AntiHBe
IP: 1-6 mo
Immune Clearance Phase - Produced in response to HBeAg
10% chronic carrier - Slow viral replication
(+) !% fulminant ↑ ALT ↓HBV-DN - (+) after cleared from HBeAg
Chr infection = <5% adults, >90% infants Eventually followed by seroconversion of Anti HBc (IgM)
HBe Ag anti HBe - Acute or recent infection
Genotypes A-H:
For undetectable HBV-DNA - Maybe (+) in low tites in 15-20% of
B and C – Asia Pacific Regions acute flares of chronic infection
Residual or Inactive Phase
A and D – Europe and Mediterranean Anti HBc (IgG)
B<C – progression of liver disease - Current or past infection
After seroconversion
C>B – risk of HCC - Found in recovery
Preceded by marked ↑HBV-DNA, Normal
A and C – more severe liver disease ALT, resolution of liver necroinflam’n Treatment
- Greater disease progression Mostly remain (+) HBeAg for lifetime
IFN or PEG IFN alpha 2a
Chronic Hepatitis B Reactivation Phase Antiviral drugs
Persistent infection=/> 6mos - Lamivudine
Reappearance of necroinflam’n of the liver
(+) HBsAg with chr inflam’n, necrosis and - Entecabir
↑ALT, (+) HBV-DNA, (+/-) HBe Ag
fibrosis of the liver - Adefovir
Approx. 50% may reactive
- Telbivudine
Jcelimpin 3D 07012012 1
- Tenofovir Hepatitis G Entecavir
Lifestlye – prevent transmission thru sex, - Immunomodulator
blood, spill, perinatal RNA virus IFN
Alcohol abstinence Parenteral Glucocorticoids
Contacts – vaccination 15% non-A, non-B, non-C cases of chronic Thymosin alpha 1
hepa
Ribavirin
Hepatitis C Associated with fulminant hepatitis
IL 2 and 12
RNA virus Pathology HCV infection treatment:
90% post BT 1. IFN A 2a – 3 MU tiw x 12mo
Parenteral, perianal, STD’s Mononuclear cell infiltration 2. IFN A 2b – 3-6 MU tiw x 12 mo
IP: 2 weeks – 6 mos Cellular ballooning and necrosis 3. Lymphoblastoid IFN – 3 MU tiw x 6
30-50%n chronic and cirrhosis, CA Condensed cytoplasm with pyknotic nuclei mo
(acidophilic bodies) 4. IF A 2b 3MU tiw + Ribavirin
Treatment: 1000mg/d
Clinical Features ***decompensated liver cirrhosis
PEG IFN liver transplantation
Malaise, anorexia, fatigue
Ribavirin
Arthritis and urticaria (common in HB) Complications
Response to Rx: - due to circulating immune complexes
influenza like syndrome in HA Fulminant hepatitis
Genotypes 2>3>4>1 50% jaundice Chronic persistent hepatitis
Hepatomegaly and tenderness Chronic active hepatitis
Hepatitis D
20% hepatomegaly Chronic carrier state
Delta hepatitis Cholestatic hepatitis
Small, defective RNA virus
Diagnosis Aplastic anemia
Infectious if (+) Hep B infection Malignancy
Serology
Relies on HB proteins for replication LFT Fulminant Hepatitis
Gen has chronic, severe infection Hepatitis profile
2-7.5% fulminant hepatitis Rare in HA
Treatment Occurs in 1-2% of Hb and HC
Hepatitis E
Common in delta agent superinfection with
Supportive acute
Small RNA virus CHB
Chronic active Hepa B:
Short IP Progressive jaundice, hepatic enceph and
- Nucleoside analogues
Probably water borne ascites
Lamivudine
10-20% MR in pregnant Common hepatorenal syndrome
Famciclovir
90-100% MR in 60yo and increase
Adefovir
Jcelimpin 3D 07012012 2
Chronic Persistent Hepatitis Risk Factors - ↑ glucose
- (-) viral markers
After HB, HC and HG Obesity - (-) autoantibodies
Increase transaminase > 6 mos Hyperglycemia – insulin resistant - US= fatty liver
(-) fibrosis Hypercholesterolemia = stigmata of Postal HPN (unusual)
Mostly asymptomatic
***2/3 are >45yo have NIDDM, obese and increase
Some have fatigue, abdominal pains,
anorexia triglyceride
Liver bx: periportal lymphocytic Etiology
infiltrates but (-) extension beyond the
portal triad Drugs and toxins
Benign course - Ex. Methotrexate, amiodarones,
diltiazem, estrogen, hydralazine,
Chronic Active Hepatitis coumarin, tamoxifen, steroids
Metabolic abnormality
Complication of HB and Hc
Acquired – DM, IBD, severe anemia
Increase transaminase >6 mo
Congenital – wilson’s disease,
May lead to cirrhosis
galatosemia, abetalipoprotein
No consistent Rx
Trials of IFN and antiviral agents Pathogenesis
Liver Bx: (+) inflammation, necrosis and
Maultifactorial Treatment
fibrosis bridging the portal areas
- Amino acid imbalance
Define risk factors for NAFLD
Chronic Carrier state - Hyperglycemia
- X’sive circulating level of anabolic (FBS, lipid profile, BMI evaluation, meds)
(+) HBs Ag
(insulin) compare to catabolic (leptin)
(+) Anti HBe Controlled weight loss
hormones and endothermia
Normal ALT
Health carrier state (-) cirrhosis Clinical features Rx DM and Hyperlipidemia
(-) hepatoma
Often asymptomatic Dic toxic meds and alc
Non Alcoholic Fatty Liver Disease Hepatomegaly – common
Splenomegaly in some
Form of chronic hepa but no tx of
Portal HPN (unusual) Monitor lab results, wt clin Rx trials
alcoholism
Lab findings
Middle age obese women Lipid levels
- ↑transaminase
Macrovesicular steatosis
- ↑alkphos
Directly proportional to body weight - ↑chol and triglycerides (common)\
Jcelimpin 3D 07012012 3
Alcoholic Liver Disease 3. Liver Cirrhosis Clinical features
Normal Liver - Long term alc is tosic to the testes Hepatomegaly
testicular atrophy impotence Hepatic bruit
90-100% Alc ↑peri levels of estrogen
- Bloody ascites
Fatty liver
gynecomastia, spider angiomas, palmar Abdominal pains
erythema Anorexia
10-35% 8-20% - Irreversible Weight loss
Complications of ALD Diagnosis
Alcoholic hepatitis cirrhosis 1. Ascites Liver Biopsy
2. GI he – from varices AFP
40% 3. Encephalopathy LFT
4. Hypoalbuminemia
Grp of liver disease due to chr alc Gallium scan (filling defect)
5. Hypoprothrombinemia
Alc> 80g/d in men; >40g/d in women CT Scan
6. Liver cirrhosis hepatoma
1. Fatty liver Treatment
Hepatoma
- Hepatomegaly (+/-) No effective Rx
Occurs 5x in men
- Gen asymp - Surgery
Peak age incidence: 40-80 yo
- ↑ transaminase and alk phos - RFA
Unknown etiology - chemoRx
- Histo: large fat droplet in liver
- Reversible - liver transplant
Risk Factors:
- chemoembolization
2. alcoholic hepatits Alcoholism
Hepatitis B and C
- In heavy alcohol consumption
Aflatoxin
- Most have >100g/d for >1yr
Cirrhosis of the liver
- Fever, jaundice, hepatomegaly, tender liver
- Abn LFT Hematochromatosis
- Liver bx: liver fat droplets Wilson’s disease
PMN infiltration NIDDM type (w/ obesity NAFLD)
Alc hyaline bodies (Mallory bodies)
- RX: supportive, alcohol abstinence
- Reversible
Jcelimpin 3D 07012012 4
Das könnte Ihnen auch gefallen
- NDT HandBook Volume 10 (NDT Overview)Dokument600 SeitenNDT HandBook Volume 10 (NDT Overview)mahesh95% (19)
- One Foot in The Grave - Copy For PlayersDokument76 SeitenOne Foot in The Grave - Copy For Playerssveni meierNoch keine Bewertungen
- Hepatitis BDokument23 SeitenHepatitis BMarty Asis100% (1)
- S O S Services Alert Level Help Sheet - REFERENCIALESDokument20 SeitenS O S Services Alert Level Help Sheet - REFERENCIALESDavid Poma100% (1)
- Wind Turbines - I. Al-BahadlyDokument664 SeitenWind Turbines - I. Al-Bahadlykevin_leigh_1Noch keine Bewertungen
- Serology of Viral Infections PDFDokument72 SeitenSerology of Viral Infections PDFAffie SaikolNoch keine Bewertungen
- Financial Statement AnalysisDokument18 SeitenFinancial Statement AnalysisAbdul MajeedNoch keine Bewertungen
- HIV&HepatitisDokument46 SeitenHIV&HepatitisRaja RuzannaNoch keine Bewertungen
- Asthma: Pio T. Esguerra II, MD, FPCP, FPCCP Pulmonary & Critical Care FEU-NRMF Medical CenterDokument98 SeitenAsthma: Pio T. Esguerra II, MD, FPCP, FPCCP Pulmonary & Critical Care FEU-NRMF Medical CenteryayayanizaNoch keine Bewertungen
- Hepatitis: Dr. Amany A. GhazyDokument44 SeitenHepatitis: Dr. Amany A. GhazyJosé Luis García GarcíaNoch keine Bewertungen
- Abacus 1 PDFDokument13 SeitenAbacus 1 PDFAli ChababNoch keine Bewertungen
- Hepatitis BUMIL, Materi DR - Emil, SP - Pd.Dokument36 SeitenHepatitis BUMIL, Materi DR - Emil, SP - Pd.yuliyanto.efendiNoch keine Bewertungen
- Kuliah YyDokument26 SeitenKuliah YyEsakumala DinantiNoch keine Bewertungen
- Viral Diagnostic TestsDokument4 SeitenViral Diagnostic TestsAhmed GaberNoch keine Bewertungen
- Hepatitis A, B, C, D & EDokument1 SeiteHepatitis A, B, C, D & EMaryam FadahNoch keine Bewertungen
- HBV Easl 2017Dokument57 SeitenHBV Easl 2017jessica100% (1)
- Haag Anti-Hav Anti-Hav, Igm: Serologia de La Hepatitis Viral Hepatitis ADokument6 SeitenHaag Anti-Hav Anti-Hav, Igm: Serologia de La Hepatitis Viral Hepatitis ATatiana Santillana RiveroNoch keine Bewertungen
- Gastroenterology Handouts Spring 2019Dokument27 SeitenGastroenterology Handouts Spring 2019Sasoo EmadNoch keine Bewertungen
- Hepatitis: Diah Puspita Rini, DR., SPPKDokument46 SeitenHepatitis: Diah Puspita Rini, DR., SPPKSetiawan SukmadjaNoch keine Bewertungen
- Hepatitis A, B and C VirusDokument46 SeitenHepatitis A, B and C VirusChyzhi SylviaNoch keine Bewertungen
- Hepatitis VirusesDokument35 SeitenHepatitis VirusesRaja RuzannaNoch keine Bewertungen
- Hepatitis B ChronicDokument8 SeitenHepatitis B ChronicmutiaraptrcNoch keine Bewertungen
- Koda Kimble Ebook-1832-1869Dokument44 SeitenKoda Kimble Ebook-1832-1869Mirna WulansariNoch keine Bewertungen
- Seurm Markers of Hepetitis VirusDokument40 SeitenSeurm Markers of Hepetitis Virusmirabel IvanaliNoch keine Bewertungen
- Ese Liaison XL Hepatitis Ab Low 4Dokument4 SeitenEse Liaison XL Hepatitis Ab Low 4Didier DjogbessiNoch keine Bewertungen
- Approach To CLDDokument39 SeitenApproach To CLDSanrio NeuroNoch keine Bewertungen
- Viral Hepatitis: Nining Sri Wuryaningsih Bagian Patologi Klinik FK UNSDokument36 SeitenViral Hepatitis: Nining Sri Wuryaningsih Bagian Patologi Klinik FK UNSdayanr02Noch keine Bewertungen
- Hepatitis B: Steve HartDokument36 SeitenHepatitis B: Steve HartangelinaNoch keine Bewertungen
- HEPATITISDokument4 SeitenHEPATITISYalin AbouhassiraNoch keine Bewertungen
- Topics For Oral Exam Hep Pneu DengueDokument4 SeitenTopics For Oral Exam Hep Pneu DenguePCRMNoch keine Bewertungen
- Hepatitis Virus 2014Dokument35 SeitenHepatitis Virus 2014Rahma MahrozaNoch keine Bewertungen
- HepatitisDokument3 SeitenHepatitisapi-648401824Noch keine Bewertungen
- Pemeriksaan Terkini Hepatitis Virus: Prof. Dr. Jusak Nugraha, DR, MS, SPPK (K) Lab Patologi Klinik FK UnairDokument53 SeitenPemeriksaan Terkini Hepatitis Virus: Prof. Dr. Jusak Nugraha, DR, MS, SPPK (K) Lab Patologi Klinik FK UnairMuh YunusNoch keine Bewertungen
- Viral Hepatitis Training Manual: Federal Ministry of Health National Hepatitis Control Program 2021Dokument11 SeitenViral Hepatitis Training Manual: Federal Ministry of Health National Hepatitis Control Program 2021Eleni HagosNoch keine Bewertungen
- Hepatitis FinalDokument73 SeitenHepatitis FinalAkhil MuraliNoch keine Bewertungen
- HepatitisDokument2 SeitenHepatitisHafify RashidNoch keine Bewertungen
- Infeksi Virus Pada Sistem Pencernaan Bawah: Hepatitis: Ety AprilianaDokument27 SeitenInfeksi Virus Pada Sistem Pencernaan Bawah: Hepatitis: Ety AprilianaAsmorowatiNoch keine Bewertungen
- Gastroenterology - Viral HepatitisDokument2 SeitenGastroenterology - Viral HepatitisEugen MNoch keine Bewertungen
- Interpretation of Hepatitis B Serologic Test Results - CDCDokument2 SeitenInterpretation of Hepatitis B Serologic Test Results - CDCmelissa kristianaNoch keine Bewertungen
- 319 - Gastrointestinal Pathology) Hepatitis - Diagnosis of Viral HepatitisDokument4 Seiten319 - Gastrointestinal Pathology) Hepatitis - Diagnosis of Viral Hepatitismirxa6756Noch keine Bewertungen
- COL Ē Hepatitis VirusDokument4 SeitenCOL Ē Hepatitis VirusaunghtutooNoch keine Bewertungen
- Cirrhosis Hepatis 1Dokument48 SeitenCirrhosis Hepatis 1Muhammad RivaileNoch keine Bewertungen
- Serologicchartv 8Dokument1 SeiteSerologicchartv 8Gautamu ZalavadiyaNoch keine Bewertungen
- Hepatitis Viruses: Dr. Muna. M. A. Yousif M.D Clinical MicrobiologyDokument45 SeitenHepatitis Viruses: Dr. Muna. M. A. Yousif M.D Clinical MicrobiologyMAxeneNoch keine Bewertungen
- Viral Hepatitis Tests PDFDokument7 SeitenViral Hepatitis Tests PDFHussein N. FarhatNoch keine Bewertungen
- Item C132. Interpretation of The Serologic Markers of Hepatitis B in Common SituationsDokument1 SeiteItem C132. Interpretation of The Serologic Markers of Hepatitis B in Common Situationsreny93Noch keine Bewertungen
- Viral Hepatitis: Umar Zein Faculty of Medicine Universitas Islam Sumatera Utara 2021Dokument23 SeitenViral Hepatitis: Umar Zein Faculty of Medicine Universitas Islam Sumatera Utara 2021yuniNoch keine Bewertungen
- serologicchartv8HepB PDFDokument1 Seiteserologicchartv8HepB PDFAlen RendakNoch keine Bewertungen
- Interpretation of Hepatitis B Serologic Test ResultsDokument1 SeiteInterpretation of Hepatitis B Serologic Test ResultsMUHAMMAD JAWAD HASSANNoch keine Bewertungen
- Interpretation of Hepatitis B Serologic Test ResultsDokument1 SeiteInterpretation of Hepatitis B Serologic Test ResultsarjumandNoch keine Bewertungen
- Serological Markers For Viral HepatitisDokument29 SeitenSerological Markers For Viral HepatitisMariah ValdehuezaNoch keine Bewertungen
- Acute VH Definition:: Diffuse Liver Inflammation Lasting Less Than 6 MonthsDokument22 SeitenAcute VH Definition:: Diffuse Liver Inflammation Lasting Less Than 6 Monthsnanda ashriNoch keine Bewertungen
- Hep B VirusDokument20 SeitenHep B VirusBhupesh ChandNoch keine Bewertungen
- Hepatitis Viral - Dr. José Gonzáles BenavidesDokument64 SeitenHepatitis Viral - Dr. José Gonzáles BenavidesEfrain Brian SilvaNoch keine Bewertungen
- Hepatitis B Dan C - PresentasiDokument31 SeitenHepatitis B Dan C - PresentasiRatu anisa Fadila balgisNoch keine Bewertungen
- Acute Viral Hepatitis: Acute Inflamation of The Liver Caused by Primarly Hepatotropic Viruses (A, B, C, D, E)Dokument35 SeitenAcute Viral Hepatitis: Acute Inflamation of The Liver Caused by Primarly Hepatotropic Viruses (A, B, C, D, E)Tarik PlojovicNoch keine Bewertungen
- Hepatitis Day 2022Dokument10 SeitenHepatitis Day 2022Bilal NafeesNoch keine Bewertungen
- Hepatitis A Serology: Acute HAV Prior HAVDokument4 SeitenHepatitis A Serology: Acute HAV Prior HAVAya AlamsjahNoch keine Bewertungen
- 2018 Hepatitis Viral InfectionDokument51 Seiten2018 Hepatitis Viral Infectionkomang nickoNoch keine Bewertungen
- Heptits Chronic BDokument31 SeitenHeptits Chronic BNicko Junior FakdawerNoch keine Bewertungen
- HBV Testing 9 Oct 2019Dokument34 SeitenHBV Testing 9 Oct 2019Joedimarzio yondaimeNoch keine Bewertungen
- Interpretation-Hepatitis-B-Serology SummaryDokument1 SeiteInterpretation-Hepatitis-B-Serology SummaryNetNoch keine Bewertungen
- He HepatitisDokument4 SeitenHe HepatitisMayar JaradNoch keine Bewertungen
- Hepatitis B & C, Alamanda GarutDokument43 SeitenHepatitis B & C, Alamanda GarutAndi Putra RegardboyNoch keine Bewertungen
- Dermatology and Hepatitis B1Dokument48 SeitenDermatology and Hepatitis B1kim yoon jungNoch keine Bewertungen
- Hepatitis B Virus and Liver DiseaseVon EverandHepatitis B Virus and Liver DiseaseJia-Horng KaoNoch keine Bewertungen
- Hepatitis C Virus-Host Interactions and Therapeutics: Current Insights and Future PerspectivesVon EverandHepatitis C Virus-Host Interactions and Therapeutics: Current Insights and Future PerspectivesNoch keine Bewertungen
- Efficacy and Safety of Pirfenidone in Patients.13Dokument7 SeitenEfficacy and Safety of Pirfenidone in Patients.13yayayanizaNoch keine Bewertungen
- Using An Incentive Spirometer Reduces Pulmonary Complications in Patients With Traumatic Rib Fractures A Randomized Controlled TrialDokument8 SeitenUsing An Incentive Spirometer Reduces Pulmonary Complications in Patients With Traumatic Rib Fractures A Randomized Controlled TrialyayayanizaNoch keine Bewertungen
- Using An Incentive Spirometer Reduces Pulmonary Complications in Patients With Traumatic Rib Fractures A Randomized Controlled TrialDokument8 SeitenUsing An Incentive Spirometer Reduces Pulmonary Complications in Patients With Traumatic Rib Fractures A Randomized Controlled TrialyayayanizaNoch keine Bewertungen
- Tamsulosin Versus Tadalafil As A Medical ExpulsiveDokument6 SeitenTamsulosin Versus Tadalafil As A Medical ExpulsiveyayayanizaNoch keine Bewertungen
- Proforma For Submission of Research Proposal Part I: Proforma For Biographical Data of ApplicantsDokument6 SeitenProforma For Submission of Research Proposal Part I: Proforma For Biographical Data of ApplicantsyayayanizaNoch keine Bewertungen
- Data Collection Proforma: Part 1: Patient Care AnaesthesiaDokument12 SeitenData Collection Proforma: Part 1: Patient Care AnaesthesiayayayanizaNoch keine Bewertungen
- EffectDokument7 SeitenEffectJ Carlos HuañapacoNoch keine Bewertungen
- EffectDokument7 SeitenEffectJ Carlos HuañapacoNoch keine Bewertungen
- Efficacy and Safety of Pirfenidone in Patients.13Dokument7 SeitenEfficacy and Safety of Pirfenidone in Patients.13yayayanizaNoch keine Bewertungen
- A Study of Proforma, A Development Methodology For Clinical ProceduresDokument22 SeitenA Study of Proforma, A Development Methodology For Clinical ProceduresyayayanizaNoch keine Bewertungen
- Proforma For Submission of Research Proposal Part I: Proforma For Biographical Data of ApplicantsDokument6 SeitenProforma For Submission of Research Proposal Part I: Proforma For Biographical Data of ApplicantsyayayanizaNoch keine Bewertungen
- Data Collection Proforma: Part 1: Patient Care AnaesthesiaDokument12 SeitenData Collection Proforma: Part 1: Patient Care AnaesthesiayayayanizaNoch keine Bewertungen
- 1113 - DMWilliams Obstetrics 25th Edition (2018)Dokument18 Seiten1113 - DMWilliams Obstetrics 25th Edition (2018)yayayanizaNoch keine Bewertungen
- 5 StarDokument13 Seiten5 StarSofie Hanafiah NuruddhuhaNoch keine Bewertungen
- M U Ltifeta L Pregnancy: Mechanisms of Multifetal GestationsDokument43 SeitenM U Ltifeta L Pregnancy: Mechanisms of Multifetal GestationsyayayanizaNoch keine Bewertungen
- 584 - Cswilliams Obstetrics 25th Edition (2018)Dokument20 Seiten584 - Cswilliams Obstetrics 25th Edition (2018)yayayanizaNoch keine Bewertungen
- 879 - Multigestationalwilliams Obstetrics 25th Edition (2018)Dokument29 Seiten879 - Multigestationalwilliams Obstetrics 25th Edition (2018)yayayanizaNoch keine Bewertungen
- 952 - Obesitywilliams Obstetrics 25th Edition (2018)Dokument9 Seiten952 - Obesitywilliams Obstetrics 25th Edition (2018)yayayanizaNoch keine Bewertungen
- 1003 - Pulmonarywilliams Obstetrics 25th Edition (2018)Dokument13 Seiten1003 - Pulmonarywilliams Obstetrics 25th Edition (2018)yayayanizaNoch keine Bewertungen
- 570 - Operative Vaginal Deliverywilliams Obstetrics 25th Edition (2018)Dokument12 Seiten570 - Operative Vaginal Deliverywilliams Obstetrics 25th Edition (2018)yayayanizaNoch keine Bewertungen
- 474 - Intrapatum Assessmentwilliams Obstetrics 25th Edition (2018)Dokument25 Seiten474 - Intrapatum Assessmentwilliams Obstetrics 25th Edition (2018)yayayanizaNoch keine Bewertungen
- 556 - Breechwilliams Obstetrics 25th Edition (2018)Dokument12 Seiten556 - Breechwilliams Obstetrics 25th Edition (2018)yayayanizaNoch keine Bewertungen
- 533 - Vaginal Deliverywilliams Obstetrics 25th Edition (2018)Dokument18 Seiten533 - Vaginal Deliverywilliams Obstetrics 25th Edition (2018)yayayanizaNoch keine Bewertungen
- Puerperium ComplicationsDokument28 SeitenPuerperium ComplicationsyayayanizaNoch keine Bewertungen
- AppendixDokument6 SeitenAppendixyayayanizaNoch keine Bewertungen
- Sexually Transmitted Infections: Obstetrics IiDokument24 SeitenSexually Transmitted Infections: Obstetrics IiyayayanizaNoch keine Bewertungen
- EBM Self Instructional Manual 2011Dokument132 SeitenEBM Self Instructional Manual 2011yayayanizaNoch keine Bewertungen
- MED II 22.1 AsthmaDokument6 SeitenMED II 22.1 AsthmayayayanizaNoch keine Bewertungen
- Saes T 883Dokument13 SeitenSaes T 883luke luckyNoch keine Bewertungen
- A Quantitative Method For Evaluation of CAT Tools Based On User Preferences. Anna ZaretskayaDokument5 SeitenA Quantitative Method For Evaluation of CAT Tools Based On User Preferences. Anna ZaretskayaplanetalinguaNoch keine Bewertungen
- MSDS Charcoal Powder PDFDokument3 SeitenMSDS Charcoal Powder PDFSelina VdexNoch keine Bewertungen
- Lit 30Dokument2 SeitenLit 30ReemAlashhab81Noch keine Bewertungen
- A Summer Training ReportDokument39 SeitenA Summer Training ReportShubham SainyNoch keine Bewertungen
- Appendix 3 COT RPMS For T I III SY 2020 2021 in The Time of COVID 19Dokument12 SeitenAppendix 3 COT RPMS For T I III SY 2020 2021 in The Time of COVID 19Marjun PachecoNoch keine Bewertungen
- Chanakya: For The Indian Television Series Based On His Life, SeeDokument11 SeitenChanakya: For The Indian Television Series Based On His Life, SeeTrinadh CrazyguyNoch keine Bewertungen
- Fish Culture in Ponds: Extension Bulletin No. 103Dokument32 SeitenFish Culture in Ponds: Extension Bulletin No. 103Bagas IndiantoNoch keine Bewertungen
- Corregidor Title DefenseDokument16 SeitenCorregidor Title DefenseJaydee ColadillaNoch keine Bewertungen
- Adhesive Film & TapeDokument6 SeitenAdhesive Film & TapeJothi Vel MuruganNoch keine Bewertungen
- De On Tap So 4-6Dokument8 SeitenDe On Tap So 4-6Quy DoNoch keine Bewertungen
- El TontoDokument92 SeitenEl TontoRobertNoch keine Bewertungen
- What Is Terrorism NotesDokument3 SeitenWhat Is Terrorism NotesSyed Ali HaiderNoch keine Bewertungen
- TOR AND SCOPING Presentation SlidesDokument23 SeitenTOR AND SCOPING Presentation SlidesSRESTAA BHATTARAINoch keine Bewertungen
- Unit: 1: Newton's Laws of Motion & Principle of Transmissibility of ForceDokument5 SeitenUnit: 1: Newton's Laws of Motion & Principle of Transmissibility of ForceKunal SinghNoch keine Bewertungen
- Mang-May-Tinh - 03a.-Dns1 - (Cuuduongthancong - Com)Dokument52 SeitenMang-May-Tinh - 03a.-Dns1 - (Cuuduongthancong - Com)Anh Quân TrầnNoch keine Bewertungen
- TSC M34PV - TSC M48PV - User Manual - CryoMed - General Purpose - Rev A - EnglishDokument93 SeitenTSC M34PV - TSC M48PV - User Manual - CryoMed - General Purpose - Rev A - EnglishMurielle HeuchonNoch keine Bewertungen
- Grammar Practice #2Dokument6 SeitenGrammar Practice #2Constantin OpreaNoch keine Bewertungen
- Ch04Exp PDFDokument17 SeitenCh04Exp PDFConstantin PopescuNoch keine Bewertungen
- Quarter 4 Week 1 EnglishDokument62 SeitenQuarter 4 Week 1 EnglishJanine Jordan Canlas-BacaniNoch keine Bewertungen
- Introduction To History AnswerDokument3 SeitenIntroduction To History AnswerLawrence De La RosaNoch keine Bewertungen
- A Vision System For Surface Roughness Characterization Using The Gray Level Co-Occurrence MatrixDokument12 SeitenA Vision System For Surface Roughness Characterization Using The Gray Level Co-Occurrence MatrixPraveen KumarNoch keine Bewertungen
- Bakteri Anaerob: Morfologi, Fisiologi, Epidemiologi, Diagnosis, Pemeriksaan Sy. Miftahul El J.TDokument46 SeitenBakteri Anaerob: Morfologi, Fisiologi, Epidemiologi, Diagnosis, Pemeriksaan Sy. Miftahul El J.TAlif NakyukoNoch keine Bewertungen
- STD Specification For Design and Integration of Fuel Energy Storage F3063Dokument7 SeitenSTD Specification For Design and Integration of Fuel Energy Storage F3063Kobus PretoriusNoch keine Bewertungen