Beruflich Dokumente
Kultur Dokumente
IndianJPsychiatry 2010 52 7 386 69274
Hochgeladen von
Divya ThomasOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
IndianJPsychiatry 2010 52 7 386 69274
Hochgeladen von
Divya ThomasCopyright:
Verfügbare Formate
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/51566713
Liaison psychiatry and Indian research
Article in Indian Journal of Psychiatry · January 2010
DOI: 10.4103/0019-5545.69274 · Source: PubMed
CITATIONS READS
18 152
2 authors:
Shubhangi Parkar Neena Sawant
King Edward Memorial Hospital King Edward Memorial Hospital
34 PUBLICATIONS 349 CITATIONS 47 PUBLICATIONS 186 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Functional Characterization of Voltage Gated calcium channel genes in Schizophrenia specific iPSCs. View project
All content following this page was uploaded by Neena Sawant on 26 May 2017.
The user has requested enhancement of the downloaded file.
Volume 52, Supplement January 2010
EDITORIAL An overview of Indian research in obsessive compulsive
Indian Psychiatry and Indian journal of Psychiatry - A journey disorder
T. S. SATHYANARAYANA RAO, G. SWAMINATH, G. PRASAD RAO S1 Y. C. JANARDHAN REDDY, NAREN P. RAO, SUMANT KHANNA S200
REVIEW ARTICLES An overview of Indian research in anxiety disorders
J. K. TRIVEDI, PAWAN KUMAR GUPTA S210
History of psychiatry in India
S. HAQUE NIZAMIE, NISHANT GOYAL S7 Research in child and adolescent psychiatry in India
Indian journal of psychiatry and psychiatric research in India: PRIYAVADAN CHANDRAKANT SHASTRI, JAY P. SHASTRI,
Past, Present and Future DIMPLE SHASTRI S219
AJAI R. SINGH S13 Learning and other developmental disorders in India
The evolution of Indian psychiatric research: An examination PHILIP JOHN S224
of the early decades of the Indian journal of Psychiatry Indian research on women and psychiatry
RAJIV RADHAKRISHNAN, CHITTARANJAN ANDRADE S19 RAKESH K. CHADDA, MAMTA SOOD S229
Research priorities for Indian psychiatry Psyche and soma: New insights into the connection
VIKRAM PATEL S26 RAHUL KUMAR, VIKRAM K. YERAGANI S233
From local to global – Contributions of Indian psychiatry to Understanding and managing somatoform disorders: Making
international psychiatry sense of non-sense
R. SRINIVASA MURTHY S30 ROY ABRAHAM KALLIVAYALIL, VARGHESE P PUNNOOSE S240
Indian psychiatry: Research and international perspectives Indian research on comorbidities
ROY ABRAHAM KALLIVAYALIL, RAKESH K. CHADDA, ASHISH SRIVASTAVA, SREEJAYAN K., ANUP M. JOSEPH,
JUAN E. MEZZICH S38 P. S. V. N. SHARMA S246
Partnerships for promoting dissemination of mental An overview of Indian research in personality disorders
health research globally PRATAP SHARAN S250
HELEN HERRMAN S43 Indian research on sleep disorders
Indian – American contributions to psychiatric research NILESH SHAH, ABHA BANG, APARNA BHAGAT S255
ANAND K. PANDURANGI S47
Sexuality research in India: An update
Mutual learning and research messages: India, UK, and Europe OM PRAKASH, T. S. SATHYANARAYANA RAO S260
GURVINDER KALRA, DINESH BHUGRA S56
Sexual variation in India: A view from the west
Psychiatrists and neuroscientists of Indian origin in GURVINDER KALRA, SUSHAM GUPTA, DINESH BHUGRA S264
Canada: Glimpses
AMRESH SHRIVASTAVA, D. NATARAJAN S64
HIV and mental health: An overview of research from India
NISHANTH JAYARAJAN, PRABHA S. CHANDRA S269
Indian psychiatry, research and Asian countries
J. K. TRIVEDI, PAWAN KUMAR GUPTA, RAHUL SAHA S68
Publications on community psychiatry
R. THARA, SUSHMA RAMESHKUMAR, C. GREESHMA MOHAN S274
Indian psychiatry and research in Pakistan
HAROON RASHID CHAUDHRY S72 Psychiatric rehabilitation
H. CHANDRASHEKAR, N. R. PRASHANTH, P. KASTHURI,
Contribution of Indian psychiatry in the development of
psychiatry in Nepal S. MADHUSUDHAN S278
TAPAS KUMAR AICH S76 Disabilities research in India
Shared challenges in psychiatric research in India and Sri Lanka H. CHANDRASHEKAR, C. NAVEEN KUMAR, N. R. PRASHANTH,
HARISCHANDRA GAMBHEERA, SHEHAN WILLIAMS S80 P. KASTHURI S281
Training and National deficit of psychiatrists in India – Indian research on disaster and mental health
A critical analysis NILAMADHAB KAR S286
M. THIRUNAVUKARASU, P. THIRUNAVUKARASU S83 Indian research on suicide
Postgraduate training in psychiatry in India LAKSHMI VIJAYAKUMAR S291
SHRIDHAR SHARMA S89 A review of Indian psychiatry research and ethics
Indian Psychiatric epidemiological studies: Learning from the past A. K. AGARWAL S297
SURESH BADA MATH, RAVINDRA SRINIVASARAJU S95 Forensic psychiatry revisited
Indian Psychiatry and classification of psychiatric disorders S. NAMBI S306
K. S. JACOB S104 Indian culture and psychiatry
Initiatives in biological research in Indian Psychiatry SHIV GAUTAM, NIKHIL JAIN S309
AMRESH SHRIVATAVA S110 Military psychiatry in India
Molecular biology research in neuropsychiatry: H. R. A. PRABHU S314
India’s contribution Research on antipsychotics in India
T. S. SATHYANARAYANA RAO, B. N. RAMESH, P. VASUDEVARAJU, AJIT AVASTHI, MUNISH AGGARWAL, SANDEEP GROVER,
K. S. J. RAO S120
MOHD KHALID RASHEED KHAN S317
Cognitive psychiatry in India Research on antidepressants in India
P. K. DALAL, T. SIVAKUMAR S128
AJIT AVASTHI, SANDEEP GROVER, MUNISH AGGARWAL S341
Biological investigations in Indian psychiatry
RISHIKESH V. BEHERE, NAREN P. RAO,
Research on mood stabilizers in India
AJIT AVASTHI, SANDEEP GROVER, MUNISH AGGARWAL S355
GANESAN VENKATASUBRAMANIAN S136
Research on electroconvulsive therapy in India: An overview
Indian research on acute organic brain syndrome: Delirium
BANGALORE N. GANGADHAR, VIVEK H. PHUTANE,
CHARLES PINTO S139
JAGADISHA THIRTHALLI S362
Indian research on aging and dementia
K. S. SHAJI, V. P. JITHU, K. S. JYOTHI S148 Psychotherapy in India
Early intervention in psychotic disorders: Challenges and L. S. S. MANICKAM S366
relevance in the Indian context Indian contribution to behavior therapy
MATCHERI S. KESHAVAN, AMRESH SHRIVASTAVA, K. KURUVILLA S371
BANGALORE N. GANGADHAR S153 Indian scales and inventories
An overview of Indian research in Schizophrenia S. VENKATESAN S378
PARMANAND KULHARA, RUCHITA SHAH, K. R. AARYA S159 Liaison psychiatry and Indian research
An overview of Indian research in bipolar mood disorder S. R. PARKAR, N. S. SAWANT S386
PRASAD G. RAO S173 Role of non-governmental organizations in mental health
An overview of Indian research in depression in India
SANDEEP GROVER, ALAKANANDA DUTT, AJIT AVASTHI S178 R. THARA, VIKRAM PATEL S389
Substance use and addiction research in India Women psychiatrists in India: A reflection of their
PRATIMA MURTHY, N. MANJUNATHA, B. N. SUBODH, contributions
PRABHAT KUMAR CHAND, VIVEK BENEGAL S189 MAMTA SOOD, RAKESH K. CHADDA S396
REVIEW ARTICLE www.indianjpsychiatry.org
Liaison psychiatry and Indian research
S. R. Parkar, N. S. Sawant
Department of Psychiatry, G.S. Medical College and King Edward Memorial Hospital, Parel, Mumbai-400 012, India
ABSTRACT
Liaison in Psychiatry refers to the branch of Psychiatry involving assessment and treatment in the general hospital of
referred patients, like in the casualty, or patients of deliberate self farm. The Indian scene also reveals major reference
from medicine, surgery, surgical super specialty and orthopedics with psychiatric disorders like anxiety, depression and
/ or organic brain syndromes seen in about 40 to 50 % of the medical or surgical patients. Though the Indian published
data is limited, most tertiary hospitals in India carry out liaison work with various departments like Neurology, Organ
transplant, Intensive Care Units and Cosmetic Surgery, so as to give comprehensive health services to patients. Liaison
in Psychiatry has thus brought the emphasis on the teaching of psycho-social aspects of medicine and also increased
research possibilities.
Key words: Liaison psychiatry, GHPU, CLP
INTRODUCTION Though general hospital psychiatry was considered to
come to light as a result of the lack of sufficient funds to
Mental health consultation is the need of the hour and initiate new lunatic asylums, today it is acknowledged as
has been emphasized on since time immemorial.[1] In the a major part of the public health system that takes care
beginning, medical professionals reacted unfavorably to of mental health problems of a large population. Today,
the admission of psychiatric patients in general hospitals. Liaison Psychiatry has acquired the status of a subspecialty
However with recognition of organicity and superimposed within psychiatry and this has helped shift psychiatry from
psychological reaction to medical illness in medical and mental hospitals to a general hospital setting. This has also
surgical departments, psychiatry was appreciated and increased referrals from the non-psychiatric departments
eventually integrated.[2] The rapid growth of general and given the psychiatrist an opportunity to directly deal
hospital psychiatric units all over the world has provided with the physically ill.[3] In general, there is no specific
impetus to consultation-liaison work carried out by the philosophy or particular clinical context being identified in
psychiatrists. Consultation liaison psychiatry (CLP) was Liaison Psychiatry, at present, in India.
generally limited to the diagnostic, research and therapeutic
activity in the non psychiatric departments of the general Referral types
hospital. It is synonymous to liaison psychiatry (psychiatric Several researchers have found a lower referral rate in the
dictionary, Oxford 1970). The mainstay CLP reports are Indian counterparts as compared to the western figures.
to recommend the referrer basic logical clinical findings, Jindal et al.(1980) found a poor referral rate in their study
appropriate treatment and follow-up programs. In addition, as compared to other studies conducted in India.[4] The in-
other objectives are educational, ethical and medico-legal. patient referral rate in their study was 0.15%, as compared
to 1.4%. in the study by Prabhakaran (1968) and 0.66% in the
Address for correspondence: Dr. Shubhangi R. Parkar, study by Parekh et al. (1968).[4-6] Chatterjee and Kutty (1977)
Department of Psychiatry, Chief: Bombay Drug deaddiction reported a referral rate of 2.64% among the out-patients as
center, G.S.Medical College and King Edward, Memorial
Hospital, Parel, Mumbai-400,012 India.
compared to 0.06% by Jindal et al.[7,4] Most studies quote
E-mail: pshubhangi@gmail.com about 60% of referrals from general medicine and 14% from
surgery and surgical super-specialties.[4-6]
DOI: *****
There is also a paucity of data concerning psychiatric
How to cite this article: Parkar SR, Sawant NS. Liaison psychiatry
emergency referral in the Indian setting. Most of the
and Indian research. Indian J Psychiatry 2010;52:S386-8.
available studies pertain to the routine inpatient referral.
S386 Indian J Psychiatry 52, Supplement, January 2010
Parkar and Sawant: Liaison psychiatry
Though psychiatric services are available in almost all symptoms.[18] This group also included those patients
teaching general hospitals in India, little is known as to why who had co-existing physical illness but symptoms were
the psychiatrist is called in emergency situations and what disproportionate to the physical condition. Analysis of final
is the magnitude of the problem. Kelkar et al. (1982) found diagnoses in this study discovered that a large majority
suicidal attempt (13%), excitement and violence (10%) and of the patients had neurotic, stress related, somatoform
altered sensorium (9%) which constituted 32% of the total disorders (indoor 36.76% and outdoor 52.29%) followed
emergency referrals.[8] In the study by Gautam (1978) a vast by mood disorders (indoor 21.08% and outdoor 18.95%).
majority (88%) of the sample of patients who presented with The authors suggest that more interaction and dialogue
somatic symptoms were neurotics.[9] between psychiatric team and referring physician is a need;
their study highlighted that types of patients referred in
General hospital psychiatry units multi specialty hospitals are vastly different and the present
General hospital psychiatry units have provided increased post-graduate training in psychiatry and psychology was
opportunities for interaction between psychiatrists and inadequate in this area.[18]
other medical specialists, making consultation-Liaison
Psychiatry more meaningful .The establishment of General Diverse research studies
Hospital Psychiatry Units (GHPU) proved an impetus for There are some diverse studies which have been reported in
Indian studies on psychiatric morbidity in medical-surgical the Indian Journal Psychiatry. They are infrequent from those
inpatients.[10] Among the first units of this nature were that follow diagnostic profile. They are worth noting in the
those of R. G. Kar Medical College and Hospital, Calcutta Indian context. In the general hospital, in the psychiatric
and Grant Medical College and J.J . Group of Hospitals, clinic, N. N. Wig (1968) reported cases of post vasectomy
Bombay, started in 1933 and 1938 respectively. By 1970, syndrome; the common pattern being that of a chronic and
about 90 psychiatric clinics were operative in India disabling neurasthenic hypochondriac state. [19] However,
(Directory of Mental Health Services in India, 1970). The till date, these aspects have not been researched in Indian
spectrum of psychiatric case material seen in general Psychiatry. There is some research documentation from
hospital psychiatry units is much wider than seen in mental army set up in IJP. A survey, by Major R. S. Mathur (1977,) of
hospitals. Unlike mental hospitals, where the clinical 638 soldiers hospitalized for physical illnesses or trauma in a
material is predominantly psychosis, in a general hospital military hospital has revealed psychiatric morbidity in 34.5%
psychiatry unit there is a wide range of clinical problems of them, manifesting mainly in states of depression (47.9%)
including psychoses, neuroses, personality disorders, and anxiety (40.9%).[20] Psycho-neuroses without obvious
drug dependence and organic brain disorders.[11-13] Referral depression or anxiety formed 11.4%. The subjects who
from inpatient services offers additional area for study in showed psychiatric morbidity with their somatic illnesses
psychosomatic illness.[14] Malhotra S (1984), in her study, found had a longer hospitalization period than the others. Positive
that it was not simply the presence of abnormal behavior correlation of psychiatric morbidity in physical diseases has
that prompted psychiatric consultation, but other reasons been noticed with certain diagnostic categories, literacy
like organic illness insufficient to explain symptoms.[3] The level and certain states of residence; and no correlation has
trends worth noting were, however, a low representation of been seen with age, marital status, and length of service or
personality disorders and drug/alcohol dependence in their rank of the subjects. In some cases of intra-cranial space
study with a uniformly low representation of psychosomatic occupying lesions, infections and cerebral seizures, who
disorder also. The possible explanations for this may be either presented as psychiatric problem or developed
the focus on classical psychiatric disorders and not the mental symptom, an attempt was` made to discuss the
personality disorders which are prevalent currently, due to pathophysiology of psychiatric symptoms in organic brain
various classification systems like Diagnostic and Statistical diseases.[21] Dash and Dash (1979) found that despite advice
Manual of Mental Disorders (DSM) and International of termination of pregnancy in certain vulnerable patients
Classification of Diseases (ICD). on psychiatric grounds, only 56 per cent of them accepted
medical advice.[22] These patients were better educated,
A high prevalence of psychiatric morbidity amongst general hailed from urban areas and belonged to higher strata of
hospital OPD patients was reported in some studies in society than those who rejected such an advice. Comparison
India, (36%) Krishnamurthy S et al. (1981)and (10.4%) by of diagnoses in the 1967 and 1977 groups showed marked
Sriram et al. (1987).[15,16] R.S. Murthy (1998), in his editorial, differences with decrease in the epilepsy and organic
stated that the developments in the twentieth century have brain syndromes due to the development of a neurology
dramatically changed concepts of mental healthcare as a department.[23]
result of new knowledge and has seen a shift from mental
illness to mental health.[17] The proportionate number of schizophrenics in the clinic
population has more than doubled over the 10-year period.
Bhogale et al. (2000) found that 47.57% of indoor referrals This is possibly because of better awareness. Indian Research
and 62.75% of outdoor referrals had unexplained physical on liaison work is mostly with cardiology, dermatology,
Indian J Psychiatry 52, Supplement, January 2010 S387
Parkar and Sawant: Liaison psychiatry
orthopedics, gynecology, medicine, gastroenterology and be able to reduce stigma related to Psychiatry. In future,
ophthalmology. Thus there is a great scope for combined however, there is a need to look at cost effective planning
service and training programs with other specialties like of these services as well as the role of socio-cultural and
internal medicine, pediatrics, neurology, obstetrics and biological parameters in liaison psychiatry.
gynecology. In fact, there is hardly any clinical specialty
which is not related to psychiatry or with which psychiatry REFERENCES
cannot combine, to organize a program.
1. Kirpal Singh. Mental Health Consultation. Indian J Psychiatry 1965;4:215-6.
2. Wig NN. General Hospital psychiatric unit- right time for evaluation. Indian
New avenues are coming up daily with the introduction J Psychiatry 1978;20:1-9.
of new services where psychiatric aspects are of great 3. Malhotra S. Liaison Psychiatry In General Hospitals. Indian J Psychiatry
1984;26:264-73.
importance in a general hospital. Cardiac surgery, epilepsy 4. Jindal RC, Hemrajani D K. A study of psychiatric referrals in a general
surgery, cosmetic surgery, dialysis units, kidney transplants, hospital. Indian J Psychiatry 1980;22:108-10.
5. Prabhakaran M. In patient psychiatric referrals in a general hospital. Indian
intensive care units and family planning services are some J Psychiatry 1968;10:73.
of the examples in this growing field. Chandra has done 6. Parekh HC , Desmukh BD, Bagadia VN, Vahia NS. Analysis of Indoor
extensive work in the area of women’s mental health in Psychiatric referrals in a General Hospital. Indian J Psychiatry 1968;10:81.
7. Chatterjee SB, Kutty PR. A study of psychiatric referrals in military practice
general and specifically the area of the interface between in India. Indian J Psychiatry 1977;19:32.
psychiatry and women’s reproductive and sexual health 8. Kelkar DK, Chaturvedi SK, Malhotra S. A study of emergency psychiatric
referrals in a teaching general hospital. Indian J Psychiatry 1982;24:366-9.
with far reaching clinical and social consequences.[24] 9. Gautam SK. A comprehensive study of patients presenting with somatic
Comparatively, a lot of work has been documented in the symptoms. Dissertation submitted to Bangalore University, Bangalore,
India, 1978.
area of deliberate self harm and suicide in Indian set-up. 10. Avasthi A, Sharan P, Kulhara P, Malhotra S, Varma VK. Psychiatric
One critical finding by R.K. Chadda and S. Shome (1996) is profiles in medical-surgical populations: need for a focused approach to
that psychiatric consultation services are not sufficiently consultation-uaison psychiatry in developing countries. Indian J Psychiatry
1998;40:224-30.
utilized by a large number of clinicians.[25] Most of them felt 11. Sethi BB, Gupta SC. An analysis of 2000 private hospital psychiatric
the need to improve upon undergraduate medical education patients. Indian J Psychiatry 1972;14:197-200.
12. Vahia NS, Doongaji DR, Jeste DV. Twenty five years of psychiatry in a
in psychiatry in India as well as a desire to have consultation teaching hospital (in India). Indian J Psychiatry 1974;13:253-7.
- liaison psychiatric units in India. In an interesting study 13. Khanna BG, Wig NN, Varma VK. General hospital psychiatric clinic an
by P. Gopala Sarma (2000), on patients attending general epidemiological study. Indian J Psychiatry 1974;16:211-20.
14. Wig NN, Shah DK. Psychiatric unit in a general hospital in India: patterns
hospital psychiatry out-patient (OP), the cost of one visit of inpatient referrals. J Indian Med Assoc 1973;60:83-6.
was Rs. 201. The management’s contribution to the total 15. Krishnamurthy S, Shamasunder C, Prakash O, Prabhakar N. Psychiatric
morbidity in general practice, a preliminary report. Indian J Psychiatry
expenditure was 68% and patients’ 32%. Salaries accounted 1981;23:40-3.
for the maximum - 48%. This was followed by loss of earnings 16. Sriram TG, Shamasunder C, Mohan KS, Shanmugham V. Psychiatric
morbidity in the medical outpatients of a general hospital. Indian J
-17%. Drugs accounted for less than 10%.[26] Psychiatry 1986;28:325-8.
17. Murthy RS. Editorial, emerging aspects of psychiatry in India. Indian J
Liaison Psychiatry has brought the emphasis on the teaching Psychiatry 1998;40:307-10.
18. Bhogale GS, Katte RM, Heble SP, Sinha UK, Paul BA. Psychiatric referrals
of psychosocial aspects of medicine in diverse manners like in multispeciality hospital. Indian J Psychiatry 2000;42:188-94.
bedside interviews, interdepartmental case conferences. 19. Wig NN. Psycho-Social Aspects of Family Planning. Indian J Psychiatry
1968;10:30-2.
Research possibilities are unlimited. There are many 20. Mathur RS. Psychiatric morbidity in soldiers hospitalised for physical
examples of psycho geriatric clinics and memory clinics in ailments. Indian J Psychiatry 1977;19:39-96.
operation in general hospital psychiatry set-ups in India 21. Vlrmanl V, Devi MG, Sawhneys B. B psychiatric symptoms in organic brain
disease. Indian J Psychiatry 1967;9:211.
and data from these set-ups will be useful in guiding these 22. Dash S, Dash S. A comparative study of acceptors and rejectors of
special services. Numerous studies on the psychosocial psychiatric referrals for medical termination of pregnancy. Indian J
Psychiatry 1977;19:39-96.
aspects of physical illness and new medical and surgical 23. Kala AK, Kala R, Bathia JC. Changing sociodemographic and clinical
procedures, such as chronic hemodialysis, open heart profile of patients attending a general hospital psychiatric clinic: some
indications of community acceptance. Indian J Psychiatry 1981;22:86-91.
surgery, organ transplantation doctor-patient relationship; 24. Chandra PS. The interface between psychiatry and women’s reproductive
stress and coping strategies; psychological antecedents of and sexual health. Indian J Psychiatry 2001;43:295-305.
illness and many other relevant clinical problems have been 25. Chadda RK, Shome S. Psychiatric aspects of clinical practive in general
hospitals: a survey of non-psychiatric clinicians. Indian J Psychiatry
carried out.[3] In all probability, an even more important 1996;38:86-93.
need of research in the area of liaison psychiatry is to put 26. Sarma GP. General hospital psychiatry: cost of one visit. Indian J
Psychiatry 2000;42:258-61.
together a “client profile” and develop tailor made services
in the most advantageous way. It is acknowledged that
Source of Support: Nil, Conflict of Interest: None declared
these services are acceptable to people and there by will
S388 Indian J Psychiatry 52, Supplement, January 2010
View publication stats
Das könnte Ihnen auch gefallen
- 2014 Karetal Indian JPsychiatryDokument9 Seiten2014 Karetal Indian JPsychiatryPeteNoch keine Bewertungen
- Training Models in IndiaDokument9 SeitenTraining Models in Indiakimxyx.dNoch keine Bewertungen
- Dalal, Ajit K. - Misra, Girishwar - New Directions in Health Psychology PDFDokument503 SeitenDalal, Ajit K. - Misra, Girishwar - New Directions in Health Psychology PDFeinsteinNoch keine Bewertungen
- Dalal & MishraDokument491 SeitenDalal & MishraKarthika M TharakanNoch keine Bewertungen
- Oedipus The Deep Rooted Reality To HomosexualityDokument136 SeitenOedipus The Deep Rooted Reality To HomosexualitySonali DeNoch keine Bewertungen
- Estern Journal of PsychiatryDokument124 SeitenEstern Journal of PsychiatryDr. Ranjan KumarNoch keine Bewertungen
- Reducing Adolescents Mental Stress Via Motivational Role Key PDFDokument151 SeitenReducing Adolescents Mental Stress Via Motivational Role Key PDFNazeer AhmadNoch keine Bewertungen
- VASPIJP2020Dokument12 SeitenVASPIJP2020ShreeNoch keine Bewertungen
- (Sasikala & Karunanidhi, 2011) - TerkunciDokument196 Seiten(Sasikala & Karunanidhi, 2011) - TerkunciNanda Tri UtamaNoch keine Bewertungen
- IndianJPsychiatry 2020 62 5 603 297769Dokument3 SeitenIndianJPsychiatry 2020 62 5 603 297769Hemangi NarvekarNoch keine Bewertungen
- Adi ShankaracharyaDokument10 SeitenAdi ShankaracharyaDinabandhu BeheraNoch keine Bewertungen
- Clinical Psy Training 2015Dokument10 SeitenClinical Psy Training 2015Tejaswi BlsNoch keine Bewertungen
- IPS CPG GuidelineDokument148 SeitenIPS CPG GuidelineSanketNoch keine Bewertungen
- Adi ShankaracharyaDokument10 SeitenAdi Shankaracharyashansesh001Noch keine Bewertungen
- Consensus Statement From Editors of Psychiatry Journals Singh IJP-23Dokument5 SeitenConsensus Statement From Editors of Psychiatry Journals Singh IJP-23JagadishaThirthalliNoch keine Bewertungen
- List of Books AvailableDokument2 SeitenList of Books AvailableVaibhav Bhatia100% (1)
- Development of Psychological Thought in IndiaDokument5 SeitenDevelopment of Psychological Thought in IndiaVikas SamotaNoch keine Bewertungen
- Effectiveness of Cognitive Behavioural and Relational Approaches in Sexual Disorder 60-69Dokument100 SeitenEffectiveness of Cognitive Behavioural and Relational Approaches in Sexual Disorder 60-69iswarya vellaisamyNoch keine Bewertungen
- Introducing Indian PsychologyDokument18 SeitenIntroducing Indian PsychologyJuan Luis Köstner MartinoNoch keine Bewertungen
- Manyaprad Article 2018Dokument140 SeitenManyaprad Article 2018Sowmit JoydipNoch keine Bewertungen
- Online Journal of Multidisciplinary Research, Vol 1Dokument27 SeitenOnline Journal of Multidisciplinary Research, Vol 1Gaurav AgrawalNoch keine Bewertungen
- IndianJPsychiatry 2019 61 4 423 262795Dokument3 SeitenIndianJPsychiatry 2019 61 4 423 262795sina giahkarNoch keine Bewertungen
- IJCPDokument84 SeitenIJCPArchana SharmaNoch keine Bewertungen
- Rorschach Profile of Indian Adults: July 2010Dokument17 SeitenRorschach Profile of Indian Adults: July 2010Suresh Lukose100% (1)
- Proposalto IPSfor Addiction Speciality Subsection 3Dokument10 SeitenProposalto IPSfor Addiction Speciality Subsection 3faradayzzzNoch keine Bewertungen
- JSA Article2010Dokument10 SeitenJSA Article2010Sagar SharmaNoch keine Bewertungen
- ISSN 2231-3265 International Journal of Health, Physical Education and Computer Science in Sports Volume No.2, No.1Dokument153 SeitenISSN 2231-3265 International Journal of Health, Physical Education and Computer Science in Sports Volume No.2, No.1Nurul ElnicaNoch keine Bewertungen
- IndianJPsychiatry 2019 61 4 423 262795Dokument2 SeitenIndianJPsychiatry 2019 61 4 423 262795gion.nandNoch keine Bewertungen
- Neuropsychology in IndiaDokument16 SeitenNeuropsychology in IndiaRahula RakeshNoch keine Bewertungen
- DPLDokument212 SeitenDPLkumarrajeev86Noch keine Bewertungen
- Mental Health Professionals MaharashtraDokument79 SeitenMental Health Professionals Maharashtraakash gaikwadNoch keine Bewertungen
- Evalution of Efficacy of Jatamansi Tail Shirodhara in Anidra Primary InsomniaDokument7 SeitenEvalution of Efficacy of Jatamansi Tail Shirodhara in Anidra Primary InsomniaPRASHANSA SINGHNoch keine Bewertungen
- UntitledDokument72 SeitenUntitledKamaldeep SinghNoch keine Bewertungen
- Caregiver Burden A NG Quality of LlfeDokument64 SeitenCaregiver Burden A NG Quality of LlfeMayesha RohellaNoch keine Bewertungen
- 34 Jan 2011 PDFDokument136 Seiten34 Jan 2011 PDFNikita JoshiNoch keine Bewertungen
- Ancient, Medieval and ModernDokument22 SeitenAncient, Medieval and ModernArastu PathakNoch keine Bewertungen
- Ayush MinistryDokument7 SeitenAyush MinistryGaming ZoneNoch keine Bewertungen
- Koneru Ramakrishna Rao - Wikipedia, The Free EncyclopediaDokument3 SeitenKoneru Ramakrishna Rao - Wikipedia, The Free EncyclopediahelloyvnNoch keine Bewertungen
- Social Modernity Asian Journal of Social Sciences Vol. 3, 1-2, 2013 PDFDokument5 SeitenSocial Modernity Asian Journal of Social Sciences Vol. 3, 1-2, 2013 PDFProf. Vibhuti PatelNoch keine Bewertungen
- Indian Journal of Clinical Psychology: EditorialDokument92 SeitenIndian Journal of Clinical Psychology: EditorialravibhargavaraamNoch keine Bewertungen
- Indian Psy-1Dokument6 SeitenIndian Psy-1जीवन sutraNoch keine Bewertungen
- 2014 FBDokument93 Seiten2014 FBtim radellNoch keine Bewertungen
- Psychology PDFDokument8 SeitenPsychology PDFRahul sharmaNoch keine Bewertungen
- IPSCPGSUDSynopsisBook2015 PDFDokument130 SeitenIPSCPGSUDSynopsisBook2015 PDFSarbartha PramanikNoch keine Bewertungen
- The International Journal of Indian Psychology Volume 1-Issue-2Dokument119 SeitenThe International Journal of Indian Psychology Volume 1-Issue-2The International Journal of Indian PsychologyNoch keine Bewertungen
- International Ayurvedic Medical Journal: Anitta Rajpuria M.R. Sajjan Shetty Varun RajpuriaDokument8 SeitenInternational Ayurvedic Medical Journal: Anitta Rajpuria M.R. Sajjan Shetty Varun RajpuriaJabidur RahmanNoch keine Bewertungen
- Book Chapter FormatDokument2 SeitenBook Chapter FormatilfmsNoch keine Bewertungen
- Ganss-2 1Dokument396 SeitenGanss-2 1srinipk1935Noch keine Bewertungen
- Study of Sallekhana in 21st CenturyDokument5 SeitenStudy of Sallekhana in 21st CenturyprembiswasNoch keine Bewertungen
- Rosescon 2014 Program FinalDokument7 SeitenRosescon 2014 Program Finalapi-248412135Noch keine Bewertungen
- JOA-XII-October - December-2018-4f4ay9OBo6ShtirVV PDFDokument144 SeitenJOA-XII-October - December-2018-4f4ay9OBo6ShtirVV PDFsillypoloNoch keine Bewertungen
- A Practical Handbook of Pancha Karma ProceduresDokument92 SeitenA Practical Handbook of Pancha Karma ProceduresHari100% (1)
- Social Work Book 2Dokument2 SeitenSocial Work Book 2Amutha VijeyNoch keine Bewertungen
- ABSTRACTDokument1 SeiteABSTRACTzhwakaylaNoch keine Bewertungen
- An Analysis of Dhatu-Varga in Bhava Prakasha Nighantu: July 2017Dokument16 SeitenAn Analysis of Dhatu-Varga in Bhava Prakasha Nighantu: July 2017Bhavyata AdminNoch keine Bewertungen
- 3BB 253 DrrohitsharmaDokument8 Seiten3BB 253 DrrohitsharmaRia SikderNoch keine Bewertungen
- Tantrapu Pāñjali: Tantric Traditions and Philosophy of KashmirDokument4 SeitenTantrapu Pāñjali: Tantric Traditions and Philosophy of KashmirGuilherme PereiraNoch keine Bewertungen
- Unit 25 AdminstrationDokument31 SeitenUnit 25 AdminstrationJennifer Dixon80% (5)
- SICA - MARCO Ingles WebDokument48 SeitenSICA - MARCO Ingles WebDivya ThomasNoch keine Bewertungen
- Care Plan On Acute Transient Psychiatric Disorder 2Dokument4 SeitenCare Plan On Acute Transient Psychiatric Disorder 2Divya ThomasNoch keine Bewertungen
- Mmse 1Dokument4 SeitenMmse 1Divya ThomasNoch keine Bewertungen
- Handing and Taking OverDokument8 SeitenHanding and Taking OverDivya ThomasNoch keine Bewertungen
- Divya Summer Field Project Report 1Dokument76 SeitenDivya Summer Field Project Report 1Divya ThomasNoch keine Bewertungen
- Death and GrievingDokument58 SeitenDeath and GrievingDivya ThomasNoch keine Bewertungen
- Eq Test PDFDokument16 SeitenEq Test PDFThu Trang Ngo ThiNoch keine Bewertungen
- Bipo Care PlanDokument5 SeitenBipo Care PlanDivya ThomasNoch keine Bewertungen
- Appendix 1 Emotional Intelligence QuestionnaireDokument7 SeitenAppendix 1 Emotional Intelligence QuestionnaireDivya ThomasNoch keine Bewertungen
- Psychological Interventions For Managing Postpartum Psychosis: A Qualitative Analysis of Women 'S and Family Members' Experiences and PreferencesDokument17 SeitenPsychological Interventions For Managing Postpartum Psychosis: A Qualitative Analysis of Women 'S and Family Members' Experiences and PreferencesDivya ThomasNoch keine Bewertungen
- Bill 2Dokument1 SeiteBill 2Divya ThomasNoch keine Bewertungen
- District Hospitals Guidelines For DevelopmentDokument199 SeitenDistrict Hospitals Guidelines For DevelopmentindroxNoch keine Bewertungen
- Personality Disorders: Abnormal Psychology, Thirteenth EditionDokument39 SeitenPersonality Disorders: Abnormal Psychology, Thirteenth EditionDivya ThomasNoch keine Bewertungen
- Income Statement: The Star Logo, and South-Western Are Trademarks Used Herein Under LicenseDokument24 SeitenIncome Statement: The Star Logo, and South-Western Are Trademarks Used Herein Under LicenseAlaa' Deen ManasraNoch keine Bewertungen
- Prevention of Domestic Violence Against Women and Children in Low-Income and Middle-Income CountriesDokument9 SeitenPrevention of Domestic Violence Against Women and Children in Low-Income and Middle-Income CountriesDivya ThomasNoch keine Bewertungen
- Health Care in Developing Countries: Challenges and OpportunitiesDokument40 SeitenHealth Care in Developing Countries: Challenges and OpportunitiesMainak MukherjeeNoch keine Bewertungen
- Macudatailor MadeprofitandlossstatementDokument13 SeitenMacudatailor MadeprofitandlossstatementDivya ThomasNoch keine Bewertungen
- Financial Statements TemplateDokument19 SeitenFinancial Statements TemplateAbdullahTufailNoch keine Bewertungen
- Measuring Emotional Intelligence of University StuDokument5 SeitenMeasuring Emotional Intelligence of University StuDivya ThomasNoch keine Bewertungen
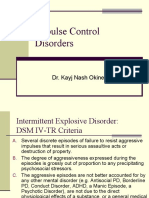
- Impulse Control Disorders: Dr. Kayj Nash OkineDokument18 SeitenImpulse Control Disorders: Dr. Kayj Nash OkineDivya ThomasNoch keine Bewertungen
- 6th Central Pay Commission Salary CalculatorDokument15 Seiten6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Alcohol Related DDokument95 SeitenAlcohol Related DDivya ThomasNoch keine Bewertungen
- Influenceofinterventionon EIDokument5 SeitenInfluenceofinterventionon EIDivya ThomasNoch keine Bewertungen
- Nursing Atlas 2007Dokument76 SeitenNursing Atlas 2007Vaishnavi JayakumarNoch keine Bewertungen
- Alcohol Related DDokument95 SeitenAlcohol Related DDivya ThomasNoch keine Bewertungen
- Anger ManagementDokument24 SeitenAnger ManagementAnjum QureshiNoch keine Bewertungen
- Thesis PDFDokument113 SeitenThesis PDFDivya ThomasNoch keine Bewertungen
- Psychiatric Disability AssessmentDokument19 SeitenPsychiatric Disability AssessmentDivya ThomasNoch keine Bewertungen
- By Hareviswan Amizhthiniyan Yogesh Sathyaseelan Aakash G: Circle Birmingham / Bryden WoodDokument15 SeitenBy Hareviswan Amizhthiniyan Yogesh Sathyaseelan Aakash G: Circle Birmingham / Bryden WoodHAREVISWAN R (RA1911201010031)Noch keine Bewertungen
- DSWD Programs and ServicesDokument12 SeitenDSWD Programs and ServicesKathryn Krystal R Lanuza100% (2)
- Early Detection and Intervention of Autism Spectrum DisorderDokument7 SeitenEarly Detection and Intervention of Autism Spectrum DisorderIgnacio WettlingNoch keine Bewertungen
- Exhibit - 1 Declaration of Allison Gilbert, M.D.Dokument23 SeitenExhibit - 1 Declaration of Allison Gilbert, M.D.File 411Noch keine Bewertungen
- David Fetterer ResumeDokument3 SeitenDavid Fetterer ResumedfettererNoch keine Bewertungen
- Avrutavata and Its ChikitsaDokument3 SeitenAvrutavata and Its ChikitsaSamhitha Ayurvedic ChennaiNoch keine Bewertungen
- Clinical Teams Mental Health ManualDokument18 SeitenClinical Teams Mental Health Manualapi-609422028Noch keine Bewertungen
- Jurnal Ketepatan Kode Ketileng PDFDokument14 SeitenJurnal Ketepatan Kode Ketileng PDFDiah Ayu KartikasariNoch keine Bewertungen
- Leg EdemaDokument13 SeitenLeg Edemacamila perillaNoch keine Bewertungen
- Formulation and Sensory Evaluation of Nutritionally Adequate Saba BananaDokument17 SeitenFormulation and Sensory Evaluation of Nutritionally Adequate Saba BananaJoyce D. FernandezNoch keine Bewertungen
- Jurnal - Mochammad Faqih FatchurDokument11 SeitenJurnal - Mochammad Faqih FatchurMochammad FaqihNoch keine Bewertungen
- Online Activity Week 2Dokument3 SeitenOnline Activity Week 2Caryl Marie Rabang86% (7)
- The Diagnoses of Community NursingDokument8 SeitenThe Diagnoses of Community NursingIOSRjournalNoch keine Bewertungen
- SOPDokument2 SeitenSOPNIGEL SAANANoch keine Bewertungen
- The BioCassava Plus Program Biofortification of CaDokument24 SeitenThe BioCassava Plus Program Biofortification of CaNodir PazNoch keine Bewertungen
- Interprofessional Collaboration IDokument10 SeitenInterprofessional Collaboration IRia Qadariah AriefNoch keine Bewertungen
- Evaluation and Management of GlossectomyDokument54 SeitenEvaluation and Management of GlossectomyKUNNAMPALLIL GEJO JOHNNoch keine Bewertungen
- Nutrition ScienceDokument13 SeitenNutrition ScienceOWAISNoch keine Bewertungen
- Respiratory Sounds: by Oluwaseun OlaiyaDokument16 SeitenRespiratory Sounds: by Oluwaseun OlaiyaOlaiya OluwaseunNoch keine Bewertungen
- Gowrishankar Potturi: B.P.T, M.PT, M.I.A.P, M.I.A.C.PDokument24 SeitenGowrishankar Potturi: B.P.T, M.PT, M.I.A.P, M.I.A.C.PMuhammad Luqmanulhakim Abu Bakar100% (1)
- CSS 21st CenturyDokument74 SeitenCSS 21st CenturyMARSON ASUNCIONNoch keine Bewertungen
- Patients ' Views of Wearable Devices and Ai in Healthcare: Findings From The Compare E-CohortDokument8 SeitenPatients ' Views of Wearable Devices and Ai in Healthcare: Findings From The Compare E-CohortPratush RajpurohitNoch keine Bewertungen
- Dispensing 1 MCQ 2BDokument22 SeitenDispensing 1 MCQ 2Bsybyl formentera100% (1)
- Action ResearchDokument27 SeitenAction Researchreymarie hermosillaNoch keine Bewertungen
- Science: ObjectiveDokument3 SeitenScience: ObjectiveOnguene Syntia100% (1)
- FCC 2018 Mopup Vacancy 270219Dokument50 SeitenFCC 2018 Mopup Vacancy 270219Anish H DaveNoch keine Bewertungen
- MTB Second Edition Step 3 ErrataDokument9 SeitenMTB Second Edition Step 3 ErrataDaniel I. SullivanNoch keine Bewertungen
- Medical Admission Proforma: Hospital Name Patient DetailsDokument11 SeitenMedical Admission Proforma: Hospital Name Patient DetailsAngelus129Noch keine Bewertungen
- MuetDokument2 SeitenMuetcheeNoch keine Bewertungen
- Nursing Process in CommunityDokument8 SeitenNursing Process in CommunityFahim Ahmed100% (1)