Beruflich Dokumente
Kultur Dokumente
142 Ethics Project
Hochgeladen von
Grace Van BeekCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
142 Ethics Project
Hochgeladen von
Grace Van BeekCopyright:
Verfügbare Formate
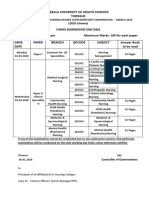
The Impact Hand Sanitizer and Face Covering Purchases has had on
Nurses During COVID-19
Taylor James, Zoie Gainey, Carly Kubiak, Carly Davis, Maddy Mazer, Tobi Poole, Angela Pumford, Olivia Eichman
We chose this topic
Masks and because wearing face
hand-sanitizers coverings and using
are essential for hand sanitizer has
nurses to become very prevalent in
perform safe, our lives and will
quality continue to be as we
patient-centered become nurses.
care.
Background
● When the pandemic started, face masks and hand sanitizer were becoming harder to find and
obtain.
● China was manufacturing a lot of masks and stopped sending them to the US when the pandemic
started.
● The US’s own supply of masks ran very low very fast.
● Masks were discouraged at first because it was taking away from healthcare providers
● Medical professionals were put at risk because of the decrease in supplies.
● The public was bulk buying these supplies and largely impacting the nurses in the hospitals.
● At first people were unsure if face masks worked, but over time research proved they do in fact
stop the spread
● Hand hygiene is a necessity for healthcare workers to stop the spread of deadly germs- this
includes alcohol based hand sanitizer
Masks
● N-95 masks are the best masks to stop the spread of the virus. N-95 masks are able to filter 95%
of small particles in the air. The Covid-19 virus has been shown to spread through the inhalation
of airborne droplets spread by coughing, sneezing, or even just speaking.
● When a N-95 mask is not available, the CDC advised people to wear a standard surgical mask or
even a cloth mask or scarf as a face covering
● Some states require masks in public settings, yet some states have still not mandated
○ The difficult part of these mandates is that not all people cooperate
● When the pandemic first started affecting the US heavily
in early March of 2020, people panicked and bought out all
the masks available in the stores, causing a shortage of masks for
nurses and healthcare professionals...
The Impact of the Mask Shortage
● Nurses and other healthcare professionals require multiple masks a day, more so during
pandemic
● At the beginning of the pandemic, people purchased more PPE than they needed, causing a
shortage for those who actually needed it, especially nurses and healthcare workers
○ N-95s, the most protective masks, were being bought by people who did not need them
more than healthcare workers
● Priority list leads to direct exposure to COVID-19 which could
lead to decrease in workers and people willing to work
● With the shortage of masks, people had to learn to improvise
Helping Hands
● With limited supplies, people started to make masks
● Substitutes like scarves and bandanas were also used
● Tutorials came out online so anyone could participate
● At the height of the shortage, some groups like the Masked Warrior Project could
create hundreds of masks a day for donations to healthcare workers
Sarah Roffman of Masked Warrior Project
Hand Sanitizer
● Coronavirus is spread through the air and surfaces, so good hand hygiene is helpful in preventing transmission
of the virus.
● Because we don’t always have access to running water, the best alternative is alcohol-based hand sanitizer.
● The World Health Organization (WHO) researchers exposed SARS-CoV-2 virus particles to 2 recommended
formulas of hand sanitizer. Both formulations inactivated the virus.
● Effective hand sanitizer needs to be composed of at least 30% concentration vol/vol of either ethanol or
isopropanol.
When there’s not a sink, use hand sanitizer! It’s
convenient and gets the job done.
The Impact of the Hand Sanitizer Shortage
● To try and slow the rapid purchasing of hand sanitizer by consumers, a variety of stores (including Publix, Walgreens and Target)
limited hand sanitizer purchasing to 2 containers per person.
● Homemade hand sanitizers made without the necessary skills, equipment, and medical-grade ingredients, however, may not
contain alcohol concentrations high enough to inactivate SARS-CoV-2.
● Vodka is unsuitable for making hand sanitizer, according to Food and Drug Administration (FDA) guidelines, because it is not
the right grade of alcohol.
● Increased risk of infection for both nurses and patients
● Created an unsafe environment for everyone
Slide narrated by:
Carly Davis
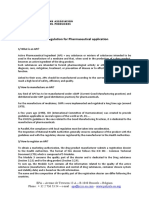
Plan to Advance the Initiative
The Code of Ethics and the Scopes of Practice inform nurses what should be done in order to
protect and advocate for the population to encourage healthy habits and sanitation to slow the
spread of COVID-19:
“Nurses should model the same health maintenance and “Legislative changes have expanded the role of nurses as
health promotion measures that they teach and research, advocates in giving voice to ethical issues for the profession
obtain health care when needed, and avoid taking and those for whom they provide care [...] nurses promote
discussion of patient-centered care, achieve consensus for
unnecessary risks to the health or safety in the course of
decision-making, empower the community to action, and
their professional and personal activities” (p.19). - Provision mentor development of self-care skills based on the
5.2 profession’s responsibility to the health and well-being of
humanity” (p. 33).
“Nurses educate the public; facilitate informed choice;
identify conditions and circumstances that contribute to
illness, injury, and disease; foster healthy lifestyles; and
participate in institutional and legislative efforts to protect
and promote health” (p. 32) - Provision 8.3
Plan to Advance the Initiative
Nurses have strong leadership in the community and in the healthcare system which has been amplified during the COVID-19 pandemic
Patricia Davidson
RN, Dean, Professor Nurses must continue to grow in their leadership. There have been
Johns Hopkins University School of Nursing several leaders come from the nursing profession and cause
“Nurses have to advocate for ourselves and substantial change.
our colleagues”
“Not every system is value driven”
● Ruth Lubic founded the first free-standing birth center in the country in 1975 and
opened the Family Health and Birth Center in 2001 to provide care to underserved
“When there are inadequate resources,
including staffing, we as nurses need to communities.
speak up and advocate for ourselves. We ● In the late 1940s and early 1950s, nurse Elizabeth Carnegie led the fight for the racial
can't take care of our patients or our families integration of nursing in Florida which she successfully accomplished through leading
if we don't also focus on taking care of by example and through her “extraordinary character and organizational skills.”
ourselves” ● Any nurse who reminded his or her colleagues to not contaminate a sterile field or
wash his or her hands because it is protocol to stop the procedure until the task is
“We're reminded that it was Florence finished.
Nightingale, the founder of modern-day
nursing, who popularized the six-foot rule
for infection control.” (Institute of Medicine (US) Committee on the Robert Wood Johnson Foundation Initiative on the Future
of Nursing, 2011)
(LaFave, 2020)
Reference Page
American Nurses Association. (2015). Code of Ethics for Nurses with Interpretive Statements. American Nurses Association.
Nursing : scope and standards of practice. (2015). . [Silver Spring, Maryland]: American Nurses Association.
Centers for Disease Control and Prevention. (2020, February 25). Clean Hands Count for Safe Healthcare. Center for Disease Control and Prevention. https://www.cdc.gov/patientsafety/features/clean-hands-count.html
Centers for Disease Control and Prevention. (2020, January 31). Hand Hygiene in Healthcare Setting. Center for Disease Control and Prevention. https://www.cdc.gov/handhygiene/providers/index.html
Healthcare Hygiene Magazine. (2020, April 16). Nurse Scientist Explains Why Hand Hygiene is Critical for Patients. Healthcare Hygiene Magazine.
https://www.healthcarehygienemagazine.com/nurse-scientist-explains-why-hand-hygiene-is-critical-for-patients/
Institute of Medicine (US) Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing. (2011). Transforming Leadership. In Bensen et al. (Eds.), The Future of Nursing: Leading Change, Advancing Health. National
Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK209867/
Khazan, Olga. (2020, April 10). Why We’re Running Out of Masks. The Atlantic. https://www.theatlantic.com/health/archive/2020/04/why-were-running-out-of-masks-in-the-coronavirus-crisis/609757/
LaFave, S. (2020, May 13). Nurses are leading the COVID-19 response around the globe. HUB for Johns Hopkins University. https://hub.jhu.edu/2020/05/13/patricia-davidson-nursing-covid-19/
McCabe, Caitlin. (2020, August 13). Face Masks Really Do Matter. The Scientific Evidence Is Growing. The Wall Street Journal. https://www.wsj.com/articles/face-masks-really-do-matter-the-scientific-evidence-is-growing-11595083298
Molteni, Megan., & Rogers, Adam. (2020, July 2). How Masks Went From Don’t-Wear to Must-Have. Wired. https://www.wired.com/story/how-masks-went-from-dont-wear-to-must-have/
TodayShow. (2020, April 3). Volunteers work with hospitals to make emergency face masks. https://www.today.com/health/volunteers-sew-homemade-face-masks-hospital-workers-t177079.
Das könnte Ihnen auch gefallen
- Region X: January 1, 2021 Advanced Life Support Standard Operating ProceduresDokument126 SeitenRegion X: January 1, 2021 Advanced Life Support Standard Operating ProceduresC ScribNoch keine Bewertungen
- Innovations in NursingDokument9 SeitenInnovations in NursingAnusha VergheseNoch keine Bewertungen
- Ortopedia Dentofacial Una Vision MultidisciplinariaDokument1 SeiteOrtopedia Dentofacial Una Vision MultidisciplinariaFrancisco Javier GutierrezNoch keine Bewertungen
- Corona Warriors: Submitted By-Devansh Harjai Class - 10 Sec - A3 Roll No - 43Dokument10 SeitenCorona Warriors: Submitted By-Devansh Harjai Class - 10 Sec - A3 Roll No - 43Custom ScreensNoch keine Bewertungen
- Summary and Opinion QuizDokument3 SeitenSummary and Opinion QuizDomingo, Viella Clarisse S.Noch keine Bewertungen
- Challenges Towards Healthcare Nursing Personnel Due To CovidDokument62 SeitenChallenges Towards Healthcare Nursing Personnel Due To CovidMounika BhallamNoch keine Bewertungen
- Chap4 PDFDokument24 SeitenChap4 PDFsameerkariaNoch keine Bewertungen
- Hand Hygiene Edited LatestDokument60 SeitenHand Hygiene Edited Latestfaizal halimNoch keine Bewertungen
- Hygiene Promotion: Chapter-4Dokument24 SeitenHygiene Promotion: Chapter-4JulesNoch keine Bewertungen
- ReportDokument11 SeitenReportapi-441408409Noch keine Bewertungen
- Taking Charge of Nursing PracticeDokument59 SeitenTaking Charge of Nursing PracticeMeia JaycelNoch keine Bewertungen
- The Effectiveness of Using A Sanitizer As A Preventive Measure in CovidDokument11 SeitenThe Effectiveness of Using A Sanitizer As A Preventive Measure in CovidNicole MargaretteNoch keine Bewertungen
- Learning Feedback3Dokument3 SeitenLearning Feedback3Clarence MirandaNoch keine Bewertungen
- Week 1 Introduction To Nursing & Nursing Theory 2020Dokument27 SeitenWeek 1 Introduction To Nursing & Nursing Theory 2020Raghad AlharbiNoch keine Bewertungen
- Nursing Ad React1Dokument2 SeitenNursing Ad React1Alyssa Santos JavierNoch keine Bewertungen
- Nurses Are Playing A Crucial Role in This Pandemic-As AlwaysDokument3 SeitenNurses Are Playing A Crucial Role in This Pandemic-As Alwaysdaniela mendez ortizNoch keine Bewertungen
- IND Toolkit 120320Dokument64 SeitenIND Toolkit 120320Asma RamadhanNoch keine Bewertungen
- Reducing Hand Recontamination of Healthcare Workers During Covid 19Dokument2 SeitenReducing Hand Recontamination of Healthcare Workers During Covid 19Lujine AłsNoch keine Bewertungen
- Chapter 19 - Hand Hygiene - APIC Text OnlineDokument13 SeitenChapter 19 - Hand Hygiene - APIC Text OnlineManalAbdelazizNoch keine Bewertungen
- Using Effective Hand Hygiene Practice To Prevent and Control InfectionDokument6 SeitenUsing Effective Hand Hygiene Practice To Prevent and Control Infectionfarida nur ainiNoch keine Bewertungen
- Human Needs and Personal HygieneDokument3 SeitenHuman Needs and Personal HygieneRohini RaiNoch keine Bewertungen
- ICMHD COVID 19 Notes On MidwiferyDokument8 SeitenICMHD COVID 19 Notes On MidwiferyP17311205009 YULIA YUSTRAENI IRAWANNoch keine Bewertungen
- HBCC Global Campaign Pitch Brief - 0722FINAL PDFDokument35 SeitenHBCC Global Campaign Pitch Brief - 0722FINAL PDFmichael musyimiNoch keine Bewertungen
- Case Study CovidDokument6 SeitenCase Study CovidAngel Faith TirolNoch keine Bewertungen
- Using Effective Hand Hygiene Practice To Prevent and Control InfectionDokument6 SeitenUsing Effective Hand Hygiene Practice To Prevent and Control InfectionerikNoch keine Bewertungen
- Example Literature Review Hand WashingDokument7 SeitenExample Literature Review Hand Washingmtxziixgf100% (1)
- Resources: Let Us Know Your IdeasDokument2 SeitenResources: Let Us Know Your IdeasAngy AroNoch keine Bewertungen
- Lifebuoy Saving Lives With SoapDokument14 SeitenLifebuoy Saving Lives With SoapSnehilNoch keine Bewertungen
- Elective 1&2Dokument26 SeitenElective 1&2Mary Queenie TulinNoch keine Bewertungen
- NursingresponsibilitiesDokument4 SeitenNursingresponsibilitiesEia LaughNoch keine Bewertungen
- Biology ReportDokument15 SeitenBiology ReportThanh Khuê LêNoch keine Bewertungen
- Evolution of NursingDokument6 SeitenEvolution of NursingAmberBrownMcElroyNoch keine Bewertungen
- Community Health Nursing Bag Technique PDFDokument2 SeitenCommunity Health Nursing Bag Technique PDFRachael50% (2)
- Nursing Midwifery and AHP Briefing MARCH ISSUEDokument6 SeitenNursing Midwifery and AHP Briefing MARCH ISSUEHào TrầnNoch keine Bewertungen
- Core Document: Philosophy and Model of Midwifery CareDokument3 SeitenCore Document: Philosophy and Model of Midwifery CareSri GustiniNoch keine Bewertungen
- T.H.I.S: "Mask Movement"Dokument6 SeitenT.H.I.S: "Mask Movement"api-310272078Noch keine Bewertungen
- Arrabaca - Prelim Journal - CPHDokument6 SeitenArrabaca - Prelim Journal - CPHREXINNE GLARIAN ARRABACANoch keine Bewertungen
- ICN Disaster-Comp-Report WEB FinalDokument16 SeitenICN Disaster-Comp-Report WEB FinalSantoNoch keine Bewertungen
- Jurnal Inter7Dokument6 SeitenJurnal Inter7Mhd FirdausNoch keine Bewertungen
- Health For All: Nursing, Global Health and Universal Health CoverageDokument60 SeitenHealth For All: Nursing, Global Health and Universal Health CoverageMukminnasriNoch keine Bewertungen
- GHD 2021 Fact SheetDokument10 SeitenGHD 2021 Fact Sheetnnnn hhhhNoch keine Bewertungen
- Review of Related LiteratureDokument4 SeitenReview of Related LiteraturePopoyNoch keine Bewertungen
- Review of Related LiteratureDokument4 SeitenReview of Related LiteraturePopoyNoch keine Bewertungen
- Review of Related LiteratureDokument4 SeitenReview of Related LiteraturePopoyNoch keine Bewertungen
- Thesis Statement On Hand WashingDokument5 SeitenThesis Statement On Hand Washingkarinathomasdenver100% (2)
- Act 222Dokument9 SeitenAct 222Angeline KimaykimayNoch keine Bewertungen
- Nursing Professional Governance Structure at Yale New Haven HospitalDokument4 SeitenNursing Professional Governance Structure at Yale New Haven HospitalNurulfitrahhafidNoch keine Bewertungen
- Our Lives & The Sciences During and After The Pandemic by Laxmi PrasadDokument8 SeitenOur Lives & The Sciences During and After The Pandemic by Laxmi PrasadLaxmi Prasad BodaNoch keine Bewertungen
- Journal NCM 118 (Lec) Nicolas, Sherena Q. BSN IV-1Dokument15 SeitenJournal NCM 118 (Lec) Nicolas, Sherena Q. BSN IV-1Sherena NicolasNoch keine Bewertungen
- Life in The Pandemic: Some Reflections On Nursing in The Context of COVID-19Dokument3 SeitenLife in The Pandemic: Some Reflections On Nursing in The Context of COVID-19Jordz PlaciNoch keine Bewertungen
- UntitledDokument26 SeitenUntitledSara Mae DungcaNoch keine Bewertungen
- English FinalDokument4 SeitenEnglish FinalSidni JeanNoch keine Bewertungen
- Theme: "Hand Hygiene For All"Dokument8 SeitenTheme: "Hand Hygiene For All"Joven PatricioNoch keine Bewertungen
- The Role of Community Health Nurses During The Pandemic-FinalDokument27 SeitenThe Role of Community Health Nurses During The Pandemic-FinalSri WahyuniNoch keine Bewertungen
- Hand Hygiene Training Toolkit PresentationDokument53 SeitenHand Hygiene Training Toolkit PresentationNoxamLasrevinuNoch keine Bewertungen
- Name of Student Name of Institute: Title of Assignment: Developing An EssayDokument3 SeitenName of Student Name of Institute: Title of Assignment: Developing An EssayBilal asifNoch keine Bewertungen
- October COVID PSADokument2 SeitenOctober COVID PSANewsChannel 9Noch keine Bewertungen
- Modern Nurse Final EditedDokument8 SeitenModern Nurse Final EditedAlli NdahuraNoch keine Bewertungen
- Advocacy For WASH in HCFs Webinar Series WorkbookDokument14 SeitenAdvocacy For WASH in HCFs Webinar Series WorkbookNadine KadriNoch keine Bewertungen
- Ucsp PTDokument4 SeitenUcsp PTKyla TorcatosNoch keine Bewertungen
- The Importance of Hand HygieneDokument5 SeitenThe Importance of Hand HygienePatricia CangNoch keine Bewertungen
- Hospital Acquired PneumoniaDokument48 SeitenHospital Acquired PneumoniaKartika RezkyNoch keine Bewertungen
- UNIT II MedicalDokument34 SeitenUNIT II Medicalangelax1.1Noch keine Bewertungen
- Bipolar Disorder: Bipolar I Disorder - Defined by Manic Episodes That Last at Least 7 Days, or by ManicDokument3 SeitenBipolar Disorder: Bipolar I Disorder - Defined by Manic Episodes That Last at Least 7 Days, or by ManicVincent Paul SantosNoch keine Bewertungen
- Legal Medicine Notes 2020Dokument8 SeitenLegal Medicine Notes 2020Iamharbeyy CastroNoch keine Bewertungen
- Reading ListDokument1 SeiteReading ListNosaaliNoch keine Bewertungen
- UTI Prevention Fact SheetDokument1 SeiteUTI Prevention Fact Sheetalifia alqibtiaNoch keine Bewertungen
- Pott's Disease NCPDokument7 SeitenPott's Disease NCPkristel_nicole18yahoNoch keine Bewertungen
- Stress WorkshopDokument14 SeitenStress Workshopapi-297796125Noch keine Bewertungen
- 4788 ID Faktor Risiko Lingkungan Kejadian Leptospirosis Di Jawa Tengah Studi Kasus Di Ko PDFDokument8 Seiten4788 ID Faktor Risiko Lingkungan Kejadian Leptospirosis Di Jawa Tengah Studi Kasus Di Ko PDFbintang nurzakiahNoch keine Bewertungen
- Kerala University of Health Sciences Thrissur: (2010 Scheme)Dokument1 SeiteKerala University of Health Sciences Thrissur: (2010 Scheme)subiNoch keine Bewertungen
- RetinoblastomaDokument24 SeitenRetinoblastomaMiguel Carlos Navarro Tacderan100% (1)
- HRM Case Study-PatelDokument11 SeitenHRM Case Study-PatelHumaira ShafiqNoch keine Bewertungen
- BMI2018Dokument9 SeitenBMI2018jeffordillasNoch keine Bewertungen
- API Legislation SummaryDokument3 SeitenAPI Legislation SummaryPavan KumarNoch keine Bewertungen
- Profile: Doris A. MendozaDokument4 SeitenProfile: Doris A. MendozaGerarld Immanuel KairupanNoch keine Bewertungen
- AMED3002 - Health Data - 2023 - DeFazioDokument68 SeitenAMED3002 - Health Data - 2023 - DeFazioThomas MarNoch keine Bewertungen
- Hepatites A, B, CDokument22 SeitenHepatites A, B, CsanthiagoschneiderNoch keine Bewertungen
- Helpful Drugs by Class Cheat SheetDokument2 SeitenHelpful Drugs by Class Cheat Sheettflannigan32Noch keine Bewertungen
- Chapter 3Dokument7 SeitenChapter 3vine32515Noch keine Bewertungen
- Nephrotic Syndrome - Nelson+JournalDokument11 SeitenNephrotic Syndrome - Nelson+JournaljeanecalvoNoch keine Bewertungen
- DPN Icu PDFDokument1 SeiteDPN Icu PDFharoonNoch keine Bewertungen
- TX Hosp Based Prac List 120120Dokument975 SeitenTX Hosp Based Prac List 120120David SantosNoch keine Bewertungen
- MLD - Chapter 5Dokument8 SeitenMLD - Chapter 5ann. ssNoch keine Bewertungen
- Skripsi Tanpa Bab PembahasanDokument54 SeitenSkripsi Tanpa Bab PembahasanMissi aslimNoch keine Bewertungen
- Datesheet End Term Exam Dec-2023Dokument34 SeitenDatesheet End Term Exam Dec-2023Neerock KhatriNoch keine Bewertungen
- Comparison of Endoscopic and Surgical Treatment For Acute Cholangitis Caused by CholedocolithiasisDokument12 SeitenComparison of Endoscopic and Surgical Treatment For Acute Cholangitis Caused by CholedocolithiasismonchoellesNoch keine Bewertungen
- Antibabesial Treatment Protocols Against Canine Babesiosis: W.R. Bandula Kumara B.V.SC., PH.DDokument8 SeitenAntibabesial Treatment Protocols Against Canine Babesiosis: W.R. Bandula Kumara B.V.SC., PH.DJehan Somasiri JayathungaNoch keine Bewertungen
- Abdominal TraumaDokument8 SeitenAbdominal Traumahatem alsrour100% (2)