Beruflich Dokumente
Kultur Dokumente
Jurnal Kimed 5
Hochgeladen von
Zilmaida SalomOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Jurnal Kimed 5
Hochgeladen von
Zilmaida SalomCopyright:
Verfügbare Formate
This open-access article is distributed under
Creative Commons licence CC-BY-NC 4.0. IN PRACTICE
CLINICAL UPDATE
Emergency management of calcium channel blocker
overdose
V S Stephen,1,2 MB ChB, MMed (Emergency Medicine), Dip PEC (SA), FCEM (SA); N A Pluymers,1 MB ChB, Dip PEC (SA);
S J Gauton,3 MB ChB, Dip PEC (SA)
1
Emergency Department, Thelle Mogoerane Regional Hospital, Vosloorus, South Africa
2
Division of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
3
Department of Internal Medicine, Thelle Mogoerane Regional Hospital, Vosloorus, South Africa
Corresponding author: V S Stephen (victoria.stephen1@wits.ac.za)
Calcium channel blockers (CCBs) are commonly used in South Africa (SA) in the management of hypertension and other cardiovascular
disease. Their ubiquitous availability makes them a common agent in drug overdose (OD), whether through accidental ingestion or
deliberate self-harm. It is essential that medical practitioners know how to recognise and manage CCB OD, as severe CCB OD is often
fatal. As there is a lack of local literature in SA, we highlight the general principles of management of CCB OD, as well as complications
and problems that may be encountered during treatment. This narrative review is based on existing clinical guidelines, retrospective studies
and systematic reviews on the emergency management of CCB OD. High-dose insulin euglycaemic therapy has become the mainstay of
treatment in severe CCB OD. The rationale, the recommended protocol for its use and its adverse effects are described.
S Afr Med J 2019;109(9):635-638. https://doi.org/10.7196/SAMJ.2019.v109i9.13704
Hypertension is a common disease in Africa. A recent study found a cells that form the cardiac conducting system.[11,13,14] Outside the
prevalence of over 40% throughout the continent.[1] In South Africa cardiovascular system, voltage-gated L-type calcium channels are
(SA), the current prevalence is estimated to be 30.4%.[2] Calcium found in the beta cells of the pancreas, central nervous system and
channel blockers (CCBs) have a prominent role in the management skeletal muscle.[11,13,14]
of hypertension in SA, and are recommended as first-line agents Non-dihydropyridine CCBs are used primarily to treat angina
in black Africans, the elderly, pregnant women, and patients with or cardiac arrhythmias.[11,13] They are lipophilic and have a higher
comorbid diseases such as angina pectoris, peripheral vascular affinity for cardiomyocytes than the dihydropyridine agents, where
disease and carotid atherosclerosis.[2-6] they reduce the influx of calcium during phase two of the action
Drug overdose (OD), whether due to deliberate self-harm or potential.[13-16] Because calcium is not able to enter the cell, excitation
accidental ingestion, is a common patient presentation encountered coupling in these cells cannot occur, resulting in reduced myocardial
in the emergency department (ED).[7,8] Medicine-related poisonings contractility.[15,16] Reduced binding of calcium to the calcium
predominate and are often severe, requiring emergency care.[7-10] channels in the conducting system leads to slowing of sinoatrial and
Medications typically reported are those that are easily accessible or atrioventricular conduction, resulting in bradycardia.[15,16]
are prescribed by healthcare professionals, with prescription drugs The dihydropyridines preferentially affect vascular smooth
identified as being of particular concern in deliberate self-harm.[7] muscle in the periphery at therapeutic dosages, thereby decreasing
Many of these prescription drugs form part of the essential drugs list, peripheral vascular resistance and reducing afterload and lowering
such as CCBs. blood pressure (BP).[11,13] They are therefore excellent agents for the
Owing to the widespread use of CCBs and a high likelihood of their management of hypertension.
being available in SA homes, the risk of OD exists. CCBs are highly
lethal in severe OD if it is not treated promptly and aggressively.[11] Toxicokinetics
Indeed, CCB ODs are responsible for more fatalities than any other Amlodipine and other slow-release CCBs are absorbed from the
cardiovascular agents in the USA, with an estimated 35% mortality gastrointestinal tract slowly, with peak serum concentrations being
rate.[12] As there is a lack of local literature in SA, we highlight the reached within 6 - 12 hours.[11] In OD, peak concentrations may
general principles of management, complications and problems that only be reached at 24 hours.[11,17] It is therefore important to note
may be encountered during treatment. Recommendations are based that patients may appear asymptomatic at the time of presentation,
on available international evidence and current best practice to assist especially when slow-release CCBs are ingested, and then deteriorate
in the emergency management of such cases. 24 hours later.[11] CCBs are primarily metabolised by the cytochrome
P450 system.[17] They are highly protein bound and have a high volume
Pharmacology of distribution, so are not amenable to removal by haemodialysis.[15,17]
CCBs are divided into two main classes, the dihydropyridines (e.g.
amlodipine and nifedipine) and the non-dihydropyridines (e.g. Toxicodynamics and pathophysiology
verapamil and diltiazem).[11] CCBs directly antagonise the voltage- In OD, non-dihydropyridines cause sinus bradycardia, atrio
gated L-type calcium channels, which are found in peripheral ventricular blocks, hypotension and cardiogenic shock.[11,15,17-19] In
vascular smooth muscle, cardiomyocytes and the pacemaker dihydropyridine OD, profound peripheral vasodilation produces
635 September 2019, Vol. 109, No. 9
IN PRACTICE
vasoplegic (distributive) shock.[11,15,17-20] A reflex tachycardia fails history taking should include whether concomitant ingestion with
to occur at toxic doses, as dihydropyridines lose their preferential other medications, poisons, alcohol or illicit drugs has occurred. Beta-
selectivity for peripheral smooth muscle and instead cause blocker co-ingestion is common and requires similar management to
bradycardia and cardiogenic shock.[11,17-20] Dysrhythmias such as CCB OD, as described below.[24]
atrioventricular blocks may also therefore be seen in dihydropyridine CCB toxicity may already be evident on examination on initial
OD.[17,20] The hallmark of CCB OD is therefore circulatory shock due presentation. BP may be normal or low with bradycardia.[11,17] Signs
to bradycardia, poor cardiac contractility and profound peripheral of distributive shock may be present, such as bounding pulses and
vasodilatation. warm peripheries, particularly in dihydropyridine OD.[11,14,17,19] These
In addition, CCBs in OD appear to exert toxic effects on L-type clinical signs should not be mistaken for adequate perfusion. The
calcium channels in the beta cells of the pancreas, preventing insulin patient may have bounding pulses from peripheral vasodilation, so
release. This results in hypoinsulinaemia and insulin resistance, the severity of shock may be underestimated and unrecognised until
causing hyperglycaemia and ketoacidosis.[11,15,17,18] In the unstressed decompensation occurs, whereupon the patient’s haemodynamics may
state, cardiomyocytes utilise free fatty acids as the primary energy deteriorate rapidly.[18] Pulmonary oedema may already be present on
substrate.[17,18] In the stressed state, cardiomyocytes switch to glucose. initial presentation if presentation to hospital was delayed.[13]
It is theorised that the hypoinsulinaemic state induced by CCBs Bedside investigations include a 12-lead electrocardiogram (ECG)
prevents glucose uptake into the cardiomyocytes, starving them of to look for arrhythmias.[11,17,22] Venous blood gas analysis is helpful to
their energy substrate, further impairing cardiac contractility.[17,18] confirm the presence of metabolic acidosis and lactic acidosis,[11,17,18]
The systemic effects of CCB-induced cardiogenic and distributive as well as to check the baseline serum potassium.[25] Females of
shock are myriad. Hypoperfusion of the brain from hypotension reproductive age should have a urine pregnancy test.[26] Pregnant
may cause impairment in consciousness. Occasionally, seizures may patients may require specific treatment, such as being nursed in a left-
occur.[11,17,19] Lactic acidosis develops from the poor perfusion to lateral position to reduce the effects of supine hypotension syndrome
end organs, as well as reduced conversion of lactate to pyruvate in caused by compression of the inferior vena cava by the uterus, which
mitochondria due to reduced entry of calcium into cells.[11,17,18] Acute may further exacerbate the shock induced by CCB OD.[26]
kidney injury occurs as a result of prolonged hypoperfusion and end- A serum paracetamol measurement should be done if concomitant
organ ischaemia.[15] Non-cardiogenic pulmonary oedema may occur medications ingested are not known, as paracetamol is the most
secondary to pulmonary vasodilation and alveolar extravasation common medication used in OD in SA, lacks a clinically detectable
of fluid.[11,15,20] In addition, excessive fluid resuscitation may also toxidrome, and requires specific life-saving management.[27] Other
contribute to its development.[11,13,17,20] serum drug levels should be guided by clinical suspicion.[28]
Management of a CCB OD Specific management in the symptomatic CCB OD
General management, resuscitation and Two intravenous lines should be established promptly, and 20 mL/
decontamination kg crystalloid can be given initially if shock is present.[14,15,17,19,22,24]
Advice from a poisons information centre should be sought if medical Avoid further excessive intravenous fluid administration, as this
staff are unfamiliar with the management of CCB OD.[11,14,18,20] is associated with an increased risk of pulmonary oedema.[11,15,20]
The Western Cape Poison Information Centre helpline is available Central venous access is extremely useful, as all but mild poisonings
24 hours a day.[21] General resuscitation measures should be started will require multiple infusions to run simultaneously, and frequent
without delay, which include supplemental oxygen, establishment of blood gas monitoring is required.[25] Access should be obtained as
reliable intravenous access and basic haemodynamic monitoring in soon as feasible.
the form of heart rate, BP and oxygen saturation.[11,22] This should be Thirty to sixty millilitres of 10% calcium gluconate or 10 - 20 mL
done in a closely monitored area, such as the resuscitation area of the 10% calcium chloride may be given intravenously over 10 - 20 minutes,
ED.[14,18,22] Endotracheal intubation and ventilation may be necessary although clinical evidence of improvement is limited. [11,14,15,17-19,22,24]
in severe poisonings where coma and cardiorespiratory failure Atropine in 0.5 - 1 mg boluses intravenously, up to a maximum of
occur.[11,13] Non-cardiogenic pulmonary oedema can occur in severe 3 mg, may be tried for CCB-induced bradycardia. [14] Glucagon has no
poisonings, requiring ventilatory support.[11,13,17] Close monitoring proven role in CCB OD, although it may be of benefit in beta-blocker
should be continued in the ED until the patient has been transferred ODs if sufficient quantities can be sourced.[11,14,18,24]
to an intensive care unit (ICU) or high-care setting, as a patient may Patients with signs of shock such as mean arterial pressure (MAP)
deteriorate precipitously.[11,17,22] <65 mmHg or lactic acidosis despite initial fluid resuscitation should
If a potentially life-threatening OD of a sustained-release CCB be started on an adrenergic agent.[12,14,15,17-19,22,24] In the SA setting,
has occurred and the patient has presented within 2 hours of adrenaline is most commonly available. Adrenaline has positive
ingestion, activated charcoal 1 g/kg may be given orally to reduce inotropic and chronotropic effects as well as vasopressor effects in
systemic absorption of the CCB.[14,17,22] Activated charcoal should higher doses.[14,17] The dosage range for infusion is between 0.05
only be given in fully awake patients who can protect their airway and 1 µg/kg/min, aiming for improvement in haemodynamics and
or via a nasogastric tube after the patient has been intubated with an perfusion.[14] A good starting point for a hypotensive patient with
endotracheal tube.[14,17,18,22] CCB OD is 0.5 µg/kg/min, which can be up- or down-titrated to
The time of ingestion and the number of tablets ingested should effect. Dopamine is generally not recommended.[22] In severely
be sought. A potentially life-threatening OD varies depending on shocked patients with CCB poisoning, adrenergic agents such as
the type of CCB ingested. The exact toxic dose for each has not adrenaline may not reverse shock adequately.[14,17,19,29-31]
been fully established. However, it is recommended that patients
are monitored for toxicity if >0.3 mg/kg of amlodipine is ingested High-dose insulin euglycaemic therapy
in children,[23] and if >10 mg is ingested by an adult. Asymptomatic If the patient is not demonstrating haemodynamic improvement with
patients should be observed for 24 hours in a monitored setting if adrenaline, high-dose insulin euglycaemic therapy (HIET) should be
a sustained-release preparation has been ingested.[11,14,22] Further initiated while the vasopressor infusion is continued.[13,14,17,22] There is
636 September 2019, Vol. 109, No. 9
IN PRACTICE
no evidence to recommend a specific timeframe, although initiating rate of HIET should be increased up to the maximum dose if shock
HIET 15 minutes after the vasopressor infusion has shown no persists.[11,14,17,18,22,24] In case reports, rates of up to 22 IU/kg/h have
improvement may be reasonable. Delayed HIET has been associated been used safely and effectively.[14,24] Target haemodynamic parameters
with increased mortality.[17,18,24,30] include MAP >65 mmHg,[30] systolic BP >90 mmHg and urine output
There are no randomised controlled studies in humans comparing 1 - 2 mL/kg in adults.[18,25] Higher MAPs and systolic BPs may be
adrenergic agents with HIET, but animal studies and case studies considered in patients known to have poorly controlled hypertension.
in humans consistently show HIET to be superior to adrenergic At the same time as the loading dose of short-acting insulin,
agents in terms of haemodynamic effects in severe CCB OD and a loading dose of 1 mL/kg of 50% dextrose water is given.[14,17,22]
shock. [14,17,18,24,25,29-32] HIET has been shown to restore haemo A 10% dextrose infusion should be commenced to maintain
dynamic stability where high doses of multiple vasopressors have normoglycaemia, and fingerprick glucose testing should be done
failed. [11,14,15,18,19,29,30] In multiple case studies it has been demonstrated 30 minutes after HIET is started and hourly thereafter.[11,14,17,23]
that when HIET was initiated in CCB-induced shock, it was possible Higher concentrations of dextrose water, for example 50%, may be
to wean patients off the high-dose vasopressors they had previously required.[25] However, hyperglycaemia despite high doses of HIET can
required.[13-15,18,19,31] For this reason, HIET is increasingly being occur[24,25] and may indicate the severity of CCB poisoning.[17]
advocated for consideration as first-line therapy,[18,19,25,30,31] although Intravenous potassium replacement should also be commenced
further evidence is required to make this standard practice. once the serum potassium level is <3.5 mmol/L, similar to the
The effect of HIET is usually seen 1 hour after initiation,[11,14,17,18,24] management of diabetic ketoacidosis.[11,14,24,25] A recommended
so adrenaline should be continued until the patient’s haemodynamics infusion rate for potassium can be found in the accompanying HIET
have normalised. HIET should not be delayed until ICU admission, protocol (see box).
as delayed HIET has been associated with increased mortality, as The rationale for HIET should be thoroughly explained to medical
mentioned above.[17,18,24,30] and nursing staff looking after the patient, as the high doses required
The mechanism for the efficacy of HIET, also known as high- may be assumed to be a drug error and stopped, leading to worsened
dose insulin therapy, is not fully understood. Its efficacy may be haemodynamic instability and death.[18,25,31]
explained in three ways. Firstly, insulin acts as a catecholamine- Patients require intensive care or high-care admission owing
independent inotrope directly on cardiomyocytes.[17,25,31] Secondly, to the intensive monitoring and multiple infusions they may
insulin enables the uptake of glucose into cardiomyocytes, which require. [11,18,22] Transfer to an ICU may occur provided that the patient
is the heart’s preferred energy substrate during stress.[17,18,25,30,31] is haemodynamically stable enough to tolerate transport out of the
Since CCBs in OD produce a hypoinsulinaemic state, glucose ED. Transfer to another hospital capable of providing ICU facilities
uptake into the cardiomyocytes cannot occur, impairing cardiac may be required if the patient initially presents to a facility lacking
contractility. Exogenous high-dose insulin and supplemental glucose these resources.
therefore enable uptake of glucose and therefore improve myocardial
contractility.[17,18] Finally, insulin acts as a peripheral vasodilator Complications during treatment
reducing afterload, which improves systemic perfusion.[30,31] In the Hypokalaemia and hypoglycaemia are two expected complications
coronary arteries, this vasodilatory effect improves perfusion and of HIET and must be monitored for and treated diligently.[11,14,17,22-25]
oxygen delivery to the heart, improving inotropy.[25,30,31] Hypokalaemia and hypoglycaemia are not indications to stop HIET
HIET is commenced with a loading dose of 1 IU/kg short-acting if haemodynamic stability has not yet been achieved. Hypokalaemia
insulin intravenously[11,14,17,22,24,25,30,31] (see ‘Practical tips’ box). An is common and seldom life threatening provided that potassium
infusion of insulin is commenced simultaneously, ranging from 1 IU/ replacement is continued during HIET and serial serum potassium
kg/h to 10 IU/kg/h, aiming for haemodynamic stability.[17,22,25] The monitoring is done.[14,18,24] Venous blood gas monitoring is done at
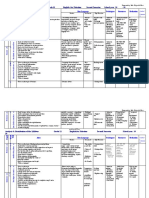
Practical tips for managing calcium channel blocker overdose
Western Cape Poison Information Centre 24-hour helpline: 0861-555-777 or (021) 938-4497
Recommended high-dose insulin euglycaemic therapy protocol
1. Loading dose of 50% dextrose 1 mL/kg intravenously.
2. Loading dose of short-acting insulin 1 IU/kg intravenously.
3. Mix insulin infusion: Withdraw 20 mL from 200 mL 0.9% saline bag. Insert 2 000 IU of short-acting insulin into the bag. Concentration
is 10 IU/mL. Start infusion at 1 IU/kg/h.
4. Commence 10% dextrose water infusion to maintain normoglycaemia. This may be changed to a 50% dextrose infusion if required. The
rate of dextrose is titrated based on hourly fingerstick glucose measurements. Administer 1 mL/kg 50% dextrose if blood glucose <3
mmol/L.
5. Check fingerstick glucose 30 minutes after infusion is commenced. Continue to check hourly thereafter.
6. Do venous blood gas analysis on arrival and then 4 - 6-hourly.
7. Start potassium chloride infusion if serum potassium is <3.5 mmol/L, aiming for a serum potassium level of 2.8 - 4.5 mmol/L.
Recommended rate 10 mmol/h, maximum rate 20 mmol/h.[34] Potassium infusions should run through a central line to avoid phlebitis
and patient discomfort.
8. Serum magnesium should be checked and replaced if low.
9. Increase insulin infusion up to 10 IU/kg/h until haemodynamic stability is achieved, i.e. mean arterial pressure >60 mmHg, heart rate
>60 bpm, normal sinus rhythm on electrocardiogram, urine output 1 mL/kg/h, lactate <2 mmol/L.
Consider transfer to a higher level of care if monitoring in a high-care setting and multiple infusions cannot be safely performed.
637 September 2019, Vol. 109, No. 9
IN PRACTICE
least 4 - 6-hourly during the first 24 - 48 hours of therapy.[18,25,30] 1. Gómez-Olivé F, Ali S, Made F, et al. Regional and sex differences in the prevalence and awareness of
hypertension across six sites in sub-Saharan Africa: An H3Africa AWI-Gen study. Reg Glob Heart
Supplemental potassium infusions should be stopped once the 2017;12(2):81-90. https://doi.org/10.1016/j.gheart.2017.01.007
patient has been weaned off the HIET, because the patient is not 2. Seedat Y, Rayner B, Veriava Y. South African Hypertension Practice Guideline 2014. Cardiovasc J Afr
2014;25(6):288-294. https://doi.org/10.5830/CVJA-2014-062
inherently potassium deficient.[14,18] 3. Rayner B, Spence J. Hypertension in blacks. J Hypertens 2017;35(2):234-239. https://doi.org/10.1097/
It is also essential to monitor for hypoglycaemia during the course HJH.0000000000001171
4. Rayner B. Hypertension: Detection and management in South Africa. Nephron Clin Pract
of treatment.[18,25,30] Supplemental 50% dextrose water boluses may 2010;116(4):c269-c273. https://doi.org/10.1159/000318788
5. Opie L, Seedat Y. Hypertension in sub-Saharan African populations. Circulation 2005;112(23):3562-
be given additionally to maintain normoglycaemia.[14,18,24,25] The 3568. https://doi.org/10.1161/CIRCULATIONAHA.105.539569
importance of strict glucose monitoring should be emphasised to 6. Brewster L, Seedat K. Why do hypertensive patients of African ancestry respond better to calcium
blockers and diuretics than to ACE inhibitors and β-adrenergic blockers? A systematic review. BMC Med
medical staff, particularly in intubated patients, to avoid unrecognised 2013;11:141. https://doi.org/10.1186/1741-7015-11-141
neuroglycopenia. 7. Veale D, Wium C, Müller G. Toxicovigilance I: A survey of acute poisoning in South Africa based on
Tygerberg Poison Information Centre data. S Afr Med J 2013;103(5):293-297. https://doi.org/10.7196/
There is limited consensus in the literature as to when HIET can be SAMJ.6647
stopped, although early or abrupt withdrawal of HIET is associated 8. Veale D, Wium C, Müller G. Toxicovigilance II: A survey of the spectrum of acute poisoning and current
practices in the initial management of poisoning cases admitted to South African hospitals. S Afr Med J
with rebound of CCB toxicity.[18,24,25] HIET should not be stopped 2013;103(5):298-303. https://doi.org/10.7196/SAMJ.6648
9. Ani J, Ross A, Campbell L. A review of patients presenting to accident and emergency department with
until haemodynamic stability is achieved and the patient no longer deliberate self-harm, KwaZulu-Natal, South Africa. Afr J Prim Health Care Fam Med 2017;9(1):a1234.
requires inotropic support with adrenaline. HIET should be weaned https://doi.org/10.4102/phcfm.v9i1.1234
10. Bantjes J, Breedt E, de Wet H, Khan M, Weiss R, Lewis I. Gender differences in epidemiology and medical
slowly, and this may be days after initiation.[24,25] The end-points of service utilisation among self-harm patients seeking treatment at an urban hospital in South Africa.
HIET therapy include maintenance of MAP >65 mmHg, heart rate Suicidol Online 2017;8(1):10-23. http://www.suicidology-online.com/pdf/Issue%202017%20Vol%20
8%20(1).pdf (accessed 31 July 2019).
>60 bpm, urine output 1 - 2 mL/kg, eradication of lactic acidosis, 11. Rietjens SJ, de Lange DW, Donker DW, Meulenbelt J. Practical recommendations for calcium channel
and improvement in the level of consciousness.[18,25,30,33] Psychological antagonist poisoning. Neth J Med 2016;74(2):60-67. http://www.njmonline.nl/getpdf.php?id=1674
(accessed 7 August 2019).
support and psychiatric evaluation are indicated in cases of deliberate 12. Watson WA, Litowitz TL, Klein-Schwartz W, et al. 2003 annual report of the American Association
of Poison Control Centers toxic exposure surveillance system. Am J Emerg Med 2004;22(5):335-404.
self-harm once the patient has been fully treated and stabilised. https://doi.org/10.1016/j.ajem.2004.06.001
13. Siddiqi TA, Hill J, Huckleberry Y, Parthasarathy S. Non-cardiogenic pulmonary edema and life-
The patient in refractory shock and the patient threatening shock due to calcium channel blocker overdose: A case report and clinical review. Respir
Care 2014;59(2):e15-e21. https://doi.org/10.4187/respcare.02244
in cardiac arrest 14. Graudins A, Lee H, Druda D. Calcium channel antagonist and beta-blocker overdose: Antidotes and
adjunct therapies. Br J Clin Pharmacol 2016;81(3):453-461. https://doi.org/10.1111/bcp.12763
Effective cardiopulmonary resuscitation and attention to advanced 15. Kumar K, Biyyam M, Bajantri B, Nayudu S. Critical management of severe hypotension caused by
cardiac life support principles remain the mainstay of therapy in amlodipine toxicity managed with hyperinsulinemia/euglycemia therapy supplemented with calcium
gluconate, intravenous glucagon and other vasopressor support: Review of literature. Cardiol Res
CCB-induced cardiac arrest.[14,23] In refractory shock, ensure that 2018;9(1):46-49. https://doi.org/10.14740/cr646w
16. Silverthorn D. Cardiovascular physiology. In: Espinoza D, German K, Yien B, Reid A, Cutt S, Earl W,
the maximum doses of HIET, up to 10 IU/kg/h, have been used; eds. Human Physiology: An Integrated Approach. 5th ed. San Francisco: Pearson Benjamin Cummings,
however, even higher doses have been used safely.[18,22,24] Intravenous 2010:467-511.
17. DeRoos F. Calcium channel blockers. In: Hoffman R, ed. Goldfrank’s Toxicologic Emergencies. 10th ed.
lipid emulsion therapy (ILE) may be tried in the peri-arrest or New York: McGraw-Hill, 2015:884-892.
arrested patient, although evidence of efficacy is scarce.[14,22,24] ILE 18. Nickson CP, Little M. Early use of high-dose insulin euglycaemic therapy for verapamil toxicity. Med J
Aust 2009;191(6):350-352. https://doi.org/10.5694/j.1326-5377.2009.tb02822.x
binds to lipophilic drugs, reducing their free concentration in target 19. Rizvi I, Ahmad A, Zaman S. Life-threatening calcium channel blocker overdose and its management.
organs. [11] A loading dose of 1.5 mL/kg of 20% lipid emulsion is given, BMJ Case Rep 2012. https://doi.org/10.1136/bcr.01.2012.5643
20. Miranda C, Xaivier L, Fiorante F, et al. Cardiac rhythm disturbances associated with amlodipine acute
followed by an infusion of 0.25 mL/kg/m over 30 - 60 minutes. [14] intoxication. Cardiovasc Toxicol 2012;12(4):359-362. https://doi.org/10.1007/s12012-012-9176-9
21. Department of Paediatrics and Child Health, University of Cape Town. Poisons Information Centre.
Lipid emulsion may be found in theatre, where it is used in cases http://www.paediatrics.uct.ac.za/poisons-information-centre (accessed 29 September 2018).
of local anaesthetic-induced cardiotoxicity. Finally, venoarterial 22. St-Onge M, Anseeuw K, Cantrell FL, et al. Experts consensus recommendations for the management
of calcium channel blocker poisoning in adults. Crit Care Med 2017;45(3):e306-e315. https://doi.
extracorporeal membrane oxygenation is a last resort for patients in org/10.1097/CCM.0000000000002087
refractory shock where this resource is available.[11,14,24] 23. Benson BE, Spyker DA, Troutman WA, Watson WA, Bakhireva LN. Amlodipine toxicity in children
less than 6 years of age: A dose-response analysis using national poison system data. J Emerg Med
2010;39(2):186-193. https://doi.org/10.1016/j.emermed.2009.02.16
Conclusions 24. Woodward C, Pourmand A, Mazer-Amirshai M. High-dose insulin therapy, an evidence-based
approach to beta-blocker/calcium channel blocker toxicity. Daru J Pharm Sci 2014;22(1):36. https://doi.
CCBs are commonly used in SA in the management of hypertension org/10.1186/2008-2231-22-36
25. Cole J, Arens A, Laes J, Klein L, Bangh S, Olives T. High dose insulin for beta-blocker and calcium
and other cardiovascular disease. It is essential that medical channel-blocker poisoning. Am J Emerg Med 2018;36(10):1817-1824. https://doi.org/10.1016/j.
practitioners know how to recognise and manage CCB OD, as severe ajem.2018.02.004
26. Nelson L, Lewin N, Howland M, Hoffman R, Goldfrank L, Flomenbaum N. Principles of managing the
CCB OD is often fatal. The Poison Information Centre in Cape acutely poisoned or overdosed patient. In: Hoffman R, ed. Goldfrank’s Toxicologic Emergencies. 10th ed.
Town has a 24-hour helpline to assist practitioners with toxicology New York: McGraw-Hill, 2015:37-44.
27. Van Hoving D, Hunter L, Gerber R, Lategan H, Marks C. The burden of intentional self poisioning on a
management. Haemodynamic monitoring and general resuscitation district-hospital public hospital in Cape Town, South Africa. Afr J Emerg Med 2018;8(3):79-83. https://
measures should be instituted without delay in patients who are doi.org/10.1016/j.afjem.2018.03.002
28. Rainey P. Laboratory principles. In: Hoffman R, ed. Goldfrank’s Toxicologic Emergencies. 10th ed. New
symptomatic. Asymptomatic patients should be monitored closely for York: McGraw-Hill, 2015:70-89.
29. Skoog C, Engebretsen K. Are vasopressors useful in toxin-induced cardiogenic shock? Clin Toxicol
at least 24 hours, particularly if a slow-release CCB has been ingested. (Phila) 2017;55(4):285-304. https://doi.org/10.1080/15563650.2017.1284329
Intravenous fluid, calcium and vasopressors form part of the initial 30. Engebretsen K, Kaczmarek K, Morgan J, Holger J. High-dose insulin therapy in beta-blocker and calcium
channel-blocker poisoning. Clin Toxicol (Phila) 2011;49(4):277-283. https://doi.org/10.3109/155636
management of CCB-induced shock. HIET should be started in 50.2011.582471
shocked patients who do not rapidly respond to initial therapy. HIET 31. Seegobin K, Maharaj S, Deosaran A, Reddy P. Severe beta blocker and calcium channel blocker overdose:
Role of high dose insulin. Am J Emerg Med 2018;36(4):736.e5-736.e6. https://doi.org/10.1016/j.
can be safely used in a monitored, high-care setting. Medical staff ajem.2018.01.038
should be educated about the rationale of the high doses used to 32. St-Onge M, Dubé P, Gosselin S, et al. Treatment of calcium channel blocker poisoning: A systematic
review. Clin Toxicol (Phila) 2014;52(9):926-944. https://doi.org/10.3109/15563650.2014.965827
avoid premature stopping of therapy and its adverse consequences. 33. Cecconi M, de Backer D, Antonelli M, et al. Consensus on circulatory shock and haemodynamic
monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med
2014;40(12):1795-1815. https://doi.org/10.1007/s00134-014-3525-z
34. National Department of Health, South Africa. Essential Drugs Programme. Hospital Level (Adults)
Acknowledgements. None. Standard Treatment Guidelines and Essential Medicines List. 4th ed. Pretoria: NDoH, 2015. http://www.
health.gov.za/index.php/standard-treatment-guidelines-and-essential-medicines-list/category/286-
Author contributions. The authors contributed equally to the writing, hospital-level-adults?download=2409:hospital-level-adult-2015-v5-0 (accessed 23 November 2018).
editing and revising of the manuscript.
Funding. None.
Conflicts of interest. None. Accepted 29 April 2019.
638 September 2019, Vol. 109, No. 9
Das könnte Ihnen auch gefallen
- Clinical Surgery Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Von EverandClinical Surgery Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Noch keine Bewertungen
- Update On (Approach To) Anemia1 (Changes)Dokument39 SeitenUpdate On (Approach To) Anemia1 (Changes)Balchand KukrejaNoch keine Bewertungen
- Behavior ResourcesDokument6 SeitenBehavior ResourcesBrook Farm Veterinary CenterNoch keine Bewertungen
- XA6 - Emergency Provision Workbook 2020 v0 - 5 - CKDokument35 SeitenXA6 - Emergency Provision Workbook 2020 v0 - 5 - CKguyNoch keine Bewertungen
- Groupwork Proposal BSW 3705 June 2022Dokument17 SeitenGroupwork Proposal BSW 3705 June 2022Mtshali Nthuseng100% (1)
- ParecoxibDokument2 SeitenParecoxibPeetah PanNoch keine Bewertungen
- Guidelines For Contemporary Air-Rotor StrippingDokument6 SeitenGuidelines For Contemporary Air-Rotor StrippingGerman Cabrera DiazNoch keine Bewertungen
- Cardiovascular Endocrinology and Metabolism: Theory and Practice of Cardiometabolic MedicineVon EverandCardiovascular Endocrinology and Metabolism: Theory and Practice of Cardiometabolic MedicineAndrew J. KrentzNoch keine Bewertungen
- High Doses Insulin ReviewDokument5 SeitenHigh Doses Insulin ReviewMau MillanNoch keine Bewertungen
- A Review: Nutrition in Chronic Kidney Disease PatientsDokument13 SeitenA Review: Nutrition in Chronic Kidney Disease Patientsscience worldNoch keine Bewertungen
- Management of Coronary Artery Disease in Patients With Chronic Kidney DiseaseDokument4 SeitenManagement of Coronary Artery Disease in Patients With Chronic Kidney Diseaseopi neanNoch keine Bewertungen
- Bihs PDFDokument4 SeitenBihs PDFFredrikus Lay Berkh MansNoch keine Bewertungen
- Coronary Artery Disease: Special Feature: Primary Care Issues For NephrologistsDokument6 SeitenCoronary Artery Disease: Special Feature: Primary Care Issues For NephrologistssyahidNoch keine Bewertungen
- Toxins: Cardiotoxicity of Uremic Toxins: A Driver of Cardiorenal SyndromeDokument29 SeitenToxins: Cardiotoxicity of Uremic Toxins: A Driver of Cardiorenal SyndromeIka AyuNoch keine Bewertungen
- Molecules 25 01465 v2 PDFDokument24 SeitenMolecules 25 01465 v2 PDFمصطفى باسم هادي B1Noch keine Bewertungen
- CV 2 Statins in Chronic Kidney Disease When and When Not To Use ThemDokument14 SeitenCV 2 Statins in Chronic Kidney Disease When and When Not To Use ThemMacarena SainzNoch keine Bewertungen
- Heart Failure Treatment in The Intensive Care Unit in ChildrenDokument28 SeitenHeart Failure Treatment in The Intensive Care Unit in ChildrenNatalia Alejandra Cardozo GomezNoch keine Bewertungen
- 8 Meq/L PH 7.2) May Require Iv Therapy (See Chap. 51) .: Evaluation of Therapeutic OutcomesDokument2 Seiten8 Meq/L PH 7.2) May Require Iv Therapy (See Chap. 51) .: Evaluation of Therapeutic OutcomesDebbyNovriozaNoch keine Bewertungen
- Dialysis-Induced Myocardial Stunning: The Other Side of The Cardiorenal SyndromeDokument9 SeitenDialysis-Induced Myocardial Stunning: The Other Side of The Cardiorenal SyndromeYoga PrabawaNoch keine Bewertungen
- Chronic Heart Failure-Part IDokument18 SeitenChronic Heart Failure-Part IdrtpkNoch keine Bewertungen
- Journal of Clinical & Translational EndocrinologyDokument7 SeitenJournal of Clinical & Translational EndocrinologyArini NurlelaNoch keine Bewertungen
- A Role For SGLT 2 Inhibitors in Treating Non Diabetic Chronic Kidney DiseaseDokument21 SeitenA Role For SGLT 2 Inhibitors in Treating Non Diabetic Chronic Kidney DiseaseCarlos Martinez SalgadoNoch keine Bewertungen
- Acute Kidney Injury in HFDokument14 SeitenAcute Kidney Injury in HFAnonymous NeRC5JYiSNoch keine Bewertungen
- Koniari 2011Dokument11 SeitenKoniari 2011rosyidmawardi7Noch keine Bewertungen
- Updates in Hyperkalemia: Outcomes and Therapeutic StrategiesDokument7 SeitenUpdates in Hyperkalemia: Outcomes and Therapeutic StrategiesNaomi AhimsaNoch keine Bewertungen
- Calcium Channel Blockers (CCBS)Dokument3 SeitenCalcium Channel Blockers (CCBS)Yohanes SutrisnoNoch keine Bewertungen
- Heart Failure and Diabetes Endo Metab Clinics North Am 17Dokument19 SeitenHeart Failure and Diabetes Endo Metab Clinics North Am 17Paulina DiazNoch keine Bewertungen
- Anaesthesia For Chronic Renal Disease and Renal TRDokument19 SeitenAnaesthesia For Chronic Renal Disease and Renal TRdiah wibowoNoch keine Bewertungen
- Therapeutic Options For The Management of The Cardiorenal SyndromeDokument11 SeitenTherapeutic Options For The Management of The Cardiorenal SyndromeAntoine SchallerNoch keine Bewertungen
- Concomitant Diabetes With Atrial Fibrillation andDokument9 SeitenConcomitant Diabetes With Atrial Fibrillation and25515okeNoch keine Bewertungen
- Effects of Statins On Renal FunctionDokument10 SeitenEffects of Statins On Renal Functionangela gagariNoch keine Bewertungen
- Inotropic and Vasoactive Drugs in Pediatric ICUDokument6 SeitenInotropic and Vasoactive Drugs in Pediatric ICUCandy RevolloNoch keine Bewertungen
- Tatalaksana GUCH Di ICUDokument12 SeitenTatalaksana GUCH Di ICUBima AryaputraNoch keine Bewertungen
- Reviews: Management of Hyperkalaemia in Chronic Kidney DiseaseDokument10 SeitenReviews: Management of Hyperkalaemia in Chronic Kidney Diseasebagir_dm10Noch keine Bewertungen
- Lewis: Medical-Surgical Nursing, 8th EditionDokument7 SeitenLewis: Medical-Surgical Nursing, 8th EditionJoyzoeyNoch keine Bewertungen
- Acute On ChronicDokument4 SeitenAcute On ChronicrendyoscaNoch keine Bewertungen
- Hypertension and Chronic Kidney Disease: Respective Contribution of Mean and Pulse Pressure and Arterial StiffnessDokument6 SeitenHypertension and Chronic Kidney Disease: Respective Contribution of Mean and Pulse Pressure and Arterial StiffnessLis Borda MuñozNoch keine Bewertungen
- Cardiovascular Pathophysiology in Chronic Kidney Disease: Opportunities To Transition From Disease To HealthDokument8 SeitenCardiovascular Pathophysiology in Chronic Kidney Disease: Opportunities To Transition From Disease To HealthABNoch keine Bewertungen
- Review of Medical Treatment of Stable Ischemic Heart DiseaseDokument11 SeitenReview of Medical Treatment of Stable Ischemic Heart DiseaseSuci NourmalizaNoch keine Bewertungen
- Double Trouble Managing Diabetic Emergencies in Patients With Heart FailureDokument5 SeitenDouble Trouble Managing Diabetic Emergencies in Patients With Heart FailurePutra AchmadNoch keine Bewertungen
- Heart Failure May 2013 Final PDFDokument52 SeitenHeart Failure May 2013 Final PDFIulia NegruNoch keine Bewertungen
- MacrocytosisDokument6 SeitenMacrocytosisAbdul QuyyumNoch keine Bewertungen
- Haemodynamic Instability During Dialysis: The Potential Role of Intra-Dialytic ExerciseDokument13 SeitenHaemodynamic Instability During Dialysis: The Potential Role of Intra-Dialytic ExerciseJevon JavierNoch keine Bewertungen
- Kjim 2017 355Dokument12 SeitenKjim 2017 355Carolina Aguilar OtáloraNoch keine Bewertungen
- Cardiovascular Complication in HD 2019 DR RubinDokument49 SeitenCardiovascular Complication in HD 2019 DR RubinASIS ADRINoch keine Bewertungen
- Acute Heart Failure Syndromes: Kelompok CDokument29 SeitenAcute Heart Failure Syndromes: Kelompok CErwin BawonoNoch keine Bewertungen
- FAQ - Denosumab-Induced Hypocalcemia in CKD and DialysisDokument9 SeitenFAQ - Denosumab-Induced Hypocalcemia in CKD and Dialysisraea.dobsonNoch keine Bewertungen
- 904 FullDokument7 Seiten904 FullMohamad MostafaNoch keine Bewertungen
- Antihypertensives 2Dokument6 SeitenAntihypertensives 2Manyal Kutin KoakNoch keine Bewertungen
- When and How To Use Direct Oral Anticoagulants in Patients With Advanced Chronic Liver Disease?Dokument6 SeitenWhen and How To Use Direct Oral Anticoagulants in Patients With Advanced Chronic Liver Disease?Felipe SotoNoch keine Bewertungen
- HHS Public Access: DPP4 Inhibitors and Cardiovascular Outcomes: Safety On Heart FailureDokument10 SeitenHHS Public Access: DPP4 Inhibitors and Cardiovascular Outcomes: Safety On Heart FailureRahmanu ReztaputraNoch keine Bewertungen
- The Role of Neprilysin Inhibitors in Cardiovascular DiseaseDokument6 SeitenThe Role of Neprilysin Inhibitors in Cardiovascular DiseaseHarold Mateo Mojica UrregoNoch keine Bewertungen
- ADHF ManagementDokument6 SeitenADHF ManagementEsti YunitaNoch keine Bewertungen
- Renal Considerations in Angiotensin Converting Enzyme Inhibitor TherapyDokument8 SeitenRenal Considerations in Angiotensin Converting Enzyme Inhibitor TherapyCondurache Ilie-AndreiNoch keine Bewertungen
- Anemia in PregnancyDokument20 SeitenAnemia in PregnancyRaguNoch keine Bewertungen
- Inotropes 2014. Journal of The American College of CardiologyDokument10 SeitenInotropes 2014. Journal of The American College of CardiologyFra1312Noch keine Bewertungen
- Toxins 13 00142 v2Dokument26 SeitenToxins 13 00142 v2Patus QuakusNoch keine Bewertungen
- Case Study Number 1Dokument5 SeitenCase Study Number 1Kevin Kyle RizarriNoch keine Bewertungen
- Diabetic Cardiomyopathy: Editorial (See Bertoni ET AL., P. 2 7 9 1)Dokument3 SeitenDiabetic Cardiomyopathy: Editorial (See Bertoni ET AL., P. 2 7 9 1)aymenNoch keine Bewertungen
- Pediatric Dilated CardiomyopathyDokument10 SeitenPediatric Dilated CardiomyopathyRiduan Adoro Lumban GaolNoch keine Bewertungen
- Disfunctii Vaculare, Ateroscleroza Si Calcificari VasculareDokument24 SeitenDisfunctii Vaculare, Ateroscleroza Si Calcificari VasculareMikaela W. Marcu100% (1)
- Falla Renal 2011Dokument8 SeitenFalla Renal 2011Mattya SalazarNoch keine Bewertungen
- Dialysis Brain Injury Davenport PDFDokument6 SeitenDialysis Brain Injury Davenport PDFTonito ManéNoch keine Bewertungen
- Long Term Complications of Hemodialysis 12 18Dokument8 SeitenLong Term Complications of Hemodialysis 12 18MutiaraHandayaniNoch keine Bewertungen
- Table 150-4 - Selected Characteristics of Some Calcium Channel BlockersDokument6 SeitenTable 150-4 - Selected Characteristics of Some Calcium Channel BlockersfaradillaNoch keine Bewertungen
- T-Type Calcium Channel Blockers: A Patent Review (2012-2018)Dokument20 SeitenT-Type Calcium Channel Blockers: A Patent Review (2012-2018)Zilmaida SalomNoch keine Bewertungen
- Jurnal Kimed 1Dokument19 SeitenJurnal Kimed 1Zilmaida SalomNoch keine Bewertungen
- Jurnal Kimed 2Dokument15 SeitenJurnal Kimed 2Zilmaida SalomNoch keine Bewertungen
- Jurnal Kimed 3Dokument10 SeitenJurnal Kimed 3Zilmaida SalomNoch keine Bewertungen
- Jurnal Kimed 6Dokument9 SeitenJurnal Kimed 6Zilmaida SalomNoch keine Bewertungen
- Perhitungan Ukuran Granul Mesh : H R H R H RDokument2 SeitenPerhitungan Ukuran Granul Mesh : H R H R H RZilmaida SalomNoch keine Bewertungen
- Registrars Manual On Band DDokument32 SeitenRegistrars Manual On Band DkailasasundaramNoch keine Bewertungen
- Chapter I Related Literature Teenage PreDokument12 SeitenChapter I Related Literature Teenage PreWilkenn Tuazon100% (3)
- Pediatrics Rapid RevisionDokument72 SeitenPediatrics Rapid RevisionWorld MedclickzNoch keine Bewertungen
- Nutritional Interventions PDFDokument17 SeitenNutritional Interventions PDFLalit MittalNoch keine Bewertungen
- Viroguard Sanitizer SDS-WatermartDokument7 SeitenViroguard Sanitizer SDS-WatermartIshara VithanaNoch keine Bewertungen
- ProVari ManualDokument16 SeitenProVari ManualPatrickNoch keine Bewertungen
- Analysis & Distribution of The Syllabus Grade 11 English For Palestine Second Semester School Year: 20 - 20Dokument3 SeitenAnalysis & Distribution of The Syllabus Grade 11 English For Palestine Second Semester School Year: 20 - 20Nur IbrahimNoch keine Bewertungen
- Written Assignment Unit 2 - HS 2212Dokument5 SeitenWritten Assignment Unit 2 - HS 2212bnvjNoch keine Bewertungen
- Strengthening Health Emergency Management System Through The ILHZDokument7 SeitenStrengthening Health Emergency Management System Through The ILHZCliff GubatNoch keine Bewertungen
- 21.JMM Promotion and Management, Inc. vs. Court of AppealsDokument3 Seiten21.JMM Promotion and Management, Inc. vs. Court of AppealsnathNoch keine Bewertungen
- Paper On Rag PickersDokument11 SeitenPaper On Rag PickershsrapsNoch keine Bewertungen
- Save Child GirlDokument2 SeitenSave Child GirlManishaNoch keine Bewertungen
- Chapter 12 Rev QuestionsDokument3 SeitenChapter 12 Rev QuestionsLidia DominguezNoch keine Bewertungen
- STD.: Xi Practice Test - 2016 Date: 0 14 - 10 - 2016 SUBJECT: Zoology Animal HusbandryDokument2 SeitenSTD.: Xi Practice Test - 2016 Date: 0 14 - 10 - 2016 SUBJECT: Zoology Animal HusbandryDr-Atin Kumar SrivastavaNoch keine Bewertungen
- Dinup BSBMGT605Dokument41 SeitenDinup BSBMGT605fhc munna100% (1)
- MFDS FAQsDokument2 SeitenMFDS FAQsSuhesh HydrosNoch keine Bewertungen
- Department of ICT Technology - DBMS Section: Level - IVDokument125 SeitenDepartment of ICT Technology - DBMS Section: Level - IVEsubalewNoch keine Bewertungen
- Lab 11 AntianginalDokument4 SeitenLab 11 AntianginalanaNoch keine Bewertungen
- Procedure Checklist On OxygenationDokument2 SeitenProcedure Checklist On OxygenationKhatlen BagaresNoch keine Bewertungen
- 2022 SWMS - Combined SWMSDokument8 Seiten2022 SWMS - Combined SWMSSteveNoch keine Bewertungen
- APDSA SRC Submitssion FormDokument2 SeitenAPDSA SRC Submitssion FormDevi 吴姗姗 GunawanNoch keine Bewertungen
- Safety Inspection Checklist Project: Location: Inspector: DateDokument2 SeitenSafety Inspection Checklist Project: Location: Inspector: Dateyono DaryonoNoch keine Bewertungen
- BotulismeDokument36 SeitenBotulismeDienjhe Love BunzNoch keine Bewertungen
- Consent ModelDokument4 SeitenConsent ModelSundaresan ChockalingamNoch keine Bewertungen
- Chapter 6 QuestionsDokument2 SeitenChapter 6 QuestionsGabo DanteNoch keine Bewertungen