Beruflich Dokumente
Kultur Dokumente
Katzung 11th - Antiagregantes Plaquetários
Hochgeladen von
Joana NunesOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Katzung 11th - Antiagregantes Plaquetários
Hochgeladen von
Joana NunesCopyright:
Verfügbare Formate
598 SECTION VI Drugs Used to Treat Diseases of the Blood, Inflammation, & Gout
namic instability, severe deep venous thrombosis such as the tions of 10 units each, separated by 30 minutes. Tenecteplase
superior vena caval syndrome, and ascending thrombophle- is given as a single intravenous bolus of 0.5 mg/kg. Anistre-
bitis of the iliofemoral vein with severe lower extremity ede- plase (where available) is given as a single intravenous injec-
ma. These drugs are also given intra-arterially, especially for tion of 30 units over 3–5 minutes. A single course of
peripheral vascular disease. fibrinolytic drugs is expensive: hundreds of dollars for strep-
Thrombolytic therapy in the management of acute myo- tokinase and thousands for urokinase and t-PA.
cardial infarction requires careful patient selection, the use of Recombinant t-PA has also been approved for use in acute
a specific thrombolytic agent, and the benefit of adjuvant ischemic stroke within 3 hours of symptom onset. In patients
therapy. Streptokinase is administered by intravenous infu- without hemorrhagic infarct or other contraindications,
sion of a loading dose of 250,000 units, followed by 100,000 this therapy has been demonstrated to provide better out-
units/h for 24–72 hours. Patients with antistreptococcal anti- comes in several randomized clinical trials. The recom-
bodies can develop fever, allergic reactions, and therapeutic mended dose is 0.9 mg/kg, not to exceed 90 mg, with 10%
resistance. Urokinase requires a loading dose of 300,000 units given as a bolus and the remainder during a 1 hour infu-
given over 10 minutes and a maintenance dose of 300,000 sion. Streptokinase has been associated with increased
units/h for 12 hours. Alteplase (t-PA) is given by intravenous bleeding risk in acute ischemic stroke when given at a dose
infusion of 60 mg over the first hour and then 40 mg at a rate of 1.5 million units, and its use is not recommended in this
of 20 mg/h. Reteplase is given as two intravenous bolus injec- setting.
BASIC PHARMACOLOGY OF ANTIPLATELET AGENTS
Platelet function is regulated by three categories of substances. use of aspirin by the general population except when pre-
The first group consists of agents generated outside the platelet scribed as an adjunct to risk factor management by smoking
that interact with platelet membrane receptors, eg, catechol- cessation and lowering of blood cholesterol and blood pres-
amines, collagen, thrombin, and prostacyclin. The second cate- sure. Meta-analysis of many published trials of aspirin and
gory contains agents generated within the platelet that interact other antiplatelet agents confirms the value of this interven-
with membrane receptors, eg, ADP, prostaglandin D2, prosta- tion in the secondary prevention of vascular events among
glandin E2, and serotonin. The third group comprises agents patients with a history of vascular events.
generated within the platelet that act within the platelet, eg,
prostaglandin endoperoxides and thromboxane A2, the cyclic
nucleotides cAMP and cGMP, and calcium ion. From this list of
CLOPIDOGREL & TICLOPIDINE
agents, several targets for platelet inhibitory drugs have been Clopidogrel and ticlopidine reduce platelet aggregation by in-
identified (Figure 34–1): inhibition of prostaglandin synthesis hibiting the ADP pathway of platelets. These drugs are thienopy-
(aspirin), inhibition of ADP-induced platelet aggregation (clo- ridine derivatives that achieve their antiplatelet effects by
pidogrel, ticlopidine), and blockade of glycoprotein IIb/IIIa re- irreversibly blocking the ADP receptor on platelets. Unlike as-
ceptors on platelets (abciximab, tirofiban, and eptifibatide). pirin, these drugs have no effect on prostaglandin metabolism.
Dipyridamole and cilostazol are additional antiplatelet drugs. Randomized clinical trials with both drugs report efficacy in
the prevention of vascular events among patients with tran-
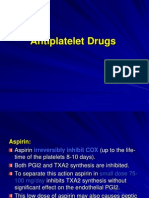
ASPIRIN sient ischemic attacks, completed strokes, and unstable angina
pectoris. Use of clopidogrel or ticlopidine to prevent throm-
The prostaglandin thromboxane A2 is an arachidonate prod- bosis is now considered standard practice in patients under-
uct that causes platelets to change shape, release their gran- going placement of a coronary stent.
ules, and aggregate (see Chapter 18). Drugs that antagonize Adverse effects of ticlopidine include nausea, dyspepsia,
this pathway interfere with platelet aggregation in vitro and and diarrhea in up to 20% of patients, hemorrhage in 5%, and,
prolong the bleeding time in vivo. Aspirin is the prototype of most seriously, leukopenia in 1%. The leukopenia is detected
this class of drugs. by regular monitoring of the white blood cell count during the
As described in Chapter 18, aspirin inhibits the synthesis of first 3 months of treatment. Development of thrombotic
thromboxane A2 by irreversible acetylation of the enzyme thrombocytopenic purpura has also been associated with the
cyclooxygenase. Other salicylates and nonsteroidal anti-inflam- ingestion of ticlopidine. The dosage of ticlopidine is 250 mg
matory drugs also inhibit cyclooxygenase but have a shorter twice daily. It is particularly useful in patients who cannot tol-
duration of inhibitory action because they cannot acetylate erate aspirin. Doses of ticlopidine less than 500 mg/d may be
cyclooxygenase; that is, their action is reversible. efficacious with fewer adverse effects.
The FDA has approved the use of 325 mg/d for primary Clopidogrel has fewer adverse effects than ticlopidine and is
prophylaxis of myocardial infarction but urges caution in this rarely associated with neutropenia. Thrombotic thrombocyto-
CHAPTER 34 Drugs Used in Disorders of Coagulation 599
penic purpura associated with clopidogrel has been reported. this receptor have a bleeding disorder called Glanzmann’s
Because of its superior side effect profile and dosing require- thrombasthenia.
ments, clopidogrel is preferred over ticlopidine. The antithrom- Abciximab, a chimeric monoclonal antibody directed
botic effects of clopidogrel are dose-dependent; within 5 hours against the IIb/IIIa complex including the vitronectin recep-
after an oral loading dose of 300 mg, 80% of platelet activity will tor, was the first agent approved in this class of drugs. It has
be inhibited. The maintenance dose of clopidogrel is 75 mg/d, been approved for use in percutaneous coronary intervention
which achieves maximum platelet inhibition. The duration of and in acute coronary syndromes. Eptifibatide is an analog of
the antiplatelet effect is 7–10 days. the sequence at the extreme carboxyl terminal of the delta
chain of fibrinogen, which mediates the binding of fibrinogen
to the receptor. Tirofiban is a smaller molecule with similar
Aspirin & Clopidogrel Resistance properties. Eptifibatide and tirofiban inhibit ligand binding to
The reported incidence of resistance to these drugs varies the IIb/IIIa receptor by their occupancy of the receptor but do
greatly, from less than 5% to 75%. In part this tremendous not block the vitronectin receptor.
variation in incidence reflects the definition of resistance The three agents described above are administered parenter-
(recurrent thrombosis while on antiplatelet therapy vs in ally. Oral formulations of IIb/IIIa antagonists are in various
vitro testing), methods by which drug response is mea- stages of development.
sured, and patient compliance. Several methods for testing
aspirin and clopidogrel resistance in vitro are now FDA-
approved; however, their utility outside of clinical trials re- ADDITIONAL ANTIPLATELET-
mains controversial. DIRECTED DRUGS
Dipyridamole is a vasodilator that inhibits platelet function by
BLOCKADE OF PLATELET inhibiting adenosine uptake and cGMP phosphodiesterase activ-
GLYCOPROTEIN IIB/IIIA RECEPTORS ity. Dipyridamole by itself has little or no beneficial effect. There-
fore, therapeutic use of this agent is primarily in combination
The glycoprotein IIb/IIIa inhibitors are used in patients with with aspirin to prevent cerebrovascular ischemia. It may also be
acute coronary syndromes. These drugs target the platelet IIb/ used in combination with warfarin for primary prophylaxis of
IIIa receptor complex (Figure 34–1). The IIb/IIIa complex thromboemboli in patients with prosthetic heart valves. A com-
functions as a receptor mainly for fibrinogen and vitronectin bination of dipyridamole complexed with 25 mg of aspirin is now
but also for fibronectin and von Willebrand factor. Activation available for secondary prophylaxis of cerebrovascular disease.
of this receptor complex is the “final common pathway” for Cilostazol is a newer phosphodiesterase inhibitor that pro-
platelet aggregation. There are approximately 50,000 copies of motes vasodilation and inhibition of platelet aggregation. Cil-
this complex on the surface of each platelet. Persons lacking ostazol is used primarily to treat intermittent claudication.
CLINICAL PHARMACOLOGY OF DRUGS USED
TO PREVENT CLOTTING
VENOUS THROMBOSIS count for the greater number of hypercoagulable patients. Al-
though the loss of function mutations is less common, they are
associated with the greatest thrombosis risk. Some patients have
Risk Factors multiple inherited risk factors or combinations of inherited and
A. Inherited Disorders acquired risk factors as discussed below. These individuals are
The inherited disorders characterized by a tendency to form at higher risk for recurrent thrombotic events and are often
thrombi (thrombophilia) derive from either quantitative or considered candidates for lifelong therapy.
qualitative abnormalities of the natural anticoagulant system.
Deficiencies (loss of function mutations) in the natural antico- B. Acquired Disease
agulants antithrombin, protein C, and protein S account for ap- The increased risk of thromboembolism associated with atrial
proximately 15% of selected patients with juvenile or recurrent fibrillation and with the placement of mechanical heart valves
thrombosis and 5–10% of unselected cases of acute venous has long been recognized. Similarly, prolonged bed rest, high-
thrombosis. Additional causes of thrombophilia include gain of risk surgical procedures, and the presence of cancer are clearly
function mutations such as the factor V Leiden mutation and associated with an increased incidence of deep venous throm-
the prothrombin 20210 mutation, elevated clotting factor and bosis and embolism. Antiphospholipid antibody syndrome is
cofactor levels, and hyperhomocysteinemia that together ac- another important acquired risk factor. Drugs may function as
Das könnte Ihnen auch gefallen
- Contraindications To Thrombolytic Therapy: Aminocaproic AcidDokument3 SeitenContraindications To Thrombolytic Therapy: Aminocaproic AcidTia Siti RoilaNoch keine Bewertungen
- Anticoagulants and Antiplatelet AgentsDokument4 SeitenAnticoagulants and Antiplatelet AgentsMark Russel Sean LealNoch keine Bewertungen
- Antiplatelet Therapy: New Antiplatelet Drugs in PerspectiveDokument4 SeitenAntiplatelet Therapy: New Antiplatelet Drugs in Perspectivegeo_mmsNoch keine Bewertungen
- Antiplatelet Treatment in Stable Coronary Artery DiseaseDokument6 SeitenAntiplatelet Treatment in Stable Coronary Artery DiseaserambutsapukusayangNoch keine Bewertungen
- Drugs Used in Disorders of CoagulationDokument61 SeitenDrugs Used in Disorders of CoagulationDUEÑAS, MARIELNoch keine Bewertungen
- Antiplatelet DrugsDokument3 SeitenAntiplatelet DrugsArnel Leonard TungbabanNoch keine Bewertungen
- PIIS1053077018310437Dokument5 SeitenPIIS1053077018310437andi rahmatNoch keine Bewertungen
- Antiplatelet DrugsDokument31 SeitenAntiplatelet DrugsSyed Usama Rashid100% (2)
- New Drugs and Technologies: PrasugrelDokument10 SeitenNew Drugs and Technologies: PrasugrelDewi FitrianaNoch keine Bewertungen
- Br. J. Anaesth. 2007 Chassot 316 28Dokument13 SeitenBr. J. Anaesth. 2007 Chassot 316 28Rhahima SyafrilNoch keine Bewertungen
- Drugs Affecting PlateletsDokument1 SeiteDrugs Affecting PlateletsDiana CentaurusNoch keine Bewertungen
- Principles of Antiplatelet Therapy: DR Htet Htet Htethtet@Imu - Edu.MyDokument36 SeitenPrinciples of Antiplatelet Therapy: DR Htet Htet Htethtet@Imu - Edu.MyAbby Liew100% (1)
- DR - Hussam Lec 3 Drugs Affecting Blood 2023 4Dokument13 SeitenDR - Hussam Lec 3 Drugs Affecting Blood 2023 4ManWol JangNoch keine Bewertungen
- 0718 4026 Rchcir 70 03 0291Dokument9 Seiten0718 4026 Rchcir 70 03 0291Erick ToHuNoch keine Bewertungen
- Manejo Perioperatorio de Pacientes Usuarios de Antiagregantes PlaquetariosDokument9 SeitenManejo Perioperatorio de Pacientes Usuarios de Antiagregantes PlaquetariosErick ToHuNoch keine Bewertungen
- AntitrombolitikDokument7 SeitenAntitrombolitikadityaNoch keine Bewertungen
- Drugs Used in Disorders of CoagulationDokument60 SeitenDrugs Used in Disorders of CoagulationTwinkle MazaredoNoch keine Bewertungen
- Prevention of Atherotrobmotic EventsDokument14 SeitenPrevention of Atherotrobmotic Eventsddandan_2Noch keine Bewertungen
- Pertemuan 7 LiyanaDokument36 SeitenPertemuan 7 LiyanaLiyana SafitriNoch keine Bewertungen
- Platelet Aggregation Inhibitors: Professor. Dr. Mahmoud KhattabDokument24 SeitenPlatelet Aggregation Inhibitors: Professor. Dr. Mahmoud KhattabfrabziNoch keine Bewertungen
- 9 - Anti-Platelet DrugsDokument12 Seiten9 - Anti-Platelet DrugsGoodone OneNoch keine Bewertungen
- Principles of An-Tiplatelet Therapy: DR Htet Htet Htethtet@Imu - Edu.MyDokument36 SeitenPrinciples of An-Tiplatelet Therapy: DR Htet Htet Htethtet@Imu - Edu.MyAbby LiewNoch keine Bewertungen
- Trimetazidine ReviewDokument9 SeitenTrimetazidine ReviewWasim ShaheenNoch keine Bewertungen
- Antiplatelet Drugs: Dr. Chandane R. DDokument34 SeitenAntiplatelet Drugs: Dr. Chandane R. Dabdul razakNoch keine Bewertungen
- Clopidogrel Resistance and Clopidogrel Treatment Failure - UpToDateDokument39 SeitenClopidogrel Resistance and Clopidogrel Treatment Failure - UpToDateRenato RamonNoch keine Bewertungen
- Antiplatelete DrugsDokument27 SeitenAntiplatelete DrugsYohannes MeridNoch keine Bewertungen
- Anticoagulacion 2Dokument9 SeitenAnticoagulacion 2Annette ChavezNoch keine Bewertungen
- Pharma DR - Hussein Drugs Effecting Hemostasis Lec 1Dokument31 SeitenPharma DR - Hussein Drugs Effecting Hemostasis Lec 1rkh647m7szNoch keine Bewertungen
- Anemia Hemolitik Autoimun (AIHA) 2Dokument23 SeitenAnemia Hemolitik Autoimun (AIHA) 2Za'in MuchtarNoch keine Bewertungen
- Antiplatelet Therapy in Flow Diversion-2019Dokument6 SeitenAntiplatelet Therapy in Flow Diversion-2019ariNoch keine Bewertungen
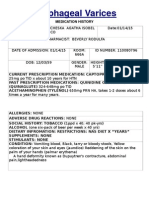
- Esophageal Varices: Medication HistoryDokument4 SeitenEsophageal Varices: Medication HistoryNeil Patrick PasuquinNoch keine Bewertungen
- Anti Platelets Agents: Dr. Sachana KC 1 Year Resident Department of AnesthesiaDokument61 SeitenAnti Platelets Agents: Dr. Sachana KC 1 Year Resident Department of AnesthesiaKshitizma GiriNoch keine Bewertungen
- Antithrombotic Drugs: Pharmacology and Implications For Dental PracticeDokument9 SeitenAntithrombotic Drugs: Pharmacology and Implications For Dental PracticeMariana VLedezmaNoch keine Bewertungen
- Myocardial Infarction Medication: Aspirin (Ascriptin, Bayer Aspirin, Aspirtab, Ecotrin, Durlaza)Dokument11 SeitenMyocardial Infarction Medication: Aspirin (Ascriptin, Bayer Aspirin, Aspirtab, Ecotrin, Durlaza)Ashutosh SinghNoch keine Bewertungen
- Cardio-Cerebrovascular Pharmacotherapy: Sutomo Tanzil Dept - of Pharmacology, Faculty of Medicine, Sriwijaya UniversityDokument32 SeitenCardio-Cerebrovascular Pharmacotherapy: Sutomo Tanzil Dept - of Pharmacology, Faculty of Medicine, Sriwijaya UniversityFarahEzzlynnNoch keine Bewertungen
- 309 Novel Anti-Platelet Agents and AnticoagulantsDokument13 Seiten309 Novel Anti-Platelet Agents and AnticoagulantsPhani NadellaNoch keine Bewertungen
- Blood Coagulation and FibrinolysisDokument63 SeitenBlood Coagulation and FibrinolysisNora AboshanadyNoch keine Bewertungen
- Antiplatelet DrugsDokument15 SeitenAntiplatelet Drugsngan321100% (1)
- Plavix (Clopidogrel)Dokument1 SeitePlavix (Clopidogrel)E50% (2)
- Why Do Some Low-Dose Aspirin Formulations Intended For Use As Anti-Platelet Medications Contain Glycine?Dokument10 SeitenWhy Do Some Low-Dose Aspirin Formulations Intended For Use As Anti-Platelet Medications Contain Glycine?Hueysha KhorNoch keine Bewertungen
- Anti Platelet Agents Stroke Tia 032013Dokument1 SeiteAnti Platelet Agents Stroke Tia 032013Nari BurathiNoch keine Bewertungen
- Blood Drugs PDFDokument4 SeitenBlood Drugs PDFOmar WaleedNoch keine Bewertungen
- Anti Platelets FKFKFKDokument17 SeitenAnti Platelets FKFKFKIndah Pujiati DtNoch keine Bewertungen
- 2006.-Abciximab Associated Thrombocytopenia...Dokument5 Seiten2006.-Abciximab Associated Thrombocytopenia...tristan9454Noch keine Bewertungen
- MagnesiumDokument1 SeiteMagnesiumRatna Sari DewiNoch keine Bewertungen
- Goodman & Gilman's, The Pharmacological Basis of Therapeutics, 12 Edition, p-1538)Dokument6 SeitenGoodman & Gilman's, The Pharmacological Basis of Therapeutics, 12 Edition, p-1538)Sandeep HavaleNoch keine Bewertungen
- Treatment of Hemostasis DisordersDokument17 SeitenTreatment of Hemostasis DisordersDiana HyltonNoch keine Bewertungen
- Antiplatelet Aggregation DrugsDokument14 SeitenAntiplatelet Aggregation Drugs백지원 (소네트리)Noch keine Bewertungen
- CPG3 Secondary Stroke PreventionDokument10 SeitenCPG3 Secondary Stroke Preventionmochamad rizaNoch keine Bewertungen
- Pharmacology and Toxicology - Anticoagulants - Medical LibraryDokument8 SeitenPharmacology and Toxicology - Anticoagulants - Medical Libraryjean PiedraNoch keine Bewertungen
- AnticoagulantDokument15 SeitenAnticoagulantMaine AsuncionNoch keine Bewertungen
- Adenosine Diphosphate InhibitorsDokument1 SeiteAdenosine Diphosphate InhibitorsFalaq2Noch keine Bewertungen
- Antiplatelet Agents in Acute Non-ST Elevation Acute Coronary SyndromesDokument31 SeitenAntiplatelet Agents in Acute Non-ST Elevation Acute Coronary SyndromesCésar Santis FuentesNoch keine Bewertungen
- Anticoagulation Module 2Dokument13 SeitenAnticoagulation Module 2angelmedurNoch keine Bewertungen
- 9 Anti PlateletDokument15 Seiten9 Anti PlateletHely PatelNoch keine Bewertungen
- Novel-Antiplatelet Therapies For Atherothrombotic Diseases: K.malleswari, D.Rama Bramha Reddy, A.Karthikeya SharmaDokument8 SeitenNovel-Antiplatelet Therapies For Atherothrombotic Diseases: K.malleswari, D.Rama Bramha Reddy, A.Karthikeya Sharma9493.karthikNoch keine Bewertungen
- Chapter 2Dokument34 SeitenChapter 2zaidhusam100% (2)
- 4.3 Final Antiplatelet and Thrombolytic DrugsDokument47 Seiten4.3 Final Antiplatelet and Thrombolytic DrugsSaurabh11102000Noch keine Bewertungen
- Novel Anticoagulants: Anesthetic Implications: A Platelet-Ligand-Platelet Matrix With FibrinogenDokument9 SeitenNovel Anticoagulants: Anesthetic Implications: A Platelet-Ligand-Platelet Matrix With FibrinogenRodrigo BarreraNoch keine Bewertungen
- Early Antithrombotic Treatment of Acute Ischemic Stroke and Transient Ischemic Attack - UpToDateDokument27 SeitenEarly Antithrombotic Treatment of Acute Ischemic Stroke and Transient Ischemic Attack - UpToDateEduardo QuinteroNoch keine Bewertungen
- RECOVER Post Vaccine Protocol-2023-02-28Dokument60 SeitenRECOVER Post Vaccine Protocol-2023-02-28foxdog2Noch keine Bewertungen
- ACS Management in JKN EraDokument36 SeitenACS Management in JKN EraErwin Freddy HutabaratNoch keine Bewertungen
- Problem Pada Pasien Stroke Yang Dirawat Inap: Peran Apoteker Dalam Mencegah Drug RelatedDokument12 SeitenProblem Pada Pasien Stroke Yang Dirawat Inap: Peran Apoteker Dalam Mencegah Drug Relatedalisia difianaNoch keine Bewertungen
- Dual Antiplatelet Therapy Using Cilostazol For SecondaryDokument10 SeitenDual Antiplatelet Therapy Using Cilostazol For SecondarySyed Shabbir HaiderNoch keine Bewertungen
- Varun Kumar Biocon ReportDokument69 SeitenVarun Kumar Biocon Reportvarunsinha1986100% (1)
- PASSMED MRCP MCQs-CARDIOLOGY & - 40 15& - 41 PDFDokument128 SeitenPASSMED MRCP MCQs-CARDIOLOGY & - 40 15& - 41 PDFzeeshan ali100% (1)
- Perioperative Care For CABG PatientsDokument32 SeitenPerioperative Care For CABG PatientsAya EyadNoch keine Bewertungen
- Dissolution Testing of Bilayer TabletsDokument10 SeitenDissolution Testing of Bilayer TabletsAmjad KhanNoch keine Bewertungen
- Aspirin (Plus Antiplatelet Medicines) - What Is Aspirin - PatientDokument9 SeitenAspirin (Plus Antiplatelet Medicines) - What Is Aspirin - Patientaasuman123Noch keine Bewertungen
- DepakoteDokument5 SeitenDepakotejNoch keine Bewertungen
- SIGN 129 - Antithrombotics: Indications and Management: A National Clinical Guideline Updated June 2013Dokument75 SeitenSIGN 129 - Antithrombotics: Indications and Management: A National Clinical Guideline Updated June 2013Kumera Dinkisa ToleraNoch keine Bewertungen
- Periprocedural Anticoagulation Guidelines - UKDokument14 SeitenPeriprocedural Anticoagulation Guidelines - UKjoshNoch keine Bewertungen
- Drug Study ClopidogrelDokument3 SeitenDrug Study ClopidogrelTri Purma SariNoch keine Bewertungen
- Pharmacology Handout Dr. Ann SpolarichDokument16 SeitenPharmacology Handout Dr. Ann SpolarichMina Lotfallah ShenoudaNoch keine Bewertungen
- Drug Study Feu NRMF IcuDokument9 SeitenDrug Study Feu NRMF IcuAnne Genesis V. PinedaNoch keine Bewertungen
- Anti Platelets FKFKFKDokument17 SeitenAnti Platelets FKFKFKIndah Pujiati DtNoch keine Bewertungen
- Drug To Drug InteractionDokument47 SeitenDrug To Drug InteractionMannan SokaNoch keine Bewertungen
- Cardiovascular and Metabolic Syndrome MOCK Test: Pharmacy PREPDokument26 SeitenCardiovascular and Metabolic Syndrome MOCK Test: Pharmacy PREPNOORNoch keine Bewertungen
- De Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IDokument43 SeitenDe Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IAkhmad HidayatNoch keine Bewertungen
- BRAIN AneurysmDokument14 SeitenBRAIN AneurysmRikizu HobbiesNoch keine Bewertungen
- Jade R. Dinolan BSN-4: Diagnosi SDokument5 SeitenJade R. Dinolan BSN-4: Diagnosi SJhade Relleta100% (1)
- Antiplatelet and Thrombolytic DrugsDokument48 SeitenAntiplatelet and Thrombolytic DrugsNofa PuspitaNoch keine Bewertungen
- New Drugs and Technologies: PrasugrelDokument10 SeitenNew Drugs and Technologies: PrasugrelDewi FitrianaNoch keine Bewertungen
- Antiplatelet Therapy For The Secondary Prevention of Ischemic Stroke - UpToDateDokument13 SeitenAntiplatelet Therapy For The Secondary Prevention of Ischemic Stroke - UpToDateSuci WijayaNoch keine Bewertungen
- A Case of Acute Ischemic Stroke With Left HemiparesisDokument18 SeitenA Case of Acute Ischemic Stroke With Left HemiparesisSafoora RafeeqNoch keine Bewertungen
- Aspirin and Aspilet Compared PDFDokument18 SeitenAspirin and Aspilet Compared PDFEfrianti Viorenta HutapeaNoch keine Bewertungen
- Triple Antithrombotic Therapy For AF and Coronary StentsDokument7 SeitenTriple Antithrombotic Therapy For AF and Coronary Stentsyesid urregoNoch keine Bewertungen
- The Pathological Effects of Hyperglycaemia On The Cardiovascular (CV) System and BrainDokument5 SeitenThe Pathological Effects of Hyperglycaemia On The Cardiovascular (CV) System and BrainRyzka Izza MayFanyNoch keine Bewertungen
- Case Analysis Kwento Ni RosarioDokument17 SeitenCase Analysis Kwento Ni RosarioMeg YunsonNoch keine Bewertungen
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 4.5 von 5 Sternen4.5/5 (82)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesVon EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesBewertung: 4.5 von 5 Sternen4.5/5 (1412)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4.5 von 5 Sternen4.5/5 (6)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (254)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceVon EverandTo Explain the World: The Discovery of Modern ScienceBewertung: 3.5 von 5 Sternen3.5/5 (51)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsVon EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsBewertung: 4.5 von 5 Sternen4.5/5 (39)
- The Marshmallow Test: Mastering Self-ControlVon EverandThe Marshmallow Test: Mastering Self-ControlBewertung: 4.5 von 5 Sternen4.5/5 (60)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingVon EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingBewertung: 4 von 5 Sternen4/5 (1138)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)