Beruflich Dokumente
Kultur Dokumente
Uterine Fibroid Thermometry
Hochgeladen von
Eva YeungOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Uterine Fibroid Thermometry
Hochgeladen von
Eva YeungCopyright:
Verfügbare Formate
MRI Guidance of Focused
Ultrasound Therapy of Uterine
Jonathan Hindley1 Fibroids: Early Results
Wladyslaw M. Gedroyc1
Lesley Regan1
Elizabeth Stewart2 OBJECTIVE. The purpose of this study was to explore our hypothesis that MRI-guided
Clare Tempany2 focused ultrasound therapy for the treatment of uterine fibroids will lead to a significant re-
Kullervo Hynnen2 duction in symptoms and improvement in quality of life. We describe focused ultrasound
Nathan Macdanold2 therapy applications and the method for monitoring the thermal energy deposited in the fi-
broids, including the MRI parameters required, in a prospective review of 108 treatments.
Yael Inbar3
MATERIALS AND METHODS. Patients presenting with symptomatic uterine fibroids
Yacov Itzchak3
who attained a minimal symptom severity score and who would otherwise have been offered
Jaron Rabinovici3 a hysterectomy were recruited. Thermal lesions were created within target fibroids using an
Kevin Kim4 MRI-guided focused ultrasound therapy system. The developing lesion was monitored using
Jean-François Geschwind4 real-time MR thermometry, which was used to assess treatment outcome in real time to
Gina Hesley5 change treatment parameters and achieve the desired outcome.
Brian Gostout5 Fibroid volume, fibroid symptoms, and quality-of-life scores were measured before treat-
Tillman Ehrenstein6 ment and 6 months after treatment. Adverse events were actively monitored and recorded.
Sylvia Hengst6 RESULTS. In this study, 79.3% of women who had been treated reported a significant improve-
Miri Sklair-Levy7 ment in their uterine fibroid symptoms on follow-up health-related quality-of-life questionnaires,
Asher Shushan7 which supports our hypothesis. The mean reduction in fibroid volume at 6 months was 13.5%, but
nonenhancing volume (mean, 51 cm3) remained within the treated fibroid at 6 months.
Ferenc Jolesz2
CONCLUSION. This early description of MRI-guided focused ultrasound therapy treat-
ment of fibroids includes follow-up data and shows that, although the volume reduction is
moderate, it correlates with treatment volume and the symptomatic response to this treatment
Received February 23, 2004; accepted after revision is encouraging.
May 15, 2004.
1Departments of Magnetic Resonance Imaging and
Academic Obstetrics and Gynaecology, Interventional MR
Unit, St Mary's Hospital London and Imperial College
School of Medicine, Praed St., London W2 1NY, England.
Address correspondence to W. Gedroyc
(w.gedroyc@imperial.ac.uk).
T he ability of ultrasound energy to
interact with biologic tissues has
been recognized for many years.
The earliest medical uses of ultrasound were
the direction of the ultrasound beam [3]. The
tissue in the path of the ultrasound beam but
away from the focus is warmed, but not to le-
thal temperatures, avoiding tissue damage ex-
2Departments of Obstetrics and Gynaecology and therapeutic rather than diagnostic, and the cept at the focus.
Reproductive Biology and Radiology, Brigham and Women’s ability of ultrasound energy to cause a rise in The possibility that focused ultrasound ther-
Hospital and Harvard Medical School, Boston, MA 02115.
3
tissue temperature was recognized as long apy might be developed as a result of control-
Department of Radiology and Obstetrics and
Gynaecology, Sheba Medical Centre, Tel-Hashomer 91120,
ago as 1927 [1]. ling these heating phenomena was introduced
Israel. Ultrasound energy propagates harmlessly by Lynn et al. [4] in the middle of the last cen-
4
Department of Radiology, Johns Hopkins School of through tissue with small amounts of energy tury. Their work was closely followed by the
Medicine, Baltimore, MD 21287. being absorbed; this energy is deposited as first descriptions of focused ultrasound therapy
5
Department of Radiology and Obstetrics and heat but is dissipated by the cooling effects of as a noninvasive surgical technique in the brain
Gynaecology, Mayo Clinic, Rochester, MN 55905. perfusion and conduction. If, however, the ul- [5]. These early uses of focused ultrasound ther-
6 trasound beam carries a high level of energy apy for Parkinson’s disease were quickly super-
Department of Radiology, Charité Medical Centre and
Humboldt University, Virchow Clinic Campus, Berlin and is brought to a tight focus, energy carried seded by drug therapies, and further
D-13353, Germany.
by the beam is rapidly converted into heat and development of this technology was delayed
7
Department of Radiology, Hadassah Medical Centre, a rise in temperature is observed [2]. If the until a resurgence in the 1990s [6]. In recent
Jerusalem 52621, Israel.
temperature at the target spot can be raised to years, focused ultrasound therapy has been used
AJR 2004;183:1713–1719
more than 55°C, protein denaturation occurs, in urology for the treatment of benign prostatic
0361–803X/04/1836–1713 resulting in cell death and the creation of a ci- hyperplasia [7, 8] and in the management of
© American Roentgen Ray Society gar-shaped lesion of coagulative necrosis in cancer of the prostate [9, 10]. There has been an
AJR:183, December 2004 1713
Hindley et al.
increase in interest in the use of focused ultra- more than 18 years old and had stated that they had The anatomic suitability for MRI-guided fo-
sound therapy in the central nervous system no future child-bearing plans. Patients who had cused ultrasound therapy was assessed using ei-
[11], and reports of soft-tissue tumors of the other pelvic or uncontrolled systemic disease were ther MRI or sonography. A clear pathway from the
liver and kidney being treated with focused ul- excluded, as were postmenopausal women, women anterior abdominal wall to the fibroid without
who weighed more than 250 lb (113 kg) (because passing through the bladder or the bowel was re-
trasound therapy are encouraging [12].
this is above the tolerance for the MRI gantry), and quired by the protocol. Fibroids greater than 10 cm
The use of focused ultrasound therapy has women who were unable to communicate with the in diameter or women with uteri greater than a 24-
been hampered by the difficulty in precise researchers during the treatment. Women who were week pregnancy equivalent were excluded from
targeting of the ultrasound beam and in re- unsuitable for MRI, such as those with cardiac pace- this early study.
ceiving feedback regarding the thermal dam- makers, were also ineligible for the study. All in- In total, 109 patients were treated at seven sites.
age created. Ultrasound guidance has been cluded women had undergone cervical smears as Fifty-two patients were treated within the United
used to target the ultrasound energy, but its required according to local guidelines. All women States, and 57 patients were treated in Europe and
thermal sensitivity is limited and therefore had negative pregnancy tests both at recruitment and Israel. The mean age was 44.8 years (range, 30–
real-time thermometry is problematic. immediately before the treatment. Women who had 58 years; SD ± 4.9). The proportion of black (Afri-
MRI guidance of focused ultrasound ther- changed their use of oral contraceptive preparation can American, African, or African Caribbean) pa-
or of nonsteroidal preparations to control menstrual tients was 11%, and the mean body mass index
apy has been explored during the past decade
loss in the preceding 3 months were ineligible for was 25.8 (range, 18.6–3.9; SD ± 5.2).
[13], and it has several attractive attributes. The the study. Women who had undergone previous ab- Of the fibroids treated, 22% were submucosal,
excellent soft-tissue resolution afforded by dominal surgery were examined for scars, and if 57% were intramural, and 21% were subserosal.
MRI enables accurate planning of the tissue to these were extensive or obviously in the path of the Those fibroids that were intramural required disrup-
be targeted. MRI parameters have an intrinsic ultrasound beam, these patients were excluded from tion to the myometrium in conventional surgery.
sensitivity to temperature change and therefore the study. Previous experience has shown that such Before the treatment, each patient was asked to
can be adapted to provide accurate, near real- scars have high ultrasound absorption as compared shave her anterior abdomen from the umbilicus to
time thermometry, and thermal damage cre- with regular tissue and may lead to pain and even the level of the upper margin of the symphysis pu-
ated by focused ultrasound therapy can be as- thermal damage at the skin surface. bis. It has been noted in previous studies [20] that
sessed immediately using MRI. This multicenter phase III clinical trial study the presence of hairs in the sonication pathway
was performed according to principles of good was associated with the formation of small air
The shift in proton resonant frequency with
clinical practice as defined by the Declaration of bubbles that absorb the ultrasound energy and po-
a rise in temperature can be detected using Helsinki. The participating sites were situated in tentially cause heating at the skin surface and even
phase imaging [14]. If sequential phase-shift Europe [2], the United States [3], and Israel [2]. skin burns.
MR images obtained during an ultrasound All sites had local approval from their ethics com- An additional pregnancy test was performed on
sonication are compared with an image ob- mittees or institutional review boards. All patients the day of treatment. All patients were counseled re-
tained immediately before that sonication, the gave fully informed consent. garding the lack of safety data for pregnancy after
changes in those images can be calibrated to Suitable subjects were asked to complete the first MRI-guided focused ultrasound therapy and, in par-
create a real-time thermal map of the increas- eight questions of a Uterine Fibroid Symptoms and ticular, the possible theoretic risk of uterine rupture
ing temperature at and close to the target [15]. Quality of Life Questionnaire [21]. Responses are suggested by the experience of women who became
The MRI-guided focused ultrasound therapy scored from 1 (not distressed) to 5 (distressed a great pregnant after undergoing laparoscopic laser myoly-
deal) and provide a screening tool for fibroid symp- sis for fibroids [22, 23]. A urinary catheter was in-
system used in this study (ExAblate 2000, In-
toms with possible results from 8 to 40. A minimum serted before the patients were positioned on the
Sightec) integrates fully with a 1.5-T MRI sys- score of 21 points was required for inclusion in the ExAblate 2000 focused ultrasound therapy system.
tem (Signa, GE Healthcare) to enable focused study. Women who scored more than 21 on the The patients were placed in the prone position on the
ultrasound therapy to be planned directly with screening questionnaire and who were enrolled in system with the fibroid placed above the transducer
MR images and to give real-time MR ther- the study went on to complete the full Uterine Fi- (Fig. 1). To ensure that an acoustic pathway was
mometry feedback of each sonication. This broid Symptoms and Quality of Life Questionnaire maintained, the transducer was positioned on the
system, or its earlier prototypes [16], has been form consisting of 37 questions. MRI table in a sealed tank of degassed water. The
used to create lesions in several different body
tissues [17–19].
MRI-guided focused ultrasound therapy
for fibroids has been shown to be a safe and
feasible treatment for uterine fibroids [20].
This article describes the details of MRI-
guided focused ultrasound therapy for fi-
broids and presents the early results of this
procedure in addition to posttreatment
changes in fibroid volumes.
Materials and Methods
Patients who presented to gynecology clinics in
participating hospitals with symptomatic fibroids
and who would otherwise have been offered conven-
tional surgical therapy were considered for MRI- Fig. 1.—Schematic representation of patient lying on ExAblate 2000 (InSightec) focused ultrasound system ready
guided focused ultrasound therapy. All patients were to be placed into MRI unit. Ultrasound transducer found in sealed water bath within MR table.
1714 AJR:183, December 2004
Focused Ultrasound Therapy of Uterine Fibroids
Fig. 2.—T2-weighted image of 38-year-old woman with symptomatic fibroids ready for Fig. 3.—Phase-shift image taken 22.2 sec after onset of sonication in 38-year-old
MRI-guided focused ultrasound therapy. She is lying prone on gel pad, which is above woman with symptomatic fibroids. High-signal area is visible due to rise in tem-
focused ultrasound therapy transducer. Sonication pathway is superimposed on image perature and can be seen along sonication pathway. Signal is greatest within tar-
and has been angled craniocaudally to avoid small bowel close to uterus. Spot where get spot and it is this area that has been heated sufficiently to cause irreversible
irreversible thermal damage is expected is also superimposed onto this image. Figure is damage. Heating of anterior pathway will be dissipated by perfusion during cool-
screen capture from ExAblate 2000 system (InSightec) at time of treatment. ing period between sonications. Figure is screen capture from ExAblate 2000 sys-
tem (InSightec) during treatment.
acoustic pathway then passed from the transducer power sonication is monitored by a thermal map used to calculate the thermal dose, and those voxels
through a thin membrane into a gel pad on which the [14] created in the coronal plane and repeated with with the dose above a threshold value of 240 equiv-
patient lay. a thermal map in the sagittal or axial plane to en- alent min at 438°C are indicated on the images [15].
Once positioned, the patient is placed into the sure that both the lateral and longitudinal targeting Thus, for each sonication a complete picture of the
MRI scanner, and the patient’s position and the are as planned. Any errors are corrected before re- tissue effect is created. Although a typical power of
sonication pathway is checked using MR images peating the verification at a therapeutic power. 140 W for 20 sec and 1.0 MHz and fibroids with an
(TR/TE, 3,600/102; matrix, 256 × 224; echo-train Once the operators are satisfied that the targeting average depth of 7 cm will lead to a rise in tempera-
length, 16; field of view, 36 cm; number of excita- is accurate, they proceed to the treatment cycle. ture to about 60°C in a fibroid, this rise is extremely
tions, 2; slice thickness, 4 mm; slice spacing, 1 The treatment itself consists of consecutive variable. It is this extreme variation in response, both
mm; scanning time, approximately 2 min 2 sec) sonications producing thermal lesions within the between and within fibroids, that makes real-time
(Fig. 2). The patient’s pelvis is imaged using T2- previously defined target area to produce a single thermal mapping so vital to the balance of safety and
weighted fast spin-echo images in the coronal, ax- large area of ablated tissue. Each sonication is efficacy in MRI-guided focused ultrasound therapy
ial, and sagittal planes. These images are then monitored using phase subtraction fast gradient- ablation of fibroids.
transferred to the workstation of the focused ultra- echo proton resonance frequency-shift-dependent Most sonication parameters can be changed in
sound therapy system in which the volume to be techniques [14]. response to the thermal maps being created. The
ablated is defined by the physician. The system Typical parameters for these scans were TR/RE, power applied can be increased or decreased.
plots the individual sonications and shows the 27/13 msec; flip angle, 30º; bandwidth, 5.68 kHz; Clearly, greater power will lead to the generation
pathway that each sonication will require. These matrix, 256 × 128; field of view, 28 cm2; and slice of a higher temperature. The aim is to reach a
pathways are carefully checked to ensure that they thickness, 3/5 mm. threshold temperature without approaching higher
do not pass through any structures that ought to be The focused ultrasound therapy system enslaves temperatures at which control of the thermal effect
avoided—such as the small bowel—that can fall in the MRI system to ensure that these sequences are may be compromised. The time for which the en-
front of the uterus. The far beam also is checked, timed and positioned to coincide with the deposition ergy is applied can be changed. Higher power for a
because some energy deposition remains after the of ultrasound energy. A baseline image is created shorter time may compensate for the cooling ef-
beam has passed through the fibroid, and struc- immediately before the sonication, and subsequent fect of perfusion in a highly vascular fibroid. The
tures such as large neurovascular bundles should images are created every few seconds during a sin- cooling time after each sonication can be assessed
be avoided. The transducer can be tilted in all di- gle heating and early cooling phase (Fig. 3). The im- by extending the thermal map into the cooling pe-
rections by up to ± 20° to find a suitable pathway. ages are compared and presented as a thermal map riod. The default cooling period of 90 sec may be
Once correct positioning has been achieved, the either as simple subtraction images or colorized with altered if the thermal map suggests that a return to
target volume defined, and the treatment planned, a threshold temperature. A graph of the temperature baseline temperature is achieved in a shorter time
verification sonications are performed. These soni- rise over time also is created to enable actual temper- or indeed if it requires more time.
cations are subtherapeutic at low power, typically atures to be assessed at any point (Fig. 4). The time The spot size can be altered in both diameter
10–70 W for 10–20 sec at 1.0 MHz. This low- and temperature information for each voxel also is and length so that the target volume can be ablated
AJR:183, December 2004 1715
Hindley et al.
Immediately after completion of the treatment,
an MRI gadolinium-based contrast agent (Omnis-
can [gadodiamide], Nycomed Amersham or equiva-
lent) was given and the effectiveness of the
treatment was assessed by measuring the nonper-
fused area that had been created in the target fibroid.
We used the following scanning parameters: T1-
weighted fast-spoiled (radiofrequency-spoiled) gra-
dient-echo, TR/TE, 200/1.2; flip angle, 75°; matrix,
256 × 128; zero interpolated to 5122; number of
excitations, 2; field of view, 36; slice thickness, 4
mm; slice spacing, 1 mm; scan time, approximately
52 sec for 17 slices (Fig. 5). The MR images were
sent to a central core laboratory where the fibroid
volume and the nonenhancing volume were mea-
sured using a standard method as described below.
The fibroid was identified on each slice, and the
Fig. 4.—Graph of temperature against sonication time. Green represents average temperature within target vol-
ume; red represents absolute temperature at specified point. This sonication has resulted in maximum temper- area of the fibroid on each image was estimated by
ature of 91.8°C. This is higher than is necessary for irreversible damage so this information can be used to drawing around that area on the workstation and us-
shorten sonication time or reduce acoustic power for subsequent sonications. Figure is screen capture from Ex- ing the workstation software to calculate the defined
Ablate 2000 system (InSightec) during treatment. area. The areas of fibroid from each slice then were
summated and multiplied by the sum of the slice
with as few sonications as possible while main- All patients remained conscious during the thickness and the interval between slices to calcu-
taining accuracy and control. treatment and were given IV analgesia and con- late the volume. This was repeated for the volume
The sonication frequency also can be altered. scious sedation as required. They remained in that did not enhance after contrast. This volume is
Increasing the transducer frequency will result in constant verbal communication with the opera- known to correspond to the thermal lesion [20].
more energy being absorbed in the near field thus tors and were asked to report any pain or dis- Before treatment, the patients were assessed for
decreasing the chance of heat buildup in structures comfort. The patients held an emergency stop symptoms and for the impact that the fibroids had
such as bone and nerves in the far field; similarly, button at all times, which enabled them to halt made on their quality of life using the Uterine Fi-
decreasing the transducer frequency will reduce further sonication. broid Symptoms and Quality of Life question-
the near-field absorption, limiting the chance of Once all the sonications in a target volume had naire. This is a disease-specific questionnaire that
skin-heating, decreasing aberration caused by the been completed, additional fibroid treatment could was developed to assess the efficacy of fibroid
beam passing through irregular structures such as be planned, up to a maximum treatment time of 3 therapies [21]. This questionnaire was used before
the muscles of the anterior abdominal wall, and in- hr or a maximum ablated volume of 100 cm3 per treatment and at 3 and 6 months after MRI-guided
creasing the depth at which treatment is possible. fibroid and a total of 150 cm3 per patient with mul- focused ultrasound therapy. The primary end-point
In our study, up to four fibroids were treated in tiple treated fibroids. This maximum treatment hypothesis for the study was defined as an im-
any one patient. A minimum margin of 1.5 cm from volume was a stipulation of the regulatory authori- provement in the Uterine Fibroid Symptoms and
the edge of the ablated area to the edge of the uterus ties and may have led to suboptimal treatment in Quality of Life Questionnaire of 10 points for at
(serosal or mucosal surfaces) was stipulated. patients with large or multiple fibroids. least 50% of patients.
Fig. 5.—41-year-old woman with symptomatic uterine fibroids.
A, T2-weighted sagittal image shows fibroid before treatment.
B, T1-weighted gadolinium-enhanced sagittal image with
fat saturation of same fibroid obtained immediately after
MRI-guided focused ultrasound therapy shows area of re-
duced enhancement corresponding to area of ablation.
A B
1716 AJR:183, December 2004
Focused Ultrasound Therapy of Uterine Fibroids
Thorough clinical examinations of the patients mally with the transducer. It was noted early in lated adverse event. This patient underwent
were performed immediately after treatment and 1 the study that the likelihood of the patient uterine artery embolization. An additional
week, 1 month, 3 months, and 6 months later. A complaining about leg or buttock pain in- patient was asked to remain in the hospital
structured interview was used to ensure that com- creased if the sacrum was in the direct far field overnight because of nausea after the treat-
mon or expected adverse events were identified
of the sonication pathway close to the target ment. This was a treatment-related event and
and recorded. Serious adverse events as defined by
the protocol (see Table 1) were reported to the lo-
area. This was presumed to be related to ther- represents the only early posttreatment
cal ethics committee or institutional review board mal nerve stimulation in the far field where a admission but probably was related to the
and to the regulatory authority (the U.S. Food and nerve passes in close proximity to the sacrum opioid analgesia used rather than the MRI-
Drug Administration, the Medical Devices Agency (3–5 mm) and patients were positioned to guided focused ultrasound therapy itself.
in the United Kingdom, and the National Helsinki maximize the distance between the thermal This patient recovered overnight and was
Committee in Israel). Adverse events were classi- spot and the pelvis in the far field. This usually discharged the next day.
fied according to whether they were device re- can be achieved by positioning the patient with Two patients reported serious adverse
lated, disease related, or incidental. the fibroid farther back so the transducer can events that were not thought to be related to
be angled caudad (Fig. 2). the treatment in any way. One had a preexist-
Results The pain and discomfort as reported by ing brain tumor that progressed during the
One hundred nine patients were treated at patients before, during, and immediately af- period of follow-up. The brain tumor was not
seven sites. Fifty two patients were treated in ter treatment were assessed on a 4-point thought to be related to the treatment and, in-
the United States, and 57 patients were scale, with 0 = none, 1 = mild, 2 = moderate, deed, the patient had excellent symptom re-
treated in Europe and Israel (age range, 30– and 3 = severe. The pain and discomfort lief. The other patient required admission
58 years; mean, 44.8 ± 4.9 [SD] years). The scores are outlined in Table 1. Although 16% with a urinary tract infection some 14 weeks
proportion of black (African American, Afri- of patients complained that the pain was se- after the treatment. She made a full recovery
can, or African Caribbean) patients was vere during the procedure, only 1% and 7% with antibiotic therapy, and it was thought
11%, and the mean body-mass index was stated that they were in severe or moderate that the temporal relationship between the
25.8 (range, 18.6–43.9; mean, ± 5.2). pain, respectively, when questioned immedi- treatment and the event made causation ex-
Of the fibroids treated, 22% were submu- ately after the treatment. ceedingly unlikely.
cosal, 57% were intramural, and 21% were Nine serious adverse events were re- One patient complained of leg and buttock
subserosal. Intramural fibroids definitively ported; of these, only one was thought defi- pain immediately after the treatment. Exami-
require disruption of the myometrium in nitely to be device related. Five of the nation of the MR images showed that the
conventional surgery. patients had continued heavy menses in the sciatic nerve was in the far field of the soni-
The mean fibroid volume in patients in weeks after the treatment, requiring blood cation pathway. Detailed MR neurography
whom only a single fibroid was treated (n = transfusions. These were thought to be re- and electromyography studies, however,
60) was 346 cm3, ± 245 cm3. In patients with lated to the underlying cause (i.e., fibroids) failed to show any intrinsic nerve damage.
multiple fibroids being treated (n = 32), the rather than to the treatment. Two of these pa- The patient subsequently made a complete
mean fibroid volume was correspondingly tients withdrew from the study to undergo recovery by the follow-up visit using only
less at 294 cm3, ± 188 cm3. The region of definitive treatment in the form of hysterec- conservative measures. The patient also had
treatment as defined by the operators before tomy. One patient reported pain and bleeding excellent symptomatic relief from fibroid-re-
sonication was 39 cm3 (± 27 cm3) for single after the treatment. These symptoms were lated symptoms and had made a complete re-
fibroids and a similar 38 cm3 (± 24 cm3) for consistent with the patient’s symptoms be- covery by the final follow-up visit. This case
multiple fibroid treatments. The actual vol- fore the treatment and were thought to reflect led to a change in operator practice, and 4 cm
ume that received a thermal dose as mea- a treatment failure rather than a device-re- is now considered the minimum distance be-
sured using MR thermometry was 36 cm3
(± 18 cm3)—around 10% of the fibroid vol-
ume, and 32 cm3 (± 23 cm3)—about 11% of TABLE 1
Pain and Overall Discomfort Before, During, and Immediately After
MRI-Guided Focused Ultrasound Therapy
the fibroid volume, for single and multiple
treatments, respectively. Before During After
The posttreatment contrast-enhanced im- Variable
No. % No. % No. %
ages showed that the volume of the fibroid
that was nonperfused was greater than the Pain
thermal dose volume at 86 cm3 (± 82 cm3) None 99 91 19 18 79 75
for patients with single fibroids and 85 cm3 Mild 6 6 36 33 19 18
(± 88 cm3) for those who had multiple fi- Moderate 2 2 36 33 7 7
broids treated; 25% and 29% of the fibroids Severe 2 2 17 16 1 1
volume, respectively. Overall discomfort
The mean time that the patients were in the None 79 72 32 30 72 68
MR scanner was 202 min (range, 90–370 min; Mild 21 19 35 33 27 25
± 56). This time is variable because much of
Moderate 7 6 31 29 7 7
the time is taken with positioning the patient
Severe 2 2 9 8 0 0
correctly to align the sonication pathway opti-
AJR:183, December 2004 1717
Hindley et al.
tween the spot and any major nerve bundles ergy delivered via the laparoscopic approach area may represent an area of burn that has
that are in close proximity to a bone surface. [26]. This resulted in significant reduction in yet to resolve. If this is the case, it is reason-
The other reported adverse events were mi- fibroid size and resolution of symptoms but able to expect further shrinkage beyond the
nor and transitory. was associated with significant side effects 6-month follow-up reported here. This is the
At 6-month follow-up, the mean fibroid vol- [27, 28]. Many of these side effects seem to case with MRI-guided laser ablation of fi-
ume was reduced by 13.5%, ± 32. Although have been negated by using an MRI-guided broids—an analogous technique also result-
the change in fibroid volume is modest, the av- technique for laser ablation with MR ther- ing in thermal damage [30]. Confirmation of
erage relative treatment volume was approxi- mometry giving real-time feedback to control this hypothesis will result when longer fol-
mately 0% and the average nonperfused the thermal lesion created [29]. Despite the low-up is available. If the nonperfused vol-
volume at the end of the treatment was approx- low incidence of adverse events, MRI-guided ume is not an unresolved burn, it is likely to
imately 25%, which should have an impact on laser ablation of fibroids appears to remain an be collagen deposits formed as a result of the
the modest shrinkage. In addition, a mean non- effective therapy for the treatment of symp- burn. If this is the case, it may be that the im-
perfused volume of 51.2 cm3 (± 62.2 cm3) ex- tomatic uterine fibroids [30]. provement in fibroid symptoms is not, in
ists on contrast-enhanced MR images at 6- To our knowledge, we have presented the fact, volume dependent but caused by the de-
month follow-up. This may represent future first short-term follow-up study using MRI- struction of the leiomyoma cells and the
shrinkage and certainly represents nonviable guided focused ultrasound therapy for uter- breakdown of local secretory pathways. The
fibroid tissue. ine fibroids. This article outlines the radiologic mechanisms by which fibroid symptoms are
Clinical follow-up shows that 79.3% of parameters involved in this new treatment mediated are not yet fully explained.
patients achieved a greater than 10-point re- technique, and we have discussed the radio- The lesion produced is shown as the non-
duction in the Uterine Fibroid Symptoms logic appearances of the uterus immediately enhancing volume in the immediate posttreat-
and Quality of Life Questionnaire score (n = after and 6 months after this treatment. Our ment contrast-enhanced MR images and is
82, p < 0.0001), thereby proving the primary study shows that, despite only a small larger that the volume expected from thermal
endpoint hypothesis to be correct. The mean change in leiomyomata volume, MRI-guided damage alone. The mechanism by which this
reduction in the symptom severity score on focused ultrasound therapy results in a occurs has not been elucidated. It may be that
Uterine Fibroid Symptoms and Quality of marked symptomatic improvement in most the temperature required for lethal damage in
Life Questionnaire was in fact 27.3 points patients at 6-month follow-up. This improve- fibroid tissue is lower than the 55°C threshold
(p < 0.0.0001; range, 18.75– -81.25 points), ment is equally marked for pressure symp- that we believed was required, but this seems
and although most of this improvement oc- toms and menstrual bleeding symptoms. unlikely because the expansion in the lesion
curs in the first 3 months after treatment There seemed to be greater improvement re- occurs laterally as well as in the direction of
(24.1 points), improvement continues between ported in the Uterine Fibroid Symptoms and the sonication pathway. This expansion may
3 and 6 months. The Uterine Fibroid Symptoms Quality of Life Questionnaire by patients who be a result of the passage of mediators of apo-
and Quality of Life Questionnaire can be bro- had a greater proportion of the fibroid treated. ptosis from the lethally damaged cells to their
ken down into symptoms caused by mass ef- The average improvement in the scores was neighbors [20], as previously shown in gene
fect—where improvement is 32.8 points (63.9/ 25.8 at 6 months in those patients in which the transfection experiments on leiomyomas
100–31.2/100)—or bleeding symptoms—in nonperfused volume on contrast-enhanced MR [31]. Other mechanisms may be responsible.
which improvement is reported to be 32.8 images obtained immediately after treatment These may include the thermal occlusion of
points (60.1/100–25.3/100). represented less than 30% of the fibroid vol- internal fibroid blood vessels leading to areas
ume compared with an improvement of 31.7 in of infarction, as has been shown in animal
patients who had more than 30% of the fibroid models [32]. The striking absence of pain af-
Discussion treated. The volume of the fibroid treated was ter the procedure, in stark contrast to uterine
Uterine fibroids are a significant cause of limited by safety margins imposed by the regu- artery embolization, suggests that pain is not
personal, social, and financial problems for latory authorities. These restrictions now have a major component in the tissue destruction
many women of childbearing age [24]. The been lifted, and the challenge remains to in- caused by MRI-guided focused ultrasound
fibrosis may be asymptomatic, but when crease the proportion of the fibroid that is ther- therapy. Local edema produced as a result of
women seek help they usually complain of mally ablated while avoiding thermal damage the thermal damage may cause a pressure rise
bleeding problems, typically heavy and pain- outside the fibroid (i.e., damage to the myo- within the fibroid. Although fibroids are not
ful menses, pressure symptoms (most often metrium, endometrium, or serosal surface). We strictly encapsulated, they tend to have well-
urinary frequency and nocturia), or problems believe that the real-time thermal map, which is demarcated edges effectively producing the
related to fertility and pregnancy [25]. Tra- integral to the performance of focused ultra- same effect as a capsule so that edema within
ditionally, and still most commonly, treat- sound therapy using the technique described, the fibroid would cause a rise in pressure that
ment for fibroids has been surgical. In recent will allow this challenge to be met. may be sufficient to explain the local exten-
years, a number of less-invasive alternatives Analysis of the contrast-enhanced images sion of the lethal volume. Another possibility
to open hysterectomy and myomectomy at 6 months reveals that in many cases the is that the delay between sonications (approx-
have been developed. The most popular of volume of the fibroid that remains nonen- imately 60–90 sec) was not sufficient to avoid
these has been hysteroscopic resection of fi- hancing is significant and therefore is not thermal buildup in the ultrasound beam path
broids and uterine artery embolization. perfused. The mean nonperfused volume on over the course of multiple sonications [33].
Thermoablative treatments for uterine fi- the 6-month contrast-enhanced scans was Because the MR thermometry only measured
broids initially were developed using laser en- 51.2 cm3 (± 62.2 cm3). This nonperfused temperature changes and a new baseline im-
1718 AJR:183, December 2004
Focused Ultrasound Therapy of Uterine Fibroids
age was acquired before each sonication, this trasound. IRE Trans Med Electron 1960;ME- 19. Tempany CM, Stewart EA, McDannold N, Quade
slow buildup of heat would not be detected 7:166–181 BJ, Jolesz FA, Hynynen K. MR imaging guided
6. Ballantine HT Jr, Bell E, Manlapaz J. Progress and focused ultrasound surgery of uterine leiomyo-
during the treatment. However, this effect
problems in the neurological application of focused mas: a feasibility study. Radiology 2003;226:
could not be the full explanation because ultrasound. J Neurosurg 1960;17:858–876 897–905
cases existed in which regions were nonen- 7. Uchida T, Muramoto M, Kyunou H, Iwamura M, 20. Stewart EA, Gedroyc WM, Tempany CM, et al.
hancing that were distant from the targeted Egawa S, Koshiba K. Clinical outcome of high- Focused ultrasound treatment of uterine fibroid
zone and clearly unheated. Further studies intensity focused ultrasound for treating benign tumors: safety and feasibility of a noninvasive
will be needed fully to explain this phenome- prostatic hyperplasia: preliminary report. Urology thermoablative technique. Am J Obstet Gynecol
non, which may of course have a multifacto- 1998;52:66–71 2003;189:48–54
8. Madersbacher S, Kratzik C, Susani M, Marberger 21. Spies JB, Coyne K, Guaou Guaou N, Boyle D,
rial explanation. It is clear that the expansion
M. Tissue ablation in benign prostatic hyperplasia Skyrnarz-Murphy K, Gonzalves SM. The UFS-
of the lesion is confined in all cases to the with high intensity focused ultrasound. J Urol QOL, a new disease-specific symptom and health-
treated fibroid with no examples of damage 1994;152:1956–1960 related quality of life questionnaire for leiomy-
to the myometrium or endometrium beyond. 9. Madersbacher S, Pedevilla M, Vingers L, Susani omata. Obstet Gynecol 2002;99:290–300
We believe that MRI-guided focused ultra- M, Marberger M. Effect of high intensity focused 22. Arcangeli S, Pasquarette M. Gravid uterine rup-
sound therapy provides a potentially important ultrasound on human prostate cancer in vivo. ture after myolysis. Obstet Gynecol 1997;89:857
Cancer Res 1995;55:3346–3351 23. Vilos GA, Daly LJ, Tse BM. Pregnancy outcome
new noninvasive and effective treatment for
10. Gelet A, Chapelon JY, Bouvier R, et al. Treatment after laparoscopic electromyolysis. J Am Assoc
uterine fibroids, particularly in women who of prostate cancer with transrectal focused ultra- Gynecol Laparosc 1998;5:289–292
wish to avoid invasive or painful therapies. In sound: early clinical experience. Eur Urol 1996; 24. Buttram VC Jr, Reiter RC. Uterine leiomyomata:
particular, the total lack of invasiveness of 29:174–183 etiology, symptomatology, and management. Fer-
MRI-guided focused ultrasound therapy com- 11. McDannold N, Moss M, Killiany R, et al. MRI- til Steril 1981;36:433–445
pared with all other fibroid procedures and the guided focused ultrasound surgery in the brain: 25. Stewart EA. Uterine fibroids: seminar. Lancet
tests in a primate model. Magn Reson Med 2001;357:293–298
fact that the procedure is performed as an out-
2003;49:1188–1191 26. Goldfarb HA. Nd:YAG laser laparoscopic coagu-
patient procedure make it particularly attrac- 12. ter Haar GR, Rivens IH, Moskovic E, Huddart R, lation of symptomatic myomas. J Reprod Med
tive for patients. Visioli A. Phase 1 clinical trial of the use of focused 1992;37:636–638
We also believe that MRI-guided focused ultrasound surgery for the treatment of soft tissue 27. Donnez J, Squifflet J, Polet R, Nisolle M. Laparo-
ultrasound therapy for fibroids may prove to tumours. In: Ryan TP, ed. Surgical appliances of scopic myolysis. Hum Reprod Update 2000;
be an important model for the spread of this energy. Bellingham, WA: International Society for 6:609–613
noninvasive, precise, controlled, tissue-de- Optical Engineering, 1998: 270–276 28. Nisolle M, Smets M, Malvaux V, Anaf V, Donnez
13. Cline HE, Schenck JF, Hynynen K, Watkins RD, J. Laparoscopic myolysis with the Nd: YAG laser.
structive technology to other disorders in a
Souza SP, Jolesz FA. MR-guided focused ultrasound J Gynecol Surg 1993;9:95–99
variety of organs. surgery. J Comput Assist Tomogr 1992; 16:956–965 29. Law PA, Gedroyc WM, Regan L. Magnetic reso-
14. Ishihara Y, Calderon A, Watanabe H, Okamoto K, nance guided percutaneous laser ablation of uter-
Suzuki Y, Kuroda K. A precise and fast tem- ine fibroids. Lancet 1999;354:2049–2050
References perature mapping using water proton chemical 30. Hindley JT, Law PA, Hickey M, et al. Clinical out-
1. ter Haar G. Wood and Loomis: the physical and shift. Magn Reson Med 1995;34:814–823 comes following percutaneous magnetic resonance
biological effects of high frequency sound waves 15. Chung A, Jolesz FA, Hynynen K. Thermal dosim- image guided laser ablation of symptomatic uterine
of great intensity. Phil Mag 1927;4:7–14 etry of a focused ultrasound beam in vivo by fibroids. Hum Reprod 2002;17:2737– 2741
2. ter Haar G. Therapeutic ultrasound. Eur J Ultra- MRI. Med Phys 1999;26:2017–2026 31. Niu H, Simari RD, Zimmermann EM, Christ-
sound 1999;9:3–9 16. Hynynen K, Freund W, Cline HE, et al. A clinical man GM. Nonviral, vector-mediated thymidine
3. Lele PP. Threshold and mechanisms of ultrasonic noninvasive MRI monitored ultrasound surgery kinase gene transfer and ganciclovir treatment
damage to organized animal tissues. Proceedings of a method. RadioGraphics 1996;16:185–195 in leiomyoma cells. Obstet Gynecol 1998:91:
symposium on biological effects and characterization 17. Hynynen K, Pomeroy O, Smith DN, et al. MR 735–740
of ultrasound sources (June 1–3). Rockville, MD: imaging-guided focused ultrasound surgery of fi- 32. Hynynen K, Colucci V, Chung A, Jolesz F. Non-
Ultrasound in Medicine & Biology, 1977;224–239 broadenomas in the breast: a feasibility study. Ra- invasive artery occlusion using MRI guided fo-
4. Lynn JG, Zwemer RL, Chick AJ, Miller AE. A diology 2001;219:176–185 cused ultrasound. Ultrasound Med Biol 1996;22:
new method for the generation and use of focused 18. Gianfelice D, Khiat A, Amara M, Belblidia A, Bou- 1071–1077
ultrasound in experimental biology. J Gen Phys- langer Y. MR imaging guided focused US ablation of 33. Damianou C, Hynynen K. Focal spacing and
iol 1942;26:179–193 breast cancer: histopathologic assessment of effec- near-field heating during pulsed high temperature
5. Fry WJ, Fry FJ. Fundamental neurological re- tiveness—initial experience. Radiology 2003;227: ultrasound therapy. Ultrasound Med Biol 1993;
search and human neurosurgery using intense ul- 849–855 19:777–787
AJR:183, December 2004 1719
Das könnte Ihnen auch gefallen
- Komoiboros Inggoris-KadazandusunDokument140 SeitenKomoiboros Inggoris-KadazandusunJ Alex Gintang33% (6)
- Blana 2004Dokument4 SeitenBlana 2004skribekbenjaminNoch keine Bewertungen
- Luis 2009Dokument10 SeitenLuis 2009obgin januari19Noch keine Bewertungen
- Kapoor SchwannomaDokument7 SeitenKapoor SchwannomaAna Clara Nunes SartoriNoch keine Bewertungen
- Epartment 0: The Appllcation of X-Rays To Orstetrics AND OynecologyDokument4 SeitenEpartment 0: The Appllcation of X-Rays To Orstetrics AND OynecologyDian Putri NingsihNoch keine Bewertungen
- 0 Original ContributionDokument6 Seiten0 Original ContributionSRI WULANDARINoch keine Bewertungen
- Ultrasonics Sonochemistry: Jae-Seong Lee, Gi-Youn Hong, Byung-Joon Park, Tea-Eung KimDokument6 SeitenUltrasonics Sonochemistry: Jae-Seong Lee, Gi-Youn Hong, Byung-Joon Park, Tea-Eung KimTantonio Tri PutraNoch keine Bewertungen
- Horner Syndrome As A Complication After Thyroid Microwave AblationDokument4 SeitenHorner Syndrome As A Complication After Thyroid Microwave AblationthedidarmawijayaNoch keine Bewertungen
- Livsey 2003Dokument6 SeitenLivsey 2003Migue PerezNoch keine Bewertungen
- Non Small-Cell Lung Cancer in A 15-Year-Old NonsmokerDokument2 SeitenNon Small-Cell Lung Cancer in A 15-Year-Old Nonsmokertonirian99Noch keine Bewertungen
- Editorial: Breast Carcinogenesis: Risk of RadiationDokument3 SeitenEditorial: Breast Carcinogenesis: Risk of RadiationGabriela Silva MartinsNoch keine Bewertungen
- New England Journal Medicine: The ofDokument10 SeitenNew England Journal Medicine: The ofsyafahalimNoch keine Bewertungen
- Brain-Sparing Radiotherapy For Neuroblastoma Skull MetastasesDokument6 SeitenBrain-Sparing Radiotherapy For Neuroblastoma Skull Metastasesasialoren74Noch keine Bewertungen
- Pregnancy Radiation Carcinoma CervixDokument2 SeitenPregnancy Radiation Carcinoma CervixsandyrraoNoch keine Bewertungen
- Ijpd 24 221Dokument2 SeitenIjpd 24 221intan yunni aztiNoch keine Bewertungen
- 7 Early Clinical Experience Using High Intensity Focused Ultrasound For Palliation of Inoperable Pancreatic CancerDokument7 Seiten7 Early Clinical Experience Using High Intensity Focused Ultrasound For Palliation of Inoperable Pancreatic CancerEvelynLisettVargasNoch keine Bewertungen
- 2.Clinical Examination or Investigational MedicineDokument2 Seiten2.Clinical Examination or Investigational Medicineunknownsince1986Noch keine Bewertungen
- Annals of Neurology - 2008 - HamaniDokument5 SeitenAnnals of Neurology - 2008 - HamaniEccoNoch keine Bewertungen
- Jkns 2018 0153Dokument7 SeitenJkns 2018 0153ioNoch keine Bewertungen
- EVIEWDokument20 SeitenEVIEWmNoch keine Bewertungen
- Tomography 09 00090Dokument16 SeitenTomography 09 00090PPDS Rehab Medik UnhasNoch keine Bewertungen
- Minimally Invasive Management of Uterine Fibroids Role of Transvaginal Radiofrequency AblationDokument5 SeitenMinimally Invasive Management of Uterine Fibroids Role of Transvaginal Radiofrequency AblationHerald Scholarly Open AccessNoch keine Bewertungen
- Download A Clinical System For Non Invasive Blood Brain Barrier Opening Using A Neuronavigation Guided Single Element Focused Ultrasound Transducer Antonios N Pouliopoulos Shih Ying Wu Mark T Bur full chapterDokument40 SeitenDownload A Clinical System For Non Invasive Blood Brain Barrier Opening Using A Neuronavigation Guided Single Element Focused Ultrasound Transducer Antonios N Pouliopoulos Shih Ying Wu Mark T Bur full chapterclarence.terry830100% (4)
- Paper 5Dokument8 SeitenPaper 5Francisco Javier Luza RamosNoch keine Bewertungen
- Nejmoa 2207586Dokument15 SeitenNejmoa 2207586Mirabela CretuNoch keine Bewertungen
- Nej M 199905203402002Dokument6 SeitenNej M 199905203402002Ridwan Hadinata SalimNoch keine Bewertungen
- 6 Forastiere2003Dokument8 Seiten6 Forastiere2003RivssNoch keine Bewertungen
- Ultrasound Therapy CTADokument5 SeitenUltrasound Therapy CTAmitchNoch keine Bewertungen
- E248048 FullDokument3 SeitenE248048 FullsilviaNoch keine Bewertungen
- Mrna 3Dokument8 SeitenMrna 3api-675909478Noch keine Bewertungen
- AJCC6 TH Ed Cancer Staging Manual Part 1Dokument8 SeitenAJCC6 TH Ed Cancer Staging Manual Part 1handrionoNoch keine Bewertungen
- Does Acupuncture Influence the Endometrium and IVF OutcomesDokument7 SeitenDoes Acupuncture Influence the Endometrium and IVF OutcomesdirkvandeweyerNoch keine Bewertungen
- RavesDokument10 SeitenRavesyingming zhuNoch keine Bewertungen
- Burud 2020Dokument8 SeitenBurud 2020Wirda Elya SariNoch keine Bewertungen
- Ye 2015Dokument4 SeitenYe 2015vernadskyiNoch keine Bewertungen
- Photodynamic Therapy (PDT) For Lung Cancer: The Yorkshire Laser Centre ExperienceDokument10 SeitenPhotodynamic Therapy (PDT) For Lung Cancer: The Yorkshire Laser Centre ExperienceRahmahh FyyNoch keine Bewertungen
- Program-SUFU 2020 Winter Meeting-2252020Dokument39 SeitenProgram-SUFU 2020 Winter Meeting-2252020Christopher KinsellaNoch keine Bewertungen
- Angle of Progression Measurements of Fetal Head at Term, A Systematic Comparison Between Open Magnetic Resonance Imaging and Transperineal UltrasoundDokument5 SeitenAngle of Progression Measurements of Fetal Head at Term, A Systematic Comparison Between Open Magnetic Resonance Imaging and Transperineal UltrasoundNella SolanoNoch keine Bewertungen
- Thyroid Ultrasound, State of The ArtDokument15 SeitenThyroid Ultrasound, State of The ArtDe DawnNoch keine Bewertungen
- (03241750 - Acta Medica Bulgarica) Minimally Invasive Radiofrequency Ablation For Large Thyroid Toxic AdenomaDokument3 Seiten(03241750 - Acta Medica Bulgarica) Minimally Invasive Radiofrequency Ablation For Large Thyroid Toxic AdenomaTeodorNoch keine Bewertungen
- ObgynDokument7 SeitenObgynHeba MahdyNoch keine Bewertungen
- Effects of Focused Ultrasound Ablation On Uterine FibroidsDokument5 SeitenEffects of Focused Ultrasound Ablation On Uterine FibroidsHafsa IlyasNoch keine Bewertungen
- Ne W Engl and Journal MedicineDokument14 SeitenNe W Engl and Journal Medicineapi-26302710Noch keine Bewertungen
- 11 Preoperative - High - Neutrophil-Lymphocyte - Ratio - MayDokument8 Seiten11 Preoperative - High - Neutrophil-Lymphocyte - Ratio - MayBridia BogarNoch keine Bewertungen
- Paclitaxel-Induced Pneumonitis in PatientsDokument5 SeitenPaclitaxel-Induced Pneumonitis in PatientsAndiie ResminNoch keine Bewertungen
- 1 s2.0 S014067362300020X MainDokument14 Seiten1 s2.0 S014067362300020X MainGERIATRIA 72Noch keine Bewertungen
- Admin A 10 1 85 3b9f306Dokument8 SeitenAdmin A 10 1 85 3b9f306Dyanne BautistaNoch keine Bewertungen
- Chen 2013Dokument5 SeitenChen 2013RenaldiPrimaSaputraNoch keine Bewertungen
- Mikropenis Dan UDTDokument4 SeitenMikropenis Dan UDTOcy BikeNoch keine Bewertungen
- Wa0004.Dokument20 SeitenWa0004.Mayra AlejandraNoch keine Bewertungen
- Extra Renal Rhabdoid Tumor in An Adult Presentin 2024 International JournalDokument5 SeitenExtra Renal Rhabdoid Tumor in An Adult Presentin 2024 International JournalRonald QuezadaNoch keine Bewertungen
- Brain Metastases From Primary Uterine Cervical Cancer: A Case Report and A Literature ReviewDokument5 SeitenBrain Metastases From Primary Uterine Cervical Cancer: A Case Report and A Literature ReviewIJAR JOURNALNoch keine Bewertungen
- Ultrasound AND Congenital Dislocation OF THE HIP: From Nuffield Orthopaedic Centre, OxfordDokument5 SeitenUltrasound AND Congenital Dislocation OF THE HIP: From Nuffield Orthopaedic Centre, OxfordRéka TéglásNoch keine Bewertungen
- Pi Is 0936655522005015Dokument8 SeitenPi Is 0936655522005015Raul Matute MartinNoch keine Bewertungen
- A case series of acupuncture treatment for female infertility with some cases 2014Dokument5 SeitenA case series of acupuncture treatment for female infertility with some cases 2014juba0015Noch keine Bewertungen
- Radiation Exposure To Operating Room PerDokument5 SeitenRadiation Exposure To Operating Room Perraden.mas.2021Noch keine Bewertungen
- Stuart-Harris 100510Dokument17 SeitenStuart-Harris 100510Liudmila RusuNoch keine Bewertungen
- Hart2018. UV Radiation-Induced ImmunosuppressionDokument13 SeitenHart2018. UV Radiation-Induced Immunosuppressioncristina.moya724Noch keine Bewertungen
- Zaid 2013Dokument3 SeitenZaid 2013Teja Laksana NukanaNoch keine Bewertungen
- Medulloblastoma: An Analysis of Recurrence Patterns Time-Dose Relationships andDokument7 SeitenMedulloblastoma: An Analysis of Recurrence Patterns Time-Dose Relationships andGabriela Silva MartinsNoch keine Bewertungen
- Alternate Fractionation in Radiotherapy: Paradigm ChangeVon EverandAlternate Fractionation in Radiotherapy: Paradigm ChangeMark TrombettaNoch keine Bewertungen
- PRI Vs SIP Trunking WPDokument3 SeitenPRI Vs SIP Trunking WPhisham_abdelaleemNoch keine Bewertungen
- Shahin CVDokument2 SeitenShahin CVLubainur RahmanNoch keine Bewertungen
- SyllabusDokument8 SeitenSyllabusrickyangnwNoch keine Bewertungen
- MagnitismDokument3 SeitenMagnitismapi-289032603Noch keine Bewertungen
- World War 2 Soldier Stories - Ryan JenkinsDokument72 SeitenWorld War 2 Soldier Stories - Ryan JenkinsTaharNoch keine Bewertungen
- Price and Volume Effects of Devaluation of CurrencyDokument3 SeitenPrice and Volume Effects of Devaluation of Currencymutale besaNoch keine Bewertungen
- Ettercap PDFDokument13 SeitenEttercap PDFwyxchari3Noch keine Bewertungen
- Unofficial Transcript - Printer FriendlyDokument4 SeitenUnofficial Transcript - Printer Friendlyapi-251794642Noch keine Bewertungen
- Simply Learn Hebrew! How To Lea - Gary Thaller PDFDokument472 SeitenSimply Learn Hebrew! How To Lea - Gary Thaller PDFsuper_gir95% (22)
- Voluntary Vs MandatoryDokument5 SeitenVoluntary Vs MandatoryGautam KumarNoch keine Bewertungen
- Preterm Labour: Muhammad Hanif Final Year MBBSDokument32 SeitenPreterm Labour: Muhammad Hanif Final Year MBBSArslan HassanNoch keine Bewertungen
- Derivatives 17 Session1to4Dokument209 SeitenDerivatives 17 Session1to4anon_297958811Noch keine Bewertungen
- Pure TheoriesDokument5 SeitenPure Theorieschristine angla100% (1)
- Ten Lessons (Not?) Learnt: Asset AllocationDokument30 SeitenTen Lessons (Not?) Learnt: Asset AllocationkollingmNoch keine Bewertungen
- AR Financial StatementsDokument281 SeitenAR Financial StatementsISHA AGGARWALNoch keine Bewertungen
- 02 Activity 1 (4) (STRA)Dokument2 Seiten02 Activity 1 (4) (STRA)Kathy RamosNoch keine Bewertungen
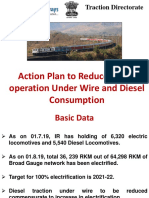
- Final DSL Under Wire - FinalDokument44 SeitenFinal DSL Under Wire - Finalelect trsNoch keine Bewertungen
- Chemistry Sample Paper 2021-22Dokument16 SeitenChemistry Sample Paper 2021-22sarthak MongaNoch keine Bewertungen
- Group Assignment Topics - BEO6500 Economics For ManagementDokument3 SeitenGroup Assignment Topics - BEO6500 Economics For ManagementnoylupNoch keine Bewertungen
- Shakespeare's Sonnets Portray a Deeper Understanding of Authentic Love Compared to Marlowe's Idealistic PerspectiveDokument3 SeitenShakespeare's Sonnets Portray a Deeper Understanding of Authentic Love Compared to Marlowe's Idealistic Perspectivemaria blascosNoch keine Bewertungen
- Evaluation of Evidence-Based Practices in Online Learning: A Meta-Analysis and Review of Online Learning StudiesDokument93 SeitenEvaluation of Evidence-Based Practices in Online Learning: A Meta-Analysis and Review of Online Learning Studiesmario100% (3)
- APPSC Assistant Forest Officer Walking Test NotificationDokument1 SeiteAPPSC Assistant Forest Officer Walking Test NotificationsekkharNoch keine Bewertungen
- TOPIC - 1 - Intro To Tourism PDFDokument16 SeitenTOPIC - 1 - Intro To Tourism PDFdevvy anneNoch keine Bewertungen
- Konsep SRA (Sekolah Ramah Anak) Dalam Membentuk Budaya Islami Di Sekolah DasarDokument10 SeitenKonsep SRA (Sekolah Ramah Anak) Dalam Membentuk Budaya Islami Di Sekolah Dasarsupriyono hasanNoch keine Bewertungen
- School of Architecture, Building and Design Foundation in Natural Build EnvironmentDokument33 SeitenSchool of Architecture, Building and Design Foundation in Natural Build Environmentapi-291031287Noch keine Bewertungen
- BMW E9x Code ListDokument2 SeitenBMW E9x Code ListTomasz FlisNoch keine Bewertungen
- Introduction To Alternative Building Construction SystemDokument52 SeitenIntroduction To Alternative Building Construction SystemNicole FrancisNoch keine Bewertungen
- The Gnomes of Zavandor VODokument8 SeitenThe Gnomes of Zavandor VOElias GreemNoch keine Bewertungen
- Written Test Unit 7 & 8 - Set ADokument4 SeitenWritten Test Unit 7 & 8 - Set ALaura FarinaNoch keine Bewertungen