Beruflich Dokumente
Kultur Dokumente
MANAGER
Hochgeladen von
api-786141610 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
10 Ansichten3 SeitenMANAGER with 30 years experience looking for a Middle Management position.
Copyright
© Attribution Non-Commercial (BY-NC)
Verfügbare Formate
TXT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenMANAGER with 30 years experience looking for a Middle Management position.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als TXT, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
10 Ansichten3 SeitenMANAGER
Hochgeladen von
api-78614161MANAGER with 30 years experience looking for a Middle Management position.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als TXT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 3
FRANK BALCO, JR.
1614 Longfellow Drive 856-354-8294
Cherry Hill, NJ 08003 fbd7ac14@westpost.net
HEALTHCARE SENIOR MANAGER
Claims Operations... Process Re-engineering... Call Center Operations...
Membership Management... Medicare / Medicaid (Governance)
* Senior-level professional offering a unique blend of operations leadership and
infrastructure management experience within the healthcare industry. Innate abi
lity to motivate and empower cross-functional teams to optimize productivity and
solve problems, resulting in significant improvements to business processes and
customer satisfaction.
* Strategic thinker who has engineered start-ups, saved tremendous dollars in co
sts, and facilitated new business. Change agent with strong focus on assessing c
ustomer needs and integrating with practical business issues from an operational
and technological perspective.
* Track record of implementing start-up operations, staff training programs, and
compliance initiatives. Diversified experience in member management, call cente
r operations, and claims administration for multi-billion dollar insurance carri
er (i.e. public and private). Highly skilled in managing Medicare, Medicaid, and
private insurance programs.
CORE COMPETENCIES
Administration... Business Re-engineering... Government Relations... Budgeting..
. Key Account Management
Start-Up Operations... Claims Management... Performance Metrics... Reporting...
Staff Training Programs
Project Management... Strategic Planning... Cost Reductions... Call Center Opera
tions... Compliance... Auditing
Systems Implementation... Product Management... Market Strategies... Process & P
rocedure Development
PROFESSIONAL EXPERIENCE
INDEPENDENCE BLUE CROSS, Philadelphia, PA * 1979 to 2010
Manager*Government Programs Enrollment (2007 to 2010)
Directed daily business affairs and overall operations of beneficiary enrollment
and ongoing account maintenance for Medicare and Medicaid Programs. Revamped be
neficiary enrollments involving learning requirements, setting up systems, and p
roducing rapid turnaround for member enrollments. Developed and administered all
staff training initiatives. Oversaw 250 indirect reports in implementing progra
m for complex and fast-growing healthcare product line (Medicare Advantage). Sup
ervised 60+ direct reports.
* Achieved full compliance with all CMS audit regulations and guidelines, includ
ing collateral development and distribution along with beneficiary account manag
ement.
* Spearheaded ongoing maintenance of member management systems designed to strea
mline reporting and data collection process; successfully identified discrepanci
es and investigated eligibility requirements.
* Partnered with training department to develop extensive curriculum that develo
ped staff to be more qualified and efficient and who could provide a higher leve
l of customer service.
* Collaborated with IS department to identify problems and develop system enhanc
ements; developed and wrote comprehensive business requirements. Participated in
efforts for testing and implementing system.
* Administered front-end mailings to beneficiaries with 70+ variations to notifi
cation letters. Additionally developed 350 unique letter templates and identifie
d processes for determining accuracy of distribution.
Manager*Claims Adjustment Services (2005 to 2007)
Selected to lead new division accountable for reducing duplication along with ha
ndling provider inquiries and other adjustments. Led design and implementation o
f logistics, facilities, hiring, and training. Developed improved system for opt
imizing workflow process in order to receive and process inquiries from provider
s more efficiently.
Oversaw entirely new production unit, consisting of 60+ staff tasked with identi
fying and resolving duplicate claims payments. Devised and executed all processe
s and procedures to meet corporate, account, and regulatory standards. Created a
nd administered staff training programs. Developed and implemented system change
s designed to provide accurate and consistent application of claim adjudication
rules. Managed all external vendors and auditing firms.
* Managed accounts receivable processes to resolve overpayments resulting from i
naccurate claims adjudication or unidentified premium receipts. Orchestrated new
area to record, deposit, and track monies; implemented process to secure A/R's
and investigate proper location for incoming checks.
* Led conversion of outdated legacy systems to enterprise-wide vendor replacemen
t claims system. Reduced systems exceptions from more than 300,000 to less than
4,000 annually.
* Participated as member of committee responsible for developing workload manage
ment system that resulted in accurately recording documentation and significantl
y increasing user satisfaction rates.
* Pivotal in reducing and eliminating duplication through initiating business pr
ocess and technology changes.
* Charged with setting performance benchmarks as member of Corporate Executive
Delegation Oversight Committee.
Manager*Claims Processing Services (1996 to 2004)
Hand-picked by senior management to launch start-up operations for division acco
untable for AmeriHealth and Keystone POS products servicing 500,000+ members. Or
chestrated strategies and action plans to meet organizational goals. Oversaw tra
ining and development. Monitored and reviewed vendor claim functions. Acted as l
iaison between delegated vendors and outside auditors. Reviewed, analyzed, and p
resented results to IBC Oversight Committee. Supervised 80+ staff.
* Designed and implemented strategic planning, organizational structure, process
re-engineering, and facilities. Created and implemented extensive training prog
ram along with reporting system within new division.
* Eliminated antiquated claims processes through efforts in identifying discrepa
ncies and instituting computerized process to compare information from two diffe
rent systems.
* Developed procedures that subsequently reduced duplication to about 2%, a 98%
accuracy rate (down from 72% duplicate processing) which reduced costs and also
resolved problems for providers and members.
* Collaborated with IS to develop standards and provide national exposure for un
ique systems platform.
Manager*Dedicated Accounts (1996 to 1997)
Promoted to position for handling 12 high-volume key accounts ranging from 300 t
o 10,000+ members in areas of customer service, claims, enrollment, and quality
assurance. Oversaw compliance for account specific corporate performance and ser
vice agreements. Selected as Account Liaison to resolve problems and reduce memb
er complaints, including site reviews and onsite staff management. Supervised 80
+ staff members.
* Developed and implemented focused training for customer service and employee r
eview process. Instituted training efforts for dedicated team members and collab
orated with training department to create curriculum.
* Worked closely and cooperatively with systems department to identify reports n
eeded to assess issues, claim problems, and account discrepancies; also created
reports to identify, analyze, and develop solutions.
* Restructured reporting format to provide consistency across accounts and prope
r analysis of comparative data for performance metrics.
* Served on Corporate Planning Committee with goal of developing market strategi
es to ensure high account retention rate, secure new clientele, and increase mar
ket share. Tasked with cross-training staff members on techniques to ensure effi
ciency, customer service, and computer accuracy.
Held increasingly accountable positions during earlier tenure-Supervisory positi
ons included Processing Services, Dedicated Accounts, Private Business Claims, M
ajor Medical Claims
TRAINING AND SEMINARS
Extensive professional development in the areas of leadership, management, and c
ommunications
1614 Longfellow Drive * Cherry Hill, NJ 08003 * 856-354-8294 * fbd7ac14@westpost
.net
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Quality Assurance in Pharma - Self Inspection Check List (Warehouse) PDFDokument3 SeitenQuality Assurance in Pharma - Self Inspection Check List (Warehouse) PDFkavya nainitaNoch keine Bewertungen
- IDC White Paper Delivering Enterprise Value With Service ManagementDokument23 SeitenIDC White Paper Delivering Enterprise Value With Service ManagementrambalajirNoch keine Bewertungen
- Auditing Notes B.com Part 2 Punjab UniversityDokument73 SeitenAuditing Notes B.com Part 2 Punjab Universitykamal sahab83% (6)
- Leadway 2020 Annual ReportDokument196 SeitenLeadway 2020 Annual Reportallder allderNoch keine Bewertungen
- CH - 7 Strategy Evaluation and ControlDokument10 SeitenCH - 7 Strategy Evaluation and ControlSneha Singh100% (1)
- Form IA-007NC (QMS Process Matrix Report) (3!26!2012)Dokument3 SeitenForm IA-007NC (QMS Process Matrix Report) (3!26!2012)granburyjohnstevensNoch keine Bewertungen
- BNM/RH/GL 005-14 Development Finance and Enterprise Department (DFE) Guidelines On Corporate Governance For Development Financial InstitutionsDokument50 SeitenBNM/RH/GL 005-14 Development Finance and Enterprise Department (DFE) Guidelines On Corporate Governance For Development Financial InstitutionsMuhammad Rafi SiratNoch keine Bewertungen
- Pertamina Annual Report 2021Dokument742 SeitenPertamina Annual Report 2021Amal Falamigi Satrio100% (1)
- FSCJ's MGT ReportDokument75 SeitenFSCJ's MGT ReportThe Florida Times-UnionNoch keine Bewertungen
- Stock Audit in Banks Compatible ModeDokument6 SeitenStock Audit in Banks Compatible ModechhayabiyaniNoch keine Bewertungen
- Cost Management Accounting SystemDokument239 SeitenCost Management Accounting SystemPathshala ki duniyaNoch keine Bewertungen
- ACIPA 2008 and 2009 Audit and AssuranceDokument35 SeitenACIPA 2008 and 2009 Audit and AssuranceSara BautistaNoch keine Bewertungen
- BRC S&D Issue 4 - English 2020novDokument158 SeitenBRC S&D Issue 4 - English 2020novdamelahora93121650% (2)
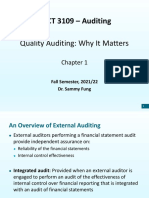
- ACCT 3109 - Auditing: Quality Auditing: Why It MattersDokument46 SeitenACCT 3109 - Auditing: Quality Auditing: Why It MattersChung CFNoch keine Bewertungen
- Job Description Internal Auditor 11-08Dokument4 SeitenJob Description Internal Auditor 11-08Muneeb ShaikNoch keine Bewertungen
- Index of Front & Back of FileDokument8 SeitenIndex of Front & Back of FileAli RazaNoch keine Bewertungen
- Vda 6-3Dokument7 SeitenVda 6-3julio_0489Noch keine Bewertungen
- PWC Greenhouse Gas Emissions Report2009Dokument28 SeitenPWC Greenhouse Gas Emissions Report2009Dalibor FuntakNoch keine Bewertungen
- Naresh Chandra Commitee 2002 - Presentation To Be Taken For Class Seminar.Dokument26 SeitenNaresh Chandra Commitee 2002 - Presentation To Be Taken For Class Seminar.sambhu_nNoch keine Bewertungen
- Audit Program For InventoriesDokument14 SeitenAudit Program For InventoriesZosimo SolanoNoch keine Bewertungen
- Computerized accounting quiz questionsDokument8 SeitenComputerized accounting quiz questionsJeacy Mae GallegoNoch keine Bewertungen
- G10148 RG Audit Assurance Resource Guide March 2020Dokument38 SeitenG10148 RG Audit Assurance Resource Guide March 2020Kevin .A. SeelyNoch keine Bewertungen
- Centinela Flot Column Quality Plan WVendor AuditDokument15 SeitenCentinela Flot Column Quality Plan WVendor AuditAndrés RodríguezNoch keine Bewertungen
- APQP Internal Assessment Checklist: Development PhaseDokument3 SeitenAPQP Internal Assessment Checklist: Development PhaseRandhir Kanwar100% (1)
- MI-F-4.3.2-app06-001 - Internal Audit ReviewDokument1 SeiteMI-F-4.3.2-app06-001 - Internal Audit ReviewHernanda ImawanNoch keine Bewertungen
- Reliance Retail LimitedDokument46 SeitenReliance Retail LimitedKumar PranayNoch keine Bewertungen
- Internal Audit ProgramDokument3 SeitenInternal Audit ProgramTakogee100% (1)
- Determine The Reliability of Financial Reporting by The Purchasing FunctionDokument9 SeitenDetermine The Reliability of Financial Reporting by The Purchasing FunctionMarisa CaraganNoch keine Bewertungen
- Supplier Manual Supplier Manual Supplier Manual Supplier ManualDokument15 SeitenSupplier Manual Supplier Manual Supplier Manual Supplier ManualTran HuyenNoch keine Bewertungen
- Factors Affecting Tax Audit EffectivenesDokument98 SeitenFactors Affecting Tax Audit Effectivenesalemakef shumiyeNoch keine Bewertungen