Beruflich Dokumente
Kultur Dokumente
Manejo de Niños Con Otitis Media
Hochgeladen von
Hector DgúezOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Manejo de Niños Con Otitis Media
Hochgeladen von
Hector DgúezCopyright:
Verfügbare Formate
doi:10.1111/j.1440-1754.2009.01564.
REVIEW ARTICLE
Management of children with otitis media: A summary of evidence from recent systematic reviews
jpc_1564 554..563
Hasantha Gunasekera,1,2 Peter S Morris,3 Peter McIntyre2,4 and Jonathan C Craig1,2
1 Centre for Kidney Research, The Childrens Hospital at Westmead, 2School of Public Health, University of Sydney, Sydney, 3Menzies School of Health Research and NT Clinical School, Flinders University, Darwin, 4National Centre for Immunisation Research and Surveillance of Vaccine Preventable Diseases, Sydney, Australia
Abstract: Health-care professionals who manage children are regularly confronted with clinical questions regarding the management of the full spectrum of otitis media: acute otitis media; otitis media with effusion; and chronic suppurative otitis media. Given the variety of potential therapies available, the wide spectrum of middle ear disorders, and the lack of consensus about management strategies, clinicians are in a difcult position when managing these children. In this review, we seek to summarise the current best evidence for answering otitis media management questions by collating existing systematic reviews. Key words: Aboriginal; children; management; otitis media.
Introduction
Middle ear disease in children spans human history. For thousands of years, various treatments for otitis media (OM) have been suggested, including: goats urine and bats wings, incising the eardrum, vinegar washes, drinking butter and maintaining silence.1,2 Hippocrates recommended breast milk, sweet wine and avoidance of smokey rooms, reserving topical therapy with lead powder for severe cases.2 Although OM is very common worldwide, has a long history and has been the subject of
Key Points 1 Indigenous children with acute otitis media (AOM) should be treated with Amoxycillin at the initial visit. Immediate antibiotic therapy is optional for non-Indigenous children with AOM, but children younger than 2 years with bilateral disease and those with otorrhoea are most likely to benet. 2 Children with otitis media with effusion (OME), and no speech and language delays, can be observed safely for 36 months. If the effusion has not resolved by then, referral to an Ear Nose and Throat surgeon for ventilation tube insertion should be arranged for children with bilateral hearing loss >25 dB. 3 Children with chronic suppurative otitis media (CSOM) need ear cleaning (e.g. dry mopping or betadine washouts) and topical antibiotics (e.g. ciprooxacin ear drops) until the discharge resolves.
Correspondence: Dr Hasantha Gunasekera, General Medicine Department, The Childrens Hospital at Westmead, 2145 NSW, Australia. Fax: +612 9845 1491; email: hasanthg@chw.edu.au Accepted for publication 6 April 2009.
multiple randomised controlled trials, there remains a great deal of variability in clinical practice in Australia and around the world.36 Australian health-care professionals need to be familiar with current evidence for OM management because Indigenous children are one of the most at-risk groups in the world.79 Since the 18th century, when letters from Australian settlers documented profusely draining ears in the local Indigenous children,10 numerous studies have highlighted the discordant OM burden suffered by Indigenous versus other Australian children, particularly those living in remote communities.5,7,11,12 Australian Indigenous children experience OM at a younger age,13,14 and have more frequent, more severe, more prolonged and more complicated OM than any other comparable population group around the world.59 OM is not just a major cause of morbidity in Indigenous children. OM affects nearly every child at least once,15 is one of the most common causes of health-care presentations,5,15 antibiotic prescriptions,515 and hearing impairment in children.16 The magnitude of this morbidity burden is highlighted by the 2003 estimate that net costs of OM management total $US 5 billion in the United States17 and are of comparable magnitude in a recent Australian analysis.18 Health-care professionals who manage children are regularly confronted with clinical questions regarding the management of the full spectrum of OM; acute otitis media (AOM), otitis media with effusion (OME) and chronic suppurative otitis media (CSOM). Given the variety of potential therapies available, the wide spectrum of middle ear disorders, and the lack of consensus about management strategies, clinicians are in a difcult position when managing these children. In this review, we seek to summarise the current best evidence for answering OM management questions by collating existing systematic reviews.
554
Journal of Paediatrics and Child Health 45 (2009) 554563 2009 The Authors Journal compilation 2009 Paediatrics and Child Health Division (Royal Australasian College of Physicians)
H Gunasekera et al.
Management of children with otitis media
Methods
We performed an electronic search for relevant studies using Medline (1950 to February 2009) by exploding the term OM and limiting to the publication types meta-analysis or review, and the language eld English. We also searched the Cochrane database for evidence-based medicine reviews. All systematic reviews which examined any management issue for any form of OM were included. Only the most recent version of a review was included when updates had been completed. Reviews identied from other sources or known to the authors were also included. Where possible, we presented data on the number of patients needed to treat per treatment for each outcome of interest. The search identied two systematic reviews on risk factors for OM, 14 on management of AOM, 10 on management of OME, and 3 on other relevant topics.
provided, with no denition used by more than six clinicians.25 Diagnosis of either AOM or OME requires the presence of an effusion, which can be reliably detected only by tympanometry and pneumatic otoscopy.26 Despite this, neither of these techniques is widely used in Australian Aboriginal Medical Services.6 We do not have any information on the use of these diagnostic techniques in other general practice or paediatric settings in Australia.
Case denitions: AOM (see Fig. 1a)
The Agency for Healthcare Research and Quality, the American Academy of Pediatrics and the Australian Therapeutic Guidelines currently use similar criteria to dene AOM.27,28 The denition of AOM can be summarised as: 1. Acute onset (within 48 h). 2. Middle ear uid (such as bulge, absent movement or bubbles). 3. Signs and symptoms (such as tympanic membrane redness, otalgia or fever).
Risk Factors for OM
There are two systematic reviews of risk factors for AOM and recurrent AOM19,20 and both identied the presence of siblings, day-care attendance, exposure to tobacco smoke, pacier or dummy use and lack of breast feeding as signicant risk factors. However, each factor, separately, had only a modest effect (see Table 1). Children at high risk of OM and its complications should be considered differently to the majority of children.21 Australian Indigenous children have consistently been shown to be at extremely high risk for severe, complicated OM.69,13,14 The Ofce of Aboriginal and Torres Strait Islander Health produced guidelines in 200121, which recommend more aggressive therapy for Indigenous than other Australian children based on their higher disease risk (see Therapeutic Guidelines22 and Table 2.) Another group at high risk of OM and its complications is children with craniofacial abnormalities, such as cleft palate.19
OME (see Fig. 1b)
OME can be dened as the presence of middle ear effusion without signs of acute infection.27 The presence of bubbles (or an air-uid level) in the middle ear cavity is a reliable sign of middle ear effusion but their absence does not reliably exclude effusion.
CSOM (see Fig. 1c)
CSOM is persistent discharge of pus through a perforated tympanic membrane. The duration of persistent varies in different studies. The World Health Organization uses a denition of 2 weeks.9 If the discharge is of shorter duration, the child would be considered to have AOM with perforation.
Diagnosis
A major obstacle to consistent management of OM is the lack of universally accepted diagnostic criteria (see Fig. 1). In a survey of 165 clinicians, 147 different clinical denitions of AOM were
Diagnostic Box
Pneumatic otoscopy
Pneumatic otoscopy requires an otoscope and a pneumatic attachment an insufator like the blood pressure cuff bulb. A small jet of air is pushed into the external ear canal. If there is an air-tight seal, the air jet will cause the tympanic membrane to move. If middle ear uid is present, the tympanic membrane will either move sluggishly or not at all. Pneumatic otoscopy has good sensitivity (94%) and specicity (80%) for the detection of middle ear effusion, using myringotomy ndings as the gold standard, when performed by experienced clinicians. It is used routinely by clinicians in the United States.26 The pneumatic attachment can be purchased from your medical supplier for approximately $20 AUD.
Table 1
Risk factors for recurrent acute otitis media (AOM)* Risk of AOM AOM Recurrent AOM Recurrent AOM Recurrent AOM AOM AOM AOM AOM RR 2.6 2.5 2.1 1.9 1.8 1.7 1.6 1.2 1.2 P value <0.001 0.003 <0.001 0.001 0.004 <0.001 0.002 0.008 0.003
Risk factor Family history of AOM Daycare outside home Not breastfeeding at all At least one sibling Child care outside home Parental smoking Family daycare Pacier use Breast feeding <3 months *Source: Uhari M et al.20
Tympanometry (see Fig. 2)
A tympanometer has a microphone, speaker and manometer. The speaker emits a constant sound (e.g. at 226 Hz), the ear canal pressure is varied (+200 to -400 daPa) and the
555
Journal of Paediatrics and Child Health 45 (2009) 554563 2009 The Authors Journal compilation 2009 Paediatrics and Child Health Division (Royal Australasian College of Physicians)
Management of children with otitis media
H Gunasekera et al.
Table 2 Summary of Australian and international guidelines for antibiotic management of AOM at initial consultation Guideline Australian OATSIH Guidelines21 Guideline Australian Therapeutic Guidelines (antibiotic)22 American Academy of Pediatrics23 United Kingdom NHS Guidelines24 For all age groups Amoxycillin 50 mg/kg/day for seven days If perforation, amoxycillin 5090 mg/kg/day for 14 days Infants <6 months Amoxycillin (45 mg/kg/day) Infants 6 months to 2 years Observation for one day If vomiting and fever, amoxycillin 45 mg/kg/ day for ve days Amoxycillin (8090 mg/kg/day) If not severe* and uncertain diagnosis, observation for two days Amoxycillin** (2040 mg/kg/day) for ve days If diagnosis uncertain, observation for three days Children 2 years
Amoxycillin (8090 mg/kg/day)
Amoxycillin** (2040 mg/kg/day) for ve days
Observation for two days If vomiting and fever, amoxycillin 45 mg/kg/ day for ve days Amoxycillin (8090 mg/kg/day) If not severe* or uncertain diagnosis, observation for two days Amoxycillin** (2040 mg/kg/day) for ve days If not severe*, observation for three days
*Severe = high fever (>39C), severe pain, perforation, bilateral disease, **The UK guidelines use an age-based rather than weight-based dosing schedule, so the dosing regimens presented here are estimates. After the observation period, most guidelines recommend starting antibiotics if symptoms persist.
Fig. 1 Typical middle ear appearances. (a) Acute otitis media, (b) Otitis media with effusion with ventilation tube, (c) Chronic suppurative otitis media, (d) Normal middle ear appearance. (Images a, b and c courtesy of Professor Harvey Coates.)
microphone picks up the returning soundwaves. The tympanometer measures the admittance or impedance and also estimates the ear canal volume. Tympanometry involves insertion of the earpiece into the external ear canal to establish an airtight seal. The tympanometer takes a few seconds to generate a graph pressure and volume measurements. When performed by a experienced operator and using B or C2 curves, tympanometry has good sensitivity (94%) but poor specicity (62%)
556
for detection of middle ear effusion against myringotomy.26 Specicity can be improved using a different cut-off (static compensated acoustic admittance of 0.1 mmHo) but this reduces sensitivity (34%).26 The best results are obtained when B curves (at tympanograms) are used as the cut-off for middle ear effusion (81% sensitivity and 75% specicity).26 Remember: do not attempt tympanometry in the presence of a discharge.
Journal of Paediatrics and Child Health 45 (2009) 554563 2009 The Authors Journal compilation 2009 Paediatrics and Child Health Division (Royal Australasian College of Physicians)
H Gunasekera et al.
Management of children with otitis media
(a)
(b)
(c)
Fig. 2 Tympanogram types. (a) Type A (no effusion). (b) Type B (effusion). (c) Type C, various subtypes (possible effusion, also referred to as Eustachian tube dysfunction).
Management (see Fig. 3)
AOM: to treat or not to treat that is the question (see Table 3)
The debate about whether or not to prescribe oral antibiotics at the rst consultation for AOM still rages. In Australia and North America, most children are given antibiotics,4,5 whereas in The Netherlands, Denmark and Norway children are increasingly managed with watchful waiting.3 Meta-analyses of antibiotics show a consistent but small clinical benet from oral antibiotics
in AOM which needs to be balanced against the similar risk of side effects. Those for antibiotics argue that some of the children in the primary studies included in the meta-analyses may have had OME rather than AOM, which could have diluted the magnitude of the effect of antibiotics. Those against antibiotics argue that the small benet from antibiotic therapy is outweighed by the harms. It is also likely that in the routine clinical setting, as opposed to clinical trials, inadequate or misinterpreted middle ear examination is much more prevalent, particularly in young infants. These reviews have been largely focused on children presenting with the initial symptoms of AOM (ear pain). In the watchful waiting cases, failures may still end up being treated with antibiotics over the next few days. It is also important to emphasise that all children should be treated for the symptoms of AOM. There is evidence favouring simple analgesia, such as paracetamol or ibuprofen, but anti-histamines and decongestants, whether alone or in combination, have no proven benet and some proven harms and so are not recommended (see Table 3). The concern has been raised that this watchful waiting approach could lead to more suppurative complications of OM, such as mastoiditis. Antibiotic use for OM in the primary healthcare setting over the last decade has reduced substantially in the UK. However, a time trend analysis did not show a concomitant signicant increase in the rate of mastoiditis, rheumatic fever or peritonsillar abscess presentations to hospital. If this is translated into general practice behaviour, it is estimated that more than 2500 children with OM would need to be treated with antibiotics to prevent a single case of mastoiditis.41 The decreased rates of mastoiditis and other severe infections are more likely to be related to other public health measures than to antibiotic use. At the initial consultation for AOM, clinicians and families may choose from three broad options: to use oral antibiotics, to not use oral antibiotics (watchful waiting) or to provide a prescription for oral antibiotics, which the family can ll if the childs symptoms persist. In one study, only 24% of UK parents in the delayed prescription group went on to ll the script.42 For those choosing to treat children with AOM with antibiotics, the strongest evidence exists for young infants (02 years) with bilateral disease and any child with otorrhoea. For the outcomes of pain and/or fever at 37 days, for every 4 children with these features treated, one child will have pain/fever prevented.31 The Australian Therapeutic Guidelines recommends 5 days of amoxycillin as rst-line treatment if antibiotics are given for AOM21 but recommends a dose of only 50 mg/kg/day compared with US recommendations of 8090 mg/kg/day (see Table 2). There is no evidence that any antibiotic is superior to amoxycillin, but in cases due to pneumococci with intermediate resistance to penicillin, doses in the higher dosage range would be needed. Outcomes following 710 days courses are similar to shorter treatment courses.38
OME (glue ear)
The majority of new middle ear effusions will clear spontaneously by three months so it is reasonable to wait for this period of time before instituting additional therapy. There is no evidence to support the immediate use of antibiotics following a new diagnosis of OME,43 but only 20% of effusions which have
557
Journal of Paediatrics and Child Health 45 (2009) 554563 2009 The Authors Journal compilation 2009 Paediatrics and Child Health Division (Royal Australasian College of Physicians)
Management of children with otitis media
H Gunasekera et al.
D I A G N O S I S Pneumatic Otoscopy
mobile immobile or sluggish
Tympanometry
Effusion unlikely
Type A
Middle ear effusion
Type B
Establish whether there are additional features of AOM 1 2
Yes
Rapid onset Signs and Symptoms (red TM, bulging TM, vomiting)
No
AOM M A N A G E M E N T
High risk? 1 Indigenous 2 Mid-face abnormalities 3 <6 months 4 <2 years and bilateral 5 Otorrhoea
Yes No
OME
Observe 3 months
Amoxycillin (50mg/kg/ day) for 7 days Analgesia
No
Observe 2 days Analgesia
If not resolved: arrange audiogram If >25dB loss, consider: Antibiotics Ventilation tubes
Fig. 3 Simplied owchart of management options for otitis media with intact tympanic membrane. AOM, acute otitis media; OME, otitis media with effusion (glue ear); TM, tympanic membrane.
Resolving?
Yes
Further follow up if parental concern
been present for three months will clear over the next three months. In these children, systematic reviews support treating children with long-term oral antibiotics to hasten resolution, but the benets are modest.40,44 There is some evidence for oral and topical steroids in the short-term but no evidence that they have an effect in the longer term.45 There is evidence of harm from decongestants and antihistamines in about 10% of chil558
dren (including gastrointestinal upset, irritability, drowsiness or dizziness) and these therapies are not recommended (see Table 4). Children with prolonged middle ear pathology, such as effusions persisting longer than 3 months and those with associated hearing impairments should be referred to an Ear Nose and Throat specialist (ENT). During the ENT consultation, the
Journal of Paediatrics and Child Health 45 (2009) 554563 2009 The Authors Journal compilation 2009 Paediatrics and Child Health Division (Royal Australasian College of Physicians)
H Gunasekera et al.
Management of children with otitis media
Table 3
Systematic reviews on AOM management Included studies 6 RCTs Review population Comparison Outcome measures and results (95% condence intervals) Too much risk of bias associated with evidence to make recommendations NNT = 10 with combined decongestantantihistamine to prevent recurrent AOM* Five to eight fold increased risk of side effects No benet in early cure rates, symptom resolution, prevention of surgery or other complications For less pain/fever at 3 to 7 days: NNT = 3 for children with otorrhoea NNT = 4 for children 02 years & bilateral AOM NNT = 8 for children without otorrhoea Need to give 5 children long-term prophylaxis to prevent 1 child experiencing AOM on treatment each year Insufcient evidence to make recommendations
Review year (source) Thanaviratananich 2008 (Cochrane)29 Coleman 2008 (Cochrane)30
1601 children (012 years) 2695 children
15 RCTs
One or two daily doses vs. Three or four daily doses of Amoxycillin (+-clavulanate) Decongestant/antihistamines vs other
Rovers 2006 (Lancet)31
6 RCTs
1643 children (6 m to 12 years)
Antibiotics vs. other
Leach 2006 (Cochrane)32 Foxlee 2006 (Cochrane)33 Glasziou 2004 (Cochrane)34 Spurling 2004 (Cochrane)35
16 RCTs
1483 children at increased risk AOM Adults and children
6 w antibiotics vs. placebo
4 RCTs
8 RCTs
2287 children
Analgesic otic preparation without antibiotics vs.Placebo or non-analgesic Antimicrobials vs. Placebo
9 RCTs
Children and adults
Delayed antibiotics vs. No or immediate antibiotics
Rosenfeld 2003 (Laryngoscope)36 Takata 2001 (Pediatrics)37 Kozyrskyj 2000 (Cochrane)38 Rosenfeld 1994 (J Ped)39 Williams 1993 (JAMA)40
63 RCTs and cohort 9 RCTs 30 RCTs
8101 children (6 m20 years) >1518 children (1 m18 years) 1524 children with AOM (1 m18 years) 5400 children (1 m18 years) 958 children
Natural history of untreated AOM Antibiotics vs. Other Antibiotic course <7 days vs. Antibiotic course >7 days Antibiotics vs. Other Prophylactic antibiotics vs. Other
No reduction in pain at 24 h 30% relative reduction (1940%) pain at 27 days NNT = 15 to prevent pain at 27 days Pain and malaise were reduced in the immediate group vs. delayed group on day 3 but not after. No difference in long-term outcomes (earache, hearing, reconsultation rates) Reduced parent satisfaction, OR = 0.51 (0.35 to 0.73). 61% had symptom relief within 24 h 80% spontaneous resolution by 3 days in untreated NNT = 8 to prevent clinical failure at 27 days
33 RCTs 9 studies
Long term outcomes were similar following a 5 day course of antibiotics compared with a 810 day course NNT = 7 to prevent clinical failure 714 days NNT = 9 to prevent one having recurrent AOM
*Higher quality studies showed no benet and no study with allocation concealment showed any benet. AOM, acute otitis media; NNT, number needed to treat; OR, odds ratio; RCT, randomised controlled trials.
benets and harms of inserting ventilation tubes and, in recurrent cases, adenoidectomy should be discussed with the family. Ventilation tubes reduce the mean time with effusion by 32% over the next year50 and improve hearing, particularly over the 69 months post-operation.50 Theoretically, transient improvement in hearing is most likely to benet very young children at a critical stage of language development. The benets need to be weighed against the risks of surgery. However, risks are low in a specialised centre with paediatric anaesthetists and adequate follow-up.52 Tympanosclerosis (or tympanic membrane scarring) is common after surgery, but not clinically
important. Ventilation tubes are complicated by persistent perforation in 2% of children with short-term tubes and up to 17% with long-term tubes52. Some of these perforations develop into chronic ear discharge. Insertion of ventilation tubes is now by far the most important risk factor for CSOM in developed countries.53 Finally, despite short-term improvement in hearing, there is no evidence for long-term improvement in either hearing or language development,54 although these ndings may not be generalisable to the Australian context and in particular to disadvantaged Australian Indigenous children.
559
Journal of Paediatrics and Child Health 45 (2009) 554563 2009 The Authors Journal compilation 2009 Paediatrics and Child Health Division (Royal Australasian College of Physicians)
Management of children with otitis media
H Gunasekera et al.
Table 4 Systematic reviews on OME management Review year (source) McDonald 2009 (Cochrane)46 Perera 2006 (Cochrane)47 Grifn 2006 (Cochrane)48 Thomas 2006 (Cochrane)45 Rovers 2005 (Archives)49 Lous 2005 (Cochrane)50 Included studies 2 RCTs Review population 148 children Comparison Outcome measures and results (95% condence intervals)
Ventilation tubes vs. Other
6 RCTs
Children and adults (most <16 years) 1737 people (most <18 years) 862 children (015 years) 1234 children 2804 children (014 years)
Autoination devices (any) vs. other Antihistamines decongestants or combination vs. other Steroids (oral or nasal) vs. other Meta-analysis of interactions between treatment options Ventilation tubes (grommets) vs. Myringotomy or non-surgical treatment
16 RCTs
11 RCTs
7 RCTs 18 RCTs
Kay 2001 (HNS)51 Cantekin 1998 (ORL)43 Williams 1993 (JAMA)40 Rosenfeld 1992 (HNS)44
64 RCTs 70 case series 8 RCTs 12 studies 10 RCTs
39 882 children
Ventilation tubes for otitis media Antibiotics vs. Other Antibiotics vs. Other Antibiotics vs. Other
Signicant increase in children with no AOM in rst 6 months after surgery in one trial (P < 0.001) but non-signicant increase in other trial. Non-signicant improvements in tympanometry and audiometry No side effects noted No benet for any combination of interventions for any outcome measure Treated subjects had 11% more side effects Both oral and topical intranasal steroids lead to quicker resolution of OME in the short-term No evidence of longer term benet The effects of conventional ventilation tubes in children studied so far are small and limited in duration Grommets reduced time with effusion by 32% (1748%) over next year Grommets improved hearing levels modestly over next 6 m Grommets increased risk of tympanosclerosis by 0.33 (0.210.45) 1 to 5 years later Chronic perforation in 4.8% ears after tube insertion Chronic otorrhoea in 3.8% children after tube insertion No effect on short-term resolution of effusion NNT = 6 to resolve effusion in short-term No evidence for long-term resolution NNT = 4 for children with chronic bilateral effusions to prevent ongoing effusion at next assessment
1292 children 1697 children 1325 children
AOM, acute otitis media; NNT, number needed to treat; OME, otitis media with effusion; RCT, randomised controlled trial.
General measures to maximise the ability of affected children to hear in the home and school environment should also be used. These include advising the teachers to allow the children to sit closer to the front of the class, advising the parents and teachers to speak to the children face-to-face, and providing temporary hearing aids or amplication systems in more severe cases. Parents need to understand that while their child has a middle ear effusion they will not hear well and behaviour problems may arise from frustration.
CSOM (Table 5)
CSOM should be treated with ear cleaning (ear toilet) and topical antibiotic drops. Ear cleaning can be achieved using tissue spears (dry mopping) or by irrigating the external ear. In Western Australia, betadine syringing is also common practice. In the past, Sofradex drops (dexamethasone-framycetingramicidin) has been the mainstay of therapy. However, there has been concern about the prolonged use of potentially ototoxic compounds in the presence of a perforation. Ciprooxacin drops are more effective in Indigenous children58 and have been listed on the PBS. Ciprooxacin drops are restricted on the
560
Pharmaceutical Benets Scheme (PBS) to Aboriginal and Torres Strait Islander children over one month of age. The consensus is that the huge burden of OM disease in the Indigenous population overrides any concerns about the development of drug resistance. While topical antibiotics are superior to oral antibiotics, the role of oral antibiotics in additional to topical antibiotics is uncertain. If chronicity is possible or if the perforation is very small, the child should be treated with topical and oral antibiotics (as for AOM with perforation).55 For children with established CSOM, topical antibiotics alone are recommended.55 A recent Dutch study showed a reduction in discharge when oral cotrimoxazole was added to standard topical therapy. This benet did not persist after the oral antibiotics were ceased.53
Conclusion
The management of OM, as with other conditions, should be based on the best available evidence. Evidence from systematic reviews provide a solid foundation for making management decisions, but clinicians also need to consider the individual circumstances of their own patient populations. In
Journal of Paediatrics and Child Health 45 (2009) 554563 2009 The Authors Journal compilation 2009 Paediatrics and Child Health Division (Royal Australasian College of Physicians)
H Gunasekera et al.
Management of children with otitis media
Table 5 Other systematic reviews on OM Review year (source) MacFadyen 2006 (Cochrane)55 Roberts 2004 (Pediatrics)56 Abes 2003 (ORL)57 Included studies Review population Comparison Outcome measures and results (95% condence intervals) Topical quinolone antibiotics better than systemic antibiotics at clearing discharge at 12 weeks (RR 3.2, 1.95.5) OME and the related hearing loss showed a small but statistically signicant correlation with lower receptive and expressive language scores. Overall cure rate better with Ooxacin 0.3% otic drops for CSOM (OR 2.73, 1.524.90) vs. other non-uoroquinolone ear drops
9 RCTs
833 people with CSOM (various denitions) Children with OME during early childhood 1484 children and adults
Any systemic vs. Any topical treatments Speech and language abilities in preschool Ooxacin otic solution Vs. Any other treatment
14 prospective studies or RCTs 9 RCTs 2 cohort studies
CSOM, chronic suppurative otitis media; OR, odds ratio; RCT, randomised controlled trials; RR, relative risk.
this review we have synthesised the current evidence regarding OM management from recent systematic reviews, so that healthcare professionals managing these children can make informed decisions and can discuss the pros and cons of the different management options with the childs parents and carers.
References
1 Pahor AL. Ear, nose and throat in ancient Egypt. J. Laryngol. Otol. 1992; 106: 67787. 2 Parry D, Roland PS. Middle ear, chronic suppurative otitis, medical treatment. Emedicine Arch. Available from: http://emedicine. medscape.com/article/859501-overview. [accessed 20 February 2009]. 3 Odenholt I, Bylander-Groth A, Frimodt-Moller N, Rokstad KS, Molstad S. Differences in antibiotic prescribing patterns between general practitioners in Scandinavia: a questionnaire study. Scand. J. Infect. Dis. 2002; 34: 6029. 4 Froom J, Culpepper L, Green LA et al. A cross-national study of acute otitis media: risk factors, severity, and treatment at initial visit. Report from the international primary care network (IPCN) and the ambulatory sentinel practice network (ASPN). J. Am. Board. Fam. Pract. 2001; 14: 40617. 5 Gunasekera H, Knox S, Morris P, Britt H, McIntyre P, Craig JC. The spectrum and management of otitis media in Australian Indigenous and non-Indigenous children: a national study. Pediatr. Infect. Dis. J. 2007; 26: 68992. 6 Gunasekera H, Morris PS, Daniels J, Couzos S, Craig JC. Management of children with otitis media: a survey of Australian Aboriginal Medical Service practitioners. J. Paediatr. Child Health 2009; 45: 45763. 7 Morris PS. A systematic review of clinical research addressing the prevalence, aetiology, diagnosis, prognosis and therapy of otitis media in Australian Aboriginal children. J. Paediatr. Child. Health 1998; 34: 48797. 8 Bluestone CD. Epidemiology and pathogenesis of chronic suppurative otitis media: implications for prevention and treatment. Int. J. Pediatr. Otorhinolaryngol. 1998; 42: 20723. 9 World Health Organization. Chronic Suppurative Otitis Media. Burden of Illness and Management Options. Geneva, Switzerland: WHO, 2004. 10 Stuart J. The history and epidemiology of ear disease in Australian Aboriginal children. Aust. J. Otolaryngol. 1995; 2: 610.
11 Moran DJ, Waterford JE, Hollows F, Jones DL. Ear disease in rural Australia. Med. J. Aust. 1979; 2: 2102. 12 Couzos S, Metcalf S, Murray RB. Systematic Review of Existing Evidence and Primary Care Guidelines on the Management of Otitis Media in Aboriginal and Torres Strait Islander Populations. Canberra: Commonwealth Department of Health and Aged Care, 2001. 13 Leach AJ, Boswell JB, Asche V, Nienhuys TG, Mathews JD. Bacterial colonization of the nasopharynx predicts very early onset and persistence of otitis media in Australian aboriginal infants. Pediatr. Infect. Dis. J. 1994; 13: 23947. 14 Boswell JB, Nienhuys TG. Onset of OM in the rst eight weeks of life in Aboriginal and non-Aboriginal Australian infants. Ann. Otol. Rhinol. Laryngol. 1995; 7: 5429. 15 Nyquist A-C, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA 1998; 279: 8757. 16 Davidson J, Hyde ML, Alberti PW. Epidemiologic patterns in childhood hearing loss: a review. Int. J. Pediatr. Otorhinolaryngol. 1989; 17: 23966. 17 Shwartz SR, Gates GA. Economic costs. In: Rosenfeld RM, Bluestone CD, eds. Evidence-Based Otitis Media, 2nd edn. Hamilton: BC Decker Inc, 2003. 18 Access Economics Pty Ltd. The cost burden of otitis media in Australia. Available from: http://www.accesseconomics.com.au/ publicationsreports/showreport.php?id=190&searchfor=2009& searchby=year. [accessed March 2009]. 19 Lubianca Neto JF, Hemb L, Silva DB. Systematic literature review of modiable risk factors for recurrent acute otitis media in childhood. J. Pediatr. (Rio J). 2006; 82: 8796. 20 Uhari M, Mantysaari K, Niemela M. A meta-analytic review of risk factors for acute otitis media. Clin. Infect. Dis. 1996; 22: 107983. 21 Morris P, Ballinger D, Leach A et al. Recommendations for Clinical Care Guidelines on the Management of Otitis Media in Aboriginal and Torres Strait Islander Populations. Canberra: Ofce for Aboriginal and Torres Strait Islander Health, Commonwealth Department of Health and Aged Care, ACT; 2001. 22 Antibiotic Expert Group. Therapeutic Guidelines. Antibiotic. Version 13. Melbourne: Therapeutic Guidelines Limited, 2006. 23 Academy Academy of Pediatrics Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics 2004; 113: 145165.
Journal of Paediatrics and Child Health 45 (2009) 554563 2009 The Authors Journal compilation 2009 Paediatrics and Child Health Division (Royal Australasian College of Physicians)
561
Management of children with otitis media
H Gunasekera et al.
24 SIGN. Diagnosis and management of childhood otitis media in primary care. A national clinical guideline, 2003. Available from: http:// www.sign.ac.uk. [accessed April 2004]. 25 Hayden GF. Acute suppurative otitis media in children. Diversity of clinical diagnostic criteria. Clin. Pediatr. 1981; 20: 99104. 26 Takata GS, Chan LS, Morphew T, Manqione-Smith R, Morton SC, Shekelle P. Evidence assessment of the accuracy of methods of diagnosing middle ear effusion in children with otitis media with effusion. Pediatrics 2003; 112 (6pt1): 137987. 27 Takata GS, Chan LS, Shekelle P et al. Diagnosis, Natural History, and Late Effects of Otitis Media with Effusion. Evidence Report/Technology Assessment: Number 55. AHRQ publication number 02-EO26. Rockville, MD: Agency for Healthcare Research and Quality, 2002. 28 Gates GA, Klein JO, Lim DJ et al. Recent advances in otitis media, 1: denitions, terminology, and classication of otitis media. Ann. Otol. Rhinol. Laryngol. 2002; 111: 818. 29 Thanaviratananich S, Laopaiboon M, Vatanasapt P. Once or twice daily versus three times daily amoxicillin with or without clavulanate for the treatment of acute otitis media. Cochrane Database Syst. Rev. 2008; Issue 4. Art. No.: CD004975. DOI: 10.1002/ 14651858.CD004975.pub2. 30 Coleman C, Moore M. Decongestants and antihistamines for acute otitis media in children. Cochrane Database Syst Rev. 2008; Issue 3. Art. No.: CD001727. DOI: 10.1002/14651858.CD001727.pub4. 31 Rovers MM, Glasziou P, Appelman CL et al. Antibiotics for acute otitis media: a meta-analysis with individual patient data. Lancet 2006; 368: 142935. 32 Leach AJ, Morris PS Antibiotics for the prevention of acute and chronic suppurative otitis media in children. Cochrane Database Syst. Rev. 2006; Issue 4. Art. No.: CD004401. DOI: 10.1002/ 14651858.CD004401.pub2. 33 Foxlee R, Johansson AC, Wejfalk J, Dawkins J, Dooley L, Del Mar C. Topical analgesia for acute otitis media. Cochrane Database Syst. Rev. 2006; Issue 3. Art. No.: CD005657. DOI: 10.1002/ 14651858.CD005657.pub2. 34 Glasziou PP, Del Mar CB, Sanders SL, Hayem M. Antibiotics for acute otitis media in children. Cochrane Database Syst. Rev. 2004; CD000219. 35 Spurling GKP, Del Mar CB, Dooley L, Foxlee R. Delayed antibiotics for symptoms and complications of respiratory infections. Cochrane Database Syst. Rev. 2004; Issue 4. CD004417. 36 Rosenfeld RM, Kay D. Natural history of untreated otitis media. Laryngoscope 2003; 113: 164557. 37 Takata GS, Chan LS, Shekelle P, Morton SC, Mason W, Marcy SM. Evidence assessment of management of acute otitis media. I. The role of antibiotics in treatment of uncomplicated acute otitis media. Pediatrics 2001; 108: 23947. 38 Kozyrskyj A, Hildes-Ripstein GE, Longstaffe SE et al. Short course antibiotics for acute otitis media. Cochrane Database Syst Rev. 2000, Issue 2. Art. No.: CD001095. DOI: 10.1002/14651858.CD001095. 39 Rosenfeld RM, Vertees JE, Carr J et al. Clinical efcacy of antimicrobial drugs for acute otitis media: metaanalysis of 5400 children from thirty-three randomized trials. J. Pediatr. 1994; 124: 35567. 40 Williams RL, Chalmers TC, STange KC, Chlamers FT, Bowlin SJ. Use of antibiotics in preventing recurrent acute otitis media and in treating otitis media with effusion. A meta-analystic attempt to resolve the brouhaha. JAMA 1993; 270: 134451. 41 Sharland M, Kendall H, Yeates D et al. Antibiotic prescribing in general practice and hospital admissions for peritonsillar abscess, mastoiditis, and rheumatic fever in children: time trend analysis. BMJ 2005; 331: 3289. 42 Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. A pragmatic randomised controlled trial of two prescribing strategies for acute otitis media. BMJ 2001; 322: 33642.
43 Cantekin EI, McGuire TW. Antibiotics are not effective for otitis media with effusion reanalysis of meta-analyses. Otorhinolaryngol. Nova. 1998; 8: 21422. 44 Rosenfeld RM, Post JC. Meta-analysis of antibiotics for the treatment of otitis media with effusion. Otolaryngol. Head Neck Surg. 1992; 106: 3780386. 45 Thomas CL, Simpson S, Butler C, van der Voort J. Oral or topical nasal steroids for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst. Rev. 2006; Issue 3. Art. No.: CD001935. DOI: 10.1002/14651858.CD001935.pub2. 46 McDonald S, Langton Hewer CD, Nunez DA. Grommets (ventilation tubes) for recurrent acute otitis media in children. Cochrane Database Syst. Rev. 2008, Issue 4, Art. No.: CD004741. DOI: 10.1002/ 14651858.CD004741.pub2. 47 Perera R, Haynes J, Glasziou P, Heneghan CJ. Autoination for hearing loss associated with otitis media with effusion. Cochrane Database Syst Rev. 2006, Issue 4, Art. No.: CD006285. DOI: 10.1002/ 14651858.CD006285. 48 Grifn G, Flynn CA, Bailey RE, Schultz JK Antihistamines and/or decongestants for otitis media with effusion (OME) in children. Cochrane Database Syst. Rev. 2006, Issue 4, Art. No.: CD003423. DOI: 10.1002/14651858.CD003423.pub2. 49 Rovers MM, Black N, Browning GG, Maw R, Zielhuis GA, Haggard MP. Grommets in otitis media with effusion: an individual patient data meta-analysis. Arch. Dis. Child 2005; 90: 4805. 50 Lous J, Burton MJ, Felding J, Ovesen T, Rovers M, Williamson I. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst. Rev. 2005; Issue 1. Art. No.: CD001801. DOI: 10.1002/14651858.CD001801. pub2. 51 Kay DJ, Nelson M, Rosenfeld RM. Meta-analysis of tympanostomy tube sequelae. Otolaryngol. Head Neck Surg. 2001; 124: 37480. 52 American Academy of Pediatrics. Clinical practice guideline otitis media with effusion. Pediatrics 2004; 113: 141229. 53 van der Veen EL, Rovers MM, Albers FWJ, Sanders EAM, Schilder AGM. Effectiveness of Trimethoprim/sulfamethoxazole for children with chronic active otitis media: a randomized, placebo-controlled trial. Pediatrics 2007; 119: 897904. 54 Paradise JL, Feldman HM, Campbell TF et al. Tympanostomy tubes and developmental outcomes at 9 to 11 years of age. NEJM 2007; 356: 24861. 55 Macfadyen CA, Acuin JM, Gamble CL Systemic antibiotics versus topical treatments for chronically discharging ears with underlying eardrum perforations. Cochrane Database Syst Rev. 2006; Issue 1. Art.No.: CD005608. DOI: 10.1002/14651858.CD005608. 56 Roberts JE, Rosenfeld RM, Zeisel SA. Otitis media and speech and language: a meta-analysis of prospective studies. Pediatrics 2004; 113: 23848. 57 Abes G, Espallardo N, Tong M et al. A systematic review of the effectiveness of ooxacin otic solution for the treatment of suppurative otitis media. Otorhinolaryngology 2003; 65: 10616. 58 Couzos S, Lea T, Mueller R, Murray R, Culbong M. Effectiveness of ototopical antibiotics for chronic suppurative otitis media in Aboriginal children: a community-based, multicentre, doubleblind randomised controlled trial. Med. J. Aust. 2003; 179: 18590.
Clinical Quiz
Q1. Aiden, a 6 year old boy, is brought to you with a history of recurrent otitis media. His right external ear canal is full of purulent discharge. What is the most likely diagnosis and best management strategy?
562
Journal of Paediatrics and Child Health 45 (2009) 554563 2009 The Authors Journal compilation 2009 Paediatrics and Child Health Division (Royal Australasian College of Physicians)
H Gunasekera et al.
Management of children with otitis media
A. He has acute otitis externa and should be treated with ear wicks and topical steroid and antibiotic drops instilled with tragal pressure. B. If Aiden is reported to have had the discharge for 2 months he should be treated with regular ear cleaning and topical antibiotic drops but does not need initial oral antibiotic therapy. C. He should be treated with topical ciprooxacin drops for chronic suppurative otitis media alone. D. If the discharge is new he should be treated with topical antibiotic with corticosteroids as oral antibiotics have never been shown to improve outcomes in acute otitis media with otorrhoea. Q2. Mary is an 18 month old Aboriginal girl from a remote community. She is brought to you as she has a developed a low grade fever today and is pulling at her left ear. On examination you notice that it is her right ear that is bulging, red, opaque, and does not move on pneumatic otoscopy. The left tympanic membrane looks normal. Which of the following is the best approach? A. She has right acute otitis media and should be started on oral antibiotics immediately as she comes from a high-risk group. B. She has bilateral acute otitis media and should be started on oral amoxycillin 50 mg/kg/day for 7 days according to the OATSIH guidelines. C. She has right otitis media with effusion and needs an urgent hearing test as she is at risk of long-term learning disability if ventilation tubes are not provided within the next 4 to 6 weeks. D. She has right acute otitis media and could be managed with watchful waiting as she is over 1 year of age. Q3. A 3 year old Sudanese refugee child called Majak is brought to see you for a general health check. He has opaque tympanic membranes bilaterally. Both eardrums move sluggishly on pneumatic otoscopy and have at tympanograms (Type B). His mother tells you that he never listens to her and has been very naughty in the last year. Which of the following is the best approach? A. He has bilateral effusions and needs tympanostomy tubes. B. He has bilateral acute otitis media and should be started on oral antibiotics immediately as he is from a high risk group. C. Flat (Type B) tympanograms are normal. Peaked tympanograms are abnormal as the peak is a measure of the degree of bulging. D. He has bilateral otitis media with effusion and can be observed for 3months. He should have a hearing test if not previously done or if the effusions do not resolve over the next 3 months.
Clinical Quiz Answers
Q1. A. Incorrect: Acute otitis media with perforation and chronic suppurative otitis media are more likely than acute otitis externa in children. B. Correct: In the Macfadyen systematic review ear cleaning and topical therapy were the best treatment options for CSOM. C. Incorrect: Therapeutic Guidelines (Antibiotic) and the OATSIH guidelines for Aboriginal children, both recommend ear cleaning (dry mopping with rolled tissue spears) before instilling drops for CSOM. D. Incorrect: AOM with otorrhoea is much more likely to benet from oral antibiotics than AOM without otorrhoea [see Rovers review] Q2. A. Correct: Aboriginal children with AOM should be treated with oral amoxycillin [see OATSIH Guidelines from 2001]. B. Incorrect: Her left ear does not have an effusion (a requirement for any diagnosis of AOM or OME), so this is unilateral AOM. C. Incorrect: She is unlikely to have a bilateral hearing loss as the left ear is normal. There no evidence of long-term learning benets from early instillation of ventilation tubes [Paradise study]). Data from high-risk populations are lacking. She has right acute otitis media and could be managed with watchful waiting as she is over 1 year of age. D. Incorrect: Aboriginal children with AOM should be treated with oral amoxycillin [see OATSIH Guidelines from 2001]. For non-Aboriginal children, this approach would be reasonable [see Rovers review]. Q3. A. Incorrect: The majority of middle ear effusions in children resolve within 3 months and no intervention is required acutely. B. Incorrect: The presentation is more consistent with OME than AOM. Refugee children may be at increased risk due to poverty and poor general health but African children in general are not a high-risk group. C. Incorrect: Flat tympanograms (Type B) accurately indicate the presence of middle ear effusions and high peaked tympanograms (Type A) accurately indicate no effusions. [See Takata review] Other tympanogram types are not accurate at predicting effusions. D. Correct: Children with bilateral effusions will have some degree of hearing impairment and the parents need to be aware of this. A hearing test is a good idea in this situation and is recommended for children with bilateral disease which does not resolve by 3 months.
Journal of Paediatrics and Child Health 45 (2009) 554563 2009 The Authors Journal compilation 2009 Paediatrics and Child Health Division (Royal Australasian College of Physicians)
563
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Materi CKD 2019Dokument88 SeitenMateri CKD 2019ditya.novianti06Noch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- 02 IV TherapyDokument3 Seiten02 IV Therapybunso padillaNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- 3 ATN Lameire2013Dokument10 Seiten3 ATN Lameire2013angela_karenina_1Noch keine Bewertungen
- Medical RecordDokument14 SeitenMedical RecordZakwan AhmadNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- MEDIWAYSDokument79 SeitenMEDIWAYSRaj KumarNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Infusion Pumps: Why They're Actually Not Pumping: Martin BeckerDokument12 SeitenInfusion Pumps: Why They're Actually Not Pumping: Martin BeckeryofiNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Medical Oncology JNR HandbookDokument50 SeitenMedical Oncology JNR Handbookhmudeveloper100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Med-Fit 3: Instruction Manual Betriebsanleitung Manuel D'instructionDokument52 SeitenMed-Fit 3: Instruction Manual Betriebsanleitung Manuel D'instructionCarlos ParraNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Bio-Medical Waste Management Rules: DR NaveenDokument26 SeitenBio-Medical Waste Management Rules: DR Naveenmani kandanNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Congenital DiseaseDokument39 SeitenCongenital DiseaseRavi SharmaNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Obsessive Compulsive DisorderDokument2 SeitenObsessive Compulsive DisorderMargaretDeniseDelRosarioNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Indicative Term Sheet Bank Islami Pakistan Limited Akbar Chowk Branch, LahoreDokument6 SeitenIndicative Term Sheet Bank Islami Pakistan Limited Akbar Chowk Branch, LahoreSaadatNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Practice HPIDokument3 SeitenPractice HPImedicalmatins100% (1)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Lowry Starla - NGR 5884 Curriculum VitaeDokument2 SeitenLowry Starla - NGR 5884 Curriculum Vitaeapi-289861911Noch keine Bewertungen
- Virginia HendersonDokument4 SeitenVirginia HendersonJoyce TanNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- CPR and First Aid PowerpointDokument21 SeitenCPR and First Aid PowerpointZawawiIbnuRosyidNoch keine Bewertungen
- Sinew Channels by J Yuen002Dokument81 SeitenSinew Channels by J Yuen002Jonathan100% (1)
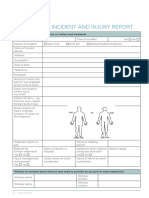
- Whs Form 10: Incident and Injury Report: 22 Safework NSWDokument2 SeitenWhs Form 10: Incident and Injury Report: 22 Safework NSWalexNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Diadens PC ManualDokument31 SeitenDiadens PC Manualvdbroger100% (1)
- GP Factsheet - Steroids and The EyeDokument6 SeitenGP Factsheet - Steroids and The EyeBima RizkiNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Prevention of Crown and Root Caries in AdultsDokument19 SeitenPrevention of Crown and Root Caries in AdultsnataliaNoch keine Bewertungen
- Cancer - January 1954 - Butler - The Use of Hypnosis in The Care of The Cancer PatientDokument14 SeitenCancer - January 1954 - Butler - The Use of Hypnosis in The Care of The Cancer PatientRenoir FontesNoch keine Bewertungen
- Chronic Renal FailureDokument18 SeitenChronic Renal FailureJoan Carla BocoNoch keine Bewertungen
- Magnesium The King of MineralsDokument19 SeitenMagnesium The King of Mineralswxcvbnnbvcxw100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Myths of DialysisDokument26 SeitenMyths of DialysisSijo Muthukad M100% (1)
- Acute PancreatitisDokument48 SeitenAcute PancreatitisapocruNoch keine Bewertungen
- Biophysics 102 Lecture 3 1Dokument13 SeitenBiophysics 102 Lecture 3 1Nada Atef KoraitemNoch keine Bewertungen
- ACLS Study Guide NewDokument35 SeitenACLS Study Guide NewNIRANJANA SHALININoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Detecting The Differences Radiculopathy, Myelopathy and Peripheral NeuropathyDokument70 SeitenDetecting The Differences Radiculopathy, Myelopathy and Peripheral Neuropathyapi-19502000100% (8)
- Drug Study For Mini Case PRESDokument11 SeitenDrug Study For Mini Case PRESKevin AliasasNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)