Beruflich Dokumente
Kultur Dokumente
FallClinical March08
Hochgeladen von
Rajesh MevawalaOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
FallClinical March08
Hochgeladen von
Rajesh MevawalaCopyright:
Verfügbare Formate
Supplement to the March 2008
skin &
AGING
Articles in this supplement are based on selected presentations from the 2007 Fall Clinical Dermatology Conference held October 1821, 2007 in Las Vegas, NV.
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
FALL CLINICAL DERMATOLOGY 2007
AN UPDATE ON ADVANCES IN ACNE AND EXCERPTS FROM WHATS NEW IN THE MEDICINE CABINET
BY JAMES Q. DEL ROSSO, D.O., F.A.O.C.D.
DERMATOLOGY RESIDENCY DIRECTOR VALLEY HOSPITAL MEDICAL CENTER LAS VEGAS, NV
ACNE UPDATE
cne vulgaris is one of the most common diagnoses encountered in clinical practice. Most advances relate to improvements in vehicle technology and new data, especially on combination therapy.
BENZOYL PEROXIDE/CLINDAMYCIN + TOPICAL RETINOID THERAPY
Clinical studies have evaluated BPO-clindamycin gel (Duac) used in combination with either tazarotene cream 0.1% (Tazorac), tretinoin microsphere gel 0.04% or 0.1% (Retin-A Micro), or adapalene gel 0.1% (Differin). The BPO-clindamycin gel and the topical retinoid were applied in the morning and at bedtime, respectively, in all of the studies. The combination topical approach of a retinoid used along with BPO-clindamycin from the outset of therapy exhibited inflammatory and non-inflammatory lesion reduc-
James Q. Del Rosso, D.O., F.A.O.C.D.
COMBINATION TOPICAL THERAPY
Topical retinoids are a vital component of both initial tre a tment and maintenance therapy for acne vulgaris. They exhibit the ability to reduce both non-inflammatory lesions and inflammatory acne lesions. Benzoyl peroxide also remains a foundation of acne treatment, exhibiting the ability to markedly reduce P ropionibacterium acnes counts and prevent emergence of P. acnes strains that are less sensitive to antibiotics, such as erythromycin and tetracycline. Benzoyl peroxide, including formulations that also contain clindamycin, is well established for reducing inflammatory acne lesions but also for decreasing non-inflammatory lesions by approximately 25% to 30% in clinical trials. Multiple clinical trials have evaluated tretinoin (Retin-A M i c ro, Tretin-X, Atralin), adapalene (Differin), and tazarotene (Tazorac), including initial pivotal monotherapy studies and trials utilizing combination therapy with a benzoyl pero x i d e (BPO)-containing formulation. The availability of newer vehicles that decrease the potential for and the intensity of initial skin irritation observed with topical retinoid therapy (retinoid dermatitis), such as tretinoin formulated in the micro s p h e re gel (Retin-A Micro) and the aqueous-based gel (Atralin), has allowed for effective combination topical therapy of acne vulgaris from the outset. With these newer vehicles, more patients are able to tolerate combination topical treatment with few or no signs of skin irritation.
NEWER VEHICLES THAT DECREASE THE POTENTIAL FOR AND THE INTENSITY OF INITIAL SKIN IRRITATION OBSERVED WITH TOPICAL RETINOID THERAPY HAVE ALLOWED FOR EFFECTIVE COMBINATION TOPICAL THERAPY OF ACNE VULGARIS.
tions after 12 weeks of at least 60% and 55%, respectively, with all 3 retinoids (Figures 14). In one of the trials, the study arm using both BPO-clindamycin gel (Duac) and tazarotene 0.1% cream (Tazorac) demonstrated a marked reduction in non-inflammatory lesions at Week 4 (34%) and Week 8 (64%) (Figure 3). Tolerability results were very favorable in all 3 trials. A case report series of BPO microsphere cream (NeoBenz Micro) applied once daily in the morning used in combination with tretinoin microsphere gel 0.04% (Retin-A Micro) once daily at night also proved to exhibit effective results with no reports of skin irritation.
PROPER SKIN CARE IN ACNE THERAPY
The use of appropriate skin care is vital in the management of acne vulgaris, allowing for preservation of epidermal barrier integrity and function. The use of a gentle facial cleanser and
SUPPLEMENT TO SKIN & AG IN G MARC H 20 08 3
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
well-formulated moisturizer both reduces the potential for skin irritation associated with topical medications and enhances the ability of acne medications to reduce lesions. A prepackaged kit is available that contains tretinoin cream, a gentle cleanser and a moisturizer (Tretin-X), thus providing an additional convenience value. A recent study evaluating the use of tazarotene 0.1% cream (Tazorac) and a ceramide-based moisturizer cream (CeraVe Cream) in subjects with acne vulgaris demonstrated that application of the moisturizer first did not interfere with therapeutic results and mitigated signs and symptoms of skin irritation.
NEWER TOPICAL RETINOID FORMULATIONS
Newer topical retinoid formulations that have emerged add to the dermatology armamentarium. Adapalene gel 0.3% (Differin 0.3%) once daily has been shown to produce twothirds of its therapeutic effect within the first month of tre a tment. A water-based gel containing tretinoin 0.05% (Atralin)
4 MARCH 2008 SUPPLEMENT TO SKIN & AGING
applied once daily proved to be comparable to, but not noninferior to, tretinoin microsphere gel 0.1% (Retin-A Micro) based on data from a 12-week controlled study; however, tolerability was superior with the aqueous-based gel. A combination aqueous polymer gel containing clindamycin phosphate 1.2% and tretinoin 0.025% (Ziana) includes tretinoin in both solubilized and crystalline forms. The crystalline form of tretinoin allows for slow release of active drug with very low skin irritation, and particle size is tightly controlled, thus providing optimal penetration. The superior efficacy of the combination clindamycin/tretinoin gel applied once daily as compared to individual active components was established in large, Phase III trials in subjects with mild, moderate, and severe acne vulgaris (Figure 5).
NEWER BENZOYL PEROXIDE FORMULATIONS
Newer formulations of BPO appear to offer the advantages of reduced skin irritation without loss of efficacy and potential-
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
ly superior efficacy in some cases, as compared to some older formulations (F i g u re 6). A triple moisturizer- i n g re dient formulation (Benziq), available as a wash and leave on gel, was shown to be less irritating than some other comparator BPO products in a cumulative irritancy study. The microsphere cream formulation of BPO 5.5% (NeoBenz Micro) has demonstrated efficacy in clinical studies with a very favorable tolerability profile; one study demonstrated superior efficacy with the tretinoin microsphere cream (NeoBenz Micro) as compared to benzoyl peroxide gel 6% (Triaz) in patients with acne vulgaris. A direct from the doctor 3-part acne treatment system (Clenziderm MD, Normal to Oily Skin) utilizing a salicylic acid 2%-containing cleanser and pore gel followed by a 5% gel containing solubilized BPO has been evaluated in several trials. Unlike conventional BPO formulations, the solubilized BPO in the 3-part proprietary system is micronized such that individual BPO particles are small enough to penetrate into the follicular orifice where P. acnes resides. This 3-part acne treatment system has demonstrated both reduction in P. acnes and efficacy comparable to benzoyl peroxide/clindamycin gel (Benzaclin) in preliminary trials along with high patient pre f e rence ratings. Another 3-part acne treatment system, available from the same manufacturer, contains solubilized BPO 5% lotion combined with a gentle cleanser and moisturizer (Clenziderm MD, Normal to Dry Skin) and does not contain the components with salicylic acid 2%.
The only progestin available in an oral contraceptive (OC) formulation that exhibits antiandrogen activity is drosperinone found in a formulation that also contains 20 mcg of ethinyl estradiol (YAZ). This formulation is approved for moderate acne and is comprised of 24 days of active therapy and 4 hormonefree days, resulting in a short menstrual cycle. In a placebocontrolled, randomized, double-blind, 6-cycle clinical study, 451 females received the active OC formulation and 442 received placebo. After the first cycle, subjects receiving active OC treatment demonstrated a markedly greater reduction in total acne lesions, which continued to progress throughout the sixth cycle (study endpoint).
ACNE APPEARS TO OCCUR SECONDARY TO INCREASED LOCAL ANDROGEN PRODUCTION WITHIN SEBACEOUS GLANDS.
ORAL CONTRACEPTIVES IN ACNE T H E R A P Y
The majority of post-teenage females with acne exhibit normal serum androgen levels. Acne appears to occur secondary to increased local androgen production within sebaceous glands. Many adult-onset or adult-persistent cases of acne vulgaris in females present with a preponderance of inflammatory lesions involving the lower cheeks, jawline, chin and lateral neck.
When using OCs to treat females with acne vulgaris, side effects may be decreased by using formulations that contain lower doses of the estrogenic component (ethinyl estradiol). In addition to reduction in acne lesions, other potential benefits of OC use include regulation of menstrual cycle, reduction in perimenstrual symptoms, such as cramping, decrease in ovarian cyst formation, reduction in bone demineralization, and decrease in risk of ovarian and colorectal cancer. Potential side effects of OC use include thromboembolism and cerebral vascular accident. It has been recommended that clinicians not prescribe OCs to women who smoke due to an increased risk of vascular-related complications.
SUPPLEMENT TO SKIN & AG IN G MARC H 20 08 5
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
ORAL ANTIBIOTICS IN ACNE T H E R A P Y
Dermatologists have been prescribing oral antibiotics, such as tetracycline, doxycycline and minocycline, for acne vulgaris since the 1950s, 1960s and 1970s, re spectively, based on clinical experience and a scattered collection of small clinical studies. However, extended-release minocycline (Solodyn) is the only oral antibiotic that is approved by
THERE IS NO SCIENTIFIC EVIDENCE THAT PILL SPLITTING OF ANY TABLET FORMULATION OF DOXYCYCLINE PRODUCES ANTI-INFLAMMATORY ACTIVITY WITHOUT AN ANTIBIOTIC EFFECT.
An enteric-coated tablet of doxycycline (Doryx) appears to provide reduced gastrointestinal (GI) upset as compared to immediate-release doxycycline formulations. However, enteric coating is not synonymous with extended-release and serves to delay initial gastric dissolution in an attempt to reduce GI upset. Enteric coating may allow for once-daily administration in some patients when using 150 mg to 200 mg of doxycycline daily. With the exception of anti-inflammatory dose doxycycline administered once daily, ie, doxycycline 40-mg delayed-release capsule (Oracea), all other formulations of doxycycline produce antibiotic activity. Anti-inflammatory dose doxycycline is FDAapproved for treatment of rosacea. There is no scientific evidence that pill splitting of any tablet formulation of doxycycline produces anti-inflammatory activity without an antibiotic effect.
WHATS NEW IN THE MEDICINE CABINET
TREATMENTS FOR ROSACEA
The only FDA-approved oral therapy for rosacea is antiinflammatory dose doxycycline (Oracea), administered as a patented doxycycline 40-mg delayed-release capsule once daily. The mechanism of anti-inflammatory dose doxycycline appears to relate at least partially to downregulation of the activity of several matrix metalloprotease enzymes (MMPs). Antiinflammatory dose doxycycline offers advantages over conventional oral antibiotic therapy. These include efficacy with a favorable safety profile, presence of long-term 9-month safety data included in approved product labeling, and lack of antibiotic activity as determined by long-term microbiologic studies evaluating oral, skin, gastrointestinal and vaginal flora. The absence of antibiotic activity with anti-inflammatory dose doxycycline is supported by the absence of vaginal candidiasis in female subjects who were actively treated in the pivotal Phase III studies.
the U.S. Food and Drug Administration (FDA) based on large-scale, Phase III studies demonstrating efficacy and safety. The extended-release formulation of minocycline produces a slower time to peak plasma level (Cmax) and a d e c rease in total cumulative exposure to minocycline as c o m p a red to immediate-release minocycline formulations. Results from Phase II and Phase III trials substantiate therapeutic equivalence for acne vulgaris with extendedrelease minocycline when dosed at 1 mg/kg/day as compared to 2 mg/kg/day and 3 mg/kg/day. Importantly, a markedly lower incidence of acute vestibular side eff e c t s (ie, dizziness) comparable to placebo was seen at 1 mg/kg/day as compared to higher doses.
6 MARCH 2008 SUPPLEMENT TO SKIN & AGING
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
Unlike anti-inflammatory dose doxycycline, doxycycline 100 mg daily administered over a 2-week period has been shown to select for multiple resistant organisms within 7 days, with more than 32.2% of organisms obtained from nasopharyngeal cultures demonstrating resistance to doxycycline as compared to 2.2% at baseline. Doxycycline 50 mg once daily achieves serum levels that exceed the minimum inhibitory concentration (MIC) of several bacteria for 2 to 4 hours. A study evaluating the combination of metronidazole gel 1% (MetroGel 1%) and anti-inflammatory dose doxycycline (Oracea), both used once daily, confirmed that the combination regimen produced superior therapeutic benefit as compared to topical metronidazole alone in patients with inflammatory rosacea. After 4 weeks, the combination regimen produced essentially the same reduction in inflammatory lesions that was achieved with metronidazole gel 1% over 12 weeks (Figure 7) . A recent trial demonstrated that azelaic acid gel 15% (Finacea) once daily is therapeutically equivalent to twicedaily application in subjects with inflammatory ro s a c e a (F i g u re 8). Study endpoints utilized quantitative, qualitative, and static assessments, including lesion count evaluations and global assessments. Once-daily use of azelaic acid gel 15% is more likely to be associated with optimal compliance and offers a cost benefit over time as compared to twice-daily application.
References 1. Del Rosso JQ. Recently approved systemic therapies for acne vulgaris and rosacea. Cutis. 2007;80(2):113120. 2. Plott RT, Wortzman MS. Key bioavailability features of a new extendedrelease formulation of minocycline hydrochloride tablets. Cutis. 2006;78(4 Suppl):610. 3. Fleischer AB Jr, Dinehart S, Stough D, et al. Safety and efficacy of a new e x t e n d e d - re lease formulation of minocycline. Cutis. 2006;78(4 Suppl):2131. 4. Del Rosso JQ. Scientific panel on antibiotic use in dermatology. Submitted for publication 2008. 5. Del Rosso JQ, Webster GF, Jackson M, et al. Two randomized phase III clinical trials evaluating anti-inflammatory dose doxycycline (40-mg doxycycline, USP capsules) administered once daily for treatment of rosacea. J Am Acad Dermatol. 2007;56(5):791802. 6. Webster G, Del Rosso JQ. Anti-inflammatory activity of tetracyclines. Dermatol Clin. 2007;25(2):133135. 7. Walker C, Webster GF, Del Rosso JQ. Effect of doxycycline 100 mg daily on emergence of antibiotic resistance. Presented at the Fall Clinical Dermatology Conference in Las Vegas, NV, October 1821, 2007. 8. Fowler JF Jr. Combined effect of anti-inflammatory dose doxycycline (40mg doxycycline, USP monohydrate contro l l e d - release capsules) and metronidazole topical gel 1% in treatment of rosacea. J Drugs Dermatol. 2007;6(6):641645. 9. Fleischer AB, Thiboutot D, Del Rosso JQ. Comparison of azelaic acid gel 15% once daily versus twice daily in the treatment of rosacea. Presented at the World Congress of Dermatology in Buenos Aires, Argentina, October 15, 2007. 10. Data on file. Allergan Inc., Irvine, CA, 2008. 11. Del Rosso JQ, Tanghetti E. The clinical impact of vehicle technology using a patented formulation of benzoyl peroxide 5%/clindamycin 1% gel: comparative assessments of skin tolerability and evaluation of combination use with a topical retinoid. J Drugs Dermatol. 2006;5(2):160164. 12. Del Rosso JQ. Study results of benzoyl peroxide 5%/clindamycin 1% gel, adapalene 0.1% gel, and use in combination for acne vulgaris. J Drugs Dermatol. 2007;6(6):616622. 13. Tanghetti E, Abramovits W, Solomon B, et al. Tazarotene versus tazarotene plus clindamycin/benzoyl peroxide in the treatment of acne vulgaris: a multicenter, double-blind, randomized, parallel-group trial. J Drugs Dermatol. 2006;5(3):256261. 14. Bikowski JB, Del Rosso JQ. Results of a case report series using tretinoin microsphere cream alone and in combination regimens for acne vulgaris. Submitted for publication 2008. 15. Del Rosso JQ, Bikowski JB. Trolamine-containing topical emulsion: clinical applications in dermatology. Cutis. In press. 16. Broughton G 2nd, Janis JE, Attinger CE. The basic science of wound healing. Plast Reconstr Surg. 2006;117(7 Suppl):12S34S.
SUPPLEMENT TO SKIN & AG IN G MARC H 20 08 7
TROLAMINE-CONTAINING TOPICAL EMULSION
Trolamine-containing topical emulsion (Biafine) is an oil-inwater formulation that has been used for more than 3 decades in both the United States and Europe. The mechanism of action of trolamine-containing topical emulsion appears to be promotion of an increase in the number of macrophages recruited to the injury site, thereby reducing the time needed for healing. Macrophages promote wound healing and serve a central role in directing the course and progression of the wound-healing process. Therapeutic applications for trolaminecontaining topical emulsion include full-thickness wounds, superficial wounds, including those that are postoperative, dermal ulcers, radiation dermatitis, minor abrasions, actinic keratosis treatment sites after cryotherapy, and wounds that require second-intention healing after dermatologic surgery. The use of trolamine-containing topical emulsion for the treatment of radiation dermatitis has made it possible to reduce overall treatment time of chemotherapy and radiotherapy because the modalities could be administered simultaneously rather than sequentially. Additionally, trolamine-containing topical emulsion differs from topical neomycin and bacitracin because the latter 2 agents are well recognized as common causes of contact allergy.
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
IS IT REALLY ROSACEA?
A DISCUSSION OF DIFFERENTIAL DIAGNOSES, TREATMENTS AND ADVANCES IN RESEARCH
BY JOSEPH BIKOWSKI, M.D.
BIKOWSKI SKIN CARE CENTER SEWICKLEY, PA
here have been few, if any, new systemic or topical medications developed in the last few years for the treatment of rosacea, so oftentimes, advancement in therapy relies upon the correct diagnosis. The right medicine will not work with the wrong diagnosis. For every individual who pre s e n t s Joseph Bikowski, M.D. with a red, scaly face, the dermatologist will consider the differential diagnoses: rosacea, seborrheic dermatitis, irritant contact dermatitis, allergic contact dermatitis, etc. Is it really rosacea? Are there other things that can look like rosacea?
DIFFERENTIAL DIAGNOSES AND UNUSUAL FACES OF ROSACEA
Demodex dermatitis. When patients present with red, scaly faces, the first consideration is whether there is an infectious component or an infestation that can be cured or suppressed for a prolonged period of time. Cases of Demodex dermatitis can be treated with permethrin (Elimite) or crotamiton (Eurax) twice daily, morning and night, for 2 to 4 weeks. Case 1. A patient had been treated for almost 2 years for rosacea and then seborrheic dermatitis without improvement (Figure 1). A potassium hydroxide (KOH) preparation revealed Demodex. Because no other treatment had been effective, the patient was started on Elimite twice daily, and within 2 weeks, his face cleared. The red, scaly rash over his forehead, nose and malar eminence disappeared. The patient remained clear at 1-year follow-up. Rosacea, seborrheic dermatitis and Demodex dermatitis can exist separately or together. Oftentimes, the red scaling is not seborrheic dermatitis with rosacea or seborrheic dermatitis alone. Rather, it may be Demodex dermatitis.
8 MAR CH 2 008 SUPPL EMEN T TO SKI N & AGING
Patients in whom the diagnosis of rosacea is suspected should have KOH preparations performed on scrapings of the scales from their faces and empirical treatment with either Elimite or Eurax twice daily, morning and night, for 2 weeks. Individuals who are not improving with anti-rosacea therapy or anti-seborrheic dermatitis therapy who still have red, scaly faces should receive one of these topicals twice daily for 2 to 4 weeks. Steroid use/abuse/misuse dermatitis. Another unusual p resentation that may resemble rosacea is stero i d use/abuse/misuse dermatitis. Any cortisone molecule used frequently over a long period of time in a susceptible individual can produce steroid use/abuse/misuse dermatitis. Case 2. A 26-year-old woman presented with an intensely pruritic, erythematous, scaly, papular eruption of 6 months duration on her face (F i g u re 2). For that period of time, she had been applying a topical corticosteroid to her face 4 times daily. The steroid responsible for this was 0.5% hydrocortisone cream.
PATIENTS IN WHOM THE DIAGNOSIS OF ROSACEA IS SUSPECTED SHOULD HAVE KOH PREPARATIONS PERFORMED ON SCRAPINGS OF THE SCALES FROM THEIR FACES.
Plaque rosacea. The usual presentation for rosacea is erythema, papules and pustules on the central third of the face. However, there is a presentation called plaque rosacea in which erythema, edema, papules and pustules appear only in one isolated area, ie, on one cheek (Figure 3). These patients respond to rosacea therapy, especially systemic therapies.
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
FIGURE 1. DEMODEX DERMATITIS: AT BASELINE (LEFT) AND AFTER 2 WEEKS OF TREATMENT WITH PERMETHRIN TWICE DAILY (RIGHT).
BASELINE
AFTER 2 WEEKS
USUAL THERAPIES FOR ROSACEA
van Zuuren et al1 conducted a literature review of 71 randomized, controlled studies of rosacea therapy. Of the 71 studies, 29 met their inclusion criteria, but the quality in general of these studies was not considered very good. The conclusions were that topical metronidazole and azelaic acid a re effective therapies for rosacea. There was some evidence that oral metronidazole and tetracycline including doxycycline and minocycline are effective, but the take-away message was that there is a great need for randomized, controlled trials examining the efficacy of present medications for the treatment of rosacea. Del Rosso et al 2 conducted two such randomized, Phase III clinical trials evaluating the anti-inflammatory doxycycline 40 mg a day administered once daily for the treatment of rosacea. They concluded that once-daily anti-inflammatory dose doxycycline appears to be effective and safe for the treatment of ro s a c e a .
UNUSUAL TREATMENTS FOR ROSACEA
Skin care. The skin of the rosacea patient can be either oily or dry. Certainly, it can be extremely sensitive in some cases. There can be altered cutaneous vascular reactivity and, most importantly, skin barrier dysfunction, which is defined as increased transepidermal water loss, increased susceptibility to irritants, allergens and pathogens, and increased skin inflammation through cytokine-mediated lipogenesis. Skin barrier dysfunction exists in most inflammatory diseases, including atopic dermatitis, psoriasis, acne and aged, actinicly damaged skin. The stratum corneum is a bricks and mortar structure. Corneocytes are the bricks, and sitting between the corneocytes is the mortar, the lipid matrix, which has a certain constitution that needs to be restored. Ceramides are most important, constituting about 40% to 50% of the lipid matrix. In addition to the ceramides, the lipid matrix contains free sterols and free fatty acid. There are also lipid bilayers, which become a moisture barrier for the stratum corneum.
SUPPLEMENT TO SKIN & AG IN G MARC H 20 08 9
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
FIGURE 2. STEROID USE/ABUSE/MISUSE DERMATITIS: A 26-YEAR-OLD WOMAN WITH A 6-MONTH HISTORY OF AN ERYTHEMATOUS, PAPULAR, SCALY, INTENSELY PRURITIC FACIAL ERUPTION.
Additionally, inside the corneocytes is natural moisturizing factor. All of these can be disrupted in inflammatory diseases, so restoring them as part of skin care and treatment for rosacea and other inflammatory diseases is most important. Products that can restore the skin barrier are available over the counter and soon by prescription. CeraVe is available over the counter as a cleanser and a moisturizer. Another over-thecounter product is Triceram from Osmotics, and Elizabeth Arden also has a line of products available over the counter. Patients being treated for inflammatory skin disease, especially rosacea, should be encouraged to purchase one of these products as a cleanser and a moisturizer.
THERE IS AN INCREASED INCIDENCE OF ROSACEA PATIENTS WITH MIGRAINE HEADACHES. BOTH ROSACEA AND MIGRAINES ARE VASCULAR DILATATION PHENOMENA.
Isotretinoin. Isotretinoin is effective in the treatment of the facial edema that can be associated with acne, and it also is an effective treatment for rosacea. Isotretinoin 30 mg twice daily for the treatment of rosacea is an off-label indication, but it is something to consider. Aspirin. While papules and pustules are not much of a challenge, erythema can be. There is an increased incidence of rosacea patients with migraine headaches. Both rosacea and migraines are vascular dilatation phenomena. The repeated flushing associated with rosacea leaves one with persistent erythema. Neurologists recommend aspirin 81 mg long acting as prophylaxis against migraine headaches. It also works for rosacea flushing and blushing. If patients are asked to keep track of their flushing and blushing episodes with a calendar diary for 30 days after starting on 81 mg of aspirin daily it becomes evident that the episodes of flushing decrease in severity, intensity and rates of occurrence. Water-based emulsion or nonsteroidal cre a m . Other options for treating the erythema of rosacea are water-based emulsions or nonsteroidal creams. In a patient who has persistent erythema in whom Demodex dermatitis has been ruled out, use of Mimyx or Atopiclair may be effective (Figure 4).
FIGURE 3. PLAQUE ROSACEA: A 48-YEAR-OLD MAN WITH A 2-YEAR HISTORY OF AN EDEMATOUS, ERYTHEMATOUS PAPULE AND PUSTULE STUDDED LESION OF THE LEFT CHEEK.
ADVANCES IN BASIC RESEARCH
Yamasaki and colleagues 3 at the University of C a l i f o rnia, San Diego, have been studying cathelicidin
10 MARCH 200 8 SUPPLEMENT TO SKIN & AGING
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
FIGURE 4. ERYTHEMA OF ROSACEA: A 41-YEAR-OLD WOMAN WITH PERSISTENT ERYTHEMA OF ROSACEA BASELINE AND AFTER 4 WEEKS OF MIMYX TWICE DAILY.
BASELINE
AFTER 4 WEEKS
and stratum corneum tryptic enzymes, which lead to abnormal peptides and the signs and symptoms of rosacea. They discovered increased levels of cathelicidin and diff e rent cathelicidins in patients who have ro s a c e a versus those who do not have rosacea, and these pep-
CONCLUSION
Few new medications have been developed for the treatment of rosacea in recent years; however, even the newest rosacea treatment will not be effective if the patient does not have rosacea. In treating cases of suspected rosacea, it is important for the dermatologist to consider the differential diagnoses, such as seborrheic dermatitis and irritant/allergic contact dermatitis, and also to be aware of unusual presentations of rosacea, such as plaque rosacea. Basic skin care remains essential in the treatment of patients with rosacea, and new products that have become available over the counter offer patients a wider variety from which to choose. Finally, further research on the role of cathelicidin in rosacea may provide dermatologists new treatment options in the future.
References 1. van Zuuren EJ, Gupta AK, Gover MD, Graber M, Hollis S. Systematic review of rosacea treatments. J Am Acad Dermatol. 2007;56(1):107115. 2. Del Rosso JQ, Webster GF, Jackson M, et al. Two randomized phase III clinical trials evaluating anti-inflammatory dose doxycycline (40-mg doxycycline, USP capsules) administered once daily for treatment of rosacea. J Am Acad Dermatol. 2007;56(5):791802. 3. Yamasaki K, Di Nardo A, Bardan A, et al. Increased serine protease activity and cathelicidin promotes skin inflammation in rosacea. Nat Med. 2007;13(8):975980.
A NEW AREA OF RESEARCH FOR ROSACEA THAT APPEARS PROMISING IS DETERMINING THE ROLE OF CATHELICIDINS AND TRYPTIC ENZYMES AND THEIR POSSIBLE ASSOCIATIONS WITH ROSACEA.
tides can lead to inflammation, which can be blocked by the use of antibiotics. Further study is warranted to determine how decreasing cathelicidin will advance rosacea therapy.
SUPPLEMENT TO SKIN & AGING MARCH 2008 11
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
TREATING ACNE WITH ORAL CONTRACEPTIVES
A GUIDE FOR SAFE, EFFECTIVE AND EFFICIENT PRESCRIBING
BY JULIE C. HARPER, M.D.
UNIVERSITY OF ALABAMA BIRMINGHAM BIRMINGHAM, AL hile some dermatologists have been prescribing oral contraceptives for the treatment of acne for many years with much success, others are resistant. The goal of this article is to assure the safe, effective and efficient prescription of oral contraceptives for acne patients, which will result in improvements in patients acne Julie C. Harper, M.D. and their overall quality of life. Acne is a complex multifactorial disorder. Since there are 4 diff e rent causes in the pathogenetic process, combination t reatments that target the multiple pathogenetic factors will offer the greatest improvement in the shortest amount of time. Oral contraceptives can be added to the armamentarium as another option for treatment. The 4 causes of acne are follicular epidermal hyperproliferation, excess sebum, Propionibacterium acnes and inflammation. During follicular epidermal hyperproliferation, plugging causes the development of comedones and microcomedones. For excess sebum, hormonal therapy, whether it is spironolactone, flutamide or oral contraceptives, creates an antiandrogen effect that has most of its impact on the sebaceous gland. While probably not the first event in the pathogenetic process, Propionibacterium acnes certainly is a cause. Also, whether or not inflammation is the first event in the process or it is secondary to P. acnes is a difficult question to answer. Oral contraceptives are not monotherapy for acne; rather, they fall into the mix of topical retinoids, benzoyl peroxides, and antibiotics. The type of oral contraceptive prescribed for acne is a combination of ethinyl estradiol and a progestin. Ethinyl estradiol varies in dose from pill to pill from 20 micrograms to 50 micrograms in a pill. The amount of ethinyl estradiol is important, because many of the risk factors associated with birth control pills are associated with higher doses of
ethinyl estradiol. The progestins in combination birth control pills vary widely but may include norethindrone acetate, levonorgestrel, desogestrel, norgestimate, and drospirenone among others. Drospirenone is the only progestin available in the United States that is antiandrogenic alone. Some other progestins can be proandrogenic. Oral contraceptives are antiandrogenic because ethinyl estradiol in combination birth control pills increases sex hormone binding globulin. Sex hormone binding globulin acts as a sponge it soaks up free testosterone and decreases the amount that is free and circulating and capable of having its impact at the sebaceous gland, for example. Also, there is a negative feedback to the hypothalamus and pituitary, which results in decreased production and release of gonadotropin releasing hormone, luteinizing hormone and follicle stimulating hormone. This then results in decreased ovarian production of hormone. Also, because ovulation is blocked, the ovary produces less androgen. The novel progestin, dro s p i renone, is equivalent to about 25 mg of spironolactone when it is in a 3 mg dose, which is available in 2 birth control pills that are on the market now in the United States. Dro s p i renone has antimineralocorticoid properties as well.
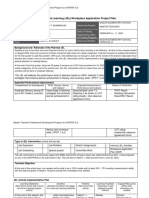
Attendees focus on new clinical information.
12 MARCH 2008 SUPPLEMENT TO SKIN & AGING
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
Attendees learning the latest in the field.
WHICH ORAL CONTRACEPTIVE WORKS IN ACNE?
It is likely that many oral contraceptives have some impact in acne. The dermatologist should choose one or two pills with which he or she feels comfortable and use those. The U.S. Food and Drug Administration (FDA) approved 3 oral contraceptives to treat acne: Estrostep, Ortho Tri-Cyclen and YAZ, which is the newcomer. YAZ was FDA approved for acne in 2007. A Cochrane meta-analysis evaluated 21 studies using oral contraceptive pills in the management of acne. The number one conclusion is it is difficult to compare trials because investigators in acne studies do not always use the same standard to measure whether or not acne is improving. The only real conclusion the authors could draw was that combination oral contraceptive pills that contained either cyproterone acetate or chlormadinone acetate both of which are not available in the United States were more effective than oral contraceptive pills that contained levonorgestrel. One study compared the effect of Yasmin to Diane-35 on cases of mild to moderate acne. Yasmin has dro s p i renone (3 mg), while Diane-35 has cyproterone acetate (2 mg), which also is antiandrogenic. In the head-to-head comparison, 128 people were included for 9 cycles of treatment. In both groups, the lesion counts were reduced by about 60% and the sex hormone binding globulin increased 3-fold in both groups. Yasmin also was compared head to head with Ortho TriCyclen. The study enrolled more than 500 women in each group for 6 months of treatment. Yasmin was superior in reduction of total lesion counts and investigators assessment, but in reduction of inflammatory lesions, the two were fairly equivalent. The newest oral contraceptive approved for the management of acne is dro s p i renone 3 mg and ethinyl estradi-
ol 20 micrograms (YAZ). In one study, 431 people were e n rolled and received either YAZ or placebo. There was about a 50% mean percent change in inflammatory lesions by the end of the sixth month of treatment. Since this was monotherapy, 50% reduction is an impressive change.
ORAL CONTRACEPTIVE RISKS
One reason dermatologists may not prescribe oral contraceptives for their acne patients is the risks associated with birth control pills. These risks include venous thromboembolism, stroke, myocardial infarction and breast cancer. Venous thromboembolism. The risk of venous thromboembolism is tripled in current users of oral contraceptives. It is increased to 4 to 18 events per 10,000 woman-years. The risk increases with higher doses of ethinyl estradiol. Also, the mortality rate doubles in women aged 35 to 45. Stroke. There is a 2.5x increase in ischemic stroke in women age 20 to 24 who use birth control pills. Again, the risk is directly proportional to the ethinyl estradiol dose. Choose pills that have a lower dose of ethinyl estradiol. The risk increases with age. It also increases when other risk factors, such as cigarette smoking, hypertension and migraine headaches, are present. Myocardial infarction. Eighty percent of myocardial infarctions that occur in women who are on birth control pills occur in women who also smoke cigarettes, with the remainder occurring in oral contraceptive users with other risk factors, such as hypertension or diabetes. Breast cancer. A large World Health Organization metaanalysis looked at more than 53,000 women with breast cancer and more than 100,000 controls. The relative risk of breast cancer was 1.24 in current users of birth control pills
SUPPLEMENT TO SKIN & AGING MARCH 2008 13
F A L L C L I N I C A L D E R M AT O L O G Y C O N F E R E N C E P R O C E E D I N G S
Exhibit area at the Fall Clinical Dermatology Conference.
and the relative risk of cancer that had spread versus remained localized was 0.88. However, those risks are rare.
ORAL CONTRACEPTIVE BENEFITS
There are several protective benefits of birth control pills. These benefits include protection against ovarian cancer, endometrial cancer, pelvic inflammatory disease, uterine leiomyomas, and ovarian cysts and regulation of the menstrual cycle. There is a 40% to 80% overall decreased risk of ovarian cancer in women who take birth control pills. Protection begins after one year of use, increases by 10% to 12% annually, and persists for another 15 to 20 years after the pill is discontinued. Similarly with endometrial cancer, there is up to a 50% decreased risk of endometrial cancer in women who take birth control pills. Again, protection begins after one year, increases with duration of use, and persists for up to 15 years after discontinuation of the medication.
ORAL CONTRACEPTIVE SIDE EFFECTS
Side effects reported with oral contraceptive use include irregular bleeding, nausea, weight gain, mood changes and breast tenderness. No clinical trials confirm that weight gain is a problem with birth control pills. The thought is the ethinyl estradiol causes water retention and associated weight gain. Drospirenone, which has some antimineralocorticoid properties, also has a diuretic effect. Using drospirenone may offset water retention and weight gain. Irregular bleeding is most common in the first 3 months of treatment. Spotting is normal during the first 3 months and does not require stopping treatment or changing the pill. After the third month, it may be necessary to increase the ethinyl estradiol dose and prescribe a different pill. Irregular bleeding is one side effect that worsens with lower ethinyl estradiol doses. Most other side effects improve with lower ethinyl estradiol doses.
history is necessary. Much of the pertinent information already will be readily available in the patients chart, but it may be necessary to spend a few extra moments talking with patients about contraindications. Contraindications include pregnancy; current breast cancer; breast feeding; age over 35 and heavy smoker (more than 15 cigarettes a day); hypertension; diabetes with nephropathy, retinopathy, neuropathy, and vascular disease; deep vein thrombosis, history or current; history of heart disease; history of stroke; and migraine headaches with focal neurological symptoms at any age or without neurological symptoms in patients > 35 years of age. When prescribing oral contraceptives, give patients re a s o nable expectations. Improvement in acne is not expected until the patient has been taking the oral contraceptive for 3 months or longer. Consider combination therapy early in the treatment of acne. Many topical and systemic acne treatments will have a positive impact on acne as early as 4 to 8 weeks. Discuss potential side effects, namely irregular bleeding, and assure the patient that it is not a sign of anything gone wrong if she spots during the first 3 months of treatment. There are several options for starting a birth control pill. One is the Sunday of the next menstrual period. The next is the first day of the next menstrual period. The last option is immediately upon obtaining a negative pregnancy test. Some combination therapies include antibiotics. Antibiotics and birth control pills can be used safely; however, of all the interactions that have been reported, 76% involve rifampin. Rifampin is a potent inducer of cytochrome p450, which increases metabolism of oral contraceptives and other medications. The hypothesis with antibiotic use is antibiotics decrease the gut flora that are needed to further degrade inactive metabolites of the oral contraceptives to active drug during enterohepatic recirculation. This theory has never been substantiated. Two studies in the dermatology literature look at pregnancy rate in women who are on birth control pills and antibiotics. The pregnancy rate was not statistically different between women who were on both versus women who were on a birth control pill alone (1.6% versus 0.96%).
CONCLUSION
Oral contraceptives prescribed effectively, safely and efficiently will greatly impact the quality of life of women with acne.
References
PRESCRIBING ORAL CONTRACEPTIVES FOR ACNE
Prior to prescribing oral contraceptives for acne patients, performing a pelvic exam is not necessary; however, taking a
14 MARCH 200 8 SUPPLEMENT TO SKIN & AGING
1. Hersh EV. Adverse drug interactions in dental practice: interactions involving antibiotics: part II of a series. J Am Dental Assoc. 1999;130(2):236251. 2. London BM, Lookingbill DP. Frequency of pregnancy in acne patients taking oral antibiotics and oral contraceptives. A rch Derm a t o l. 1994;130(3):392393.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- We Don't Eat Our: ClassmatesDokument35 SeitenWe Don't Eat Our: ClassmatesChelle Denise Gumban Huyaban85% (20)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Bob Jones - Science 4Dokument254 SeitenBob Jones - Science 4kage_urufu100% (4)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Alpha Arbutin BrochureDokument4 SeitenAlpha Arbutin BrochureRajesh MevawalaNoch keine Bewertungen
- Olivem 300Dokument11 SeitenOlivem 300Rajesh Mevawala100% (1)
- 14-Caserini Int J Clin Pharmacol Ther 2014Dokument8 Seiten14-Caserini Int J Clin Pharmacol Ther 2014Rajesh MevawalaNoch keine Bewertungen
- Tlimus MOADokument2 SeitenTlimus MOARajesh MevawalaNoch keine Bewertungen
- Swot (Strengths, Weaknesses, Opportunities & Threats) AnalysisDokument16 SeitenSwot (Strengths, Weaknesses, Opportunities & Threats) AnalysisRajesh MevawalaNoch keine Bewertungen
- Basic Selling SkillsDokument71 SeitenBasic Selling SkillsTamara Qaraqe'Noch keine Bewertungen
- DandruffDokument14 SeitenDandruffRajesh MevawalaNoch keine Bewertungen
- Anti Fungal Agents - Mode of Action, Mechanisms of Resistance, and Correlation of These Mechanisms With Bacterial Resistance - GDokument17 SeitenAnti Fungal Agents - Mode of Action, Mechanisms of Resistance, and Correlation of These Mechanisms With Bacterial Resistance - GRajesh MevawalaNoch keine Bewertungen
- How to Identify Urticaria and Treat Autoimmune Chronic CasesDokument13 SeitenHow to Identify Urticaria and Treat Autoimmune Chronic CasesRajesh MevawalaNoch keine Bewertungen
- Longman - New Total English Elementary Video BankDokument26 SeitenLongman - New Total English Elementary Video Bankyuli100% (1)
- Scent of Apples: Does The Author Make Us Think Seriously of Life? Why Do You Say So?Dokument2 SeitenScent of Apples: Does The Author Make Us Think Seriously of Life? Why Do You Say So?carl tom BondiNoch keine Bewertungen
- Hospital Registration Orientation 3 - EQRs With Operating ManualDokument33 SeitenHospital Registration Orientation 3 - EQRs With Operating ManualElshaimaa AbdelfatahNoch keine Bewertungen
- Circumstances Which Aggravate Criminal Liability People vs. Barcela GR No. 208760 April 23, 2014 FactsDokument8 SeitenCircumstances Which Aggravate Criminal Liability People vs. Barcela GR No. 208760 April 23, 2014 FactsJerome ArañezNoch keine Bewertungen
- Why Narcissists Need You To Feel Bad About Yourself - Psychology TodayDokument51 SeitenWhy Narcissists Need You To Feel Bad About Yourself - Psychology Todaytigerlo75Noch keine Bewertungen
- Bhaktisiddhanta Appearance DayDokument5 SeitenBhaktisiddhanta Appearance DaySanjeev NambalateNoch keine Bewertungen
- 2200SRM0724 (04 2005) Us en PDFDokument98 Seiten2200SRM0724 (04 2005) Us en PDFMayerson AlmaoNoch keine Bewertungen
- The Art of Woodworking Shaker FurnitureDokument147 SeitenThe Art of Woodworking Shaker Furnituremalefikus100% (2)
- Life and Works of Jose RizalDokument5 SeitenLife and Works of Jose Rizalnjdc1402Noch keine Bewertungen
- United States Court of Appeals, Sixth CircuitDokument5 SeitenUnited States Court of Appeals, Sixth CircuitScribd Government DocsNoch keine Bewertungen
- Jolly Phonics Teaching Reading and WritingDokument6 SeitenJolly Phonics Teaching Reading and Writingmarcela33j5086100% (1)
- New Democracy June-August 2017Dokument32 SeitenNew Democracy June-August 2017Communist Party of India - Marxist Leninist - New DemocracyNoch keine Bewertungen
- (Cambridge Series in Statistical and Probabilistic Mathematics) Gerhard Tutz, Ludwig-Maximilians-Universität Munchen - Regression For Categorical Data-Cambridge University Press (2012)Dokument574 Seiten(Cambridge Series in Statistical and Probabilistic Mathematics) Gerhard Tutz, Ludwig-Maximilians-Universität Munchen - Regression For Categorical Data-Cambridge University Press (2012)shu100% (2)
- 17 Lagrange's TheoremDokument6 Seiten17 Lagrange's TheoremRomeo Jay PragachaNoch keine Bewertungen
- Cash Flow StatementDokument57 SeitenCash Flow StatementSurabhi GuptaNoch keine Bewertungen
- General Ledger Journal Import ProcessDokument13 SeitenGeneral Ledger Journal Import ProcessMadhavi SinghNoch keine Bewertungen
- ASSIGNMENTDokument5 SeitenASSIGNMENTPanchdev KumarNoch keine Bewertungen
- Ais 301w Resume AssignmentDokument3 SeitenAis 301w Resume Assignmentapi-532849829Noch keine Bewertungen
- Row 1Dokument122 SeitenRow 1abraha gebruNoch keine Bewertungen
- Forms and Types of Business OrganizationDokument2 SeitenForms and Types of Business Organizationjune hetreNoch keine Bewertungen
- BUMANGLAG - CLASS D - JEL PlanDokument3 SeitenBUMANGLAG - CLASS D - JEL PlanMAUREEN BUMANGLAGNoch keine Bewertungen
- Chap 4 eDokument22 SeitenChap 4 eHira AmeenNoch keine Bewertungen
- Banking & Finance Awareness 2016 (Jan-Nov) by AffairsCloudDokument167 SeitenBanking & Finance Awareness 2016 (Jan-Nov) by AffairsCloudkaushikyNoch keine Bewertungen
- APCHG 2019 ProceedingsDokument69 SeitenAPCHG 2019 ProceedingsEnrico SocoNoch keine Bewertungen
- DRF1301 1000V 15A 30MHz MOSFET Push-Pull Hybrid DriverDokument4 SeitenDRF1301 1000V 15A 30MHz MOSFET Push-Pull Hybrid DriverAddy JayaNoch keine Bewertungen
- Hitachi Datasheet Thin Image SnapshotDokument2 SeitenHitachi Datasheet Thin Image Snapshotemail7urangNoch keine Bewertungen
- The Ontological Argument.: A Basic IntroductionDokument12 SeitenThe Ontological Argument.: A Basic IntroductionJas PalNoch keine Bewertungen
- Lecture 15 (91 Slides)Dokument91 SeitenLecture 15 (91 Slides)Hasnain GoharNoch keine Bewertungen