Beruflich Dokumente
Kultur Dokumente
Case Study
Hochgeladen von
Lyndsay Taylor HeatonOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Case Study
Hochgeladen von
Lyndsay Taylor HeatonCopyright:
Verfügbare Formate
A 71 year old white male presented to his primary care physician for a routine checkup.
He had his blood drawn for a workup, and the only complaint he had was of an increase in the frequency of urination. The patient is on several medications, Lisinopril, hydrochlorothiazide, simvastatin, baby aspirin, and a liver cleanse formula. When asked about his past medical history it included hypertension, hyperlipidemia, which is stable, tendonitis gastroesophageal reflux and borderline diabetes. He has had a tonsillectomy and carotid artery surgery. His family history included diabetes, stroke, hypertension, and myocardial infarction. As for the patient's social history, he is married with eight adult children. He does not smoke, He drinks six alcoholic beverages per week and two coffee/sodas per day. He is retired from the flooring installation business and has a lot of exposure to inhaled chemicals. The lab results came back with an increased PSA of 9.25 ( 0-4.0ng/mL Avg 5.0 2xAvg 9.6 ). The patient has had increased PSA in the past, about three years ago, with negative biopsies. His Primary Care Physician referred him to a urologist for follow up. Ten days later the patient had his first appointment with the urologist. A prostate massage was biopsy.
Six weeks after his initial visit with the urologist he presents for a prostate ultrasound and biopsy. The patient had no definitive hypo-echoic areas. The capsule is intact, and the seminal vesicles are normal size, though there were some scattered central and peripheral calcifications. The procedure involved 1
taking 18 biopsies from 7 sites. The Pathology report revealed a prostatic adenocarcinoma with a Gleason score 3+3=6) involving 3% of one core in the right base and focal high-grade prostatic intraepithelial neoplasia was identified in the right mid, left base and left apex. Perineural invasion was also identified in the right base. This refers to the cancer spreading into the space surrounding a nerve. Radiotherapy was discussed with the patient as well as waiting and watching. The patient expressed interest in proceeding with radiotherapy. He was referred to an oncologist. Cancer is a disease in which abnormal cells in the body grow out of control. The prostate is a small, walnut sized structure that makes up part of a man's reproductive system. It is located located just below the bladder and in front of the rectum, it surrounds the urethra. The job of the prostate is to produce fluid that makes up a part of semen. Prostate cancer are cancer cells from the prostate. It is classified as an adenocarinoma, glandular cancer. Early-stage prostate cancer grows slowly, because of this it can take 10 to 30 years before a prostate tumor is large enough to cause symptoms or for doctors to find it. Some of the symptoms that are associated with prostate cancer are Delayed or slowed start of urinary stream, leakage of urine, slow urinary stream, straining when urinating or not being able to empty all urine, blood in the urine or semen, and bone pain or tenderness, this is only when the cancer has spread. Though most of the time these symptoms are caused by other prostate problems that are not cancer. The PSA blood test is done to screen for prostate cancer. Because of this testing, most prostate cancers are found before they can cause any symptoms. 2
This also will be used to monitor your cancer after treatment, this level should begin to rise before there are any symptoms. A Prostate biopsy is the only test that can confirm the diagnosis of prostate cancer. This is where tissue from the prostate is viewed underneath a microscope. Biopsy results are reported using something called a Gleason grade and a Gleason score. The Gleason grade is how aggressive the prostate cancer might be. Grades tumors on a scale of 1-5 based on how different from the normal tissue cells are. Often more than one grade is present in the same sample. The grade is used to make a Gleason score, on a scale of 2-10. This is done by adding the two most prominent grades together. The more increased the score the more likely the cancer is to have spread beyond the prostate gland. 2-4 low grade; 5-7; 8-10 high grade cancer ( poorly differentiated cells). High-grade prostatic intraepithelial neoplasia, HGPIN, is characterized by complex structurally benign glands lined by cells which are similar morphologically to prostate cancer and is generally considered to be a precursor of prostate cancer. Prostate Cancer is the third most common cause of death, from cancer, in men and is the most common in men over the age of 75. It is rarely found in men younger than 40 years old. People who are at higher risk include: AfricanAmerican men, who are also likely to develop cancer at every age, men who are older than 60 and have a father or brother with prostate cancer. Others that are at risk include: Men who are exposed to agent orange, abuse alcohol, eat a diet
high in fat, especially animal fat, who are tire plant workers, painters or farmers or who have been exposed to cadmium. The prognosis varies greatly, and it is affected by whether the cancer has spread outside of the prostate and how abnormal the cancer cells are when diagnosed. Those who have prostate cancer that has not spread, as well as some whose cancer has not spread much outside of the prostate, can be cured. Hormone treatment can extend life for many years for those patients who cannot be cured. Two days later the patient had his first appointment with the Oncologist to discuss treatment options. The treatment option discussed were External beam radiation therapy alone vs external beam radiation therapy plus permanent interstitial seed implant vs radical prostatectomy. Radiation therapy uses high energy radiation to kill the cancer cells by damaging their DNA. Because this can also damage normal healthy cells as well, treatment has to be carefully planned so that side effects are minimized. The radiation that is used for treatment may come from a machine that is outside of the body, or it may come from a radioactive material placed in the body near the tumor cells, or injected into the bloodstream. External-beam radiation therapy is mostly delivered in the form of photon beams, either x-rays or gamma rays. A machine aims the radiation at the cancer and moves around the body which sends radiation from all directions. The exact location of the prostate is mapped and then treatments will be received over time. Generally 5 days a week for 6 to 9 weeks, each of these treatments is about 15 minutes in length and should be painless. Patients usually receive external-beam radiation therapy in
daily treatment sessions over the course of several weeks. The number of sessions depends on many factors, including the total dose of radiation that will be given to the patient. Brachytherapy is a choice for men who have low risk prostate cancer. This is a type of internal radiation therapy where the doctor places radioactive material inside the prostate. There are two kinds, Low dose and High dose. This can be used with external beam radiation therapy. In Low dose rate(LDR) Brachytherapy, a low-dose sources of radiation, or seed implants, are placed throughout the prostate. Each seed is smaller than a grain of rice. The number of seeds depends on the size of the prostate. Each day the radiation will get weaker and it will run out in 2 to 10 months. Once it is gone, the seeds will remain in the prostate. The seeds are implanted as an outpatient procedure. In High dose rate(HDR) Brachytherapy, tiny catheters are placed throughout the prostate. One or more sources of high does radiation will be placed in the catheters for each treatment, then the material will be removed after a few minutes. These catheters will be in the prostate for the entire course of treatment, but will be removed once all treatments have been received. This requires the patient to stay in the hospital or clinic for the entire course of the treatment. Surgery is a choice for men who have early-stage prostate cancer and are in good health. This surgery is called a prostatectomy. There are a few different options for surgery. First is an open prostatectomy, The prostate is removed through a single long cut made in the abdomen, and the lymph nodes can be checked to see if the cancer has spread. This can also be used for nerve-sparing surgery. Second, laparoscopic surgery, in which the doctor uses a laparoscope. This surgery involves several small cuts in the naval and abdomen where the surgery tools are inserted. Nerve-sparing surgery is also an option with this type. Third, is a perineal prostatectomy, this type of surgery is not used very often. It is when the prostate is removed through an incision between the scrotum and anus. The surgeon is
not able to check the lymph nodes and nerve-sparing surgery is harder to do. The patient has decided on external beam radiation therapy plus LDR Brachytherapy. Five days later the patient presented for gold seed fiducial implantation. The seeds were placed initially at left base and apex and then the right and mid-gland. One week after implantation patient presented for stimulation. External beam radiation therapy treatment started two weeks after stimulation for 5 days a week for 43 treatments, about 9 weeks. The patient had blood drawn three weeks after starting treatment. CBC WBC 4.5 (4.1-10.9 K/uL) Lymph 1.0 23.2%L (0.6 4.1 K/uL) 10.0-58.5%L Mid 0.5 10.5%M (0.0- 1.8 K/uL) 0.1- 24.0%M Gran 3.0 66.3%G ( 2.0- 7.8 K/uL) 37.0-92.0%G RBC 4.23 M/uL (4.20 -6.30 M/uL) Hgb 11.5 g/dL (12.0-18.0 g/dL) Hct 36.8 % (37.0-51.0 %) MCV 87.0 fL (80.0-97.0 fL) MCH 27.2 pg (26.0-32.0 pg) MCHC 31.3 g/dL (31.0- 36.0 g/dL) RDW 13.8 % (11.5 -14.5 %) PLT 268 K/uL ( 140-440 K/uL) MPV 9.1 fL (0.0 -99.8 fL) His WBC and RBC are on the lower end of normal and his Hgb and Hct are both just under normal. These results are consistent with someone who is going through radiation therapy. Throughout the treatments the patient was more tired than normal, He had blood drawn again two weeks later and a complete metabolic panel and a lipid panel run. All results were in normal range except for the patients Glucose, which was 204 mg/dL ( 80100mg/dL). Three weeks later the doctor ordered another glucose. Glucose 113 ( 80-100 mg/dL) HBA1c 5.9 ( 4.0-6.9%) est avg glucose 123 mg/dL 6
A week after treatment the patient had another PSA run. The results came back as 2.7 ng/mL ( 0.0-4.0 ng/mL). The patient's PSA was back within normal range. Two months after treatment the patient had another Complete metabolic panel run and all test were in normal range except for the Glucose 112 mg/dL ( 80-100mg/dL). In conclusion,I do not believe the patient's increased glucose is related to the cancer, since it was increased before the patient found out about the cancer, and it was still increased after the treatments ended. The patient's treatment was successful, but he will be watched closely to make sure that it does not come back or spread. This will involve regular checkup's and will include serial PSA tests, every three months.
Das könnte Ihnen auch gefallen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Apr 4Dokument2 SeitenApr 4Rambabu SatipedakalaNoch keine Bewertungen
- Strength and Conditioning Coach or Sports Performance Coach or FDokument3 SeitenStrength and Conditioning Coach or Sports Performance Coach or Fapi-121340325Noch keine Bewertungen
- Advance Directive FormDokument21 SeitenAdvance Directive FormCommunityBridgesNoch keine Bewertungen
- Devarajan, Dss DGN ArdsDokument4 SeitenDevarajan, Dss DGN ArdsrantiadrianiNoch keine Bewertungen
- Holistic VillageDokument5 SeitenHolistic VillagemeghadurganNoch keine Bewertungen
- Revised Sample Scheme of Work and Lesson Plan For Nursing Class (Koya)Dokument6 SeitenRevised Sample Scheme of Work and Lesson Plan For Nursing Class (Koya)NATHANIEL YERINoch keine Bewertungen
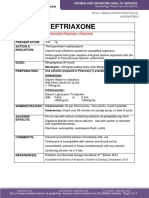
- Ceftriaxone PDFDokument1 SeiteCeftriaxone PDFveniNoch keine Bewertungen
- JST Chang & NylundDokument18 SeitenJST Chang & Nylundab yaNoch keine Bewertungen
- CANINE-Medical Management of Chronic Otitis in DogsDokument11 SeitenCANINE-Medical Management of Chronic Otitis in Dogstaner_soysuren100% (1)
- Discharge Planning ProjectDokument6 SeitenDischarge Planning Projectapi-280998981Noch keine Bewertungen
- Black AdonisDokument4 SeitenBlack Adonisapi-74769985Noch keine Bewertungen
- Problems Related To Abuse or NeglectDokument25 SeitenProblems Related To Abuse or Neglectapi-3797941100% (5)
- Covance ReportDokument8 SeitenCovance ReportkcarnegieNoch keine Bewertungen
- SKINNER: Behavioral Analysis: Characteristics of ScienceDokument5 SeitenSKINNER: Behavioral Analysis: Characteristics of ScienceRustumme Mirelle ReyesNoch keine Bewertungen
- PL3257 Tutorial 5 Emotion RegulationDokument18 SeitenPL3257 Tutorial 5 Emotion RegulationRobin TanNoch keine Bewertungen
- ABRSM Exam TipsDokument10 SeitenABRSM Exam TipsLou Smith100% (1)
- Study: Observational Travelers' DiarrheaDokument5 SeitenStudy: Observational Travelers' DiarrheaFathah MuhammadNoch keine Bewertungen
- Santos, Ivan Jamil S. NCM 112-Or Rle Fear (Pre-Op) Assessment Diagnosis Planning Intervention Rationale Evaluation SubjectiveDokument1 SeiteSantos, Ivan Jamil S. NCM 112-Or Rle Fear (Pre-Op) Assessment Diagnosis Planning Intervention Rationale Evaluation SubjectiveIvan SantosNoch keine Bewertungen
- Bladder Calculus Resulting From The Migration of An IntrauterineDokument8 SeitenBladder Calculus Resulting From The Migration of An IntrauterineFabrien Hein WillemNoch keine Bewertungen
- Protein C & S DeficiencyDokument20 SeitenProtein C & S DeficiencyAhmad Ariff Azmer MunshiNoch keine Bewertungen
- Lesson 12 - Overview of The Wastewater Treatment ProcessDokument6 SeitenLesson 12 - Overview of The Wastewater Treatment ProcessZar ChiNoch keine Bewertungen
- Bahasa Inggris: Taking Vital Sign (Injection)Dokument7 SeitenBahasa Inggris: Taking Vital Sign (Injection)iyal09Noch keine Bewertungen
- Narayana Hrudalaya - Section D Group 7Dokument4 SeitenNarayana Hrudalaya - Section D Group 7Prateek100% (1)
- Soyabean Milk ReportDokument10 SeitenSoyabean Milk Reportprakhalgoyal100% (1)
- Planetary ThreadsDokument2 SeitenPlanetary ThreadsViviana PueblaNoch keine Bewertungen
- Web - The Eight Principles of Diagnosis in Traditional Chinese MedicineDokument8 SeitenWeb - The Eight Principles of Diagnosis in Traditional Chinese MedicineJing CruzNoch keine Bewertungen
- Movement Diagrams - Rayner & Smale PDFDokument6 SeitenMovement Diagrams - Rayner & Smale PDFItai IzhakNoch keine Bewertungen
- Three Tiny Little Points On EarDokument7 SeitenThree Tiny Little Points On Eardineshgomber100% (1)
- EssayDokument2 SeitenEssayFelipe AndinoNoch keine Bewertungen
- Myopia APDF PDFDokument14 SeitenMyopia APDF PDFRao Sab100% (1)