Beruflich Dokumente
Kultur Dokumente
NCP For Dehydration
Hochgeladen von
peter_degamo2000Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
NCP For Dehydration
Hochgeladen von
peter_degamo2000Copyright:
Verfügbare Formate
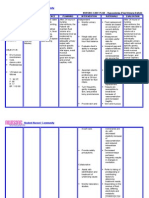
ASSESSMENT
DIAGNOSIS
PLANNING
INTERVENTION
RATIONALE
EVALUATION / OUTCOME Goal met. Patient maintained adequate fluid volume as evidenced by N vital signs, adequate urinary output with normal specific gravity, moist mucous membranes, good skin turgor, and patient s Verbalization that thirst is not excessive.
Subjective Cues: >Patient states, I am very thirsty. Objective Cues: > excessive thirst > dry oral mucous membranes > increased heart rate (HR= 140) > decreased BP (BP= 80/57) > increased body temperature (T= 38) > severe polyuria (>7L/day) > urine specific gravity= 1.001 > decreased skin turgor > weakness > irritability
Fluid Volume Deficit related to excessive urination secondary to diabetes insipidus (A state in which an individual is at risk of experiencing vascular, cellular, or intracellular dehydration due to active or regulatory losses of body water in excess of needs or replacement Capability.)
Within 8 hours, patient will maintain adequate fluid volume as evidenced by: > vital signs within N range for age > urine output of 5080ml/hr > urine specific gravity between 1.004 and 1.030 > moist mucous membranes > good skin turgor > patient verbalizing that thirst is no longer excessive
Independent: Monitored vital signs; noted changes in body Temperature. Observed for postural BP changes; encouraged gradual position changes. Palpated peripheral pulses, assessed capillary refill, mucous membranes, and skin turgor; observed for changes in mental status. Monitored I/O qh; obtained daily weights and compared with 24hr I/O. Encouraged increase in fluid intake and consumption of foods high in fluid content. Turned patient q2h and provided
> Increased HR along with decreased BP and elevated temperature, is present in conditions with fluid Volume deficit. Increased body temperature also increases fluid loss by increasing Metabolism. > Patients with may experience varying degrees of postural hypotension depending on degree of fluid volume deficit. > Excessive fluid loss through regulatory mechanisms failure may result in severe dehydration, circulatory collapse and shock. Decreased cerebral perfusion may result in changes in mentation.
support for body prominences. Provided skin and mouth care, massaged skin, and applied emolients as necessary. Monitored IV flow rates regularly; observed for marked elevations in BP, restlessness, moist cough, dyspnea, basilar crackles, and frothy sputum. Provided health teacings on the need for lifelong hormonal replacement. Dependent: Administered IV fluids as ordered. Administered desmopressin (DDAVP) intanasally as ordered. Collaborative: Monitored laboratory studies such as urine specific
> Fluid replacement needs are based on correction of current deficits and ongoing losses. Decreased urinary output may require aggressive fluid replacement. A sudden weight increase may indicate third-spacing. > Relieves thirst and aids in body fluid replacement. > Patients with fluid volume deficit are more at risk for skin breakdown. > Regular skin and mouth care relieves dryness and discomfort. Light massage promotes circulation. Use of emolients and mild soaps promotes good hygiene and comfort without excessive drying of the skin. > Patients on IV fluid therapy may be at risk for cardiopulmonary
gravity, electrolytes, and blood coagulation studies
compromise. > Lifelong fluid replacement to control polyuria and polydipsia is necessary for patients with Diabetes Insipidus. > Aggressive fluid replacement may be required to correct fluid volume deficit. > Desmopressin is the drug of choice for Diabetes Insipidus. > Other imbalances that require correction may be present with fluid volume deficit
Das könnte Ihnen auch gefallen
- Fluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsDokument17 SeitenFluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsA.Noch keine Bewertungen
- Risk For Infection Related To Inadequate Primary Defenses: Broken SkinDokument2 SeitenRisk For Infection Related To Inadequate Primary Defenses: Broken SkinReylan Garcia100% (8)
- NCP-Deficient Fluid VolumeDokument1 SeiteNCP-Deficient Fluid Volumejanmichael8Noch keine Bewertungen
- NCP Risk For Fluid Volume DeficitDokument3 SeitenNCP Risk For Fluid Volume DeficitAtheena Diaz50% (4)
- Impaired Tissue Integrity Nursing Care PlanDokument2 SeitenImpaired Tissue Integrity Nursing Care PlanLynnette Adams Mayotte95% (20)
- Fluid and ElectrolytesDokument179 SeitenFluid and ElectrolytesTrixie Al Marie75% (4)
- NCP3 Skin IntegrityDokument3 SeitenNCP3 Skin IntegritySheng Arquiza67% (3)
- Deficient Fluid Volume (AGEDokument2 SeitenDeficient Fluid Volume (AGENursesLabs.com83% (6)
- (NCP) Deficient Fluid Volume - HypovolemiaDokument3 Seiten(NCP) Deficient Fluid Volume - HypovolemiaMacaRonie PepeRownie del Rio100% (4)
- Nursing Care Plans for Deficient Fluid VolumeDokument6 SeitenNursing Care Plans for Deficient Fluid VolumeLalaine RomeroNoch keine Bewertungen
- Risk For Deficient Fluid Volume Best NCPDokument2 SeitenRisk For Deficient Fluid Volume Best NCPAlbean DelojeroNoch keine Bewertungen
- NCP DehydrationDokument4 SeitenNCP DehydrationYnah Sayoc100% (2)
- Nursing Care Plan for Diabetes Mellitus Fluid Volume DeficitDokument5 SeitenNursing Care Plan for Diabetes Mellitus Fluid Volume DeficitAnnisa Silvera II50% (2)
- Diarrhea NCPDokument2 SeitenDiarrhea NCPNoriel FabrosNoch keine Bewertungen
- Fluid Volume DeficitDokument12 SeitenFluid Volume DeficitKersee GailNoch keine Bewertungen
- Provide Ensuresbedside comfort,commode as privacy andneeded. convenience for patientDokument4 SeitenProvide Ensuresbedside comfort,commode as privacy andneeded. convenience for patientImang Dela Cruz100% (9)
- Deficient Fluid Volume - Nursing Diagnosis & Care PlanDokument9 SeitenDeficient Fluid Volume - Nursing Diagnosis & Care PlanEricsonMitraNoch keine Bewertungen
- NCP - Fluid Volume DeficitDokument2 SeitenNCP - Fluid Volume DeficitMarielle Osalvo83% (59)
- NURSING CARE PLAN On Impaired Skin IntegrityDokument2 SeitenNURSING CARE PLAN On Impaired Skin Integrityapi-371817493% (30)
- Fluid Imbalance (NCP)Dokument9 SeitenFluid Imbalance (NCP)Putry RainismNoch keine Bewertungen
- NCP Fluid Volume DeficitDokument2 SeitenNCP Fluid Volume DeficitRez Apego0% (1)
- NCP-Risk For Fluid Volume DeficitDokument3 SeitenNCP-Risk For Fluid Volume DeficitJai Go100% (1)
- Risk For Deficient Fluid Volume Best NCPDokument2 SeitenRisk For Deficient Fluid Volume Best NCPMikko Anthony Pingol Alarcon83% (46)
- NCP For Deficient Fluid VolumeDokument2 SeitenNCP For Deficient Fluid VolumeRedwing_Dc_854758% (12)
- Dengue Fever Nursing Care Plan-High Risk For Fluid Volume DeficitDokument1 SeiteDengue Fever Nursing Care Plan-High Risk For Fluid Volume Deficitemman_abz100% (5)
- NCP Deficient Fluid Volume Related To Fluid Loss DHNDokument2 SeitenNCP Deficient Fluid Volume Related To Fluid Loss DHNMa. Elaine Carla Tating38% (8)
- NCP. Deficient Fluid Volume by Eben D.C.Dokument1 SeiteNCP. Deficient Fluid Volume by Eben D.C.dominoredwing2024100% (1)
- Assess and Care for Impaired Oral Mucous MembranesDokument2 SeitenAssess and Care for Impaired Oral Mucous MembranesNolan Cabral100% (1)
- Risk For Deficient Fluid Volume - NCPDokument2 SeitenRisk For Deficient Fluid Volume - NCPAyla Mar100% (1)
- Nursing Care Plan Cues Diagnosis Justification: Sodium-132 Mmol/l (Low)Dokument3 SeitenNursing Care Plan Cues Diagnosis Justification: Sodium-132 Mmol/l (Low)rei_alina75% (4)
- NCP-Acute Gastroenteritis PediatricDokument11 SeitenNCP-Acute Gastroenteritis PediatricJhoevina Dulce Capicio0% (1)
- Ineffective Tissue PerfusionDokument1 SeiteIneffective Tissue PerfusionRhae RaynogNoch keine Bewertungen
- Nursing Care Plan for Fluid Volume DeficitDokument2 SeitenNursing Care Plan for Fluid Volume DeficitXtinego89% (9)
- NCP Risk For Fluid Volume DeficitDokument2 SeitenNCP Risk For Fluid Volume DeficitJeanineReyes44% (9)
- 5 Nursing Diagnosis For GlomerulonephritisDokument2 Seiten5 Nursing Diagnosis For GlomerulonephritisGeorich Narciso67% (3)
- NCP (Diarrhea)Dokument2 SeitenNCP (Diarrhea)Rodj Bilang Jr.83% (30)
- NCP-Fluid Volume DeficitDokument2 SeitenNCP-Fluid Volume Deficitanon_207994234100% (1)
- NCP-Fluid Volume DeficitDokument2 SeitenNCP-Fluid Volume Deficitjava_biscocho122979% (33)
- SAMPLE NCP For Diabetes InsipidusDokument3 SeitenSAMPLE NCP For Diabetes InsipidusClancy Anne Garcia Naval50% (2)
- Imbalanced NutritionDokument3 SeitenImbalanced NutritionKM100% (6)
- Fluid Volume Deficit Related To Loose Watery Stool Diarrhea)Dokument2 SeitenFluid Volume Deficit Related To Loose Watery Stool Diarrhea)Jesse James Advincula Edjec100% (15)
- Risk For DehydrationDokument2 SeitenRisk For DehydrationJahne CM80% (5)
- Risk For Impaired Skin Integrity and Readiness For Enhanced PowerDokument3 SeitenRisk For Impaired Skin Integrity and Readiness For Enhanced PowerdanaNoch keine Bewertungen
- NCP StressDokument2 SeitenNCP StressWaqas Javed100% (7)
- NCP For DehydrationDokument1 SeiteNCP For Dehydrationjxhel63% (8)
- Fluid Volume Deficient Patient with Diabetes MellitusDokument2 SeitenFluid Volume Deficient Patient with Diabetes MellitusMarlon AnryNoch keine Bewertungen
- Short Term: Independent: Independent: Short TermDokument2 SeitenShort Term: Independent: Independent: Short TermAndre ImperialNoch keine Bewertungen
- Fluid Volume DeficitDokument3 SeitenFluid Volume Deficitprickybiik100% (1)
- Nursing Care Plan AGNDokument2 SeitenNursing Care Plan AGNAlexis Coronado50% (2)
- Ncp.-Fluid Volume DeficitDokument1 SeiteNcp.-Fluid Volume DeficitAdia Cavrinni De JesusNoch keine Bewertungen
- Hypertonic SolutionsDokument4 SeitenHypertonic SolutionsVanessa PaguiriganNoch keine Bewertungen
- Deficit)Dokument2 SeitenDeficit)Lee DeeNoch keine Bewertungen
- NCP RiskDokument3 SeitenNCP RiskMaricar Azolae MascualNoch keine Bewertungen
- NCP (Deficient Fluid VolumeDokument3 SeitenNCP (Deficient Fluid VolumeNica RespondoNoch keine Bewertungen
- Nursing DiagnosisDokument4 SeitenNursing DiagnosisMavy AndresNoch keine Bewertungen
- 3 Hydration Related ConditionDokument3 Seiten3 Hydration Related ConditionCzeremar ChanNoch keine Bewertungen
- Assessment Diagnosis Scientific Explanation Goal Intervention Rationale Expected Outcome SubjectiveDokument4 SeitenAssessment Diagnosis Scientific Explanation Goal Intervention Rationale Expected Outcome SubjectiveKeith MirasolNoch keine Bewertungen
- Deficient Fluid VolumeDokument1 SeiteDeficient Fluid VolumeSheila ErpeloNoch keine Bewertungen
- AssessmentDokument2 SeitenAssessmentWajiha Esmula TiuNoch keine Bewertungen
- Nursing Diagnosis Objectives Nursing Interventions Rationale EvaluationDokument9 SeitenNursing Diagnosis Objectives Nursing Interventions Rationale EvaluationJezza Sanchez-Rellita VillariasNoch keine Bewertungen
- NVIDIA Display Driver For Windows 2000/XP Version 185.85, 04/30/2009Dokument2 SeitenNVIDIA Display Driver For Windows 2000/XP Version 185.85, 04/30/2009zezentNoch keine Bewertungen
- Nursing Care Plan For Ineffective Airway ClearanceDokument7 SeitenNursing Care Plan For Ineffective Airway Clearancepeter_degamo20000% (1)
- A Prevalence Study of Xerophthalmia in The Philippines: Implications For Supplementation StrategiesDokument2 SeitenA Prevalence Study of Xerophthalmia in The Philippines: Implications For Supplementation Strategiespeter_degamo2000Noch keine Bewertungen
- BiochemistryDokument2 SeitenBiochemistrypeter_degamo2000Noch keine Bewertungen