Beruflich Dokumente
Kultur Dokumente
A A A A A A A A A A A A A A A A A A A A A A A A A A
Hochgeladen von
johannalomuljoOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
A A A A A A A A A A A A A A A A A A A A A A A A A A
Hochgeladen von
johannalomuljoCopyright:
Verfügbare Formate
General Information Patient CG, 60/F, from Las Pinas City, single, and is currently working as a househelper.
Chief Complaint: Breast mass on the right upper quadrant of the right breast History of Present Illness: The patient was apparently well until 14 months PTC when she experienced localized pain on the right upper quadrant of the right breast which she described as parangtinutusokngkarayom , with a pain score of 10/10, sponstaneous on onset, no aggravating factors, and alleviated by massaging the area. She said that she experienced this pain around 2-3 times per week. Around 11 months PTC, the patient was able to palpate a mass on the right upper quadrant of the right breast about the size of a corn kernel . She still experiences the pain around this time. The patient did nothing for the breast pain and breast mass. Four months PTC, the patient noticed an increased in size of the mass from a corn kernel to the size of a bean and she still experienced the breast pain. She consulted a district hospital and underwent core needle biopsy. The results said that the mass is an Invasive Ductal Carcinoma, not otherwise specified, well-differentiated (Nothingham histologic grade 4). The patient was advised surgery but opted for a second opinion from another hospital. Three months PTC, the patient went to the Philippine General Hospital to seek second opinion for the breast pain and breast mass which she was still experiencing. The patient was advised to undergo several diagnostic tests before going back to the physician. Bone scintigraphy(PGH) revealed a Breast CA stage III B, with degenerative changes but no bone metastasis. Chest X-Ray (PGH) revealed calcified densities around the aortic knob, aorta was torturous, spurs were seen in the lateral aspect of the vertebral endplates, and slight left curvature of the thoracic spine. Two months PTC, the patient had a mammogram (PGH) and results indicated the presence of fibroglandular tissue, and lobulated nodular density with speculated borders measuring 2.5 x 2.7 x 2.3 cm (CC x W x AP). Another biopsy (PGH) was done and results showed that there was Invasive Ductal Carcinoma, Breast (Right). One month PTC, patient went back to the physician in PGH and was advised to undergo surgery. However, due to the lack of available bed in the hospital, she was told that she will be informed for any vacancy which will allow the operation to push through. Two days PTC, the patient was informed by the physician via text message to immediately go to PGH for there was a bed vacancy. She immediately complied with the physician and hospital admission was done. Course in the Wards The patient underwent several blood extractions in preparation for surgery. Her operation is scheduled on Thursday or Friday this week. ROS (+) colds (+) blurring of vision (+) hip and knee joint pain (relieved by medicol) (-) constipation (-) headache (-) nocturia (-) weight loss (-) cough (-) difficulty of breathing (-) orthopnea (-) PND (-) abdominal pain (-) changes in urine and bowel movement (urination-5/day, colorless; defecation 1-2/daydark brown)
PMHx (+) hypertension (currently on amlodipine 5mg OD) (+) cyst on the dorsal left wrist (-) DM, CA (Unconfirmed PTB) dumurangdugo, took medications for 1 month, x-ray negative FMHx (Unconfirmed) DM, Hypertension, Asthma, PTB (+) breast mass (aunt mother s side) (+) cervical lymphadenopathy (mother) Maternal/Menstrual Hx The patient is single with no children. She had a sexual partner when she was 42 or 45 yo. which lasted for a year. They used no protection during intercourse. Patient had her menarche when she was 15yo. She experienced irregular menses until she was 20; from then on, her menses were regular, lasting for 34 days, consuming 10 napkins for the entire duration of menstruation. Patient had her menopause when she was 49yo. PSHx (+) Alcohol intake (social drinker) (-) Smoking (-) Illicit drugs Diet (vegetables, firsh and meat) Hobbies (gardening, watching TV) The patient is currently living with herpamangkin, amo, misisniamo and 2 children niamo. ROS (+) colds (+) blurring of vision (+) hip and knee joint pain (relieved by medicol) (-) constipation (-) headache (-) nocturia (-) weight loss (-) cough (-) difficulty of breathing (-) orthopnea (-) PND (-) abdominal pain (-) changes in urine and bowel movement (urination-5/day, colorless; defecation 1-2/daydark brown)
PMHx (+) hypertension (currently on amlodipine 5mg OD) (+) cyst on the dorsal left wrist (-) DM, CA (Unconfirmed PTB) dumurangdugo, took medications for 1 month, x-ray negative FMHx (Unconfirmed) DM, Hypertension, Asthma, PTB (+) breast mass (aunt mother s side) (+) cervical lymphadenopathy (mother) Maternal/Menstrual Hx The patient is single with no children. She had a sexual partner when she was 42 or 45 yo. which lasted for a year. They used no protection during intercourse. Patient had her menarche when she was 15yo. She experienced irregular menses until she was 20; from then on, her menses were regular, lasting for 34 days, consuming 10 napkins for the entire duration of menstruation. Patient had her menopause when she was 49yo. PSHx (+) Alcohol intake (social drinker) (-) Smoking (-) Illicit drugs Diet (vegetables, firsh and meat) Hobbies (gardening, watching TV) The patient is currently living with herpamangkin, amo, misisniamo and 2 children niamo.
Vital Signs BP Temp PR HR RR 140/90 36.4C 80 80 18
Dermatologic Exam Skin Good skin turgor, warm to touch Hair Normal distribution (-) alopecia Nails Pink nail beds
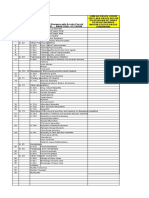
(-) clubbing, deformities Musculoskeletal Screening (-) muscle and joint pains (-) difficulty in dressing up (-) difficulty in climbing stairs Inspection Normal gait; normal posture and arm swing; normal turn Spine midline; normal curvatures (-) muscle wasting (-) atrophy, edema, deformities, inflammation Palpation (-) Warm and tender joints (-) pain upon palpation (-) crepitus (-) stiffness Range of motion Full range of motion of all extremities Muscle strength 5/5 for all extremities Breast Examination Inspection (+) nipple retraction (-) edema Symmetrical breast When arms were raised, the right breast was higher than the left (skin retraction) Palpation (+) solitary, hard, movable, well-circumscribed with irregular border, tender mass measuring 7 x 5 cm in the middle of the right breast (+) 1 cm mid-axillary lymph node, firm, movable (Level I axillary lymph node) Diagram: (small circle lymph node; oblong breast mass)
HEENT examination
Head Normocephalic skull, normal hair distribution with average texture Eyes Pink conjunctiva, anicteric sclerae, (-) ptosis, (+) bilateral pericorneal opacity Ears Normal external contours of the ear, (-) otitis externa Nose Septum midline, mucosa and turbinates cannot be visualized due to lack of speculum, no sinus tenderness Throat Lips pink, oral mucosa pink, ulcers, masses, exudates Neck Supple neck, (-) masses, (-) CLAD, trachea midline, (-) thyroid enlargement, tenderness nor masses Neurologic examination Mental Status Alert, responds to verbal and tactile stimuli, appropriate affect and behavior; oriented to time, place, and person; intact attention, remote and recent memory, and new learning ability Cranial nerve examination Cranial Nerves CN I CN II CN III CN IV CN V CN VI CN VII CN VIII CN IX & X CN XI CN XII Findings Normal perception of scent for each nostril. VA OD 20/50 - 1 OS 20/50 - 1 Normal Visual Fields (+) ROR, orange retinal background (-) Bilateral hemorrhages, (-) neovascularisation Right: AV ratio is 2:3 3mm pupillary size Normal EOM movements Normal direct and consensual pupillary reflex
Intact superior oblique Sensory: Symmetrical reaction to pain and light touch Motor: Equal bilateral strength of muscles for mastication Intact lateral rectus Symmetrical facial muscle movement Screening: Intact Weber test: lateralizes to the right Rinne test: AC>BC for both ears Normal Swallowing Midline Uvula Intact elevation of soft palate (+) Gag reflex (-) atrophy of trapezius and sternocleidomastoid Symmetrical shoulder shrug (-) Tongue deviation, symmetrical muscle bulk (-) atrophy Sensory Tests No sensory deficits for light touch and pain, except for pain sensation of C6 on the right (80%) less than the left (100%). Reflexes Noted decrease reflexes on the right (-) Babinski reflex Inspection Abdomen is flat without visible masses A concavity was noted at the junction of the last rib and LUQ No bulging flanks No visible peristalsis and pulsations No scars, striae, or dilated veins Auscultation Bowel sounds were hypoactive in all quadrants Percussion Tympanitic in all quadrants Liver span = 8cm Intact Traube s space Palpation Light Palpation No masses were palpated Pain was not elicited Deep Palpation No masses were palpated Pain was not elicited No rebound tenderness Spleen was palpable Special Tests Negative fluid shift test was not performed No pain on kidney punch Cardio Exam Inspection
HR=68 adynamic precordium
Palpation
Auscultation
2 round circular erythematous patches with central clearing accompanied with pruritus No heaves, thrills and tenderness Apex beat not displaced and coincides with PMI solitary mass on left breast (refer to derma) Regular rate and rhythm with no skipped beats No murmurs and extra heart sounds S2 loud at the 2nd ICS left and right parasternal border S1 same intensity as S2 (relatively decreased S1) in the tricuspid and mitral area
Pulmo Exam Inspection
Palpation Auscultation
Percussion
Equal Chest expansion normal chest shape trachea midline not in respiratory distress no use of accessory muscles for breathing No masses, nodules and tenderness equal tactile fremiti on both lung fields Clear bronchovesicular breath sounds no adventitious sounds equal vocal fremiti on both lung fields no bronchophony, egophony and whispered petriloquey Equally resonant lungs on percussion
Vascular Exam CVP: 3cm water JVP: 8 cm water Full regular and equal bouncing pulses on both upper and lower extremities
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Human Eye PowerPointDokument69 SeitenThe Human Eye PowerPointKemoy Francis100% (1)
- DSM 5 - DSM 5Dokument7 SeitenDSM 5 - DSM 5Roxana ClsNoch keine Bewertungen
- Hypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumDokument5 SeitenHypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumMelodia Turqueza GandezaNoch keine Bewertungen
- Musculoskeletal System (20000 Series) : A) 20205 B) 20206 C) 20225 D) 27324Dokument8 SeitenMusculoskeletal System (20000 Series) : A) 20205 B) 20206 C) 20225 D) 27324JJKNoch keine Bewertungen
- Classic Radiology SignsDokument9 SeitenClassic Radiology SignsJui DirDapNoch keine Bewertungen
- Steliarova Foucher - Et - Al 2005 CancerDokument11 SeitenSteliarova Foucher - Et - Al 2005 CancerNur Melani Sari WardaniNoch keine Bewertungen
- Small Animal Surgery Internship - Proposed Program Description (2021)Dokument4 SeitenSmall Animal Surgery Internship - Proposed Program Description (2021)Shubham HarishNoch keine Bewertungen
- Depression in Older AdultsDokument9 SeitenDepression in Older Adultsapi-509881562Noch keine Bewertungen
- Benefits of HijamaDokument3 SeitenBenefits of HijamaBateria MeaNoch keine Bewertungen
- A Review of Selected Systemic Antifungal Drugs For Use in Dogs and CatsDokument2 SeitenA Review of Selected Systemic Antifungal Drugs For Use in Dogs and CatsannygiacoNoch keine Bewertungen
- Australian Dental Journal - 2015 - Ettinger - Treatment Planning Concepts For The Ageing PatientDokument15 SeitenAustralian Dental Journal - 2015 - Ettinger - Treatment Planning Concepts For The Ageing PatientLorri - Ann LamontNoch keine Bewertungen
- Guillain - Barre SyndromeDokument1 SeiteGuillain - Barre SyndromeGrant Kenneth Dumo AmigableNoch keine Bewertungen
- DERMA SPMC LeprosyDokument9 SeitenDERMA SPMC LeprosyNicole Alexandra KhoNoch keine Bewertungen
- KC Basic English 2021Dokument11 SeitenKC Basic English 2021ShafanaiNoch keine Bewertungen
- Substance Use Disorder Fact SheetDokument2 SeitenSubstance Use Disorder Fact Sheetrandey92Noch keine Bewertungen
- Research Project ProposalDokument8 SeitenResearch Project ProposalAthena Irish LastimosaNoch keine Bewertungen
- Restrospective Study Inguinal HerniaDokument6 SeitenRestrospective Study Inguinal HerniaDaniela VidalNoch keine Bewertungen
- Analise Dinamica Sorriso - Mudanças Com A IdadeDokument2 SeitenAnalise Dinamica Sorriso - Mudanças Com A IdadeCatia Sofia A PNoch keine Bewertungen
- Cerebrovit X-CelDokument36 SeitenCerebrovit X-CelzuzuzazaziziNoch keine Bewertungen
- ExamView - Chapter - 33 PDFDokument8 SeitenExamView - Chapter - 33 PDFChizua OkoyeNoch keine Bewertungen
- Sebina CM CVDokument3 SeitenSebina CM CVShabna CmNoch keine Bewertungen
- Performance Task #111 & 2 EappDokument3 SeitenPerformance Task #111 & 2 EappEricka Rivera SantosNoch keine Bewertungen
- Conjunctivitis A Systematic Review of Diagnosis and TreatmentDokument18 SeitenConjunctivitis A Systematic Review of Diagnosis and TreatmentdasityarachmanNoch keine Bewertungen
- Twin Block Case ReportDokument5 SeitenTwin Block Case ReportwjeelaniNoch keine Bewertungen
- Azas-Azas Umum Toksikologi (Nasib Racun Dalam Tubuh)Dokument27 SeitenAzas-Azas Umum Toksikologi (Nasib Racun Dalam Tubuh)Nitasolikhah0703Noch keine Bewertungen
- Acute Gastrointestinal HemorrhageDokument21 SeitenAcute Gastrointestinal HemorrhageWarthinNoch keine Bewertungen
- 14 Factitious Disorders and MalingeringDokument13 Seiten14 Factitious Disorders and Malingeringkrysdana22100% (1)
- Pharmacology of Phenadoxone dN-Morpholino 4:4 Diphenyl: HydrochlorideDokument17 SeitenPharmacology of Phenadoxone dN-Morpholino 4:4 Diphenyl: Hydrochlorideisaev201Noch keine Bewertungen
- Icd-10 Oktober 2021Dokument9 SeitenIcd-10 Oktober 2021Nia KurniawatiNoch keine Bewertungen
- Pregnancy Induced HypertensionDokument67 SeitenPregnancy Induced HypertensionTrisha OrtegaNoch keine Bewertungen