Beruflich Dokumente
Kultur Dokumente
Camfil Tech
Hochgeladen von
leong2007Originalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Camfil Tech
Hochgeladen von
leong2007Copyright:
Verfügbare Formate
Technology & Services
Nosocomial Infections and Air Filtration in Operating Theatre Suites Application of French Standard NFS90-351:2003
a report by
Fabrice Dorchies
Corporate Product Manager Clean Concept, Camfil Farr
The Problem
The incidence of nosocomial infections in the hospital environment ranges from 5% to 8%. It is estimated that almost 20% of these infections are contracted in an operating theatre suite with possible irreversible consequences for patients. According to the etymological meaning of the word (nosos illness and komein treat), the term nosocomial is used to describe infections contracted following treatment. When this type of infection is diagnosed, therefore, cause and responsibility rest with the healthcare facility. The media give regular reminders of this issue, e.g., the sports clinic scandal. The increasing involvement of the public should also be noted, who not only increasingly demand more transparency, but also wish to understand how the health system works. At the same time, they are less willing to accept risk, which they cannot control, or have not chosen. Against this backdrop of public pressure and increased public awareness, healthcare professionals are justified in paying ever-closer attention to nosocomial infections. Each year in France, 60,000 to 100,000 patients admitted to hospital contract nosocomial infections, which corresponds to a prevalence in the range of 6% to 10%. Five thousand to 10,000 people die of the infections. In terms of public health, these figures are as alarming as the statistics for road-traffic accidents (7,800 deaths in 2002). To this picture must also be added the aspect of cost for the healthcare structures and, therefore, for the local authorities nosocomial infections extend not only the list of treatments to be provided but also the length of stay in hospital. Faced with this issue, many European countries are currently drawing up documents intended to standardise the most reliable solutions. The recent French standard, NF S90-351:2003, relative to clean rooms and similar controlled environments in healthcare facilities, provides
recommendations for the development of the project, as well as the construction and maintenance of air-treatment facilities. For its part, Spain has also adopted a new standard UNE 100713:2003: air conditioning in hospitals with the same objectives. In the UK, hospital air conditioning is now under scrutiny from the Association of Local Authority Risk Managers (ALARM) the UK national forum for risk management in the public sector. This body has stated that failing to manage the risks associated with heating and ventilation systems in premises, particularly hospitals, could have catastrophic results. Their view is that failure to control or minimise exposure to dust fumes, airborne contaminants and bacteria could leave anyone in the building at risk of developing a range of illnesses. The containment of the risk of Legionella has now been coupled with increased emphasis on the containment of methicillin resistant stephalococcus aureus (MRSA) and all hospital-acquired infections. Although cleanliness programmes are often aimed at contact spread, airborne spread is now being treated increasingly seriously and appropriate filter systems, particularly for recirculated air flows, are fundamental to the hospitals infection control team. Camfil offer consultative advice to prioritise the fitting of correct filter systems and on-going advice on hygienically focused preventative maintenance. The emphasis is placed on the air handling unit (AHU) section and the operating theatre suite.
Filters Compliant with European Standards
The EN 779:2002 Standard
This standard deals with air filters used to trap particles in the general ventilation system. It includes a protocol for evaluating their gravimetric efficiency so that filters can be classified and compared. In particular, this standard enables evaluation of the filters capacity for the filtration
BUSINESS BRIEFING: HOSPITAL ENGINEERING & FACILITIES MANAGEMENT 2005
Technology & Services
of fine particles (0.3m to 3m) and to assess its dust-holding capacity. It applies only to filters with an initial efficiency of less than 98% for particles of 0.4m.
The EN 1822-1 to 5 Standard
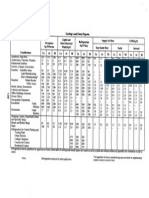
Table 1
Pr P 1 2 3 4
Part 1 of this standard supplements the previous standard, as it specifies a method for the classification of high efficiency particulate air (HEPA) filters and ultra-low penetration air (ULPA) filters. Part 2 concentrates on describing the measurement methods and instruments. Parts 3, 4 and 5 describe the testing systems.
The EN-ISO 14698-1/2 Standard (March 2004)
1 2 3 4
1 2 3 4
2 4 6 8
3 6 9 12
4 8 12 16
Pr = risk factor associated with the procedure P = risk factor associated with the patient Score of 1216: zone 4 (very high risk zone); score of 69: zone 3 (high risk zone); score of 24: zone 2 (moderate risk zone); score of 1: zone 1 (low risk zone).
With regards to the methods of use, the standard focuses on the air flow systems for the area to be protected (unidirectional or non-unidirectional flow), the air exchange rate in the room and the decontaminable aspects of the exposed materials. The following types of operating theatre suites are normally classified as level 4 risk areas traumatology, ophthalmology (OPH), major burns, cardiovascular surgery and neurosurgery, etc. The procedures carried out in these operating theatre suites combine the risk factors associated with the procedure (duration and complexity of the procedures, etc.) and the risk factors associated with the state of the patients health (age, effectiveness of the antibiotic therapy and immunedeficient condition, etc.).
Level 4 Risk Areas
The scope of this future standard will cover the biocontamination control of clean room air. Furthermore, this standard introduces the idea of risk assessment.
The ISO 14644-1 to 4 Standards (Classification Index X44-101 to 104)
Although not specific to the healthcare environment, the classification system proposed by this standard means that the clients requirements and aims can be incorporated. This dimension can prove to be a determining factor in the design, operation and construction of clean rooms in a hospital environment.
Industrial Analysis and Know-how
According to NFS90-351, level 4 risk areas must fulfil the following criteria: minimum filtration chain F6 (AHU input), F7 (AHU outlet) and H13 (ceiling diffusion); ISO 5 particulate classification (ISO 14644-1); CP10 particulate decontamination kinetic classification; target bacteriological classification B10; use of easily decontaminable materials; unidirectional flow; and air exchange rate of the room > 50vol/h.
2 Types 1A /1B
The contamination control requirements vary in healthcare facilities according to the medical procedures carried out and the areas allocated to these activities. In response to these requirements, the NF S90-351 standard points out the need to initially conduct a risk assessment to define the particulate cleanliness classification appropriate to the specific needs of each area. Two factors determine the infection risk in an operating site. The first concerns the surgical procedure itself, the other the patients state of health. The combination of these two factors determines the biocontamination risk specific to the procedure (see Table 1). Having completed this procedure, the required performance efficiency for the facility can then be analysed and the most appropriate equipment selected in line with the surgical procedures carried out. From risk 4 (the highest) to risk 1 (non-specific areas), each risk area will be classified and linked with a target technical efficiency level.
Rooms for operating theatre suites (according to UNE100713:2003) must fulfil the following criteria: three-stages of filtration, (F6 and F9) in AHU and H13/h14 (ceiling diffusion); filters F6 and F9, according En 779; filters H13 according EN 1822; two types of air flow for classes 1, A or B; type 1A unidirectional flow; type 1B unidirectional flow or nonunidirectional flow;
BUSINESS BRIEFING: HOSPITAL ENGINEERING & FACILITIES MANAGEMENT 2005
Nosocomial Infections and Air Filtration in Operating Theatre Suites
air exchange rate of the room > 30vol/h; 100% fresh air; and roomside access for filters controls.
The Solutions
Figure 1
With a view to providing a point-by-point response to this new standard as regards to level 4 risk areas (and/or 3), Camfil has developed a unidirectional flow filtration ceiling, the CamHOSP Screentek finish. As a result of Camfils 40 years of experience and knowledge of the hospital environment, their engineering department has concentrated on: frequent replacement). swift implementation with guaranteed results (class B seal, according to EN 1886, EN-1822and En779:2002-certified filters); reduced maintenance costs through the use of universal mechanical seal filters, providing the operator with a guarantee that filters can be replaced very easily and independently (unlike gel-seal filters, which are not suitable for This system is particularly suitable for hospitals, as it allows frequent and efficient cleaning and disinfection; The CamHOSP complies perfectly with Appendix D paragraph 1.2 of standard NF S90-35, as it is free of surface unevenness and porosity that could promote the retention of particulate and chemical contam-ination or the development of micro-biological contamination.
BUSINESS BRIEFING: HOSPITAL ENGINEERING & FACILITIES MANAGEMENT 2005
Das könnte Ihnen auch gefallen
- Taman EquineDokument2 SeitenTaman Equineleong2007Noch keine Bewertungen
- BeSS Bank Calorie, Bahagian Pemakanan: KKMDokument107 SeitenBeSS Bank Calorie, Bahagian Pemakanan: KKMnazrinirfan037217Noch keine Bewertungen
- Eat HealtyDokument1 SeiteEat Healtyleong2007Noch keine Bewertungen
- IC Nos. Distance GL IL D Gradient M M M M IC-1 7.1 5.90 1.20 20 1:80 IC-2 7.1 5.65 1.45 5.1 1:80 IC-3 7.1 5.59 1.51 20 1:80 IC-4 7.1 5.34 1.76 20 1:80 IC-5 7.1 5.09 2.01 13 1:80 Mh4 - Pil 4.92Dokument2 SeitenIC Nos. Distance GL IL D Gradient M M M M IC-1 7.1 5.90 1.20 20 1:80 IC-2 7.1 5.65 1.45 5.1 1:80 IC-3 7.1 5.59 1.51 20 1:80 IC-4 7.1 5.34 1.76 20 1:80 IC-5 7.1 5.09 2.01 13 1:80 Mh4 - Pil 4.92leong2007Noch keine Bewertungen
- ReadmeDokument1 SeiteReadmeluantinh10985Noch keine Bewertungen
- SCAE MT 4040 Traffic Light Controller Spare PartsDokument3 SeitenSCAE MT 4040 Traffic Light Controller Spare Partsleong2007Noch keine Bewertungen
- Tender BQ Color PDFDokument1 SeiteTender BQ Color PDFleong2007Noch keine Bewertungen
- PicturesDokument2 SeitenPicturesleong2007Noch keine Bewertungen
- Total Price RM 391,005.45: Acre SQFT RM RM/SQFT 1 43,560.00 75,000.00 1.72Dokument1 SeiteTotal Price RM 391,005.45: Acre SQFT RM RM/SQFT 1 43,560.00 75,000.00 1.72leong2007Noch keine Bewertungen
- Schedule of Internal Manhole DetailsDokument3 SeitenSchedule of Internal Manhole Detailsleong2007Noch keine Bewertungen
- Floor Floor Area m2 Gallon Ground 57 10 570 125.4 1st 68 10 680 149.6 2nd 68 10 680 149.6Dokument1 SeiteFloor Floor Area m2 Gallon Ground 57 10 570 125.4 1st 68 10 680 149.6 2nd 68 10 680 149.6leong2007Noch keine Bewertungen
- Green Building Guide Water Efficiency TipsDokument8 SeitenGreen Building Guide Water Efficiency Tipsleong2007Noch keine Bewertungen
- APN Series PDFDokument1 SeiteAPN Series PDFleong2007Noch keine Bewertungen
- CoolingLoadCheck PDFDokument1 SeiteCoolingLoadCheck PDFleong2007Noch keine Bewertungen
- Advanced SketchUp Training Installation GuideDokument1 SeiteAdvanced SketchUp Training Installation Guideleong2007Noch keine Bewertungen
- 3Q14 CIMB Group Financial Statements PDFDokument50 Seiten3Q14 CIMB Group Financial Statements PDFleong2007Noch keine Bewertungen
- EsbraySprinklerPump PDFDokument2 SeitenEsbraySprinklerPump PDFleong2007Noch keine Bewertungen
- Esbray80 26supercededDokument2 SeitenEsbray80 26supercededleong2007Noch keine Bewertungen
- Es Bray Sprinkler PumpDokument2 SeitenEs Bray Sprinkler Pumpleong2007Noch keine Bewertungen
- CCDDokument4 SeitenCCDleong2007Noch keine Bewertungen
- Fs 65Dokument8 SeitenFs 65leong2007Noch keine Bewertungen
- Span Stainless Steel Meter StandDokument2 SeitenSpan Stainless Steel Meter Standleong2007Noch keine Bewertungen
- Advanced SketchUp Training Installation GuideDokument1 SeiteAdvanced SketchUp Training Installation Guideleong2007Noch keine Bewertungen
- How To Layout and Scale A Drawing in AutoCADDokument4 SeitenHow To Layout and Scale A Drawing in AutoCADMad HouseNoch keine Bewertungen
- APN SeriesFanDokument1 SeiteAPN SeriesFanleong2007Noch keine Bewertungen
- KidsDokument1 SeiteKidsleong2007Noch keine Bewertungen
- Tonhr KWhrComputationDokument2 SeitenTonhr KWhrComputationleong2007Noch keine Bewertungen
- HVAC Equations Data and Rules of ThumbVentilationDokument11 SeitenHVAC Equations Data and Rules of ThumbVentilationleong2007Noch keine Bewertungen
- Cooling Load CheckDokument1 SeiteCooling Load Checkleong2007Noch keine Bewertungen
- HVAC Equations Data and Rules of ThumbDokument8 SeitenHVAC Equations Data and Rules of Thumbleong20070% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Suffolk 2023 Directory Care HomesDokument80 SeitenSuffolk 2023 Directory Care HomesChey1242Noch keine Bewertungen
- Clinical Audit: Pain Management in Total Knee Replacement Aadhar Hospital January - July 2018Dokument29 SeitenClinical Audit: Pain Management in Total Knee Replacement Aadhar Hospital January - July 2018Relacy Healthcare100% (2)
- Attachment and InterventionDokument13 SeitenAttachment and InterventioneducacionchileNoch keine Bewertungen
- Chapter 176Dokument13 SeitenChapter 176Intan Sanditiya AlifNoch keine Bewertungen
- Ched Memorandum OrderDokument4 SeitenChed Memorandum OrderEhlla Llausas AhmeeNoch keine Bewertungen
- Plansa Remed PDFDokument2 SeitenPlansa Remed PDFmihaipopescu0100% (1)
- UGH Syndrome After Lens Implantation PDFDokument2 SeitenUGH Syndrome After Lens Implantation PDFkameliasitorusNoch keine Bewertungen
- Wim Hof MethodDokument4 SeitenWim Hof MethodAdiMulahasanovicNoch keine Bewertungen
- Bioscalar Energy: The Healing PowerDokument4 SeitenBioscalar Energy: The Healing PowerSagarsinh RathodNoch keine Bewertungen
- 403-1 VersamedLM IventDokument9 Seiten403-1 VersamedLM IventCARLOS2285Noch keine Bewertungen
- DR - Syafrizal NST, SP - PDDokument69 SeitenDR - Syafrizal NST, SP - PDDenis Harli SiregarNoch keine Bewertungen
- MH CBIS ManualDokument79 SeitenMH CBIS ManualAnonymous Ax12P2srNoch keine Bewertungen
- Adherence To Antipsychotics in Schizophrenia PDFDokument168 SeitenAdherence To Antipsychotics in Schizophrenia PDFCosmin Ungureanu100% (1)
- Electronic Cigarettes-Users Profile, Utilization, Satisfaction and Perceived EfficiacyDokument12 SeitenElectronic Cigarettes-Users Profile, Utilization, Satisfaction and Perceived Efficiacyanalog_100% (1)
- The Discomfort of Labor: Pailz and and BirthDokument11 SeitenThe Discomfort of Labor: Pailz and and BirthIhwan ZoffonNoch keine Bewertungen
- Hypnotism Secret 8Dokument5 SeitenHypnotism Secret 8parasNoch keine Bewertungen
- Diagnostic ThermographyDokument21 SeitenDiagnostic Thermographyhoneysharlotte_6348100% (2)
- ArrhythmiasDokument48 SeitenArrhythmiasHarshan JeyakumarNoch keine Bewertungen
- Stimulant Equivalency TableDokument1 SeiteStimulant Equivalency Tablethor888888Noch keine Bewertungen
- Extinction Operant Conditioning PDFDokument2 SeitenExtinction Operant Conditioning PDFNateNoch keine Bewertungen
- Initial Assessment and Management of Trauma PatientsDokument8 SeitenInitial Assessment and Management of Trauma PatientsAlvin De LunaNoch keine Bewertungen
- Useful Books PDFDokument3 SeitenUseful Books PDFAyubkhan2Noch keine Bewertungen
- Dental Trauma LectureDokument10 SeitenDental Trauma Lectureasop06Noch keine Bewertungen
- Rheumatic Heart Disease Causes, Symptoms, and TreatmentDokument4 SeitenRheumatic Heart Disease Causes, Symptoms, and TreatmentJhen Jhen100% (1)
- Pediatric Acute Respiratory Distress SyndromeDokument2 SeitenPediatric Acute Respiratory Distress SyndromeTry Febriani SiregarNoch keine Bewertungen
- Thalasemmia, Hemophilia & Blood Cancer at Hamza Foundation Peshawar Field Work Report by Fakhre Alam Mohmand Dept of Social Work University of PeshawarDokument26 SeitenThalasemmia, Hemophilia & Blood Cancer at Hamza Foundation Peshawar Field Work Report by Fakhre Alam Mohmand Dept of Social Work University of PeshawarFakhrealamswNoch keine Bewertungen
- Clinical History TakingDokument36 SeitenClinical History Takingapi-1964133775% (4)
- Kazdin 2007 PDFDokument29 SeitenKazdin 2007 PDFDaniela UrreaNoch keine Bewertungen
- Maintenance Fluid Therapy in ChildrenDokument4 SeitenMaintenance Fluid Therapy in ChildrenNicole_0Noch keine Bewertungen
- ACT For Psychosis Recovery A Practical Manual For Group-Based Interventions Using Acceptance and Commitment Therapy by Emma K. O'Donoghue Eric M.J. Morris Joseph E. Oliver Louise C. Johns Steven C. HaDokument286 SeitenACT For Psychosis Recovery A Practical Manual For Group-Based Interventions Using Acceptance and Commitment Therapy by Emma K. O'Donoghue Eric M.J. Morris Joseph E. Oliver Louise C. Johns Steven C. HaHarriet Osakwe0% (1)