Beruflich Dokumente
Kultur Dokumente
Upper Git Journal
Hochgeladen von
Michael ValdezOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Upper Git Journal
Hochgeladen von
Michael ValdezCopyright:
Verfügbare Formate
Esophagus
The American Journal of Gastroenterology 106, 1447-1455 (August 2011)
Epidemiology and Natural History of Intestinal Metaplasia of the Gastroesophageal Junction and Barrett's Esophagus: A Population-Based Study
Kee Wook Jung, Nicholas J Talley, Yvonne Romero, David A Katzka, Cathy D Schleck, Alan R Zinsmeister, Kelly T Dunagan, Lori S Lutzke, Tsung-Teh Wu, Kenneth K Wang, Mary Frederickson, Debra M Geno, G Richard Locke andGanapathy A Prasad OBJECTIVES: Population-based data on the epidemiology and outcomes of subjects with intestinal metaplasia of the gastroesophageal junction (IMGEJ) and Barrett's esophagus (BE) are limited. The objectives of this study were to (i) estimate the incidence of IMGEJ and BE diagnosed from clinically indicated endoscopy in Olmsted County, MN, over three decades (1976 2006) and prevalence as of 1 January 2007, (ii) compare baseline characteristics of subjects with IMGEJ and BE, and (iii) study the natural history and survival of both cohorts. METHODS: This was a population-based cohort study. The study setting was Olmsted County, MN. Patients with BE (columnar segment >1cm with intestinal metaplasia) and IMGEJ (intestinal metaplasia in biopsies from the gastroesophageal junction) from 1976 to 2006 in Olmsted County, MN, were identified using Rochester Epidemiology Project resources. Demographic and clinical data were abstracted from medical records and pathology confirmed by gastrointestinal pathologists. The association of baseline characteristics with overall and progression-free survival was assessed using proportional hazards regression models. Outcome measures were baseline characteristics and overall survival of subjects with IMGEJ compared to those with BE.
RESULTS: In all, 487 patients (401 with BE and 86 with IMGEJ) were identified and followed for a median interval of 7 (BE subjects) to 8 (IMGEJ subjects) years. Subjects with BE were older, heavier, reported reflux symptoms more often, and had higher prevalence of advanced neoplasia than those with IMGEJ. No patient with IMGEJ progressed to esophageal adenocarcinoma (EAC) in contrast to BE subjects who had a cumulative risk of progression of 7% at 10 years and increased risk of death from EAC (standardized mortality ratio 9.62). The overall survival of subjects with BE and IMGEJ did not differ from that expected in similar age- and sexdistributed white Minnesota populations. CONCLUSIONS: Subjects with IMGEJ appear to have distinct clinical characteristics and substantially lower cancer progression risk compared to those with BE.
Response of Regurgitation to Proton Pump Inhibitor Therapy in Clinical Trials of Gastroesophageal Reflux Disease
Peter J Kahrilas, Colin W Howden and Nesta Hughes
Abstract
OBJECTIVES: The typical symptoms of gastroesophageal reflux disease (GERD) are heartburn and regurgitation. Extensive analysis has characterized heartburn and its responsiveness to proton pump inhibitor (PPI) therapy, but regurgitation has received relatively little attention. This study aimed to evaluate the response of regurgitation to PPI therapy in GERD trials. METHODS: Studies were identified by systematic searches in PubMed and Embase, as well as searching congress abstracts and the reference lists of Cochrane reviews.
RESULTS: Regurgitation was not an entry criterion or the primary end point in any of the 31 clinical trials reporting the response of regurgitation to PPI treatment in GERD. The definitions of regurgitation and responsiveness varied among trials and over half used investigator assessment of response. Owing to these inconsistencies, no meta-analysis was attempted. In seven placebo-controlled trials of PPI therapy, the therapeutic gain for regurgitation response averaged 17% relative to placebo and was >20% less than that observed for heartburn. Studies comparing PPIs with histamine-2 receptor antagonists or prokinetics found the comparator drug response similar to the placebo response rates seen in the placebo-controlled trials. CONCLUSIONS: The therapeutic gain with PPIs over placebo or comparator agents for the relief of regurgitation is modest, and considerably lower than for heartburn. Thus, regurgitation is likely to be an important factor for determining incomplete response to PPI treatment in GERD. Future trials would benefit from using regurgitation as a primary end point, applying an unambiguous definition of the symptom and of a positive treatment response, and using a validated patient-reported instrument for regurgitation assessment.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Leave Form CS Form No Version 1Dokument2 SeitenLeave Form CS Form No Version 1Michael ValdezNoch keine Bewertungen
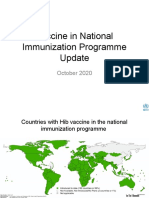
- Vaccine in National Immunization Programme Update: October 2020Dokument12 SeitenVaccine in National Immunization Programme Update: October 2020Michael ValdezNoch keine Bewertungen
- Quarter - : (Month) (Month) (Month) (Month) (Month) (Month)Dokument8 SeitenQuarter - : (Month) (Month) (Month) (Month) (Month) (Month)Michael ValdezNoch keine Bewertungen
- Central Luzon Doctors' Hospital Educational Institution, IncDokument2 SeitenCentral Luzon Doctors' Hospital Educational Institution, IncMichael ValdezNoch keine Bewertungen
- Organizational Politics and PowerDokument23 SeitenOrganizational Politics and PowerMichael Valdez100% (1)
- Ethical PrinciplesDokument7 SeitenEthical PrinciplesMichael ValdezNoch keine Bewertungen
- BIOETHICS Professional Issues HandoutsDokument2 SeitenBIOETHICS Professional Issues HandoutsMichael ValdezNoch keine Bewertungen
- CataractsDokument5 SeitenCataractsMichael ValdezNoch keine Bewertungen
- PulseoximetryDokument2 SeitenPulseoximetryRakshith NagarajaiahNoch keine Bewertungen
- Futuristic Nursing: - Sister Elizabeth DavisDokument14 SeitenFuturistic Nursing: - Sister Elizabeth DavisPhebeDimple100% (2)
- Diet's CardDokument8 SeitenDiet's CardJORGE ATRIANONoch keine Bewertungen
- Herbicides ToxicityDokument51 SeitenHerbicides ToxicityAdarshBijapurNoch keine Bewertungen
- 2014-1 Mag LoresDokument52 Seiten2014-1 Mag LoresLi SacNoch keine Bewertungen
- Coca Cola Fairlife CaseDokument4 SeitenCoca Cola Fairlife Caseapi-315994561Noch keine Bewertungen
- AM LOVE School Form 8 SF8 Learner Basic Health and Nutrition ReportDokument4 SeitenAM LOVE School Form 8 SF8 Learner Basic Health and Nutrition ReportLornaNirzaEnriquezNoch keine Bewertungen
- 2018 Overview Digestive System HandoutDokument11 Seiten2018 Overview Digestive System HandoutdraganNoch keine Bewertungen
- Eular References For Website 2015Dokument240 SeitenEular References For Website 2015Antonio BernalNoch keine Bewertungen
- Kardiomed-700-User ManualDokument87 SeitenKardiomed-700-User ManualJulia TimakovaNoch keine Bewertungen
- WEEK 2 ILP Grade 4Dokument5 SeitenWEEK 2 ILP Grade 4jean arriolaNoch keine Bewertungen
- Social Science Class 10 Understanding Economic DevelopmentDokument93 SeitenSocial Science Class 10 Understanding Economic DevelopmentkannansesNoch keine Bewertungen
- 23 Medicinal Plants The Native Americans Used On A Daily Basis - MSYCDokument15 Seiten23 Medicinal Plants The Native Americans Used On A Daily Basis - MSYCLeandro RodriguesNoch keine Bewertungen
- Checking Vital SighnDokument14 SeitenChecking Vital SighnAdimas AnggaraNoch keine Bewertungen
- Pork TocinoDokument1 SeitePork TocinoMaria Ivz ElborNoch keine Bewertungen
- JPNC 02 00096Dokument9 SeitenJPNC 02 00096Catalina StoicescuNoch keine Bewertungen
- Module 7. Presented - The Phil Health Program On Degenerative Diseases 93Dokument105 SeitenModule 7. Presented - The Phil Health Program On Degenerative Diseases 93Roma ClaireNoch keine Bewertungen
- Et CareDokument15 SeitenEt CarePaulo GarciaNoch keine Bewertungen
- Osteoarthritis of The Hip and Knee Flowchart PDFDokument2 SeitenOsteoarthritis of The Hip and Knee Flowchart PDFsilkofosNoch keine Bewertungen
- Esmeron 10 MG/ML Solution For Injection Rocuronium Bromide Prescribing InformationDokument3 SeitenEsmeron 10 MG/ML Solution For Injection Rocuronium Bromide Prescribing InformationVeeta Ruchi LieNoch keine Bewertungen
- BNMHGDokument34 SeitenBNMHGAnonymous lt2LFZHNoch keine Bewertungen
- Anemia in PregnancyDokument5 SeitenAnemia in PregnancySandra GabasNoch keine Bewertungen
- Know About Dengue FeverDokument11 SeitenKnow About Dengue FeverKamlesh SanghaviNoch keine Bewertungen
- Dokumen - Tips Biology Investigatory Project 561e79b91f5a0Dokument17 SeitenDokumen - Tips Biology Investigatory Project 561e79b91f5a0Upendra LalNoch keine Bewertungen
- Action Plan GPPDokument3 SeitenAction Plan GPPMa Rk AntonioNoch keine Bewertungen
- Secondary P.E. 10 Q3Dokument9 SeitenSecondary P.E. 10 Q3Jayzi VicenteNoch keine Bewertungen
- Platelet Analysis - An Overview: HistoryDokument7 SeitenPlatelet Analysis - An Overview: HistoryPieter Du Toit-EnslinNoch keine Bewertungen
- Cultural Landscape An Introduction To Human Geography 11th Edition Rubenstein Solutions ManualDokument16 SeitenCultural Landscape An Introduction To Human Geography 11th Edition Rubenstein Solutions Manualheathergarciafbqedgosyp100% (13)
- Climbing Training Log - TemplateDokument19 SeitenClimbing Training Log - TemplateKam Iqar ZeNoch keine Bewertungen
- Feeding Norms Poultry76Dokument14 SeitenFeeding Norms Poultry76Ramesh BeniwalNoch keine Bewertungen