Beruflich Dokumente
Kultur Dokumente
Lymphoma-Associated Hemophagocytic Syndrome - Clinical Features and Treatment Outcome - 2007 Ann Hematol
Hochgeladen von
William KristantoOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Lymphoma-Associated Hemophagocytic Syndrome - Clinical Features and Treatment Outcome - 2007 Ann Hematol
Hochgeladen von
William KristantoCopyright:
Verfügbare Formate
Ann Hematol (2007) 86:493498 DOI 10.
1007/s00277-007-0278-6
ORIGINAL ARTICLE
Lymphoma-associated hemophagocytic syndrome: clinical features and treatment outcome
A-Reum Han & Hye Ran Lee & Byeong-Bae Park & In Gyu Hwang & Sarah Park & Sang Cheol Lee & Kihyun Kim & Ho Yeong Lim & Young H. Ko & Sun Hee Kim & Won Seog Kim
Received: 8 January 2007 / Accepted: 23 February 2007 / Published online: 9 March 2007 # Springer-Verlag 2007
Abstract The clinical features and prognostic factor of lymphoma-associated hemophagocytic syndrome (LAHS), diagnosed according to World Health Organization classification, were investigated by reviewing the clinical records of 29 patients between September 1994 and September 2006. Compared with patients with T or natural killer (NK)/T cell LAHS, patients with B cell LAHS were older (p=0.022), were less likely to exhibit disseminated intravascular coagulation (DIC; p=0.011), and had less direct involveA-Reum Han and Hye Ran Lee contributed equally to this study. A.-R. Han Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea H. R. Lee Division of HematologyOncology, Department of Medicine, Paik Hospital, Inje University School of Medicine, Seoul, South Korea B.-B. Park : I. G. Hwang : S. Park : S. C. Lee : K. Kim : H. Y. Lim : W. S. Kim (*) Division of HematologyOncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, 50 Ilwon-Dong, Kangnam-Ku, Seoul 135-710, South Korea e-mail: wskimsmc@smc.samsung.co.kr Y. H. Ko Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea S. H. Kim Department of Laboratory Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea
ment of bone marrow (p=0.03). Clinical response was achieved in 15 (65.2%) and complete remission (CR) was achieved in 4 (17%) of 23 patients who received chemotherapy. Four patients received high-dose chemotherapy and autologous stem cell transplantation (A-SCT), and three of these four patients showed CR. The median survival was 36 days (95%CI, 20.251.8). Univariate analysis showed that poor performance status (p=0.028), T or NK/T cell lymphoma (p=0.016), presence of jaundice (p=0.063), the presence of DIC (p=0.002), and poor clinical response to treatment (p<0.001) predicted poor overall survival. These data suggest that the clinical features differ significantly between B cell LAHS and T or NK/T cell LAHS. Intensive treatment including highdose chemotherapy and A-SCT should be investigated. Keywords Hemophagocytic syndrome . Lymphoma-associated hemophagocytic syndrome
Introduction Hemophagocytic syndrome (HPS) is a clinicopathological disease entity characterized by histiocytic proliferation, fever, hepatosplenomegaly, cytopenia, deranged liver function, and frequent coagulopathy [1, 9, 21]. Acquired HPS in adults is associated with various conditions including infections, connective tissue diseases, and hematological malignancies, mainly non-Hodgkins lymphoma [1, 48, 1113, 15, 16, 18, 20, 21]. Among these conditions, most cases of lymphoma-associated hemophagocytic syndrome (LAHS) are associated with T cell or natural killer (NK)/T cell lymphoma, and LAHS secondary to B cell lymphoma is quite rare [4, 5, 7, 16, 20].
DO00278; No of Pages
494
Ann Hematol (2007) 86:493498
The clinical features, proper treatment, and prognostic factors of LAHS remain ill-defined because of its rarity, difficulty in diagnosis, and the poor general condition of the patient at the time of diagnosis [1, 8]. Although some studies on the clinical features of LAHS have been reported [5, 12, 18, 20, 21], few reports have used current World Health Organization (WHO) classification. In this retrospective study, we tried to clarify the clinical and laboratory characteristics of LAHS and to determine the effect of various factors on survival of patients with LAHS diagnosed according to WHO classification.
began and the date when disease progression was recognized or the date of the last follow-up visit. Overall survival duration was measured from the date of diagnosis to the date of death or the last follow-up visit. Survival rates were compared using either the log-rank test or the Breslow tests.
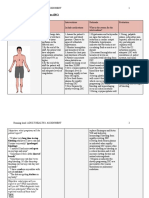
Table 1 Patient characteristics Characteristics Values
Materials and methods Patients Between September 1994 and September 2006, 52 patients were diagnosed with HPS in the bone marrow based on histological and immunological studies; 29 were diagnosed finally with LAHS. In all patients, haematoxylin and eosin slides and immunostaining for CD20, and light chains, CD3, CD4, CD8, CD30, and CD56 were performed, and the diagnosis for subtype was made according to WHO classification. To rule out minimal bone marrow involvement of the lymphoma cells, bilateral bone marrow sections were immunostained for CD3, CD20, and CD56 according to routine procedures. The clinical records were reviewed to characterize the clinical features and treatment outcomes. Statistical analysis The response was assessed according to response criteria of Cheson et al. [3] and/or clinical response criteria [17]. A clinical tumour response was defined as improved symptoms and improved laboratory findings or decreased size of a measurable lesion. Improved laboratory findings were defined as (1) decreased lactate dehydrogenase (LDH) concentration to the normal level or by one half; or (2) improved liver function test to normal values or bilirubin< 3 mg/dl if the baseline was >10 mg/dl; or (3) improved cytopenia (i.e., absent in next cycle) and without deterioration of other laboratory findings [17]. We defined two different responses: a transient response and a persistent response. A transient response was defined as a clinical response that did not last until the next cycle of chemotherapy. A persistent response was defined as a clinical response that lasted until the next cycle of chemotherapy. Clinical response rates and clinical features were compared with Fishers exact test. The KaplanMeier product-limit method was used to estimate the response duration and overall survival. The clinical response duration was determined from the difference between the date treatment
Patients Male Female Total Median age (year) Diagnosis Aggressive NK/T cell leukemia Peripheral T cell lymphoma, NOS Diffuse large B cell lymphoma Extranodal NK/T cell lymphoma, nasal type Anaplastic large cell lymphoma, primary systemic type ALK gene rearrangement: negative Performance status (ECOG) 02 34 Symptoms and signs Fever Hepatosplenomegaly Night sweating Weight loss Laboratory data Neutropenia (ANC1.0109/l) Anemia (Hb9.0 g/dl) Thrombocytopenia (PC100109/l) Hyperferritinemia (1,000 ng/ml, n=14) Hyper-LDH-nemia (500 IU/l, n=26) Hypofibrinogenemia (1.5 g/l, n=26) DIC Internal prognostic index (IPI) Low-intermediate High-intermediate High EBV ISH positive Aggressive NK/T cell lymphoma (n=10) Extranodal NK/T cell lymphoma (n=3) Peripheral T cell lymphoma, NOS (n=4) Diffuse large B cell lymphoma (n=2) Previous lymphoma history T or NK/T cell lymphoma (n=24) Diffuse large B cell lymphoma (n=5)
16 (55.2%) 13 (44.8%) 29 46 (range 987) 11 (37.9%) 8 (27.6%) 5 (17.2%) 3 (10.3%) 2 (6.9%)
17 (58.6%) 12 (41.4%) 29 (100%) 27 (93.1%) 9 (33.3%) 8 (27.6%) 11 (37.9%) 16 (55.2%) 25 (86.2%) 13 (92.9%) 26 (100%) 15 (57.7%) 16 (55.2%) 3 (10.3%) 14 (48.2%) 12 (41.4%) 8 2 2 1 (80.0%) (66.7%) (50.0%) (50.0%)
2 (8.3%) 2 (40%)
ALK Anaplastic lymphoma kinase, ECOG Eastern Cooperative Oncology Group, ANC absolute neutrophil count, PC platelet count, DIC disseminated intravascular coagulopathy, EBV EpsteinBarr virus, ISH in situ hybridization
Table 2 Patient characteristics Major involvement CRx 4 CRx D (days) nasal pharynx, spleen, lung, LN liver liver, spleen, LN liver, spleen LN 33 PR CR ++ ++ 64 1,983+ DVP#1 PR + 22 BM, BM BM, BM BM, BM BM, BM, IMVP-16/PD#1 NYII (doxorubicin/Ara-c) DHAP#1 PD + 37 6 17 8 49 36 127 1,991+ Treatment Rxa Survival (days)
Ann Hematol (2007) 86:493498
Number
Age/sex
Diagnosis
1 2 3 4 5 6 7 8
57/F 14/F 14/F 81/M 50/M 76/M 37/M 25/F
ENK/T PTCL ANKL PTCL ANKL PTCL ANKL ANKL
skin
CVP#1->DEC#3->mobilization DEC#3->mobilization->autoPBSCT-> VIP#3->mobilization->autoPBSCT CHOP#1 CHOP#1 CVP#1 + DEC#1
9 10 11 12 13 14 15 16 17 LN LN ascites, pleural effusion, LN CHOP#1 R-IMVP-16/PD#7 DEC#4->mobilization->IMVP16#5->MiniBEAM#2->DHAP#1 Cytoxan/cytarabine/vincristine DEC#2 DEC#2 DEC#3->mobilization->autoPBSCT->VIP#2 BVP#1 VIPD#6->Alemtuzumab #1 CHOP#6->mobilization->auto PBSCT DEC#2 R-CHOP#3->auto PBSCT CVP#1->IMVP-16/PD#2->Gemcitabine #1 PD CR PD CR PD CR SD ++ ++ PD PR + + ++ ++ ++ ++ ++ ++
60/M 34/M 62/M 67/F 22/F 87/F 46/M 68/M 21/M
ANKL PTCL ANKL PTCL ALCL PTCL PTCL DLBL ANKL
BM BM, BM BM BM BM, BM BM, BM,
1,534 138
51 8 21 4 7 8 21 1,541b 330
18 19 20 21 22
9/F 68/M 29/F 22/M 31/M
PTCL DLBL ANKL ANKL ENK/T
13 6 48
3 28 29 58 175
23 24 25 26 27 28 29
43/M 68/M 35/M 17/F 49/F 54/F 74/F
ANKL DLBL ENK/T ALCL ANKL DLBL DLBL
BM, ascites Liver BM, lung, skin BM BM, skin, nose, oral cavity, pleural and pericardial effusion BM, pleural effusion, ascites BM, LN, nose BM, scrotum, peritoneum, LN, testis BM, liver, lung, LN BM, spleen, LN LN Lung, adrenal gland
162 1,068+ 26 136+ 41
2 5 173 1,112+ 49 144+ 103
Response criteria according to Cheson et al. [3] Died of pneumonia Rx Response; CRx D clinical response duration; ENK/T extranodal NK/T cell lymphoma, nasal type; PTCL peripheral T cell lymphoma, not otherwise specified; ANKL aggressive NK/T-cell lymphoma; ALCL anaplastic large cell lymphoma, primary systemic type; DLBL diffuse large cell lymphoma; BM bone marrow; LN lymph node; (minus sign) no clinical response; (single plus sign) transient clinical response; (double plus sign) persistent clinical response; IMVP-16/PD ifosfamide, mesna, methotrexate, ectoposide, and prednisolone; DHAP cisplatin, cytarabine, and dexamethasone; DVP daunorubicn, vincristine, and prednisolone; CVP cyclophosphamide, vincristine, and prednisolone; DEC dose escalated CHOP; CHOP cyclophosphamide, doxorubicin, vincristine, and prednisolone; R-IMVP-16/PD rituximab and IMVP-16/PD; Mini BEAM BCNU, ectoposide, cytarabine, and melphalan; BVP bleomycin, vincristine, and prednisolone; VIPD ectoposide, ifosphamide, cisplatin, and dexamethasone 495
496 Table 3 Clinical features according to histopathologic type B cell n=5 Patients gender Male Female Age (year) 60 >60 Weight loss No Yes Night sweating No Yes PS 1 2 3 4 ANC (109/l) 1.0 >1.0 Hb (g/dl) 9 >9 Platelet count (109/l) 20 >20 TB (mg/dl) 2 >2 PT (INR) 1.7 >1.7 Fibrinogen (g/l) 1.5 >1.5 Ferritin (ng/ml) 1,000 >1,000 IPI Low Intermediate High Intermediate High DIC No Yes BM involvement No Yes HPS onset With lymphoma After lymphoma T or NK/T cell n=24 p value
Ann Hematol (2007) 86:493498
Results Patient characteristics The clinical characteristics of the 29 patients are given in Tables 1 and 2. The median age was 46 years, and the range was 987 years. The most frequent histopathological subtype was aggressive NK/T cell leukemia, followed by (in decreasing frequency) peripheral T cell lymphoma, not otherwise specified (PTCL-NOS), diffuse large B cell lymphoma (DLBL), extranodal NK/T cell lymphoma, nasal type, and anaplastic large cell lymphoma, primary systemic type. Among the DLBL patients, one patient was diagnosed with intravascular large B cell lymphoma (patient no. 29). The most frequent symptom was fever (100%). Neutropenia (absolute neutrophil count1.0109/l) was observed in 11 patients (37.9%). Twenty-five patients (86.2%) showed thrombocytopenia (platelet count100109/l). Elevation of LDH concentration and hyperferritinemia were observed in >90% of the patients. Most patients (89.6%) were high-intermediate risk or high risk according to the international prognostic index. The clinical features differed significantly between patients with B cell LAHS and patients with T or NK/T cell LAHS (Table 3). Patients with B cell LAHS were older (p=0.022), were less likely to exhibit disseminated intravascular coagulation (DIC; p=0.011), and had less direct involvement of bone marrow (p=0.03). Treatment and response to the therapy
1.000 0.033
3 2 1 4 3 2 1 4 2 2 1 0 1 4 5 0 0 5 3 2 3 2 N=4 0 4 n=4 0 4 1 1 3 5 0 3 2 3 2
13 11 19 5 18 6 8 16 5 8 7 4 10 14 11 13 8 16 10 14 16 8 N=22 14 8 n=10 1 9 2 13 9 8 16 0 24 22 2
1.000
0.022
0.597
1.000
0.65
0.622
0.048
0.283
0.632
1.000
Twenty-three of 29 patients received various kinds of chemotherapies. Thirteen of 23 patients who received chemotherapy had measurable lesions. Of them, four patients achieved complete remission (CR), and three patients achieved PR according to the response criteria of Cheson et al. [3]. Fifteen of the 23 patients attained a
1.0
0.359
0.8
0.011
Overall survival
0.6
0.03
0.4
0.127
0.2 0.0
PS Performance scale, ANC absolute neutrophil count, Hb hemoglobin, TB total bilirubin, PT prothrombin time, IPI international prognostic index, DIC disseminated intravascular coagulopathy, BM bone marrow, HPS hemophagocytic syndrome
1000
2000
Time(days) Fig. 1 KaplanMeier plots of overall survival
Ann Hematol (2007) 86:493498 Table 4 Prognostic factors for overall survival (univariate analysis) Factors Age (60 vs >60) Sex PS Lymphoma type (NK/T vs T vs B cell) ANC count (1.0109/l vs >1.0109/l) Platelet count (20109/l vs >20109/l) Hb (9 g/dl vs >9 g/dl) TB (2 mg/dl vs >2 mg/dl) PT [1.7 (INR) vs >1.7 (INR)] Fibrinogen (1.5 g/l vs >1.5 g/l) Treatment anthracycline DIC IPI Clinical response Univariate (p) 0.231 0.627 0.028 0.016 0.666 0.546 0.387 0.063 0.002 0.006 0.496 0.002 0.348 <0.001
497
PS performance scale, ANC absolute neutrophil count, Hb hemoglobin, TB total bilirubin, PT prothrombin time, DIC disseminated intravascular coagulopathy, IPI international prognostic index, INR international normalized ratio
clinical response (65.2%, 95%CI, 44.286.3%). The clinical response rate did not differ between patients treated with or without anthracycline (p=1.0). Ten of the 15 responders achieved a persistent response, and four patients (nos. 8, 16, 26, and 28) achieved CR. The response was maintained for 4 to 1,983+ days (Table 2). In four patients (nos. 8, 22, 26, and 28), high-dose chemotherapy and autologous stem cell transplantation (A-SCT) was planned. Patient nos. 26 and 28 received A-SCT while in CR and patient no. 22 while in the refractory state. Patient no. 8 received A-SCT twice because remaining tumour cells were found in her bone marrow after the first A-SCT; she achieved CR eventually. Prognosis With median follow-up of 1,999 days (range 144 3,584 days), median survival of all patients was 36 days (range 21,991+ days); the overall survival curve is shown in Fig. 1. Univariate analysis showed that the following parameters predicted poor survival (Table 4): poor performance status (p=0.028), T or NK/T cell lymphoma (p=0.016), the presence of jaundice (p=0.063), the presence of DIC (p=0.002), and poor clinical response to treatment (p<0.001). The survival differences are shown in Fig. 2. However, no significant prognostic factor was found in the multivariate analysis.
The most common cause of acquired HPS in adults is LAHS [1, 7, 11, 21]. Most cases of LAHS have been known to be associated with T cell or NK/T cell lymphoma, and LAHS cases secondary to B cell lymphoma are rare [2, 4, 5, 7, 16, 20]. Most of our 29 patients with LAHS (83%) were associated with T or NK/T cell lymphoma as expected from the literature [5, 1113]. Interestingly, B cell LAHS was associated with significantly different clinical features (Table 3), in particular, the relatively low incidence (40%) of direct bone marrow infiltration by malignant cell. In the report by Florena et al., one of two patients with B cell LAHS showed only hemophagocytosis without malignant cells in the bone marrow. However, one of nine patients with T cell LAHS showed hemophagocytosis only without malignant cells in the bone marrow [7]. In addition, patients older than 60 years were more common in B cell LAHS (80%). These features are similar to those reported previously [5, 13, 15, 16]. Patients with B cell LAHS had a lower frequency of full-blown DIC, which is consistent with previous reports [12, 16]. Miyahara et al. [12] reported seven cases of B cell LAHS and found no serious coagulation abnormalities. Shimazaki et al. [16] also found only one patient with elevated D-dimmer of four patients tested. However, DIC was observed in all patients with intravascular large B cell LAHS [13]. Based on this observation, the pathogenesis of B cell LAHS seems to differ between intravascular large B cell LAHS and other types of B cell LAHS [14]. Because the majority of cases had no measurable lesion, it is difficult to evaluate the response to chemotherapy according to established response criteria. Based on our response criteria, the clinical response to chemotherapy was 65.2%, including four CRs. However, in many patients, the response could not be maintained until the next chemotherapy cycle, giving only a transient response. Early and
1.0
0.8
Overall survival
: Persistent response (n =10) : Transient response (n =5) : No response (n =8) p value < 0.001
0.6
0.4
0.2 0.0
Discussion HPS is a reactive histiocytic abnormality with dramatic clinical features including fever and cytopenia [7, 11, 21].
1000
2000
Time(days)
Fig. 2 KaplanMeier plots of overall survival according to clinical response
498
Ann Hematol (2007) 86:493498 9. Kumakura S (2005) Hemophagocytic syndrome. Intern Med 44:278280 10. Lee PS, Hwang WS (2002) Aggressive natural killer cell lymphoma/leukemia. Zhonghua Yi Xue Za Zhi (Taipei) 65:622 626 11. Majluf-Cruz A, Sosa-Camas R, Perez-Ramirez O, Rosas-Cabral A, Vargas-Vorackova F, Labardini-Mendez J (1998) Hemophagocytic syndrome associated with hematological neoplasias. Leuk Res 22:893898 12. Miyahara M, Sano M, Shibata K, Matsuzaki M, Ibaraki K, Shimamoto Y, Tokunaga O (2000) B-cell lymphoma-associated hemophagocytic syndrome: clinicopathological characteristics. Ann Hematol 79:378388 13. Murase T, Nakamura S, Tashiro K, Suchi T, Hiraga J, Hayasaki N, Kimura M, Murakami M, Mizoguchi Y, Suzuki T, Saito H (1997) Malignant histiocytosis-like B-cell lymphoma, a distinct pathologic variant of intravascular lymphomatosis: a report of five cases and review of the literature. Br J Haematol 99:656664 14. Murase T, Yamaguchi M, Suzuki R, Okamoto M, Sato Y, Tamaru J, Kojima M, Miura I, Mori N, Yoshino T, Nakamura S (2007) Intravascular large B-cell lymphoma (IVLBCL): a clinicopathologic study of 96 cases with special reference to the immunophenotypic heterogeneity of CD5. Blood 109:478485 15. Ohno T, Miyake N, Hada S, Hirose Y, Imura A, Hori T, Uchiyama T, Saiga T, Mizumoto T, Furukawa H (1998) Hemophagocytic syndrome in five patients with EpsteinBarr virus negative B-cell lymphoma. Cancer 82:19631972 16. Shimazaki C, Inaba T, Shimura K, Okamoto A, Takahashi R, Hirai H, Sudo Y, Ashihara E, Adachi Y, Murakami S, Saigo K, Fujita N, Nakagawa M (1999) B-cell lymphoma associated with haemophagocytic syndrome: a clinical, immunological and cytogenetic study. Br J Haematol 104:672679 17. Song SY, Kim WS, Ko YH, Kim K, Lee MH, Park K (2002) Aggressive natural killer cell leukemia: clinical features and treatment outcome. Haematologica 87:13431345 18. Su IJ, Hsu YH, Lin MT, Cheng AL, Wang CH, Weiss LM (1993) EpsteinBarr virus-containing T-cell lymphoma presents with hemophagocytic syndrome mimicking malignant histiocytosis. Cancer 72:20192027 19. Tsuchiyama J, Imajo K, Yoshino T, Nanba N, Toyota A, Yoshida C, Fujii K, Kondo E, Okazuka K, Hashimoto S, Toba K, Fuse I, Aizawa Y, Harada M, Tsubota T (2002) High-dose chemotherapy and autologous peripheral blood stem cell transplantation for treatment of unspecified peripheral T-cell lymphoma presented with hepatosplenomegaly and hypercytokinemia syndrome: report of three cases. Ann Hematol 81:588592 20. Wilson MS, Weiss LM, Gatter KC, Mason DY, Dorfman RF, Warnke RA (1990) Malignant histiocytosis. A reassessment of cases previously reported in 1975 based on paraffin section immunophenotyping studies. Cancer 66:530536 21. Wong KF, Chan JK (1992) Reactive hemophagocytic syndrome a clinicopathologic study of 40 patients in an Oriental population. Am J Med 93:177180
intensive chemotherapy regimens have been recommended by some authors [8, 10, 11, 17]. The role of high-dose chemotherapy and A-SCT in prolonging response and survival needs to be investigated [8, 19]. In our study, three of four patients receiving A-SCT achieved CR. Univariate analysis revealed that poor prognosis was related to poor performance status, T or NK/T cell lymphoma, jaundice, DIC, and poor response to chemotherapy. However, no prognostic factors were found in multivariate analysis. Large studies are needed to investigate further the relationship prognostic predictors in patients with LAHS. LAHS is one of the rarest and least well-characterized disease, and the treatment outcomes have been described only in a small series [1, 5, 1113, 15, 16, 18, 19]. Large series studies are needed to investigate the optimal treatment. References
1. Allory Y, Challine D, Haioun C, Copie-Bergman C, Delfau-Larue MH, Boucher E, Charlotte F, Fabre M, Michel M, Gaulard P (2001) Bone marrow involvement in lymphomas with hemophagocytic syndrome at presentation: a clinicopathologic study of 11 patients in a Western institution. Am J Surg Pathol 25:865874 2. Bhagwati NS, Oiseth SJ, Abebe LS, Wiernik PH (2004) Intravascular lymphoma associated with hemophagocytic syndrome: a rare but aggressive clinical entity. Ann Hematol 83:247250 3. Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, Coiffier B, Fisher RI, Hagenbeek A, Zucca E, Rosen ST, Stroobants S, Lister TA, Hoppe RT, Dreyling M, Tobinai K, Vose JM, Connors JM, Federico M, Diehl V (2007) Revised response criteria for malignant lymphoma. J Clin Oncol 25:579586 4. Cheung MM, Chan JK, Lau WH, Foo W, Chan PT, Ng CS, Ngan RK (1998) Primary non-Hodgkins lymphoma of the nose and nasopharynx: clinical features, tumor immunophenotype, and treatment outcome in 113 patients. J Clin Oncol 16:7077 5. Falini B, Pileri S, De Solas I, Martelli MF, Mason DY, Delsol G, Gatter KC, Fagioli M (1990) Peripheral T-cell lymphoma associated with hemophagocytic syndrome. Blood 75:434444 6. Fisman DN (2000) Hemophagocytic syndromes and infection. Emerg Infect Dis 6:601608 7. Florena AM, Iannitto E, Quintini G, Franco V (2002) Bone marrow biopsy in hemophagocytic syndrome. Virchows Arch 441:335344 8. Imashuku S (1997) Differential diagnosis of hemophagocytic syndrome: underlying disorders and selection of the most effective treatment. Int J Hematol 66:135151
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Heat Stroke: Review Open AccessDokument8 SeitenHeat Stroke: Review Open AccessJulian HuningkorNoch keine Bewertungen
- CCRN QuestionsDokument19 SeitenCCRN QuestionsMelissaDavis67% (6)
- Contemporary Management of Major Haemorrhage in Critical CareDokument13 SeitenContemporary Management of Major Haemorrhage in Critical CareYo MeNoch keine Bewertungen
- Acute Infectious Purpura FulminansDokument15 SeitenAcute Infectious Purpura FulminansFranklin Aranda100% (2)
- Capillary Fragility/ Resistance Test: Tourniquet or Rumpel-Leede or Hess TestDokument4 SeitenCapillary Fragility/ Resistance Test: Tourniquet or Rumpel-Leede or Hess TestGerly MaglangitNoch keine Bewertungen
- APTTDokument2 SeitenAPTTApril Lady Faith P. PaundogNoch keine Bewertungen
- Hesi Exit Exam ReviewDokument35 SeitenHesi Exit Exam ReviewIndia91% (92)
- DIC Case StudyDokument3 SeitenDIC Case StudyJuliaNoch keine Bewertungen
- Pediatric Critical Care Medicine: EditorsDokument269 SeitenPediatric Critical Care Medicine: EditorsCk1NhiKhoa2020 chuyenkhoaNoch keine Bewertungen
- Electrical Burn PathophysiologyDokument1 SeiteElectrical Burn PathophysiologydanicaNoch keine Bewertungen
- MCQ ON Acute Posthemorrhagic AnemiaDokument22 SeitenMCQ ON Acute Posthemorrhagic AnemiaSampath KumarNoch keine Bewertungen
- Maternal Notes Google DocsDokument24 SeitenMaternal Notes Google DocsOracion, Bernette Meiji B.Noch keine Bewertungen
- Disseminated Intravascular CoagulationDokument19 SeitenDisseminated Intravascular CoagulationAnna MilliziaNoch keine Bewertungen
- D Dimer Testing in Clinical PracticeDokument3 SeitenD Dimer Testing in Clinical PracticePrashantNoch keine Bewertungen
- Sepsis and The Systemic Inflammatory Response SyndromeDokument9 SeitenSepsis and The Systemic Inflammatory Response SyndromeHandi Tri EffendiNoch keine Bewertungen
- Acquired Coagulation DisordersDokument12 SeitenAcquired Coagulation DisordersaymenNoch keine Bewertungen
- Pregnancy Induced Hypertension Case StudyDokument75 SeitenPregnancy Induced Hypertension Case StudyJing CruzNoch keine Bewertungen
- Sepsis Induced Coagulopathy A Comprehensive.2Dokument16 SeitenSepsis Induced Coagulopathy A Comprehensive.2antoine.dovalNoch keine Bewertungen
- Sepsis: Sepsis and Septic ShockDokument22 SeitenSepsis: Sepsis and Septic ShockWialda Dwi rodyahNoch keine Bewertungen
- CoagulopathyDokument121 SeitenCoagulopathyMegat Mohd Azman AdzmiNoch keine Bewertungen
- Antepartum HaemorrhageDokument65 SeitenAntepartum HaemorrhageAmit RamrattanNoch keine Bewertungen
- Hematologic DisordersDokument197 SeitenHematologic DisordersDanica Mae BianitoNoch keine Bewertungen
- 1-4 Hemostasis, Surgical Bleeding and TransfusionDokument17 Seiten1-4 Hemostasis, Surgical Bleeding and TransfusionRobin Tolentino100% (3)
- Learning ObjectivesDokument12 SeitenLearning ObjectivesjmcvicenteNoch keine Bewertungen
- Clinical Internship: Hematology: WBC AnomaliesDokument8 SeitenClinical Internship: Hematology: WBC AnomaliesNaomi NicoleNoch keine Bewertungen
- Hema Notes (Lec)Dokument50 SeitenHema Notes (Lec)Anonymous 0zrCNQNoch keine Bewertungen
- Hyperleukocytosis and Leukostasis in Hematologic MalignanciesDokument17 SeitenHyperleukocytosis and Leukostasis in Hematologic MalignanciesAna María Díaz MedinaNoch keine Bewertungen
- Pathology: Fluid & Hemodynamic Derangement - MCQDokument5 SeitenPathology: Fluid & Hemodynamic Derangement - MCQahmed jaradNoch keine Bewertungen
- OB 1.05 Late HemorrhageDokument15 SeitenOB 1.05 Late HemorrhageMaikka IlaganNoch keine Bewertungen