Beruflich Dokumente
Kultur Dokumente
Tube Feeding Policis Sesaona
Hochgeladen von
Pa'Trice ShepardOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Tube Feeding Policis Sesaona
Hochgeladen von
Pa'Trice ShepardCopyright:
Verfügbare Formate
Protocol NICU/NBN Unit Practice Manual John Dempsey Hospital Department of Nursing The University of Connecticut Health Center
er PROTOCOL FOR: POLICY:
Page 1 of 7
Feedings: Nasogastric (NG) / Orogastric (OG): Continuous / Intermittent 1. It is up to the discretion of the nurse to decide whether the feeding tube should be placed orally or nasally. NG feeds may increase airway resistance. a. OG placement is preferable when infant is on infant flow CPAP or other CPAP device. b. Nasal tubes are most commonly used for intubated infants. c. The infants gag and behavioral responses to the tube will influence the feeding tube location. 2. Feeds are ordered by the physician or AP to be given either continuously or intermittently. 3. Intermittent gavage feedings that are administered by gravity are to be given with the RN in attendance for the duration of the feeding. This allows regulation of flow of the feeding, ongoing assessment of accurate tube placement, provision of non-nutritive sucking, and human contact to make feeding a positive experience. a. Intermittent gavage feeds are not to be suspended with feeding infusing at an unregulated rate. b. 6.5 or 8 French feeding tubes are recommended for intermittent gavage feeds. c. The desired duration of a feeding is a minimum of 10 minutes (before full feeding volume is reached), then 15 to 30 minutes (once full volume is reached). d. When possible, hold the infant during the feeding. 4. Intermittent feeds may be given over a period of time on a pump. The decision to do this is made collaboratively between nursing and medicine. When intermittent feeds are administered by infusion pump, the infant should be checked frequently to ensure that the tube position is correct, and that the infant is not experiencing distress related to the rate and/or volume of feeding. 5. Indwelling feeding tubes are usually placed in smaller infants when the anticipated duration of tube feedings is months or several weeks. 6. Feeding tubes will be replaced according to the following schedule: a. Intermittent or single use, for example, polyvinyl chloride (PVC) tubes every 24 hours. b. Polyurethane tubes, such as Indwell every 4 weeks. c. Silicone tubes (such as Nutricath) as needed when they fall out. If silicone tube is not grossly contaminated (e.g., slips out of nose and remains in isolette), you may clean tube with warm water and dish soap, rinse well and replace.
Protocol NICU/NBN Unit Practice Manual John Dempsey Hospital Department of Nursing The University of Connecticut Health Center PROTOCOL FOR:
Page 2 of 7
Feedings: Nasogastric (NG) / Orogastric (OG): Continuous / Intermittent 7. Breast milk or formula will be kept at room temperature for no longer than 4 hours. a. If on intermittent pump feeds every 3 to 4 hours, the entire feeding setup is changed with each feeding. b. Bottles and nipples that have been used for oral feeding are to be discarded after 1 hour. 8. Only tubings designed for enteral use should be used for pump feedings.
DESIRED PATIENT OUTCOMES:
1. Will tolerate gastric feedings with no increase in physiologic distress. 2. Will have minimal stress placed on a GI tract that is developmentally and physiologically immature. 3. Will demonstrate desired weight gain when full volume achieved. 4. Pain or discomfort will be minimized by use of comfort measures during and after tube placement.
EQUIPMENT:
Feeding tube of size appropriate for infant 3 ml syringe (for check of residuals) Water-soluble lubricant Feeding reservoir (appropriate size syringe or feeding bag) Prescribed breast milk or formula Stethoscope Pump (if applicable) Enteral tubing for pump (if applicable)
CLINICAL ASSESSMENT AND CARE:
1. Assess the following prior to each feeding (intermittent), every 4 hours minimum (continuous) or as ordered: a. Amount, color, consistency of gastric aspirates. 1) Immediately report blood, coffee ground, or bilious aspirates. 2) Report aspirates greater than one hours volume of feeding (if continuous feeds) or more than 50% of feeding volume (if intermittent feedings). 3) Report frequent or large emesis. b. Assess abdominal girth a minimum of every 4 hours until full feedings tolerated for one week, then measure every other feeding. 1) Report increase in abdominal girth, decreased or absent bowel sounds. 2) Immediately report presence of a tense, distended and/or discolored abdomen, clinically enlarged bowel loops, and/or absence of bowel sounds.
Protocol NICU/NBN Unit Practice Manual John Dempsey Hospital Department of Nursing The University of Connecticut Health Center PROTOCOL FOR:
Page 3 of 7
Feedings: Nasogastric (NG) / Orogastric (OG): Continuous / Intermittent
c. Guaiac stools as ordered or when there is evidence of feeding intolerance/blood in stools. 1) Report heme positive stools. d. Verify tube position every 8 hours (continuous) or before each feeding (intermittent). The tube marking at the lip should be visible when the tube is secured. 1) Check to be sure that the tape on the tube has not slipped. e. Perform ongoing assessment for apnea and bradycardia. 1) Report increased frequency or severity of spells. f. Assess readiness for intermittent gavage feedings. The general goal is to remove the indwelling tube by 34 weeks corrected gestational age. Infants on CPAP may need a longer time with indwelling feeding tubes. 2. Refeed gastric residuals of partially-digested formula because there residuals also contain gastric acid, enzymes, and electrolytes. Consult with AP/MD to determine if the volume of the residual is to be given in addition to the ordered feeding volume or included in the total feeding volume. Use of Human Milk Fortifier with Expressed Breast Milk:
1. Prepare a clean work surface; wipe the area with a Sani-wipe. 2. Add the ordered number of packets per volume of expressed breast milk. 3. Gently mix well with a spoon to dissolve the Human Milk Fortifier (HMF). DO NOT SHAKE VIGOROUSLY as this will break up the fat molecules in the milk and cause them to stick to the sides of the syringe or the tubing. 4. Place the desired amount of prepared breast milk in the syringe. 5. If on continuous feeding: a. Place on a syringe pump and infuse with the pump at a 25 to 45 degree angle to enhance fat delivery. b. The HMF will begin to settle toward the syringe plunger over time. At least every hour, gently shake and rotate the syringe pump to remix the HMF into the milk. If this is not done, the HMF settles to the bottom of the syringe and the infant will either not get the HMF because it is stuck in the tubing or will get a bolus of HMF at the end of the feeding which may affect feeding tolerance.
Protocol NICU/NBN Unit Practice Manual John Dempsey Hospital Department of Nursing The University of Connecticut Health Center PROTOCOL FOR: Criteria for Using Indwelling Tubes:
Page 4 of 7
Feedings: Nasogastric (NG) / Orogastric (OG): Continuous / Intermittent
1. Indwelling tubes area generally used for smaller infants when it is anticipated that tube feeding will be needed for months or several weeks. 2. Indwelling tubes may be indicated in late preterm or term infants who: a. Have a mature gag reflex and aversive response to tube placement. b. Have more than 3 consecutive feedings with emesis or gagging during feedings. The infant shows obvious clinical distress by pulling away and/or arching during feedings. c. Are not consistently taking the entire feeding orally and the remainder of feeding needs to be gavaged. d. Are emerging po feeders that tire and need to rest and have a pump feed after 2 to 3 consecutive oral feedings. e. Are recovering from severe lung disease with or without PPHN who may have disorganized feeding related to illness and/or withdrawal from opioids.
PROCEDURE: ACTION 1. Select appropriate feeding tube according to infants size: a. Silicone tube (such as Nutricath) for continuous feeding infants < 1500 grams. POINTS OF EMPHASIS 1. Guidelines for tube size.
a. A 5 French tube is usually appropriate for continuous NG feeds. On larger babies with rapid infusion rates, a 8 French tube may be necessary. b. Size 6.5 or 8 French tubes are generally used for intermittent feedings that are infused by gravity. It is very difficult to infuse feeds by gravity through a #5 French feeding tube. Feedings should not be injected under pressure.
b. Polyurethane tubes (such as Indwell) for infants > 1500 grams.
2. Place OG or NG feeding tube. a. Measure tip of nose to ear lobe and to a point halfway between xiphoid and the umbilicus. Mark feeding tube at this length. b. Dip end of tube in water-soluble lubricant. b. Lubricating decreases possible damage of mucous membranes.
Protocol NICU/NBN Unit Practice Manual John Dempsey Hospital Department of Nursing The University of Connecticut Health Center PROTOCOL FOR:
Page 5 of 7
Feedings: Nasogastric (NG) / Orogastric (OG): Continuous / Intermittent c. To prevent aspiration if vomiting occurs. d. If the infant experiences any sign of compromise, remove the feeding tube and allow the infant to recover.
c. Turn head to side.
d. Pass feeding tube gently through mouth or nares to the desired depth.
e. Place a piece of tape with date of insertion on tube. 3. Check for tube placement. a. Aspirate tube with a 3 ml syringe to determine the amount of residual and observe the stomach. b. Inject a small amount of air into feeding tube while listening with stethoscope over stomach for gurgling. 4. Position infant so infant is well supported taking into account maturity, diagnoses and unique developmental needs. Consider holding infants, when possible, to support positive interactions during feeding. 5. Offer non-nutritive sucking experiences, taking into account infants cues and responses. 6. Administer ordered feedings that have been prepared to reduce the likelihood of infectious complications. 4. Skin to Skin (Kangaroo) care during feeding may enhance the feeding experience for the infant and the parent. a. Proper placement of feeding tube is essential for prevention of formula introduction into lungs.
5. Non-nutritive sucking will enhance the transition to oral feeding.
6. Breast milk or formula should not be kept at room temperature for more than 4 hours. Excessive warming can destroy components of breast milk that are heat sensitive, such as IgA and enzymes and can initiate bacterial proliferation.
a. Place prescribed amount of formula in syringe or feeding bag. b. If a pump is being used for feeding, prime with formula. 1) Intermittent Gravity Feeds a) Attach syringe of formula and administer by gravity over at least 10 minutes. Allow formula to enter slowly to prevent distention and diarrhea or discomfort. b) When removing the feeding tube, pinch the tubing to prevent air from entering stomach. a) Regulate flow by raising or lowering syringe. Feedings should not be injected under pressure. Do not leave unattended during feeding.
b) To decrease chance of abdominal distention.
Protocol NICU/NBN Unit Practice Manual John Dempsey Hospital Department of Nursing The University of Connecticut Health Center PROTOCOL FOR:
Page 6 of 7
Feedings: Nasogastric (NG) / Orogastric (OG): Continuous / Intermittent
c) Remove the tube smoothly and quickly, keeping the infants head turned to the side.
c) An NG tube may be kept in place between feeds if the nurse assesses that the infant tolerates this better.
d) Burp infant. 2) Intermittent Pump Feedings a) Attach the primed pump tubing to the feeding tube and set the pump to infuse the feeding over the desired amount of time. a) The duration of feeding should be comparable to that of gravity feedings, at least 10 minutes if full volume feeds have not been reached and 15 to 30 minutes for full volume feedings. A slower rate (30 minutes to 1 hour) is needed for those who have not been able to tolerate bolus feedings and need a longer infusion time. a) Interact with infant as per readiness cues of and state of arousal with the goal of feeding as a time of social interaction. Provide opportunities for nonnutritive sucking. b) Check the infant periodically during the feeding to ensure that the tube position is correct and that the infant is not experiencing distress related to the rate and/or volume of the feeding. c) Clear the feeding tube with air or sterile water at the completion of the feeding, unless the tube is being removed. 3) Continuous Feeds a) Attached primed pump tubing to feeding tube and start infusion at the ordered rate. a) Based on infants cues and state of arousal, interact with infant and provide opportunities for non-nutritive sucking so that feeding becomes a positive interaction.
APPROVAL: EFFECTIVE DATE:
Nursing Standards Committee 2/89
Protocol NICU/NBN Unit Practice Manual John Dempsey Hospital Department of Nursing The University of Connecticut Health Center PROTOCOL FOR: REVISION DATES:
Page 7 of 7
Feedings: Nasogastric (NG) / Orogastric (OG): Continuous / Intermittent 3/90, 6/91, 8/93, 11/93, 12/94, 6/97, 12/97, 11/98, 7/99, 1/00, 10/01, 1/03, 11/07, 7/10 11/04, 9/05, 11/06, 12/08, 10/09
REVIEWED DATES:
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Atlas of Oral Maxillofacial SurgeryDokument2 SeitenAtlas of Oral Maxillofacial SurgeryStefan PutnikNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- MAHESH S DHA Anesthesia TechnologyDokument4 SeitenMAHESH S DHA Anesthesia TechnologyGloria JaisonNoch keine Bewertungen
- Surgical Consent For Exploratory LapDokument1 SeiteSurgical Consent For Exploratory LapNoor KameliaNoch keine Bewertungen
- Wound Assessment Tools. ReviewDokument9 SeitenWound Assessment Tools. ReviewNguyễn Nhật LinhNoch keine Bewertungen
- Female Genital CutingDokument80 SeitenFemale Genital CutingTarek AnisNoch keine Bewertungen
- AmnioGenix MTMDokument2 SeitenAmnioGenix MTMBlake McClellan0% (1)
- Nutrients 10 01568 PDFDokument13 SeitenNutrients 10 01568 PDFمالك مناصرةNoch keine Bewertungen
- CIS Self-Study Lesson Plans: Surgical Instrumentation For Gynecological ProceduresDokument3 SeitenCIS Self-Study Lesson Plans: Surgical Instrumentation For Gynecological Proceduresjerimiah_manzonNoch keine Bewertungen
- New ResumeDokument3 SeitenNew Resumeapi-400175269Noch keine Bewertungen
- Jacqueline Mora: Client Care Specialist - Affinity RecoveryDokument3 SeitenJacqueline Mora: Client Care Specialist - Affinity RecoveryJames LanierNoch keine Bewertungen
- Five Years of Cerebral Palsy Claims - A Thematic Review of NHS Resolution DataDokument92 SeitenFive Years of Cerebral Palsy Claims - A Thematic Review of NHS Resolution DataUsman NarooNoch keine Bewertungen
- MultiCare NewsletterDokument3 SeitenMultiCare NewsletterAnitaCarminNoch keine Bewertungen
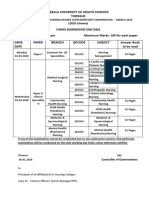
- Kerala University of Health Sciences Thrissur: (2010 Scheme)Dokument1 SeiteKerala University of Health Sciences Thrissur: (2010 Scheme)subiNoch keine Bewertungen
- Enhanced Recovery After Surgery ERAS. ANMFDokument17 SeitenEnhanced Recovery After Surgery ERAS. ANMFTaufiqurrahman RizkiNoch keine Bewertungen
- National Vital Statistics ReportsDokument15 SeitenNational Vital Statistics ReportssunnewsNoch keine Bewertungen
- Leiomioma - Miomectomia LaparoscopicaDokument20 SeitenLeiomioma - Miomectomia LaparoscopicaNella SolanoNoch keine Bewertungen
- Hysterectomy - Abdominal - Bilateral - SO PDFDokument2 SeitenHysterectomy - Abdominal - Bilateral - SO PDFkatNoch keine Bewertungen
- Muhs 2013 Winter Time TableDokument70 SeitenMuhs 2013 Winter Time Tablepappu6600Noch keine Bewertungen
- StainsDokument4 SeitenStainsManikanta Chaitanya LokanadhamNoch keine Bewertungen
- Stress UlcerDokument20 SeitenStress UlcerTaufik Akbar Faried LubisNoch keine Bewertungen
- 2002physiciansandnursesGRIEF PDFDokument11 Seiten2002physiciansandnursesGRIEF PDFizza istqmhNoch keine Bewertungen
- Urinary Pics ADokument22 SeitenUrinary Pics A46bwilsonNoch keine Bewertungen
- Terapi Pijat English PDFDokument6 SeitenTerapi Pijat English PDFari dwiNoch keine Bewertungen
- Show Mom HowDokument20 SeitenShow Mom HowWeldon Owen Publishing75% (4)
- Fibroid UterusDokument29 SeitenFibroid UterusrumasadraunaNoch keine Bewertungen
- American Council On Science and Health - Meet Your New Organ - The Mesentery - 2017-02-17Dokument3 SeitenAmerican Council On Science and Health - Meet Your New Organ - The Mesentery - 2017-02-17RovanNoch keine Bewertungen
- Krista L Switzer ResumeDokument2 SeitenKrista L Switzer Resumeapi-247358875Noch keine Bewertungen
- Table : Number of Population, Hospitals and Beds in All Over JordanDokument8 SeitenTable : Number of Population, Hospitals and Beds in All Over JordanjNoch keine Bewertungen
- Facts and Definition of EclampsiaDokument5 SeitenFacts and Definition of EclampsiaChoi Gong JuNoch keine Bewertungen
- Test Taking StrategiesDokument85 SeitenTest Taking StrategiesNyjil Patrick Basilio ColumbresNoch keine Bewertungen