Beruflich Dokumente
Kultur Dokumente
Heart Inflammation
Hochgeladen von
api-3738852Originalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Heart Inflammation
Hochgeladen von
api-3738852Copyright:
Verfügbare Formate
It is clear that inflammation is linked to heart disease, and
that one of the body’s most common sources of inflammation
is periodontal disease. Does poor oral health contribute to
heart disease risk? Although the jury is still out while
scientists investigate this link, here is what we know about
inflammation’s role in atherosclerosis. | BY PETER LIBBY
HeartHealth
INFLAMMATION AGE
IN
THE
O N L Y A D E C A D E A G O, most physicians would have confidently described sometimes fail. It also highlights the
need for better prevention, detection
atherosclerosis as a plumbing problem: Fat-laden gunk gradually builds up on and treatment. In industrialized na-
tions, deaths from heart attacks and
artery walls. If a deposit (plaque) grows large enough, it closes off an affected strokes exceed those from cancer—and
they are also becoming more prevalent
“pipe,” preventing blood flow. Eventually, Such research has established in- in developing countries.
the blood-starved tissue dies. If that flammation’s key role in atherosclerosis.
happens in the heart or the brain, a heart This process—the same one that causes IGNITING TROUBLE
attack or stroke occurs. infected cuts to become swollen, hot we know that inflammation symp-
Few believe that tidy explanation and painful—underlies everything from toms reflect a pitched struggle on a mi-
anymore. Twenty years of research show the creation of plaques to their growth croscopic battlefield. After sensing
that arteries bear little resemblance to and rupture. (rightly or wrongly) a microbial inva-
pipes. They contain living cells that When microbes invade, inflamma- sion, certain types of white blood
communicate with one another and tion (literally meaning “on fi re”) fights cells—the immune system’s frontline
their environment. They also partici- infection. But with atherosclerosis, in- warriors—convene in the threatened
pate in the development of the fatty de- fl ammation proves harmful; our own tissue. There they secrete chemicals to
posits that grow within vessel walls— defenses bombard us with friendly fire, limit infection: oxidants that damage
few which actually shrink vessels to a just as they do in lupus and other auto- invaders and signaling molecules (in-
pinpoint. Most heart attacks and many immune disorders. This revised picture cluding proteins called cytokines) that
M AT T COLLINS
strokes stem from interior plaques that resolves two disturbing mysteries: why orchestrate the activities of defensive
rupture suddenly, spawning a blood clot many heart attacks strike without warn- cells. Their presence in tissue signifies
that blocks blood flow. ing and why preventative therapies an inflammatory response. >>
12 ORAL AND WHOLE BODY HEALTH
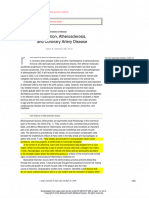
CROSS-SECTION
OF HEALTHY
CORONARY
INFLAMMATION’S MANY ROLES
ARTERY INFLAMMATION—a central player in atherosclerosis—occurs when
white blood cells, the body’s first line of defense against infec-
Blood channel tion, invade and become active in tissue. These diagrams
depict atherosclerotic plaque growth in a coronary
Intima artery; the close-ups highlight some inflam-
matory processes triggered by elevated
Media low-density lipoprotein (LDL) in
the blood.
Adventitia
LOL
T cell Endothelial 1
Monocyte Adhesion
cell
Scavenger Foam
2
molecule receptor cell 3 Blood channel
INTIMA
Modified LOL
Chemokine
Plaque Thrombus
4 5
Microphage Inflammatory
Elastic tissue mediators
MEDIA Smooth muscle cells
BIRTH OF A PLAQUE PLAQUE
PROGRESSION
1 Excess LDL accumulates in
ar tery walls, undergoing
chemical changes. Modified
LDLs stimulate endothelial cells to
display adhesion molecules, which
2 Monocytes mature into active
macrophages in the intima;
with T cells, they produce
inflammatory mediators, including
cytokines that carr y signals
3 The macrophages display
“scavenger receptors” to help
ingest modif ied LDLs;
macrophages feast on them, filling
with frothy, fatty droplets. These
4 Inflammatory
molecules trigger further
plaque growth. A fibrous cap
develops over the lipid core when the
molecules induce smooth muscle
capture circulating monocytes (key between immune system cells and “foam cells” combine with T cells, cells to migrate to the intima surface,
players in inflammation) and T cells factors that promote cell division. comprising the fatty streak—early multiplying and producing a tough,
(immune cells). Endothelial cells atherosclerotic plaque. fibrous matrix that glues cells
also secrete “chemokines,” luring together. The cap makes the plaque
snared cells into the intima. larger and walls it off from the blood.
Cholesterol studies on both animals As LDLs accumulate, their lipids mature into active macrophages, ready
and cultured cells have elaborated in- oxidize—a corrosive process similar to to unleash their weapons against the
flammation’s role in atherosclerosis. Sci- the one that rusts pipes. Cells in the body’s enemies. These warriors set about
entists have long known that although blood vessel wall react to these changes clearing perceived invaders from vessel
we need cholesterol, excessive amounts by calling for reinforcements from the walls. Scavenger receptor molecules cap-
clog arteries. But until recently, no one body’s defense system. Adhesion mole- ture modified LDL particles and help
knew how this happened. Low-density cules on the endothelial cells that line macrophages “eat” them—until they’re
lipoprotein (LDL)—also known as bad vessels latch like Velcro onto mono- so full of fatty droplets that they look
cholesterol—is composed of fatty mol- cytes, inflammatory cells that normally foamy under a microscope, giving them
ecules (lipids) and protein. Its job: trans- circulate in the blood, attaching them to their “foam cell” nickname.
port cholesterol (another lipid) from its artery walls. Endothelial and smooth T lymphocytes (a type of white blood
source in the liver and intestines to other muscle cells inside vessels then secrete cell) also attach themselves to artery
organs. The trouble begins when LDLs chemokines—chemicals that attract walls, releasing cytokines that intensify
from the blood collect in the intima, the monocytes. Much as hounds track the inflammation. The fi rst visible athero-
interior wall of an artery. At low concen- scent of their prey, more monocytes fol- sclerotic lesion, a yellow “fatty streak,”
KEITH K A SNOT
trations in the blood, LDLs can pass in low the chemical trail into the intima. is a mix of foamy macrophages and T
and out of the intima; in excess, LDLs Stimulated by chemokines and other lymphocytes. These lesions are a precur-
become stuck in the cell matrix. substances, the monocytes multiply and sor of the complex plaques that later dis-
14 ORAL AND WHOLE BODY HEALTH
PLAQUE RUPTURE
sel surface. Once there, they form a fi- channel. This also explains why bypass
5 Foam cells secr ete inf lammator y
subs tances that weaken the cap,
digesting matrix molecules and damaging
smooth muscle cells that normally repair it.
Foam cells may produce tissue factor, a potent
brous covering over the original plaque.
Underneath this cap, some foam cells
die, releasing their load of lipids.
surgery or therapies such as angioplasty
or stents that widen obstructed arteries
can ease angina—yet often fail to pre-
Atherosclerotic plaques usually ex- vent a heart attack. Even when blocked
clot-promoter. If the plaque ruptures, a clot
forms. A large clot can halt blood fl ow to the pand outward, not inward to block an arteries are treated, they often clog up
heart, causing a heart attack—the death of artery’s blood-carrying channel. When again fairly quickly—it seems that the
cardiac tissue. they do push in, blood flow to tissues is treatment itself elicits a robust inflam-
restricted, especially when arteries matory response.
Thrombus would normally expand. During exer-
Matrix-degrading
enzyme cise or stress, blood flow through a com- BEYOND BAD CHOLESTEROL
Cytokines that
disrupt smooth promised heart artery fails to meet the several other atherosclerosis risk fac-
muscle cells
Fibrous increased demand. This causes angina tors exhibit intriguing inflammatory fea-
cap
pectoris, a feeling of tightness or pres- tures: diabetes, for instance, elevates
sure usually under the breastbone. Nar- blood sugar levels, which can enhance
rowing in other arteries can cause pain- LDL’s inflammatory properties. Smoking
ful cramping of the calves or buttocks causes oxidants to form, possibly hasten-
during exertion. ing LDL oxidation—and fostering arte-
rial inflammation even in people with
CAUSING CRISES average LDL levels. Obesity contributes
only about 15 percent of heart at- to diabetes and vascular inflammation.
tacks are caused by large plaques that Conversely, high-density lipoprotein
block arteries. Autopsies have shown (HDL) seems beneficial; as levels of this
that most attacks occur after a plaque’s “good cholesterol” decline, the likeli-
fibrous cap ruptures, prompting a blood hood of suffering a heart attack goes up.
clot to develop over the break. Inflamma- HDL may achieve its beneficial effects
tion makes the cap vulnerable. My labo- in part by reducing inflammation, be-
ratory found that when stimulated by cause along with cholesterol, HDL
inflammatory chemicals, macrophages transports antioxidant enzymes that
secrete enzymes that degrade a cap’s break down oxidized lipids.
strong collagen fibers and stop smooth Given inflammation’s usual respon-
CUTAWAY VIEW OF ARTERY
AFFLICTED BY ATHEROSCLEROSIS muscle cells from extruding fresh colla- sibility in the body—blocking and elim-
gen to repair and maintain it. inating infectious agents—biologists
Clots form when blood seeps have wondered whether arterial infec-
through a fi ssure in a cap and coagu- tions might contribute to inflammation
figure arteries. Many Americans begin lates. Although our bodies produce sub- in the arteries. Recent studies suggest
plaque buildup as early as their teens. stances that can prevent or degrade that atherosclerosis can develop in the
blood clots, infl amed plaques release absence of infection. However, circum-
FUELING PLAQUE GROWTH chemicals that impede this clot-busting stantial evidence suggests that certain
when an inflammatory response in, machinery. If a clot does clear naturally microorganisms, such as herpes viruses
say, a scraped knee successfully blocks or with medication, the healing process or the bacterium Chlamydia pneumoni-
infection, macrophages release molecules may kick in once again, restoring the ae could induce or aggravate atheroscle-
that promote healing. A “healing” pro- cap but also enlarging the plaque by rosis. C. pneumoniae appears in many
cess is also part of the chronic, low-level forming scar tissue. Considerable evi- atherosclerotic plaques—and can trig-
inflammation that operates in athero- dence suggests that plaques grow in fits ger inflammatory responses.
sclerosis. But instead of restoring artery and starts as inflammation comes and Infections might also act from a dis-
walls, the process perversely remodels goes and as clots emerge and dissolve. tance, in an “echo effect.” When the
them, generating a bigger plaque. This new picture of atherosclerosis body fights infections, inflammatory me-
Recently, biologists have learned explains why many heart attacks seem diators can escape into the blood and
that both macrophages and cells within to come from out of the blue. Plaques travel to distant sites. Because the mouth
an inflamed vessel wall secrete sub- that rupture may not protrude very far can be a source of chronic infection, re-
stances that create a kind of scar tissue. into a blood channel—and may not searchers are exploring the potential im-
Smooth muscle cells migrate to the ves- cause angina or appear on images of the pact of gum disease. Infection from peri-
ORAL AND WHOLE BODY HEALTH 15
EVALUATING THE DATA:
Could Periodontal Disease Increase the Risk for
Cardiovascular Disease? BY K AUMUDI JOSHIPURA
HEART DISEASE AND PERIODONTAL DISEASE have several loss-induced dietary
things in common. One of them is inflammation, which both narrows changes(e.g.,shunning
coronary arteries and breaks down the tissues that hold teeth in fruits, vegetables and
place. Could periodontal disease increase your risk for developing dietary fiber) that
heart disease, perhaps due to bacterial pathogens or inflammatory increase heart risks.
chemicals carried by the blood from the mouth to the heart? If so, The link between the
could you reduce your heart disease risk by preventing or treating two diseases may
periodontal disease? derive from factors that
Research suggests that there may be links between the two influence both. For
conditions. Animal studies in particular offer provocative evidence example, cigarette
that certain biologic pathways might allow one disease to influence smoking is a major risk
the other. Periodontal bacteria are found in the plaque deposits that factor for heart disease
narrow coronary arteries; inducing periodontal disease in rabbits and for periodontal
causes plaque accumulations in their coronary arteries. disease, and a genetic
Other evidence comes from observational human studies. The sus c ep tibili ty to
largest such study, the National Health and Nutrition Examination inflammation might
Survey (NHANES), involved 10,000 Americans between the ages of 18 cause someone to develop both diseases (see chart).
and 74. It found that people with periodontal disease were much more Although periodontal disease seems to be associated with heart
likely to be diagnosed with heart disease than those without disease, more studies are needed before we can say with certainty
periodontal disease. that one disease actually causes the other. Meanwhile, everyone
Not all studies have yielded similar results. For example, my colleagues should be conscientious about treating gum disease, but it is not yet
and I examined a group of health care professionals and failed to find an clear that doing so will protect you from heart disease. •
overall association. Interestingly, our study and several others did detect
a significant association between tooth loss (often a result of severe KAUMUDI JOSHIPURA is director of the Division of Dental Public
periodontal disease) and heart disease. So the “connection” between Health at the University of Puerto Rico and also teaches at Har-
periodontal disease and heart disease may be indirect, involving tooth- vard University.
odontal disease pumps a continuous flow measuring the heat of blood vessels (be- tion’s ability to ward off infection out-
of bacteria and cytokines into the blood- cause heat normally accompanies in- weighed its drawbacks. Today, as we live
stream. Bacteria also produce toxins that flammation); and altering existing im- longer, exercise less, eat too much, and
can trigger inflammatory responses. Cy- aging technologies, such as MRI or CT smoke, many of us suffer from inflam-
tokines and bacterial toxins can stimu- scans, to improve their ability to peer mation’s dark side—including its ability
late the white cells in atherosclerotic inside vessel walls. Scientists are trying to contribute to atherosclerosis and other
plaques, prompting plaque growth or to develop molecular imaging tech- chronic disorders. Scientists continue to
rupture. Despite these links between in- niques to “visualize” biological process- pursue a deeper understanding of in-
fection and atherosclerosis, current clin- es such as infl ammation, looking be- flammation’s role in atherosclerosis, and
ical evidence does not support the use of yond the anatomical features of blood to decipher the intricate interactions that
antibiotics to prevent recurrent compli- vessels. Geneticists are hunting for genes ignite and drive the inflammatory pro-
cations following a heart attack. that predispose some people to chronic cesses in the arteries. These insights
inflammation and atherosclerosis so should enable us to make further inroads
TOWARD EARLY DETECTION they can seek more aggressive monitor- against a disease with growing world-
noninvasive methods for identifying ing and treatment. wide impact that causes extensive dis-
vulnerable plaques might help pinpoint For most of human history, inflamma- ability and takes far too many lives. •
at-risk individuals who lack warning
signs of potential heart attack or stroke. PETER LIBBY, who earned his M.D. from the University of California, San Diego, is chief of
Ideas include testing for elevated levels cardiovascular medicine at Brigham and Women’s Hospital, Mallinkrodt Professor of
of C-reactive protein, a substance in the Medicine at Harvard Medical School, and co-editor of Heart Disease, a classic cardiology
blood that signifies acute inflammation; textbook (W.B. Saunders, 2001).
16 ORAL AND WHOLE BODY HEALTH
Das könnte Ihnen auch gefallen
- Pathology For The Health Professions 5th Edition Damjanov Solutions ManualDokument25 SeitenPathology For The Health Professions 5th Edition Damjanov Solutions ManualKevinRobertsbfak98% (56)
- Healing Power of Sunlight by Jakob LorberDokument34 SeitenHealing Power of Sunlight by Jakob LorberEtiandro MarcosNoch keine Bewertungen
- Mike Mahler - Live Life Aggressively! What Self-Help Gurus Should Be Telling YouDokument263 SeitenMike Mahler - Live Life Aggressively! What Self-Help Gurus Should Be Telling Youbobsyaruncle4814100% (5)
- Fundamentals or Nursing ExamDokument18 SeitenFundamentals or Nursing Examapi-371817494% (16)
- Hormones Affecting Your Health Fat LossDokument14 SeitenHormones Affecting Your Health Fat Lossivan2504100% (8)
- Jurding DR SaugiDokument44 SeitenJurding DR SaugiDian FitriNoch keine Bewertungen
- Atherosclerosis: CH ApterDokument22 SeitenAtherosclerosis: CH ApterAnonymous mmA06fqNEdNoch keine Bewertungen
- Maynard Sam Lazo 2B-UstfmsDokument8 SeitenMaynard Sam Lazo 2B-UstfmsAnonymous HH3c17osNoch keine Bewertungen
- The Pathophysiology of Acute Coronary SyndromesDokument6 SeitenThe Pathophysiology of Acute Coronary SyndromesTulisan NonaNoch keine Bewertungen
- The Biology of Atherosclerotic Cardiovascular DiseaseDokument62 SeitenThe Biology of Atherosclerotic Cardiovascular DiseaseNovia HartantiNoch keine Bewertungen
- Tinywow - L.3 Condorelli Atherosclerosis - 28139364Dokument14 SeitenTinywow - L.3 Condorelli Atherosclerosis - 28139364filymascoloNoch keine Bewertungen
- The Wound Module: Excerpt FromDokument7 SeitenThe Wound Module: Excerpt Fromandres mesaNoch keine Bewertungen
- Concept of Inflammatory and Immune SystemDokument15 SeitenConcept of Inflammatory and Immune SystemUchiha Dominic100% (1)
- T11. Natural Defenses Against DiseaseDokument26 SeitenT11. Natural Defenses Against DiseaseTitular De la cuentaNoch keine Bewertungen
- GFCH Internal Treatment of TraumaDokument24 SeitenGFCH Internal Treatment of TraumaAndré LourivalNoch keine Bewertungen
- Lecture 7 - Atherosclerosis and Ischemic Heart DiseaseDokument39 SeitenLecture 7 - Atherosclerosis and Ischemic Heart Diseasemayag3243Noch keine Bewertungen
- Interleukin-17 and Atherosclerotic Vascular DiseaseDokument3 SeitenInterleukin-17 and Atherosclerotic Vascular DiseaseAdrián Asael Rodriguez CortesNoch keine Bewertungen
- Patogenesis AterosklerosisDokument3 SeitenPatogenesis AterosklerosisMarsella Epifania SuwignyoNoch keine Bewertungen
- Compiled Patho ExercisesDokument7 SeitenCompiled Patho ExercisesAnonymous HH3c17osNoch keine Bewertungen
- Physiology: Anatomy LectureDokument4 SeitenPhysiology: Anatomy Lecturewesrdftyghuijkol wasedrftgyhuijkolNoch keine Bewertungen
- Semana 6 AteroesclerosisDokument5 SeitenSemana 6 AteroesclerosisrobertoNoch keine Bewertungen
- 1 s2.0 S0092867422004007 Main PDFDokument16 Seiten1 s2.0 S0092867422004007 Main PDFPrecious IJNoch keine Bewertungen
- Inflammation PPT - OdpDokument82 SeitenInflammation PPT - OdpBhanu PraseedhaNoch keine Bewertungen
- Essential of Special Patholog by DR Zair Hassan: December 2015Dokument271 SeitenEssential of Special Patholog by DR Zair Hassan: December 2015pdf pediatriNoch keine Bewertungen
- Role of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CDokument10 SeitenRole of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CMarianne Dennesse100% (1)
- The Internal Treatment of Traumatic InjuryDokument24 SeitenThe Internal Treatment of Traumatic Injuryyevgenfomin7Noch keine Bewertungen
- Inflammation Inflammatory Response and FeverDokument5 SeitenInflammation Inflammatory Response and FeverPrincess Denice OrtalezaNoch keine Bewertungen
- Inflammation and RepairDokument34 SeitenInflammation and Repairanshum guptaNoch keine Bewertungen
- Events in Acute InflammationDokument4 SeitenEvents in Acute InflammationChoky ArdynNoch keine Bewertungen
- InflammationDokument83 SeitenInflammationpriyaNoch keine Bewertungen
- Patologi AnatomiDokument26 SeitenPatologi AnatomiNia AnestyaNoch keine Bewertungen
- Tiomico - BSP 2A - Tissue RepairDokument14 SeitenTiomico - BSP 2A - Tissue RepairpiescesNoch keine Bewertungen
- Cells 10 00226Dokument26 SeitenCells 10 00226spraptamaNoch keine Bewertungen
- Peña Stiven Bahamon Carolina Fragoso Angela Ortega KarolDokument15 SeitenPeña Stiven Bahamon Carolina Fragoso Angela Ortega KarolGledys PissiottiNoch keine Bewertungen
- Inflammation 2Dokument21 SeitenInflammation 2Umar'Farouq OniNoch keine Bewertungen
- Lecture 3Dokument56 SeitenLecture 3w2tz2qrqxdNoch keine Bewertungen
- Histopathology - c3 - Acute and Chronic Inflammation - MasterDokument28 SeitenHistopathology - c3 - Acute and Chronic Inflammation - MasterGhinescu AdrianNoch keine Bewertungen
- SICA FisiopatologiaDokument11 SeitenSICA Fisiopatologiaselene Mendez JuarezNoch keine Bewertungen
- Vascular Endothelium e Gatekeeper of Vessel Health: AtherosclerosisDokument17 SeitenVascular Endothelium e Gatekeeper of Vessel Health: AtherosclerosisLia FitriaNoch keine Bewertungen
- A M - P II: B V B C: Molecular MedicineDokument3 SeitenA M - P II: B V B C: Molecular MedicineEyip SinayNoch keine Bewertungen
- Tutorial Case Report Case 3 Cvs ACS STEMI Inferior With LHF As Complication and First Degree AV BlockDokument47 SeitenTutorial Case Report Case 3 Cvs ACS STEMI Inferior With LHF As Complication and First Degree AV Blockcoas 17Noch keine Bewertungen
- NeuroiflammationDokument9 SeitenNeuroiflammationGabrielaNoch keine Bewertungen
- DB13 - Pathophysiology of AtherosclerosisDokument2 SeitenDB13 - Pathophysiology of Atherosclerosisi_vhie03Noch keine Bewertungen
- Chapter 2 Basicc Immunology Ppts DZ 2010Dokument85 SeitenChapter 2 Basicc Immunology Ppts DZ 2010TofikNoch keine Bewertungen
- New InflammationDokument135 SeitenNew Inflammation77 Weam AliNoch keine Bewertungen
- Inflammation in Atherosclerosis: History of DiscoveryDokument8 SeitenInflammation in Atherosclerosis: History of DiscoveryFarras Amany HusnaNoch keine Bewertungen
- Atherosclerosis: Jana NovotnáDokument28 SeitenAtherosclerosis: Jana Novotnásunita_aug801Noch keine Bewertungen
- 101 - PDFsam - Robbins & Cotran Pathologic Basis of Disease, 9eDokument20 Seiten101 - PDFsam - Robbins & Cotran Pathologic Basis of Disease, 9eRizky Angga PerdanaNoch keine Bewertungen
- Chap. 2Dokument34 SeitenChap. 2NadineNoch keine Bewertungen
- Basic Biology of The Cardiovascular SystemDokument12 SeitenBasic Biology of The Cardiovascular SystemangelNoch keine Bewertungen
- Nutrition and AtherosclerosisDokument19 SeitenNutrition and AtherosclerosisJOSE RICARDO LOPEZ PALESTINANoch keine Bewertungen
- InflammationDokument117 SeitenInflammationPraiseNoch keine Bewertungen
- Week 4 - Drugs Acting On The Immune SystemDokument16 SeitenWeek 4 - Drugs Acting On The Immune SystemDino MicaNoch keine Bewertungen
- The Cardiovascular Atherosclerotic Disease Is One of The Causes of Mortality and Economic BurdenDokument14 SeitenThe Cardiovascular Atherosclerotic Disease Is One of The Causes of Mortality and Economic BurdenBryantNoch keine Bewertungen
- I. Inflammatory MsDokument2 SeitenI. Inflammatory Mslalisa manobanNoch keine Bewertungen
- Inflammation, Wound Healing and Foreign Body ResponseDokument22 SeitenInflammation, Wound Healing and Foreign Body Responseharry potterNoch keine Bewertungen
- Group Work: Write Up Activity 5 - Non Specific Defenses: What Are The Different Stages of Phagocytosis?Dokument9 SeitenGroup Work: Write Up Activity 5 - Non Specific Defenses: What Are The Different Stages of Phagocytosis?Marson RosaritoNoch keine Bewertungen
- The Journey of LeukocytesDokument12 SeitenThe Journey of LeukocytesNauzaina IjazNoch keine Bewertungen
- Inflammation, Atherosclerosis, and Coronary Artery Disease: Review ArticleDokument11 SeitenInflammation, Atherosclerosis, and Coronary Artery Disease: Review ArticleEduardo PeñaNoch keine Bewertungen
- SG 4,5,6Dokument20 SeitenSG 4,5,6Itadori YujiNoch keine Bewertungen
- 13 - Atherosclerotic Plaque HealingDokument12 Seiten13 - Atherosclerotic Plaque HealingAndres Felipe Hurtado BautistaNoch keine Bewertungen
- The Cell Cycle: Chapter 2: Cellular ReproductionDokument1 SeiteThe Cell Cycle: Chapter 2: Cellular ReproductionJielyn AnneNoch keine Bewertungen
- The Immune System: Dr. Anuar Sani FPSK UsimDokument35 SeitenThe Immune System: Dr. Anuar Sani FPSK Usimcikgu_baruNoch keine Bewertungen
- A Simple Guide to the Blood Cells, Related Diseases And Use in Disease DiagnosisVon EverandA Simple Guide to the Blood Cells, Related Diseases And Use in Disease DiagnosisNoch keine Bewertungen
- Defeating Depression in Just Minutes A DayDokument52 SeitenDefeating Depression in Just Minutes A DaydrkapilkohliNoch keine Bewertungen
- Resources Baby Boomer ConfDokument24 SeitenResources Baby Boomer Confapi-3738852Noch keine Bewertungen
- Herb IndexDokument34 SeitenHerb Indexapi-3738852100% (1)
- Voucher TopamaxDokument2 SeitenVoucher Topamaxapi-3738852100% (1)
- Diagnosis Unknown EbookDokument252 SeitenDiagnosis Unknown Ebookapi-3738852Noch keine Bewertungen
- Illuminati Formula Chapters3 Mind DrugsDokument16 SeitenIlluminati Formula Chapters3 Mind Drugsapi-3738852Noch keine Bewertungen
- NLP - Peter Shepard - Know Your Own Mind (Personality Questionnaire)Dokument134 SeitenNLP - Peter Shepard - Know Your Own Mind (Personality Questionnaire)fannyblumNoch keine Bewertungen
- MestastaseDokument10 SeitenMestastaseCahyono YudiantoNoch keine Bewertungen
- The Role of Cytokines in Orthodontic Tooth MovemenDokument17 SeitenThe Role of Cytokines in Orthodontic Tooth MovemenvivigaitanNoch keine Bewertungen
- Azzi1983bone ESCANEADODokument5 SeitenAzzi1983bone ESCANEADOCristhian BurbanoNoch keine Bewertungen
- Ultimate Fountain of Youth ProtocolDokument12 SeitenUltimate Fountain of Youth ProtocolChristian100% (1)
- Bio Energetic TherapyDokument19 SeitenBio Energetic TherapyVishnu Moorthy Raja Singam100% (2)
- Inhalers in Pediatric AsthmaDokument53 SeitenInhalers in Pediatric AsthmaKishore Chandki100% (2)
- Robbins & Cotran Pathologic Basis of Disease - With STUDENT CONSULT Online Access, 8e (PDFDrive - Com) - 89-105Dokument17 SeitenRobbins & Cotran Pathologic Basis of Disease - With STUDENT CONSULT Online Access, 8e (PDFDrive - Com) - 89-105bgfhnfgNoch keine Bewertungen
- Ashwagandha: Somnifera, and It's Also Known by Several Other Names, Including Indian GinsengDokument17 SeitenAshwagandha: Somnifera, and It's Also Known by Several Other Names, Including Indian GinsengJef BarrettNoch keine Bewertungen
- Metabolic ResponseDokument22 SeitenMetabolic ResponsenelsonNoch keine Bewertungen
- Diseases of Poultry - COBBDokument17 SeitenDiseases of Poultry - COBBRinaldy ManurungNoch keine Bewertungen
- Immunomodulation Mediated by Azithromycin in Experimental Periapical in AmmationDokument7 SeitenImmunomodulation Mediated by Azithromycin in Experimental Periapical in AmmationARUNA BharathiNoch keine Bewertungen
- Address The StressDokument5 SeitenAddress The Stresstodoroff71Noch keine Bewertungen
- Elemental Zinc H H CapsulesDokument5 SeitenElemental Zinc H H CapsulesArunjyothi pNoch keine Bewertungen
- Micro Lec Ars Sessions 17 23Dokument9 SeitenMicro Lec Ars Sessions 17 23rica sebabillonesNoch keine Bewertungen
- Path Important Questions CompatibleDokument12 SeitenPath Important Questions Compatiblecarol_nditaNoch keine Bewertungen
- A Study On The Effects of Smoking On Serum Creactive Protein, Complete Blood Counts and Magnesium Levels Among Healthy Adult Male SmokersDokument4 SeitenA Study On The Effects of Smoking On Serum Creactive Protein, Complete Blood Counts and Magnesium Levels Among Healthy Adult Male SmokersiajpsNoch keine Bewertungen
- Nicola Maffulli (Eds.) - Platelet Rich Plasma in Musculoskeletal Practice-Springer-Verlag London (2016) PDFDokument256 SeitenNicola Maffulli (Eds.) - Platelet Rich Plasma in Musculoskeletal Practice-Springer-Verlag London (2016) PDFedbraga-1Noch keine Bewertungen
- Peran Vitamin B6 Terhadap Inflamasi Pada Adhesi Peritoneal Pasca Laparotomi: Tinjauan PustakaDokument7 SeitenPeran Vitamin B6 Terhadap Inflamasi Pada Adhesi Peritoneal Pasca Laparotomi: Tinjauan PustakaDiBi DBNoch keine Bewertungen
- NCP Rheumatoid Arthritis DX IpmDokument2 SeitenNCP Rheumatoid Arthritis DX IpmPatty RomeroNoch keine Bewertungen
- Neutrophilic Urticarial Dermatosis As A Presenting Feature of Systemic Juvenile Idiopathic ArthritisDokument3 SeitenNeutrophilic Urticarial Dermatosis As A Presenting Feature of Systemic Juvenile Idiopathic Arthritismaya_fitrianaNoch keine Bewertungen
- JAP321 Test Prep 9Dokument4 SeitenJAP321 Test Prep 9BartNoch keine Bewertungen
- Joyce Y. Visitacion NCM 104 Bsn-4Aj SY 2008-2009 Musculoskeletal SystemDokument33 SeitenJoyce Y. Visitacion NCM 104 Bsn-4Aj SY 2008-2009 Musculoskeletal Systemyawdle100% (6)
- ANAPHY Lec Session #17 - SAS (Agdana, Nicole Ken)Dokument9 SeitenANAPHY Lec Session #17 - SAS (Agdana, Nicole Ken)Nicole Ken AgdanaNoch keine Bewertungen
- Capobianco ChapmansReflexes PDFDokument63 SeitenCapobianco ChapmansReflexes PDFxavi5_5100% (1)
- Understanding Recovery: A Wound Healing Model: by Dave StaplinDokument3 SeitenUnderstanding Recovery: A Wound Healing Model: by Dave StaplinluckydexxxNoch keine Bewertungen
- Aggressive PeriodontitisDokument101 SeitenAggressive Periodontitisdileep900100% (1)
- Host Modulation Therapy An Updated ReviewDokument4 SeitenHost Modulation Therapy An Updated Reviewpaper kitaNoch keine Bewertungen