Beruflich Dokumente
Kultur Dokumente
NCP PSH
Hochgeladen von
Margareth OrtizOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
NCP PSH
Hochgeladen von
Margareth OrtizCopyright:
Verfügbare Formate
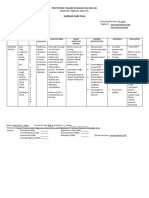
DATE:__________________________ NURSING CARE PLAN ASSESSMENT NURSING DIAGNOSIS Acute urinary retention related to enlarged prostate as evidence by dribbling
of urine secondary to benign prostatic hypertrophy. Definition: Incomplete emptying of the bladder. SCIENTIFIC REFERENCE Benign Prostatic Hyperplasia characterized by progressive enlargement of the prostate gland (commonly seen in men older than 50 years old), causing varying degrees of urethral obstruction and restriction of urinary flow. GOAL/ OBJECTIVES That after 8 hours of comprehensive nursing intervention, patient will be able to; Void in sufficient amount, for at least 30-60 cc/hr with no palpable bladder distention. INTERVENTION RATIONALE EVALUATION
Subjective cues
Objective cues
Gagmay akong ihi, as verbalized by the patient. putol-putol ug ginagmay ang pag pangihi ni papa, as verbalized by the daughter.
Dribbling urine as verbalized by the daughter of the patient. Bladder distention.
Maintained accurate intake and output measurement. Drained accurately cystoclysis output from urobag every hour as ordered. Established catheter patency.
Loss of kidney function results in decrease fluid elimination and accumulation of toxic waste may progress to complete renal shutdown. To maintain free flowing drainage and fluid volume excess To prevent ascending urinary tract infection and maintaining free flow of the drain.
After 8 hours of comprehensive nursing intervention, patient was able to; Void sufficiently with a urinary output of 60-220 ml/hr.
Ensured the prevention of the backflow of the drain Collaborative: Underwent TURP procedure last September 26, 2011.
Source: Doenges, Marilynn E. ,et. al., Nursing Care Plans., 7th
Source: Doenges, Marilynn E. ,et. al., Nursing Care Plans., 7th Edition., 2006
Done to relieve urinary symptoms by removing a portion of the prostate gland immediately surrounding the
DATE:__________________________ Edition., 2006 urethra
DATE:__________________________ NURSING CARE PLAN ASSESSMENT NURSING DIAGNOSIS Deficient knowledge related to lack of specific to necessary information for client and SO to make informed choices regarding condition, treatment and lifestyle changes.. SCIENTIFIC REFERENCE Benign Prostatic Hyperplasia is characterized by progressive enlargement of the prostate gland (commonly seen in men older than 50 years old), causing varying degrees of urethral obstruction and restriction of urinary flow. GOAL/ OBJECTIVES That after 8 hours comprehensive nursing care patient and significant others will be able to; verbalize understanding of disease process/ prognosis and potential complications. INTERVENTION RATIONALE EVALUATION
Subjective cues Sige ug sinusitison akong papa nya tagaan namu siya ug Sinutab taga mutukar. Mao man ni siya nagkainingon ani tungod sa Sinutab, as verbalized by the daughter.
Objective cues
Reviewed disease process and clients information.
Patient and SO are asking questions regarding the causes of his condition. Statement of misconception. Inaccurate treatment of perceived condition.
Provides knowledge base from which client can make informed therapy choices. Helping client work through feeling can be vital to rehabilitation. May cause prostatic irritation with resulting congestion.
Encouraged verbalization of patients fears and concerns.
After 8 hours comprehensive nursing care patient and significant others was able to; verbalize understanding of disease process/ prognosis and potential complications.
Recommended avoiding spicy foods, coffee, alcohol, rapid intake of fluids. Instructed significant other/s to report any signs of unusualities (eg fever, chills, diminished urine output) to healthcare providers immediately.
Definition: Absence or deficiency of cognitive information related to specific topic. Source: Doenges, Marilynn E. ,et. al., Nursing Care Plans., 7th Edition., 2006
Prompt interventions may prevent more serious complications.
Source: Doenges, Marilynn E. ,et. al., Nursing
DATE:__________________________ Care Plans., 9th Edition., 2006 Dependent: Requested the ROD to explain to the patient the entire disease process and his condition. To provide accurate information regarding the condition.
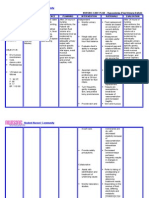
DATE:__________________________ NURSING CARE PLAN ASSESSMENT NURSING DIAGNOSIS Activity intolerance related to functional changes accompanying aging secondary to Benign Prostatic Hyperplasia. Definition: Insufficient physiological energy to endure or complete required or desired daily activities. SCIENTIFIC REFERENCE Benign Prostatic Hyperplasia in characterized by progressive enlargement of the prostate gland (commonly seen in men older than 50 years old), causing varying degrees of urethral obstruction and restriction of urinary flow. GOAL/ OBJECTIVES That 8 hours of comprehensive nursing care patient will be able to; participate in exercise and social activities to the extent possible. INTERVENTION RATIONALE EVALUATION
Subjective cues
Objective cues 68 y.o Unable to tolerate prolonged sitting and standing Reports of fatigue or weakness upon exertion of activities Exertional discomfort Inability to maintain usual routine Lethargic
Clustered nursing care and adjust activities within limits of tolerance
Sige rakog higda, as verbalized by the patient.
To provide adequate rest periods and prevent overexertion. To increase stamina and enhance ability to participate in activity. Enhance ability to participate in activity to improve strength. Helps identify or monitor degree of fatigue and potential for complications. To help improve his quality life.
Encouraged patient to become involved in simple exercise such as walking and assist with ADLS. Adjust activities, reduce intensity level or discontinued as needed. Monitor response to activity including BP, pulse, respiratory rate, skin color and behavior. Establish realistic goals for improving patients activity
That 8 hours of comprehensive nursing care patient was able to participate in simple exercise to the extent possible.
kinahanglan jud niya ug kuyog kung magbakonbakon ug mubalik ra pud ug higda dayon kay daling kapuyon as verba;lized by the daughter.
That after 1 week of comprehensive nursing care patient will be able to; tolerate prolong sitting and standing
That after 1 week of comprehensive nursing care patient will be able to; tolerate prolong sitting and standing and perform basic ADLS.
Source: Doenges, Marilynn E. ,et. al., Nursing Care Plans., 9th Edition., 2006
Source: Doenges, Marilynn E. ,et. al., Nursing Care Plans., 7th Edition., 2006
DATE:__________________________ level, considering his physical limitations and energy level.
DATE:__________________________ NURSING CARE PLAN ASSESSMENT NURSING DIAGNOSIS Risk for infection related to urine stasis as evidenced by decreased urine output secondary to Benign Prostatic Hyperplasia. Definition: At increased risk of being invaded by pathogenic organisms. SCIENTIFIC REFERENCE Benign Prostatic Hyperplasia in characterized by progressive enlargement of the prostate gland (commonly seen in men older than 50 years old), causing varying degrees of urethral obstruction and restriction of urinary flow that will cause urine stasis which can contribute to bacterial growth. GOAL/ OBJECTIVES That after 8 hours of comprehensive nursing care patient will be able to; Be free from infection; and identify interventions to prevent/ reduce risk of infection. Long Term: Patients significant others will know the ways to prevent ascending infection and observe proper aseptic technique. INTERVENTION RATIONALE EVALUATION
Subjective cues
Objective cues With cystoclysis attached to uroguard draining blood tinged urine
Monitored vital signs for fever.
Indicators of sepsis requiring prompt evaluation and intervention. Reduces risk of cross contamination. Prevents exposure to infectious organism. To prevent contamination that would promote further complication.
Observed careful handling of patient and thorough hand washing. Provided clean and freshly laundered bed linens/ gowns. Instructed patients SO to wash hands frequently before handling patient and making sure the environment is always clean. Ensured the placement of the urobag.
After 8 hours of comprehensive nursing care management patient was; free from any signs of infection; and the SO was able to identify interventions to prevent/ reduce risk of infection.
Source: Doenges, Marilynn E. ,et. Al., Nursing Care Plans., 9th Edition., 2006
Source: Doenges, Marilynn E. ,et. Al., Nursing Care Plans., 7th Edition., 2006
To prevent ascending UTI and maintaining the flow of the drain. Reduces bacterial
Promoted
DATE:__________________________ meticulous perianal care. colonization.
Dependent: Administered Vigocid 2.25 g IVTT every 8 hours. To treat existing infection and prevent any further infection.
DATE:__________________________ NURSING CARE PLAN ASSESSMENT NURSING DIAGNOSIS Sleep pattern disturbance related to medical regimen as evidence by vital signs monitoring every hour secondary to essential hypertension. Definition: Time limited disruption of sleep amount and quality. SCIENTIFIC REFERENCE Clients with sleeping problems have difficulty falling asleep or difficulty staying asleep. Various factors may be involved. These include frequent changes in sleep time, changes in sleep environment, physical discomfort or pain, or anxiety about actual or anticipated loss. GOAL/ OBJECTIVES After 8 hours of nurse-patient interventions the patient will be able to: >verbalize understanding of sleep disturbance >identify individually appropriate interventions to promote sleep Long Term: Patient will be able to sleep during uninterrupted night time and wakes up during day time. INTERVENTION RATIONALE EVALUATION
Subjective cues dili ko katulog magbii as verbalized by the patient.
Objective cues Dark circles noted around the eyes Appears weak Noted frequent yawning
Noted waking and sleeping hours. Discussed or implemented effective age appropriate bed time rituals such as going to bed at same time each night, drinking warm milk and switching on dim lights. Limited intake of chocolate and caffeinated drinks.
To assess patients sleeping pattern Enhance clients ability to fall asleep, reinforce that bed is a place to sleep
After 8 hours of nurse-patient interventions the patient was able to verbalize that the interventions done here in the hospital are important.
di mani siya matulog ug gabie, sa buntag man ni siya matulog, as verbalized by the daughter.
Asleep during the day until 2pm Monitor vital sign such as BP, TPR every hour
To assist patient to establish optimal sleep or rest patterns
Source: Doenges, Marilynn E. ,et. al., Nursing Care Plans., 9th Edition., 2006
Encouraged to avoid afternoon naps.
Source: (Kozier, et. al. Fundamentals of Nursing, 7th ed. page 1122).
Napping in the afternoon can disrupt normal sleep pattern To promote minimal interruption and enhance sleep or
Clustered fast and organized care and visited at intervals; observed silence at
DATE:__________________________ all times during patients visit, close the door slowly. rest
DATE:__________________________ ASSESSMENT NURSING DIAGNOSIS SCIENTIFIC REFERENCE GOAL/ OBJECTIVES INTERVENTION RATIONALE EVALUATION
Subjective cues
Objective cues
DATE:__________________________ ASSESSMENT Subjective Kanus-a ni tangtangon ang mga tubo sa askon ihi? as verbalized by patient. Objective Insomnia NURSING DIAGNOSIS SCIENTIFIC REFERENCE Vague and easy feeling of discomfort or dread accompanied by an autonomic response: a feeling of apprehension caused by anticipation of danger. It is an altering signal that warns of impending danger and enables the individual to take measures to deal with threat. Source: (Kozier, et. al. Fundamentals of Nursing, GOAL/ OBJECTIVES After 8 hours of nurse-patient interaction the patient will be able to: >appear relax and report that anxiety is reduced After 2 days: >verbalized awareness of feelings of anxiety >use resources or support system effectively >identify healthy ways to deal with and express anxiety
INTERVENTION Established a therapeutic relationship conveying empathy and conditional positive regard. Encouraged verbalization of feelings and discomforts. Instructed to have breathing exercises and provided comfort measures such as calm environment, well lit room and television. Provided accurate information about the Identify healthy ways to deal with and express anxiety Dependent: Let the ROD explain to the patient the disease process and
RATIONALE It will encourage client to acknowledge and to express feelings To assist client to identify feelings and begin to deal with problems. Promotes relaxation and diverts the attention of the client
EVALUATION After 8 hours of nurse-patient interaction the patient was relaxed and showed a good response by participating well during procedures
Mild Anxiety related to Sleep change in disturbances health status secondary to Worried the disease process Expressed concerns Definition: about Vague changes. uneasy feeling of discomfort or dread accompanied by an autonomic response Source: Doenges, Marilynn E. ,et. al., Nursing Care Plans., 9th Edition., 2006
Helps client identify what is reality based.
To be aware of the disease process and the
DATE:__________________________ 7th ed. page 1122). his condition. possible changes in health status.
DATE:__________________________ ASSESSMENT NURSING Subjective Objective DIAGNOSIS Dili kaayo ko ganahan mukaon karon as verbalized by the patient with loss of appetite food served not taken reported altered taste sensation lack of interest in food Imbalanced Nutrition: less than body requirements related to loss of appetite. Definition: Intake of nutrients insufficient to meet metabolic needs.
SCIENTIFIC REFERENCE Intake of nutrients insufficient to meet metabolic needs. Adequate nutrition is necessary to meet the bodies demands nutritional status can be affected by disease or injury states; physical factors; social factors; psychological factors. During times of illness adequate nutrition place an important role in healing and recovery.
GOAL/ INTERVENTION OBJECTIVES After 8 hours of nursing intervention, the patient will have an increase in appetite and will consume the food provided to him Noted total daily intake, patterns and times of eating. RATIONALE To reveal changes that should be made in clients dietary intake To stimulate appetite EVALUATION After 8 hours of comprehensive nursing interventions, the patient was able to have an increase in appetite, consumed the food provided to him.
Encouraged patient to choose foods that are appealing to him Promoted pleasant, relaxing environment, including socialization Minimized unpleasant odors and sights Encouraged to wash mouth before and after meals.
To enhance intake
May have a negative effect on appetite. Eliminating unpleasant taste may enhance appetite. Hesitation to eat may be result of fear that food will cause exacerbation of symptoms
Source: Doenges, Marilynn E. ,et. al., Nursing Care Plans., 9th Edition., 2006
Encouraged patient to verbalize feelings concerning resumption of diet.
DATE:__________________________ ASSESSMENT Subjective Gi operahan ko unya gi butangan ko ug tubo para sa paglimpyo sa akong dugo ug para sa akong ihi, as verbalized by the patient. Objective presence of surgical incision at the right femoral area for Hemodiaysis with intact ; dry dressing with cystoclysis incision at right suprapubic area attached to uroguard draining bloodtinged urine NURSING DIAGNOSIS Impaired skin integrity related to a break of continuity of the skin secondary to AV shunt incision and cystoclysis. SCIENTIFIC REFERENCE Benign Prostatic Hyperplasia in characterized by progressive enlargement of the prostate gland (commonly seen in men older than 50 years old), causing varying degrees of urethral obstruction and restriction of urinary flow that will cause urine stasis which can contribute to bacterial growth. GOAL/ OBJECTIV ES After 1 whole shift (8 hours) of nursing interventio n the patient will be able to maintain dry intact dressing and prevent itchiness.
INTERVENTION
RATIONALE
EVALUATION
Assessed the skin of patient and noted for skin turgor and color
establishes a comparative baseline for a timely intervention To assess for signs of infection Moisture may contribute to skin maceration and itching Removes waste products from skin while preventing skin dryness. May decrease skin irritation and need for scratching To prevent occurrence of ulcers. Prevents skin excoriation and infection from scratching.
Inspect incision sites for any signs of infection. Encouraged patient and SO to keep a wellventilated room.
Definition: Altered epidermis or dermis. Source: Doenges, Marilynn E. ,et. al., Nursing Care Plans., 9th Edition., 2006
Provide frequent skin care and to avoid soaps and alcohol-based lotions
After 1 whole shift (8 hours) of nursing intervention, the patient still has intact Right femoral catheter, clean and dry dressing.
Recommended to patient and SO to avoid harsh detergents.
Encouraged ambulation as tolerated
Advised patient and SO to keep fingernails short and smooth.
DATE:__________________________ ASSESSMENT NURSING DIAGNOSIS Impaired physical mobility related to presence of blood in the urine secondary to cystoclysis. SCIENTIFIC REFERENCE Benign Prostatic Hyperplasia characterized by progressive enlargement of the prostate gland (commonly seen in men older than 50 years old), causing varying degrees of urethral obstruction and restriction of urinary flow. GOAL/ OBJECTIVES That after 8 hours of nursing intervention, patient will be able to understand the medical management and to know that blood in the urine is normal. INTERVENTION RATIONALE EVALUATION
Subjective cues Sige Rako anig higda, as verbalized by the patient
Objective cues On bed always With ongoing cyctoclysis of PNSS 1L attached to uroguard Blood-tinged urine noted on the uroguard upon moving
Independent: Explained that presence of blood in the urine is temporary and normal due to operation, (CTURP) Encouraged to perform ROM exercises. To relieved patients anxiety and know the post-op consideration of C-TURP. To help patient realized and understand that activities are encouraged. Prevents incidence of skin and respiratory complication. Refocuses attention, enhances diets sense of control and self worth.
After 8 hours of nursing intervention patient was able to ambulate with assistance to and from the comfort room.
Repositioned periodically and encouraged coughing and deep breathing exercises. Encouraged participation in divertional activities (wathching television)
Source: Doenges, Marilynn E. ,et. al., Nursing Care Plans., 9th Edition., 2006
DATE:__________________________
Das könnte Ihnen auch gefallen
- NCP Risk For InfectionDokument6 SeitenNCP Risk For InfectionCazze SunioNoch keine Bewertungen
- NCP PryllDokument6 SeitenNCP PryllpjcolitaNoch keine Bewertungen
- Nursing Care Plan For Tissue InjuryDokument2 SeitenNursing Care Plan For Tissue InjuryJobelle AcenaNoch keine Bewertungen
- Risk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.Dokument2 SeitenRisk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.eleinsamNoch keine Bewertungen
- Compartment Syndrome NCP (PAIN)Dokument2 SeitenCompartment Syndrome NCP (PAIN)eunica16Noch keine Bewertungen
- NCP Acute PainDokument3 SeitenNCP Acute PainSheene Lysethea Sioteco AguilosNoch keine Bewertungen
- NCP Acitivity IntoleranceDokument3 SeitenNCP Acitivity IntolerancegizelleNoch keine Bewertungen
- Disturbed Sleep Pattern Related To Environmental FactorsDokument9 SeitenDisturbed Sleep Pattern Related To Environmental Factorsalaisah dimaporoNoch keine Bewertungen
- Gout N C P BY BHERU LALDokument1 SeiteGout N C P BY BHERU LALBheru LalNoch keine Bewertungen
- Ineffective Airway Clearance - PTBDokument2 SeitenIneffective Airway Clearance - PTBIrish Eunice FelixNoch keine Bewertungen
- Acute GastroenteritisDokument2 SeitenAcute GastroenteritisErika CadawanNoch keine Bewertungen
- Nursingcrib Com NURSING CARE PLAN Hepatitis A PDFDokument2 SeitenNursingcrib Com NURSING CARE PLAN Hepatitis A PDFswapnilazarusNoch keine Bewertungen
- Nursing Care PlansDokument4 SeitenNursing Care Plansapi-19762967Noch keine Bewertungen
- Nursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NDokument2 SeitenNursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NnananaNoch keine Bewertungen
- NCPDokument9 SeitenNCPYesha Mae MartinNoch keine Bewertungen
- Surgical NCPDokument6 SeitenSurgical NCPAreeya SushmitaNoch keine Bewertungen
- Chronic Renal Failure Nursing Care PlanDokument6 SeitenChronic Renal Failure Nursing Care PlanRuva Oscass JimmyNoch keine Bewertungen
- Cholecystectomy Nursing Care Plan: Intraoperative Problem: Risk For AspirationDokument1 SeiteCholecystectomy Nursing Care Plan: Intraoperative Problem: Risk For AspirationJess GoNoch keine Bewertungen
- Nursing Care Plan 2Dokument2 SeitenNursing Care Plan 2Isabel Barredo Del MundoNoch keine Bewertungen
- NCP Acute Pain OB Ward PDFDokument2 SeitenNCP Acute Pain OB Ward PDFambiit25Noch keine Bewertungen
- Nursing Care Plan Rheumatoid ArthritisDokument3 SeitenNursing Care Plan Rheumatoid ArthritisJashAnia MarIe EvArdo FloresNoch keine Bewertungen
- Nursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleDokument8 SeitenNursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleTrysna Ayu SukardiNoch keine Bewertungen
- NCP For Ears Nose ThroatDokument1 SeiteNCP For Ears Nose ThroatMcmac YangoNoch keine Bewertungen
- NCP GCP FinalDokument15 SeitenNCP GCP FinalssilvozaNoch keine Bewertungen
- DP Discharge Plan@@@@@@@@Dokument6 SeitenDP Discharge Plan@@@@@@@@Maemae SumalinogNoch keine Bewertungen
- Actual Nursing Care Plan GT DisorderDokument3 SeitenActual Nursing Care Plan GT DisordermandzkievonnieNoch keine Bewertungen
- NCP Background, Demographic Data, Dordon's Functional Health, Drug Study SAint Louis UniversityDokument21 SeitenNCP Background, Demographic Data, Dordon's Functional Health, Drug Study SAint Louis Universitypa3kmedinaNoch keine Bewertungen
- NCP Imbalanced NutritionDokument7 SeitenNCP Imbalanced NutritionNora VarshavskiNoch keine Bewertungen
- Word Ncp.......... TetanusDokument6 SeitenWord Ncp.......... TetanusaianrNoch keine Bewertungen
- NCP GastroenteritisDokument1 SeiteNCP GastroenteritisFranchesca PaunganNoch keine Bewertungen
- NCP Pedia SleepapneaDokument2 SeitenNCP Pedia SleepapneaDavid Brillo100% (1)
- As Needed.: Environmental Stimuli 6Dokument4 SeitenAs Needed.: Environmental Stimuli 6Nicole GumolonNoch keine Bewertungen
- Goboy - Risk For Infection NCPDokument3 SeitenGoboy - Risk For Infection NCPLouise GermaineNoch keine Bewertungen
- NCPsDokument13 SeitenNCPsRocel DevillesNoch keine Bewertungen
- Pharmacologic Class: Contraindications: CNS: Headache, BeforeDokument4 SeitenPharmacologic Class: Contraindications: CNS: Headache, BeforeGwyn RosalesNoch keine Bewertungen
- NCPDokument4 SeitenNCPAnn AquinoNoch keine Bewertungen
- NCP Infection NewDokument3 SeitenNCP Infection NewXerxes DejitoNoch keine Bewertungen
- Assessment Nursing Diagnosis Rationale Desired Outcome Interventions Justification EvaluationDokument7 SeitenAssessment Nursing Diagnosis Rationale Desired Outcome Interventions Justification EvaluationPJNoch keine Bewertungen
- NCPDokument3 SeitenNCPJoevelyn LaynoNoch keine Bewertungen
- NCPDokument7 SeitenNCPAbbie TantengcoNoch keine Bewertungen
- NCP Klippel Trenaunay SyndromeDokument3 SeitenNCP Klippel Trenaunay SyndromePaola Marie VenusNoch keine Bewertungen
- College of Nursing and Allied Medical Sciences: WesleyanDokument3 SeitenCollege of Nursing and Allied Medical Sciences: WesleyanPrince Juzzel Banag100% (1)
- Nursing Care Plan For Low SelfDokument3 SeitenNursing Care Plan For Low SelfMarissa AsimNoch keine Bewertungen
- NCP 4Dokument1 SeiteNCP 4marohunkNoch keine Bewertungen
- Cell Ab ActivitiesDokument7 SeitenCell Ab ActivitiesJanelle Cabida Supnad100% (1)
- Hypovolemia (Fluid Deficit)Dokument2 SeitenHypovolemia (Fluid Deficit)Lyn Reyes100% (1)
- NCPDokument6 SeitenNCPAngelaTrinidadNoch keine Bewertungen
- NCP Close Complete Fracture Knowledge DeficitDokument2 SeitenNCP Close Complete Fracture Knowledge DeficitArt Christian Ramos0% (1)
- NCP Urine RetentionDokument4 SeitenNCP Urine RetentionKingJayson Pacman06Noch keine Bewertungen
- NCP Making (Ulcerative Colitis & Crohn's Disease)Dokument2 SeitenNCP Making (Ulcerative Colitis & Crohn's Disease)R Hornilla ArcegaNoch keine Bewertungen
- Skin IntegrityDokument2 SeitenSkin IntegrityJonica CamposNoch keine Bewertungen
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation SubjectiveDokument3 SeitenAssessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation SubjectiveDanica Kate GalleonNoch keine Bewertungen
- NCPDokument2 SeitenNCPsphinx809100% (2)
- Assessment Diagnosis Planning Intervention EvaluationDokument2 SeitenAssessment Diagnosis Planning Intervention EvaluationCharissa Magistrado De LeonNoch keine Bewertungen
- Drug Study 2Dokument10 SeitenDrug Study 2jedialecarceleryahooNoch keine Bewertungen
- CASE STUDY Intestinal ObstructionDokument68 SeitenCASE STUDY Intestinal ObstructionMaria Paula Bungay91% (22)
- Hypertension Nursing Care PlanDokument1 SeiteHypertension Nursing Care PlanSheila Mae Cabahug100% (1)
- BEN Final Case Study OSMAKDokument24 SeitenBEN Final Case Study OSMAKEunice CariasNoch keine Bewertungen
- Constipation NCPDokument2 SeitenConstipation NCPDemilyn Olofernes-Fat100% (1)
- 7 Gastroenteritis Nursing Care Plans - NurseslabsDokument8 Seiten7 Gastroenteritis Nursing Care Plans - NurseslabsHikaru Takishima91% (23)
- IV. Recognizing National Issues and Concern - E-Substance Abuse EducationDokument9 SeitenIV. Recognizing National Issues and Concern - E-Substance Abuse EducationMicsjadeCastillo0% (1)
- Scientific Book Jicccim 2018Dokument171 SeitenScientific Book Jicccim 2018ngwinda90Noch keine Bewertungen
- Eosinophil Biology and Causes of Eosinophilia - UpToDateDokument35 SeitenEosinophil Biology and Causes of Eosinophilia - UpToDateBls PriyaNoch keine Bewertungen
- Abc Abuso 1 PDFDokument6 SeitenAbc Abuso 1 PDFMDMNoch keine Bewertungen
- Onbeing Ill: by Virginia WoolfDokument14 SeitenOnbeing Ill: by Virginia Woolf馬思宇Noch keine Bewertungen
- Farmakologi Geriatri: Oleh: P. Santoso, S.Si.,M.Biomed, AptDokument40 SeitenFarmakologi Geriatri: Oleh: P. Santoso, S.Si.,M.Biomed, AptEva Dharma WahyuniNoch keine Bewertungen
- Burn NotesDokument4 SeitenBurn NotesRiza Angela BarazanNoch keine Bewertungen
- ComplianceDokument13 SeitenCompliancextremist2001Noch keine Bewertungen
- A Comprehensive Overview On Osteoporosis and Its Risk FactorsDokument21 SeitenA Comprehensive Overview On Osteoporosis and Its Risk Factorsdenta aeNoch keine Bewertungen
- Changes in Diet and Lifestyle and Long-Term Weight Gain in Women and MenDokument13 SeitenChanges in Diet and Lifestyle and Long-Term Weight Gain in Women and MenemanvitoriaNoch keine Bewertungen
- About Monkey PoxDokument3 SeitenAbout Monkey PoxObakoma Josiah100% (1)
- 5.ICMR ProjectsDokument10 Seiten5.ICMR ProjectsVishnu Praba ANoch keine Bewertungen
- PronounDokument8 SeitenPronounGhulam NabiNoch keine Bewertungen
- Referentne Laboratorije Engleski Jan2021Dokument5 SeitenReferentne Laboratorije Engleski Jan2021Laki SreckoNoch keine Bewertungen
- League of Nations SuccessDokument12 SeitenLeague of Nations SuccessMubaiwaNoch keine Bewertungen
- Symptoms of ColitisDokument5 SeitenSymptoms of ColitisChatrina TandiloloNoch keine Bewertungen
- Legal Aid Society Complaint Re Homeless YouthDokument65 SeitenLegal Aid Society Complaint Re Homeless YouthPaul SchindlerNoch keine Bewertungen
- Key Points: Information About Your Procedure From The British Association of Urological Surgeons (BAUS)Dokument6 SeitenKey Points: Information About Your Procedure From The British Association of Urological Surgeons (BAUS)diva aurelliaNoch keine Bewertungen
- BangkasDokument5 SeitenBangkasJulianne BangkasNoch keine Bewertungen
- 3 Most Common Biochemical ImbalancesDokument4 Seiten3 Most Common Biochemical Imbalancescarlos100% (1)
- Stroke - Final ReportDokument16 SeitenStroke - Final ReportgolokipokNoch keine Bewertungen
- Pancreatic Cancer - Case AnalysisDokument37 SeitenPancreatic Cancer - Case AnalysisMavy CantonNoch keine Bewertungen
- DR Antonious CV N & AEDokument27 SeitenDR Antonious CV N & AEdoctorantoniNoch keine Bewertungen
- CREW: Department of Veterans Affairs: Regarding PTSD Diagnosis: Quick Referenec To Laws and Regulatinos Relating To Psychiactric DisordersDokument30 SeitenCREW: Department of Veterans Affairs: Regarding PTSD Diagnosis: Quick Referenec To Laws and Regulatinos Relating To Psychiactric DisordersCREWNoch keine Bewertungen
- NCP OsteosarcomaDokument6 SeitenNCP OsteosarcomaNiksNoch keine Bewertungen
- Scheduling: IndiaDokument5 SeitenScheduling: IndiaCristinaNoch keine Bewertungen
- Unit 7.VARIETY OF LIFEDokument120 SeitenUnit 7.VARIETY OF LIFEPika PiNoch keine Bewertungen
- Endometriosis: Endometriosis: Symptoms, Treatment, DiagnosisDokument4 SeitenEndometriosis: Endometriosis: Symptoms, Treatment, DiagnosisrizkiaautikasariNoch keine Bewertungen
- 2009 Fee ScheduleDokument1.123 Seiten2009 Fee ScheduleNicole HillNoch keine Bewertungen
- Chapter 7. CirculationDokument54 SeitenChapter 7. CirculationankurbiologyNoch keine Bewertungen